Abstract
A safer and more effective vaccine than the unlicensed Francisella tularensis Live Vaccine Strain (LVS) is needed to protect against the biowarfare agent F. tularensis. Previously, we developed an LVS ΔcapB mutant that is significantly safer than LVS and provides potent protective immunity against F. tularensis respiratory challenge when administered intranasally but limited protection when administered intradermally unless as part of a prime-boost vaccination strategy. To improve the immunogenicity and efficacy of LVS ΔcapB, we developed recombinant LVS ΔcapB (rLVS ΔcapB) strains overexpressing various F. tularensis Francisella Pathogenicity Island (FPI) proteins - IglA, IglB and IglC, and a fusion protein (IglABC) comprising immunodominant epitopes of IglA, IglB, and IglC downstream of different Francisella promoters, including the bacterioferritin (bfr) promoter. We show that rLVS ΔcapB/bfr-iglC and bfr-iglABC express more IglA, IglB, IglC or IglABC than parental LVS ΔcapB in broth and in human macrophages, and stably express FPI proteins in macrophages and mice absent antibiotic selection. In response to IglC and heat-inactivated LVS, spleen cells from mice immunized intradermally with rLVS ΔcapB/bfr-iglC or bfr-iglABC secrete greater amounts of interferon-gamma and/or interleukin-17 than those from mice immunized with LVS ΔcapB, comparable to those from LVS-immunized mice. Mice immunized with rLVS ΔcapB/iglA, iglB, iglC or iglABC produce serum antibodies at levels similar to LVS-immunized mice. Mice immunized intradermally with rLVS ΔcapB/bfr-iglABC and challenged intranasally with virulent F. tularensis Schu S4 survive longer than sham- and LVS ΔcapB-immunized mice. Mice immunized intranasally with rLVS ΔcapB/bfr-iglABC - but not with LVS - just before or after respiratory challenge with F. tularensis Schu S4 are partially protected; protection is correlated with induction of a strong innate immune response. Thus, rLVS ΔcapB/bfr-iglABC shows improved immunogenicity and protective efficacy compared with parental LVS ΔcapB and, in contrast to LVS, has partial efficacy as immediate pre- and post-exposure prophylaxis.
Keywords: Francisella tularensis, Vaccine, LVS ΔcapB, Francisella Pathogenicity Island, Type VI Secretion System, Bioterrorism
1. Introduction
Francisella tularensis subsp. tularensis is a Tier 1 Select Agent that can cause highly fatal pneumonic tularemia when inhaled [1–4]. As pneumonic tularemia is difficult to diagnose, requires hospitalization - typically in an intensive care unit - and can be fatal even with appropriate treatment [5, 6], the most practicable way to defend against an intentional airborne attack with F. tularensis is with a safe and effective vaccine. The unlicensed F. tularensis Live Vaccine Strain (LVS), derived from the less virulent subsp. holarctica and the only vaccine against tularemia currently available, is protective but retains significant toxicity [3].
Several strategies have been employed to develop a safer and more efficacious tularemia vaccine including 1) using further attenuated subsp. holarctica LVS strains [7, 8]; 2) using deletional mutants of subsp. tularensis Schu S4 [8, 9]; and 3) using attenuated F. novicida strains [10]. Deletional mutants of subsp. holarctica are safer than LVS; however, only a few of them have been tested against subsp. tularensis Schu S4 challenge in animal models [7, 8]. The deletional mutants of subsp. tularensis are typically either hyper- or hypo- attenuated, rendering them either poorly immunogenic or too virulent for use [8].
We previously developed LVS ΔcapB, an LVS mutant with a targeted deletion in a putative capsular gene, capB. This vaccine is highly protective against respiratory challenge with the highly virulent F. tularensis Schu S4 strain when administered by the intranasal (i.n.) route, comparable in efficacy to LVS, but poorly protective when administered by the intradermal (i.d.) route unless used as a prime vaccine in a heterologous prime-boost vaccination strategy [11]. We also previously developed recombinant LVS ΔcapB (rLVS ΔcapB) vaccines expressing Francisella pathogenicity island (FPI) proteins IglA or IglC downstream of the F. tularensis groES (FTL_1715) promoter; these vaccines generally showed improved efficacy compared with LVS ΔcapB [11] when administered i.d. These proteins and IglB are part of a FPI-encoded Type VI Secretion System (T6SS) which F. tularensis requires to escape from its phagosome and multiply intracellularly in host cells; IglA/IglB heterodimers assemble to form the Francisella T6SS outer sheath [12], which upon contraction, thrusts an inner tube likely comprising IglC through the bacterial wall and into the target phagosomal membrane.
In the present study, to improve the immunogenicity and efficacy of the rLVS ΔcapB vaccines expressing FPI proteins, we have evaluated two additional transcription promoters as drivers of the FPI protein expression cassette in the shuttle plasmid – the promoter of the F. tularensis bacterioferritin (bfr, FTL_0617), which is about 10 times more potent than the groES promoter [13], and the promoter of a putative outer membrane protein 26 (omp, FTN_1451) [14]. We additionally have evaluated rLVS ΔcapB vaccines expressing several versions of a fusion protein of IglA, IglB, and IglC that are major constituents of the Francisella T6SS, essential for virulence, and immunogenic [11, 15–21]. The T6SS requires assembly of hundreds of these three proteins; hence, by virtue of their abundance, they are likely to be available for processing and presentation by antigen presenting cells. This is especially so for IglC, which is secreted by the T6SS; this laboratory has developed several potent vaccines based upon abundantly secreted proteins of intracellular pathogens [22–27]. Hence, these three T6SS proteins are promising vaccine candidates.
2. Materials and Methods
2.1. Bacteria and vaccines
F. tularensis LVS and Schu S4 strains were obtained from the Centers for Disease Control and Prevention (Atlanta, Ga.). Stocks of LVS, Schu S4, heat-inactivated (HI) LVS, LVS ΔcapB, and attenuated recombinant rLVS ΔcapB strains expressing F. tularensis antigens were prepared as described previously [7, 11, 28].
2.2. Mice
Six to eight week old specific-pathogen-free female BALB/c mice were purchased from Charles River Laboratory (Wilmington, MA) and used according to protocols approved by the Institutional Animal Care and Use Committees of UCLA and Colorado State University (CSU).
2.3. Construction of recombinant attenuated LVS strains expressing F. tularensis proteins
LVS ΔcapB strains overexpressing F. tularensis FPI protein(s) IglA, IglB, or IglC under the control of groES promoter [29] - rLVS ΔcapB/gro-iglA (previously rLVS ΔcapB/iglA), rLVS ΔcapB/gro-iglB, and rLVS ΔcapB/gro-iglC (previously rLVS ΔcapB/iglC) - were constructed by electroporating a shuttle plasmid carrying an F. tularensis antigen expression cassette into LVS ΔcapB [11]. The shuttle plasmid for expressing IglA, IglB, IglC, or the fusion protein comprising the immunodominant epitopes of IglA, IglB, and IglC (IglABC) under the control of the F. tularensis bfr or omp promoter followed by a Shine-Dalgarno sequence was constructed by multi-step overlap extension PCRs and traditional cloning methods as described in the supplemental methods.
2.4. Growth kinetics, protein expression, and shuttle plasmid stability of recombinant vaccines in broth and in PMA-differentiated monocytic THP-1 cells
To follow the growth kinetics of individual vaccines in broth, we cultured bacteria on chocolate agar for 2 days, scraped the colonies into Chamberlain Defined Medium (CDM) [30] or 3% Tryptic Soy Broth supplemented with 0.1% L-cysteine (TSBC), adjusted to an optical density of 0.01 at 540 nm, and incubated at 37 C with vigorous shaking for 24 hours. Intra-macrophage (THP-1) growth and protein expression of individual vaccines were examined as described [7, 28] and in the supplemental methods.
