Abstract
Objective
In spite of efforts to guarantee that patients are adequately informed about their risk of fertility loss and offered treatment for fertility preservation (FP), previous studies have reported that this topic is not routinely discussed with patients, especially with younger patient populations. A mixed method systematic review was undertaken to explore the factors shaping the discussion of FP with children (0-15 years) and adolescents/young adults (16-24 years) with cancer.
Methods
Six databases were searched independently using a combination of keywords and controlled vocabulary/subject headings relating to cancer and fertility. Inclusion criteria consisted of: 1) being published in a peer-reviewed journal; 2) a focus on healthcare professionals’ (HCPs’) beliefs, attitudes or practices regarding fertility issues in cancer patients; 3) primary data collection from HCPs; and 4) a focus on HCPs who provide services to young patients. Of the 6276 articles identified in the search, 16 articles presenting the results of 14 studies were included in the final review.
Results
Common themes reported across studies indicate that five main factors influence HCPs’ discussion of FP with young cancer patients: 1) HCPs’ knowledge; 2) HCPs’ sense of comfort; 3) Patient factors (i.e., sexual maturity, prognosis, partnership status, and whether or not they initiate the conversation); 4) Parent factors (i.e., HCPs’ perception of the extent of their involvement); and 5) Availability of educational materials.
Conclusions
Future work should ensure that HCPs possess knowledge of cancer-related FP and that they receive adequate training on how to consent and discuss information with young patients and their parents.
Keywords: cancer, fertility, oncology, young patient, healthcare professionals, systematic review
INTRODUCTION
A significant amount of the work carried out by healthcare professionals (HCPs) caring for cancer patients involves helping patients manage the long-term effects of treatment. One of the most common of these effects in young people is temporary or permanent fertility loss. The extent of the impact on an individual’s reproductive capabilities depends upon the type of cancer, the age of the patient, and the specific therapies administered (1,2). Fertility loss can have devastating emotional consequences for patients and can create a strain on their social relationships and disrupt their plans for the future (3).
At the same time, a subset of assisted reproductive technologies (ARTs), termed “fertility preservation,” has become available in recent decades and offers newly diagnosed individuals the option of freezing their reproductive gametes and tissues (i.e., sperm, eggs, embryos, ovarian tissue, or testicular tissue) before treatment begins (4). After treatment, those materials can be accessed to create a genetically-related pregnancy using in vitro fertilization (IVF) or other methods (5). Guidelines have been put in place in different countries to ensure that patients are adequately informed of their risk of fertility loss and are offered treatment for fertility preservation (FP) if available (1). Professional organizations have highlighted healthcare professionals’ duty to identify patients at risk, disclose the necessary information, provide referrals to specialists, or offer available treatments (6,7).
In spite of these guidelines and general awareness among healthcare professionals of the consequences of cancer treatment on fertility, several studies have indicated that this topic is not widely or routinely discussed with patients (7-9). Previous research has found that healthcare professionals fail to carry out these discussions due to their lack of knowledge about fertility preservation procedures, guidelines, facilities, costs, and educational materials for patients designed to facilitate the discussion (10-12). Other factors identified as barriers are embarrassment, beliefs about the efficacy of fertility preservation procedures and the degree to which they will delay cancer treatment, or the fact that they might not consider these discussions to be part of their professional role (13,14). HCPs’ decision to discuss fertility loss and options for fertility preservation is also influenced by patient factors such as their prognosis, partnership status, sexual orientation, financial capacity, cultural background, age, ability to cope with the diagnosis, and insurance coverage (15). HCP communication factors are important because the type and method of discussion about fertility preservation plays a critical role in patient decision-making and follow-through (16). Furthermore, institutional factors play a role in the uptake of fertility preservation, such as the availability of fertility specialists and facilities (17,18).
In the case of young patient populations such as children, adolescents, and young adults, previous research has indicated that additional factors might play a role in healthcare professionals’ ability and willingness to discuss their risk of fertility loss and the fertility preservation procedures available to them. Current guidelines such as ASCO and the NCCN Clinical Practice Guidelines in Oncology for Adolescent and Young Adult Oncology have only recently recommended that HCPs provide information on fertility preservation to all post-pubertal young patients before their treatment begins (19). In the case of pre-pubertal girls and boys, most fertility preservation procedures are still experimental, so healthcare professionals might not initiate discussions on fertility loss because they cannot provide patients with fertility preservation options (20-22). Fertility preservation is a sensitive topic to discuss with this patient population as it involves talking about bodily changes and sexual practices (such as masturbation and sexual activity) and making assumptions about the sexual maturity of the patient (23). These discussions are further complicated by the fact that, in some cases, parents might want or need to be involved. This means that healthcare professionals need to be knowledgeable of the legal rights and responsibilities of all parties in order to make decisions on who to involve in conversations on this topic and how these conversations should be carried out (23-25). Furthermore, the level of involvement of parents might vary according to the child’s age or their sense of autonomy, making the strategies used with pediatric patients unsuitable for addressing the same issue with adolescents and young adults (25).
Research with children, adolescents, and young adults has indicated that reproductive health is an area of concern for this patient population (26,27) and many young patients are dissatisfied with the way information on fertility is communicated to them by healthcare professionals (28). In light of the unique needs of this population relating to age and life stage, this systematic review was designed to explore the factors shaping HCP discussion of FP with children, adolescents, and young adults with cancer. It includes studies that collected primary data directly from healthcare professionals with the purpose of identifying factors that might act as barriers or enablers in the communication of information on fertility loss and preservation to young patients.
