Abstract
Nonalcoholic steatohepatitis (NASH) is the main cause of chronic liver disease in the Western world and a major health problem, owing to its close association with obesity, diabetes, and the metabolic syndrome. NASH progression results from numerous events originating within the liver, as well as from signals derived from the adipose tissue and the gastrointestinal tract. In a fraction of NASH patients, disease may progress, eventually leading to advanced fibrosis, cirrhosis and hepatocellular carcinoma. Understanding the mechanisms leading to NASH and its evolution to cirrhosis is critical to identifying effective approaches for the treatment of this condition. In this review, we focus on some of the most recent data reported on the pathogenesis of NASH and its fibrogenic progression, highlighting potential targets for treatment or identification of biomarkers of disease progression.
Keywords: fibrosis, inflammation, chemokines, genetics, microbiota, pattern-recognition receptors, nuclear receptors, hepatic stellate cells, macrophages
1. Introduction
Nonalcoholic fatty liver disease (NAFLD) is an expanding health problem, which varies in prevalence among ethnic groups, occurring with an estimated global prevalence of 25% [1]. NAFLD associates with obesity, insulin resistance or type 2 diabetes and other metabolic abnormalities, such as dyslipidemia and hypertension, collectively termed metabolic syndrome. In high risk populations, the prevalence of NAFLD may be as high as 70%–90% [2,3]. NAFLD covers a spectrum of pathological abnormalities. Although most patients have simple steatosis, around 7%–30% develop nonalcoholic steatohepatitis (NASH), that in at least a third of cases progresses to advanced fibrosis or cirrhosis. The tendency to develop hepatic steatosis differs among ethnic groups, with African-Americans having a lower (24%) and Hispanics a higher (45%) frequency of the disease than Americans of European descent (33%). The causes for these ethnic differences in prevalence of hepatic steatosis and liver injury are not entirely understood.
NASH is characterized by hepatocellular damage, inflammation and fibrosis [4,5]. In general, simple steatosis is considered a less severe form of NAFLD, although recent data indicate a possible risk of progression [6,7]. In contrast, NASH is a significant risk factor for the development of cirrhosis and hepatocellular carcinoma [8,9,10]. Although NASH was first documented more than 30 years ago [11], its pathogenesis is still not fully elucidated. Initially, a two-hit hypothesis, based on appearance of steatosis (first hit), followed by a second hit leading to inflammation, hepatocyte damage, and fibrosis, was proposed by Day and James [12]. While accumulation of triglycerides is necessary for the development of NASH, they may actually have a protective role against hepatocytes lipotoxicity, which is mainly induced by fatty acids and derived metabolites such as diacylglycerols, acylcarnitines or ceramides [13,14]. In addition, it is still unclear whether NASH develops sequentially, on the grounds of a fatty liver, or it is rather a de novo response to a lipotoxic environment. The multiparallel hypothesis proposed more recently [15] suggests that NASH is the result of numerous conditions acting in parallel, including genetic predisposition, abnormal lipid metabolism, oxidative stress, lipotoxicity, mitochondrial dysfunction, altered production of cytokines and adipokines, gut dysbiosis and endoplasmic reticulum stress. According to this hypothesis, hepatic inflammation in NASH may even precede steatosis. As more contributing factors are continuously identified, a more complex picture of NASH pathogenesis is emerging [16] (Figure 1).
Figure 1.
Outline of the pathogenesis of NASH. Signals generated inside the liver as a consequence of increased lipid accumulation, together with signals derived from extrahepatic organs cooperate to induce inflammation and fibrosis. FFA, free fatty acids; PAMPs, pathogen-associated molecular patterns; ER, endoplasmic reticulum; ROS, reactive oxygen species; HSC, hepatic stellate cell.
2. Genetic Factors
The relevance of genetic factor in the context of NASH has been recently and elegantly outlined by twin studies [17]. A long list of genes potentially implicated in NAFLD appearance and progression has been reported, and these data have been the subject of a recent review [18].