2.5. Immunization of mice, vaccine dissemination, clearance, stability, and immunology studies
Mice were immunized i.d. with phosphate buffer saline (PBS, sham control), 104 CFU LVS, 106 CFU LVS ΔcapB, or 106 CFU of rLVS ΔcapB/bfr-iglA, iglB, iglC or iglABC or i.n. with 102 CFU LVS or 105 CFU of LVS ΔcapB, rLVS ΔcapB/bfr-iglA, iglB, iglC or iglABC; euthanized at days 1, 4, 7, and 14 post-vaccination; and their spleen, liver, lung, skin (at the base of tail, the site of i.d. immunization), and inguinal lymph nodes removed and assayed for bacterial CFU [31] and plasmid stability. T-cell mediated immune responses were examined by preparing single cell splenic suspensions; incubating with T-cell medium comprising Advanced RPMI-1640 (Invitrogen) supplemented with 2% heat-inactivated (HI) fetal bovine serum (Seradigm Premium Grade), penicillin (100 I.U./ml), streptomycin (100μg/ml), 0.1 mM non-essential amino acids, 4 mM L-glutamine, 1 mM sodium pyruvate, and 0.05 mM β-mercaptoethanol in the presence of various F. tularensis antigens; and assaying for mouse interferon-gamma (IFN-γ) and interleukin-17A (IL-17A) [11] or quantitating intracellular cytokine staining by flow cytometry analysis [28]. Humoral immune responses were examined by analyzing sera for levels of IgG and subtypes IgG1 and IgG2a antibodies specific for HI-LVS [11].
To assay IFN-γ and IL-17A secretion by splenocytes from mice sham-immunized or immunized with various vaccines, we seeded single cell suspensions of splenocytes at 1.5 ×105 cells per well in 96-well plates and incubated with T-cell medium in the presence IglC protein (10 μg/ml, prepared from recombinant E. coli) [28] or HI-LVS (5 × 107/ml) for 3 days. After 3 days, the culture supernatant fluid was collected and assayed for mouse IFN-γ and IL-17A using a mouse cytokine EIA kit (BD Biosciences) following the manufacturer’s instructions, as described previously [11].
To assay cytokine expression by intracellular cytokine staining, we seeded single cell suspensions of 1.5 ×106 splenocytes per well in U-bottom 96-well plates and incubated the cells with T-cell medium in the presence of Interleukin 2 (BD Pharmingen, 2 U/ml) and IglC protein (10 μg/ml), an IglC peptide (TDEAWGIMIDLSNLE, kindly provided by Justin Skoble of Aduro Biotech) (2μg/ml), or HI-LVS (5 × 107/ml) overnight. Then, GolgiPlug (protein transport inhibitor containing Brefeldin A) diluted in T cell medium was added to all wells and PMA was additionally added to positive control wells. Cells were incubated for an additional four hours, harvested, and stained with AlexaFlour 700-conjugated anti-CD4 antibodies (clone RM 4–5), PerCp-Cy5.5-conjugated anti-CD8 antibodies (clone 53-6.7), V450-conjugated anti-CD3 antibodies (clone 17-A2), and panels of antibodies against intracellular markers IFN-γ (PE conjugated, clone XMG 1.2), TNF (PE-Cy7 conjugated, clone MP6-XT22), and IL-2 (APC conjugated, clone JES6-5H4), as described previously (16). All intracellular cytokine staining reagents were purchased from BD Biosciences except where noted. 100,000 lymphocytes per sample were acquired with an LSRII-HT (BD) flow cytometer. The frequencies of live CD4+ and CD8+ T cells expressing IFN-γ, TNF, and/or IL-2 were determined using FACSDiva (BD) software. Background numbers of cells producing cytokines without antigen stimulation were subtracted.
2.6. Protective Efficacy and Pre- and Post-Exposure Prophylaxis
Efficacy studies were conducted at CSU as described [7, 11, 28]. For study of rLVS ΔcapB/bfr-iglABC efficacy as an immediate pre- or post-exposure vaccine, mice were immunized i.n with 1 × 106, 5 × 106, or 5 × 107 CFU of rLVS ΔcapB/bfr-iglABC or 102 CFU of LVS as a control from 2 days before to 2 days after i.n. challenge with a lethal dose (~ 10 CFU) of F. tularensis Schu S4. Challenged mice were weighed and monitored for illness and death for 3 – 4 weeks.
2.7. Cytokine assay
Mice were immunized as described above. At day 2 post-immunization, mice were anesthetized, bled, and euthanized; blood collected in Capiject tubes (Terumo) and serum isolated by following the manufacturer’s instructions; lungs removed and homogenized in 1 ml PBS supplemented with Complete Ultra Proteinase Inhibitor (Roche). Cytokine analysis was performed by the Immune Assessment Core at UCLA and as described by others [32, 33]. Briefly, a magnetic multiplex kit for mouse cytokines and chemokines (32-plex) was purchased from EMD Millipore and used per the manufacturer’s instructions. 25 μl of undiluted mouse lung homogenate and diluted (1:2) mouse serum samples were mixed with 25 μl magnetic beads, and allowed to incubate overnight at 4°C while shaking. Separate standards were made for both sample types, using the appropriate sample matrix. After washing the plate two times with wash buffer in a Biotek ELx405 washer, 25 μl of biotinylated detection antibody was added and incubated for 1 hour at room temperature. 25 μl streptavidin-phycoerythrin conjugate was then added to the reaction mixture and incubated for another 30 minutes at room temperature. Following two additional washes, beads were resuspended in sheath fluid, and fluorescence was quantified using a Luminex FLEXMAP 3D instrument. Data were analyzed using MILLIPLEX Analyst 5.1 software.
2.8. Statistics
Statistical analyses were performed as described previously [11]. Briefly, ANOVA with Tukey’s multiple comparisons test was performed using GraphPad Prism 6.04 (San Diego, CA) to determine significance in comparisons of mean mouse bacterial burden, mean cytokine production, mean serum antibody endpoint titer, and mean frequencies of cytokine-producing CD4+ and CD8+ T cells among mice in vaccinated and control groups. A log-rank analysis (Mantel-Cox test) using GraphPad Prism 6.04 was used to determine significance of survival curves among mice in immunized and control groups.
3. Results
3.1. Construction of rLVS ΔcapB overexpressing FPI T6SS proteins
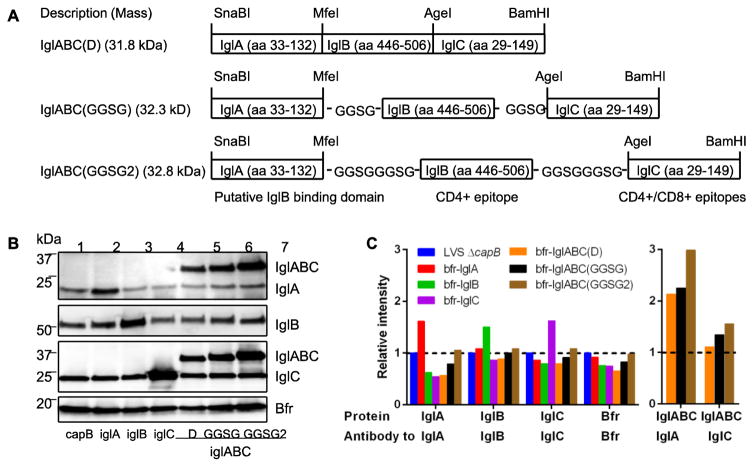
To improve the potency of the rLVS ΔcapB vaccines, especially for i.d. administration, we sought to improve the activity of the promoter for antigen expression in the shuttle plasmid and to increase the F. tularensis antigen pool. To improve promoter activity, we constructed rLVS ΔcapB strains expressing FPI proteins under the control of the groE, bfr, or omp promoters and compared their protein expression levels. To increase the antigen pool, we constructed rLVS ΔcapB expressing the fusion protein of IglA (residues 33–132, necessary for efficient binding to IglB and for IglB protein stability and intramacrophage growth [34]), IglB (residues 446 – 506, mapped as CD4+ epitopes in C57BL/6 mice [21]) and IglC (residues 29 – 149, containing CD4+ or CD8+ immunodominant epitopes in BALB/c or C57BL/6 mice [personal communication, Justin Skoble]) – proteins that comprise the outer sheath (IglA and IglB) or inner core (IglC) of the F. tularensis T6SS. The three protein residues were expressed either directly fused to each other in frame or separated by a flexible linker - GGSG or GGSGGGSG (Fig. 1A) - and downstream of the bfr or omp promoter and the Shine-Dalgarno sequence. Western blotting analyses using polyclonal antibodies specific to IglA (BEI Resources) or IglC (prepared by our laboratory) or monoclonal antibody to IglB (BEI Resources) showed that IglA, IglB, and IglC expression by rLVS ΔcapB/bfr-iglA, rLVS ΔcapB/bfr-iglB, and rLVS ΔcapB/bfr-iglC was 1.5 – 1.6-fold higher than that of the parental LVS ΔcapB (Fig. 1B, 1C). IglABC fusion proteins, whether the three protein residues were directly fused or linked by flexible linkers, were expressed by each rLVS ΔcapB/bfr-iglABC and detected by antibody to IglA or IglC; fusion protein expression was higher when the protein residues were linked by flexible linkers than when fused directly, and the IglABC fusion protein with two linkers had a higher expression level than the one with one linker. In subsequent studies, rLVS ΔcapB/bfr-iglABC(GGSG) induced greater IglC- and HI-LVS-specific humoral and cell-mediated immune responses than rLVS ΔcapB expressing IglABC with the protein residues linked directly or by GGSGGGSG (data not shown). Hence, we chose rLVS ΔcapB/bfr-iglABC(GGSG) (simplified as rLVS ΔcapB/bfr-iglABC) for further analysis.
