Abstract
Aim
Outcomes for pediatric out-of-hospital cardiac arrest (OHCA) are poor. Our objective was to determine temporal trends in incidence and mortality for pediatric OHCA.
Methods
Adjusted incidence and hospital mortality rates of pediatric non-traumatic OHCA patients from 2007-2012 were analyzed using the 9 region Resuscitation Outcomes Consortium - Epidemiological Registry (ROC-Epistry) database. Children were divided into 4 age groups: perinatal (< 3 days), infants (3 days - 1 year), children (1 - 11 years), and adolescents (12 - 19 years). ROC regions were analyzed post-hoc.
Results
We studied 1,738 children with OHCA. The age- and sex-adjusted incidence rate of OHCA was 8.3 per 100,000 person-years (75.3 for infants vs. 3.7 for children and 6.3 for adolescents, per 100,000 person-years, p<0.001). Incidence rates differed by year (p<0.001) without overall linear trend. Annual survival rates ranged from 6.7-10.2%. Survival was highest in the perinatal (25%) and adolescent (17.3%) groups. Stratified by age group, survival rates over time were unchanged (all p>0.05) but there was a non-significant linear trend (1.3% increase) in infants. In the multivariable logistic regression analysis, infants, unwitnessed event, initial rhythm of asystole, and region were associated with worse survival, all p<0.001. Survival by region ranged from 2.6-14.7%. Regions with the highest survival had more cases of EMS-witnessed OHCA, bystander CPR, and increased EMS-defibrillation (all p<0.05).
Conclusions
Overall incidence and survival of children with OHCA in ROC regions did not significantly change over a recent 5 year period. Regional variation represents an opportunity for further study to improve outcomes.
Keywords: pediatric, cardiac arrest, resuscitation, outcomes, epidemiology
Introduction
While the incidence of pediatric out-of-hospital cardiac arrest (OHCA) is low (8 per 100,000 person-years), survival to hospital discharge is only 6%1. Poor outcomes after pediatric OHCA have been related to patient, event, resuscitation, and post-resuscitation care factors. These include a high frequency of unwitnessed arrests, asphyxial events, unfavorable presenting rhythms, long duration of pulselessness, and lack of effective post-resuscitation care therapies2-5.
Multiple efforts have led to improved pediatric in-hospital cardiac arrest (IHCA) survival (14% to 43% over a 10-year study period) without an increase in the frequency of severe disability among survivors6,7. Data from the Resuscitation Outcomes Consortium (ROC) has also shown increased survival over time for adult OHCA victims but regional variation exists8,9. Data from Australia/New Zealand and Denmark have not demonstrated improvements in survival after pediatric OHCA but recent data from Sweden in children aged 0-21 years showed that 30-day survival increased from 6% in 1992–1998 to 14% in 2007–201210,11.
Little is known about regional trends in the incidence and outcomes after pediatric OHCA in North America. The purpose of this study was to determine temporal trends in incidence and mortality for pediatric OHCA using the prospective ROC Epidemiological Registry (ROC-Epistry) database. We hypothesized that the incidence and survival to hospital discharge following pediatric OHCA have improved over time.
Methods
Design and setting
This is a prospective cohort of consecutive pediatric OHCA cases. The ROC is a collaboration of 10 regional sites in the United States and Canada managed through a single Data Coordinating Center. Formed in 2004, the ROC's primary goal is to conduct out-of-hospital randomized controlled trials in patients with life threatening trauma and cardiac arrest. The regional sites consist of the participating Emergency Medical Support (EMS) agencies and receiving hospitals serving a combined population of approximately 24 million individuals12.
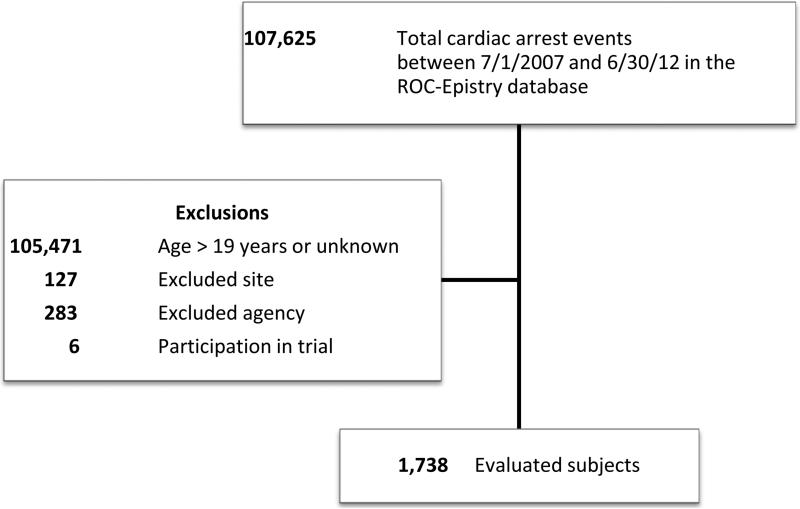
The primary data source for this analysis was the ROC-Epistry database13. This prospective observational population based registry collects data on all OHCA cases responded to by participating EMS agencies. The present study included 9 regions (3 Canadian and 6 American) that continuously participated in ROC-Epistry during a five-year period between July 1, 2007 and June 30, 2012. We excluded one region and the initial registry start-up years (2005-2006) because of incomplete case capture. Because EMS agency participation varied over the period, only cases in which the first responding agency participated in the registry for the full 5 year study period were included for internal consistency.
Study population
Subjects included children ages 0-19 years of age and excluded children with traumatic causes of cardiac arrest and those participating in ongoing clinical trials (age 18 years and older). Treated cases were defined as children who received EMS treatment, including cardiopulmonary resuscitation (CPR) or defibrillation at any time. Non-treated cases were those children who did not receive EMS treatment, presumably due to do-not-resuscitate status or obvious signs of death such as rigor mortis or dependent livid appearance. We divided subjects a priori into 4 age groups: perinatal (less than 3 days), infants (4 days up to 1 year), children (1 to 11 years), and adolescents (12 to 19 years)1. This observational study met the requirements for waiver of informed consent for minimal risk research in the United States and Canada, and was approved by 74 Institutional Review boards and 34 Research Ethics boards1.
Data collection, management, quality and outcome measures
Data from EMS records were transferred to ROC data collection forms by trained research coordinators. Details of ROC data management and quality assurance have been reported previously9. Clinical variables included patient demographics, Advanced and Basic Life Support team response, median time to EMS response; cardiac arrest and resuscitation interventions, and outcomes which included return of spontaneous circulation (ROSC) and survival to hospital discharge. We did not analyze functional outcome, etiology of arrest, and race/ethnicity, because information about these variables was incomplete or not available.
