Abstract
Study Objectives:
To determine the prevalence, correlates, and predictors of insomnia in US Army personnel prior to deployment.
Methods:
Cross-sectional cohort design assessing insomnia and other psychosocial variables in active duty service members (n = 4,101), at Fort Hood, Texas, prior to military deployment. Insomnia was defined as an Insomnia Severity Index ≥ 15.
Results:
The prevalence of insomnia was 19.9%. Enlisted personnel were five times more likely to report insomnia than officers (odds ratio [OR] = 5.17). Insomnia was higher among American Indian/Alaskan Natives than other groups (ORs = 1.86–2.85). Those in the Insomnia Group were older, had longer military careers, and reported more marriages, children, and military deployments (ds = 0.13–0.34) than the No Insomnia group. The Insomnia Group reported more severe mental health symptoms, more recent stressful life events, greater childhood abuse, and lower levels of trait resilience, social support, and unit cohesion (Cohen ds = 0.27–1.29). After controlling for covariates, the Insomnia Group was more likely to have a history of head injuries and clinically significant posttraumatic stress disorder (PTSD), anxiety, depression, alcohol use problems, back pain, extremity pain, headaches, and fatigue (ORs = 1.40–3.30). A simultaneous logistic regression found that greater PTSD, depression, fatigue, stressful life events, headaches, anxiety, alcohol use problems, extremity pain, history of head injury, childhood physical neglect, back pain, number of times married, and lower leader support/unit cohesion and tangible social support were statistically significant predictors of insomnia status.
Conclusions:
Insomnia occurs in about one of five service members prior to a military deployment and is associated with a wide array of psychosocial stressors and mental and physical health problems.
Citation:
Taylor DJ, Pruiksma KE, Hale WJ, Kelly K, Maurer D, Peterson AL, Mintz J, Litz BT, Williamson DE, STRONG STAR Consortium. Prevalence, correlates, and predictors of insomnia in the US Army prior to deployment. SLEEP 2016;39(10):1795–1806.
Keywords: anxiety, Army, depression, insomnia, military, PTSD
Significance.
This was the largest study to date using validated measures of insomnia and psychosocial correlates in a typically healthy active-duty Army sample prior to deployment. Results indicate that, as in civilian populations, insomnia is a significant public health problem among active duty military that is associated with a range of mental and physical health problems. This study highlights the importance of addressing insomnia in this population. Longitudinal studies are needed to understand the course of insomnia and other sleep disorders (e.g., apnea, shift work, sleep deprivation) in the military and to determine temporal relationships with comorbidities. Studies are also needed to determine best practice guidelines for treating insomnia within the demanding work schedule of the military.
INTRODUCTION
Military service members face a number of stressors and challenges that place them at increased risk for insomnia compared to most civilians. These include, but are not limited to, frequent overnight and early-morning shift work, exposure to deployment stressors, frequent changes in duty assignments, and changes in duty station. To date, the prevalence and correlates of insomnia have not been evaluated comprehensively in a large cohort of service members. Table 1 includes a summary of select previous studies examining insomnia in active duty samples. As summarized in Table 1, existing evidence suggests that insomnia in the military ranges from 8% to 63%.1–7 This wide range in estimates is likely a result of the different operational definitions of insomnia used, as well as the varied, primarily medical samples assessed. Studies of insomnia in the military have not thoroughly examined the demographic characteristics, the types of stressors service members face, the resources that may mitigate stress, or the mental health and physical health predictors of insomnia.
Table 1.
Select previous studies examining insomnia in active duty samples, ordered by definition and date of publication.
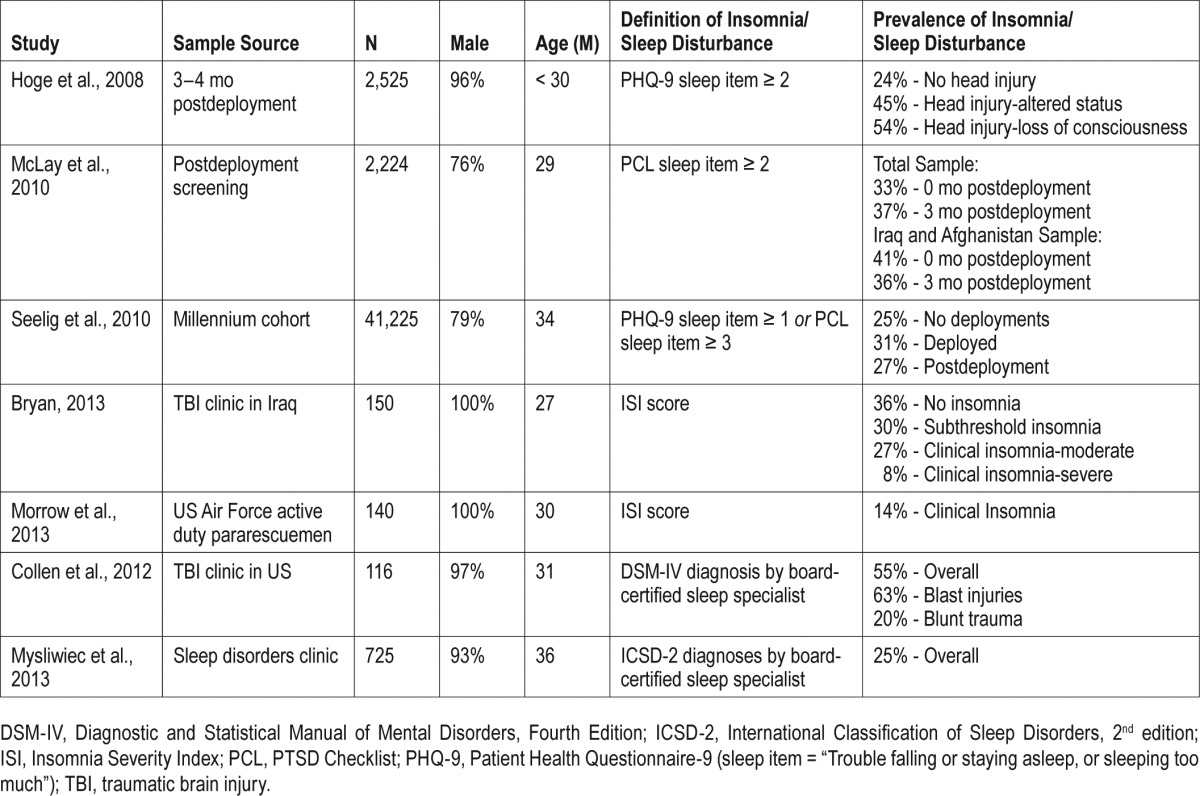
The most frequent method of assessing insomnia in the military has been a single sleep-relevant item from measures of depression or posttraumatic stress disorder (PTSD). These items are inadequate because they assess one or two symptoms of insomnia. For instance, two military studies1,6 utilized the sleep item from the PTSD Checklist-Military Version (PCLM),8 which asks how “bothered” (from “not at all” to “extremely”) respondents have been in the past month by “Trouble falling or staying asleep.” Considering that “Trouble falling or staying asleep” is only one diagnostic criterion of insomnia, this single item may be too sensitive, artificially inflating prevalence estimates by including individuals with subclinical insomnia. Two other studies3,6 utilized the sleep item from the Patient Health Questionnaire-9 (PHQ-9),9 which asks about the frequency of “Trouble falling or staying asleep, or sleeping too much,” which is problematic on two levels. First, similar to the PCL-M, the “Trouble falling or staying asleep…” component is too sensitive. Second, “sleeping too much” is a symptom of an entirely different class of sleep disorders (e.g., sleep apnea), which artificially inflates insomnia prevalence estimates by including individuals with sleep disorders other than insomnia.
Previous studies of military personnel that utilized valid assessment methods (e.g., validated insomnia questionnaires, structured clinical interviews, polysomnography) have limited external validity because they evaluated small samples in clinical contexts (e.g., in sleep disorder clinics), which substantially and artificially inflates prevalence estimates.10 For instance, although Bryan et al.5 utilized the empirically validated Insomnia Severity Index (ISI),11 the population surveyed was a small sample of males evaluated at a traumatic brain injury clinic during a deployment to Iraq (N = 150). Similarly, Morrow et al.7 used the ISI in a small (N = 140) group of US Air Force pararescuemen. Two studies2,4 used “gold standard” clinical interviews and polysomnography (i.e., sleep studies) administered and interpreted by a sleep specialist to determine insomnia diagnoses and rule out other sleep disorders. However, one study4 evaluated a small sample (N = 116) of soldiers returning from combat with mild to moderate traumatic brain injury. The other study2 evaluated a large sample (N = 725) of service members referred to a specialty sleep disorders clinic.
