Abstract
Research over the past 30 years has identified mechanistic biochemical oxidation pathways that contribute to asthma pathophysiology. Redox imbalance is present in asthma and strongly linked to the pathobiology of airflow obstruction, airway hyperreactivity, and remodeling. High levels of reactive oxygen species, reactive nitrogen species, and oxidatively modified proteins in the lung, blood, and urine provide conclusive evidence for pathologic oxidation in asthma. Concurrent loss of antioxidants, such as superoxide dismutases and catalase, is attributed to redox modifications of the enzymes, and further amplifies the oxidative injury in the airway. The presence of high levels of urine bromotyrosine, an oxidation product of eosinophil peroxidase, identifies activated eosinophils, and shows promise for use as a noninvasive biomarker of poor asthma control.
Keywords: asthma, eosinophil, oxidants, nitric oxide, superoxide dismutase
A wealth of studies point to an immunologic genesis of asthmatic airway inflammation, but, ultimately, most effector cells produce reactive oxygen species (ROS) and reactive nitrogen species (RNS), which produce pathophysiologic outcomes of airway reactivity, injury, and remodeling (1–4). This article summarizes information on oxidant biology that was presented at the Thomas L. Petty Lecture at the Thomas L. Petty Aspen Lung 2015 Conference. Comprehensive overview of oxidative processes in asthma can be found in work by Comhair and colleagues (5) and Ghosh and colleagues (6, 7).
ROS in Asthma
Enhanced oxidant production is well documented in asthma. Mitochondria are the primary intracellular source of superoxide generation under normal physiologic states (8), but high levels of superoxide can be formed by the reduced nicotinamide adenine dinucleotide phosphate (NADPH) oxidases that are found in granulocytes, including neutrophils and eosinophils (9–12). High levels of hydrogen peroxide can also be formed by NADPH oxidases, Duox1 and -2, expressed in bronchial epithelial cells upon activation by histamine binding to cell-surface receptor (13). Eosinophils and/or neutrophils are present in increased numbers in airways of subjects with asthma and produce much more ROS than in cells found in healthy lungs (14–22). Early studies showed that the amount of ROS generated by eosinophils and/or neutrophils is directly correlated to the severity of hyperreactivity in patients with asthma (16, 21, 23). Experimental exposure of subjects with atopic asthma to allergen, or asthma exacerbations, lead to even greater amounts of superoxide (16, 24), with airspace cells in subjects with asthma producing up to 8 × 106 nmol superoxide/million cells/h (16, 25).
Bromotyrosine, a Biomarker of the Activated Eosinophil
Eosinophils are cellular biomarkers of atopic, or Th2-high, asthma (26–29, 30–33). Activated eosinophils degranulate to release major basic protein, eosinophilic cation protein, and eosinophil peroxidase (EPO) (26–29, 34). EPO is one of the mammalian peroxidase superfamily, which also includes myeloperoxidase (MPO), lactoperoxidase, thyroid peroxidase, and prostaglandin H synthase. All use peroxide for the oxidizing equivalents for catalysis (35). MPO is present in neutrophils and monocytes, and secreted during cell activation (35). EPO and MPO both use hydrogen peroxide to oxidize thiocyanate (36, 37). MPO may also use bromide and chloride as substrates, but at plasma levels of halides, MPO uses chloride over 500-fold more than bromide (38, 39). On the other hand, EPO can use bromide, but cannot use chloride as a substrate. Multiple studies of various inflammation models using either MPO-knockout or EPO-knockout mice confirm consistently that bromotyrosine generation in vivo is absent or reduced to virtually nondetectable levels in the EPO-knockout mouse, and chlorotyrosine formation is absent in the MPO-knockout mouse (40, 41). Thus, chlorotyrosine is specific for MPO, and bromotyrosine is highly selective for EPO in vivo (4, 42–45). Bromotyrosine is found at high levels in asthmatic airways and increases with asthma exacerbations (43, 46). Bromotyrosine is stable and excreted in urine, where it can be quantitated and used as a biomarker of the activated eosinophil (42, 47). Urine bromotyrosine levels increase during asthma exacerbation (42), and the presence of high levels of urine bromotyrosine identifies subjects with asthma with poor control, or at risk of exacerbation (48, 49)
Nitric Oxide and Airway Inflammation
In addition to ROS, RNS are also increased in asthma. Nitric oxide (NO) is higher in asthmatic airways as compared with nonasthmatic airways (1, 3, 50, 51). Measurement of the fraction of exhaled NO (FeNO) is a sensitive biomarker of airway inflammation (52–57), and was approved by the U.S. Food and Drug Administration for evaluation of antiinflammatory treatment responses in asthma (57–62). NO synthases (NOSs) produce NO by converting L-arginine to L-citrulline (63). The inducible NOS (iNOS; NOS2) is induced by cytokines, including IFN-γ, IL-1β, TNF-α, IL-4 and/or IL-13 (63–65). The Th2 cytokines are not essential for iNOS expression; hence, FeNO does not perfectly correlate with Th2 biomarkers, such as eosinophils or bromotyrosine (66). The higher-than-normal FeNO in asthma is associated with greater transcriptional activation of the NOS2 gene and iNOS protein expression (3, 64, 67, 68). The signal transduction effects of NO are classically related to binding to guanyl cyclases, but its byproducts also have biologic effects. NO reacts with oxygen or ROS to form nitrite, nitrate, and RNS, such as peroxynitrite. The addition of NO to thiol residues (nitrosothiol) is called nitrosation, and can alter function and/or structure of proteins (69–71). NO addition to tyrosyl residues (nitrotyrosine) is termed nitration, and occurs in the setting of increased RNS. Nitration usually leads to inactivation of proteins (72–75). EPO may use nitrite for nitration of protein-bound tyrosyl residues (76); in fact, up to 70% of nitrotyrosine formed in the murine asthma model is produced by EPO (40). Studies show that subjects with well controlled asthma have higher levels than individuals without asthma of airway NO, nitrate, and nitrotyrosine, and very low levels of S-nitrosothiols (1, 77). Nitrotyrosine is present at very high levels in airways of patients during asthma attacks (4, 78, 79). Unbiased metabolomic profiling has recently revealed a unique NO-associated endotype of asthma typified by changes in taurine transport and bile acid metabolism, which are known systemic effects of NO (80).
