Abstract
Background
Inadequate sleep quantity and quality are associated with a higher risk of type 2 diabetes. This relationship is not well-examined in US Hispanics/Latinos, and prior analyses may be confounded by sleep apnea. This cross-sectional study examined joint associations of sleep duration and insomnia with diabetes among diverse US Hispanic/Latinos.
Methods
Baseline data on sleep quantity and quality were obtained from 15227 participants (mean age 41; range 18–74 years) from the Hispanic Community Health Study/Study of Latinos. Complex survey multinomial logistic regression was used to examine associations between prevalent diabetes and six phenotypes defined by cross-classifying sleep duration (short ≤6 h, average >6–9 h, long >9 h) and insomnia, adjusting for sex, age, site and Hispanic/Latino background interaction, education, physical activity, diet quality, and sleep apnea.
Results
In the weighted population, 14% had diabetes, 28% had insomnia, 9% were short sleepers, and 19% were long sleepers. Compared with those with average sleep and no insomnia, those with short sleep and insomnia were more likely to have diabetes (odds ratio [OR] 1.46; 95% confidence interval [CI] 1.02, 2.11). Average sleepers with insomnia (1.28; 95% CI 1.02, 1.61) and long sleepers without insomnia (1.33; 95% CI 1.07, 1.65) also had elevated odds of diabetes. Further adjustment for body mass index attenuated associations, except with long sleep without insomnia.
Conclusions
Both decreased quantity and quality of sleep are associated with diabetes in Hispanic/Latinos, with the greatest odds among those with short sleep duration and insomnia. The association is largely explained by obesity.
Keywords: acculturation, Hispanic Americans, insomnia, sleep, type 2 diabetes mellitus
Introduction
Hispanic/Latinos, the largest US minority group,1 are 66% more likely to have type 2 diabetes (T2D) and develop it at younger ages than non-Hispanic Whites.2 Understanding modifiable risk factors in this population can inform interventions to reduce health disparities. Sleep has emerged as a novel prevention target.3 Both quality and quantity of sleep are associated with T2D,4 weight gain,5 obesity, coronary heart disease, and stroke.6,7 In experimental and observational studies, shortened or disturbed sleep has been related to glucose intolerance, insulin resistance, and reduced acute insulin response to glucose, thus predisposing individuals to T2D.8–11 These results may be mediated through effects on adipose tissue function, because reduced sleep duration affects the secretion of hormones that regulate inflammation and insulin resistance.12
Recent work by Vgontzas et al.13 indicates that the combination of short sleep duration with insomnia may be associated with the highest risk of hypertension and diabetes, suggesting examination of both quality and quantity of sleep is warranted. The increased cognitive–physiological arousal and activation of the hypothalamic–pituitary–adrenal axis characteristic of this phenotype is associated with a higher risk of hypertension, diabetes, and mortality.14 Short sleep duration with insomnia may reflect an underlying pathologic condition that persists over time, whereas average or longer sleep durations with insomnia may be more responsive to psychological intervention alone. Yet, few studies have examined joint associations of sleep duration and insomnia with chronic diseases.15 Further, prior studies on the metabolic impact of poor sleep quantity or quality have not addressed confounding by sleep apnea, a common sleep disorder associated with poor sleep and T2D.16,17
Although racial or ethnic disparities in sleep quantity or quality are gaining attention,18–20 sleep duration and insomnia are not well studied among diverse Hispanic/Latinos.21 Prior studies included mainly Mexican Americans, with small numbers of other Hispanic/Latino participants.22 Limited literature suggests sleep characteristics vary according to ethnic heritage22–24 and by nativity25–27 and language preference.28 For example, in the National Health and Nutrition Survey (NHANES), the relationship between objective hypertension and very short sleep duration (<5 h/night, self-reported) was only seen among non-Mexican Hispanics/Latinos, but not in the largest subgroup (Mexican Americans).29 These results indicate potential differences according to Hispanic/Latino background before taking nativity into account. Interestingly, US-born Mexican Americans reported shorter sleep duration and more insomnia compared with Mexican-born immigrants in the NHANES.26
The present study examined the joint associations of sleep quantity (self-reported duration) and quality (insomnia) with prevalent diabetes among diverse US Hispanic/Latino adults, adjusting for sleep apnea and potential confounders. Secondary analyses assessed whether associations varied by acculturation level (nativity and language preference) or were attenuated by adjustment for body mass index (BMI), a potential pathway through which sleep may relate to diabetes. We hypothesized that individuals with reduced quantity or quality of sleep have higher odds of diabetes, that associations are stronger among more acculturated individuals, and that adjustment for would BMI attenuate the associations.
Methods
Study population
The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) is a population-based study that recruited 16 415 Hispanic/Latinos aged 18–74 years between March 2008 and June 2011 from randomly selected households in four US communities (Bronx, NY; Chicago, IL; Miami, FL; San Diego, CA). Households were selected using a stratified two-stage area probability design to ensure a representative sample, as described previously.30 Participants included Hispanic/Latinos from Cuban, Dominican, Mexican, Puerto Rican, Central American, and South American backgrounds. The study was approved by institutional review boards at each institution. Written informed consent was obtained from all participants.
The present cross-sectional analysis included 15 227 participants after excluding participants with missing data on diabetes (n = 21), BMI (n = 71), insomnia (n = 560), weekend or weekday sleep duration (n = 885), and possible type 1 diabetes (n = 33, diagnosis before 30 years of age and insulin as first medication). Analyses where HbA1c was the outcome excluded participants missing HbA1c (n = 97). Those excluded compared with those included had similar health and demographic characteristics, but diabetes prevalence differed (19% vs 14%).
Glycemic status
Baseline examinations included questionnaires (in Spanish or English), anthropometry, and a blood draw, as detailed previously.30,31 Because sleep duration affects insulin resistance, we classified glycemic status into a three-category outcome, separating diabetics from pre-diabetics and normoglycemics, according to the 2010 American Diabetes Association guidelines.32 As in previous HCHS/SOL publications,33 diabetes was defined as fasting glucose ≥126 mg/dL or 2-h post-load glucose ≥200 mg/dL or HbA1c ≥6.5% or the use of hypoglycemic medications; prediabetes was defined as fasting glucose of 100–125 mg/dL or 2-h post-load glucose of 140–200 mg/dL or HbA1c between 5.7% and <6.5% among subjects without diabetes; and normoglycemia was defined as fasting glucose <100 mg/dL, 2-h post-load glucose <140 mg/dL, HbA1c <5.7%, and no hypoglycemic medications.