Previous studies of insomnia in the military have also not sufficiently explored potential predictors (putative causes and consequences) of insomnia. This is an important gap considering that insomnia is one of the most common symptoms of and risk factors for psychological health and medical conditions.10,12,13 Without this information, research on identification of risk and prevention is impeded. Some of the studies in Table 1 suggest that service members with significant insomnia symptoms are more likely to be female,2 have more mental health symptoms (e.g., PTSD, depression, anxiety, problem drinking),2,5,6 and physical health symptoms.2,6 They are also more likely to have previously deployed and to have had an increased number and severity of head injuries.2,3,5 However, insomnia has also been associated with a number of other psychosocial, mental health, and physical health problems in civilians, including irritability, fatigue, accidents, absenteeism, suicidality, reduced quality of life, concentration problems, and decreased immune functioning.10,12–16
The primary aim of this study was to determine the prevalence of insomnia in a large sample of active-duty military personnel using a valdiated measure of insomnia. We predicted that rates of insomnia among service members would be higher than rates found in civilian samples17 but lower than rates found in previous studies of military cohorts because of the use of the validated measure of insomnia. The secondary aim was to replicate previous findings from military samples that have shown an association of insomnia symptoms and various demographic,2 mental health,2,5,6 and physical health2,3,5,6 correlates. The third aim was to explore the association between insomnia and additional variables associated with insomnia in civilian samples including anger,18 stressful life events,19 childhood abuse,20,21 trait resilience,20 social support,22 and marital status.23 Finally, an exploratory aim was to examine the association between insomnia and unit cohesion and the number of children in this cohort, because these are unique potential sources of strain or potential resources for managing stress in the military.24–26
METHODS
Participants
This study analyzed the predeployment baseline data from a prospective, longitudinal, epidemiological study of the genetic and environmental predictors of combat-related PTSD in active-duty military personnel. We analyzed data from 4,101 of the 4,120 active duty service members at Fort Hood in Killeen, TX enrolled at baseline in the parent study. Participants were included if they were: (1) English-speaking; (2) active duty, activated Reserve, or activated National Guard Service Members of any branch of the US Armed Services; and (3) were scheduled for deployment in support of Operation Iraqi Freedom or Operation Enduring Freedom.
The mean age of the sample was 27.2 (± 6.1) y, and 91.2% were male. The ethnicity of the sample was 80.2% not Hispanic or Latino, 18.6% Hispanic or Latino, and 1.2% not reported. The racial breakdown was 64.1% Caucasian, 15.2% African American, 2.3% American Indian/Alaskan Native, 2.1% Asian, 1.7% Native Hawaiian or Other Pacific Islander, 12.3% other, and 2.3% not reported. Service members were from the US Army and were largely enlisted (93.9%) with at least a high school education (99.3%). Marital status breakdown was 56.0% married, 10.7% separated or divorced, 2.8% in a relationship and living with partner, 11.4% in a relationship but not living with a partner, and 19.0% never married and single.
Procedure
With the support of military commanders, active-duty service members were recruited at unit-level briefings during predeployment processing. After providing written informed consent, participants were given a packet of self-report measures to complete. There were 10 to 15 research staff on hand at each data collection event to answer any participant questions. All scales were administered during one session. The survey battery took an average of 45 min to complete, but service members were given as much time as needed. Research staff reviewed self-report packets to verify completion. The data were collected from units deploying between November 2010 and June 2011. All procedures were approved by the Institutional Review Boards at the University of Texas Health Science Center at San Antonio and Brooke Army Medical Center as well as the US Army Medical Research and Materiel Command Human Research Protection Office. Anonymity of the participants was maintained throughout the study.
Materials
The measures used in the study are common assessment measures with well-established reliability and validity. The reading level was appropriate to active-duty service members, most (99.3%) with high-school education and most with advanced specialized training. The internal consistency reliability measures (i.e., Cronbach alpha) are reported for each measure. In an effort to make the results clinically meaningful and comparable to previous epidemiological studies,10,12,13,27 we created post hoc clinical groups on various variables, as described in the next section.
Demographics and Military Service Characteristics Form
Demographics and military service characteristics were collected with a form developed by the investigators to measure standard demographics (age, sex, race, ethnicity, marital status, number of children) and military service information (e.g., military grade, service length, number of deployments).
Insomnia Severity Index
The ISI is a seven-item measure of the perceived severity of insomnia (i.e., difficulties falling asleep, staying asleep, and waking up too early, and daytime distress related to sleep), with total scores ranging from 0 to 28, where higher scores indicate greater insomnia severity. The Cronbach alpha for the ISI was 0.92 in the current study. Scores are typically classified as No Insomnia (0–7), Subthreshold Insomnia (8–14), Clinical Insomnia-Moderate (15–21), and Clinical Insomnia-Severe (22–28).11 Participants were further categorized into a No Insomnia Group (i.e., ISI ≤ 14 [No and Subthreshold Insomnia]) and an Insomnia Group (i.e., ISI ≥ 15 [Clinical Insomnia-Moderate and Severe), based on a diagnostic utility study.17
Beck Anxiety Inventory
The Beck Anxiety Inventory (BAI) is a 21-item measure of symptoms of anxiety, with total scores ranging from 0–63, where higher scores indicate greater anxiety symptoms.28 The Cronbach alpha for the BAI was 0.94 in the current study. A cutoff score ≥ 16 (i.e., Moderate to Severe Anxiety symptoms) was used to define clinically significant anxiety.
Beck Depression Inventory-II
The Beck Depression Inventory-II (BDI-II)29 is a 21-item measure of symptoms of depression with total scores ranging from 0–63, where higher scores indicate greater depression symptoms. The Cronbach alpha for the BDI-II was 0.94 in the current study. A cutoff score ≥ 20 (i.e., Moderate to Severe Depression symptoms) was used to determine clinically significant depression.
PTSD Checklist-Military Version
The PCL-M is a 17-item measure of symptoms of PTSD indexed to military experiences, with total scores ranging from 17 to 85, where higher scores indicate greater PTSD symptoms.8 The Cronbach alpha for the PCL-M was 0.95 in the current study. We defined PTSD caseness conservatively. Service members had probable PTSD if their total severity score was ≥ 50 and they met the diagnostic criteria for PTSD as outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). The meeting diagnostic criteria was defined as endorsing the requisite reexperiencing, avoidance and numbing, and hyperarousal symptoms at least to a moderate degree.
Alcohol Use Disorders Identification Test
The Alcohol Use Disorders Identification Test (AUDIT) is a 10-item measure of alcohol consumption that has become harmful to health, with total scores ranging from 0–40, where higher scores indicate a greater likelihood of an alcohol use disorder.30 The Cronbach alpha for the AUDIT was 0.95 in the current study. A cutoff score of ≥ 8 was used to define an alcohol use disorder.
State Trait Anger Expression Inventory State Anger Scale
The State Trait Anger Expression Inventory (STAXI) state anger scale is a 10-item measure of the intensity of anger felt at a particular moment in time, with total scores ranging from 10–40, where higher scores represent greater levels of anger.31 The Cronbach alpha for the STAXI was 0.94 in the current study.
The Patient Health Questionnaire-15
The PHQ-15 is a 15-item measure of medical symptom severity, with total scores ranging from 0–30.32 The Cronbach alpha for the PHQ-15 was 0.85 in the current study. The current study focused on individual items (i.e., symptoms) rather than PCL-15 total score. Responses of “bothered a lot” (item score = 2) were considered indicative of clinically significant difficulties.
History of Head Injuries
An augmented version of the Defense and Veterans Brain Injury Center (DVBIC) 3-Item Screening Tool33 was administered to all participants to assess for history of head injuries. As recommended by the DVBIC, participants were considered to have a history of head injuries when they endorsed an injury (Question 1) and altered consciousness (Question 2, Items A-E: “dazed,” “confused,” or “seeing stars”; “not remembering the injury”; “losing consciousness (knocked out) for [ < 1 min, 1–20 min, > 20 min]”) for the worst head injury sustained.
Psychiatric Epidemiology Research Interview Life Events Scale – Brief
The Psychiatric Epidemiology Research Interview Life Events Scale34 is a 102-item measure, designed to assess the number and severity of low- and moderate-magnitude stressful life events that a person has experienced in the previous 6 mo. In order to minimize time burden, the 10 items most relevant to the military population were selected by military subject matter experts. In some cases, the military experts combined items to adequately cover all of the major content areas of the original measure with the fewest number of items. No internal consistency measure was calculated because this is a measure of events and not a measure of a unitary construct.
Childhood Trauma Questionnaire
The Childhood Trauma Questionnaire35,36 is a 28-item measure that assesses five types (five items each) of potentially traumatizing childhood experiences (i.e., sexual abuse, physical abuse, emotional abuse, emotional neglect, and physical neglect) and minimization/denial (three items indicating the potential underreporting of maltreatment). Trauma subscale total scores range from 5 to 25, where higher scores represent greater exposure to potentially traumatizing events, and the minimization/denial scale total scores range from 0 to 3, with scores > 1 indicating possible underreporting of maltreatment. The Cronbach alpha for the Childhood Trauma Questionnaire was 0.89 in the current study.
Response to Stressful Experiences Scale
The Response to Stressful Experiences Scale (RSES)37 is a 22-item measure assessing cognitive, emotional, and behavioral traits that promote resilience in the face of life stressors, with total scores ranging from 0 to 110, where higher scores represent greater trait-levels of resilience. The Cronbach alpha for the RSES was 0.92 in the current study.