Fig. 1. Construction of shuttle plasmids for antigen expression cassettes of IglABC(D), IglABC(GGSG), and IglABC(GGSG2) and expression of F. tularensis FPI T6SS proteins by the recombinant LVS ΔcapB strains.
A. Antigen expression cassette for fusion protein of IglABC. The coding sequences for IglA (residues 33–132), IglB (residues 446 – 506), and IglC (residues 29 – 149) either fused directly in frame with each other [IglABC(D)] or linked by a flexible linker GGSG [IglABC(GGSG)] or GGSGGGSG [IglABC (GGSG2)] was amplified by using overlap PCRs from the genomic DNA of a recent clinical isolate of F. tularensis subsp. tularensis and primer pairs listed in Supplemental Table 1 as described in the supplemental methods. B. The F. tularensis IglA, IglC, IglC and IglABC are overexpressed by rLVS ΔcapB cultured in broth medium. Various rLVS ΔcapB glycerol stocks were grown in TSBC for overnight with agitation; the overnight culture was sub-cultured to mid-log phase in TSBC; cells collected by centrifugation and lysed in SDS buffer; cell lysates equivalent to 1 ×108 bacteria were analyzed by SDS-PAGE and Western blotting using polyclonal antibodies (pAb) to IglA (top), monoclonal antibody (mAb) to IglB (upper middle), pAb to IglC (lower middle) and pAb to Bacterioferritin (Bfr, bottom) (loading control). Note, the membrane probed with mAb to IglB was stripped and re-probed with pAbs to IglA and Bacterioferritin; a separated membrane applied with the same amount of cell lysates was probed with pAb to IglC. Lane 1, LVS ΔcapB; Lane 2, rLVS ΔcapB/bfr-iglA; Lane 3, rLVS ΔcapB/bfr-iglB; Lane 4, rLVS ΔcapB/bfr-iglC; Lane 5, rLVS ΔcapB/bfr-iglABC(D); Lane 6, rLVS ΔcapB/bfr-iglABC(GGSG); Lane 7, rLVS ΔcapB/bfr-iglABC(GGSG2). C. Relative intensity of protein expression. The intensity of protein bands detected by various antibodies were analyzed by QuantityOne (Bio-Rad) and compared with the same protein expressed by the parental LVS ΔcapB (IglA, IglB, IglC, and Bfr, left panel) or with the endogenous protein from the same strain (IglA or IglC, right penel). Results were representative of multiple protein expression experiments tested in broth culture (CDM and TSBC) and in infected human (THP-1) and mouse macrophage-like cell lines.
3.2. Growth kinetics and plasmid stability of rLVS ΔcapB vaccines in vitro
To examine whether the protein expression cassette driven by the groE, bfr or omp promoter in the shuttle plasmid affected the growth kinetics of rLVS ΔcapB vaccine candidates in broth, we cultured the vaccines on chocolate agar, inoculated them into CDM or TSBC medium, and followed their growth kinetics by measuring optical density at 540 nm. As shown in sFig. 1, rLVS ΔcapB strains overexpressing IglA, IglB, or IglC under the control of the groE, bfr or omp promoter grew similarly to LVS and LVS ΔcapB in TSBC (sFig. 1A – 1C) and CDM (sFig. 1D – 1F). Moreover, these vaccines grew similarly in PMA-differentiated THP-1 cells (sFig. 1G – I). These results indicate that the shuttle plasmids carried by the rLVS ΔcapB vaccines did not affect their growth kinetics. The shuttle plasmids were stable under non-selective conditions in infected THP-1 cells (sFig. 2.).
3.3. Safety, dissemination, clearance, and shuttle plasmid stability of rLVS ΔcapB vaccines in vivo
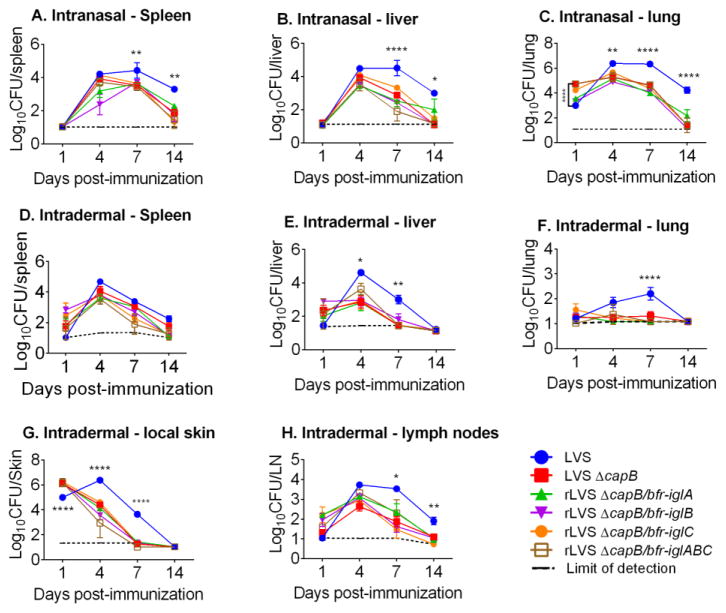
To verify the safety, dissemination and clearance of rLVS ΔcapB/bfr-iglA, iglB, iglC, and iglABC, we infected BALB/c mice i.n. or i.d. with LVS, LVS ΔcapB, or rLVS ΔcapB/bfr-iglA, iglB, iglC, or iglABC, and monitored the mice for signs of illness for 14 days. At 1, 4, 7, and 14 days post-immunization, we assayed the bacterial burden in various organs. As shown in Fig. 2, after i.n. vaccination, rLVS ΔcapB/bfr-iglA, iglB, iglC, and iglABC peaked in the spleen (Fig. 2A), liver (Fig. 2B), and lung (Fig. 2C) at Day 4 post-vaccination and were largely cleared by most mice at day 14 post-vaccination, similar to parental LVS ΔcapB in all three organs. These strains were cleared significantly faster than LVS; LVS grew to much higher levels (1–2 logs higher) at Day 4 and/or Day 7 and maintained higher levels through Day 14, at which point its level was >1 log higher (p < 0.05 to p < 0.0001) than the other vaccines in all three organs. After i.d. vaccination (Fig. 2D–2H), rLVS ΔcapB/bfr-iglA, iglB, iglC and iglABC peaked at Day 4 post-vaccination in the spleen and liver and had minimal growth in the lung, and these vaccines were largely cleared from spleen, liver, and lung of all mice at Day 14 post-vaccination. In the local skin, the rLVS ΔcapB strains were detected on Day 1 and Day 4 post-vaccination and cleared by all mice at Day 7 post-vaccination. In the inguinal lymph nodes, the rLVS ΔcapB strains were detected at 1, 4, and 7 days post-vaccination and cleared (Limit of Detection) at Day 14 post-vaccination, similarly to the parental LVS ΔcapB. LVS grew to higher levels in all these sites, peaking at Day 4 (spleen, liver, skin, and lymph nodes) or Day 7 (lung) and was not cleared from the spleen and lymph nodes by Day 14. Both i.n. and i.d. vaccination with rLVS ΔcapB strains did not induce any signs of illness, indicating that these vaccines were as safe as the LVS ΔcapB parental strain. In contrast, ~25% of mice immunized i.n. with 200 CFU LVS died and mice immunized i.d. with 106 CFU LVS showed ruffled fur in some of our experiments – evidence of toxicity of LVS by both the i.n. and i.d. route in BALB/c mice.