Sleep assessment
We assessed sleep quality using a five-item validated and reliable instrument, namely the Women’s Health Initiative Insomnia Rating Scale (WHIIRS), dichotomized at 10 and abbreviated throughout as “insomnia”.34 The WHIIRS asks participants to rank the severity of different insomnia symptoms (e.g. sleep latency, sleep maintenance, early morning awakening, and sleep quality) on a five-point scale through the following questions: “Did you have trouble falling asleep?”; “Did you wake up several times at night?”; “Did you wake up earlier than you planned to?”; “Did you have trouble getting back to sleep after you woke up too early?”; and “Overall, was your typical night’s sleep during the past 4 weeks: very sound or restful; sound or restful; average quality; restless; or very restless?”
To assess sleep quantity, participants were prompted to consider “the times you get in and out of bed in order to sleep (not including naps)” and asked to report habitual bed and wake times separately for weekdays and weekends in response to the following questions: “What time do you usually go to bed?” and “What time do you usually wake up?” The difference between wake-time and bedtime was calculated for weekdays and weekends separately and combined in a weighted average. Sleep duration was categorized as short (<6 h), average (6–9 h) or long (>9 h). For our main exposure, we assigned participants to one of six sleep phenotypes defined on the basis of sleep duration (short, average or long) and presence (WHIIRS >10) or absence (WHIIRS < 10) of insomnia.
Covariate assessment
Body mass index was calculated as weight (in kg) divided by height squared (m2) based on research measurements obtained at the in-person baseline visit. Information was obtained by interviewer-administered questionnaires on demographics, socioeconomics (education and household income), smoking, self-reported physical activity, medical history and medication, language preference at survey completion (Spanish or English), and nativity (born in 50 US states or Washington DC vs born outside mainland US, including Puerto Rico). Education was categorized as less than high school, high school diploma, or greater than high school education. Physical activity was categorized as high, moderate or low (metabolic equivalent units for days/week of recreational or work physical activity) through the Global Physical Activity Questionnaire.35 Missing values for education (n = 29) or physical activity (n = 48) were assigned to the largest category, “less than high school” and “low physical activity.”
Dietary intake was ascertained by two 24-h dietary recalls, administered approximately 6 weeks apart. The Alternate Healthy Eating Index 2010 (AHEI-2010) measured diet quality.36 Higher AHEI-2010 scores (range 0–110) represent healthier diets. Missing observations (n = 144) were assigned to the mean (48.97).
Participants used a home or portable sleep apnea monitor for one night. As described previously,24 this device measures airflow, hemoglobin oxygen saturation and pulse rate, head movement and position, and snoring, but cannot assess sleep duration.37 Sleep apnea severity was assessed using the apnea–hypopnea index (AHI; respiratory events/sleep hour, counting hypopneas with desaturation >3%). We used a three-category variable: moderate–severe obstructive sleep apnea (AHI >15 events/h); mild–no sleep apnea (<15 events/h); and a missing indicator category (n = 1654).
Statistical analyses
All values other than sample size were weighted, adjusting for probability of selection and non-response using complex survey procedures in SAS 9.3 (SAS Institute, Cary, NC, USA).30 Weights are the product of a “base weight” (inverse selection probability) and adjustments: (i) non-response relative to sampling frame; (ii) trimming to handle extreme values; and (iii) calibration to 2010 US Census for age, sex, and Hispanic background. Adjustment results in statistics representative of the target population: Hispanic/Latino adults 18–74 years residing in HCHS/SOL sites.
Descriptive characteristics were computed overall and by sleep phenotype. Multinomial logistic regression identified predictors of diabetes, prediabetes, or normoglycemia. Linear regression identified predictors of HbA1c levels. Models adjusted for sex, age, cross-classification of recruitment site and Hispanic/Latino background, education, physical activity, diet, and sleep apnea. Body mass index, a potential mediator, was added in secondarily. The degree of attenuation with adjustment for BMI was interpreted as an indirect effect of sleep on diabetes status through BMI.
Sensitivity analyses
We excluded participants conducting night-shift work; circadian disruption increases diabetes independent of shortened sleep in shift workers.38 Because there is no accepted threshold for “short” or “long” sleep durations, we repeated analyses defining sleep duration in the following alternative categories: short (<5 h), average (5–8 h) or long (>8 h). In case of residual confounding by sleep apnea severity, we considered adjustment for AHI as a continuous variable. To assess whether the results may be mediated through psychological distress, we also considered adjustment for anxiety (10-item State-Trait Anxiety Inventory [STAI-10]39 summary score) and depressive symptoms (10-item Center for Epidemiologic Studies Depression [CES-D10]40 scale, calculated excluding restless sleep for a total possible score of 27). To reduce reverse causation, we excluded participants with HbA1c >10% and then separately excluded those with diagnosed diabetes >10 years; hyperglycemic nocturia and peripheral neuropathy disrupt sleep. Before conducting analyses stratified by acculturation (language and nativity), we used likelihood ratio tests (LRT) to compare models with and without product terms of sleep phenotypes with these measures. Because our sample included diverse Hispanic/Latino subgroups, we further tested product terms of each sleep phenotype with each Hispanic/Latino background.
Results
Participant characteristics accounting for sampling weights are given in Table 1. Compared with those without insomnia, all groups reporting insomnia had a higher proportion of females and older age. Short sleepers without insomnia had the lowest unemployment, whereas long sleepers without insomnia were younger with the lowest mean BMI. Regardless of insomnia, long sleepers were the least physically active group; short sleepers were the most active. The prevalence of moderate–severe sleep apnea did not differ by sleep phenotype, although insomnia groups had higher indices of apnea or hypopnea.
Table 1.