Interpersonal Support Evaluation List-Short Form
The Interpersonal Support Evaluation List-Short Form (ISELSF) is a 12-item measure of multiple dimensions of perceived social support (i.e., Appraisal, Belonging, and Tangible), with subscale total scores ranging from 1 to 16, where higher scores indicate more perceived social support.38 The Cronbach alpha for the ISEL-SF was 0.84 in the current study.
Walter Reed Army Institute of Research Horizontal and Vertical Cohesion Scales
The Walter Reed Army Institute of Research Horizontal and Vertical Cohesion Scales39 is a 12-item measure of perceived unit cooperation, dependence, and support. Horizontal support assesses attitudes about, and support from, peers within the military unit, and vertical support assesses attitudes and support from leaders of the military unit. Subscale total scores ranged from 1 to 30, where higher scores indicate greater cohesion. The Cronbach alpha for the horizontal, vertical, and total scales were 0.93, 0.91, and 0.092, respectively, in the current study.
Statistical Methods
For each individual measure, prorated total scores were computed for a participant if he or she provided responses > 70% but < 100% of the items in the measure, with missing responses being replaced by the individual's mean for the remaining items. Those individuals who provided less than 70% of the data for a given measure were considered invalid, and, consequently, did not receive a total score for that measure. After this procedure, scale-level missing data were minimal (< 3%) and appeared to be missing completely at random. Therefore, given that the sample size was large, missing data were not imputed at the scale level, following the recommendations of Tabachnick and Fidell.40
Statistical analyses were performed using the Statistical Package for Social Sciences (SPSS 20.0; IBM, Armonk, NY, USA). First, descriptive statistics for ISI scores were examined. Next, groups (No Insomnia vs. Insomnia) were compared on demographic variables, mental health symptom severity and other psychosocial measures previously described using chi-square tests of independence and analyses of variance. Next, unadjusted and adjusted (i.e., controlling for all other significant variables from unadjusted analyses) logistic regression analyses were performed to examine the relationships between insomnia and clinically significant physical and mental health problems. Finally, to determine which clinically significant correlates were most closely related to insomnia status, a simple logistic regression was performed, with insomnia (yes or no) entered as the dependent variable and significant variables from the chi-square, analysis of variance, and adjusted logistic regression analyses entered simultaneously as the predictor variables. In instances where there were dichotomous and continuous versions of certain predictors (e.g. PCL-M score vs. PTSD diagnosis) that were significantly related in earlier analyses, we elected to use the dichotomous versions of these variables for ease of interpretation. Similarly, when the predictors were continuous demographic characteristics (e.g., age, number of children, number of times married), a simple median split was used. Subscale scores for measures were used if prior analyses had examined both subscale scores and total scores in order to avoid problems with multicollinearity. Effect sizes, odds ratios (ORs), and confidence intervals of various outcomes can be found in Table 1 through Table 6.
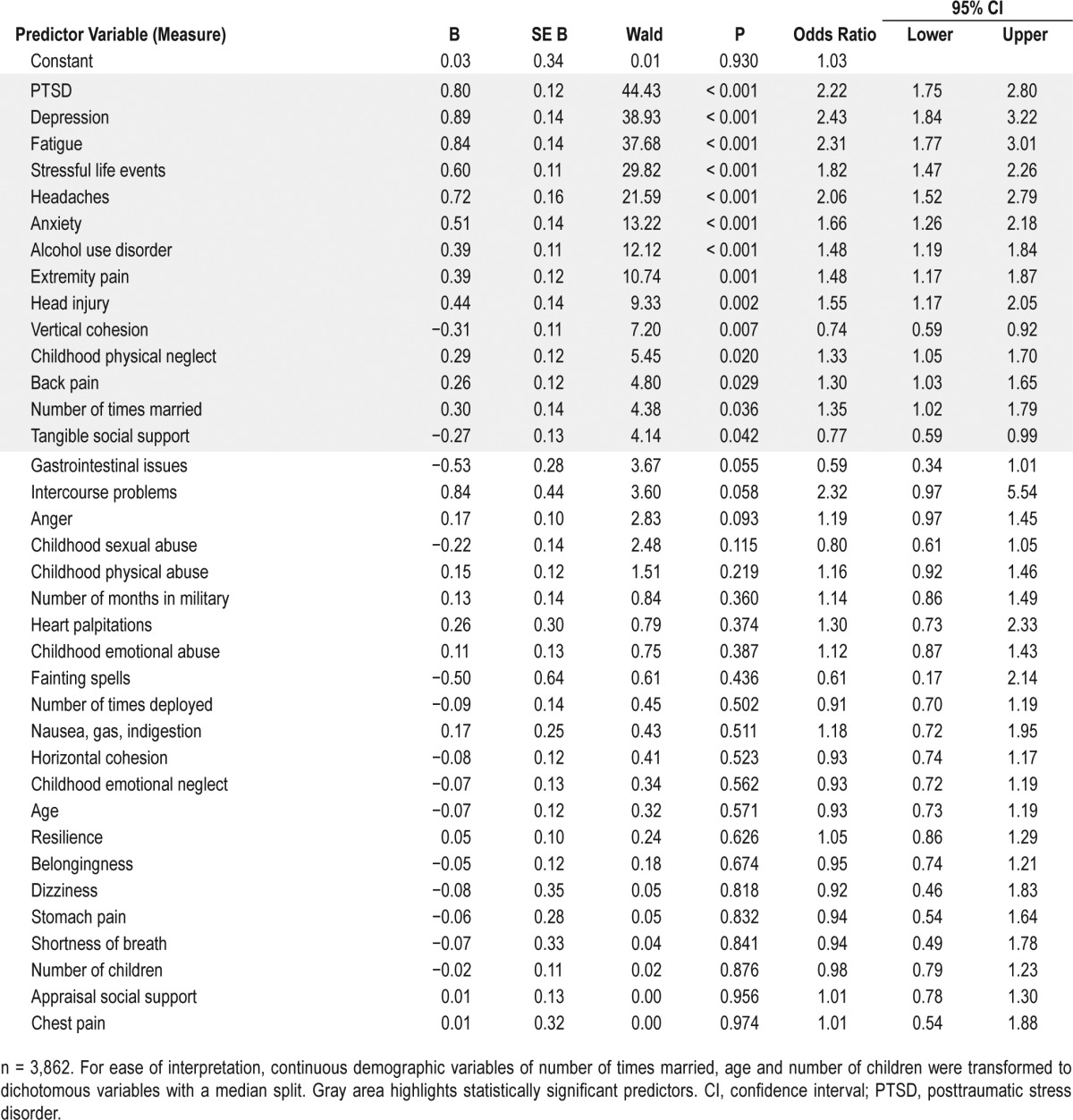
Table 6.
Predictors from simultaneous logistic regression analysis for variables predicting insomnia.