To our knowledge, this is the first systematic review on HCP’s discussion of fertility preservation with children, adolescents, young adults, and their families. Previous systematic reviews on fertility preservation have mainly focused on patients’ views or include healthcare professionals’ experiences as a small part of larger reviews (3,29-31). In cases where these reviews do report on studies documenting healthcare professionals’ views, they only include five (3) or six studies (30) and do not distinguish between different patient age groups.
METHODS
Search Strategy
The authors, two social scientists (CVP and KD) and two medical research librarians (JC and IL), conducted a review of published literature using multiple databases in January 2014: PubMed, Web of Science, PsycINFO, CINAHL, Social Science Abstracts and POPLINE. A second search was conducted in December 2014 to update the content. The search used a combination of keywords and controlled vocabulary/subject headings for the concepts of cancer and fertility where appropriate (Appendix 1). Results were combined into RefWorks, and duplicates were removed. The reference lists of included articles were screened to identify additional relevant publications. Grey literature was not included in the review. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement and AMSTAR were used to guide the review (32,33). A review protocol was developed for internal use, but it has not been published.
Study Selection
Two authors (CVP and KD) screened the articles in three phases (title and article type, abstract, and full text) based on the following inclusion criteria: 1) published in a peer-reviewed journal; 2) focused on HCPs’ beliefs, attitudes or practices regarding fertility issues in cancer patients; 3) involved primary data collection from HCPs; and 4) focused on HCPs who provide services to young cancer patients under the age of 24. Young cancer patients were defined as either children (0-15 years) or young people (16 to 24 years). We based this definition of young cancer patient on the latest guidance issued by the National Institute for Health and Care Excellence (NICE) which aims to set care standards across the UK (NICE 2014). We did not limit the selection of studies by research design and included quantitative, qualitative, and mixed-methods studies.
Data Extraction
The included articles were analyzed using a data extraction form developed in RedCap (Research Electronic Data Capture) (34). The categories used in the data extraction form are summarized in Appendix 2. The form was developed after the initial screening of full-text articles. It was then piloted independently by two researchers (CVP and KD) using a random sample of five articles. Disagreements between them were discussed until consensus was reached. The form was refined based on the findings from the pilot.
Quality Assessment
The methodological quality of all studies was critically appraised using the Mixed Methods Appraisal Tool (MMAT) (35-37). The MMAT was developed to allow systematic reviewers to assess the methodological quality of diverse study designs, including qualitative, quantitative, and mixed methods. It is content validated and has been used in more than 50 published systematic reviews to date (37). Following Souto et al. (37) and Pace et al. (35), two of the authors independently reviewed each study to assess methodological quality. They then discussed responses and inter-rater reliability was estimated pre- and post-discussion using the kappa statistic (k) (Landis and Koch 1977) in which k < 0 (poor agreement); k = 0-0.20 (slight agreement); k = 0.21-0.40 (fair agreement); k = 0.41-0.60 moderate agreement; k = 0.61-0.80 (substantial agreement); and k = 0.81-1.00 (near-perfect agreement).
RESULTS
Identification of Studies
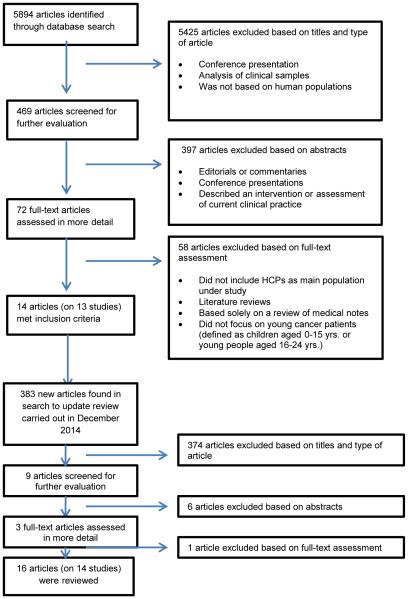
The initial search yielded 5894 published articles (343 from CINAHL, 122 from PsycINFO, 4495 from PubMed, 5 from Social Science Abstracts, and 929 from Web of Science). These were screened based on title and type of article, resulting in 469 (Figure 1). Screening based on abstracts left 72 articles for full-text review. This phase in screening led to 14 articles that presented the results of 13 studies. Prior to publication of this review, a final search was conducted for articles published through December 2014. The same procedures used in the first search were followed, resulting in a total of 383 additional articles. Screening based on title and type resulted in nine articles, while screening by abstract led to three. Full-text review led to the inclusion of two articles. Thus, the final review included 16 articles representing 14 studies out of a total of 6276 published articles.
Figure 1.
Study Selection Procedure
We excluded articles that only mapped available clinic services as well as retrospective chart reviews, case studies, conference abstracts, literature reviews, editorials, and commentaries because they did not collect primary data directly from healthcare professionals. No limits to language or date of publication were applied to the search.
Study Characteristics
The characteristics of the 14 studies included in the review are presented in Table 1. Most studies were conducted in North America (9) or Western Europe (4), specifically the USA (8), United Kingdom (2), Canada (1), and the Netherlands (2). One study took place in Australia.
Table 1.