Demographic and health characteristics by sleep phenotype, Hispanic Community Health Study/Study of Latinos (HCHS/SOL) 2008–11
| Overall | Short sleep, insomnia | Long sleep, insomnia | Average sleep, insomnia | Short sleep, no insomnia | Long sleep, no insomnia | Average sleep, no insomnia | |
|---|---|---|---|---|---|---|---|
| No. subjects | 15 227 | 661 (4%) | 840 (6%) | 3262 (21%) | 793 (5%) | 1923 (13%) | 7748 (51%) |
| Exposures | |||||||
| Sleep duration (h/day) | 8.0 (7.9, 8.0) | 5.2 (5.2, 5.3) | 10.1 (10, 10.2) | 7.8 (7.7, 7.8) | 5.4 (5.3, 5.5) | 10.0 (9.9, 10.0) | 7.8 (7.8, 7.8) |
| WHIIRS | 6.7 (6.6, 6.9) | 14.9 (14.5, 15.3) | 13.8 (13.5, 14) | 13.5 (13.4, 13.7) | 4.0 (3.6, 4.3) | 3.8 (3.6, 4) | 3.9 (3.8, 4) |
| Demographics | |||||||
| Age (years) | 41.1 (40.6, 41.6) | 45.1 (42.9, 47.2) | 43.0 (41.4, 44.6) | 45.0 (44.1, 45.9) | 41.5 (40.0, 42.9) | 35.9 (34.9, 36.9) | 40.5 (39.9, 41.1) |
| Women (%) | 52.3 (51.1, 53.4) | 57.8 (51.8, 63.9) | 66.1 (61.5, 70.6) | 60.4 (57.8, 63.1) | 41.7 (36.1, 47.3) | 53.7 (50.5, 56.9) | 48.2 (46.5, 49.8) |
| Ethnic heritage (%) | |||||||
| Dominican | 9.5 (8.1, 10.9) | 12.3 (8.8, 15.8) | 11.6 (8.6, 14.5) | 11.1 (9.1, 13.2) | 8.2 (4.9, 11.4) | 9.6 (7.4, 11.8) | 8.6 (7.2, 10.0) |
| Central/South American | 12.2 (10.9, 13.6) | 9.1 (6.3, 11.9) | 9.9 (7.3, 12.5) | 11.1 (9.5, 12.7) | 14 (10.7, 17.3) | 11.1 (9.1, 13) | 13.3 (11.8, 14.9) |
| Cuban | 19.8 (16.5, 23.1) | 20.3 (14.8, 25.8) | 18.9 (14.5, 23.4) | 21.4 (17.3, 25.5) | 16.3 (12.1, 20.4) | 19.5 (15.6, 23.4) | 19.7 (16.1, 23.2) |
| Mexican | 38.4 (35.2, 41.7) | 21.1 (15.3, 26.8) | 33.8 (28.3, 39.2) | 30.1 (26.4, 33.7) | 35.5 (29, 41.9) | 41.7 (37.2, 46.2) | 42.7 (39, 46.4) |
| Puerto Rican | 15.9 (14.3, 17.5) | 31.8 (24.2, 39.4) | 21.6 (17.7, 25.5) | 22.1 (19.3, 24.8) | 19.3 (13.9, 24.7) | 13.9 (11.5, 16.2) | 12.1 (10.6, 13.6) |
| Other/more than one | 4.1 (3.5, 4.7) | 5.5 (2.1, 8.9) | 4.3 (2.2, 6.3) | 4.3 (2.9, 5.7) | 6.8 (2.3, 11.3) | 4.2 (2.9, 5.6) | 3.6 (2.9, 4.3) |
| Born in mainland US† (%) | 22.7 (21.2, 24.3) | 26.4 (19.9, 32.9) | 25.5 (21.1, 29.8) | 23.5 (20.9, 26.1) | 22.1 (17.7, 26.4) | 30.0 (26.8, 33.3) | 20.0 (18.2, 21.7) |
| English-Preference (%) | 25.2 (23.4, 27) | 28.3 (21.6, 35.1) | 29.4 (24.4, 34.3) | 27.0 (23.9, 30.1) | 30.4 (24.4, 36.3) | 29.0 (25.8, 32.2) | 22.3 (20.3, 24.2) |
| Married or partnered (%) | 49.2 (47.7, 50.8) | 40.9 (35.1, 46.7) | 39.2 (34.2, 44.2) | 47.2 (44.5, 49.8) | 50.3 (44.7, 55.9) | 41.4 (38.3, 44.6) | 53.6 (51.6, 55.7) |
| >High school or GED (%) | 39.6 (37.9, 41.2) | 35.2 (28.7, 41.6) | 30.6 (26.1, 35.1) | 41.3 (38.5, 44.0) | 35.9 (31, 40.9) | 36.8 (33.6, 39.9) | 41.2 (38.9, 43.5) |
| Household income <US$30 000/year (%) | 60.9 (59, 62.8) | 66.2 (60.2, 72.1) | 72.0 (67.8, 76.3) | 64.3 (61.4, 67.2) | 58.2 (52.4, 63.9) | 63.5 (60.2, 66.7) | 57.7 (55.1, 60.3) |
| % Unemployed (not retired) | 40.8 (39.4, 42.3) | 40.6 (34.7, 46.5) | 58.7 (53.9, 63.4) | 44.1 (41.2, 47) | 28.7 (23.5, 33.9) | 53.6 (50.3, 57) | 35.7 (33.9, 37.4) |
| Health attributes | |||||||
| AHI‡ | 5.5 (5.2, 5.8) | 6.6 (5.0, 8.2) | 5.8 (4.3, 7.2) | 6.2 (5.5, 7.0) | 5.5 (4.6, 6.4) | 4.5 (3.9, 5.0) | 5.4 (5.0, 5.8) |
| AHEI-2010 | 47.6 (47.2, 47.9) | 46.3 (45.5, 47.1) | 46.7 (46.0, 47.4) | 47.4 (46.9, 47.9) | 47.1 (46.2, 48.1) | 46.6 (46, 47.1) | 48.1 (47.7, 48.6) |
| BMI (kg/m2) | 29.3 (29.2, 29.5) | 30.9 (30.1, 31.8) | 29.7 (29.2, 30.3) | 30.0 (29.7, 30.4) | 30.1 (29.3, 31.0) | 28.4 (28.1, 28.8) | 29.1 (28.9, 29.3) |
| Low physical activity§ (%) | 41.9 (40.7, 43.2) | 33.9 (28.4, 39.4) | 50.6 (45.9, 55.3) | 44.9 (42.3, 47.4) | 36.2 (31.4, 40.9) | 45.7 (42.5, 48.9) | 40.1 (38.3, 41.9) |
Data are given as the mean or percentage with 95% confidence intervals in parentheses. All values are weighted for study design and non-response, except the number and percentage of individuals in each sleep phenotype category.