Fig. 2. The rLVS ΔcapB vaccines are disseminated and cleared similarly to the parental strain after i.n. and i.d. vaccination.
Mice (4/group) were immunized i.n. (top panels) with 102 CFU of LVS or 105 CFU of LVS ΔcapB or rLVS ΔcapB/bfr-iglA, iglB, iglC or iglABC vaccines, or immunized i.d. (middle and bottom panels) with 104 CFU of LVS or 106 CFU of LVS ΔcapB or rLVS ΔcapB/bfr-iglA, iglB, iglC, or iglABC vaccines; euthanized at various times post-vaccination, as indicated on the X-axis; and their organs removed and assayed for F. tularensis bacterial burden. Values are means ± SE. Shown are the results combined from 3 independent experiments comprising 4 – 8 mice per group.
To examine whether the shuttle plasmid with the bfr promoter is stable in vivo in the absence of antibiotic selection, we harvested animal organs at various times post-vaccination, cultured organ homogenates on chocolate agar in the presence or absence of kanamycin for 3 – 5 days, and tested colonies selected from different animals by colony PCR, amplifying the F. tularensis antigen expression cassette in the shuttle plasmid. We found that the shuttle plasmids for IglA and IglC were more stable than the one for IglB (suppl. Tables 2 & 3). That the expression cassette for the large protein IglB was slightly less stable than the others may indicate that stability depends to some degree on the size of the antigen expression cassette.
3.4. Immunization with rLVS ΔcapB overexpressing FPI T6SS proteins induces high antigen-specific cytokine production and a Th1-type antibody response
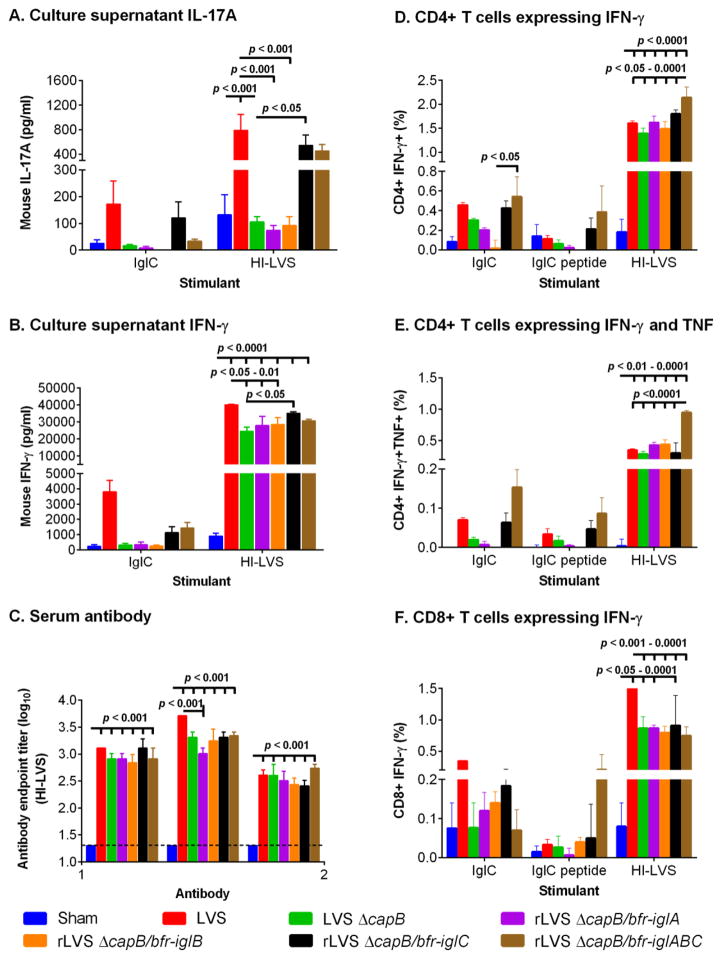
Previous studies have shown that IFN-γ, TNF-α, and/or IL-17 are critical for protection against challenge with F. tularensis and other intracellular pathogens [35–38]. To examine T cell immune responses generated by the rLVS ΔcapB vaccines, we immunized BALB/c mice i.d. with various vaccines at Week 0, euthanized them at Week 4, and assayed T-cell mediated immune responses and serum antibody. In response to in vitro stimulation with IglC protein (produced from recombinant E. coli as we described previously [28]), splenocytes from mice immunized with rLVS ΔcapB/bfr-iglC or bfr-iglABC secreted greater amounts of IL-17A (Fig. 3A) and IFN-γ (Fig. 3B) into the culture supernatant than sham- or LVS ΔcapB -immunized mice, although the differences did not reach statistical significance. In response to in vitro stimulation with HI-LVS, splenocytes from mice immunized with rLVS ΔcapB/bfr-iglC or bfr-iglABC also secreted greater amounts of IL-17A into the culture supernatant than sham- or LVS ΔcapB-immunized mice, comparable to splenocytes from LVS-immunized mice. Consistently, splenocytes from these mice generated significantly greater frequencies of Th1-type CD4+ T cells expressing IFN-γ (Fig. 3D, sFig. 3), or IFN-γ +TNF (Fig. 3E), TNF + IL-2, or IFN-γ + TNF + IL-2 (data not shown) in response to in vitro stimulation with IglC, IglC peptide or HI-LVS than splenocytes from LVS ΔcapB-immunized mice. Splenocytes from mice immunized with rLVS ΔcapB/bfr-iglABC showed the highest frequencies of Th1-type CD4+ T cells expressing IFN-γ (Fig. 3D) or IFN-γ +TNF (Fig. 3E) in response to in vitro stimulation with IglC and HI-LVS. However, splenocytes from LVS ΔcapB- and rLVS ΔcapB-immunized mice had significantly lower frequencies of CD8+ IFN-γ+ T cells in response to HI-LVS (Fig. 3F) than splenocytes from LVS-immunized mice. With respect to humoral immune responses, all vaccine candidates induced HI-LVS-specific balanced IgG2a and IgG1 antibody levels that were significantly greater than that induced by the sham-immunized mice; LVS-immunized mice had the highest level of IgG2a serum antibody (Fig. 3C). Thus, overall, the rLVS ΔcapB vaccines overexpressing IglC or the fusion protein of IglABC had enhanced T-cell mediated immune responses compared with the parental LVS ΔcapB vaccine.
Fig. 3. Immunization with rLVS ΔcapB overexpressing FPI T6SS proteins induces greater T-cell mediated immune response and a Th1-type antibody response.
Mice (3/group) were immunized i.d. with various vaccines; euthanized 4 weeks later; and their splenocytes isolated and stimulated with IglC or HI-LVS overnight or for 3 days. The culture supernatant was assayed for IL-17A (A) or IFN-γ (B) after 3 days incubation with antigen and the cells assayed for CD4+ or CD8+ T cells expressing IFN-γ or IFN-γ +TNF as indicated after overnight incubation with antigen (D–F). Their sera were isolated and assayed for antibodies specific to HI-LVS (C). Values are means ± SE. *, P<0.05; **, P < 0.01; ***, P< 0.001; ****, P< 0.0001 by Two-Way ANOVA with multiple comparisons (Prism 6.04); all comparisons are between the vaccine directly beneath the open bar and the other vaccines. The results from the experiment shown are representative of two independent experiments.