Studies Included in the Review
| Authors | Country | Study Design |
Population | Data Collection Methods |
Factors playing a role in the discussion of FP |
|---|---|---|---|---|---|
| Anderson et al. (2008) | UK | Quantitative | Oncologists for 1030 new patients (exact number of oncologists not reported) |
Data sheet filled out for each new patient registered |
Patient factors: age, gender |
| Clayton et al. (2008) | USA | Quantitative | 210 pediatric oncology nurses | Self-administered questionnaires |
Patient factors: marital status, have children |
| Crawshaw et al. (2004) | UK | Qualitative | 22 doctors, nurses, scientists and social workers working in assisted conception or pediatric oncology |
Semi-structured interviews |
Sense of comfort Knowledge of consenting pediatric patients |
| De Vries et al. (2009) | Netherlands | Qualitative | 14 pediatric oncology physicians; 15 parents of male adolescent cancer patients |
Semi-structured interviews |
Parent factors: parental role and degree of involvement of the young person |
| Goodwin et al. (2007) | USA | Quantitative | 16 pediatric oncology physicians, 14 nurses or nurse practitioners |
Self-administered questionnaires |
Knowledge of the effects of treatment Patient factors: timing of treatment |
| Kohler et al. (2011) | USA | Quantitative | 209 pediatric oncology specialists (93% pediatric oncologists, 3% nurse or nurse practitioners, 1% reproductive endocrinologists, 3% other) |
Online questionnaires | Knowledge of guidelines Patient factors: gender |
| Nagel & Neal (2008) | Canada | Qualitative | 17 oncology nurses and 3 reproductive health nurses |
Open-ended, self- administered questionnaire |
Sense of comfort Knowledge of process and consequences of treatment Availability of educational resources for patients |
| Overbeek et al. (2014) | Netherlands | Quantitative | 37 pediatric oncologists | Mailed survey | Knowledge of FP options Patient factors: prognosis, distress Availability of educational materials to counsel patients |
| Quinn et al. (2009a)* | USA | Qualitative | Pooled data from 2 studies: 26 pediatric oncologists and 28 adult oncologists |
Semi-structured interviews | Knowledge of FP options Patient factors: perception of distress, prognosis Parent factors: perception of distress |
| Reebals, Brown & Bruckner (2006) | USA | Quantitative | 27 nurses and nurse practitioners caring for male adolescent cancer patients |
Self-administered questionnaires |
Knowledge of FP procedure |
| Schover et al. (2002) * | USA | Quantitative | 162 oncology physicians and fellows (63% medical oncologists, 21% surgical oncologists, and 16% radiation oncologists) |
Mailed questionnaires |
Knowledge of FP procedure Knowledge of costs Parent factors: involvement in the consent process Patient factors: involvement in the consent/assent process |
| Thompson, Holland, & Joubert (2013) | Australia | Mixed methods |
60 oncology professionals (15 allied health workers, 32 nurses, 6 oncologists, 7 from Victoria AYA Cancer Service) |
Questionnaire with close-ended and open-ended questions |
Sense of comfort Knowledge of fertility preservation Parent factors: Involvement of parents in the consent process Availability of educational materials |
|
Vadaparampil et al. (2007)
Vadaparampil et al. (2008b) |
USA | Quantitative | 115 pediatric oncology nurses | Self-administered questionnaires |
Sense of comfort Patient factors: HIV status, marital/partnership status, patient initiated conversation, sexual maturity, prognosis, timing of treatment Parent factors: interest in the topic Availability of educational materials |
|
Vadaparampil et al. (2008a)
Quinn et al. (2009b) |
USA | Qualitative | 24 pediatric hematologists/oncologists |
Semi-structured interviews |
Sense of comfort Knowledge of how to have discussions with young people Patient factors: cultural background, receptiveness, age, insurance Parent factors: receptiveness and cultural background Availability of educational resources |
This article includes data from HCPs treating both adult and young patients. It was included in this review because it discusses the specific factors influencing the discussion of fertility preservation with children and young people.
The majority of studies had quantitative designs (8), while 5 were qualitative and one used a mixed methods design. By far the most common quantitative data collection method was the self-administered, close-ended questionnaire (7) or sections of questionnaires (1, in the case of the mixed methods study). Qualitative methods included interviews (4) and open-ended surveys (1) or sections of surveys (1, in the case of the mixed-methods study).
Oncologists were participants in the majority of studies (11). Other populations included nurses/nurse practitioners (6) radiation oncologists (2), and allied healthcare workers (1). One study also surveyed parents in addition to the healthcare professionals.
Quality Assessment
The studies used different types of designs, data collection methods, and analysis techniques. The results from the quality assessment are presented in Table 2. Inter-rater agreement between the two raters was 96.7%, with a Cohen’s Kappa indicating near-perfect agreement (k = 0.88; p < 0.001; 95% CI). Disagreements between the raters were generally related to two components in the qualitative studies appraisal section, in which raters are asked to evaluate authors’ consideration of how findings relate to the study context or to the researchers’ influence.
Table 2.
Quality assessment
| STUDY | MMAT Score |
|---|---|
| Quantitative | |
| Anderson (2008) | **** |
| Clayton (2008) | **** |
| Goodwin (2007) | *** |
| Kohler (2011) | ** |
| Overbeek (2014) | *** |
| Reebals (2006) | ** |
| Schover (2002) | *** |
| Vadaparampil et al. (2007; 2008b) | **** |
| Qualitative | |
| Crawshaw (2004) | ** (lower) *** (higher) |
| De Vries (2009) | ** (lower) *** (higher) |
| Nagel (2008) | *** |
| Quinn et al. (2009a) | ** |
|
Quinn et al. (2009b); Vadaparampil et al. (2008a) |
**** |
| Mixed Methods | |
| Thompson (2013) | *** |
Findings: Factors Affecting the Discussion of Fertility Preservation with Children and Young People
The studies included in this review pointed to a wide range of factors playing a role in healthcare professionals’ discussion of fertility preservation with children, young people, and their families. We grouped the most common ones in five main categories: 1) knowledge, 2) sense of comfort, 3) patient factors, 4) parent factors, and 5) availability of educational materials. Table 3 summarizes these main findings.
Table 3.