A significant association with a SNP was identified in patatin-like phospholipase domain-containing 3 (PNPLA3) on chromosome 22. The variant (rs738409 c.444 C>G, p.I148M), a non-synonymous cytosine to guanine mutation resulting in isoleucine to methionine conversion, correlates with increased hepatic lipid content and predisposes to fatty liver-associated liver disease, from simple steatosis to steatohepatitis, fibrosis and hepatocellular carcinoma [19,20]. PNPLA3 encodes for a 481 amino acid protein, whose role has not been fully elucidated. It appears to function as acylglycerol hydrolase, acting on triacylglycerol, diacylglycerol, and monoacylglycerol [21,22]. Additional evidence indicates that PNPLA3 also acts as lysophosphatidic acid acetyltransferase [23,24]. Overexpression of the I148M variant in mouse liver promotes accumulation of triacylglycerol, increased synthesis of fatty acids and impaired hydrolysis of triacylglycerol [25]. Moreover, the PNPLA3 genotype has been reported to influence liver storage of retinol and retinol serum levels in obese subjects [26], suggesting a potential role of PNPLA3 in regulating retinol metabolism and hepatic stellate cell (HSC) biology [27]. Remarkably, PNPLA3 has been recently shown to be expressed in hepatic stellate cells [28]. Interestingly, the prevalence of the PNPLA3 I148M allele varies considerably among different ethnic groups, with the highest frequency in Hispanics (0.49), and lower frequencies in European Americans (0.23) and African-Americans (0.17) [20]. This is in agreement with the different prevalence of NAFLD in the three ethnic groups.
Carriage of a non-synonymous genetic variant in TM6SF2 (rs58542926 c.449 C>T, p.E167K) on chromosome 19 (19p13.11) has been reported to correlate with steatosis and increased risk of advanced fibrosis in NAFLD patients [29,30], independently of other factors, including diabetes, obesity, or PNPLA3 genotype. The minor allele frequency in one of the NAFLD populations tested was 0.12, compared to a frequency of 0.07 in a reference population. TM6SF2, is a transmembrane protein localized in endoplasmic reticulum (ER) and ER–Golgi compartments and functions as a lipid transporter [31]. The amino acid change E167K causes loss of function of TM6SF2 protein. Studies performed in cell lines showed that downregulation of TM6SF2 reduces lipoproteins and apolipoprotein B (APOB) levels, and increases hepatic deposition of triglycerides and the amount and size of lipid droplets. In contrast, the size and number of lipid droplets diminishes when TM6SF2 is overexpressed, indicating that TM6SF2 plays a role in regulating hepatic lipid efflux [29,31].
A broad spectrum of other genes has been associated with NAFLD. Polymorphism was reported in genes involved in carbohydrate and lipid metabolism, insulin-induced pathways, as well as inflammatory response, oxidative stress and fibrogenesis. A study by Dongiovanni et al. reported that non-synonymous SNPs in ectoenzyme nucleotide pyrophosphate phosphodiesterase 1 (ENPP1 or PC1) (rs1044498, K121Q) and insulin receptor substrate-1 (IRS1) (rs1801278, Q972R), are associated with insulin resistance, through impairment of insulin receptor-mediated pathways, such as reduced AKT activation, and promote fibrosis in NAFLD patients [32].
A functional non-synonymous variant (rs1260326, P446L) of glucokinase regulatory protein (GCKR) has also been associated with NAFLD [33]. This variant produces a GCKR with defective inhibitory function, leading to increased glucokinase activity and hepatic glucose uptake [34]. The resultant unimpeded hepatic glycolysis reduces glucose levels, inducing malonyl-CoA synthesis, a substrate for lipogenesis that causes liver fat deposition and impairs mitochondrial β-oxidation. A polymorphism in the solute carrier family 2 member 1 gene (SLC2A1), a glucose transporter, has been reported in NAFLD subjects. SLC2A1 downregulation in hepatocytes results in lipid accumulation and oxidative stress [35].
Several genes involved in oxidative stress have been investigated. Two reports correlated the C282Y variant in hemochromatosis gene (HFE) with NASH and higher susceptibility to more severe disease, as fibrosis or cirrhosis [36,37]. However, these findings have not been confirmed by other studies [38,39,40]. Very recently, the rs641738 genotype at the MBOAT7-TMC4 locus, encoding for the membrane bound O-acyltransferase domain-containing 7 was associated with more severe liver damage and increased risk of fibrosis in patients with NAFLD. This effect has been ascribed to changes in remodeling of the hepatic phosphatidylinositol acyl-chain [41].