Redox Abnormalities in Asthma
The lung has a wide variety of antioxidants (e.g., glutathione, catalase, and superoxide dismutases (SODs) (81), but increased ROS and RNS in asthma overcome antioxidant defenses (5, 82). Airways of individuals with asthma have higher-than-normal levels of glutathione. Maintenance of the optimal intracellular thiol/dithiol redox ratio is important to cell functions and survival. Protein cysteinyl thiols are susceptible to oxidation, and cells can resist oxidation of thiols by protein thiolation (83), particularly with glutathione to generate S-glutathionyated proteins (i.e., mixed disulfides) (84). Recent work suggests alterations in glutathionylation in asthmatic airways (85, 86). The intracellular redox in asthmatic airway cells appears to be shifted to greater intracellular reducing potential, with higher ratio of the reduced-to-oxidized glutathione (87), perhaps as a response to the repetitive oxidative stress (2). Recently, quantitative nuclear imaging using the radiopharmaceutical, [99 mTc-exametazime (HMPAO)], which is retained in tissues dependent on intracellular reduced glutathione levels, confirmed a greater intracellular reducing potential in asthma in vivo, and predominantly in lower central regions of the lungs (88).
Redox-Mediated Loss of Antioxidant Activities
In addition to greater ROS and RNS, asthmatic lungs have lower-than-normal SOD and catalase activities (2, 77, 87, 89–91). The loss of SOD is associated with more severe airflow obstruction and greater airway hyperreactivity and remodeling (2, 5, 89–91, 92). The redox thiol/dithiol imbalance in asthma results in systemic change in cytosolic copper-zinc SOD (CuZnSOD), such that CuZnSOD is susceptible to autoinactivation by hydrogen peroxide (2, 5, 89–91, 92, 93). On the other hand, the decrease in mitochondrial manganese SOD (MnSOD) activity is associated with nitration of tyrosyl residues in the protein (2, 91). Similarly, catalase activity is decreased in the asthmatic airway in association with increased oxidation of specific tyrosyl residues in the protein (77). Murine asthma models verify a mechanistic role of SOD loss in pathophysiology of asthma. The CuZnSOD transgenic mice have less airway inflammation and hyperreactivity in comparison to wild-type mice in a murine asthma model (94). In human studies, exposure to second hand smoke is associated with even lower levels of serum SOD in asthma, and, overall, more severe asthma (93). Increased ROS in asthma is usually attributed to leukocyte activation, but murine models of asthma also point to metabolic–mitochondrial origins of greater ROS in the asthmatic airway smooth muscle (95). Subjects with asthma who were provided coenzyme Q, an essential component of mitochondrial electron transport chain and a mitochondrial antioxidant (96), recovered SOD activity and redox thiol balance to healthy, nonasthmatic levels (97).
Conclusions
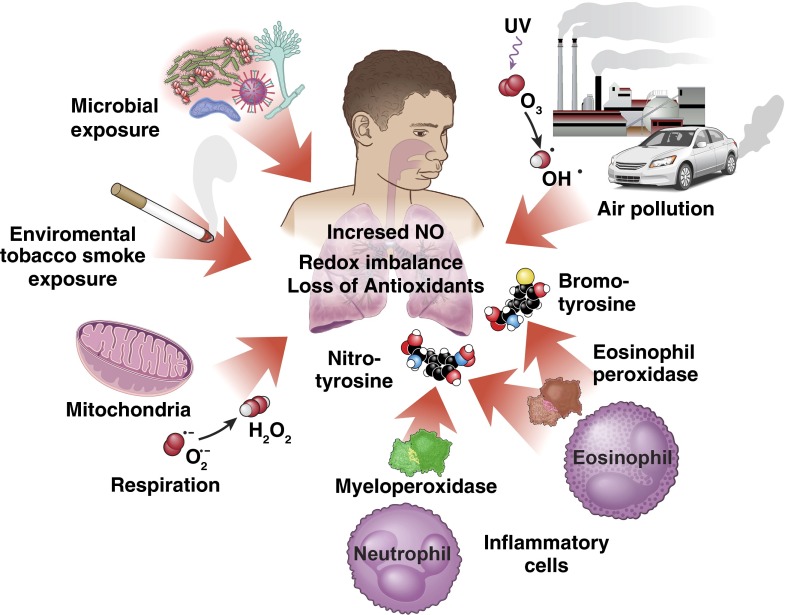
Altogether, the inflammation in asthma is defined by oxidant biology and alterations of airway redox (Figure 1). Redox abnormalities are amplified by infections, exposure to pollutants, and/or allergen in subjects with atopic asthma. EPO-mediated reactions produce high levels of brominating and oxidizing species that damage proteins. High levels of NO production and reactive nitrogen oxides contribute to the oxidant pathophysiology. Loss of enzymic antioxidant activities further fuels redox disturbances and injury to the airway. Future studies to develop noninvasive signature biochemical biomarkers of oxidative pathways, and/or to design therapies targeting redox mechanisms to limit formation of damaging oxidant species, may be useful to provide optimal care of the patient with asthma.