Participants born in Puerto Rico were considered to be born outside mainland US.
The sleep apnea–hypopnea index (AHI; 3% desaturation); AHI 0–5, normal range; 5 < AHI < 15 mild sleep apnea; 15 < AHI < 30 moderate sleep apnea; AHI >30, severe sleep apnea.
Self-reported physical activity from the Global Physical Activity Questionnaire, which was categorized as high, medium or low according to the metabolic equivalent units for moderate or vigorous intensity work and leisure activities in a typical week.
GED, general education degree; AHEI-2010, Alternative Healthy Eating Index, 2010 (range 0–110); BMI, body mass index; WHIIRS, Women’s Health Initiative Insomnia Rating Score; average S sleep, >6–9 h/night; short sleep, <6 h/night; long sleep, >9 h/night; insomnia (WHIIRS >10).
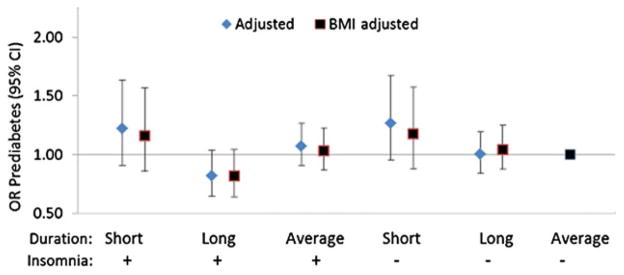
Figure 1 shows associations of sleep phenotypes with diabetes status, with and without adjustment for BMI. Before BMI adjustment, compared with average sleep duration and no insomnia, all other phenotypes had higher odds of diabetes. As hypothesized, short sleepers with insomnia had the greatest odds ratio [OR] for diabetes (1.46; 95% confidence interval [CI] 1.02, 2.11) compared with normoglycemia. The corresponding OR for average sleepers with insomnia (1.28; 95% CI 1.02, 1.61), long sleepers with insomnia (1.33; 95% CI 0.99, 1.78) and long sleepers without insomnia (1.33; 95% CI 1.07, 1.65) were of similar magnitude, whereas the OR for short sleepers without insomnia was 1.16 (95% CI 0.84, 1.59). Adjustment for BMI attenuated all associations, except long sleep without insomnia (OR 1.39; 95% CI 1.11, 1.74). No association was identified with any phenotype and prediabetes (Fig. 2).
Figure 1.
Odds ratios (OR) and 95% confidence intervals (CI) for diabetes as predicted by sleep phenotype. Adjusted, results from a single multinomial logistic regression model treating diabetes status as a polytomous outcome (diabetes, prediabetes or normoglycemia [reference]), adjusted for study design, non-response, cross-classification of site of recruitment and Hispanic/Latino background, age, sex, educational attainment, diet quality, self-reported physical activity level, apnea–hypopnea index; BMI adjusted, results are from a second multinomial logistic regression model further adjusted for body mass index (BMI). Average sleep, >6–9 h/night; short sleep, <6 h/night; long sleep, >9 h/night; insomnia (Women’s Health Initiative Insomnia Rating Scale >10).
Figure 2.
Odds ratios (OR) and 95% confidence intervals (CI) for prediabetes as predicted by sleep phenotype. Adjusted, results from a single multinomial logistic regression model treating diabetes status as a polytomous outcome (diabetes, prediabetes, or normoglycemia [reference]), adjusted for study design, non-response, cross-classification of site of recruitment and Hispanic/Latino background, age, sex, educational attainment, diet quality, self-reported physical activity level, apnea/hypopnea index; BMI adjusted, results from a second multinomial logistic regression model further adjusted for body mass index (BMI). Average sleep, >6–9 h/night; short sleep, <6 h/night; long sleep, >9 h/night; insomnia (Women’s Health Initiative Insomnia Rating Scale >10).
The effect of insomnia, regardless of sleep duration, was similar across acculturation levels (Table 2). Although confidence intervals overlapped, a difference was noted in short sleepers without insomnia. English speakers and US born with short sleep but no insomnia had the highest odds of diabetes (OR 1.75 [95% CI 0.88, 3.48; NS] and 2.26 [95% CI 1.03, 4.95]), whereas among Spanish speakers and non-US born, no association of short sleep without insomnia and diabetes was identified (OR 1.01 [95% CI 0.72, 1.42] and 1.00 [95% CI 0.72, 1.38]). There was statistical evidence of an interaction for both nativity (LRT P < 0.0001) and language preference (LRT P = 0.0003).
Table 2.
Diabetes status as predicted by sleep phenotype: Results by acculturation
| Short sleep, insomnia | Long sleep, insomnia | Average sleep, insomnia | Short sleep, no insomnia | Long sleep, no insomnia | Average sleep, no insomnia | |
|---|---|---|---|---|---|---|
| Spanish language preference (n = 12197) | ||||||
| Diabetes | 1.54 (1.05, 2.28) | 1.34 (0.98, 1.84) | 1.28 (1.00, 1.63) | 1.01 (0.72, 1.42) | 1.31 (1.03, 1.67) | 1.00 (ref) |
| Prediabetes | 1.17 (0.84, 1.63) | 0.82 (0.63, 1.06) | 1.11 (0.93, 1.31) | 1.12 (0.85, 1.48) | 0.91 (0.75, 1.09) | 1.00 (ref) |
| English language preference (n = 3030) | ||||||
| Diabetes | 1.22 (0.54, 2.78) | 1.32 (0.65, 2.68) | 1.27 (0.76, 2.13) | 1.75 (0.88, 3.48) | 1.16 (0.69, 1.95) | 1.00 (ref) |
| Prediabetes | 1.45 (0.82, 2.56) | 0.86 (0.52, 1.41) | 1.00 (0.67, 1.51) | 1.75 (0.95, 3.23) | 1.35 (0.96, 1.91) | 1.00 (ref) |
| Born outside mainland US (n = 12568) | ||||||
| Diabetes | 1.45 (0.98, 2.16) | 1.39 (1.00, 1.92) | 1.32 (1.04, 1.67) | 1.00 (0.72, 1.38) | 1.38 (1.10, 1.74) | 1.00 (ref) |
| Prediabetes | 1.24 (0.90, 1.70) | 0.82 (0.64, 1.05) | 1.06 (0.89, 1.26) | 1.22 (0.90, 1.66) | 0.91 (0.76, 1.09) | 1.00 (ref) |
| US born (n = 2645) | ||||||
| Diabetes | 1.53 (0.76, 3.05) | 1.21 (0.61, 2.40) | 1.03 (0.62, 1.71) | 2.26 (1.03, 4.95) | 0.77 (0.41, 1.44) | 1.00 (ref) |
| Prediabetes | 1.18 (0.63, 2.23) | 0.86 (0.48, 1.53) | 1.13 (0.77, 1.67) | 1.38 (0.78, 2.44) | 1.36 (0.95, 1.96) | 1.00 (ref) |
Data are given as odds ratios with 95% confidence intervals in parentheses for polytomous outcome (diabetes or prediabetes vs normoglycemia). Odds ratios that differ significantly from 1 are bolded.