Summary of main findings
| Factor | Main findings |
|---|---|
| Knowledge | Knowledge gaps were found in relation to:
|
| Sense of comfort | HCPs reported feeling embarrassed about discussing the topic with young people and their parents. Sense of comfort was associated with:
|
| Patient factors | Patient factors associated with discussing the topic included:
|
| Parent factors | HCPs’ views on the inclusion of parents in conversations on fertility preservation varied, but, in most cases, HCPs believed young patients’ preferences should be prioritized |
| Educational resources for patients and families | Lack of educational material (or knowledge of where to find it) was a reported barrier in discussing this topic with young patients and their parents |
Knowledge
Knowledge was identified by healthcare professionals in all studies as one of the main factors affecting the discussion of fertility preservation with children and young people. Three studies found a high level of awareness among healthcare professionals of the effects of cancer treatment on fertility and fertility preservation options (20,22,38). However, gaps in knowledge were found in relation to existing guidelines (17,21,25,39), fertility preservation procedures (22,25,38,40-42), costs (41,43), fertility facilities and specialists (38,43), educational materials for patients (25,44), how to carry out the informed consent process with young people and parents (24), and how to have general discussions on this topic with this particular patient population (25). Four studies found differences in professionals’ knowledge of fertility preservation procedures in relation to gender, concluding that knowledge on the options available for girls and young women are less known (21,22,38,45).
Sense of comfort
In four studies, healthcare professionals reported embarrassment discussing the topic of fertility preservation with children, young people, and/or their parents (24,25,42,44,45). Embarrassment was linked to the fear of introducing a topic of discussion that might not be considered “appropriate” for the age or sexual maturity of the patient (45). Healthcare professionals did not feel comfortable asking the young person questions about their sexual practices, such as masturbation or if they were sexually active (40), either in private or in front of their parents (42). They also expressed concerns about suggesting the use of fertility preservation procedures, such as sperm banking, which could require the use of erotic materials (44).
Patient factors
Healthcare professionals were less likely to initiate discussions on fertility preservation with young patients if they had a negative prognosis (17,39,43,44), were HIV positive (41,43,44), could not afford treatment costs (20,21,25,39,43), or were considered too young (20). Eight studies found that healthcare professionals expressed doubts on how to carry out conversations on fertility preservation with young patients, who should be involved and when these conversations should happen. The healthcare professionals interviewed by DeVries et al. (23) reported always wanting to have a separate conversation with the adolescent patients on sperm banking. Similarly, the study carried out by Vadaparampil et al. (45) highlighted that HCPs thought it was the young patient’s right to be involved in conversations concerning their fertility. Three studies found that HCPs were more likely to discuss the topic if the patient brought it up (41,43,44).
Parent factors
Ten studies touched on issues related to the role of parents during discussions on fertility preservation. In most cases, healthcare professionals believed there were instances where parents’ opinions contradicted those of the young patient. This raised ethical concerns regarding the degree to which they should be involved in conversations about the young patient’s fertility preservation. Three studies indicated that parents’ ability to make appropriate decisions could be potentially compromised by the anxiety produced by coping with their child’s cancer (17) and their desire to limit delays in their child’s medical treatment (sometimes at the expense of minimizing the long-term effects of treatment such as fertility loss) (25,45). Their presence during these conversations also created embarrassment for the young patient and the parent, and healthcare professionals felt that discussion of this topic could produce additional distress for families (17,25,39,42,45). In some cases, healthcare professionals believed that parents limited young people’s ability to make fully informed decisions on the preservation of their fertility by filtering the information they received from healthcare professionals (23). As a result, two studies questioned if parents should be involved in conversations about the young patient’s fertility preservation (24,25) and three studies found that healthcare professionals did not feel it was necessary to have parental consent to discuss this matter with the patient, even if he or she was under the age of 18 (17,41,43).
Educational resources for patients and families
Seven studies found that healthcare professionals reported not having adequate educational material to distribute to patients during fertility preservation discussions (22,40-45). In two of these studies, healthcare professionals indicated they would be more likely to discuss this topic with their patients if they had these types of materials at their disposal (41,43).
DISCUSSION
This systematic review identified a range of factors across studies that play a role in HCPs’ discussion of fertility preservation with young patients and their families. We found that HCPs had general awareness of the risk of fertility loss produced by cancer treatment, but gaps in knowledge were identified in particular areas, specifically: the suitability of certain procedures for young patients, the steps involved in carrying out FP procedures (particularly sperm banking), practice guidelines, and the availability of suitable educational materials to hand out to patients and their families. In one study, the topic of potential fertility risk was not even discussed because the patient was considered too young for the available fertility preservation options (20). Authors highlighted gaps in knowledge as a source of concern because they led to misconceptions about which patients were suitable for FP procedures, created barriers in the transmission of information from HCP to the young patient and family, and ultimately affected young people’s capacity to make informed decisions about their treatment and quality of life (38,42,43).
One of the important findings of this review was the lack of knowledge reported by HCPs on the fertility preservation options available for girls and young women. This issue coincides with findings from a recent study of the fertility information needs of teenagers and young adults with cancer where female patients reported problems with and even lack of sharing of information on fertility by HCPs (31). In several cases, it was up to the female patients to raise the issue for discussion (31).
HCPs’ sense of comfort was also an important factor influencing their willingness and ability to discuss the topic. When HCPs reported embarrassment or discomfort discussing the topic with the young patient and/or parent, they were less likely to do so. Some studies with adult patients have identified “embarrassment” as a potential barrier in the communication of information on FP to patients (39). In the case of children and young people, embarrassment was mainly produced by the fact that talking about FP entails asking questions about the young person’s sexual practices, sometimes in front of their parents. Discussions about FP also touch on the young person’s future childbearing plans, an issue that patients and parents may not have yet contemplated (17).