RESULTS
Prevalence of Insomnia
The mean total score of the ISI for the total sample was 7.97 (SD = 6.98), which is on the border of the standard cutoff score of 7 to distinguish between “No Insomnia” and “Subclinical Insomnia.”11 The single sleep items of the PCL-M and PHQ-9 showed only medium correlations with the ISI (r = 0.71 and r = 0.64, respectively, Ps < 0.05), suggesting modest to poor construct validity for these items. Using standard classification levels,11 the ISI classified 54.3% of the sample as having No Insomnia, 25.8% as Subthreshold Insomnia, 15.5% as Clinical Insomnia-Moderate, and 4.4% as Clinical Insomnia-Severe. As discussed previously, participants were then dichotomized into a No Insomnia Group (80.1 % (n = 3,286); i.e., ISI ≤ 14 [No and Subthreshold Insomnia]) and an Insomnia Group (19.9% (n = 815); i.e., ISI ≥ 15 [Clinical Insomnia-Moderate and Severe).17
Correlates of Insomnia
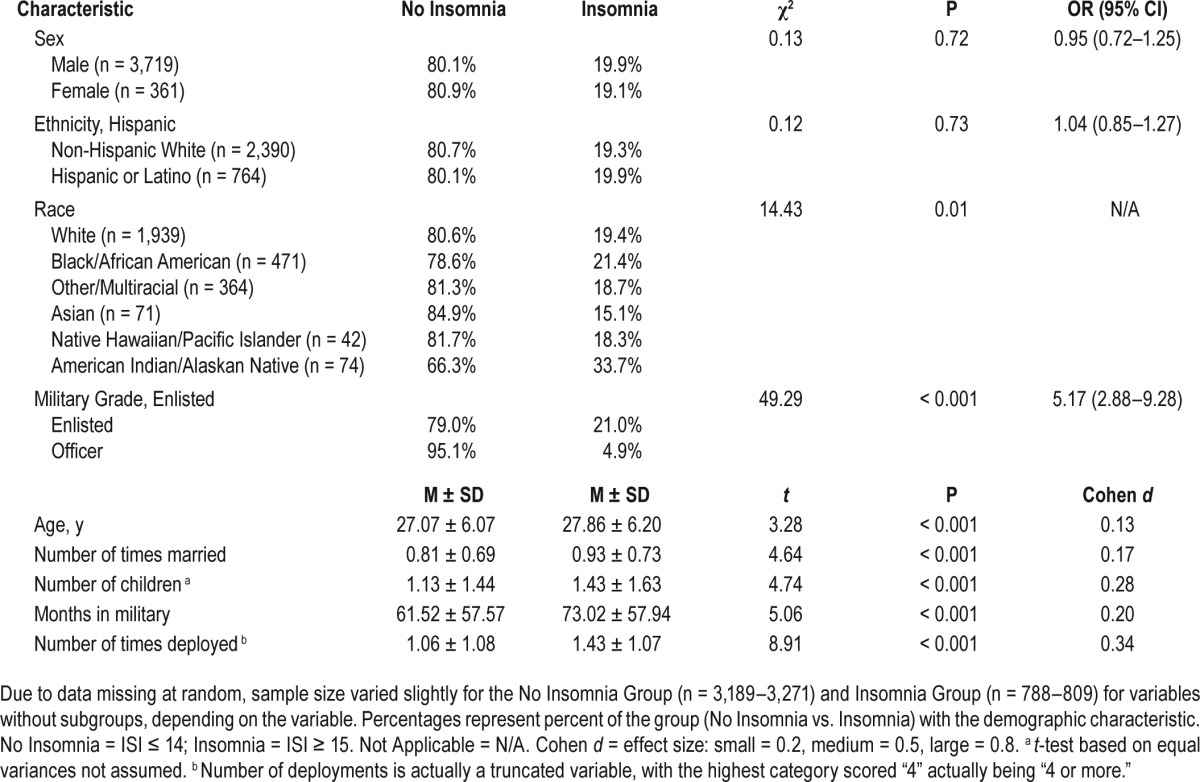
Demographics
Table 2 shows the prevalence of insomnia within demographic groups. As can be seen in Table 2, there were no significant differences between the No Insomnia and Insomnia Groups on sex or ethnicity. There were significant differences among races, with the American Indian/Alaskan Native group having significantly higher rates of insomnia than Caucasians (OR = 2.11; 95% confidence interval [CI] = 1.36–3.26), other (OR = 2.25; 95% CI = 1.37–3.58), African Americans (OR = 1.86; 95% CI = 1.17–2.98), Asians (OR = 2.85; 95% CI = 1.38–5.90), and Native Hawaiian or Other Pacific Islanders (OR = 2.27; 95% CI = 1.09–4.73). There were also significant differences between military grades, with enlisted personnel having significantly higher rates of insomnia than officers. In addition, the Insomnia Group was significantly older, had been married more times, had more children, had served longer in the military, and had more military deployments.
Table 2.
Prevalence of insomnia within demographic groups.
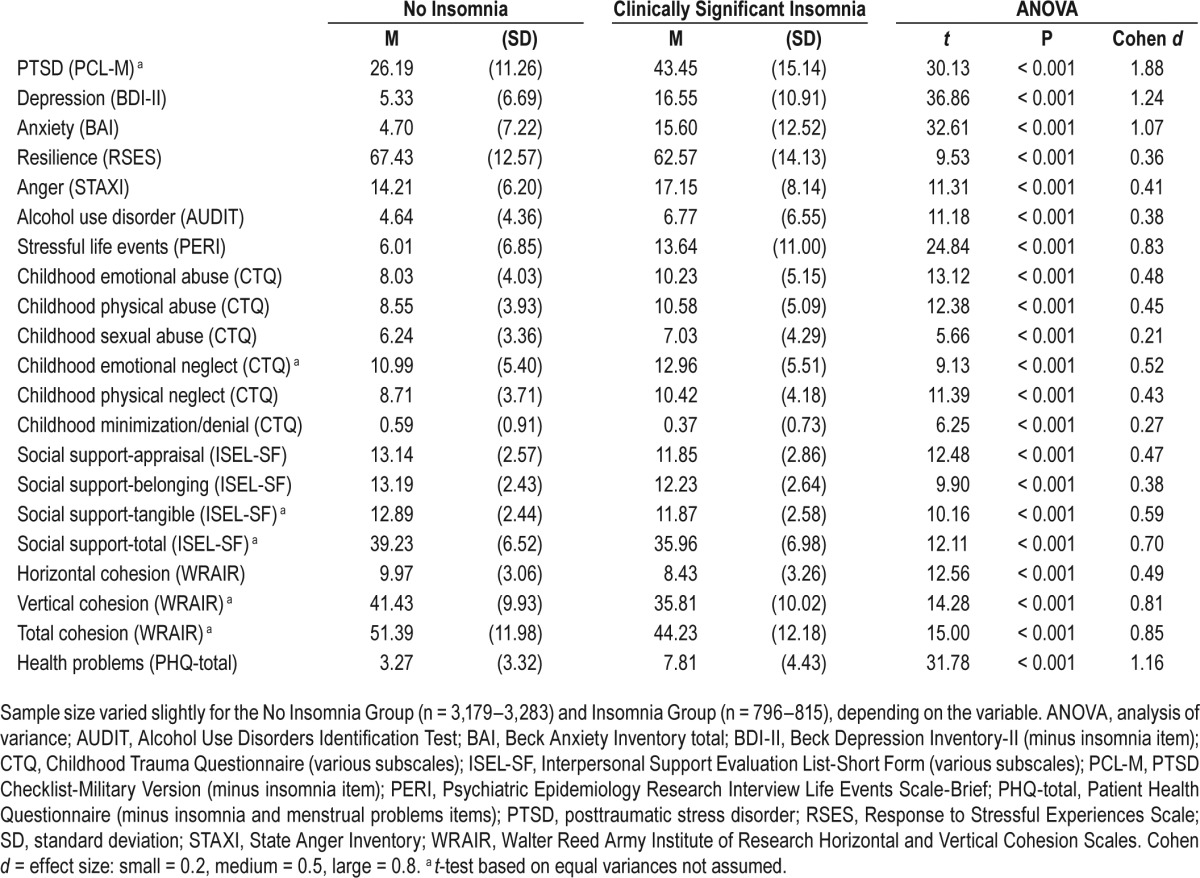
Mental and Physical Health Variables
The univariate analyses of self-reported psychosocial and sleep variables for the Insomnia and No Insomnia Groups are included in Table 3. As expected, service members in the Insomnia Group reported greater symptom severity of self-reported PTSD, depression, anxiety, anger, and alcohol use problems as compared to the No Insomnia Group. They also reported more stressful life events in the past 6 mo, greater childhood abuse, and lower levels of trait resilience, social support, and unit cohesion than the No Insomnia Group.
Table 3.
Univariate analyses of self-reported psychosocial and sleep variables for Insomnia and No Insomnia.
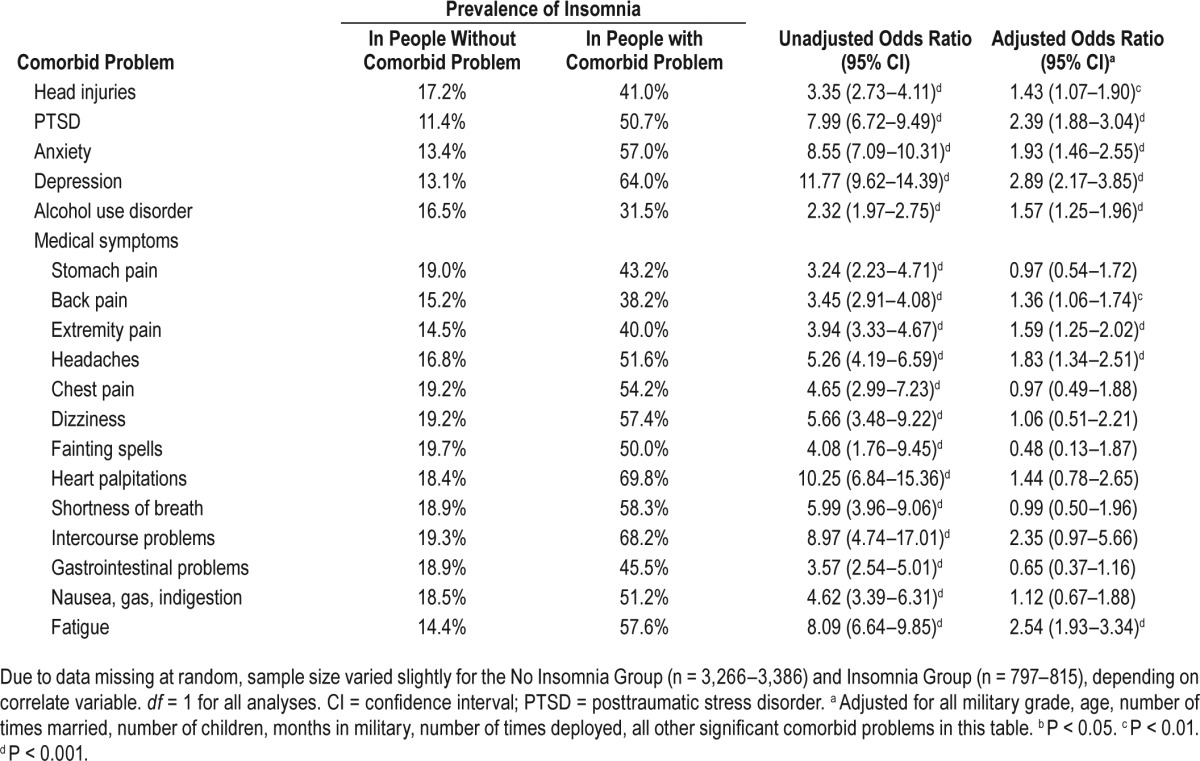
The prevalence of insomnia in groups with and without comorbid physical and mental health problems is included in Table 4. The prevalence of insomnia was higher in those with a history of head injuries (41.0% vs. 17.2%), clinically significant PTSD (50.7% vs. 11.4%), anxiety (57.0% vs. 13.4%), depression (64.0% vs. 13.1%), and alcohol usage (31.5% vs. 16.5%) than those without clinically significant levels of these difficulties. These differences stayed significant even after controlling for all other significant demographic variables and comorbid problems. The prevalence of insomnia was also significantly higher in individuals with any clinically significant medical symptom (38.2% to 69.8% vs. 14.4% to 19.7%), but after controlling for all other significant demographic variables and comorbid problems, statistical significance remained only in those individuals experiencing clinically significant back pain (OR = 1.36; 95% CI = 1.06–1.74), extremity pain (OR = 1.59; 95% CI = 1.25–2.02), headaches (OR = 1.83; 95% CI = 1.34–2.51), and fatigue (OR = 2.54; 95% CI = 1.93–3.34).