The primary outcomes were trends in incidence of pediatric OHCA and survival to hospital discharge over the study period controlling for year, age, sex, and region. The secondary outcomes were incidence and survival by region and variables associated with survival. Regions were defined by the 9 ROC geographic regions, each comprised of participating EMS agencies within the region13.
Statistical analysis
We examined subject characteristics, cardiac arrest event and treatment factors, treatment status, EMS response characteristics, as well as outcomes by age group, region, and year using descriptive statistics. Complete variables were available only for EMS-treated cardiac arrest episodes and not for non-treated cases.
To calculate incidence rates, we first identified catchment areas by determining the location of all cardiac arrests by census tract, as defined according to the United States 2010 or the 2011 Canada census. We converted locations recorded using the geographical coordinate systems of Universal Transverse Mercator (UTM) or latitude and longitude to the corresponding census tract. Cases entered with a census tract designation from previous versions of the censuses were updated to the most recent tract designation using conversion tables provided by the census bureaus. With the collection of identified tracts, we defined the catchment area of a region to include all tracts with two or more cases or an adjacent tract with one case. We used the reported pediatric population in a specific catchment area from the 2010/2011 censuses as the denominator for our incidence calculations. The numerator was the number of pediatric cases occurring in the area. We reported incidence rates for three age groups: perinatal/infants, children, and adolescents, where the first two age groups were combined to match available census age group data. Canadian episodes that occurred outside of a census tract were not included in our incidence calculations. When reporting incidence rates we standardized to a population that had a uniform distribution of age and gender.
We tested for difference in incidence rates by age group, year, and region using a chi-squared test with 0.05 as the criterion for significance. We estimated linear differences in incidence rates using linear regression with Wald tests. We evaluated differences in survival to hospital discharge in treated cardiac arrest subjects using adjusted logistic regression models and the likelihood ratio test to jointly test factorized forms of age group, year period (from July to June), and region. We a priori selected covariates to include in the multiple regression models, as listed in the table footnotes. Statistical analyses were performed in SAS, version 9.3 and R, version 2.15.2, with the packages Maps, Maptools and US Census2010.
Results
Patient and system characteristics
We studied 1,738 children with OHCA in 9 regions in the US and Canada with an estimated total pediatric population of 4,178,251 (Table 1). Of these cases, 1,429 (82%) received EMS treatment. Perinatal (98%) cases had the highest frequency of treatment by EMS compared to infants (85%), children (86%), and adolescents (74%).
Table 1.
OHCA incidence, event characteristics, and interventions by age groups.
| Perinatal | Infants | Children | Adolescents | All | |
|---|---|---|---|---|---|
| All cardiac arrests, n | 60 | 720 | 410 | 548 | 1,738 |
| Male, n (%*) | 25 (42.4) | 387 (58.3) | 223 (58.5) | 301 (64.9) | 936 (59.7) |
| Incidence** | 75.3 | 3.7 | 6.3 | 8.3 | |
| Population | 206,692 | 2,235,577 | 1,735,982 | 4,178,251 | |
| EMS-treated cardiac arrests, n | 59 | 615 | 352 | 403 | 1,429 |
| Male, n (%*) | 25 (42.4) | 362 (59.1) | 207 (58.8) | 266 (66.0) | 860 (60.3) |
| Location | |||||
| Home, n (%*) | 53 (89.8) | 579 (94.3) | 298 (84.9) | 302 (75.1) | 1,232 (86.4) |
| Other private location, n (%*) | 1 (1.7) | 18 (2.9) | 6 (1.7) | 20 (5.0) | 45 (3.2) |
| Public location, n (%*) | 5 (8.5) | 17 (2.8) | 47 (13.4) | 80 (19.9) | 149 (10.4) |
| Unknown, n (%) | 0 (0.0) | 1 (0.2) | 1 (0.3) | 1 (0.2) | 3 (0.2) |
| Initial rhythm | |||||
| VT/VF, n (%) | 1 (1.7) | 8 (1.3) | 16 (4.5) | 78 (19.4) | 103 (7.2) |
| PEA, n (%) | 7 (11.9) | 73 (11.9) | 61 (17.3) | 63 (15.6) | 204 (14.3) |
| Asystole, n (%) | 13 (22.0) | 451 (73.3) | 223 (63.4) | 219 (54.3) | 906 (63.4) |
| Other/unknown, n (%) | 38 (64.4) | 83 (13.5) | 52 (14.8) | 43 (10.7) | 216 (15.1) |
| Witnessed status, n (%) | 41 (69.5) | 90 (14.6) | 133 (37.8) | 163 (40.4) | 427 (29.9) |
| Bystander CPR, n (%) | 14 (23.7) | 304 (49.4) | 198 (56.3) | 201 (49.9) | 717 (50.2) |
| EMS interventions | |||||
| Airway | |||||
| Bag/mask, n (%) | 55 (93.2) | 577 (93.8) | 330 (93.8) | 384 (95.3) | 1,346 (94.2) |
| Intubation attempted, n (%) | 26 (44.1) | 362 (58.9) | 237 (67.3) | 275 (68.2) | 900 (63.0) |
| Supraglottic attempted, n (%) | 0 (0.0) | 5 (0.8) | 15 (4.3) | 62 (15.4) | 82 (5.7) |