Results from multinomial logistic regressions on the polytomous outcome diabetes status (diabetes, prediabetes or normoglycemia [reference]), adjusted for study design, non-response, cross-classification of site of recruitment and Hispanic/Latino background, age, sex, educational attainment, diet quality, self-reported physical activity level, and apnea–hypopnea index. Models were fit separately by language preference and nativity.
Average sleep, >6–9 h/night; short sleep, <6 h/night; long sleep, >9 h/night; insomnia (Women’s Health Initiative Insomnia Rating Scale >10).
As a secondary outcome, we examined associations of sleep phenotypes with HbA1c separately among participants with and without diabetes (Table 3). Among diabetics, short sleepers with insomnia had worse glycemic control compared with average sleepers without insomnia: mean HbA1c percentage difference of 0.47 (95% CI 0.13, 0.81). Among diabetics, those with insomnia and average or long sleep had a lesser change in HbA1c levels (not significant), whereas no association was found when insomnia was absent. A borderline significant association between short sleep without insomnia and higher HbA1c was observed among non-diabetic individuals before adjustment for BMI.
Table 3.
HbA1c as predicted by sleep phenotype: Results by diabetes status (n = 15 058)
| Short sleep, insomnia | Long sleep, insomnia | Average sleep, insomnia | Short sleep, no insomnia | Long sleep, no insomnia | Average sleep, no insomnia | |
|---|---|---|---|---|---|---|
| Mean difference (95% CI) in HbA1c (%) versus average sleep and no insomnia | ||||||
| Diabetes (n = 2910) | ||||||
| Adjusted model | 0.47 (0.13, 0.81) | 0.22 (−0.20, 0.63) | 0.27 (−0.06, 0.60) | 0.05 (−0.47, 0.58) | 0.06 (−0.25, 0.38) | 0.00 (Reference) |
| Adjusted model + BMI | 0.48 (0.14, 0.82) | 0.27 (−0.15, 0.69) | 0.26 (−0.06, 0.58) | 0.04 (−0.49, 0.57) | 0.05 (−0.27, 0.37) | 0.00 (Reference) |
| Prediabetes and normoglycemia (n = 12 148) | ||||||
| Adjusted model | 0.04 (−0.01, 0.10) | 0.00 (−0.03, 0.03) | 0.00 (−0.02, 0.02) | 0.04 (0.00, 0.08) | 0.00 (−0.03, 0.02) | 0.00 (Reference) |
| Adjusted model + BMI | 0.03 (−0.02, 0.08) | 0.00 (−0.03, 0.03) | 0.00 (−0.02, 0.02) | 0.03 (−0.01, 0.07) | 0.00 (−0.02, 0.03) | 0.00 (Reference) |
| Mean difference (95% CI) in HbA1c (mmol/mol) versus average sleep and no insomnia | ||||||
| Diabetes (n = 2910) | ||||||
| Adjusted model | 5.19 (1.50, 8.87) | 2.37 (−2.15, 6.89) | 2.93 (−0.66, 6.51) | 0.53 (−5.22, 6.27) | 0.64 (−2.79, 4.08) | 0.00 (Reference) |
| Adjusted model + BMI | 5.48 (1.70, 9.25) | 2.53 (−1.98, 7.04) | 2.97 (−0.60, 6.54) | 0.66 (−5.16, 6.47) | 0.53 (−2.92, 3.99) | 0.00 (Reference) |
| Prediabetes and normoglycemia (n = 12 148) | ||||||
| Adjusted model | 0.45 (−0.12, 1.01) | −0.05 (−0.41, 0.31) | 0.04 (−0.20, 0.28) | 0.46 (0.01, 0.91) | −0.05 (−0.32, 0.23) | 0.00 (Reference) |
| Adjusted model + BMI | 0.32 (−0.22, 0.86) | −0.03 (−0.40, 0.34) | −0.03 (−0.27, 0.21) | 0.34 (−0.12, 0.79) | 0.02 (−0.25, 0.29) | 0.00 (Reference) |
Results from linear regression fit separately among diabetic and non-diabetic participants, adjusted for study design, non-response, cross-classification of site of recruitment and Hispanic/Latino background, age, sex, educational attainment, diet quality, self-reported physical activity level, apnea–hypopnea index, and, where indicated, for body mass index (BMI).
Odds ratios that differ significantly from 1 are bolded.
Average sleep, >6–9 h/night; short sleep, <6 h/night; long sleep, >9 h/night; insomnia (Women’s Health Initiative Insomnia Rating Scale >10); CI, confidence interval.
In sensitivity analyses, excluding participants reporting night-shift work (n = 1361) slightly strengthened associations of sleep phenotypes with diabetes, whereas excluding HbA1c >10% (n = 405) or diabetes >10 years (n = 864) attenuated estimates. Further adjustment for the STAI-10 and CES-D10 did not alter estimates by >10%. When the threshold for short sleep duration was lowered to <5 h/night, estimates did not differ substantially, although associations of short sleep with insomnia and diabetes were strengthened (OR 2.23; 95% CI 1.23–4.04); importantly, relatively few participants reported sleep durations this short (n = 294). No evidence of interaction between sleep phenotype and Hispanic/Latino background was detected (LRT Pinteraction = 0.57).