3.5. Immunization with rLVS ΔcapB/bfr-iglABC induces improved protective immunity against respiratory challenge with F. tularensis Schu S4
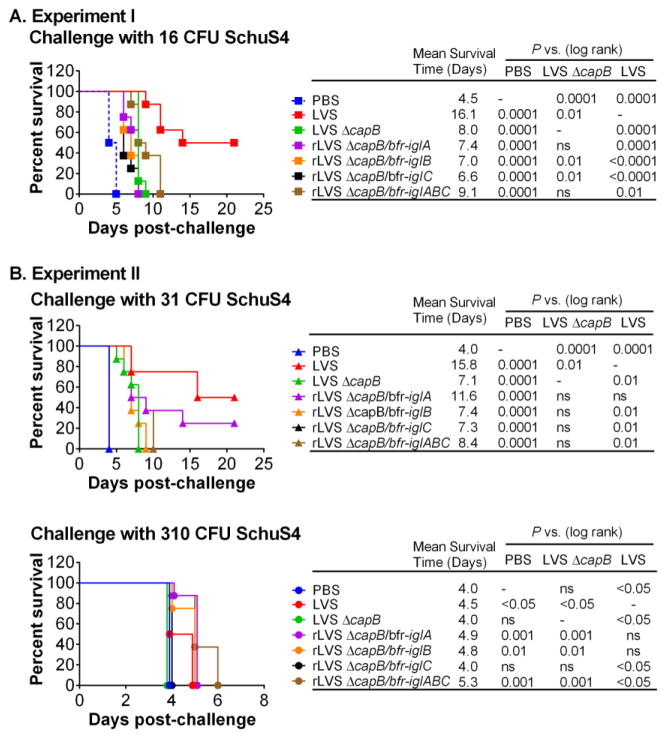
To evaluate rLVS ΔcapB/bfr-iglA, iglB, iglC, or iglABC for efficacy in mice against respiratory challenge with virulent F. tularensis Schu S4, we immunized mice i.d. with PBS (Sham), LVS, LVS ΔcapB, or rLVS ΔcapB, challenged them 7 weeks later i.n. with a high lethal dose of F. tularensis Schu S4 (16 CFU, equivalent to 5 × LD50), and observed the mice closely for signs of illness and death. Mice immunized with rLVS ΔcapB/bfr-iglABC survived longer (mean survival time 9.1 days) than sham-immunized mice (mean survival time 4.5 days) (p<0.0001) and mice immunized with the parental LVS ΔcapB or rLVS ΔcapB/bfr-iglA, iglB, or iglC (mean survival time 6.6–8.0 days; difference not statistically significant) (Fig. 4A).
Fig. 4. Mice immunized with attenuated rLVS ΔcapB/bfr-iglABC, comprising immunodominant epitopes of IglA, IglB, and IglC, survive longer than sham-immunized mice and mice immunized with the parental LVS ΔcapB.
BALB/c mice (8/group) were immunized i.d. with various vaccines, challenged with (A) 16 CFU at 49 days post-immunization (A, Experiment I) or with 31 (B) or 310 (C) CFU F. tularensis Schu S4 at 42 days (B, Experiment II) and monitored for signs of illness and death for 21 days. Mean Survival Day was calculated by dividing the sum of the surviving days of all mice by the total number of mice examined, with animals surviving until the end of the experiment given a survival time of 21 days, when the experiment was terminated. Survival curves between different groups were compared by log-rank test (Mantel-Cox) (Prism 6.04).
To verify further the efficacy of rLVS ΔcapB vaccines against challenge with F. tularensis Schu S4, we repeated the above experiment and challenged mice i.n. 6 weeks later with two higher lethal doses (31 and 310 CFU) of F. tularensis Schu S4, equivalent to approximately 10 and 100 LD50, respectively. Consistently, after i.n. challenge with 31 CFU of Schu S4, mice immunized with rLVS ΔcapB/bfr-iglA, iglB, iglC, or iglABC survived longer than sham-immunized mice (p < 0.0001) and generally longer than LVS ΔcapB-immunized mice (differences not statistically significant). In this experiment, mice immunized with rLVS ΔcapB/bfr-iglA were especially well protected - mean survival time 11.6 days vs. 4 days for sham-immunized mice and 7.1 days for LVS ΔcapB-immunized mice - but not as well protected as LVS-immunized mice (mean survival time 15.8 days), but this difference was not statistically significant (Fig. 4B, upper section). After i.n. challenge with 310 CFU of Schu S4, although all mice died by day 6 post-challenge, mice immunized with rLVS ΔcapB/bfr-iglABC survived significantly longer than all other mice including LVS-immunized mice (Fig. 4B, lower section). Mice immunized with rLVS ΔcapB/bfr-iglA or iglB survived significantly longer than sham- and LVS ΔcapB-immunized mice, comparable to LVS-immunized mice.
To explore the efficacy of rLVS ΔcapB/bfr-iglABC by the i.n. route, we immunized mice i.n. and challenged them 6 weeks later with 26 CFU of F. tularensis SchuS4. As shown in sFig. 4, the majority of immunized mice survived. Mice immunized with rLVS ΔcapB/bfr-iglABC survived significantly longer than sham-immunized mice (p < 0.0001); differences in survival between rLVS ΔcapB/bfr-iglABC-immunized mice and mice immunized with LVS ΔcapB or LVS were not statistically significant (sFig. 4A). Immunized mice that survived challenge showed temporary weight loss from which they recovered by 2weeks post-challenge (sFig. 4B).
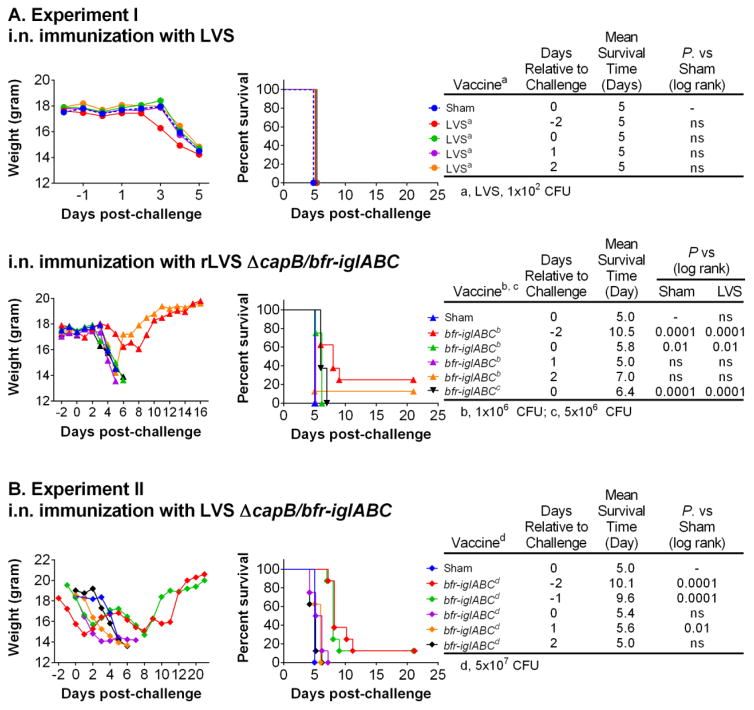
3.6. Immediate pre- or post-exposure prophylaxis with rLVS ΔcapB/bfr-iglABC but not LVS induces partial protective immunity against respiratory challenge with F. tularensis Schu S4 strain and protection is correlated with the induction of a strong innate immune response
To evaluate the efficacy of rLVS ΔcapB/bfr-iglABC as a pre- or post-exposure vaccine, we immunized mice i.n. with PBS (Sham), 102 CFU LVS, or 1 × 106 or 5 × 106 CFU rLVS ΔcapB/bfr-iglABC two days before (−2 days), the same day as (0 day), or one day (1 day) or two days (2 days) after Schu S4 respiratory challenge and monitored mice closely for signs of illness and weight change. We evaluated mice for illness using a Clinical Score (CS) of 0–4 as follows: 0, normal; 1, questionable illness; 2, mild but definitive illness; 3, moderate to severe illness (euthanized if poorly responsive); 4, severe illness, moribund and euthanized. All sham- and LVS-immunized mice became ill (CS ≥ 3) by Day 3 or 4 post-challenge and became moribund and were euthanized (CS = 4) at Day 5 post-challenge (Fig. 5A, upper section). In contrast, mice immunized with 1× 106 CFU of rLVS ΔcapB/bfr-iglABC at −2 days were not sick (CS 0 or 1 except one mouse with CS = 2) until Day 6 post-challenge and survived significantly longer (mean survival time 10.5 days) than both sham- and LVS-immunized mice (mean survival time 5 days). Mice immunized with 1 × 106 CFU or 5 × 106 CFU (Fig. 5A, lower section) of rLVS ΔcapB/bfr-iglABC on the day of challenge (Day 0) also survived significantly longer (mean survival times 5.8 and 6.4 days, respectively) than both sham-immunized mice and mice immunized with LVS at Day 0. When immunized at 1 or 2 days post-challenge, mice immunized with rLVS ΔcapB/bfr-iglABC had mean survival times comparable to sham-and LVS-immunized mice (Fig. 5A, lower section).