3. Epigenetics
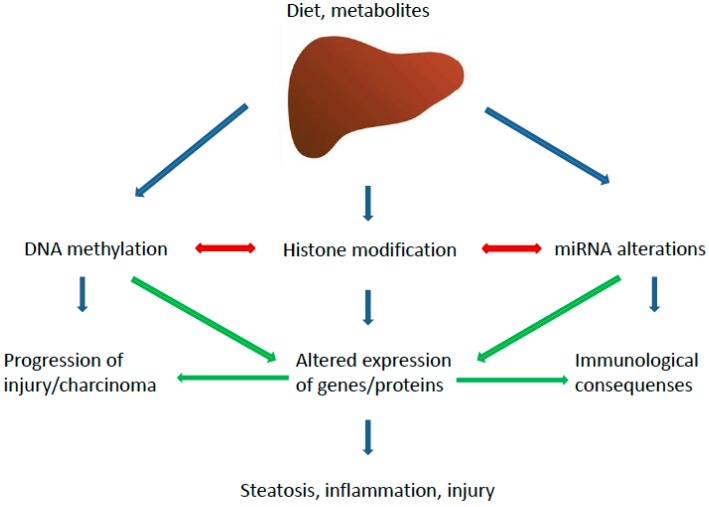
Epigenetic changes consist in modifications at the transcriptional level affecting gene expression and phenotype. A number of epigenetic aberrations have been associated with NAFLD pathogenesis, causing alterations in lipid metabolism, insulin resistance (IR), dysfunction of endoplasmic reticulum (ER) and mitochondria, oxidative stress and inflammation [42]. The different epigenetic pathways potentially involved in NAFLD are summarized in Figure 2.
Figure 2.
Epigenetic pathways implicated in the pathogenesis of NASH. The major pathways and their main effectors are depicted.
Aberrant DNA methylation is a major epigenetic process in NAFLD development and progression to NASH [43]. It occurs through methyltransferases (DNMTs) that catalyze the conversion of cytosine to 5-methylcytosine [44], leading to gene silencing. It has been reported that mice fed with a methyl-deficient diet show reduced levels of hepatic S-adenosylmethionine (SAM), associated with methylation of genes involved in DNA damage and repair, lipid and glucose metabolism and fibrosis progression [45]. In agreement, food-derived methyl donors, such as folate, betaine and choline, responsible for SAM synthesis, counteract DNA methylation [46] whereas folate deficiency correlates with enhanced fatty acid synthesis and hepatic accumulation of triglycerides (TG) via DNA methylation [47]. Methyl donor supplementation reverts liver lipid deposition induced by high fat/high sucrose-diet, lowering global hepatic DNA methylation and methylation levels of the promoter regions of different regulatory factors [48]. Betaine has been demonstrated to diminish the methylation levels of the promoter of microsomal triglyceride transfer protein (MTP), enhancing hepatic TG export and ameliorating liver steatosis in mice administered a high-fat diet (HFD) [43]. In addition, epigenetic changes of peroxisome proliferator-activated receptor gamma (PPARγ) in the liver of NAFLD patients seems to promote IR [49].
Although most epigenetic alterations are transient, DNA methylation can be inherited from parents [50]. It has been reported that maternal Western diet during prenatal time can increase the susceptibility to NAFLD of male progeny [51]. Novel evidence indicates that mitochondrial DNA (mtDNA) methylation may also play a role in NAFLD pathogenesis [52,53]. Liver methylation of NADH dehydrogenase 6 (MT-ND6) correlates with NAFLD severity, resulting in significantly lower expression of MT-ND6 mRNA in NASH than in patients with simple steatosis [54].
Histone acetylation, regulated by histone acetyltransferases (HATs) and histone deacetylases (HDACs), has been extensively associated with NAFLD [55,56]. High-fat maternal diet was shown to lead to depletion of fetal hepatic HDAC1, suggesting that diet-induced maternal obesity can alter fetal chromatin via histone modifications [55]. Carbohydrate-responsive element-binding protein (ChREBP), an activator of lipogenic and glycolytic pathways involved in NAFLD progression, is regulated by the HAT activator p300. Glucose-activated p300 induces ChREBP hyperacetylation, stimulating its transcriptional activity and hepatic lipogenesis in mice, and p300 overexpression is associated with steatosis and IR [56].
NAFLD has been also correlated with histone methylation. Lipid accumulation in the liver of HFD mice has been associated with H3K4 and H3K9 histone trimethylation of peroxisome proliferator-activated receptor alpha (PPARα) and lipolysis-related genes [57]. In addition, trans-generational changes in histone methylation promote lipogenesis and ER stress, acting on endoplasmic reticulum oxidoreductin 1α (ERO1α) and liver X receptor α (LXRα) [58].