Discussions about FP with young people are also shaped by the HCPs’ perception of who should be involved in these conversations. The decision to involve children, adolescents, and young adults is dependent upon HCPs’ views on the level of autonomy that should be afforded to young people. Several of the studies included in this review pointed to HCPs’ belief that young people should be included in conversations and decision-making about their fertility and should be given the opportunity to discuss these issues with HCPs regardless of their parents’ opinions or wishes (17,23). Our review also pointed to the need to consider the diversity within this patient population and acknowledge the fact that the communication strategies used in pediatric settings might not be suitable for adolescents and young adults (25). Discussions on fertility risk and preservation options, therefore, need to be tailored to the particular characteristics of the young patient, where information is shared openly and honestly (46), but sensitively. This is especially relevant for the case of adolescent and young adult patients who, as Quinn and Vadaparampil have argued, “are not quite pediatric patients but not yet legal adults” (25).
The findings from this review point to a potential facilitator of open discussions about FP between HCPs and young patients: the development and widespread dissemination of educational materials on FP specifically tailored for children, adolescents, young adults, and their families. Previous work on the development of educational materials for AYA populations on sperm banking has indicated that these materials can help address HCPs’ knowledge gaps, reduce discomfort when discussing the topic and empower patients to ask questions about their risk of fertility loss and procedures available for fertility preservation (47).
Findings from this review should be interpreted with its limitations in mind. The literature search was initially carried out in January 2014 and updated in December 2014, but any articles published after this date were not included. Furthermore, although we used multiple broad search terms, it is possible that we missed articles that did not use these terms. The review focused on published articles, leaving out potentially relevant sources in the grey literature. The reviewed studies covered a wide range of designs and methodologies, making it difficult to draw general conclusions. The quality assessment of the studies included in the review pointed to evident inconsistencies in reporting information on the reasons why eligible participants chose not to take part in the study, how findings relate to the context in which data are collected, and how findings relate to the researchers’ influence. Most studies did not specify the ages of the patients the healthcare professionals cared for, making it difficult to identify differences in the factors affecting the discussion of fertility preservation with child, adolescent, and young adult patients.
CONCLUSIONS
This review has indicated that even though attempts have been made to encourage HCPs to openly discuss fertility issues with young cancer patients, important factors exist that determine if and how this discussion takes place. Research with adolescents and young adults has indicated that open communication is a critical component of their treatment, as it promotes concordance and is linked to more positive treatment experiences (48-50). Open communication involves several factors: providing information directly to the patient, allowing time for cognitive processing and question-asking, delivering information in a caring manner, and providing the patient with age-appropriate educational materials (51). Future work needs to be undertaken with HCPs to ensure they have knowledge of fertility preservation during cancer treatment (including procedures, costs, and the availability of age-appropriate educational materials), and that they receive adequate training on how to consent and discuss information with young patients and their parents (52).
Acknowledgments
Funding
Karen E. Dyer received funding from the National Cancer Institute R25-CA093423-07 (Training Program in Behavioral and Health Services Cancer Control Research).
APPENDIX 1.
Sample Keywords and Controlled Vocabulary/Subject Headings Used in Search
| Sample search strategy for PubMed / MEDLINE |
| ("fertility"[MeSH] OR "infertility"[MeSH] OR "fertility preservation"[MeSH] OR "reproductive health"[MeSH] OR "fertility preservation"[MeSH Terms] OR "reproductive health"[MeSH Terms] OR "fertility preservation"[tiab] OR "fertility preserving"[tiab] OR oncofertility OR fertil*[tiab] OR infertil*[tiab] OR sterility[tiab] OR (egg[tiab] AND freez*[tiab]) OR (sperm[tiab] AND bank*[tiab]) OR (embryo[tiab] AND freez*[tiab]) OR (ovar*[tiab] AND tissue[tiab] AND freez*[tiab]) OR ((testic*[tiab] OR testes[tiab]) AND tissue[tiab] AND freez*[tiab])) |
| AND (cancer[tiab] OR neoplasm[tiab] OR "neoplasms"[MeSH] OR "radiotherapy"[MeSH] OR "antineoplastic agents"[MeSH] OR "antineoplastic combined chemotherapy protocols"[MeSH] OR "radiation injuries"[MeSH]) |
| AND (teen[tiab] OR adolescent[tiab] OR child[tiab] OR "young adult"[tiab] OR young*[tiab] OR childhood[tiab] OR infant[MeSH] OR child[MeSH] OR adolescent[MeSH] OR young adult[MeSH]) |
APPENDIX 2.
Categories Used in the Data Extraction Form (Selected Items)
| Fields Used in RedCap Data Extraction Form | Response Boxes |
|---|---|
| Country where the study took place | |
| Participants (HCP specialty) | Oncologists Surgeons Hematologists Doctors (not specified) Radiation oncologists GYN Nurses Other |
| Definition of young patient (age range) | |
| Study design | Quantitative Qualitative Mixed-methods |
| Qualitative research methods | Interviews Questionnaires Observations Focus groups Medical chart review Other |
| Quantitative research methods | Online surveys Telephone surveys Face-to-face surveys Mailed surveys Clinical measures Other |
| Reasons for not communicating information or referring patient |
Uncertain prognosis Clinical features of the cancer Type of treatment Patient is too old Patient is too young Patient marital or family characteristics Patient’s Fatherhood or motherhood goals Patient’s positive outlook Not part of the HCP’s professional role FPT would delay treatment Lack of HCP knowledge about FP options Attitude (low priority) Attitude (willingness to discuss) Financial issues/too expensive Not covered by insurance Lack of information on where to refer patient Difficulty explaining information Embarrassment or uncomfortable discussing Sexual orientation Patient ethnicity/cultural beliefs Patient information overload Fertility will be restored Lack of guidelines Ethical issues (what happens if the patient dies?) Beliefs about the efficacy of FPT Other patient-related factors Institutional/structural factors Other |
| Reasons why HCPs felt patient would not choose a FPT | Patient’s views on their family Patient’s outlook on life Financial issues Ethnicity/cultural beliefs Uncertain prognosis Sexual orientation Other |
| Tools that help HCPs in disclosure and/or referral | Fertility expert in MDTs Information or decision aid for patients Clear referral guidelines Information on FP part of routine practice Information on FP is provided multiple times (not just at diagnosis) Other |
| Percentage of HCPs that discuss FP with patient | |
| Type of HCP knowledge assessed | Practice guidelines Fertility preservation procedures Fertility clinics Referral processes Resources for patients (education, financial) Where information can be found Risk of infertility produced by the treatment Other |
| Information sources for HCPs | Scientific literature Professional guidelines Discussions with fertility specialists Own clinical experience Continuing education programs Patient education materials Other |
| What does current practice entail? | Provision of oral information Provision of written information Patient-nurse conversations Patient-doctor conversations Discussion in MDT meetings Request of input from fertility specialists Use of guidelines FP not discussed Other |
| Recommendations for changes in practice/guidelines | |
| Limitation identified in article | |
Footnotes
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
ETHICS
No ethics approval was required as this is a systematic review.