| Resuscitation drug, n (%) | 9 (15.3) | 386 (62.8) | 243 (69.0) | 310 (76.9) | 948 (66.3) |
| Epinephrine | 9 (15.3) | 385 (62.6) | 239 (67.9) | 300 (74.4) | 933 (65.3) |
| Bicarbonate | 0 (0.0) | 63 (10.2) | 35 (9.9) | 84 (20.8) | 182 (12.7) |
| Atropine | 1 (1.7) | 98 (15.9) | 85 (24.1) | 208 (51.6) | 392 (27.4) |
| Calcium | 0 (0.0) | 8 (1.3) | 2 (0.3) | 12 (3.0) | 22 (1.5) |
| IV or IO attempts | 12 (20.3) | 460 (74.8) | 293 (83.2) | 351 (87.1) | 1,116 (78.1) |
| EMS defibrillation | 2 (3.4) | 18 (2.9) | 36 (10.2) | 108 (26.8) | 164 (11.5) |
| #shocks, mean (sd)*** | 1.5 (0.7) | 1.6 (0.9) | 2.1 (1.5) | 3.0 (2.9) | 2.6 (2.5) |
| Scene time (min), median | 14.8 | 16.0 | 19.5 | 24.0 | 19.7 |
| Interquartile range | 10.3, 24.0 | 9.5, 24.3 | 12.7, 26.0 | 17.7, 31.7 | 12.0, 27.5 |
| ROSC prior to hospital arrival, n (%) | 16 (26.7) | 47 (6.5) | 71 (17.3) | 148 (27.0) | 282 (16.2) |
| ROSC at ED arrival, n (%) | 16 (26.7) | 38 (5.3) | 58 (14.1) | 127 (23.2) | 239 (13.8) |
| Survival to hospital discharge, n (%) | 13 (24.5) | 23 (3.2) | 37 (9.3) | 69 (12.7) | 142 (8.3) |
| Transported to hospital with ongoing resuscitation, n (%) | 58 (98.3) | 467 (75.9) | 305 (86.6) | 311 (77.2) | 1,141 (79.8) |
| ROSC prior to hospital arrival, n (%) | 16 (27.1) | 47 (7.6) | 71 (20.2) | 148 (36.7) | 282 (19.7) |
| ROSC at ED arrival, n (%) | 16 (27.1) | 38 (6.2) | 58 (16.5) | 127 (31.5) | 239 (16.7) |
| Survival to hospital discharge, n (%*) | 13 (25.0) | 23 (3.8) | 37 (10.9) | 71 (17.3) | 142 (10.2) |
| Odds ratio for survival# (95% CI) | 1.4 (0.5, 4.1) | 0.4 (0.2, 0.8) | Referent | 1.0 (0.5, 1.8) | n/a |
Percent known
For 100,000 person-years, adjusted for sex; incidence rates by age group is statistically significant at p < 0.001 from a chi-squared test
For those administered one or greater shocks
EMS, emergency medical services; VT/VF, ventricular tachycardia/ventricular fibrillation; PEA, pulseless electrical activity; IV, intravenous; IO, intraosseous
Adjusted for covariates of: sex, advanced airway attempts, epinephrine, iv/io attempts, initial rhythm, witness status, region, and first arriving ALS EMS crew; survival by age group statistically significant at p = 0.02, likelihood ratio test
ROSC, return of spontaneous circulation; EMS, emergency medical services; ALS, advanced life support; ED, emergency department
Eighty-six percent of treated OHCA cases occurred at home, 70% were unwitnessed events, and 50% received bystander CPR overall. Seventy-eight percent of children presented with asystole or pulseless electrical activity as the initial cardiac rhythm. In nearly all cases, an advanced life support (ALS) EMS crew was on the scene during resuscitation, with a basic life support (BLS) EMS crew arriving first in 56% of cases. Median (interquartile range [IQR]) response time of any EMS crew was 5.2 (4.0, 6.7) minutes and was < 8 minutes in 85% of cases. Among EMS-treated children, endotracheal intubation was attempted by EMS in 63% of cases, placement of intravenous (IV) or intraosseous (IO) vascular access catheter was attempted in 78% of cases, and bolus epinephrine was administered in 65% of cases.
Incidence over the study period
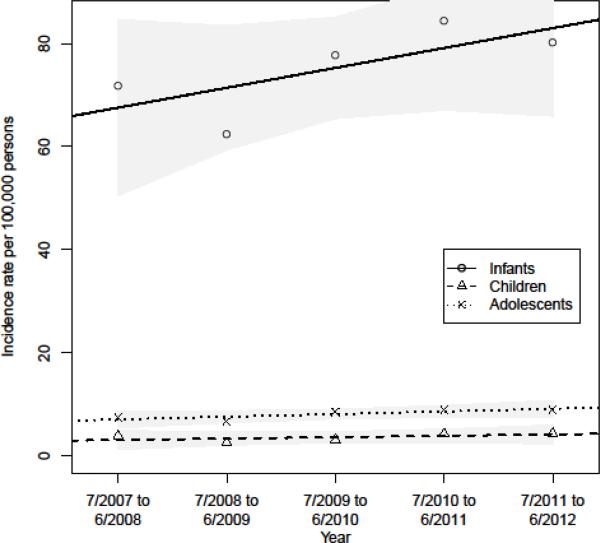
Age- and sex-adjusted incidence rate for all OHCA over the study period was 8.3 per 100,000 person-years. Infants under 1 year of age had the highest incidence compared to other age groups (infants 75.3 vs. children 3.7 and adolescents 6.3 per 100,000 person-years, p<0.001) (Table 1). Incidence rates differed by year (p<0.001) but there was no linear trend (point estimate of an average increase of 0.46 cases per year (95% CI: −0.06, 0.99)) (Table 2). Estimated annual linear difference by age group for incidence (per 100,000 person-years) over the study period were: infants 3.86 (95% CI: −3.12, 10.83), children 0.27 (95% CI: −0.49, 1.02), and adolescents 0.52 (95% CI: −0.16, 1.19) (Figure 2).
Table 2.
Incidence and outcomes by year.
| 7/2007 to 6/2008 | 7/2008 to 6/2009 | 7/2009 to6/2010 | 7/2010 to6/2011 | 7/2011 to 6/2012 | All | |
|---|---|---|---|---|---|---|
| All cardiac arrests, n | 339 | 280 | 348 | 388 | 383 | 1,738 |
| Perinatal, n (%) | 12 (3.5) | 8 (2.9) | 15 (4.3) | 12 (3.1) | 13 (3.4) | 60 (3.5) |
| Infants, n (%) | 137 (40.4) | 121 (43.2) | 146 (42.0) | 163 (42.0) | 153 (39.9) | 720 (41.4) |
| Children, n (%) | 87 (25.7) | 58 (20.7) | 70 (20.1) | 97 (25.0) | 98 (25.6) | 410 (23.6) |
| Adolescents, n (%) | 103 (30.4) | 93 (33.2) | 117 (33.6) | 116 (29.9) | 119 (31.1) | 548 (31.5) |
| Male, n (%*) | 176 (57.9) | 151 (58.1) | 208 (60.6) | 223 (60.4) | 178 (61.7) | 936 (59.7) |
| Incidence** | 8.1 | 6.7 | 8.3 | 9.3 | 9.1 | 8.3 |
| EMS treated, % | 83.5 | 84.6 | 82.5 | 85.3 | 76.0 | 82.2 |
| Survival to hospital discharge, n (%*) | 22 (6.7) | 23 (8.3) | 36 (10.2) | 30 (7.2) | 36 (9.3) | 142 (8.3) |
| EMS-treated cardiac arrests, n | 283 | 237 | 287 | 331 | 291 | 1,429 |
