Abstract
Study Objectives:
To explore the perceptions and experiences of parents whose children were using melatonin.
Methods:
A qualitative exploratory study was undertaken using face-to-face semi-structured interviews that were audio recorded and transcribed verbatim. Data was thematically analyzed via open coding and subsequent axial coding. Data collection continued until theoretical saturation occurred.
Results:
Eleven interviews with parents of children with a neurodevelopmental disorder were conducted. Each parent perceived melatonin as effective in alleviating their child's sleep disturbance, and in restoring family functioning after many years of hardship and stress. The perceived “naturalness” of melatonin was valued by participants, who tended to favor it over other medications prescribed for sleep. The cost of melatonin was also commented on by every participant; however, all perceived the benefits of melatonin for the child and the family to outweigh the cost burden. When discussing the future, some parents were unsure of whether their child would still be using melatonin; however, others were happy for their child to continue melatonin indefinitely. In addition, many parents expressed a desire for prescribers to have greater knowledge about melatonin, and to acknowledge the positive impact melatonin had had on their lives.
Conclusions:
Parents perceive melatonin to be effective in alleviating their child's sleep disturbance and in improving their behavior, as well as restoring family functioning.
Citation:
Waldron AY, Spark MJ, Dennis CM. The use of melatonin by children: parents' perspectives. J Clin Sleep Med 2016;12(10):1395–1401.
Keywords: melatonin, parents' perspectives, qualitative research, sleep disturbances
INTRODUCTION
The endogenous hormone melatonin, predominately secreted at night, has multiple functions within the human body; melatonin plays a fundamental role in initiating and maintaining sleep and in regulating circadian rhythms.1 Therapeutically, melatonin has been used for the management of sleep disorders and jet lag and for the resynchronization of circadian rhythms in situations such as blindness and shift work.2,3 In Australia melatonin is a prescription-only medicine,4 and the only approved indication is for the short-term treatment of primary insomnia in adults over 55 years of age.5 In the UK, where melatonin is also unlicensed for use in children, use in children older than 1 month with a range of neurological conditions is suggested for a treatment of some sleep disorders, in doses of 2 to 10 mg with review every 6 months.2 Despite this recommendation, GPs in the UK have been reported as reluctant to write repeat prescriptions for melatonin prescribed previously by a psychiatrist.6 Diminished melatonin levels and/or disruption of the rhythmic secretion of melatonin can cause sleep disorders, and administration of exogenous melatonin has been found to improve the quality and duration of sleep.7,8 Melatonin is not addictive and, following long-term use, has been shown to elicit less residual drowsiness or withdrawal effects than other medications commonly used for sleep disturbances.9 Consequently, melatonin is gaining popularity, particularly in children with a neurodevelopmental disability, as a sleep promoting agent.6
Sleep disturbances in children and adolescents are relatively common. Approximately 10% of otherwise healthy preschool and school-aged children have been reported to experience some sleep difficulty10; the prevalence increases in children with neurodevelopmental disabilities and may be as high as 80% in this population.11 Sleep difficulties have been shown to be a major source of stress, not just for the child, but the entire family. Stress is especially noticeable in families of children with neurodevelopmental disabilities, where sleep problems add to the stresses associated with having a child with a disability.12 In severe instances, this stress may lead to breakdown in family functioning, as parents are affected by their child's lack of sleep.12–15 The consequences of a child's sleep disturbances on parental sleep are often the reason why a child is brought to the attention of a medical professional.16,17
BRIEF SUMMARY
Current Knowledge/Study Rationale: Sleep disorders in children can be stressful for both the child and their family and holistic care for children requires an understanding of parents' perceptions of alternative treatments. This study was undertaken to investigate parents' perspectives of melatonin use by their children.
Study Impact: Prescribers are provided with an insight into parents' perception that melatonin treatment has transformed both their child's and their lives. Knowing that parents and health care professionals can have different priorities and perceptions could improve the quality of care offered to families with children with sleep disturbances.
Parental acceptability of treatment options is influenced by their beliefs and the extent to which parents are affected by their child's sleep disturbance. As the severity of children's sleep problems increases, parents have been reported to be more likely to prefer melatonin treatment to behavioral treatment alone.18 Cultural differences are also known to influence perceptions of sleep and acceptable treatment regimens.13 The type of treatment accepted by parents can be influenced by their beliefs, so it is important that parental perceptions and emotions are acknowledged by health professionals.