Discussion
In the present community-based study of 15 227 US Hispanic/Latino adults, combinations of sleep duration and insomnia were associated with prevalent diabetes compared with average sleep without insomnia. Although associations were strongest for short sleep with insomnia, confidence intervals overlapped. Pathways likely differ, with an important mediating role for obesity in most but not all phenotypes; this is suggested by the attenuation and non-significant associations of all sleep phenotypes after adjustment for BMI, except long sleep without insomnia.
Limited research suggests that short sleep is a risk factor for diabetes among Hispanics/Latinos.41 Regarding sleep quality, a report from the Behavioral Risk Factor Surveillance System, which included primarily Mexican Americans and used a single non-validated question for sleep quality and self-reported diabetes, estimated that the OR for diabetes was 1.88 (95% CI 1.46, 2.42) reporting insufficient rest or sleep for the prior month compared with those with sufficient rest or sleep among Hispanic/Latinos.6 Similar to our finding that diabetic short sleepers with insomnia had elevated HbA1c, a cross-sectional study (n = 571 Caucasian and African Americans) found insomnia was associated with higher fasting glucose and insulin, but only among diabetics.42
The present study found the strongest associations with diabetes for short sleepers with insomnia. In keeping with this, Vgontzas et al.13 found, using polysomnography (n = 1741 mostly Caucasians), that individuals reporting insomnia who slept <5 h/night (vs no insomnia and >6 h/night) had the highest odds of diabetes (OR 2.95; 95% CI 1.2, 7.0).13 Consistent with these results, lowering the threshold for short sleep duration to <5 h/night strengthened associations of short sleep and insomnia with diabetes in the present study. The combination of self-reported short sleep with insomnia may identify severe insomnia and/or the presence of chronic psychological stress, which compounds the physiological hyperarousal in insomnia (e.g. hyperactivity of the hypothalamic–pituitary–adrenal and sympatho–adrenal–medullary axes) and leads to more severe consequences.14 However, adjustment for anxiety and depressive symptoms in sensitivity analyses did not substantially alter the point estimates.
After controlling for obesity, associations of diabetes with short sleep and insomnia (and with all other sleep phenotypes except long sleep without insomnia) were attenuated and became non-significant. This is consistent with mounting literature linking sleep duration to weight gain.43 In addition to excess adiposity, short sleep can decrease glucose tolerance and insulin sensitivity.9 With chronic sleep curtailment, the increased load on the pancreas from insulin resistance may tax β-cell function, leading to T2D. Both insomnia and short sleep duration have been related to changes in leptin and ghrelin, which could stimulate hunger and energy intake and contribute to obesity and impaired glucose regulation.9,13 Although the contribution of insomnia to weight gain and insulin resistance independent of or in combination with extremes of sleep duration is not as well studied, our results are consistent with obesity mediating the association between poor sleep and diabetes. We observed elevated BMI among all sleep phenotypes other than long sleep with or without insomnia and elevated odds of obesity among average (OR 1.16; 95% CI 1.02, 1.32) and short (OR 1.50; 95% CI 1.14, 1.96) sleepers with insomnia, but not other groups (data not shown).
Importantly, confidence intervals for sleep phenotypes overlapped and estimated diabetes odds were elevated for all forms of disturbed sleep, including long sleep without insomnia. In the case of long sleep, some,44 but not all,45 prospective studies observe associations with T2D. Long sleep may reflect underlying illness, sleep disorders such as insomnia or sleep apnea,46 or confounding: low exercise and extremes of alcohol intake are associated with long sleep and increased risk for T2D and other morbidities.46,47 However, adjustment for alcohol, physical activity, sleep apnea, and BMI did not weaken estimated associations with long sleep, and the strongest associations were seen for long sleepers without insomnia. Importantly, in the present study sleep duration was assessed as habitual bed minus wake time and not all time in bed is spent asleep, and this may be particularly true for self-reported long sleepers. Consistent with this, Youngstedt and Jean-Louis48 suggest excessive time in bed has detrimental effects on health that account for the association between long sleep and increased morbidity and mortality.48 Results suggest the underlying causes of disturbed sleep differ for different phenotypes and warrant further investigation.
Acculturation may modify the association of sleep phenotypes with diabetes status. Short sleep without insomnia had an association with diabetes among more acculturated individuals that was not present among those born outside the mainland US or those who were Spanish speaking; however, it is important to note that the confidence intervals overlapped substantially. Chronic short sleep without insomnia may result from voluntary sleep restriction due to work, recreational media use, or other causes. Although estimated associations did not change with adjustment for employment, the proportion of participants who reported full-time employment was highest in the short sleep without insomnia category, suggesting work schedules may be one cause. Acculturation is also associated with prolonged television viewing,49 perhaps contributing to shorter or disturbed sleep.50 These results underscore the need to distinguish separate sleep phenotypes, as well as to examine underlying causes of sleep disturbance by acculturation level.
Strengths and limitations
The unprecedented diversity and size of the HCHS/SOL cohort makes this the first study to examine associations of sleep phenotypes with diabetes status among Hispanic/Latinos of various ethnic backgrounds, enhancing generalizability. We also examined whether associations vary by acculturation. Further, objective diabetes assessment and detailed insomnia measurement are major strengths; much prior work has used self-reported diabetes and single-question measures of sleep quality. Control for potential confounding using objectively measured sleep apnea is an advantage.
As in all cross-sectional studies, we cannot establish the temporal ordering of sleep symptoms and diabetes, an association that is likely bidirectional.51 Reverse causation is possible because disturbed sleep is common among people with diabetes.52 However, excluding participants with disease duration >10 years or HbA1c >10% did not materially change associations. Another limitation of the present study was self-reported sleep duration. People with insomnia may under-report sleep compared with over-reporting observed in people without insomnia with similar sleep times.14,53 Thus, self-reported short sleep and insomnia could represent more severe insomnia but not objectively shorter sleep duration. In the present study, sleep duration was measured as reported bed minus wake time; thus, participants with insomnia may have had the same duration of time in bed with fewer hours of sleep.
Extremes of sleep duration in combination with insomnia are associated with prevalent diabetes in Hispanic/Latino adults, with a large portion of the association explained by obesity. Sleep quality and quantity may be potential targets for disease management or preventive intervention in Hispanic/Latino populations with or at high risk for diabetes.