| Transported to hospital w/ ongoing resuscitation | 229 (80.9) | 186 (78.5) | 234 (81.5) | 259 (78.2) | 233 (80.1) | 1,141 (79.8) |
| ROSC prior to ED arrival | 46 (16.3) | 46 (19.4) | 66 (23.0) | 70 (21.1) | 54 (18.6) | 282 (19.7) |
| ROSC at hospital | 40 (14.1) | 40 (16.9) | 55 (19.2) | 55 (16.6) | 49 (16.8) | 239 (16.7) |
| Survival to hospital discharge, n (%*) | 22 (8.1) | 23 (9.8) | 35 (12.4) | 27 (8.5) | 35 (12.3) | 142 (10.2) |
| Odds ratio for survival***, (95% CI) | referent | 0.9 (0.4, 2.0) | 1.5 (0.7, 3.2) | 0.9 (0.4, 1.9) | 1.7 (0.7, 4.1) | n/a |
| Male, n (%*) | 168 (59.4) | 140 (59.3) | 176 (61.3) | 198 (60.0) | 178 (61.3) | 860 (60.3) |
| Location | ||||||
| Home, n (%*) | 248 (87.6) | 196 (82.7) | 247 (86.1) | 285 (86.4) | 256 (88.6) | 1232 (86.4) |
| Other private location, n (%*) | 10 (3.5) | 9 (3.8) | 5 (1.7) | 11 (3.3) | 10 (3.5) | 45 (3.2) |
| Public location, n (%*) | 25 (8.8) | 32 (13.5) | 35 (12.2) | 34 (10.3) | 23 (8.0) | 149 (10.4) |
| Unknown, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.3) | 2 (0.7) | 3 (0.2) |
| Initial Rhythm | ||||||
| VT/VF, n (%) | 19 (6.7) | 12 (5.1) | 24 (8.4) | 26 (7.9) | 22 (7.6) | 103 (7.2) |
| PEA, n (%) | 35 (12.4) | 35 (14.8) | 42 (14.6) | 51 (15.4) | 41 (14.1) | 204 (14.3) |
| Asystole, n (%) | 184 (65.0) | 142 (59.9) | 172 (59.9) | 215 (65.0) | 193 (66.3) | 906 (63.4) |
| Other/unknown, n (%) | 45 (15.9) | 48 (20.3) | 49 (17.1) | 39 (11.8) | 35 (12.0) | 216 (15.1) |
| Witnessed Status, n (%) | 79 (27.9) | 61 (25.7) | 86 (30.0) | 116 (35.0) | 85 (29.2) | 427 (29.9) |
| Bystander CPR, n (%) | 147 (51.9) | 111 (46.8) | 143 (49.8) | 166 (50.2) | 150 (51.5) | 717 (50.2) |
| EMS interventions | ||||||
| Airway | ||||||
| Bag/mask, n (%) | 259 (91.5) | 222 (93.7) | 277 (96.5) | 309 (93.4) | 279 (95.9) | 1346 (94.2) |
| Intubation attempted, n (%) | 201 (71.0) | 161 (67.9) | 178 (62.0) | 200 (60.4) | 160 (55.0) | 900 (63.0) |
| Supraglottic attempted, n (%) | 11 (3.9) | 16 (6.8) | 20 (7.0) | 17 (5.1) | 18 (6.2) | 82 (5.7) |
| Resuscitation drug therapy, n (%) | 185 (65.4) | 157 (66.2) | 196 (68.3) | 221 (66.8) | 189 (64.9) | 948 (66.3) |
| Epinephrine | 179 (63.3) | 155 (65.4) | 191 (66.6) | 220 (66.5) | 188 (64.6) | 933 (65.3) |
| Bicarbonate | 36 (12.7) | 34 (14.3) | 41 (14.3) | 36 (10.9) | 35 (12.0) | 182 (12.7) |
| Atropine | 97 (34.3) | 79 (33.3) | 82 (28.6) | 96 (29.0) | 38 (13.1) | 392 (27.4) |
| Calcium | 5 (1.8) | 8 (3.4) | 6 (2.1) | 3 (0.9) | 0 (0.0) | 22 (1.5) |
| IV or IO attempts | 220 (77.7) | 180 (75.9) | 224 (78.0) | 261 (78.9) | 231 (79.4) | 1116 (78.1) |
| EMS defibrillation | 38 (13.4) | 25 (10.5) | 40 (13.9) | 37 (11.2) | 24 (8.2) | 164 (11.5) |
| Number shocks, mean (sd)# | 2.5 (2.5) | 2.4 (1.5) | 2.3 (2.3) | 2.8 (2.2) | 3.3 (3.9) | 2.6 (2.5) |
Percent known
For 100,000 person-years, adjusted for sex and age group; incidence rates by year significant at p < 0.001, chi-squared test, but no linear trend identified
Adjusted for covariates of: sex, 911 to EMS arrival, age group, initial rhythm, witness status, region, first arriving ALS EMS crew, bystander witness, and advanced airway attempts; survival rates by year not statistically significant at p=0.24, likelihood ratio test
EMS, emergency medical services; ROSC, return of spontaneous circulation, ALS, advanced life support
For those administered one or greater shocks
Figure 2.
Incidence Rates by Year and Age Group with Estimated Linear Differences. Shaded areas represent 95% confidence intervals.
ROSC and survival to hospital discharge over the study period
Of treated cases, 19.7% of children had ROSC prior to emergency department (ED) arrival (range 7.6% for infants to 36.7% for adolescents) (Table 1). ROSC in ED had similar or slightly lower rates than ROSC prior to ED arrival by age group and was 16.7% overall.
Survival to hospital discharge in treated cardiac arrest was 10.2% overall, highest in the perinatal (25%) and adolescent (17.3%) groups. Age, as a categorical variable, was associated with survival after adjusting for covariates (p=0.02) (Table 1). Pairwise comparisons indicated higher survival in perinatal and child age groups compared to the infant age group (OR 3.66, 95% CI: 1.20, 11.21 and OR 2.60, 95% CI: 1.26, 5.37, respectively for survival). The adolescent age group had increased survival versus the infant age group (OR 2.50, 95% CI: 1.25, 4.96).
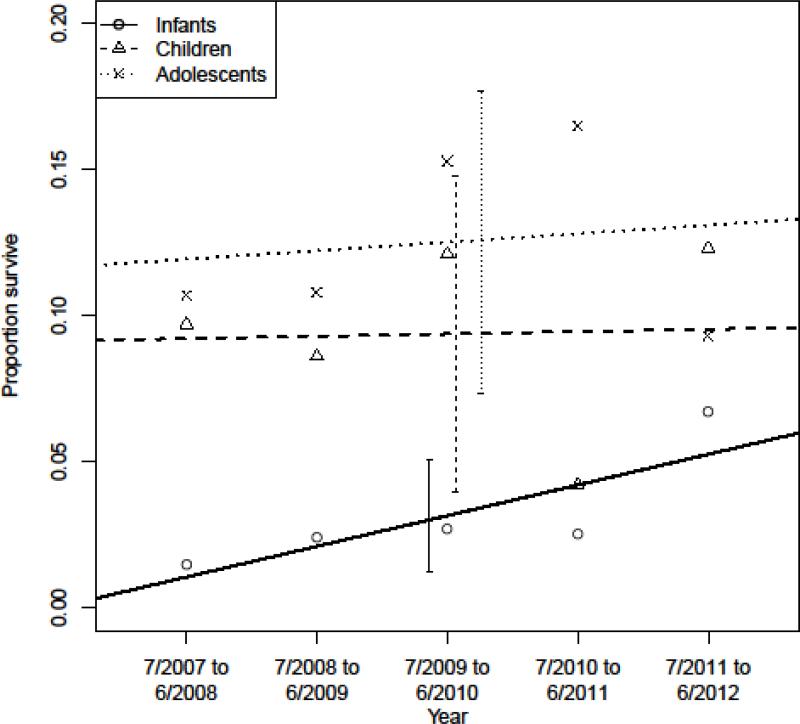
Survival rates did not vary by year during the study period in an adjusted analysis with year as a continuous or ordered variable. Within stratified analyses by age group, survival rates over time did not differ (all p>0.05). There was a positive non-significant linear trend of a 1.3% increase in survival in infants over the study period (Figure 3). In the multivariable logistic regression analysis, infant age group, unwitnessed event, initial rhythm of asystole, and region were associated with lower survival, p<0.001 (Table 3).