Figure 1.
Oxidant biology in asthma. Reactive oxygen and nitrogen species and proteins oxidatively modified by nitration and/or bromination are increased in asthma. The higher levels of oxidants are generated endogenously by inflammatory cells and epithelial cells, and amplified by inhalational exposure to microbes, allergens, pollutants, and environmental tobacco smoke. Loss of antioxidants and alterations in thiol/dithiol balance further augment pathologic oxidative processes. NO = nitric oxide.
Footnotes
Supported, in part, by National Heart, Lung, and Blood Institute grants HL081064, HL103453, and HL109250, and by the Alfred Lerner Chair for Biomedical Research.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Dweik RA, Comhair SA, Gaston B, Thunnissen FB, Farver C, Thomassen MJ, Kavuru M, Hammel J, Abu-Soud HM, Erzurum SC. NO chemical events in the human airway during the immediate and late antigen-induced asthmatic response. Proc Natl Acad Sci USA. 2001;98:2622–2627. doi: 10.1073/pnas.051629498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Comhair SA, Bhathena PR, Dweik RA, Kavuru M, Erzurum SC. Rapid loss of superoxide dismutase activity during antigen-induced asthmatic response. Lancet. 2000;355:624. doi: 10.1016/S0140-6736(99)04736-4. [DOI] [PubMed] [Google Scholar]
- 3.Guo FH, Comhair SA, Zheng S, Dweik RA, Eissa NT, Thomassen MJ, Calhoun W, Erzurum SC. Molecular mechanisms of increased nitric oxide (NO) in asthma: evidence for transcriptional and post-translational regulation of NO synthesis. J Immunol. 2000;164:5970–5980. doi: 10.4049/jimmunol.164.11.5970. [DOI] [PubMed] [Google Scholar]
- 4.MacPherson JC, Comhair SA, Erzurum SC, Klein DF, Lipscomb MF, Kavuru MS, Samoszuk MK, Hazen SL. Eosinophils are a major source of nitric oxide-derived oxidants in severe asthma: characterization of pathways available to eosinophils for generating reactive nitrogen species. J Immunol. 2001;166:5763–5772. doi: 10.4049/jimmunol.166.9.5763. [DOI] [PubMed] [Google Scholar]
- 5.Comhair SA, Erzurum SC. Redox control of asthma: molecular mechanisms and therapeutic opportunities. Antioxid Redox Signal. 2010;12:93–124. doi: 10.1089/ars.2008.2425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ghosh S, Erzurum SC. Nitric oxide metabolism in asthma pathophysiology. Biochim Biophys Acta. 2011;1810:1008–1016. doi: 10.1016/j.bbagen.2011.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ghosh S, Erzurum SC. Modulation of asthma pathogenesis by nitric oxide pathways and therapeutic opportunities. Drug Discov Today Dis Mech. 2012;9:e89–e94. doi: 10.1016/j.ddmec.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Halliwell B. Free radicals, antioxidants, and human disease: curiosity, cause, or consequence? Lancet. 1994;344:721–724. doi: 10.1016/s0140-6736(94)92211-x. [DOI] [PubMed] [Google Scholar]
- 9.Conner EM, Grisham MB. Inflammation, free radicals, and antioxidants. Nutrition. 1996;12:274–277. doi: 10.1016/s0899-9007(96)00000-8. [DOI] [PubMed] [Google Scholar]
- 10.Chance B, Sies H, Boveris A. Hydroperoxide metabolism in mammalian organs. Physiol Rev. 1979;59:527–605. doi: 10.1152/physrev.1979.59.3.527. [DOI] [PubMed] [Google Scholar]
- 11.Babior BM. Oxygen-dependent microbial killing by phagocytes (second of two parts) N Engl J Med. 1978;298:721–725. doi: 10.1056/NEJM197803302981305. [DOI] [PubMed] [Google Scholar]
- 12.Davies KJ. Oxidative stress: the paradox of aerobic life. Biochem Soc Symp. 1995;61:1–31. doi: 10.1042/bss0610001. [DOI] [PubMed] [Google Scholar]
- 13.Rada B, Boudreau HE, Park JJ, Leto TL. Histamine stimulates hydrogen peroxide production by bronchial epithelial cells via histamine H1 receptor and dual oxidase. Am J Respir Cell Mol Biol. 2014;50:125–134. doi: 10.1165/rcmb.2013-0254OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Busse WW, Horwitz RJ, Reed CE.Asthma: definition and pathogenesisInMiddleton E, Jr, Reed CE, Ellis EF, Adkinson NF, Jr, Yunginger JW, Busse WW.Allergy: principles and practice 5th ed.St. Louis: Mosby-Year Book; 1998838–858. [Google Scholar]
- 15.Busse W, Elias J, Sheppard D, Banks-Schlegel S. Airway remodeling and repair. Am J Respir Crit Care Med. 1999;160:1035–1042. doi: 10.1164/ajrccm.160.3.9902064. [DOI] [PubMed] [Google Scholar]