Significant findings of the study
Examining joint associations of sleep and insomnia with prevalent diabetes among 15 227 Hispanic/Latinos revealed decreased quality and quality of sleep are associated with diabetes. Short sleep with insomnia has the highest odds of diabetes, which was explained by obesity.
What this study adds
Few studies examine both sleep quality and quality in relation to type 2 diabetes; no prior study has examined joint associations of sleep duration and insomnia with diabetes in Hispanic/Latino Americans, a population in which sleep is not well-studied.
Acknowledgments
The authors thank the HCHS/SOL staff and participants for their contributions. The HCHS/SOL was supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following fund NHLBI for HCHS/SOL: National Institute on Minority Health and Health Disparities, National Institute on Deafness and Other Communication Disorders, National Institute of Dental and Craniofacial Research, National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institute of Neurological Disorders and Stroke, National Institutes of Health (NIH) Institution–Office of Dietary Supplements. EMC was supported by NIDDK T32-DK007703.
Footnotes
Disclosure
None declared.
References
- 1.Ennis S, Rios-Vargas M, Albert N. [accessed 11 March 2013];Census briefs: The Hispanic population: 2010. 2010 Available from: http://www.census.gov/prod/cen2010/briefs/c2010br-04.pdf.
- 2.Centers for Disease Control and Prevention. [accessed 26 February 2014];National diabetes fact sheet: National estimates and general information on diabetes and prediabetes in the United States. 2011 Available from: http://www.cdc.gov/diabetes/pubs/factsheet11.htm.
- 3.Schmid SM, Hallschmid M, Schultes B. The metabolic burden of sleep loss. Lancet Diabetes Endocrinol. 2015;3:52–62. doi: 10.1016/S2213-8587(14)70012-9. [DOI] [PubMed] [Google Scholar]
- 4.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: A systematic review and meta-analysis. Diabetes Care. 2010;33:414–20. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xiao Q, Arem H, Moore SC, Hollenbeck AR, Matthews CE. A large prospective investigation of sleep duration, weight change, and obesity in the NIH-AARP Diet and Health Study cohort. Am J Epidemiol. 2013;178:1600–10. doi: 10.1093/aje/kwt180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vishnu A, Shankar A, Kalidindi S. Examination of the association between insufficient sleep and cardiovascular disease and diabetes by race/ethnicity. Int J Endocrinol. 2011;2011:789358. doi: 10.1155/2011/789358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu Y, Wheaton AG, Chapman DP, Croft JB. Sleep duration and chronic diseases among U.S. adults age 45 years and older: Evidence from the 2010 Behavioral Risk Factor Surveillance System. Sleep. 2013;36:1421–7. doi: 10.5665/sleep.3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yaggi HK, Araujo AB, McKinlay JB. Sleep duration as a risk factor for the development of type 2 diabetes. Diabetes Care. 2006;29:657–61. doi: 10.2337/diacare.29.03.06.dc05-0879. [DOI] [PubMed] [Google Scholar]
- 9.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–9. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 10.Lucassen EA, Rother KI, Cizza G. Interacting epidemics? Sleep curtailment, insulin resistance, and obesity. Ann N Y Acad Sci. 2012;1264:110–34. doi: 10.1111/j.1749-6632.2012.06655.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gottlieb DJ, Punjabi NM, Newman AB, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165:863–7. doi: 10.1001/archinte.165.8.863. [DOI] [PubMed] [Google Scholar]
- 12.Hayes AL, Xu F, Babineau D, Patel SR. Sleep duration and circulating adipokine levels. Sleep. 2011;34:147–52. doi: 10.1093/sleep/34.2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Bixler EO. Insomnia with objective short sleep duration is associated with type 2 diabetes: A population-based study. Diabetes Care. 2009;32:1980–5. doi: 10.2337/dc09-0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vgontzas AN, Fernandez-Mendoza J, Liao D, Bixler EO. Insomnia with objective short sleep duration: The most biologically severe phenotype of the disorder. Sleep Med Rev. 2013;17:241–54. doi: 10.1016/j.smrv.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sands-Lincoln M, Loucks EB, Lu B, et al. Sleep duration, insomnia, and coronary heart disease among postmenopausal women in the Women’s Health Initiative. J Womens Health (Larchmt) 2013;22:477–86. doi: 10.1089/jwh.2012.3918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muraki I, Tanigawa T, Yamagishi K, et al. Nocturnal intermittent hypoxia and the development of type 2 diabetes: The Circulatory Risk in Communities Study (CIRCS) Diabetologia. 2010;53:481–8. doi: 10.1007/s00125-009-1616-0. [DOI] [PubMed] [Google Scholar]
- 17.Kendzerska T, Gershon AS, Hawker G, Tomlinson G, Leung RS. Obstructive sleep apnea and incident diabetes: A historical cohort study. Am J Respir Crit Care Med. 2014;190:218–25. doi: 10.1164/rccm.201312-2209OC. [DOI] [PubMed] [Google Scholar]
- 18.Jackson CL, Redline S, Kawachi I, Hu FB. Association between sleep duration and diabetes in black and white adults. Diabetes Care. 2013;36:3557–65. doi: 10.2337/dc13-0777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jackson CL, Hu FB, Redline S, Williams DR, Mattei J, Kawachi I. Racial/ethnic disparities in short sleep duration by occupation: The contribution of immigrant status. Soc Sci Med. 2014;118:71–9. doi: 10.1016/j.socscimed.2014.07.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hall MH, Matthews KA, Kravitz HM, et al. Race and financial strain are independent correlates of sleep in midlife women: The SWAN sleep study. Sleep. 2009;32:73–82. [PMC free article] [PubMed] [Google Scholar]
- 21.Knutson KL. Association between sleep duration and body size differs among three Hispanic groups. Am J Hum Biol. 2011;23:138–41. doi: 10.1002/ajhb.21108. [DOI] [PubMed] [Google Scholar]