Understanding parental perceptions of melatonin use in their children would enable health practitioners to provide holistic patient care. However, a gap has been identified in health professionals' understanding of parental perceptions as well as incongruity in recognizing the needs of parents.19,20 While parents' perceptions about sleep and treatment have been investigated previously, information was gathered quantitatively using a questionnaire.10 Questionnaires using questions developed from the researcher's perspective may not allow a true reflection of parental perceptions, but rather what the researcher believes parents may have experienced. Investigation of parents' perceptions of melatonin use by their children through semi-structured interviews would allow for a truer reflection of parents' experiences, fill a current gap in the literature and provide valuable knowledge for health professionals and investigators alike. Therefore, using qualitative methodology, this study aimed to explore parents' perceptions of melatonin, together with influencing factors and reasons for deciding to give melatonin to their child(ren).
METHODS
Procedure
A descriptive qualitative approach was used, because its exploratory nature is suited for exploring the perspectives of others.21,22 Semi-structured interviews that followed an interview guide were conducted between July and October 2013; data analysis began after the first interview and continued throughout the data collection period with adaption of the interview guide after each interview. This allowed unexpected themes that emerged to be explored in subsequent interviews, enabling a clearer reflection of parents' perceptions of melatonin use by their children.22 Interviews were audio recorded and transcribed verbatim. Thematic analysis of transcribed interviews involving inductive identification of codes was undertaken. This method allowed for the organization of data and identification of recurring themes.23 Open coding was used to develop initial categories, and the specificity of these categories was improved using subsequent axial coding.24 Interviews were double coded to enhance rigor. Member checking was also utilized, where emerging themes from their interview were sent to participants to review for accuracy.25 Interviews were conducted by one interviewer (AW) at a location that was convenient for the participant, which included the participant's home, La Trobe University, or a quiet corner of a café.
Participants
Participants were recruited through criterion sampling.24 In Australia, pediatric melatonin products are only available from a compounding pharmacy; therefore, the research project was advertised to parents through two compounding pharmacies (one regional and one metropolitan) that were members of Professional Compounding Chemists of Australia (PCCA). Posters were displayed in the pharmacies notifying parents of the study. Invitation letters were provided to parents on request and also included with each compounded melatonin product prepared for a child. Parents expressed their desire to participate in the study by returning their contact information to the University using the pre-paid envelope provided. They were then contacted via telephone to determine eligibility; following this, an interview time was organized. Participants were included if they were over the age of 18, had the ability to speak, read, and write English, and had a child under the age of 18 who had been using, or had previously used, melatonin for at least one month. Interviews continued until no new themes emerged after two consecutive interviews and data saturation could be considered to have been obtained.