REFERENCES
- (1).Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006 Jun 20;24(18):2917–2931. doi: 10.1200/JCO.2006.06.5888. [DOI] [PubMed] [Google Scholar]
- (2).Levine J, Canada A, Stern CJ. Fertility preservation in adolescents and young adults with cancer. J Clin Oncol. 2010 Nov 10;28(32):4831–4841. doi: 10.1200/JCO.2009.22.8312. [DOI] [PubMed] [Google Scholar]
- (3).Tschudin S, Bitzer J. Psychological aspects of fertility preservation in men and women affected by cancer and other life-threatening diseases. Hum Reprod Update. 2009 Sep-Oct;15(5):587–597. doi: 10.1093/humupd/dmp015. [DOI] [PubMed] [Google Scholar]
- (4).Ajala T, Rafi J, Larsen-Disney P, Howell R. Fertility preservation for cancer patients: A review. Obstetrics and Gyneacology International. 2010;2010:1–9. doi: 10.1155/2010/160386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (5).Schover LR. Psychosocial aspects of infertility and decisions about reproduction in young cancer survivors: a review. Med Pediatr Oncol. 1999 Jul;33(1):53–59. doi: 10.1002/(sici)1096-911x(199907)33:1<53::aid-mpo10>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- (6).Quinn G, Vadaparampil S. More research, more responsibility: the expansion of duty to warn in cancer patients considering fertility preservation. Am J Obstet Gynecol. 2013;209(2):98–102. doi: 10.1016/j.ajog.2013.02.031. P. T. [DOI] [PubMed] [Google Scholar]
- (7).Adams E, Hill E, Watson E. Fertility preservation in cancer survivors: a national survey of oncologists' current knowledge, practice and attitudes. Br J Cancer. 2013 Apr 30;108(8):1602–1615. doi: 10.1038/bjc.2013.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (8).Arafa MA, Rabah DM. Attitudes and Practices of Oncologists Toward Fertility Preservation. J Pediatr Hematol Oncol. 2011 Apr;33(3):203–207. doi: 10.1097/MPH.0b013e3182068047. [DOI] [PubMed] [Google Scholar]
- (9).Collins IM, Fay L, Kennedy MJ. Strategies for fertility preservation after chemotherapy: awareness among Irish cancer specialists. Ir Med J. 2011 Jan;104(1):6–9. [PubMed] [Google Scholar]
- (10).Gilbert E, Adams A, Mehanna H, Harrison B, Hartshorne GM. Who should be offered sperm banking for fertility preservation? A survey of UK oncologists and haematologists. Ann Oncol. 2011 May;22(5):1209–1214. doi: 10.1093/annonc/mdq579. [DOI] [PubMed] [Google Scholar]
- (11).King JW, Davies MC, Roche N, Abraham JM, Jones AL. Fertility preservation in women undergoing treatment for breast cancer in the UK: a questionnaire study. Oncologist. 2012;17(7):910–916. doi: 10.1634/theoncologist.2012-0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (12).Loren AW, Brazauskas R, Chow EJ, Gilleece M, Halter J, Jacobsohn DA, et al. Physician perceptions and practice patterns regarding fertility preservation in hematopoietic cell transplant recipients. Bone Marrow Transplant. 2013 Aug;48(8):1091–1097. doi: 10.1038/bmt.2013.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (13).Barbour RS, Porter MA, Peddie VL, Bhattacharya S. Counselling in the context of fertility and cancer: some sociological insights. Hum Fertil (Camb) 2013 Mar;16(1):54–58. doi: 10.3109/14647273.2013.775512. [DOI] [PubMed] [Google Scholar]
- (14).de Ziegler D, Streuli I, Vasilopoulos I, Decanter C, This P, Chapron C. Cancer and fecundity issues mandate a multidisciplinary approach. Fertil Steril. 2010 Feb;93(3):691–696. doi: 10.1016/j.fertnstert.2008.12.028. [DOI] [PubMed] [Google Scholar]
- (15).Quinn GP, Vadaparampil ST, Gwede CK, Miree C, King LM, Clayton HB, et al. Discussion of fertility preservation with newly diagnosed patients: oncologists' views. J Cancer Surviv. 2007 Jun;1(2):146–155. doi: 10.1007/s11764-007-0019-9. [DOI] [PubMed] [Google Scholar]
- (16).Achille MA, Rosberger Z, Robitaille R, Lebel S, Gouin JP, Bultz BD, et al. Facilitators and obstacles to sperm banking in young men receiving gonadotoxic chemotherapy for cancer: the perspective of survivors and health care professionals. Hum Reprod. 2006 Dec;21(12):3206–3216. doi: 10.1093/humrep/del307. [DOI] [PubMed] [Google Scholar]
- (17).Clayton H, Quinn GP, Lee JH, King LM, Miree CA, Nieder M, et al. Trends in clinical practice and nurses' attitudes about fertility preservation for pediatric patients with cancer. Oncol Nurs Forum. 2008 Mar;35(2):249–255. doi: 10.1188/08.ONF.249-255. [DOI] [PubMed] [Google Scholar]
- (18).Vadaparampil ST, Quinn GP, Clayton HB, King LM, Miree CA. Institutional availability of fertility preservation. Clin Pediatr. 2008;47(3):302–305. doi: 10.1177/0009922807309420. [DOI] [PubMed] [Google Scholar]