Sirtuins (SIRTs) belong to the silent information regulator-2 family. SIRT1 deacetylation has been recognized as a regulatory mechanism for several proteins involved in NAFLD pathogenesis [59] and low SIRT1 expression has been observed in NAFLD models [60]. In addition, SIRT1-mediated regulation of fetal metabolome and epigenome has been reported under maternal HFD [61]. SIRT3 is localized in mitochondria and regulates fatty acid oxidation. SIRT3 knockout mice fed HFD develop hepatic steatosis and IR [62].
MicroRNAs (miRNAs) modulate gene expression via post-transcriptional mechanisms, regulating the main cellular processes, such as lipid metabolism, inflammation, apoptosis, cell growth and differentiation. In the last few years, aberrant miRNA expression has been reported in a number of diseases including metabolic disorders [63,64], whereas an increasing number of dysregulated miRNAs, implicated in fatty acid synthesis, uptake and storage of triglycerides or oxidation, have been recently identified in NAFLD [65] (Table 1). Among these, miR-122, which negatively regulates hepatic lipogenesis, is reduced in NASH patients [66] whereas miR-34a, that induces β-oxidation and inhibits synthesis of fatty acids via a sirtuin1/5′ adenosine monophosphate-activated protein kinase/3-hydroxy-3-methylglutaryl-CoA reductase (SIRT1-AMPK-HMGCR) mechanism, is upregulated in NAFLD patients [67]. miRNA-33a has been recently reported to participate in NASH development, counteracting cholesterol 7alpha-hydroxylase (CYP7A1). Sterol response element-binding protein 2 (SREBP2) binds to its own gene promoter to induce miR-33a, which leads to a decrease in cholesterol efflux to HDL and bile acid synthesis in Cyp7a1-tg mice [68]. In addition, miR-33a inhibits CYP7A1 and bile acid synthesis to inhibit cholesterol catabolism.
Table 1.
Modulation of miRNA expression relevant to NAFLD/NASH. Δ indicates up- (↑) or downregulation (↓). CYP7A1: cholesterol 7α1-hydroxylase; SREBP2: sterol response element-binding protein 2; SIRT1: sirtuin1; AMPK: 5′ adenosine monophosphate-activated protein kinase; HMGCR: 3-hydroxy-3-methylglutaryl-CoA reductase; FAS: fatty acid synthase; ACC: Acetyl-CoA carboxylase; mTOR: mammalian target of rapamycin; ROS: reactive oxygen species; RAC1: Ras-related C3 botulinum toxin substrate 1; ?: mechanism and/or target unknown.
| miR | Δ | Disease | Model | Role | Validated/Predicted Target | Reference |
|---|---|---|---|---|---|---|
| 33a | ↑ | NASH | Mouse Liver | Cholesterol and bile acid homeostasis | CYP7A1, SREPB2 | [68] |
| 34a | ↑ | NAFLD/NASH | Human Biopsies | Lipid homeostasis | SIRT1-AMPK-HMGCR | [67,69] |
| 103a2 | ↑ | NAFLD | Human Biopsies | Insulin signaling, metabolism, inflammation | ? | [30,70] |
| 160b | ↑ | NAFLD | Human Biopsies | Insulin signaling | ? | [30] |
| 122 | ↓ | NASH | HFD mice/Human Biopsies | Lipid and cholesterol metabolism | HMGCR, FAS, SREBP1/2, ACC | [66,71] |
| 301a-3p | ↑ | Steatosis/NAFLD/NASH | Human Biopsies | ? | ? | [69] |
| 375 | ↓ | NAFLD/NASH/Cirrhosis | Human Biopsies | ? | ? | [69] |
| 576-5p | ↑ | NAFLD | Human Biopsies | Insulin signaling, metabolic homeostasis, inflammation | mTOR signaling, ephrin B signaling, ROS production, RAC1 | [70] |
| 892a | ↑ | NAFLD | Human Biopsies | Kupffer cell activation ? | ? | [70] |
| I137 | ↑ | NAFLD | Human Biopsies | ? | ? | [70] |
| 1282 | ↓ | NAFLD | Human Biopsies | Insulin signaling, metabolism, inflammation | ? | [70] |
| 3663-5p | ↑ | NAFLD | Human Biopsies | Insulin signaling, metabolism, inflammation | ? | [70] |
| 3924 | ↑ | NAFLD | Human Biopsies | Insulin signaling, metabolism, inflammation | ? | [70] |
More recently, other dysregulated miRNAs have been identified in NAFLD livers [70]. Among these, the most significantly upregulated (miR-103a-2, miR-106b, miR-576-5p, miRPlus-I137, miR-892a, miR-1282, miR-3663-5p, and miR-3924) play critical roles in insulin signaling, metabolism homeostasis, inflammation and cancer. In particular, miR-576-5p influences multiple pathways implied in NAFLD, including mammalian target of rapamycin (mTOR), a kinase modulated by insulin that induces hepatic lipogenesis through a PPARγ-dependent mechanism [72]. miR-576-5p also regulates eukaryotic translation initiation factor 4 (eIF4), p70S6 kinase (p70S6K) and phosphatidylinositol-4,5-bisphosphate 3-kinase (PI3K), pathways associated with insulin action and metabolic control. Moreover, a direct target of miR-576-5p is the small GTPase RAC1, which promotes lipotoxicity via c-Jun N-terminal kinase (JNK) activation. RAC1 is negatively modulated by miR-576-5p, triggering a protective effect against NAFLD progression [72]. Finally, in a study conducted in biopsy-staged NAFLD patients, increased miR-301a-3p and miR-34a-5p and decreased miR-375 significantly correlated with disease progression [69].