Participants provided informed consent prior to the commencement of their interview. Ethics approval was obtained from the Faculty of Science, Technology and Engineering Human Ethics Committee, La Trobe University.
RESULTS
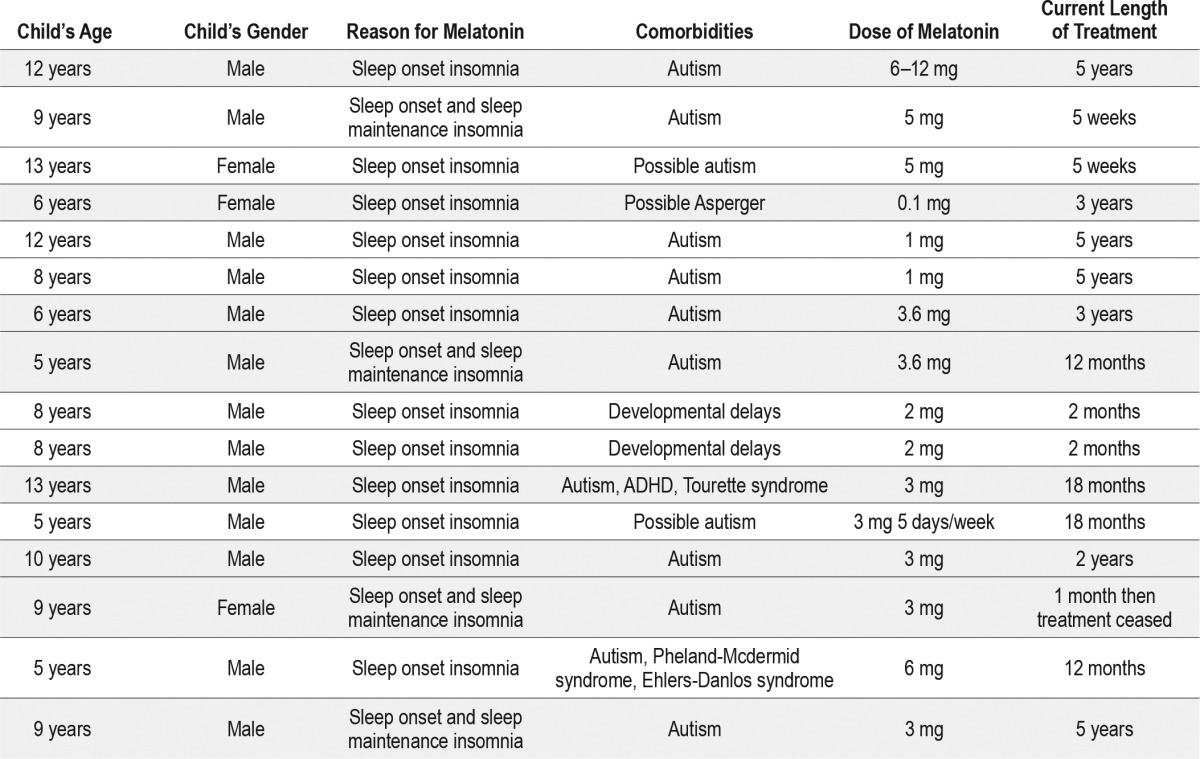
Eleven 30–90 minute interviews were conducted, with 13 parents (11 mothers and 2 fathers) who had 16 children between them, including one set of twins (Table 1). The children ranged in age from 5 to 13 years. All of the children had a neurodevelopmental disorder; 10 had autism, one had Tourette syndrome along with autism and ADHD, two experienced developmental delays, one suffered from rare chromosomal syndromes called Pheland Mcdermid syndrome and Ehlers-Danlos syndrome as well as autism, and for two the possibility of an autism diagnosis was being explored. All of the parents interviewed for this study said that their children had not experienced side effects when using melatonin. All children had been prescribed melatonin to assist with sleep onset.
Table 1.
Children from the 11 families (shaded groups) who were using, or had used, melatonin.
Six main themes emerged from the data, and these were divided into three broad categories; life before melatonin (reasons for giving melatonin and perceived naturalness of melatonin), life with melatonin (effectiveness and cost), and the future (long-term use and desire for more information and better relationships with prescribers).
Life before Melatonin
Reasons for Giving Melatonin
The pursuit of pharmacological treatment (including melatonin) was not parents' first line treatment and often occurred once parents felt that they could not handle the situation any longer. “I was at the end of my tether” M1. Parents were reluctant to give a medication, especially one that was not natural. Medications, such as sedating antihistamines, were recognized as having poor side effect profiles and long-term consequences such as tolerance. A range of behavioral and homeopathic treatments were used before melatonin was introduced ahead of other treatments, such as antihistamines, which were described by parents as unsafe. Behavioral and homeopathic treatments that had been tried were perceived to be ineffective; each treatment failure and worsening of symptoms exacerbated their sense of desperation. Once parents perceived that all possible “natural” options had been tried, pharmacological treatment was sought, often after discussing options with friends and family.
Before melatonin was introduced, each participant described the stress their child's sleep disturbance had on the entire family, and their desperation to find a solution. “I could quite understand why some mothers would put the pillow over their heads and smother their children, because that's how I felt, I just felt like for God's sake will you just go to sleep, because I wasn't getting enough sleep myself” M11.
Many participants described their child's sleep disturbance as being present from birth. Consequently, many years of these kinds of thoughts and emotions had been experienced before a solution was found. “The first three and a half years of his life were just hell” M6. In addition, many participants attributed lack of sleep as an influencing factor for poor daytime behavior and therefore, the impact of sleep disturbances were seen not only at night but also during the day. “It was just constant like all day all night all day” M5.