Figure 3.
Survival to Hospital Discharge for Cardiac Arrest by Year and Age Group with Estimated Linear Differences. Vertical bars represent standard error.
Table 3.
Multivariable regression for survival to hospital discharge.
| Variable | Odds Ratio (95% CI) | P-value |
|---|---|---|
| Year of OHCA (integer) | 1.11 (0.91, 1.33) | 0.29 |
| Age group | 0.25 | |
| Perinatal | 1.51 (0.50, 4.54) | 0.46 |
| Infant | 0.35 (0.17, 0.72) | 0.005 |
| Child | Referent | |
| Adolescent | 0.74 (0.38, 1.42) | 0.36 |
| Male | 0.73 (0.44, 1.21) | 0.22 |
| Witnessed | 3.92 (2.31, 6.65) | <0.001 |
| Bystander CPR | 1.33 (0.80, 2.19) | 0.12 |
| EMS arrival <8 minutes | 0.76 (0.35, 1.66) | 0.50 |
| ALS first on-scene | 0.83 (0.41, 1.69) | 0.61 |
| Advanced airway attempted | 0.64 (0.37, 1.13) | 0.12 |
| Initial rhythm | <0.001 | |
| VF/VT | 32.48 (14.86, 71.00) | <0.001 |
| PEA | 5.21 (2.53, 10.72) | <0.001 |
| Asystole | Referent | <0.001 |
| Other/unknown | 7.76 (3.80, 15.87) | <0.001 |
| Region | <0.001 | |
| 1 | 0.26 (0.04, 1.84) | 0.17 |
| 2 | Referent | |
| 3 | 0.51 (0.14, 1.83) | 0.30 |
| 4 | 1.08 (0.42, 2.77) | 0.87 |
| 5 | 5.37 (1.64, 17.61) | 0.01 |
| 6 | 1.12 (0.35, 3.55) | 0.85 |
| 7 | 2.08 (0.70, 6.13) | 0.19 |
| 8 | 0.50 (0.18, 1.40) | 0.19 |
| 9 | 1.90 (0.64, 5.61) | 0.24 |
Post-hoc analysis
Regional incidence
The incidence rates of pediatric OHCA differed between ROC regions (5.8-12.7 per 100,000 person-years, p<0.001) (Table 4). Comparing the regions, the median annual linear change in annual incidence was 0.31 with a range of −0.37 to 2.05.
Table 4.
Incidence, treatment characteristics, and outcome by region.
| Region | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| All cardiac arrests | |||||||||
| Incidence* | 12.5 | 12.7 | 9.7 | 6.9 | 12.0 | 8.1 | 9.6 | 5.8 | 6.2 |
| Perinatal, % | 0.9 | 2.2 | 3.0 | 2.9 | 0.0 | 1.4 | 2.7 | 7.8 | 4.7 |
| Infants, % | 49.1 | 47.2 | 51.5 | 25.8 | 59.7 | 42.8 | 50.2 | 32.7 | 32.6 |
| Children, % | 24.1 | 28.9 | 14.9 | 23.9 | 17.9 | 23.2 | 18.4 | 27.8 | 20.5 |
| Adolescents, % | 25.9 | 21.7 | 30.6 | 47.4 | 22.4 | 32.6 | 28.7 | 31.7 | 42.1 |
| ALS on scene, % | 99.1 | 100.0 | 95.5 | 88.0 | 98.5 | 100.0 | 91.5 | 92.9 | 77.9 |
| EMS response, min | |||||||||
| Median | 5.2 | 4.4 | 4.0 | 5.3 | 5.2 | 5.2 | 5.0 | 5.8 | 6.7 |
| <8 minutes, % | 81.5 | 86.9 | 94.0 | 78.5 | 83.6 | 91.3 | 91.0 | 88.7 | 68.9 |
| EMS treated, % | 74.1 | 71.9 | 88.1 | 81.3 | 92.5 | 77.5 | 86.5 | 91.6 | 82.6 |
| Survival to discharge, %** | 1.9 | 5.7 | 3.7 | 8.3 | 11.9 | 9.6 | 12.6 | 8.9 | 12.2 |
| EMS-treated cardiac arrests | |||||||||
| Bystander CPR, %* | 47.5 | 41.7 | 26.3 | 54.7 | 53.2 | 66.4 | 69.4 | 45.2 | 51.6 |
| Witnessed, % | 30.0 | 24.7 | 27.1 | 30.6 | 21.0 | 32.7 | 28.5 | 37.1 | 29.9 |
| Initial rhythm, % | |||||||||
| VT/VF | 3.8 | 3.9 | 5.1 | 6.5 | 3.2 | 11.2 | 7.8 | 11.0 | 8.3 |
| PEA | 6.3 | 13.9 | 12.7 | 11.8 | 3.2 | 9.3 | 17.6 | 19.1 | 17.8 |
| Asystole | 76.3 | 64.1 | 74.6 | 67.1 | 79.0 | 73.8 | 64.2 | 48.8 | 55.4 |
| Other/Unknown | 13.8 | 18.1 | 7.6 | 14.7 | 14.5 | 5.6 | 10.4 | 21.2 | 18.5 |
| EMS interventions | |||||||||
| Airway | |||||||||
| Bag/valve mask, % | 80.0 | 92.3 | 88.1 | 99.4 | 96.8 | 90.7 | 98.4 | 96.5 | 95.5 |
| Intubation attempt, % | 56.3 | 34.7 | 62.7 | 65.3 | 45.2 | 74.8 | 81.9 | 70.7 | 70.7 |
| SGA attempt,% | 1.3 | 12.4 | 11.0 | 7.1 | 14.5 | 7.5 | 0.0 | 0.4 | 3.8 |
| Resuscitation drug, % | 32.5 | 69.5 | 90.7 | 62.9 | 61.3 | 72.9 | 76.7 | 60.1 | 59.9 |
| Epinephrine, % | 32.5 | 69.1 | 88.1 | 62.9 | 61.3 | 68.2 | 74.6 | 60.1 | 58.6 |
| Bicarbonate, % | 3.8 | 5.8 | 13.6 | 2.4 | 14.5 | 6.5 | 53.4 | 1.1 | 14.0 |
| Atropine, % | 23.8 | 24.3 | 33.9 | 24.7 | 33.9 | 43.0 | 34.2 | 19.4 | 25.5 |
| IV/IO attempts, % | 63.8 | 82.6 | 94.1 | 79.4 | 74.2 | 80.4 | 83.9 | 72.1 | 68.2 |
| EMS defibrillation, % | 6.3 | 6.6 | 5.9 | 8.8 | 8.1 | 16.8 | 13.5 | 17.3 | 14.0 |
| Shocks, mean*** | 0.8 | 1.1 | 1.8 | 1.2 | 1.4 | 2.0 | 4.1 | 2.7 | 2.8 |
| Scene time (min), median | 9.0 | 13.9 | 30.0 | 18.1 | 12.7 | 17.2 | 27.4 | 18.2 | 23.6 |
| Interquartile range | 6.7, 13.9 | 9.7, 18.8 | 25.0, 35.0 | 10.7, 24.1 | 7.7, 22.3 | 12.0, 23.0 | 20.1, 37.3 | 13.0, 25.2 | 13.5, 33.2 |
| Outcomes Transported to hosp., % | 92.5 | 99.2 | 40.7 | 91.2 | 88.7 | 74.8 | 46.6 | 93.6 | 74.5 |
| ROSC before ED, % | 2.5 | 12.0 | 23.7 | 20.0 | 11.3 | 21.5 | 34.7 | 16.3 | 28.0 |
| ROSC at ED arrival, % | 2.5 | 8.9 | 19.5 | 17.6 | 9.7 | 18.7 | 32.1 | 12.7 | 23.6 |
| Survival to discharge % | 2.6 | 8.0 | 4.2 | 10.2 | 12.9 | 12.5 | 14.7 | 9.8 | 14.7 |
| Odds ratio**** | 0.3 | referent | 0.5 | 1.0 | 5.3 | 1.1 | 1.6 | 0.5 | 1.7 |
| Confidence interval | 0.0, 1.8 | referent | 0.1, 1.8 | 0.4, 2.6 | 1.6, 17.6 | 0.3, 3.4 | 0.6, 4.9 | 0.2, 1.3 | 0.6, 5.2 |
For 100,000 person-years, adjusted for sex and age group; incidence rates by year significantly significant at p < 0.001, chi-squared test
Percent known
For those administered one or greater shocks