4. Dietary Factors
Lifestyle changes focusing on weight loss remain the keystone of NAFLD and NASH treatment [73]. Recent reports indicate that lifestyle modifications based on decreased energy intake and/or increased physical activity during 6–12 months cause improvement in biochemical and metabolic parameters and reduce steatosis and inflammation [74]. Conversely, increased consumption of sugar-sweetened food and beverages has been associated with NAFLD development and progression. High intake of fructose, used as food and drink sweetener, is implicated in NAFLD pathogenesis through several mechanisms. In addition, a fructose-enriched diet contributes to induce liver fibrosis in animal models of NASH [75]. Via the portal vein, dietary fructose reaches the liver in high concentrations, exerting a lipogenic action by activation of the transcription factors SREBP1 and ChREBP and subsequent induction of acetyl-CoA carboxylase (ACC) 1, fatty acid synthase (FAS) and stearoyl-CoA desaturase 1 (SCD1) [76]. These effects persist in liver-specific insulin receptor knockout mice, indicating that fructose stimulates lipogenesis independently of insulin signaling [77]. Fructose-induced de novo lipogenesis (DNL), enhancing malonyl-CoA concentration, inhibits mitochondrial β-oxidation and decreases mitochondrial ATP production [78]. In addition, fructose stimulates lipogenesis by inducing ER stress and subsequently activating the transcription factor X-box binding protein 1 (XBP1), which, in turn, upregulates lipogenic enzymes, as demonstrated in mice fed with a 60% fructose diet [79]. In concomitance, phosphorylation of fructose to fructose-1-phosphate leads to depletion of hepatic ATP and increase in ADP and inosine monophosphate (IMP), which is converted to uric acid [80], that promotes steatosis inducing mitochondrial oxidative stress [81]. Generation of reactive oxygen species (ROS) is also induced by fructose metabolism [82], and nutrient-derived ROS have been associated with enhanced steatosis via insulin-independent PI3K pathway [83]. Moreover, upregulating ketohexokinase, fructose potentiates its own metabolism and ketohexokinase inhibition leads to decreased fatty liver and reduced liver inflammation in high-fat/high-sucrose fed mice [84]. Finally, fructose-induced metabolic disorders can be mediated by epigenetic changes, such as alterations in genomic or mitochondrial DNA (mtDNA) methylation [85,86].
Dietary iron overload has been recently implicated in NASH pathogenesis. A study by Handa et al. [87] shows that dietary iron excess leads to a severe NASH phenotype in an obese, diabetogenic mouse model characterized by oxidative stress, inflammation and ballooning. Different molecular mechanisms are involved, including upregulation of cytokines (interleukin 6, IL-6, tumor necrosis factor α, TNFα) and immune mediators (Toll-like receptor 4, TLR4, inducible nitric oxide synthase, NOS, interferon gamma, IFNγ), and induction of inflammasome related factors (NOD like receptor 3, NLRP3, interleukin 18, IL-18) and genes associated with lipid metabolism. Moreover, emerging evidence indicates that hepatic copper (Cu) deficiency is associated with NAFLD development and progression. In an experimental rat model, a Cu deficient diet coupled with high sucrose intake provoked NASH, even in the absence of obesity or severe steatosis. Rats fed low-Cu/high-sucrose diet displayed enhanced liver expression of lipogenic enzymes, such as ATP citrate lyase (ACLY) and FAS, and of inflammatory and pro-fibrogenic factors (TNFα, C–C motif chemokine CCL2, CCL3), together with hepatic stellate cell activation. While low Cu alone promotes lipid peroxidation, as indicated by increased levels of malondialdehyde (MDA), its combination with high sucrose (or fructose), that causes a further reduction of hepatic Cu, causes insulin resistance and liver damage, with hepatocyte ballooning and occurrence of Mallory-Denk bodies. In addition, Cu deficiency influences Fe retention and partitioning in animals as well as in NAFLD patients [88].