- 16.Calhoun WJ, Reed HE, Moest DR, Stevens CA. Enhanced superoxide production by alveolar macrophages and air-space cells, airway inflammation, and alveolar macrophage density changes after segmental antigen bronchoprovocation in allergic subjects. Am Rev Respir Dis. 1992;145:317–325. doi: 10.1164/ajrccm/145.2_Pt_1.317. [DOI] [PubMed] [Google Scholar]
- 17.Jarjour NN, Calhoun WJ. Enhanced production of oxygen radicals in asthma. J Lab Clin Med. 1994;123:131–136. [PubMed] [Google Scholar]
- 18.Jarjour NN, Busse WW, Calhoun WJ. Enhanced production of oxygen radicals in nocturnal asthma. Am Rev Respir Dis. 1992;146:905–911. doi: 10.1164/ajrccm/146.4.905. [DOI] [PubMed] [Google Scholar]
- 19.Hoshino T, Okamoto M, Takei S, Sakazaki Y, Iwanaga T, Aizawa H. Redox-regulated mechanisms in asthma. Antioxid Redox Signal. 2008;10:769–783. doi: 10.1089/ars.2007.1936. [DOI] [PubMed] [Google Scholar]
- 20.Sedgwick JB, Calhoun WJ, Vrtis RF, Bates ME, McAllister PK, Busse WW. Comparison of airway and blood eosinophil function after in vivo antigen challenge. J Immunol. 1992;149:3710–3718. [PubMed] [Google Scholar]
- 21.Postma DS, Renkema TE, Noordhoek JA, Faber H, Sluiter HJ, Kauffman H. Association between nonspecific bronchial hyperreactivity and superoxide anion production by polymorphonuclear leukocytes in chronic air-flow obstruction. Am Rev Respir Dis. 1988;137:57–61. doi: 10.1164/ajrccm/137.1.57. [DOI] [PubMed] [Google Scholar]
- 22.Bast A, Haenen GR, Doelman CJ. Oxidants and antioxidants: state of the art. Am J Med. 1991;91:2S–13S. doi: 10.1016/0002-9343(91)90278-6. [DOI] [PubMed] [Google Scholar]
- 23.Sanders SP. Nitric oxide in asthma: pathogenic, therapeutic, or diagnostic? Am J Respir Cell Mol Biol. 1999;21:147–149. doi: 10.1165/ajrcmb.21.2.f158. [DOI] [PubMed] [Google Scholar]
- 24.Sanders SP, Zweier JL, Harrison SJ, Trush MA, Rembish SJ, Liu MC. Spontaneous oxygen radical production at sites of antigen challenge in allergic subjects. Am J Respir Crit Care Med. 1995;151:1725–1733. doi: 10.1164/ajrccm.151.6.7767513. [DOI] [PubMed] [Google Scholar]
- 25.Comhair SA, Bhathena PR, Farver C, Thunnissen FB, Erzurum SC. Extracellular glutathione peroxidase induction in asthmatic lungs: evidence for redox regulation of expression in human airway epithelial cells. FASEB J. 2001;15:70–78. doi: 10.1096/fj.00-0085com. [DOI] [PubMed] [Google Scholar]
- 26.Wardlaw AJ. Eosinophils in the 1990s: new perspectives on their role in health and disease. Postgrad Med J. 1994;70:536–552. doi: 10.1136/pgmj.70.826.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Horwitz RJ, Busse WW. Inflammation and asthma. Clin Chest Med. 1995;16:583–602. [PubMed] [Google Scholar]
- 28.Gleich GJ, Ottesen EA, Leiferman KM, Ackerman SJ. Eosinophils and human disease. Int Arch Allergy Appl Immunol. 1989;88:59–62. doi: 10.1159/000234749. [DOI] [PubMed] [Google Scholar]
- 29.Bousquet J, Jeffery PK, Busse WW, Johnson M, Vignola AM. Asthma: from bronchoconstriction to airways inflammation and remodeling. Am J Respir Crit Care Med. 2000;161:1720–1745. doi: 10.1164/ajrccm.161.5.9903102. [DOI] [PubMed] [Google Scholar]
- 30.Bousquet J, Van Vyve T, Chanez P, Enander I, Michel FB, Godard P. Cells and mediators in bronchoalveolar lavage of asthmatic patients: the example of eosinophilic inflammation. Allergy. 1993;48(17) Suppl:70–75. doi: 10.1111/j.1398-9995.1993.tb04703.x. discussion 76. [DOI] [PubMed] [Google Scholar]
- 31.Griffin E, Håkansson L, Formgren H, Jörgensen K, Peterson C, Venge P. Blood eosinophil number and activity in relation to lung function in patients with asthma and with eosinophilia. J Allergy Clin Immunol. 1991;87:548–557. doi: 10.1016/0091-6749(91)90014-f. [DOI] [PubMed] [Google Scholar]
- 32.Sanz ML, Parra A, Prieto I, Diéguez I, Oehling AK. Serum eosinophil peroxidase (EPO) levels in asthmatic patients. Allergy. 1997;52:417–422. doi: 10.1111/j.1398-9995.1997.tb01021.x. [DOI] [PubMed] [Google Scholar]
- 33.Wardlaw AJ, Dunnette S, Gleich GJ, Collins JV, Kay AB. Eosinophils and mast cells in bronchoalveolar lavage in subjects with mild asthma: relationship to bronchial hyperreactivity. Am Rev Respir Dis. 1988;137:62–69. doi: 10.1164/ajrccm/137.1.62. [DOI] [PubMed] [Google Scholar]