Adjusted for covariates of: 911 to EMS arrival time, bystander CPR, witness status, sex, initial rhythm, age group, and ALS EMS crew arrival before BLS.
Outcomes by region statistically significant at p < 0.001, likelihood ratio test with multivariate regression.
EMS, emergency medical services; ALS, advanced life support; SGA, supraglottic airway; CPR, cardiopulmonary resuscitation; IV, intravenous; IO, intraosseous; ROSC, return of spontaneous circulation
Regional survival to hospital discharge
EMS treated cases in ROC regions ranged from 71.9% to 92.5%. ROSC rates prior to and after hospital arrival varied by region, ranging between 2.5% to 34.7% and 2.5% to 32.1%, respectively. Survival to hospital discharge among EMS-treated cases differed between regions, ranging from 2.6%-14.7% (10.2% [8.0, 12.9]) (Table 4).
To examine region level variation in more detail, patient, event, and scene characteristics for each region in each year were analyzed (data not shown). At the region level, age, proportion treated, patient sex, and arrival time were consistent over time. Regions with the greatest increases in survival over time exhibited increases in EMS-witnessed OHCA, increased frequency of bystander CPR, and increased EMS-defibrillation compared to regions that did not see increases in survival over time. Regions that demonstrated decreased or fluctuating survival over time reported a lower proportion of ventricular tachyarrhythmia cases over time.
Discussion
The key findings of this study were as follows: 1) Incidence and survival rates of pediatric OHCA did not statistically change over the study period; and 2) Incidence and survival rates of pediatric OHCA varied across ROC regions.
The incidence of pediatric OHCA is largely driven by the high rate in infants, which, similar to Atkins et al, was ten-fold higher than the rate in older children and adolescents, stressing the increased vulnerability of this developmental period1. Moreover, the OHCA incidence rate in infants was greater than that previously reported in adults (18+ years of age) (52 per 100,000 persons)9. Prior studies show that in the infant age group, OHCA is caused most frequently by sudden infant death syndrome (SIDS)1,2. Despite sleeping hygiene being recognized as an important contributing factor in the occurrence of SIDS, guidelines are infrequently practiced14,15.
Survival rates in our study were similar to those previously reported in North America2,16. Tijssen et al recently reported trends in improvement in survival rates in adolescents, and although these data were also from the ROC registry, they did not control for the changing mixture of agencies in ROC over time, as in this study17. Recent longitudinal data from Australia/New Zealand and Japan failed to show improvement in pediatric OHCA survival over 10 and 5 years duration, respectively18,19. In Kitamura, et al, reported that the incidence of OHCA due to non-cardiac etiology decreased slightly in children 1-4 years of age18. They also found that 1 month survival with favorable neurological outcome did not improve over time for children with bystander or witnessed OHCA of either cardiac or non-cardiac etiology. Straney, et al, reported trends of fewer SIDS cases but more drownings resulting in OHCA in Australia/New Zealand19. As noted, race/ethnicity or etiology of OHCA were not consistently available for analysis, but these types of data could be helpful to direct public health advocacy initiatives to prevent OHCA in children. Time to first epinephrine dose, a primary component of pediatric advanced life support, was associated with survival in a study of pediatric IHCA20,21. Interestingly, only 65% of children were given epinephrine by EMS in this study. Some possible explanations for this finding include brief transport times combined with a lack of IV/IO access and the fact that most pediatric OHCA are due to asphyxia, with airway and breathing interventions alone leading to ROSC.
The lack of improved survival in this study contrasts with increased survival (8.2 to 10.4%) in an adult OHCA study utilizing the ROC registry over a similar time period8. Survival increased most among adults with ventricular tachyarrhythmia as the presenting rhythm and those who received bystander CPR. In contrast with adults, children have more events with asystole as the presenting rhythm (ventricular etiology was 7% in this study), asphyxial etiology, and unwitnessed status2. While bystander CPR was not associated with survival in our study, in Japan, bystander CPR for witnessed pediatric OHCA events plus automated external defibrillator use were associated with improved survival outcomes22. The Swedish registry study demonstrating an impressive doubling of survival (including children < 1 year of age) over the course of 20 years in pediatric OHCA, but reasons for this improvement were not analyzed23.