Fig. 5. Immediate pre- or post-exposure prophylaxis with rLVS ΔcapB/bfr-iglABC but not LVS induces partial protective immunity against respiratory challenge with F. tularensis Schu S4.
BALB/c mice were sham-immunized or immunized i.n. with 102 CFU of LVS (A, Experiment I, upper panel), 1 × 106 CFU or 5 × 106 CFU of rLVS ΔcapB/bfr-iglABC (A, Experiment I, lower panel), or 5 × 107 CFU of rLVS ΔcapB/bfr-iglABC (B, Experiment II) 2 days before (−2), 1 day before (−1), the day of (0), 1 day after (1), or 2 days after (2) challenge i.n. with 10 CFU F. tularensis Schu S4, and monitored for signs of illness and death for up to 21 days. Shown are the results from two independent experiments (one in A&B and the other in C). Mean Survival Day was calculated by dividing the sum of the surviving days of all mice by the total number of mice examined, with animals surviving until the end of the experiment given a survival time of 21 days, when the experiment was terminated. Survival curves between different groups were compared by log-rank test (Mantel-Cox) (Prism 6.04). In Experiment I, at day 3 post challenge, before any mice had died, the mean weight of mice immunized with LVS on day −2 was significantly lower than that of the sham-immunized mice (p < 0.05), mice immunized with 1×106 rLVS ΔcapB/bfr-iglABC at day −2, 0, and 2, and mice immunized with 5×106 rLVS ΔcapB/bfr-iglABC at day 0 (A, left panels). At days 4 and 5 post challenge, the mean weight of mice immunized with rLVS ΔcapB/bfr-iglABC (Day −2, 1×106) was significantly greater than that of sham-immunized mice and mice immunized with rLVS ΔcapB/bfr-iglABC at day 0 and day 1 post challenge (A, lower left panel). In Experiment II, mice immunized with 5×107 rLVS ΔcapB/bfr-iglABC had transient weight loss that partially or fully recovered if they were immunized at day −2 or −1 before challenge (B, left panel).
To explore the efficacy of a higher dose of rLVS ΔcapB/bfr-iglABC as immediate pre- and post-exposure prophylaxis against Schu S4 respiratory challenge, we repeated the experiment described above with an immunizing dose of 5 × 107 CFU (tested as generally safe, but somewhat toxic as evidenced by transient weight loss, sFig. 5 and Fig. 5B, left panel, Days −2 to 0 relative to challenge). The extent of protection was directly dependent upon the time relative to challenge, with mice immunized sooner surviving longer. Mice immunized with 5 × 107 CFU rLVS ΔcapB/bfr-iglABC at −2, −1, or even 1 day post-challenge with Schu S4 survived significantly longer than sham-immunized mice (Fig. 5B, middle and right panel).
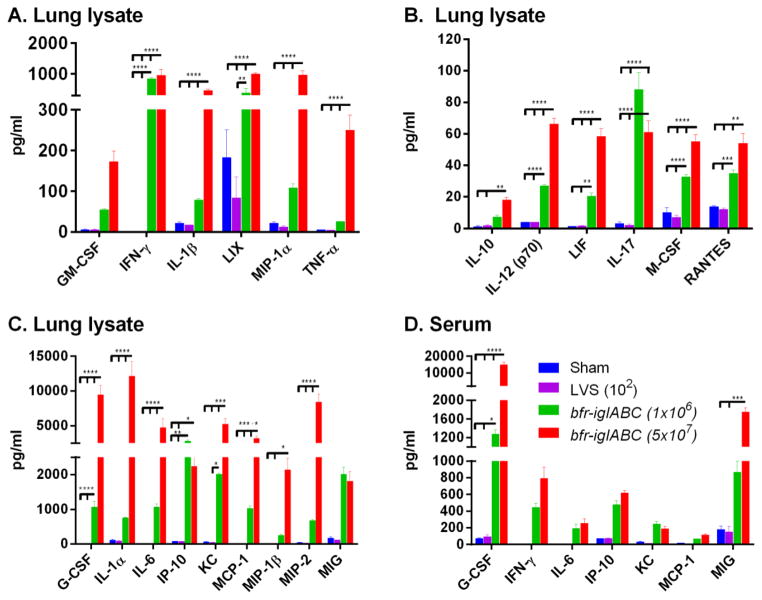
To explore the mechanism of protection provided by immediate pre-exposure prophylaxis with rLVS ΔcapB/bfr-iglABC, we immunized mice in groups of 3 i.n. with PBS (Sham), 102 CFU LVS, or 1 ×106 or 5 ×107 CFU rLVS ΔcapB/bfr-iglABC; euthanized them 2 days later; and assayed lung lysates and sera for cytokine/chemokine production using a mouse 32-Plex cytokine/chemokine kit. We found that mice immunized with 1 ×106 or 5 × 107 rLVS ΔcapB/bfr-iglABC had significantly higher levels of pro-inflammatory cytokines/chemokines in their lungs (21 out of 32 cytokines/chemokines assayed) and sera (7 out of the 32) than sham-immunized mice and mice immunized with LVS (Fig. 6A–6D); many of the cytokines in rLVS ΔcapB/bfr-iglABC-immunized mice were orders of magnitude higher than in sham-and LVS-immunized mice. In most but not all cases, mice immunized with the higher dose of rLVS ΔcapB/bfr-iglABC had higher cytokine/chemokine levels than mice immunized with the lower dose of this vaccine. In contrast, there were no significant differences in cytokine/chemokine levels between LVS- and sham-immunized mice in the lungs or sera (Fig. 6A–6D). These results show that mice immunized with rLVS ΔcapB/bfr-iglABC, which could be administered safely at very high doses, rapidly develop a strong innate immune response in the lung and blood, whereas mice immunized with LVS, which could be administered safely at only very low doses, do not. Taken together with the above results on the efficacy of immediate pre-exposure prophylaxis, where rLVS ΔcapB/bfr-iglABC but not LVS provided near-term protection, these data show that the level of near-term protection correlates with the level of the innate immune response.
Fig. 6.
Immediate pre-exposure prophylaxis with rLVS ΔcapB/bfr-iglABC but not LVS induces strong innate immunity. Mice were immunized with PBS (Sham), 102 of LVS, or 1 ×106 or 5 × 107 of rLVS ΔcapB/bfr-iglABC (bfr-iglABC) as indicated and euthanized at day 2 post immunization. Their lung lysates (A – C) and sera (D) were assayed for cytokine/chemokine production by a mouse 32-Plex kit. Shown are means ± SE (n = 3 mice) for each cytokine/chemokine. *, P<0.05; **, P < 0.01; ***, P< 0.001; ****, P< 0.0001 by Two-Way ANOVA with multiple comparisons (Prism 6.04).
4. Discussion
In this study, to improve upon the immunogenicity and efficacy of LVS ΔcapB, we developed recombinant LVS ΔcapB (rLVS ΔcapB) vaccines overexpressing F. tularensis FPI secreted proteins that comprise a T6SS. We show that these vaccines express the T6SS proteins in broth culture and in human macrophages, grow similarly to LVS ΔcapB in macrophages, are stable in vivo in the absence of antibiotic selection, induce humoral immune responses, and induce cell-mediated immune responses comparable to or greater than parental LVS ΔcapB. In general, when administered by the intradermal route, rLVS ΔcapB vaccines overexpressing FPI proteins IglA, IglB, IglC or IglABC are more efficacious than the parental LVS ΔcapB vaccine against F. tularensis Schu S4 respiratory challenge. Nevertheless, protection by this route is suboptimal; adequate protection will likely require heterologous prime-boost immunization, as shown in our previous study [11]. Administered by the intranasal route, rLVS ΔcapB/bfr-iglABC protected the majority of animals against F. tularensis Schu S4 respiratory challenge, and protection was not significantly different from the more toxic and sometimes lethal LVS vaccine.