The extent of daytime misbehaviors as well as the severity of the child's sleep disturbance seemed to influence the time that elapsed before parents pursued pharmacological treatment. The more severe the daytime behavior and the greater the negative impact on the family, the earlier treatment was initiated. The behavior of M4's daughter was described as “out of control”: “They were crazy times, she used to try and run out on the road and get the car to run her over, oh God, it was so hard, it was so hard, without melatonin” M4. In comparison, the impact of lack of sleep on M3's daughter manifested as physical and psychological issues rather than behavioral disturbances. While these were not described as disrupting family functioning, they worried the participant. “Visibly, she's not pale with black rings she looks a lot better now, she looks healthier and she looks more relaxed um, she's a very um, she's not a high energy child but she just looks more relaxed and she tells me that she's happy now that she can sleep” M3.
Parents' lack of sleep made their own daytime functioning more challenging, and simple everyday tasks became more difficult. “How can you drive a car with no sleep?” M5. Despite these impacts on the child and family, parents had often tried many other options before pursuing pharmacological treatment, and melatonin was never the parents' first line treatment. “I tried all the other things and I was at the end, like he was just in this cycle of not sleeping and his behavior was getting quite bad, so I just wanted to try something that would help him get out of that cycle, so when I actually got to the point of him having it, I was just like, something else yes!” M1.
Participants had experienced a sense of desperation before melatonin was found, not only because of the negative impact of disturbed sleep on the entire family, but because all the techniques attempted previously had failed.
Perceived Naturalness of Melatonin
When treatment with melatonin was suggested its acceptability was increased if the child's medical practitioner or independent research described melatonin as a hormone that occurred naturally in the body. Often respondents did not regarded melatonin as a drug. “It's not a drug, it's natural” M4. “I probably didn't think that it would react like a drug because it's homeopathic” M11. The fact that exogenous melatonin was perceived as being natural was often described as being reassuring, and many parents expressed disbelief that an effective natural compound was available and able to restore family functioning.
Life with Melatonin
Effectiveness
Melatonin was reported to assist children to fall asleep by some parents and to keep children asleep by others. Following years of sleep deprivation and previous treatment failures, each participant did not expect melatonin to work. Yet, melatonin was reported as immediately effective in relieving 15 children's sleep disturbances. Parents also described their child's daytime behavior improving after the introduction of melatonin, which further alleviated parental stress and helped to restore their quality of life. The effectiveness of melatonin produced a sense of relief; that after years of hardship, a solution had finally been discovered. “It was a huge burden that was lifted” F3. “It was instant, it was amazing, which is why I kept getting up [during the night to check on her son], I thought it couldn't have possibly kicked in that quickly, and then I was panicking thinking oh my God he's died in his sleep or something” M10.
Disbelief and positive emotions were experienced after melatonin was introduced. However, the juxtaposition of life before and after using melatonin was blurred in one instance by the dosing regimen of melatonin. In this case, melatonin was given to the child for 5 nights each week, with 2 nights being drug free, as ordered by the prescriber. For the 2 nights each week that the child was not using melatonin, the mother was once again reliving life without melatonin, which elicited a sense of dread, illustrating the difference between life with and without melatonin. “Sometimes it's just dread, like oh tonight's the night when he doesn't have it and you think well what's it going to bring…It's sort of like, oh good I got through those nights” M1.
Nights without melatonin had been experienced by some other families when they either ran out of the medication or wanted to try a drug-free period. Some parents attempted to test the placebo effect by giving their child a substance that appeared to be melatonin, without telling the child. However, in each case, a sleep inducing effect was not observed when the placebo was given. “We ran out and we thought we might get the placebo effect if he thinks he's taking his melatonin but no it didn't work” M10. When parents ceased melatonin use for a short period to trial the effect, varying responses were seen. In some children, the effect of melatonin lasted for a few days after melatonin was stopped; however, in others the effect terminated immediately.
Sleep disturbance itself was described differently between families; some parents described sleep onset insomnia, while others detailed sleep maintenance insomnia. While melatonin was seen as effective no matter what type of sleep disturbance was reported, differences in the outcome of ceasing melatonin may be attributed to the type of sleep disturbance, along with other factors. Differences were also observed in the level of effectiveness over time. In one participant, the effectiveness of melatonin seemed to decrease once the child turned twelve, and the dose was increased to overcome this. Increasing the dose of melatonin was perceived to be safe and acceptable, due to its perceived naturalness. The reported decrease in effectiveness as the child matured did not detract from the parent's positive perception of melatonin.
The use of melatonin was also seen as providing parents time at night to relax and consequently relieved not only parental stress, but stress experienced by siblings.