- 22.Loredo JS, Soler X, Bardwell W, Ancoli-Israel S, Dimsdale JE, Palinkas LA. Sleep health in U.S. Hispanic population. Sleep. 2010;33:962–7. doi: 10.1093/sleep/33.7.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30:1096–103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Redline S, Sotres-Alvarez D, Loredo J, et al. Sleep-disordered breathing in Hispanic/Latino individuals of diverse backgrounds. The Hispanic Community Health Study/Study of Latinos. Am J Respir Crit Care Med. 2014;189:335–44. doi: 10.1164/rccm.201309-1735OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Whinnery J, Jackson N, Rattanaumpawan P, Grandner MA. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep. 2014;37:601–11. doi: 10.5665/sleep.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Seicean S, Neuhauser D, Strohl K, Redline S. An exploration of differences in sleep characteristics between Mexico-born US immigrants and other Americans to address the Hispanic Paradox. Sleep. 2011;34:1021–31. doi: 10.5665/SLEEP.1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hale L, Rivero-Fuentes E. Negative acculturation in sleep duration among Mexican immigrants and Mexican Americans. J Immigr Minor Health. 2011;13:402–7. doi: 10.1007/s10903-009-9284-1. [DOI] [PubMed] [Google Scholar]
- 28.Hale L, Troxel WM, Kravitz HM, Hall MH, Matthews KA. Acculturation and sleep among a multiethnic sample of women: The Study of Women’s Health Across the Nation (SWAN) Sleep. 2014;37:309–17. doi: 10.5665/sleep.3404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grandner MA, Chakravorty S, Perlis ML, Oliver L, Gurubhagavatula I. Habitual sleep duration associated with self-reported and objectively determined cardio-metabolic risk factors. Sleep Med. 2014;15:42–50. doi: 10.1016/j.sleep.2013.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lavange LM, Kalsbeek WD, Sorlie PD, et al. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20:642–9. doi: 10.1016/j.annepidem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Daviglus ML, Talavera GA, Aviles-Santa ML, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308:1775–84. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–9. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schneiderman N, Llabre M, Cowie CC, et al. Prevalence of diabetes among Hispanics/Latinos from diverse backgrounds: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Diabetes Care. 2014;37:2233–9. doi: 10.2337/dc13-2939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Levine DW, Dailey ME, Rockhill B, Tipping D, Naughton MJ, Shumaker SA. Validation of the Women’s Health Initiative Insomnia Rating Scale in a multicenter controlled clinical trial. Psychosom Med. 2005;67:98–104. doi: 10.1097/01.psy.0000151743.58067.f0. [DOI] [PubMed] [Google Scholar]
- 35.Hoos T, Espinoza N, Marshall S, Arredondo EM. Validity of the Global Physical Activity Questionnaire (GPAQ) in adult Latinas. J Phys Act Health. 2012;9:698–705. doi: 10.1123/jpah.9.5.698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chiuve SE, Fung TT, Rimm EB, et al. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. 2012;142:1009–18. doi: 10.3945/jn.111.157222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Westbrook PR, Levendowski DJ, Cvetinovic M, et al. Description and validation of the apnea risk evaluation system: A novel method to diagnose sleep apnea–hypopnea in the home. Chest. 2005;128:2166–75. doi: 10.1378/chest.128.4.2166. [DOI] [PubMed] [Google Scholar]
- 38.Pan A, Schernhammer ES, Sun Q, Hu FB. Rotating night shift work and risk of type 2 diabetes: Two prospective cohort studies in women. PLoS Med. 2011;8:e1001141. doi: 10.1371/journal.pmed.1001141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Spielberger CD, Gorsuch RL, Lushene RE. STAI Manual. Consulting Psychologist Press; Palo Alto: 1970. [Google Scholar]
- 40.Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J Aging Health. 1993;5:179–93. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 41.Beihl DA, Liese AD, Haffner SM. Sleep duration as a risk factor for incident type 2 diabetes in a multiethnic cohort. Ann Epidemiol. 2009;19:351–7. doi: 10.1016/j.annepidem.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 42.Knutson KL, Van Cauter E, Zee P, Liu K, Lauderdale DS. Cross-sectional associations between measures of sleep and markers of glucose metabolism among subjects with and without diabetes: The Coronary Artery Risk Development in Young Adults (CARDIA) Sleep Study. Diabetes Care. 2011;34:1171–6. doi: 10.2337/dc10-1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Patel SR. Reduced sleep as an obesity risk factor. Obes Rev. 2009;10(Suppl 2):61–8. doi: 10.1111/j.1467-789X.2009.00664.x. [DOI] [PubMed] [Google Scholar]
- 44.Ayas NT, White DP, Al-Delaimy WK, et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care. 2003;26:380–4. doi: 10.2337/diacare.26.2.380. [DOI] [PubMed] [Google Scholar]
- 45.Holliday EG, Magee CA, Kritharides L, Banks E, Attia J. Short sleep duration is associated with risk of future diabetes but not cardiovascular disease: A prospective study and meta-analysis. PLoS ONE. 2013;8:e82305. doi: 10.1371/journal.pone.0082305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stranges S, Dorn JM, Shipley MJ, et al. Correlates of short and long sleep duration: A cross-cultural comparison between the United Kingdom and the United States: The Whitehall II Study and the Western New York Health Study. Am J Epidemiol. 2008;168:1353–64. doi: 10.1093/aje/kwn337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB. Correlates of long sleep duration. Sleep. 2006;29:881–9. doi: 10.1093/sleep/29.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Youngstedt SD, Jean-Louis G. Long sleep a greater mortality risk than short sleep in older adults. J Am Geriatr Soc. 2011;59:957–8. doi: 10.1111/j.1532-5415.2011.03396.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Banna JC, Kaiser LL, Drake C, Townsend MS. Acculturation, physical activity and television viewing in His-panic women: Findings from the 2005 California Women’s Health Survey. Public Health Nutr. 2012;15:198–207. doi: 10.1017/S1368980011001273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Basner M, Dinges DF. Dubious bargain: Trading sleep for Leno and Letterman. Sleep. 2009;32:747–52. doi: 10.1093/sleep/32.6.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Martins RC, Andersen ML, Tufik S. The reciprocal interaction between sleep and type 2 diabetes mellitus: Facts and perspectives. Braz J Med Biol Res. 2008;41:180–7. doi: 10.1590/s0100-879x2006005000194. [DOI] [PubMed] [Google Scholar]
- 52.Plantinga L, Rao MN, Schillinger D. Prevalence of self-reported sleep problems among people with diabetes in the United States, 2005–2008. Prev Chronic Dis. 2012;9:E76. [PMC free article] [PubMed] [Google Scholar]
- 53.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: How similar are they? Epidemiology. 2008;19:838–45. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]