While rLVS ΔcapB/bfr-iglABC was consistently more efficacious than the parental LVS ΔcapB vaccine, it was not consistently more efficacious than LVS; in two of three comparisons where the vaccines were administered by the intradermal route, LVS was significantly more potent than rLVS ΔcapB/bfr-iglABC, and in one comparison, rLVS ΔcapB/bfr-iglABC was significantly more potent than LVS. In general, both vaccines induced strong cellular and humoral immune responses, with LVS sometimes inducing a significantly stronger response than rLVS ΔcapB/bfr-iglABC (CD8+ T cells expressing IFN-γ; Fig. 3F), and sometimes rLVS ΔcapB/bfr-iglABC inducing a significantly stronger immune response than LVS (CD4+ T cells expressing IFN-γ alone or IFN-γ +TNF; Fig. 3D and E).
In the event of an intentional aerosol release of F. tularensis in a bioterrorism attack, it is estimated that the epidemic curve for tularemia by days after exposure would be most severe during the first 3 days, with 0% of cases at <1 day; 1% at 1 day; 15% at 2 days; and 45% at 3 days post-exposure [39]. This raises the possibility that an immediate post-exposure, or in the event of knowledge of an imminent attack, pre-exposure vaccine may be useful. Exploring this possibility, we found that, in contrast to the LVS vaccine, which was not at all protective immediately pre- or post-challenge, the rLVS ΔcapB/bfr-iglABC vaccine offered partial protection when administered 1 or 2 days prior to challenge. Administered post-challenge, the rLVS ΔcapB/bfr-iglABC vaccine delayed death, but survival was negligible. Protection was correlated with the induction of a strong innate immune response in the lung and blood by the rLVS ΔcapB/bfr-iglABC vaccine; the strong innate immune response induced by this vaccine but not by the LVS vaccine was likely a consequence of the fact that it could be administered safely at very high doses, whereas the LVS vaccine could not be. To our knowledge, this is the first report on the feasibility of using a live attenuated vaccine as near-term pre-exposure prophylaxis against F. tularensis. While the vaccine may have some utility in this regard, the relatively low level of protection of near-term prophylaxis compared with long-term prophylaxis when vaccines are administered intranasally or using a heterologous prime-boost vaccination strategy underscores the importance of long-term prophylaxis for protection against this bioterrorist threat.
In summary, we have shown that live attenuated rLVS ΔcapB/bfr-iglABC has improved immunogenicity and protective efficacy compared with its parental LVS ΔcapB vaccine and, in contrast to LVS, has partial efficacy when used as immediate pre- or post-exposure prophylaxis.
Supplementary Material
Highlights.
LVS ΔcapB overexpressing FPI proteins IglA, IglB, & IgC and fusion protein IglABC are constructed.
LVS ΔcapB express high amounts of FPI proteins from the bacterioferritin (bfr) promoter.
rLVS ΔcapB/bfr-iglC and bfr-iglABC express more IglC or IglABC than parental LVS ΔcapB in human macrophages and are stable in mice.
rLVS ΔcapB/bfr-iglC or bfr-iglABC induce greater T-cell immunity than LVS ΔcapB.
rLVS ΔcapB/bfr-iglABC administered i.d. provides better protection against F. tularensis Schu S4 respiratory challenge than LVS ΔcapB.
rLVS ΔcapB/bfr-iglABC administered i.n. provides high level protection against F. tularensis Schu S4 respiratory challenge.
rLVS ΔcapB/bfr-iglABC - but not LVS – provides partial efficacy as immediate pre- and post-exposure prophylaxis; protection is correlated with induction of a strong innate immune response.
Acknowledgments
This study was supported by NIH Grant AI101189 (M.A.H.) from the National Institutes of Health. We thank Nicole Marlenee for assistance with the animal studies.
Flow cytometry was performed in the UCLA Jonsson Comprehensive Cancer Center (JCCC) and Center for AIDS Research Flow Cytometry Core Facility that is supported by National Institutes of Health awards P30 CA016042 and 5P30 AI028697, and by the JCCC, the UCLA AIDS Institute, and the David Geffen School of Medicine at UCLA.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Qingmei Jia, Email: QJia@mednet.ucla.edu.
Richard Bowen, Email: rbowen@rams.colostate.edu.
Bai-Yu Lee, Email: BaLee@mednet.ucla.edu.
Barbara Jane Dillon, Email: BDillon@mednet.ucla.edu.
Saša Masleša-Galić, Email: SGalic@mednet.ucla.edu.
References
- 1.Bell JF, Owen CR, Larson CL. Virulence of Bacterium tularense. I. A study of the virulence of Bacterium tularense in mice, guinea pigs, and rabbits. J Infect Dis. 1955;97:162–6. doi: 10.1093/infdis/97.2.162. [DOI] [PubMed] [Google Scholar]
- 2.Day WC, Berendt RF. Experimental tularemia in Macaca mulatta: relationship of aerosol particle size to the infectivity of airborne Pasteurella tularensis. Infect Immun. 1972;5:77–82. doi: 10.1128/iai.5.1.77-82.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saslaw S, Eigelsbach HT, Prior JA, Wilson HE, Carhart S. Tularemia vaccine study. II. Respiratory challenge. Arch Intern Med. 1961;107:702–14. doi: 10.1001/archinte.1961.03620050068007. [DOI] [PubMed] [Google Scholar]
- 4.Saslaw S, Eigelsbach HT, Wilson HE, Prior JA, Carhart S. Tularemia vaccine study. I. Intracutaneous challenge. Arch Intern Med. 1961;107:689–701. doi: 10.1001/archinte.1961.03620050055006. [DOI] [PubMed] [Google Scholar]
- 5.Matyas BT, Nieder HS, Telford SR., 3rd Pneumonic tularemia on Martha’s Vineyard: clinical, epidemiologic, and ecological characteristics. Ann N Y Acad Sci. 2007;1105:351–77. doi: 10.1196/annals.1409.013. [DOI] [PubMed] [Google Scholar]
- 6.Feldman KA, Enscore RE, Lathrop SL, Matyas BT, McGuill M, Schriefer ME, et al. An outbreak of primary pneumonic tularemia on Martha’s Vineyard. N Engl J Med. 2001;345:1601–6. doi: 10.1056/NEJMoa011374. [DOI] [PubMed] [Google Scholar]
- 7.Jia Q, Lee BY, Bowen R, Dillon BJ, Som SM, Horwitz MA. A Francisella tularensis live vaccine strain (LVS) mutant with a deletion in capB, encoding a putative capsular biosynthesis protein, is significantly more attenuated than LVS yet induces potent protective immunity in mice against F. tularensis challenge. Infect Immun. 2010;78:4341–55. doi: 10.1128/IAI.00192-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marohn ME, Barry EM. Live attenuated tularemia vaccines: recent developments and future goals. Vaccine. 2013;31:3485–91. doi: 10.1016/j.vaccine.2013.05.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Conlan JW, Shen H, Golovliov I, Zingmark C, Oyston PC, Chen W, et al. Differential ability of novel attenuated targeted deletion mutants of Francisella tularensis subspecies tularensis strain SCHU S4 to protect mice against aerosol challenge with virulent bacteria: effects of host background and route of immunization. Vaccine. 2009;28:1824–31. doi: 10.1016/j.vaccine.2009.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cong Y, Yu JJ, Guentzel MN, Berton MT, Seshu J, Klose KE, et al. Vaccination with a defined Francisella tularensis subsp. novicida pathogenicity island mutant (DeltaiglB) induces protective immunity against homotypic and heterotypic challenge. Vaccine. 2009;27:5554–61. doi: 10.1016/j.vaccine.2009.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jia Q, Bowen R, Sahakian J, Dillon BJ, Horwitz MA. A heterologous prime-boost vaccination strategy comprising the Francisella tularensis live vaccine strain capB mutant and recombinant attenuated Listeria monocytogenes expressing F. tularensis IglC induces potent protective immunity in mice against virulent F. tularensis aerosol challenge. Infect Immun. 2013;81:1550–61. doi: 10.1128/IAI.01013-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clemens DL, Ge P, Lee BY, Horwitz MA, Zhou ZH. Atomic structure of T6SS reveals interlaced array essential to function. Cell. 2015;160:940–51. doi: 10.1016/j.cell.2015.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zaide G, Grosfeld H, Ehrlich S, Zvi A, Cohen O, Shafferman A. Identification and characterization of novel and potent transcription promoters of Francisella tularensis. Appl Environ Microbiol. 2011;77:1608–18. doi: 10.1128/AEM.01862-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gallagher LA, Ramage E, Jacobs MA, Kaul R, Brittnacher M, Manoil C. A comprehensive transposon mutant library of Francisella novicida, a bioweapon surrogate. Proc Natl Acad Sci U S A. 2007;104:1009–14. doi: 10.1073/pnas.0606713104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Santic M, Molmeret M, Klose KE, Jones S, Kwaik YA. The Francisella tularensis pathogenicity island protein IglC and its regulator MglA are essential for modulating phagosome biogenesis and subsequent bacterial escape into the cytoplasm. Cell Microbiol. 2005;7:969–79. doi: 10.1111/j.1462-5822.2005.00526.x. [DOI] [PubMed] [Google Scholar]