“When you don't have to do that it means you can spend some time with the other one that's close to her age and he's not feeling so sad because [daughter] has ruled the whole family you know” M4.
Many parents mourned the fact that melatonin had not been found sooner which further highlighted the improved quality of life that melatonin brought to them.
Cost
Each participant mentioned the cost of melatonin, which is not government subsidized in Australia. “The only downfall was that it was so expensive, you know like it was nearly $70 for a bottle but God you couldn't go without it” M2. Many of the participants had private health coverage and were able to claim a portion of the cost back, so that out-of-pocket expenses equated to that of government subsidized medication.26 Despite this, melatonin was still perceived as expensive. Some families avoided the cost burden by obtaining melatonin from an online site, rather than a compounding pharmacy. “We just get it online now and it's just so much cheaper” M9. This presents a legal issue; in order to possess a prescription-only medication, a prescription from an Australian-registered medical practitioner is required, and therefore, use should only legally occur if a prescription is held.27 Despite the cost, all parents perceived the benefits of melatonin for the child and the family to be greater than the cost burden. “My husband and I would happily re-mortgage the house if I had to, to pay for this stuff” M7.
Future
Long-Term Use
Parents had differing views on how long they believed their child would be using melatonin. While some were happy for the child to use melatonin indefinitely, others were unsure and perceived melatonin to be a short-term intervention. These perceptions seemed to depend on the extent lack of sleep had impacted negatively on the child and the family. The greater the negative impact the higher the acceptability of long term use. Expected duration of treatment also depended on the amount of research the participant had done, and whether information about long term use had been found. Overall, many considered the benefits of melatonin to outweigh perceived long term consequences. “I just worry about what's happening to their minds when they're feeling so horrible from lack of sleep week after week, month after month, year after year so I think weighing that against the melatonin, I think I feel very happy about giving them the melatonin” M3.
Many participants expressed the desire for more information regarding melatonin and its long term use, to enable them to make informed decisions.
Desire for More Information and Better Relationships with Prescribers
Parents not only expressed a desire for more information about melatonin, but for family doctors (GPs) to be more knowledgeable about melatonin and to be aware of the negative impact of lack of sleep. “GPs know nothing, so we're constantly telling the GPs about stuff with regards to melatonin” M6. A pediatrician was usually the initial prescriber of melatonin, often offering melatonin as a treatment for a child's sleep disorder. When parents experienced difficulty in accessing pediatricians for ongoing treatment they asked their GP to prescribe melatonin, with mixed response. Consequently, several parents perceived GPs to have poor knowledge regarding melatonin, and one described a traumatic experience when their GP was unwilling to prescribe melatonin. “They're making me feel like I'm a drug addict…I cried in the office because she [doctor] wouldn't give it to her [child]” M4. One participant felt as though she was not taken seriously by the GP when describing her child's sleep disorder.
“It's crazy and it's torture, it's terrible, and for doctors to keep dismissing me that I'm tired just because all mothers are tired…it's more than that. So there are two things, they need to recognize the seriousness of lack of sleep and they have to recognize that there is a solution there which, after everything that's been tried, melatonin might be worth a go” M5.
Not all families experienced conflict with prescribers. In general, those parents who described conflict with a doctor had approached them to prescribe melatonin after hearing about it from support groups, friends, or family. If prescribers acknowledge parental perceptions, conflict such as this would be avoided, and better relationships could be developed, allowing for better patient care.
Accessing information was difficult for participants and they expressed a desire that more information about melatonin be given to them by their health professionals. “I think we should be given some more information about melatonin and that's the thing, we just don't know as parents a lot of the time and we rely on health professionals to do the right thing by our child” M8.
Some parents described a desire for doctors to know more about melatonin to spare this conflict for other families. In addition, some parents described their excitement in participating in this study in order to contribute to the information available to health professionals about melatonin. “I definitely would like to take these results back to the pediatrician and the GP just to help educate them a bit more” M5. It is clear that life before the commencement of melatonin was a hardship, with the child's sleep disturbance negatively impacting the life of the entire family. Then when melatonin was initiated and found to effectively relieve their child's sleep disturbance, parents experienced a sense of relief, making the future seem a brighter prospect.