- 34.Hamann KJ, Strek ME, Baranowski SL, Munoz NM, Williams FS, White SR, Vita A, Leff AR. Effects of activated eosinophils cultured from human umbilical cord blood on guinea pig trachealis. Am J Physiol. 1993;265:L301–L307. doi: 10.1152/ajplung.1993.265.3.L301. [DOI] [PubMed] [Google Scholar]
- 35.Klebanoff SJCRA.The neutrophil: function and clinical disorders. Amsterdam: Elsevier/North Holland Biomedical Press; 1978
- 36.Arlandson M, Decker T, Roongta VA, Bonilla L, Mayo KH, MacPherson JC, Hazen SL, Slungaard A. Eosinophil peroxidase oxidation of thiocyanate: characterization of major reaction products and a potential sulfhydryl-targeted cytotoxicity system. J Biol Chem. 2001;276:215–224. doi: 10.1074/jbc.M004881200. [DOI] [PubMed] [Google Scholar]
- 37.Wang Z, Nicholls SJ, Rodriguez ER, Kummu O, Hörkkö S, Barnard J, Reynolds WF, Topol EJ, DiDonato JA, Hazen SL. Protein carbamylation links inflammation, smoking, uremia and atherogenesis. Nat Med. 2007;13:1176–1184. doi: 10.1038/nm1637. [DOI] [PubMed] [Google Scholar]
- 38.van Dalen CJ, Kettle AJ. Substrates and products of eosinophil peroxidase. Biochem J. 2001;358:233–239. doi: 10.1042/0264-6021:3580233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.van Dalen CJ, Whitehouse MW, Winterbourn CC, Kettle AJ. Thiocyanate and chloride as competing substrates for myeloperoxidase. Biochem J. 1997;327:487–492. doi: 10.1042/bj3270487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brennan ML, Wu W, Fu X, Shen Z, Song W, Frost H, Vadseth C, Narine L, Lenkiewicz E, Borchers MT, et al. A tale of two controversies: defining both the role of peroxidases in nitrotyrosine formation in vivo using eosinophil peroxidase and myeloperoxidase-deficient mice, and the nature of peroxidase-generated reactive nitrogen species. J Biol Chem. 2002;277:17415–17427. doi: 10.1074/jbc.M112400200. [DOI] [PubMed] [Google Scholar]
- 41.Denzler KL, Borchers MT, Crosby JR, Cieslewicz G, Hines EM, Justice JP, Cormier SA, Lindenberger KA, Song W, Wu W, et al. Extensive eosinophil degranulation and peroxidase-mediated oxidation of airway proteins do not occur in a mouse ovalbumin-challenge model of pulmonary inflammation. J Immunol. 2001;167:1672–1682. doi: 10.4049/jimmunol.167.3.1672. [DOI] [PubMed] [Google Scholar]
- 42.Wu W, Chen Y, d’Avignon A, Hazen SL. 3-Bromotyrosine and 3,5-dibromotyrosine are major products of protein oxidation by eosinophil peroxidase: potential markers for eosinophil-dependent tissue injury in vivo. Biochemistry. 1999;38:3538–3548. doi: 10.1021/bi982401l. [DOI] [PubMed] [Google Scholar]
- 43.Wu W, Samoszuk MK, Comhair SA, Thomassen MJ, Farver CF, Dweik RA, Kavuru MS, Erzurum SC, Hazen SL. Eosinophils generate brominating oxidants in allergen-induced asthma. J Clin Invest. 2000;105:1455–1463. doi: 10.1172/JCI9702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brennan ML, Hazen SL. Amino acid and protein oxidation in cardiovascular disease. Amino Acids. 2003;25:365–374. doi: 10.1007/s00726-003-0023-y. [DOI] [PubMed] [Google Scholar]
- 45.Mitra SN, Slungaard A, Hazen SL. Role of eosinophil peroxidase in the origins of protein oxidation in asthma. Redox Rep. 2000;5:215–224. doi: 10.1179/135100000101535771. [DOI] [PubMed] [Google Scholar]
- 46.Aldridge RE, Chan T, van Dalen CJ, Senthilmohan R, Winn M, Venge P, Town GI, Kettle AJ. Eosinophil peroxidase produces hypobromous acid in the airways of stable asthmatics. Free Radic Biol Med. 2002;33:847–856. doi: 10.1016/s0891-5849(02)00976-0. [DOI] [PubMed] [Google Scholar]
- 47.Mita H, Higashi N, Taniguchi M, Higashi A, Kawagishi Y, Akiyama K. Urinary 3-bromotyrosine and 3-chlorotyrosine concentrations in asthmatic patients: lack of increase in 3-bromotyrosine concentration in urine and plasma proteins in aspirin-induced asthma after intravenous aspirin challenge. Clin Exp Allergy. 2004;34:931–938. doi: 10.1111/j.1365-2222.2004.01968.x. [DOI] [PubMed] [Google Scholar]
- 48.Wedes SH, Wu W, Comhair SA, McDowell KM, DiDonato JA, Erzurum SC, Hazen SL. Urinary bromotyrosine measures asthma control and predicts asthma exacerbations in children. J Pediatr. 2011;159:248–255.e241. doi: 10.1016/j.jpeds.2011.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wedes SH, Khatri SB, Zhang R, Wu W, Comhair SA, Wenzel S, Teague WG, Israel E, Erzurum SC, Hazen SL. Noninvasive markers of airway inflammation in asthma. Clin Transl Sci. 2009;2:112–117. doi: 10.1111/j.1752-8062.2009.00095.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Persson MG, Zetterström O, Agrenius V, Ihre E, Gustafsson LE. Single-breath nitric oxide measurements in asthmatic patients and smokers. Lancet. 1994;343:146–147. doi: 10.1016/s0140-6736(94)90935-0. [DOI] [PubMed] [Google Scholar]