In a revelatory study of adult OHCA, Nichol et al found striking regional variation among 10 ROC sites, with incidences ranging from 72-159 per 100,000 and survival to hospital discharge ranging from 3-16% among regions9. They postulated that differences in the region's population risk of OHCA and factors associated with EMS and post-resuscitation care likely contributed to these findings9. More recently, Girotra et al found that bystander CPR and automated external defibrillator (AED) use accounted for 40% of the survival variation in adult OHCA, in which survival rates by U.S. county ranged from 3.4-22.0%24. In an exploratory analysis, we found variations in the regional incidence (2 fold) and regional survival (5.6 fold) of pediatric OHCA patients. Reasons for these differences are not clear but some postulates can be submitted. For example, better performing regions had less infant and nonventricular arrhythmia-induced OHCA and more EMS-witnessed or AED treatable events1. In addition, sites with the highest treatment rates tended to have higher survival rates. Reasons for non-treatment were not available and there are likely to be differences in regional EMS protocols on this issue25,26. Similarly, higher ROSC rates before or at the ED also aligned with better survival. On visual inspection, provision of epinephrine and advanced airway and intravenous or intraosseous attempt do not align with survival20. Finally, post-resuscitation in-hospital care and course were not accounted for in this study and could impact outcomes3,4. Others have also reported regional differences after pediatric OHCA. In a publication from Japan, smaller (1.4-3.5% over four years) regional variation in 1 month survival with favorable neurological outcome was seen in pediatric OHCA27. Notably, OHCA incidence rates in our study were higher than that reported in children in Denmark (8.3 vs. 3.3 per 100,000 persons) while survival was slightly better (10.2% vs. 8.1% for all children treated or not)10. In pediatric IHCA, significant hospital variation in adjusted survival (29-48%) was found among 30 hospitals studied in the Get With The Guidelines (GWTG)28.
This disappointing lack of improvement in outcomes speaks to the need to continue to rigorously track pediatric OHCA events and should prompt vigorous, renewed focus on strategies to improve outcomes for children with OHCA1. For children, consideration should be given to modifying the chain of survival to stress preventative measures for respiratory and cardiac arrest events, educational efforts for faster recognition and highest quality treatment performance of the deteriorating child by bystander and first responders, discovery of effective therapeutic interventions, and rehabilitative strategies21,29.
Finally, achieving ROSC prior to reaching the emergency department is consistently associated with better survival16. Infants, the group with the highest incidence and worst survival rates, were also the age group least likely to have had a witnessed event and/or ROSC by hospital arrival, representing a special cohort for focused study and advocacy. Regional variability in ROSC rates appear to account for a significant portion of differences in ROSC and survival rates. Therefore, another strategy towards improving outcome is to perform an in-depth regional analysis of key singular or systematic elements leading to better outcomes.
Limitations
This study lacked statistical power to prove trends in incidence and survival over time. We were not able to report etiology of OHCA, airway success rates, and major social determinants of health which are important variables that may be associated with mortality10,30. Only short term survival outcomes were available; longer term and functional outcomes were not collected. The study was limited to data collected from sites with consistent and high quality reporting across as many years as possible. We are unable to adjust for changes in post-resuscitation care processes, especially in hospital care, that may have occurred over time as these variables were not captured consistently over time in ROC-Epistry. As with any registry-level data, there is the possibility for residual confounding since traditional Utstein factors thought to predict survival accounted incompletely for variation in survival between ROC sites31. Finally, EMS agencies reporting to the ROC-Epistry may not be representative of all North American communities therefore these findings may or may not be completely generalizable.
Conclusion
The overall incidence and survival of children with OHCA in regions of North America participating in the ROC registry has remained unchanged over a recent 5 year period. Finding explanations for the regional variation in incidence and survival differences holds promise for breakthroughs that lead to improved outcomes.
Figure 1.
CONSORT Diagram.
Acknowledgements
We wish to acknowledge and thank all of the participating EMS personnel, agencies and medical directors, as well as the hospitals that collected and contributed data for this project.
Funding/Support: The study was supported through research grants from: The ROC is supported by a series of cooperative agreements to nine regional clinical centers and one Data Coordinating Center (5U01 HL077863-University of Washington Data Coordinating Center, HL077866-Medical College of Wisconsin, HL077867-University of Washington, HL077871-University of Pittsburgh, HL077872-St. Michael's Hospital, HL077873-Oregon Health and Science University, HL077881-University of Alabama at Birmingham, HL077885-Ottawa Hospital Research Institute, HL077887-University of Texas SW Medical Ctr/Dallas, HL077908-University of California San Diego) from the National Heart, Lung and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke, U.S. Army Medical Research & Material Command, The Canadian Institutes of Health Research (CIHR) - Institute of Circulatory and Respiratory Health, Defence Research and Development Canada and the Heart, Stroke Foundation of Canada and the American Heart Association. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung and Blood Institute or the National Institutes of Health.
Dr. Fink reports funding from the Patient Centered Outcomes Research Institute and National Institutes of Health, neither of which had involvement in this research paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Disclosures
Role of the Funders/Sponsors: Monies received paid for support for a biostatistician and data collection. The funding sources had no input into the design and conduct of the study; management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; nor decision to submit the manuscript for publication.