DISCUSSION
All participants perceived melatonin to be effective, whether their child had difficulty going to sleep or staying asleep. When their children's ability to sleep improved, family stress was alleviated and family functioning restored, which parents attributed to melatonin. The life of the family was often so disrupted prior to melatonin that even a small improvement was viewed as significant. This concept is consistent with other findings, where the improvement in a child's sleep was more obvious the more severe their sleep disorder.28 Parents play a large role in diagnosis and treatment and health professionals' have been found to rely on them to raise sleep issues during clinic visits29; consequently, parental perceptions and families varying criteria for effectiveness should be acknowledged by health professionals.
None of the parents had any expectation that melatonin would solve their child's sleep issues, exemplifying the significance of the perceived effectiveness of melatonin. In clinical situations where there is marked parental anxiety, there is often a high expectation that any medical intervention and treatment may assist their child's condition, and thus a high placebo response is generated.28 This was unlikely to be a major factor for melatonin given that each parent had no expectation of melatonin working due to many experiences of treatment failure. The response to melatonin has been reported to vary between children, depending on the underlying cause and the presence of neurodevelopmental disorders.28 Sleep disturbance is often multifactorial consequently the differing responses to specific doses of melatonin could be explained by other differences between children such as age and coexisting conditions.28 The effect of exogenous melatonin may also be influenced by the timing of the dose. In adults 0.5 and 3 mg doses of melatonin have been found to be equally effective at moving sleep, with doses given mid-afternoon being more effective at moving sleep forward than doses given close to bedtime.30 While melatonin was perceived as being effective by every participant, one parent reported that the effect of melatonin decreased after her son turned twelve, and that a dose increase was needed to have the same effect. As the participant's son was entering puberty, a time when melatonin excretion has been reported to increase,31 this could explain the need for a melatonin dose increase. Health professionals should discuss with parents differences in melatonin effectiveness that may be seen between children, and throughout the course of melatonin treatment.
The daytime behavior of every child was perceived to have improved. Most children in this study had autism and many parents described improvement of the associated symptoms and characteristics. Sleep disorders in children with autism have been reported to be associated with developmental regression, poor social interaction, increased stereotypy, problems with communication, and overall autistic behavior, many of which improved with more sleep.32 This could explain the report of one participant that following the introduction of melatonin, increased sleep had changed her child's behavior so much that a possible diagnosis of Asperger syndrome had been discarded, suggesting that symptoms associated with serious conditions could be caused by lack of sleep resulting in misdiagnosis.
Under-diagnosis of children with sleep disorders is another potential problem described by participants who felt they were not taken seriously when describing their child's sleep disturbance. Undetected sleep problems in children have been attributed to insufficient training of health professionals and lack of knowledge about childhood sleep, as medical and mental health professionals receive little or no formal training in pediatric sleep.33 Given the potential for sleep problems to impact upon child development and parental well-being, these possible diagnostic problems and subsequent lack of treatment can have disastrous consequences for families. Improving health professionals' appreciation of parental perceptions of their child's sleep is one way to avoid under-diagnosis of sleep disorders or misdiagnosis of neurodevelopmental conditions, allowing for appropriate treatment to be implemented.
That Australian parents perceived melatonin to be expensive yet continue to purchase it is an indication of the perceived positive effect of treatment. For parents in countries (similar to Australia) where melatonin use in children is unlicensed the cost of melatonin treatment for their children is likely to be an issue. In these countries not only are the products likely to be more expensive but also the cost of obtaining prescriptions if family doctors are reluctant to prescribe melatonin, as has been reported in the United Kingdom.6 While cost may not be an issue for parents in countries where melatonin is relatively inexpensive the continued purchase of melatonin products when they are expensive is an indication of the value parents place on melatonin treatment for their children.
While this study adds to the current knowledge of melatonin use in children, it has some limitations. The extent of parental perceptions explored in the interviews was potentially restricted by the interviewer and it is possible that themes were missed or inadequately explored. The small number of interviews could be considered a limitation; however, it was within the anticipated range of between 6 and 12 interviews previously reported to be enough interviews to reach data saturation.34 The interviews were all conducted in Victoria so may not be representative of the views of parents from other states or countries, particularly countries such as the USA where melatonin is freely available. A strength of the study was its qualitative methodology, providing insight into and reporting the perceptions of parents whose children were using melatonin to alleviate their sleep disturbance.