Table 4.
Prevalence of insomnia in groups with and without comorbid physical and mental health problems.
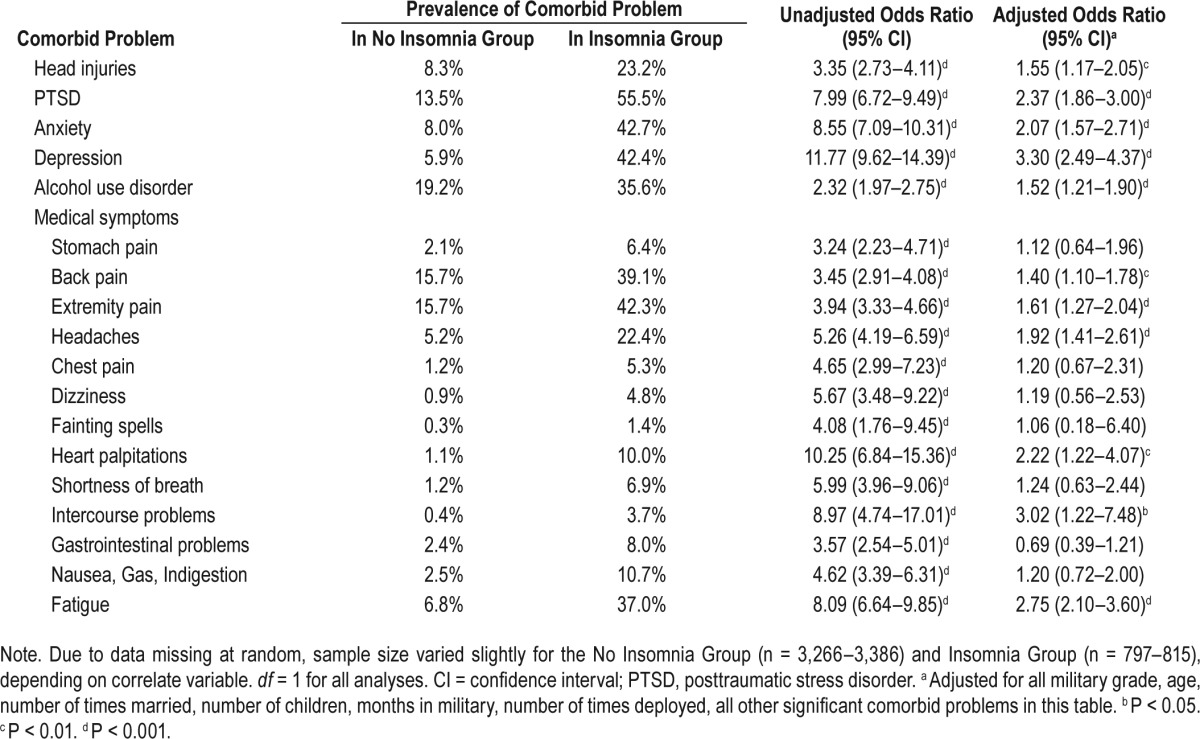
The prevalence of comorbid physical and mental health problems in the Insomnia and No Insomnia Groups is included in Table 5. The Insomnia Group had higher rates of head injuries (23.20% vs. 8.3%) and clinically significant PTSD (55.5% vs. 13.5%), anxiety (42.7% vs. 8.0%), depression (42.4% vs. 5.9%), and alcohol use disorder (35.6% vs. 19.2%) than the No Insomnia Group. These differences stayed significant even after controlling for all other significant demographic variables and comorbid problems. The prevalence of all clinically significant medical symptoms was also significantly higher in Insomnia than No Insomnia (1.4% to 42.3% vs. 0.3% to 15.7%), but after controlling for all other significant demographic variables and comorbid problems, statistical significance remained only for significant back pain (OR = 1.40; 95% CI = 1.10–1.78), extremity pain (OR = 1.61; 95% CI = 1.27–2.04), headaches (OR = 1.92; 95% CI = 1.41–2.61), heart palpitations (OR = 2.22; 95% CI = 1.22–4.07), intercourse problems (OR = 3.02; 95% CI = 1.22–7.48), and fatigue (OR = 2.75; 95% CI = 2.10–3.60).
Table 5.
Prevalence comorbid physical and mental health problems in Insomnia vs. No Insomnia Groups.
Predictors of Insomnia
The predictors from simultaneous logistic regression analysis for variables predicting insomnia are included in Table 6. The overall regression model (n = 3,862) with all 36 originally significant predictors of insomnia was significant (χ2(8) = 46.71, P < 0.001), with Nagelkerke R2 indicating that 39.20% of the variation in insomnia was accounted for by the predictors. As Table 6 shows, 14 of the original 36 variables remained significant, including PTSD, depression, fatigue, stressful life events, headaches, anxiety, alcohol use problems, extremity pain, history of head injury, vertical cohesion, childhood physical neglect, back pain, number of times married, and tangible social support.
DISCUSSION
This study evaluated a large sample of active-duty US military personnel (n = 4,101) prior to deploying to locations in and around Iraq and Afghanistan. The results indicated that almost one out of five service members (19.9%) met criteria for insomnia using a conservative cutoff (≥ 15) on the seven-item ISI. Rates of insomnia were more than five times as likely in enlisted personnel (21.0%) as compared to officers (4.9%). Insomnia was also higher in American Indian/Alaskan Native than in all other groups (33.7% vs. 15.1% to 21.4%; all Ps < 0.05), although this minority group represented only 2.3% of the sample population. The Insomnia Group was also older, had been married more times, had more children, had been in the military longer, and had more military deployments (all Ps < 0.001). The Insomnia Group reported greater symptom severity of PTSD, depression, anxiety, anger, alcohol use problems, medical symptoms, more stressful life events in past 6 mo, more childhood abuse, and lower levels of resilience, minimization/denial of childhood abuse, social support and unit cohesion than the No Insomnia Group (all Ps < 0.001).
Similarly, individuals in the Insomnia Group were more likely than the No Insomnia Group to report a history of head injuries, clinically significant PTSD, anxiety, depression, or alcohol use problems, back pain, extremity pain, headaches, heart palpitations, intercourse problems, and fatigue (ORs = 1.40–3.30). After controlling for all other significant demographics and comorbid problems, individuals with a history of head injuries, clinically significant PTSD, anxiety, depression, or alcohol use problems, back pain, extremity pain, headaches, and fatigue were more likely (ORs = 1.36–2.89) to report insomnia.
Although numerous variables predicted insomnia status individually, the final logistic regression showed that, holding all other predictors constant, PTSD, depression, fatigue, stressful life events, headaches, anxiety, alcohol use problems, extremity pain, history of head injury, vertical cohesion, childhood physical neglect, back pain, number of times married, and tangible social support remained statistically significant predictors of insomnia status.