- (19).Johnson RH, Kroon L. Optimizing fertility preservation practices for adolescent and young adult cancer patients. J Natl Compr Canc Netw. 2013 Jan 1;11(1):71–77. doi: 10.6004/jnccn.2013.0010. [DOI] [PubMed] [Google Scholar]
- (20).Anderson RA, Weddell A, Spoudeas HA, Douglas C, Shalet SM, Levitt G, et al. Do doctors discuss fertility issues before they treat young patients with cancer? Hum Reprod. 2008 Oct;23(10):2246–2251. doi: 10.1093/humrep/den252. [DOI] [PubMed] [Google Scholar]
- (21).Kohler TS, Kondapalli LA, Shah A, Chan S, Woodruff TK, Brannigan RE. Results from the survey for preservation of adolescent reproduction (SPARE) study: gender disparity in delivery of fertility preservation message to adolescents with cancer. J Assist Reprod Genet. 2011 Mar;28(3):269–277. doi: 10.1007/s10815-010-9504-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (22).Overbeek A, van den Berg M, Louwe L, Wendel E, ter Kuile M, Kaspers G, et al. Practice, attitude and knowledge of Dutch paediatric oncologists regarding female fertility. Neth J Med. 2014 Jun;72(5):264–270. [PubMed] [Google Scholar]
- (23).de Vries MC, Bresters D, Engberts DP, Wit JM, van Leeuwen E. Attitudes of physicians and parents towards discussing infertility risks and semen cryopreservation with male adolescents diagnosed with cancer. Pediatr Blood Cancer. 2009 Sep;53(3):386–391. doi: 10.1002/pbc.22091. [DOI] [PubMed] [Google Scholar]
- (24).Crawshaw M, Glaser A, Hale J, Sloper P. Professionals' views on the issues and challenges arising from providing a fertility preservation service through sperm banking to teenage males with cancer. Hum Fertil (Camb) 2004 Mar;7(1):23–30. doi: 10.1080/1464727042000198087. [DOI] [PubMed] [Google Scholar]
- (25).Quinn GP, Vadaparampil ST. Fertility Preservation Research Group. Fertility preservation and adolescent/young adult cancer patients: physician communication challenges. J Adolesc Health. 2009 Apr;44(4):394–400. doi: 10.1016/j.jadohealth.2008.08.014. [DOI] [PubMed] [Google Scholar]
- (26).Klosky JL, Simmons JL, Russell KM, Foster RH, Sabbatini GM, Canavera KE, et al. Fertility as a priority among at-risk adolescent males newly diagnosed with cancer and their parents. Support Care Cancer. 2015 Aug 2; doi: 10.1007/s00520-014-2366-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (27).Murphy D, Klosky JL, Termuhlen A, Sawczyn KK, Quinn GP. The need for reproductive and sexual health discussions with adolescent and young adult cancer patients. Contraception. 2013 Aug;88(2):215–220. doi: 10.1016/j.contraception.2012.08.041. [DOI] [PubMed] [Google Scholar]
- (28).Oosterhuis BE, Goodwin T, Kiernan M, Hudson MM, Dahl GV. Concerns about infertility risks among pediatric oncology patients and their parents. Pediatr Blood Cancer. 2008 Jan;50(1):85–89. doi: 10.1002/pbc.21261. [DOI] [PubMed] [Google Scholar]
- (29).Goncalves V, Sehovic I, Quinn G. Childbearing attitudes and decisions of young breast cancer survivors: a systematic review. Hum Reprod Update. 2014 Sep 27; doi: 10.1093/humupd/dmt039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (30).Goossens J, Delbaere I, Van Lancker A, Beeckman D, Verhaeghe S, Van Hecke A. Cancer patients' and professional caregivers' needs, preferences and factors associated with receiving and providing fertility-related information: A mixed-methods systematic review. Int J Nurs Stud. 2014 Feb;51(2):300–319. doi: 10.1016/j.ijnurstu.2013.06.015. [DOI] [PubMed] [Google Scholar]
- (31).Wright CI, Coad J, Morgan S, Stark D, Cable M. 'Just in case': the fertility information needs of teenagers and young adults with cancer. Eur J Cancer Care (Engl) 2014 Mar;23(2):189–198. doi: 10.1111/ecc.12137. [DOI] [PubMed] [Google Scholar]
- (32).Shea BJ, Hamel C, Wells GA, Bouter LM, Kristjansson E, Grimshaw J, et al. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. Journal of clinical epidemiology. 2009;62(10):1013–1020. doi: 10.1016/j.jclinepi.2008.10.009. [DOI] [PubMed] [Google Scholar]
- (33).Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ. 2009;339:332–336. [PMC free article] [PubMed] [Google Scholar]
- (34).Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomedical Informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (35).Pace R, Pluye P, Bartlett G, Macauley AC, Salsberg J, Jagosh J, et al. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed methods studies. International Journal of Nursing Studies. 2012;49:47–53. doi: 10.1016/j.ijnurstu.2011.07.002. [DOI] [PubMed] [Google Scholar]