- 51.Dweik RA, Laskowski D, Abu-Soud HM, Kaneko F, Hutte R, Stuehr DJ, Erzurum SC. Nitric oxide synthesis in the lung: regulation by oxygen through a kinetic mechanism. J Clin Invest. 1998;101:660–666. doi: 10.1172/JCI1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kharitonov SA, Yates D, Robbins RA, Logan-Sinclair R, Shinebourne EA, Barnes PJ. Increased nitric oxide in exhaled air of asthmatic patients. Lancet. 1994;343:133–135. doi: 10.1016/s0140-6736(94)90931-8. [DOI] [PubMed] [Google Scholar]
- 53.Ricciardolo FL, Gaston B, Hunt J. Acid stress in the pathology of asthma. J Allergy Clin Immunol. 2004;113:610–619. doi: 10.1016/j.jaci.2003.12.034. [DOI] [PubMed] [Google Scholar]
- 54.Smith AD, Cowan JO, Brassett KP, Herbison GP, Taylor DR. Use of exhaled nitric oxide measurements to guide treatment in chronic asthma. N Engl J Med. 2005;352:2163–2173. doi: 10.1056/NEJMoa043596. [DOI] [PubMed] [Google Scholar]
- 55.Dinakar C. Exhaled nitric oxide in pediatric asthma. Curr Allergy Asthma Rep. 2009;9:30–37. doi: 10.1007/s11882-009-0005-6. [DOI] [PubMed] [Google Scholar]
- 56.Nordvall SL, Janson C, Kalm-Stephens P, Foucard T, Torén K, Alving K. Exhaled nitric oxide in a population-based study of asthma and allergy in schoolchildren. Allergy. 2005;60:469–475. doi: 10.1111/j.1398-9995.2005.00735.x. [DOI] [PubMed] [Google Scholar]
- 57.Silkoff PE, Carlson M, Bourke T, Katial R, Ogren E, Szefler SJ. The aerocrine exhaled nitric oxide monitoring system NIOX is cleared by the US Food and Drug Administration for monitoring therapy in asthma. J Allergy Clin Immunol. 2004;114:1241–1256. doi: 10.1016/j.jaci.2004.08.042. [DOI] [PubMed] [Google Scholar]
- 58.Massaro AF, Mehta S, Lilly CM, Kobzik L, Reilly JJ, Drazen JM. Elevated nitric oxide concentrations in isolated lower airway gas of asthmatic subjects. Am J Respir Crit Care Med. 1996;153:1510–1514. doi: 10.1164/ajrccm.153.5.8630594. [DOI] [PubMed] [Google Scholar]
- 59.Silkoff PE, Sylvester JT, Zamel N, Permutt S. Airway nitric oxide diffusion in asthma: role in pulmonary function and bronchial responsiveness. Am J Respir Crit Care Med. 2000;161:1218–1228. doi: 10.1164/ajrccm.161.4.9903111. [DOI] [PubMed] [Google Scholar]
- 60.Mehta S, Lilly CM, Rollenhagen JE, Haley KJ, Asano K, Drazen JM. Acute and chronic effects of allergic airway inflammation on pulmonary nitric oxide production. Am J Physiol. 1997;272:L124–L131. doi: 10.1152/ajplung.1997.272.1.L124. [DOI] [PubMed] [Google Scholar]
- 61.Kharitonov SA, O’Connor BJ, Evans DJ, Barnes PJ. Allergen-induced late asthmatic reactions are associated with elevation of exhaled nitric oxide. Am J Respir Crit Care Med. 1995;151:1894–1899. doi: 10.1164/ajrccm.151.6.7767537. [DOI] [PubMed] [Google Scholar]
- 62.Khatri SB, Ozkan M, McCarthy K, Laskowski D, Hammel J, Dweik RA, Erzurum SC. Alterations in exhaled gas profile during allergen-induced asthmatic response. Am J Respir Crit Care Med. 2001;164:1844–1848. doi: 10.1164/ajrccm.164.10.2106119. [DOI] [PubMed] [Google Scholar]
- 63.Stuehr DJ. Mammalian nitric oxide synthases. Biochim Biophys Acta. 1999;1411:217–230. doi: 10.1016/s0005-2728(99)00016-x. [DOI] [PubMed] [Google Scholar]
- 64.Guo FH, Uetani K, Haque SJ, Williams BR, Dweik RA, Thunnissen FB, Calhoun W, Erzurum SC. Interferon gamma and interleukin 4 stimulate prolonged expression of inducible nitric oxide synthase in human airway epithelium through synthesis of soluble mediators. J Clin Invest. 1997;100:829–838. doi: 10.1172/JCI119598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chibana K, Trudeau JB, Mustovich AT, Hu H, Zhao J, Balzar S, Chu HW, Wenzel SE. IL-13 induced increases in nitrite levels are primarily driven by increases in inducible nitric oxide synthase as compared with effects on arginases in human primary bronchial epithelial cells. Clin Exp Allergy. 2008;38:936–946. doi: 10.1111/j.1365-2222.2008.02969.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cowan DC, Taylor DR, Peterson LE, Cowan JO, Palmay R, Williamson A, Hammel J, Erzurum SC, Hazen SL, Comhair SA. Biomarker-based asthma phenotypes of corticosteroid response. J Allergy Clin Immunol. 2015;135:877–883.e871. doi: 10.1016/j.jaci.2014.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Grasemann H, Yandava CN, Storm van’s Gravesande K, Deykin A, Pillari A, Ma J, Sonna LA, Lilly C, Stampfer MJ, Israel E, et al. A neuronal NO synthase (NOS1) gene polymorphism is associated with asthma. Biochem Biophys Res Commun. 2000;272:391–394. doi: 10.1006/bbrc.2000.2794. [DOI] [PubMed] [Google Scholar]