As hypothesized, the 19.9% prevalence rate for insomnia found in this study using the ISI was lower than the 25% that Seelig and colleagues6 found in the largest military sample (n = 41,225) of individuals predeployment using single self-report items. Rates were also lower than the 35% that Bryan5 found using the same ISI criteria (i.e., ISI total score ≥ 15) in a military traumatic brain injury clinic in Iraq, but they were higher than the 16% found in the Morrow et al.7 study of pararescuemen. Rates found in the current study were also lower than the 25% that Mysliwiec et al.2 found using gold standard sleep specialist diagnosis and PSG in a military sleep disorders clinic, but they were similar to the 20% that Collen et al.4 found in service members with a blunt trauma history at a military traumatic brain injury clinic in the US. Finally, the 19.9% found here was higher than the 13% that Morin et al.17 found in a civilian sample using the same criteria (i.e., ISI total score ≥ 15). The prevalence estimates found in the current study were likely lower than most previous military studies because (1) a validated measure with a conservative case definition was used to assess insomnia, rather than a single item, and (2) a large population of military service members was assessed prior to deployment, rather than a medical sample. The rates found here were likely higher than the Morrow et al.7 study because they had a smaller (N = 140), healthier sample, as evidenced by their lower PTSD and depression rates than previous studies, which likely contributed to lower insomnia rates. Overall, these data affirm that insomnia is highly prevalent in the military, affecting approximately one in five service members.
This study was unique in part because it included a racially and ethnically diverse sample, allowing the first examination of the prevalence of insomnia in the military using National Institutes of Health definitions41 of race and ethnicity. The findings that the American Indian/Alaskan Native group had significantly higher rates of insomnia (40.3%) than all other groups was unexpected only in that very little research has been performed on this group. One study of a small sample (N = 449) of older (age 55 y and older) American Indians found that approximately 40% reported “Sometimes” having “difficulty falling asleep or staying asleep” and 16.6% reported “Often” having this problem.42 An unpublished dissertation43 reported that 25% of an adolescent American Indian/Alaskan Native group reported insomnia defined as “trouble falling asleep or staying asleep at least once a week.” They went on to show that insomnia was significantly related to depression but not suicide. The nonsignificant differences between the other racial and ethnic backgrounds were not altogether unexpected, as this literature has been mixed. Although one meta-analysis found differences between non-Hispanic whites and African Americans on symptoms of insomnia,44 other studies have found that these differences are primarily found in middle-aged adults and women,45–47 both of which were underrepresented in the current study (i.e., only 4.8% older than 40 y and 8.8% female).48
This current study replicated previous studies showing that the number of military deployments is highly related to insomnia.1,6,49 With respect to other demographic factors, the results were consistent with previous studies in civilian samples showing that insomnia is related to increasing age,50,51 but this was the first study to demonstrate this relationship in a military sample. This study was also the first to identify that military personnel with insomnia had been married more times, had more children, and had been in the military longer. The previous finding from Mysliwiec et al.2 indicating higher rates of insomnia among women than among men was not replicated. It is unclear why this result was not found, especially given it is a consistent finding in civilian samples,52 but it may be related to women in the military being healthier, having better access to health care, and being less likely to engage in health risk behaviors than civilian women.48
The results of this study replicated those from previous studies showing insomnia is related to a history of head injuries,3,5 PTSD,2,5,6,53 depression,2,6 anxiety,2,6 and problematic drinking6 in active duty service members. The results also replicated results from studies of civilian samples with regard to levels of anger,18 exposure to potentially traumatizing events during one's lifetime54 or childhood,20,21 trait resilience,20 social support,22 and marital status.23 Finally, this was the first study to demonstrate that service members with insomnia reported lower levels of unit cohesion, which likely reduces resilience against a wide array of stressors that may impact sleep.24,25
The rates of insomnia in those with a history of head injury in the current study (41.0%) were in line with those reported by Bryan5 and Hoge et al.3 (i.e., 50.0% to 53.8%). The rates of clinically significant anxiety and depression in the Insomnia Group were twice the rates seen in some civilian samples (42.7 and 42.4% vs. 19.3 and 20.0%, respectively).13 The rates of clinically significant problems in the Insomnia Group were greater than those found by Mysliwiec et al.2 for PTSD (55.5% vs. 20.7%, respectively), depression (42.4% vs. 31.4%, respectively), and anxiety (42.7% vs. 23.4%, respectively), but less for head injuries (23.2% vs. 31.9%, respectively). The rest of the results were new findings in this sample and were in line with the overall pattern of results of the Insomnia Group having worse functioning than the No Insomnia Group.
Finally, logistic regressions were run predicting insomnia to address the issue of symptom overlap among the many constructs measured (e.g., insomnia, depression, PTSD, medical problems). Consistent with other research in civilian samples, PTSD,55–59 depression,12,13,60–70 and medical problems10,71 (i.e., fatigue, headaches, extremity pain, history of head injury, back pain) strongly predicted insomnia status.12,27 Additional predictors included stressful life events, anxiety, alcohol use problems, vertical cohesion, childhood physical neglect, number of times married, and tangible social support. This is not to imply that insomnia is necessarily secondary to these problems, as research has begun to show that insomnia often has a reciprocal relationship with these and other problems.12,13,16 For instance, there is now substantial evidence that insomnia is involved in the development and course of depression12,13,60–70 and PTSD.56,59 Sleep disturbances may also serve to exacerbate many medical problems such as pain,72–74 cardiovascular disease,75–77 and gastrointestinal problems.78 However, one can safely assume that when the risk of having insomnia is more than twofold greater in a particular comorbidity (e.g., depression, PTSD, anxiety) the comorbidity is likely causing some portion of the insomnia. More prospective, experimental, and intervention research is needed to help clarify these relationships if precision medicine is going to become a reality.
One limitation of the current study was that insomnia status was characterized with a self-report scale rather than a structured clinical interview performed by an expert in sleep medicine. Although not as rigorous as those provided by the DSM-579 or the quantitative80 or Research Diagnostic Criteria,81 the ISI has excellent reliability and validity. It also is a significant improvement over the single items from the PCL and PHQ more commonly used in this population1,3,6 and comparable to those used by Bryan5 and Morrow et al.5 Within a large-scale study such as this, which included some occurrences in which hundreds of service members were screened per day as they were preparing for deployment, it is difficult to perform structured clinical interviews of the kind needed to reliably assess diagnostic criteria as described previously. Thus the ISI or similar diagnosis-specific measures, rather than nonspecific single items, might be the next best option.
Another limitation of the current study was that a cross-sectional sample of convenience was employed. Therefore, the results are not generalizable to all service members, the direction of the association between insomnia and the various correlates is unknown, and the intra-individual temporal courses or trajectories of insomnia are also not known (e.g., the percentage of cases that spontaneously remit is unknown). However, these data do improve our understanding of the prevalence and correlates of insomnia in the Army, using a better assessment of insomnia in a more general sample, which hopefully will stimulate prevention and treatment strategies.82 Future studies should investigate insomnia in other branches of the military.
This study was also limited because all the active-duty service members included in this sample were preparing to deploy. The stress associated with this situation may have altered sleep. However, active-duty service members experience a number of stressful transitions (e.g., changes in duty assignments and duty stations). The degree to which preparing to deploy differentially affects sleep compared to other transitions is unknown.
Notwithstanding these problems, these findings are consistent with a growing body of literature showing that insomnia is an important public health problem in active-duty military and highlight the importance of assessing and addressing insomnia in this population. Larger-scale longitudinal studies are needed, as a great deal remains to be learned about prevalence and temporal relationships of sleep disorders (e.g., insomnia, apnea, shift work, sleep deprivation) and correlates and comorbidities in the military. In addition, more studies are needed to help determine how best to treat those individuals with insomnia in the unique work culture of the military.
DISCLOSURE STATEMENT
The work was performed at the United States Army installation at Fort Hood in Killeen, TX. The views expressed in this article are solely those of the authors and do not reflect an endorsement by or the official policy of the US Army, the US Air Force, the Department of Defense, the Department of Veterans Affairs, or the US Government. Funding for this work was made possible by the US Department of Defense through the US Army Medical Research and Materiel Command, Congressionally Directed Medical Research Programs, Psychological Health and Traumatic Brain Injury Research Program awards W81XWH-08-2-0110 (Dr. Williamson), W81XWH-08-02-109 (Dr. Peterson), and W81XWH-10-1-0828 (Dr. Taylor). There was no other financial support for this research nor are there any conflicts of interest for any of the authors. No off-label or investigational drugs were used in this study. Portions of these findings have previously been presented: Taylor DJ, Pruiksma KE, Kelly K, Maurer D, Litz B, Peterson A, Mintz J, Williamson DE. Insomnia in the military: prevalence and comorbidities. Sleep 2015;38(Abstract Suppl):A614.
ACKNOWLEDGMENTS
The authors thank Raymond Aguilar, Antoinette Brundige, Katherine Compton, Tamara DeFranc, Paul Fowler, Sonia Holloman, and Helen Knapp, who supported data collection for this study; Antoinette Brundige, Gary Burk, and Susan Deason, who supported this study as part of the STRONG STAR Administrative Core; Raymond Aguilar and Kevin Muenzler, who supported this study as part of the STRONG STAR Data and Biostatistics Core; Kathryn Marczyk, who supported data entry for this study; Kimberly Del Carmen and Holly Campbell-Rosen, who supported this study as grant officer representatives; and Julie Collins and Joel Williams, who provided editorial support for this manuscript.