- (36).Pluye P, Gagnon MP, Griffiths F, Johnson-Lafleur J. A scoring system for appraising mixed methods research, and concomitantly appraising qualitative, quantitative, and mixed methods primary studies in Mixed Studies Reviews. International Journal of Nursing Studies. 2009;46:529–546. doi: 10.1016/j.ijnurstu.2009.01.009. [DOI] [PubMed] [Google Scholar]
- (37).Souto RQ, Khanassov V, Hong QN, Bush PL, Vedel I, Pluye P. Systematic mixed studies reviews: Updating results on the reliability and efficiency of the mixed methods appraisal tool. International Journal of Nursing Studies. 2015;52:500–501. doi: 10.1016/j.ijnurstu.2014.08.010. [DOI] [PubMed] [Google Scholar]
- (38).Goodwin T, Elizabeth Oosterhuis B, Kiernan M, Hudson MM, Dahl GV. Attitudes and practices of pediatric oncology providers regarding fertility issues. Pediatr Blood Cancer. 2007 Jan;48(1):80–85. doi: 10.1002/pbc.20814. [DOI] [PubMed] [Google Scholar]
- (39).Quinn GP, Vadaparampil ST, King L, Miree CA, Wilson C, Raj O, et al. Impact of physicians' personal discomfort and patient prognosis on discussion of fertility preservation with young cancer patients. Patient Educ Couns. 2009 Dec;77(3):338–343. doi: 10.1016/j.pec.2009.09.007. [DOI] [PubMed] [Google Scholar]
- (40).Nagel K, Neal M. Discussions regarding sperm banking with adolescent and young adult males who have cancer. J Pediatr Oncol Nurs. 2008 Mar-Apr;25(2):102–106. doi: 10.1177/1043454208314459. [DOI] [PubMed] [Google Scholar]
- (41).Reebals JF, Brown R, Buckner EB. Nurse Practice Issues Regarding Sperm Banking in Adolescent Male Cancer Patients. Journal of Pediatric Oncology Nursing. 2006;23(4):182–188. doi: 10.1177/1043454206289868. [DOI] [PubMed] [Google Scholar]
- (42).Thompson K, Dyson G, Holland L, Joubert L. An exploratory study of oncology specialists' understanding of the preferences of young people living with cancer. Soc Work Health Care. 2013;52(2-3):166–190. doi: 10.1080/00981389.2012.737898. [DOI] [PubMed] [Google Scholar]
- (43).Schover LR, Brey K, Lichtin A, Lipschultz LI, Jeha S. Oncologists' attitudes and practices regarding banking sperm before cancer treatment. J Clin Oncol 2002. 2002;20(7):1890–1897. doi: 10.1200/JCO.2002.07.174. [DOI] [PubMed] [Google Scholar]
- (44).Vadaparampil ST, Clayton H, Quinn GP, King LM, Nieder M, Wilson C. Pediatric oncology nurses' attitudes related to discussing fertility preservation with pediatric cancer patients and their families. Journal of Pediatric Oncology Nursing. 2007;24(5):255–263. doi: 10.1177/1043454207303878. [DOI] [PubMed] [Google Scholar]
- (45).Vadaparampil S, Quinn G, King L, Wilson C, Nieder M. Barriers to fertility preservation among pediatric oncologists. Patient Educ Couns. 2008;72(3):402–410. doi: 10.1016/j.pec.2008.05.013. [DOI] [PubMed] [Google Scholar]
- (46).Morgan S, Davies S, Palmer S, Plaster M. Sex, drugs, and rock 'n' roll: caring for adolescents and young adults with cancer. J Clin Oncol. 2010 Nov 10;28(32):4825–4830. doi: 10.1200/JCO.2009.22.5474. [DOI] [PubMed] [Google Scholar]
- (47).Nagel K, Wizowski L, Duckworth J, Cassano J, Hahn SA, Neal M. Using plain language skills to create an educational brochure about sperm banking for adolescent and young adult males with cancer. Journal of Pediatric Oncology Nursing. 2008;25(4):220–226. doi: 10.1177/1043454208319973. [DOI] [PubMed] [Google Scholar]
- (48).Freyer DR, Mattano LJ. Information and resources for young adults and adolescents with cancer. In: Bleyer WA, Barr RD, editors. Cancer in Adolescents and Young Adults. Springer Verlag; New York: 2007. pp. 469–487. [Google Scholar]
- (49).Kyngas H. Compliance of adolescents with chronic disease. J Clin Nurs. 2000;9:549–566. doi: 10.1046/j.1365-2702.2000.00368.x. [DOI] [PubMed] [Google Scholar]
- (50).Palmer S, Mitchell A, Thompson K, Sexton M. Unmet needs among adolescent and cancer patients: A pilot study. Palliat Support Care. 2007;5:127–134. doi: 10.1017/s1478951507070198. [DOI] [PubMed] [Google Scholar]
- (51).D'Agostino NM, Penney A, Zebrack B. Providing developmentally appropriate psychosocial care to adolescent and young adult cancer survivors. Cancer. 2011 May 15;117(10 Suppl):2329–2334. doi: 10.1002/cncr.26043. [DOI] [PubMed] [Google Scholar]
- (52).Nagel K, Cassano J, Wizowski L, Neal MS. Collaborative multidisciplinary team approach to fertility issues among adolescent and young adult cancer patients. Int J Nurs Pract. 2009 Aug;15(4):311–317. doi: 10.1111/j.1440-172X.2009.01755.x. [DOI] [PubMed] [Google Scholar]