CONCLUSIONS
Life before melatonin was described as a burden; the introduction of melatonin turned family's lives around. Parents of children with neurodevelopmental disorders reported melatonin to be effective both in alleviating their child's sleep disturbance and in improving their behavior, as well as restoring family functioning. Melatonin was perceived to be natural, which enhanced its acceptability to parents. Despite melatonin being considered expensive the benefits were considered to outweigh the cost burden. Overall, parents wanted health professionals' knowledge about melatonin to be improved, and for health professionals to acknowledge the difference melatonin had made to their family's life. Sleep disturbance in children is a real and detrimental problem that many families experience, and melatonin was perceived as an effective option for ameliorating sleep disturbances.
DISCLOSURE STATEMENT
This was not an industry supported study. There were no external sources of funding. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors acknowledge the pharmacies that assisted in recruiting participants for the study, as well as the parents who volunteered to share their experiences of using compounded melatonin in their children.
ABBREVIATIONS
- BMI
body mass index
- GP
general practitioner (family doctor)
- OSA
obstructive sleep apnea
- UK
United Kingdom
- USA
United States of America
REFERENCES
- 1.Carter MD, Juurlink DN. Five things to know about melatonin. Can Med Assoc J. 2012;184:1923. [Google Scholar]
- 2.Brayfield A, editor. Martindale the complete drug reference. 28th ed. London: Pharmaceutcial Press; 2014. Melatonin; pp. 2551–2. [Google Scholar]
- 3.Arendt J, Skene DJ. Melatonin as a chronobiotic. Sleep Med Rev. 2005;9:25–39. doi: 10.1016/j.smrv.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 4.The Therapeutic Goods Administration. The Poisons Standard (the SUSMP) [Accessed April 1, 2014]. http://www.tga.gov.au/industry/scheduling-poisons-standard.htm.
- 5.Rossi S, editor. Australian Medicines Handbook. Adelaide, SA: AMH Pty Ltd; 2014. [Google Scholar]
- 6.Bramble D, Feehan C. Psychiatrists' use of melatonin with children. J Child Adolesc Ment Health. 2005;10:145–9. doi: 10.1111/j.1475-3588.2005.00358.x. [DOI] [PubMed] [Google Scholar]
- 7.Wirojanan J, Jacquemont S, Diaz R, Anders SBTF, Hagerman RJ, Goodlin-Jones BL. The efficacy of melatonin for sleep problems in children with autism, fragile X syndrome, or autism and fragile X syndrome. J Clin Sleep Med. 2009;5:145–50. [PMC free article] [PubMed] [Google Scholar]
- 8.Skidmore-Roth L. Herbs & natural supplements. 4th ed. Missouri: Mosby Elsevier; 2010. [Google Scholar]
- 9.Kostoglou-Athanassiou I. Therapeutic applications of melatonin. Ther Adv Endocrinol Metab. 2013;4:13–24. doi: 10.1177/2042018813476084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Banta S. Use of melatonin in children and adolescents: clinicians' and parents' perspective. J Child Adolesc Ment Health. 2008;13:82–4. doi: 10.1111/j.1475-3588.2007.00459.x. [DOI] [PubMed] [Google Scholar]
- 11.Ross C, Davies P, Whitehouse W. Melatonin treatment for sleep disorders in children with neurodevelopmental disorders: an observational study. Dev Med Child Neurol. 2002;44:339–44. doi: 10.1017/s0012162201002171. [DOI] [PubMed] [Google Scholar]
- 12.Hoffman CD, Sweeney DP, Lopez-Wagner MC, Hodge D, Nam CY, Botts BH. Children with autism: sleep problems and mothers' stress. Focus Autism Other Dev Disabl. 2008;23:155–65. [Google Scholar]
- 13.Doo S, Wing YK. Sleep problems of children with pervasive developmental disorders: correlation with parental stress. Dev Med Child Neurol. 2006;48:650–5. doi: 10.1017/S001216220600137X. [DOI] [PubMed] [Google Scholar]
- 14.Larson AM, Ryther RCC, Jennesson M, et al. Impact of pediatric epilepsy on sleep patterns and behaviors in children and parents. Epilepsia. 2012;53:1162–9. doi: 10.1111/j.1528-1167.2012.03515.x. [DOI] [PubMed] [Google Scholar]