- 16.de Bruin OM, Duplantis BN, Ludu JS, Hare RF, Nix EB, Schmerk CL, et al. The biochemical properties of the Francisella pathogenicity island (FPI)-encoded proteins IglA, IglB, IglC, PdpB and DotU suggest roles in type VI secretion. Microbiology. 2011;157:3483–91. doi: 10.1099/mic.0.052308-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lai XH, Golovliov I, Sjostedt A. Expression of IglC is necessary for intracellular growth and induction of apoptosis in murine macrophages by Francisella tularensis. Microb Pathog. 2004;37:225–30. doi: 10.1016/j.micpath.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 18.Barker JR, Klose KE. Molecular and genetic basis of pathogenesis in Francisella tularensis. Ann N Y Acad Sci. 2007;1105:138–59. doi: 10.1196/annals.1409.010. [DOI] [PubMed] [Google Scholar]
- 19.Havlasova J, Hernychova L, Halada P, Pellantova V, Krejsek J, Stulik J, et al. Mapping of immunoreactive antigens of Francisella tularensis live vaccine strain. Proteomics. 2002;2:857–67. doi: 10.1002/1615-9861(200207)2:7<857::AID-PROT857>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 20.Janovska S, Pavkova I, Hubalek M, Lenco J, Macela A, Stulik J. Identification of immunoreactive antigens in membrane proteins enriched fraction from Francisella tularensis LVS. Immunol Lett. 2007;108:151–9. doi: 10.1016/j.imlet.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 21.Valentino MD, Maben ZJ, Hensley LL, Woolard MD, Kawula TH, Frelinger JA, et al. Identification of T-cell epitopes in Francisella tularensis using an ordered protein array of serological targets. Immunology. 2011;132:348–60. doi: 10.1111/j.1365-2567.2010.03387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blander SJ, Horwitz MA. Vaccination with the major secretory protein of Legionella pneumophila induces cell-mediated and protective immunity in a guinea pig model of Legionnaires’ disease. J Exp Med. 1989;169:691–705. doi: 10.1084/jem.169.3.691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horwitz MA, Harth G, Dillon BJ, Maslesa-Galic S. Recombinant bacillus calmette-guerin (BCG) vaccines expressing the Mycobacterium tuberculosis 30-kDa major secretory protein induce greater protective immunity against tuberculosis than conventional BCG vaccines in a highly susceptible animal model. Proc Natl Acad Sci U S A. 2000;97:13853–8. doi: 10.1073/pnas.250480397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Horwitz MA, Harth G. A new vaccine against tuberculosis affords greater survival after challenge than the current vaccine in the guinea pig model of pulmonary tuberculosis. Infect Immun. 2003;71:1672–9. doi: 10.1128/IAI.71.4.1672-1679.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Horwitz MA, Harth G, Dillon BJ, Maslesa-Galic S. A novel live recombinant mycobacterial vaccine against bovine tuberculosis more potent than BCG. Vaccine. 2006;24:1593–600. doi: 10.1016/j.vaccine.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 26.Horwitz MA, Harth G, Dillon BJ, Maslesa-Galic S. Extraordinarily few organisms of a live recombinant BCG vaccine against tuberculosis induce maximal cell-mediated and protective immunity. Vaccine. 2006;24:443–51. doi: 10.1016/j.vaccine.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 27.Tullius MV, Harth G, Maslesa-Galic S, Dillon BJ, Horwitz MA. A Replication-Limited Recombinant Mycobacterium bovis BCG vaccine against tuberculosis designed for human immunodeficiency virus-positive persons is safer and more efficacious than BCG. Infect Immun. 2008;76:5200–14. doi: 10.1128/IAI.00434-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jia Q, Lee BY, Clemens DL, Bowen RA, Horwitz MA. Recombinant attenuated Listeria monocytogenes vaccine expressing Francisella tularensis IglC induces protection in mice against aerosolized Type A F. tularensis. Vaccine. 2009;27:1216–29. doi: 10.1016/j.vaccine.2008.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maier TM, Havig A, Casey M, Nano FE, Frank DW, Zahrt TC. Construction and characterization of a highly efficient Francisella shuttle plasmid. Appl Environ Microbiol. 2004;70:7511–9. doi: 10.1128/AEM.70.12.7511-7519.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chamberlain RE. Evaluation of Live Tularemia Vaccine Prepared in a Chemically Defined Medium. Appl Microbiol. 1965;13:232–5. doi: 10.1128/am.13.2.232-235.1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.KuoLee R, Harris G, Conlan JW, Chen W. Oral immunization of mice with the live vaccine strain (LVS) of Francisella tularensis protects mice against respiratory challenge with virulent type A F. tularensis. Vaccine. 2007;25:3781–91. doi: 10.1016/j.vaccine.2007.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shen H, Harris G, Chen W, Sjostedt A, Ryden P, Conlan W. Molecular immune responses to aerosol challenge with Francisella tularensis in mice inoculated with live vaccine candidates of varying efficacy. PLoS One. 2010;5:e13349. doi: 10.1371/journal.pone.0013349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Griffin AJ, Crane DD, Wehrly TD, Bosio CM. Successful protection against tularemia in C57BL/6 mice is correlated with expansion of Francisella tularensis-specific effector T cells. Clin Vaccine Immunol. 2015;22:119–28. doi: 10.1128/CVI.00648-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Broms JE, Lavander M, Sjostedt A. A conserved alpha-helix essential for a type VI secretion-like system of Francisella tularensis. J Bacteriol. 2009;191:2431–46. doi: 10.1128/JB.01759-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Golovliov I, Twine SM, Shen H, Sjostedt A, Conlan W. A DeltaclpB mutant of Francisella tularensis subspecies holarctica strain, FSC200, is a more effective live vaccine than F. tularensis LVS in a mouse respiratory challenge model of tularemia. PLoS One. 2013;8:e78671. doi: 10.1371/journal.pone.0078671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lin JS, Kummer LW, Szaba FM, Smiley ST. IL-17 contributes to cell-mediated defense against pulmonary Yersinia pestis infection. J Immunol. 2011;186:1675–84. doi: 10.4049/jimmunol.1003303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Khader SA, Bell GK, Pearl JE, Fountain JJ, Rangel-Moreno J, Cilley GE, et al. IL-23 and IL-17 in the establishment of protective pulmonary CD4+ T cell responses after vaccination and during Mycobacterium tuberculosis challenge. Nature immunology. 2007;8:369–77. doi: 10.1038/ni1449. [DOI] [PubMed] [Google Scholar]
- 38.Elkins KL, Cowley SC, Bosio CM. Innate and adaptive immunity to Francisella. Ann N Y Acad Sci. 2007;1105:284–324. doi: 10.1196/annals.1409.014. [DOI] [PubMed] [Google Scholar]
- 39.Kaufmann AF, Meltzer MI, Schmid GP. The economic impact of a bioterrorist attack: are prevention and postattack intervention programs justifiable? Emerg Infect Dis. 1997;3:83–94. doi: 10.3201/eid0302.970201. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.