STRONG STAR Consortium group authors include (alphabetically): Elisa V. Borah, PhD, School of Social Work, University of Texas at Austin, Austin, TX; Antoinette Brundige, MA, and Stacey Young-McCaughan, RN, PhD, Department of Psychiatry, University of Texas Health Science Center at San Antonio, San Antonio, TX.
REFERENCES
- 1.McLay RN, Klam WP, Volkert SL. Insomnia is the most commonly reported symptom and predicts other symptoms of post-traumatic stress disorder in U.S. service members returning from military deployments. Mil Med. 2010;175:759–62. doi: 10.7205/milmed-d-10-00193. [DOI] [PubMed] [Google Scholar]
- 2.Mysliwiec V, McGraw L, Pierce R, Smith P, Trapp B, Roth BJ. Sleep disorders and associated medical comorbidities in active duty military personnel. Sleep. 2013;36:167–74. doi: 10.5665/sleep.2364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in US soldiers returning from Iraq. N Engl J Med. 2008;358:453–63. doi: 10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- 4.Collen J, Orr N, Lettieri CJ, Carter K, Holley AB. Sleep disturbances among soldiers with combat-related traumatic brain injury. Chest. 2012;142:622–30. doi: 10.1378/chest.11-1603. [DOI] [PubMed] [Google Scholar]
- 5.Bryan CJ. Repetitive traumatic brain injury (or concussion) increases severity of sleep disturbance among deployed military personnel. Sleep. 2013;36:941–6. doi: 10.5665/sleep.2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seelig AD, Jacobson IG, Smith B, et al. Sleep patterns before, during, and after deployment to Iraq and Afghanistan. Sleep. 2010;33:1615. doi: 10.1093/sleep/33.12.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morrow CE, Bryan CJ, Stephenson JA, Bryan AO, Haskell J, Staal M. Posttraumatic stress, depression, and insomnia among U.S. Air Force pararescuemen. Mil Psychol. 2013;25:568–76. [Google Scholar]
- 8.Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist (PCL): reliability, validity, & diagnostic utility. Paper presented at: International Society of Traumatic Stress 9th Annual Meeting; October 1993; San Antonio, TX. [Google Scholar]
- 9.Kroenke K, Spitzer RL, Williams JB. The Phq-9. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, Bush AJ. Comorbidity of chronic insomnia with medical problems. Sleep. 2007;30:213–8. doi: 10.1093/sleep/30.2.213. [DOI] [PubMed] [Google Scholar]
- 11.Morin CM. New York, NY: Guilford Press; 1993. Insomnia: psychological assessment and management. [Google Scholar]
- 12.Taylor DJ, Lichstein KL, Durrence HH. Insomnia as a health risk factor. Behav Sleep Med. 2003;1:227–47. doi: 10.1207/S15402010BSM0104_5. [DOI] [PubMed] [Google Scholar]
- 13.Taylor DJ, Lichstein KL, Durrence HH, Riedel BW, Bush AJ. Epidemiology of insomnia, depression, and anxiety. Sleep. 2005;28:1457–64. doi: 10.1093/sleep/28.11.1457. [DOI] [PubMed] [Google Scholar]
- 14.Kuppermann M, Lubeck DP, Mazonson PD, et al. Sleep problems and their correlates in a working population. J Gen Intern Med. 1995;10:25–32. doi: 10.1007/BF02599573. [DOI] [PubMed] [Google Scholar]
- 15.Roth T, Roehrs T. Sleepiness and motor vehicle accidents. Int Clin Psychopharmacol. 1988;3(Suppl 1):111–6. [PubMed] [Google Scholar]
- 16.Walsh JK. Clinical and socioeconomic correlates of insomnia. J Clin Psychiatry. 2004;65(Suppl 8):13–9. [PubMed] [Google Scholar]
- 17.Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–8. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Waters WF, Adams SG, Binks P, Varnado P. Attention, stress and negative emotion in persistent sleep-onset and sleep maintenance insomnia. Sleep. 1993;16:128–36. doi: 10.1093/sleep/16.2.128. [DOI] [PubMed] [Google Scholar]
- 19.Morin CM, Rodrigue S, Ivers H. Role of stress, arousal, and coping skills in primary insomnia. Psychosom Med. 2003;65:259–67. doi: 10.1097/01.psy.0000030391.09558.a3. [DOI] [PubMed] [Google Scholar]
- 20.Chambers E, Belicki K. Using sleep dysfunction to explore the nature of resilience in adult survivors of childhood abuse or trauma. Child Abuse Negl. 1998;22:753–8. doi: 10.1016/s0145-2134(98)00059-3. [DOI] [PubMed] [Google Scholar]
- 21.Bader K, Schaefer V, Schenkel M, Nissen L, Schwander J. Adverse childhood experiences associated with sleep in primary insomnia. J Sleep Res. 2007;16:285–96. doi: 10.1111/j.1365-2869.2007.00608.x. [DOI] [PubMed] [Google Scholar]
- 22.Nakata A, Haratani T, Takahashi M, et al. Job stress, social support, and prevalence of insomnia in a population of Japanese daytime workers. Soc Sci Med. 2004;59:1719–30. doi: 10.1016/j.socscimed.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 23.Morin CM, LeBlanc M, Daley M, Gregoire J, Merette C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. 2006;7:123–30. doi: 10.1016/j.sleep.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 24.Oliver LW, Harman J, Hoover E, Hayes SM, Pandhi NA. A quantitative integration of the military cohesion literature. Mil Psychol. 1999;11:57–83. [Google Scholar]
- 25.Brailey K, Vasterling JJ, Proctor SP, Constans JI, Friedman MJ. PTSD symptoms, life events, and unit cohesion in US soldiers: baseline findings from the neurocognition deployment health study. J Trauma Stress. 2007;20:495–503. doi: 10.1002/jts.20234. [DOI] [PubMed] [Google Scholar]
- 26.Lundberg U, Mårdberg B, Frankenhaeuser M. The total workload of male and female white collar workers as related to age, occupational level, and number of children. Scand J Psychol. 1994;35:315–27. doi: 10.1111/j.1467-9450.1994.tb00956.x. [DOI] [PubMed] [Google Scholar]
- 27.Pallesen S, Nordhus IH, Nielsen GH, et al. Prevalence of insomnia in the adult Norwegian population. Sleep. 2001;24:771–9. [PubMed] [Google Scholar]
- 28.Beck AT, Steer RA, Garbin MG, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–7. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 29.Beck AT, Steer RA, Brown GK. San Antonio, TX: Psychological Corporation; 1996. Manual for the Beck Depression Inventory-II. [Google Scholar]
- 30.Saunders JB, Aasland OG, Babor TF, Grant M. Development of the Alcohol Use Disorders Identification Test (Audit): WHO collaborative project on early detection of persons with harmful alcohol consumption: II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 31.Spielberger CD. Odessa, FL: Psychological Assessment Resources; 1988. State-Trait Anger Expression Inventory (STAXI) [Google Scholar]
- 32.Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64:258–66. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 33.Schwab KA, Ivins B, Cramer G, et al. Screening for traumatic brain injury in troops returning from deployment in Afghanistan and Iraq: initial investigation of the usefulness of a short screening tool for traumatic brain injury. J Head Trauma Rehabil. 2006;22:377–89. doi: 10.1097/01.HTR.0000300233.98242.87. [DOI] [PubMed] [Google Scholar]
- 34.Dohrenwend BS, Krasnoff L, Askenasy AR, Dohrenwend BP. Exemplification of a method for scaling life events: the Peri Life Events Scale. J Health Soc Behav. 1978;19:205–29. [PubMed] [Google Scholar]
- 35.Bernstein DP, Stein JA, Newcomb MD, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27:169–90. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 36.Bernstein DP, Fink L. San Antonio, TX: Psychological Corporation; 1998. Childhood trauma questionnaire: a retrospective self-report questionnaire and manual. [Google Scholar]
- 37.Johnson DC, Polusny MA, Erbes CR, et al. Development and initial validation of the Response to Stressful Experiences Scale. Mil Med. 2011;176:161–9. doi: 10.7205/milmed-d-10-00258. [DOI] [PubMed] [Google Scholar]
- 38.Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. Appl Soc Psychol. 1983;58:304–9. [Google Scholar]
- 39.Vaitkus MA. Fort Detrick, MD: U.S. Army Medical Research and Materiel Command; 1994. [Accessed January 13, 2016]. Unit manning system: human dimensions field evaluation of the COHORT company replacement model. Available at: http://oai.dtic.mil/oai/oai?verb=getRecord&metadataPrefix=html&identifier=ADA285942. [Google Scholar]
- 40.Tabachnick BG, Fidell LS. Using multivariate statistics. 5th ed. Boston, MA: Pearson/Allyn & Bacon; 2007. [Google Scholar]
- 41.National Institutes of Health. NIH policy on reporting race and ethnicity data: subjects in clinical research. 2001. [Accessed January 13, 2016]. Available from: http://grants.nih.gov/grants/guide/notice-files/NOT-OD-01-053.html.