- 15.Meltzer LJ, Mindell JA. Relationship between child sleep disturbances and maternal sleep, mood, and parenting stress: a pilot study. J Fam Psychol. 2007;21:67–73. doi: 10.1037/0893-3200.21.1.67. [DOI] [PubMed] [Google Scholar]
- 16.Couturier JL, Speechley KN, Steele M, Norman R, Stringer B, Nicolson R. Parental perception of sleep problems in children of normal intelligence with pervasive developmental disorders: prevalence, severity, and pattern. J Am Acad Child Adolesc Psychiatry. 2005;44:815–22. doi: 10.1097/01.chi.0000166377.22651.87. [DOI] [PubMed] [Google Scholar]
- 17.Goldman SE, Bichell TJ, Surdyka K, Malow BA. Sleep in children and adolescents with Angelman syndrome: association with parent sleep and stress. J Intellect Disabil Res. 2012;56:600–8. doi: 10.1111/j.1365-2788.2011.01499.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Keenan RA, Wild MR, McArthur I, Espie CA. Children with developmental disabilities and sleep problems: parental beliefs and treatment acceptability. J Appl Res Intellect Disabil. 2007;20:455–65. [Google Scholar]
- 19.Latour JM, Hazelzet JA, Duivenvoorden HJ, van Goudoever JB. Perceptions of parents, nurses, and physicians on neonatal intensive care practices. J Pediatr. 2010;157:215–20. doi: 10.1016/j.jpeds.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 20.Latour JM, van Goudoever J, Duivenvoorden H, et al. Differences in the perceptions of parents and healthcare professionals on pediatric intensive care practices. Pediatr Crit Care Med. 2011;12:215–20. doi: 10.1097/PCC.0b013e3181fe3193. [DOI] [PubMed] [Google Scholar]
- 21.Chenail RJ. How to conduct clinical qualitative research on the patient's experience. Qual Rep. 2011;16:1173–90. [Google Scholar]
- 22.O'Leary Z. London: SAGE Publications; 2010. The essential guide to doing your research project. [Google Scholar]
- 23.Atkinson P, Coffey A. Thousand Oaks: SAGE; 1996. Making sense of qualitative data: complementary research strategies. [Google Scholar]
- 24.Liamputtong P, Ezzy D. Qualitative Research Methods. 2nd ed. South Melbourne: Oxford University Press; 2005. [Google Scholar]
- 25.Schneider Z, Elliot D, LoBiondo-Wood G, Haber J. Nursing research: methods, critical appraisal and utilisation. 2nd ed. Marrickville: Elsevier; 2003. [Google Scholar]
- 26.Australian Government Department of Health. About the PBS. [Accessed October 17, 2013]. http://www.pbs.gov.au/info/about-the-pbs.
- 27.Therapeutic Goods Administration. Personal importation scheme. [Accessed October 20, 2013]; http://www.tga.gov.au/consumers/personal-importation-scheme.htm. [Google Scholar]
- 28.Phillips L, Appleton RE. Systematic review of melatonin treatment in children with neurodevelopmental disabilities and sleep impairment. Dev Med Child Neurol. 2004;46:771–5. doi: 10.1017/s001216220400132x. [DOI] [PubMed] [Google Scholar]
- 29.Schreck KA, Richdale AL. Knowledge of childhood sleep: a possible variable in under or misdiagnosis of childhood sleep problems. J Sleep Res. 2011;20:589–97. doi: 10.1111/j.1365-2869.2011.00922.x. [DOI] [PubMed] [Google Scholar]
- 30.Burgess HJ, Revell VL, Molina TA, Eastman CI. Human phase response curves to three days of daily melatonin: 0.5 mg versus 3.0 mg. J Clin Endocrinol Metab. 2010;95:3325–31. doi: 10.1210/jc.2009-2590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Penny R. Melatonin excretion in normal males and females: increase during puberty. Metabolism. 1982;31:816–23. doi: 10.1016/0026-0495(82)90081-6. [DOI] [PubMed] [Google Scholar]
- 32.Rossignol DA, Frye RE. Melatonin in autism spectrum disorders: a systematic review and meta-analysis. Dev Med Child Neurol. 2011;53:783–92. doi: 10.1111/j.1469-8749.2011.03980.x. [DOI] [PubMed] [Google Scholar]
- 33.Stein SM, Chowdhury U. London: Jessica Kingsley Publishers; 2006. Disorganized children: a guide for parents and professionals. [Google Scholar]
- 34.Guest G, Bunce A, Johnson L. How Many Interviews Are Enough? Field Methods. 2006;18:59–82. [Google Scholar]