- 68.Guo FH, Erzurum SC. Characterization of inducible nitric oxide synthase expression in human airway epithelium. Environ Health Perspect. 1998;106:1119–1124. doi: 10.1289/ehp.98106s51119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Molina y Vedia L, McDonald B, Reep B, Brüne B, Di Silvio M, Billiar TR, Lapetina EG. Nitric oxide–induced S-nitrosylation of glyceraldehyde-3-phosphate dehydrogenase inhibits enzymatic activity and increases endogenous ADP-ribosylation. J Biol Chem. 1992;267:24929–24932. [PubMed] [Google Scholar]
- 70.Liu L, Hausladen A, Zeng M, Que L, Heitman J, Stamler JS. A metabolic enzyme for S-nitrosothiol conserved from bacteria to humans. Nature. 2001;410:490–494. doi: 10.1038/35068596. [DOI] [PubMed] [Google Scholar]
- 71.Reynaert NL, Ckless K, Korn SH, Vos N, Guala AS, Wouters EF, van der Vliet A, Janssen-Heininger YM. Nitric oxide represses inhibitory kappaB kinase through S-nitrosylation. Proc Natl Acad Sci USA. 2004;101:8945–8950. doi: 10.1073/pnas.0400588101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Crow JP, Beckman JS. Reactions between nitric oxide, superoxide, and peroxynitrite: footprints of peroxynitrite in vivo. Adv Pharmacol. 1995;34:17–43. doi: 10.1016/s1054-3589(08)61079-0. [DOI] [PubMed] [Google Scholar]
- 73.Freeman BA, White CR, Gutierrez H, Paler-Martínez A, Tarpey MM, Rubbo H. Oxygen radical–nitric oxide reactions in vascular diseases. Adv Pharmacol. 1995;34:45–69. doi: 10.1016/s1054-3589(08)61080-7. [DOI] [PubMed] [Google Scholar]
- 74.Radi R, Denicola A, Freeman BA. Peroxynitrite reactions with carbon dioxide–bicarbonate. Methods Enzymol. 1999;301:353–367. doi: 10.1016/s0076-6879(99)01099-x. [DOI] [PubMed] [Google Scholar]
- 75.Rochelle LG, Fischer BM, Adler KB. Concurrent production of reactive oxygen and nitrogen species by airway epithelial cells in vitro. Free Radic Biol Med. 1998;24:863–868. doi: 10.1016/s0891-5849(97)00375-4. [DOI] [PubMed] [Google Scholar]
- 76.Wu W, Chen Y, Hazen SL. Eosinophil peroxidase nitrates protein tyrosyl residues: implications for oxidative damage by nitrating intermediates in eosinophilic inflammatory disorders. J Biol Chem. 1999;274:25933–25944. doi: 10.1074/jbc.274.36.25933. [DOI] [PubMed] [Google Scholar]
- 77.Ghosh S, Janocha AJ, Aronica MA, Swaidani S, Comhair SA, Xu W, Zheng L, Kaveti S, Kinter M, Hazen SL, et al. Nitrotyrosine proteome survey in asthma identifies oxidative mechanism of catalase inactivation. J Immunol. 2006;176:5587–5597. doi: 10.4049/jimmunol.176.9.5587. [DOI] [PubMed] [Google Scholar]
- 78.Kaminsky DA, Mitchell J, Carroll N, James A, Soultanakis R, Janssen Y. Nitrotyrosine formation in the airways and lung parenchyma of patients with asthma. J Allergy Clin Immunol. 1999;104:747–754. doi: 10.1016/s0091-6749(99)70283-6. [DOI] [PubMed] [Google Scholar]
- 79.Saleh D, Ernst P, Lim S, Barnes PJ, Giaid A. Increased formation of the potent oxidant peroxynitrite in the airways of asthmatic patients is associated with induction of nitric oxide synthase: effect of inhaled glucocorticoid. FASEB J. 1998;12:929–937. [PubMed] [Google Scholar]
- 80.Comhair SA, McDunn J, Bennett C, Fettig J, Erzurum SC, Kalhan SC. Metabolomic endotype of asthma. J Immunol. 2015;195:643–650. doi: 10.4049/jimmunol.1500736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Heffner JE, Repine JE. Pulmonary strategies of antioxidant defense. Am Rev Respir Dis. 1989;140:531–554. doi: 10.1164/ajrccm/140.2.531. [DOI] [PubMed] [Google Scholar]