- 42.Sabanayagam C, Shankar A, Buchwald D, Goins RT. Insomnia symptoms and cardiovascular disease among older American Indians: the Native Elder Care Study. J Envir Public Health. 2011;2011 doi: 10.1155/2011/964617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Farrell EI. Sleep disturbance as an independent predictor of suicidality in American Indian/Alaskan Native adolescents [Dissertation] Walden University. 2013. [Accessed January 13, 2016]. Available at: http://search.proquest.com/docview/1491163297.
- 44.Ruiter ME, DeCoster J, Jacobs L, Lichstein KL. Sleep disorders in African Americans and Caucasian Americans: a meta-analysis. Behav Sleep Med. 2010;8:246–59. doi: 10.1080/15402002.2010.509251. [DOI] [PubMed] [Google Scholar]
- 45.Katz DA, McHorney CA. Clinical correlates of insomnia in patients with chronic illness. Arch Intern Med. 1998;158:1099–107. doi: 10.1001/archinte.158.10.1099. [DOI] [PubMed] [Google Scholar]
- 46.Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep. 1995;18:425–32. doi: 10.1093/sleep/18.6.425. [DOI] [PubMed] [Google Scholar]
- 47.Kripke DF, Brunner R, Freeman R, et al. Sleep complaints of postmenopausal women. Clin J Women's Health. 2001;1:244–52. doi: 10.1053/cjwh.2001.30491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lehavot K, Hoerster KD, Nelson KM, Jakupcak M, Simpson TL. Health indicators for military, veteran, and civilian women. Am J Prev Med. 2012;42:473–80. doi: 10.1016/j.amepre.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 49.Peterson AL, Goodie JL, Satterfield WA, Brim WL. Sleep disturbance during military deployment. Mil Med. 2008;173:230–5. doi: 10.7205/milmed.173.3.230. [DOI] [PubMed] [Google Scholar]
- 50.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 51.Lichstein KL, Durrence HH, Riedel BW, Taylor DJ, Bush AJ. Mahwah, NJ: Erlbaum; 2004. Epidemiology of sleep: age, gender, and ethnicity. [Google Scholar]
- 52.Zhang B, Wing Y-K. Sex differences in insomnia: a meta-analysis. Sleep. 2006;29:85–93. doi: 10.1093/sleep/29.1.85. [DOI] [PubMed] [Google Scholar]
- 53.Plumb TR, Peachey JT, Zelman DC. Sleep disturbance is common among service members and veterans of Operations Enduring Freedom and Iraqi Freedom. Psychol Serv. 2013;11:209–19. doi: 10.1037/a0034958. [DOI] [PubMed] [Google Scholar]
- 54.Lavie P. Sleep disturbances in the wake of traumatic events. N Engl J Med. 2001;345:1825–32. doi: 10.1056/NEJMra012893. [DOI] [PubMed] [Google Scholar]
- 55.Ross RJ, Ball WA, Sullivan KA, Caroff SN. Sleep disturbance as the hallmark of posttraumatic stress disorder. Am J Psychiatry, 1989;146:697–707. doi: 10.1176/ajp.146.6.697. [DOI] [PubMed] [Google Scholar]
- 56.Spoormaker VI, Montgomery P. Disturbed sleep in post-traumatic stress disorder: secondary symptom or core feature? Sleep Med Rev. 2008;12:169–84. doi: 10.1016/j.smrv.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 57.Germain A, Buysse DJ, Nofzinger E. Sleep-specific mechanisms underlying posttraumatic stress disorder: integrative review and neurobiological hypotheses. Sleep Med Rev. 2008;12:185–95. doi: 10.1016/j.smrv.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Babson KA, Feldner MT. Temporal relations between sleep problems and both traumatic event exposure and PTSD: a critical review of the empirical literature. J Anxiety Disord. 2010;24:1–15. doi: 10.1016/j.janxdis.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Germain A. Sleep disturbances as the hallmark of PTSD: where are we now? Am J Psychiatry. 2013;170:372–82. doi: 10.1176/appi.ajp.2012.12040432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Taylor DJ. Insomnia and depression. Sleep. 2008;31:447–8. doi: 10.1093/sleep/31.4.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Perlis ML, Giles DE, Buysse DJ, Tu X, Kupfer DJ. Self-reported sleep disturbance as a prodromal symptom in recurrent depression. J Affect Disord. 1997;42:209–12. doi: 10.1016/s0165-0327(96)01411-5. [DOI] [PubMed] [Google Scholar]
- 62.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262:1479–84. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 63.Chang PP, Ford DE, Mead LA, Cooper-Patrick L, Klag MJ. Insomnia in young men and subsequent depression. The Johns Hopkins Precursors Study. Am J Epidemiol. 1997;146:105–14. doi: 10.1093/oxfordjournals.aje.a009241. [DOI] [PubMed] [Google Scholar]
- 64.Dryman A, Eaton WW. Affective symptoms associated with the onset of major depression in the community: findings from the US National Institute of Mental Health Epidemiologic Catchment Area Program. Acta Psychiatr Scand. 1991;84:1–5. doi: 10.1111/j.1600-0447.1991.tb01410.x. [DOI] [PubMed] [Google Scholar]
- 65.Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39:411–8. doi: 10.1016/0006-3223(95)00188-3. [DOI] [PubMed] [Google Scholar]
- 66.Roberts RE, Shema SJ, Kaplan GA, Strawbridge WJ. Sleep complaints and depression in an aging cohort: a prospective perspective. Am J Psychiatry. 2000;157:81–8. doi: 10.1176/ajp.157.1.81. [DOI] [PubMed] [Google Scholar]
- 67.Weissman MM, Greenwald S, Nino-Murcia G, Dement WC. The morbidity of insomnia uncomplicated by psychiatric disorders. Gen Hosp Psychiatry. 1997;19:245–50. doi: 10.1016/s0163-8343(97)00056-x. [DOI] [PubMed] [Google Scholar]
- 68.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–9. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 69.Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rossler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31:473–80. doi: 10.1093/sleep/31.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res. 2006;40:700–8. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 71.Budhiraja R, Roth T, Hudgel DW, Budhiraja P, Drake CL. Prevalence and polysomnographic correlates of insomnia comorbid with medical disorders. Sleep. 2011;34:859–67. doi: 10.5665/SLEEP.1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Affleck G, Urrows S, Tennen H, Higgins P, Abeles M. Sequential daily relations of sleep, pain intensity, and attention to pain among women with fibromyalgia. Pain. 1996;68:363–8. doi: 10.1016/s0304-3959(96)03226-5. [DOI] [PubMed] [Google Scholar]
- 73.McCracken L, Iverson G. Disrupted sleep patterns and daily functioning in patients with chronic pain. Pain Res Manag. 2001;7:75–9. doi: 10.1155/2002/579425. [DOI] [PubMed] [Google Scholar]
- 74.Moldofsky H. Sleep and pain. Sleep Med Rev. 2001;5:385–96. doi: 10.1053/smrv.2001.0179. [DOI] [PubMed] [Google Scholar]
- 75.Friedman GD, Ury HK, Klatsky AL, Siegelaub A. A psychological questionnaire predictive of myocardial infarction: results from the Kaiser-Permanente epidemiologic study of myocardial infarction. Psychosom Med. 1974;36:327–43. doi: 10.1097/00006842-197407000-00007. [DOI] [PubMed] [Google Scholar]
- 76.Phillips B, Mannino DM. Do insomnia complaints cause hypertension or cardiovascular disease? J Clin Sleep Med. 2007;3:489–94. [PMC free article] [PubMed] [Google Scholar]
- 77.Schwartz S, Anderson WM, Cole SR, Cornoni-Huntley J, Hays JC, Blazer D. Insomnia and heart disease: a review of epidemiologic studies. J Psychosom Res. 1999;47:313–33. doi: 10.1016/s0022-3999(99)00029-x. [DOI] [PubMed] [Google Scholar]
- 78.Jarrett M, Heitkemper M, Cain KC, Burr RL, Hertig V. Sleep disturbance influences gastrointestinal symptoms in women with irritable bowel syndrome. Dig Dis Sci. 2000;45:952–9. doi: 10.1023/a:1005581226265. [DOI] [PubMed] [Google Scholar]
- 79.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2012. [Google Scholar]
- 80.Lichstein KL, Durrence HH, Taylor DJ, Bush AJ, Riedel BW. Quantitative criteria for insomnia. Behav Res Ther. 2003;41:427–45. doi: 10.1016/s0005-7967(02)00023-2. [DOI] [PubMed] [Google Scholar]
- 81.Edinger JD, Bonnet MH, Bootzin RR, et al. Derivation of research diagnostic criteria for insomnia: report of an American Academy of Sleep Medicine Work Group. Sleep. 2004;27:1567–96. doi: 10.1093/sleep/27.8.1567. [DOI] [PubMed] [Google Scholar]
- 82.Troxel WM, Shih RA, Pedersen E, et al. Santa Monica, CA: RAND Corporation; 2015. [Accessed July 11, 2016]. Sleep in the military: promoting healthy sleep among U.S. service members. Available at http://www.rand.org/pubs/research_reports/RR739.html#download. [Google Scholar]