References
- 1.Atkins DL, Everson-Stewart S, Sears GK, et al. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Circulation. 2009;119:1484–91. doi: 10.1161/CIRCULATIONAHA.108.802678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Young KD, Gausche-Hill M, McClung CD, Lewis RJ. A prospective, population-based study of the epidemiology and outcome of out-of-hospital pediatric cardiopulmonary arrest. Pediatrics. 2004;114:157–64. doi: 10.1542/peds.114.1.157. [DOI] [PubMed] [Google Scholar]
- 3.Topjian AA, French B, Sutton RM, et al. Early postresuscitation hypotension is associated with increased mortality following pediatric cardiac arrest. Crit Care Med. 2014;42:1518–23. doi: 10.1097/CCM.0000000000000216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Del Castillo J, Lopez-Herce J, Matamoros M, et al. Hyperoxia, hypocapnia and hypercapnia as outcome factors after cardiac arrest in children. Resuscitation. 2012;83:1456–61. doi: 10.1016/j.resuscitation.2012.07.019. [DOI] [PubMed] [Google Scholar]
- 5.Johnson MA, Grahan BJ, Haukoos JS, et al. Demographics, bystander CPR, and AED use in out-of-hospital pediatric arrests. Resuscitation. 2014;85:920–6. doi: 10.1016/j.resuscitation.2014.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Girotra S, Spertus JA, Li Y, Berg RA, Nadkarni VM, Chan PS. Survival trends in pediatric in-hospital cardiac arrests: an analysis from Get With the Guidelines-Resuscitation. Circulation Cardiovascular quality and outcomes. 2013;6:42–9. doi: 10.1161/CIRCOUTCOMES.112.967968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moler FW, Donaldson AE, Meert K, et al. Multicenter cohort study of out-of-hospital pediatric cardiac arrest. Crit Care Med. 2011;39:141–9. doi: 10.1097/CCM.0b013e3181fa3c17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daya MR, Schmicker RH, Zive DM, et al. Out-of-hospital cardiac arrest survival improving over time: Results from the Resuscitation Outcomes Consortium (ROC). Resuscitation. 2015;91:108–15. doi: 10.1016/j.resuscitation.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. Jama. 2008;300:1423–31. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rajan S, Wissenberg M, Folke F, et al. Out-of-hospital cardiac arrests in children and adolescents: incidences, outcomes, and household socioeconomic status. Resuscitation. 2015;88:12–9. doi: 10.1016/j.resuscitation.2014.11.025. [DOI] [PubMed] [Google Scholar]
- 11.Straney LD, Schlapbach LJ, Yong G, et al. Trends in PICU Admission and Survival Rates in Children in Australia and New Zealand Following Cardiac Arrest. Pediatr Crit Care Med. 2015;16:613–20. doi: 10.1097/PCC.0000000000000425. [DOI] [PubMed] [Google Scholar]
- 12.Davis DP, Garberson LA, Andrusiek DL, et al. A descriptive analysis of Emergency Medical Service Systems participating in the Resuscitation Outcomes Consortium (ROC) network. Prehosp Emerg Care. 2007;11:369–82. doi: 10.1080/10903120701537147. [DOI] [PubMed] [Google Scholar]
- 13.Morrison LJ, Nichol G, Rea TD, et al. Rationale, development and implementation of the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Resuscitation. 2008;78:161–9. doi: 10.1016/j.resuscitation.2008.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Colvin JD, Collie-Akers V, Schunn C, Moon RY. Sleep environment risks for younger and older infants. Pediatrics. 2014;134:e406–12. doi: 10.1542/peds.2014-0401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moon RY. SIDS and other sleep-related infant deaths: expansion of recommendations for a safe infant sleeping environment. Pediatrics. 2011;128:e1341–67. doi: 10.1542/peds.2011-2284. [DOI] [PubMed] [Google Scholar]
- 16.Pitetti R, Glustein JZ, Bhende MS. Prehospital care and outcome of pediatric out-of-hospital cardiac arrest. Prehosp Emerg Care. 2002;6:283–90. doi: 10.1080/10903120290938300. [DOI] [PubMed] [Google Scholar]
- 17.Tijssen JA, Prince DK, Morrison LJ, et al. Time on the scene and interventions are associated with improved survival in pediatric out-of-hospital cardiac arrest. Resuscitation. 2015;94:1–7. doi: 10.1016/j.resuscitation.2015.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kitamura T, Iwami T, Kawamura T, et al. Nationwide improvements in survival from out-of-hospital cardiac arrest in Japan. Circulation. 2012;126:2834–43. doi: 10.1161/CIRCULATIONAHA.112.109496. [DOI] [PubMed] [Google Scholar]
- 19.Straney LD, Schlapbach LJ, Yong G, et al. Trends in PICU Admission and Survival Rates in Children in Australia and New Zealand Following Cardiac Arrest. Pediatr Crit Care Med. 2015 doi: 10.1097/PCC.0000000000000425. [DOI] [PubMed] [Google Scholar]
- 20.Andersen LW, Berg KM, Saindon BZ, et al. Time to Epinephrine and Survival After Pediatric In-Hospital Cardiac Arrest. JAMA. 2015;314:802–10. doi: 10.1001/jama.2015.9678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maconochie IK, de Caen AR, Aickin R, et al. Part 6: Pediatric basic life support and pediatric advanced life support: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation. 2015;95:e147–68. doi: 10.1016/j.resuscitation.2015.07.044. [DOI] [PubMed] [Google Scholar]
- 22.Akahane M, Tanabe S, Ogawa T, et al. Characteristics and outcomes of pediatric out-of-hospital cardiac arrest by scholastic age category. Pediatr Crit Care Med. 2013;14:130–6. doi: 10.1097/PCC.0b013e31827129b3. [DOI] [PubMed] [Google Scholar]
- 23.Gelberg J, Stromsoe A, Hollenberg J, et al. Improving Survival and Neurologic Function for Younger Age Groups After Out-of-Hospital Cardiac Arrest in Sweden: A 20-Year Comparison. Pediatr Crit Care Med. 2015;16:750–7. doi: 10.1097/PCC.0000000000000503. [DOI] [PubMed] [Google Scholar]
- 24.Girotra S, van Diepen S, Nallamothu BK, et al. Regional Variation in Out-of-Hospital Cardiac Arrest Survival in the United States. Circulation. 2016;133:2159–68. doi: 10.1161/CIRCULATIONAHA.115.018175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jaslow D, Barbera JA, Johnson E, Moore W. Termination of nontraumatic cardiac arrest resuscitative efforts in the field: a national survey. Acad Emerg Med. 1997;4:904–7. doi: 10.1111/j.1553-2712.1997.tb03817.x. [DOI] [PubMed] [Google Scholar]
- 26.Hall WL, 2nd, Myers JH, Pepe PE, Larkin GL, Sirbaugh PE, Persse DE. The perspective of paramedics about on-scene termination of resuscitation efforts for pediatric patients. Resuscitation. 2004;60:175–87. doi: 10.1016/j.resuscitation.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 27.Okamoto Y, Iwami T, Kitamura T, et al. Regional variation in survival following pediatric out-of-hospital cardiac arrest. Circulation journal : official journal of the Japanese Circulation Society. 2013;77:2596–603. doi: 10.1253/circj.cj-12-1604. [DOI] [PubMed] [Google Scholar]
- 28.Jayaram N, Spertus JA, Nadkarni V, et al. Hospital variation in survival after pediatric in-hospital cardiac arrest. Circulation Cardiovascular quality and outcomes. 2014;7:517–23. doi: 10.1161/CIRCOUTCOMES.113.000691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sutton RM, Case E, Brown SP, et al. A Quantitative Analysis of Out-of-Hospital Pediatric and Adolescent Resuscitation Quality-A Report from the ROC Epistry-Cardiac Arrest. Resuscitation. 2015 doi: 10.1016/j.resuscitation.2015.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Matos RI, Watson RS, Nadkarni VM, et al. Duration of cardiopulmonary resuscitation and illness category impact survival and neurologic outcomes for in-hospital pediatric cardiac arrests. Circulation. 2013;127:442–51. doi: 10.1161/CIRCULATIONAHA.112.125625. [DOI] [PubMed] [Google Scholar]
- 31.Rea TD, Cook AJ, Stiell IG, et al. Predicting survival after out-of-hospital cardiac arrest: role of the Utstein data elements. Ann Emerg Med. 2010;55:249–57. doi: 10.1016/j.annemergmed.2009.09.018. [DOI] [PubMed] [Google Scholar]