- 82.Gaston B. The biochemistry of asthma. Biochim Biophys Acta. 2011;1810:1017–1024. doi: 10.1016/j.bbagen.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 83.Dominici S, Valentini M, Maellaro E, Del Bello B, Paolicchi A, Lorenzini E, Tongiani R, Comporti M, Pompella A. Redox modulation of cell surface protein thiols in U937 lymphoma cells: the role of gamma-glutamyl transpeptidase–dependent H2O2 production and S-thiolation. Free Radic Biol Med. 1999;27:623–635. doi: 10.1016/s0891-5849(99)00111-2. [DOI] [PubMed] [Google Scholar]
- 84.Thomas JA, Poland B, Honzatko R. Protein sulfhydryls and their role in the antioxidant function of protein S-thiolation. Arch Biochem Biophys. 1995;319:1–9. doi: 10.1006/abbi.1995.1261. [DOI] [PubMed] [Google Scholar]
- 85.Reynaert NL, Wouters EF, Janssen-Heininger YM. Modulation of glutaredoxin-1 expression in a mouse model of allergic airway disease. Am J Respir Cell Mol Biol. 2007;36:147–151. doi: 10.1165/rcmb.2006-0259RC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Reynaert NL, Ckless K, Guala AS, Wouters EF, van der Vliet A, Janssen-Heininger YM. In situ detection of S-glutathionylated proteins following glutaredoxin-1 catalyzed cysteine derivatization. Biochim Biophys Acta. 2006;1760:380–387. doi: 10.1016/j.bbagen.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 87.Ghosh S, Willard B, Comhair SA, Dibello P, Xu W, Shiva S, Aulak KS, Kinter M, Erzurum SC. Disulfide bond as a switch for copper-zinc superoxide dismutase activity in asthma. Antioxid Redox Signal. 2013;18:412–423. doi: 10.1089/ars.2012.4566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ratanamaneechat S, Neumann DR, Difilippo FP, Comhair SA, Asosingh K, Ghosh S, Grandon D, Khan A, Aronica MA, Erzurum SC. Redox imaging of inflammation in asthma. Am J Respir Crit Care Med. 2014;189:743–746. doi: 10.1164/rccm.201310-1872LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Comhair SA, Ricci KS, Arroliga M, Lara AR, Dweik RA, Song W, Hazen SL, Bleecker ER, Busse WW, Chung KF, et al. Correlation of systemic superoxide dismutase deficiency to airflow obstruction in asthma. Am J Respir Crit Care Med. 2005;172:306–313. doi: 10.1164/rccm.200502-180OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Comhair SA, Xu W, Ghosh S, Thunnissen FB, Almasan A, Calhoun WJ, Janocha AJ, Zheng L, Hazen SL, Erzurum SC. Superoxide dismutase inactivation in pathophysiology of asthmatic airway remodeling and reactivity. Am J Pathol. 2005;166:663–674. doi: 10.1016/S0002-9440(10)62288-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.De Raeve HR, Thunnissen FB, Kaneko FT, Guo FH, Lewis M, Kavuru MS, Secic M, Thomassen MJ, Erzurum SC. Decreased Cu,Zn-SOD activity in asthmatic airway epithelium: correction by inhaled corticosteroid in vivo. Am J Physiol. 1997;272:L148–L154. doi: 10.1152/ajplung.1997.272.1.L148. [DOI] [PubMed] [Google Scholar]
- 92.Comhair SA, Erzurum SC. Antioxidant responses to oxidant-mediated lung diseases. Am J Physiol Lung Cell Mol Physiol. 2002;283:L246–L255. doi: 10.1152/ajplung.00491.2001. [DOI] [PubMed] [Google Scholar]
- 93.Comhair SA, Gaston BM, Ricci KS, Hammel J, Dweik RA, Teague WG, Meyers D, Ampleford EJ, Bleecker ER, Busse WW, et al. National Heart Lung Blood Institute Severe Asthma Research Program. Detrimental effects of environmental tobacco smoke in relation to asthma severity. PLoS One. 2011;6:e18574. doi: 10.1371/journal.pone.0018574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Larsen GL, White CW, Takeda K, Loader JE, Nguyen DD, Joetham A, Groner Y, Gelfand EW. Mice that overexpress Cu/Zn superoxide dismutase are resistant to allergen-induced changes in airway control. Am J Physiol Lung Cell Mol Physiol. 2000;279:L350–L359. doi: 10.1152/ajplung.2000.279.2.L350. [DOI] [PubMed] [Google Scholar]
- 95.Mabalirajan U, Dinda AK, Kumar S, Roshan R, Gupta P, Sharma SK, Ghosh B. Mitochondrial structural changes and dysfunction are associated with experimental allergic asthma. J Immunol. 2008;181:3540–3548. doi: 10.4049/jimmunol.181.5.3540. [DOI] [PubMed] [Google Scholar]
- 96.Alam MA, Rahman MM. Mitochondrial dysfunction in obesity: potential benefit and mechanism of co-enzyme Q10 supplementation in metabolic syndrome. J Diabetes Metab Disord. 2014;13:60. doi: 10.1186/2251-6581-13-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Comhair SA, Grandon D, Khan A, Zhang R, Hazen SL, Erzurum SC. Coenzyme Q in asthma. Am J Respir Crit Care Med. 2015;191:1336–1338. doi: 10.1164/rccm.201412-2259LE. [DOI] [PMC free article] [PubMed] [Google Scholar]