Several lines of evidence correlate hepatic free fatty acids (FFAs) and free cholesterol (FC) accumulation to NAFLD pathogenesis. Dysregulation of lipid homeostasis plays an essential role in NAFLD pathogenesis, induced by a surplus of dietary free fatty acids, enhanced DNL and augmented lipolysis [89]. Rather than total hepatic fat content, the role of specific lipid classes in the development and progression of NAFLD is emerging [90]. In particular, accumulation of different lipids as well as upregulation of distinct enzymes mediating DNL was found to be associated with macrovesicular or microvesicular steatosis, the latter correlating with mitochondrial dysfunction and NAFLD [91]. Among toxic lipids, saturated fatty acids have been shown to be elevated in NASH patients [92] and induce inflammation and hepatocyte apoptosis by activating JNK and mitochondrial pathways. Other lipids having a role in NAFLD include ceramide, diacylglycerol (DAG) and sphingosine [90,93,94,95,96]. In particular, DAG and ceramide impair insulin capability to stimulate glycogen synthesis and suppress gluconeogenesis, through protein kinase-C epsilon (PKCε) activation [97]. In contrast, unsaturated fatty acids do not affect cell viability and an increase in their content leads to enhanced hepatic synthesis of TG. In turn, TG accumulation is not toxic but may protect the liver from the excessive deposition of toxic TG precursors [98,99]. Omega-3 polyunsaturated fatty acids (PUFAs) plasma levels are reduced in patients with NASH. However, pharmacologic supplementation did not induce an amelioration of the histologic picture of NASH [100], and in an experimental model it was even associated with more severe damage [101].
Emerging evidence underscores the role of cholesterol as a prominent risk factor for the pathogenesis of NAFLD/NASH. In humans a progressive increase in hepatic FC during NAFLD progression to NASH has been observed [102,103]. In experimental models increase in dietary cholesterol has been shown to promote hepatic inflammation and fibrosis [104,105,106], whereas a cholesterol-free diet ameliorates NASH [107]. The molecular mechanisms underlying FC accumulation during NASH development are multiple and only partially elucidated. Current data indicate that cholesterol homeostasis is dysregulated in NAFLD, due to an increase in cholesterol synthesis and uptake or dysfunction in cholesterol metabolism. Accordingly, the activity of two key regulators of cholesterol synthesis, HMGCR and SREBP2, is elevated in NASH patients [103,108,109]. Similarly, expression analysis of genes involved in cholesterol metabolism reveals a number of altered pathways in individuals with NASH [108].
Cholesterol uptake from lipoproteins is mediated by different proteins, including the low density lipoprotein receptor (LDLR) and the scavenger receptor class B type I (SR-BI) [110]. Hepatic uptake of LDL-cholesterol occurs via the scavenger receptor pathway in unrestrained manner, leading to deposition of cholesterol crystals in hepatocytes and generation of foamy Kupffer cells, two critical features of NASH [111,112]. Intracellular accumulation of free cholesterol represents a key event for inflammasome activation and inflammatory response [112] and sensitizes cells to transforming growth factor beta (TGF-β), TNF-α and Fas, leading to liver damage and disease progression [104,113]. Moreover, LDL cholesterol can be oxidized to oxidized low-density lipoprotein (oxLDL) cholesterol, which has been found in high concentrations in the plasma of NASH patients [114] and induces proinflammatory cytokine secretion accumulating in lysosomes of Kupffer cells [111,112]. Recently, a reduced efflux of FC has been observed in injured (foam) hepatocytes of NAFLD patients, associated with reduced expression of ATP-binding cassette sub-family G member 8 (ABCG8), which regulates cholesterol excretion trough the bile [108]. In addition, decreased expression of CYP7A1 and CYP27A responsible for cholesterol transformation into bile acids (BA) has been found in human NAFLD/NASH [108], as well as in a rat model of NASH induced by dietary cholesterol overload [115].
Oxysterols, the oxidative products of cholesterol generated during bile acid synthesis, have been described to induce liver damage through mitochondrial impairment. A study by Bellanti et al. [116] shows that mice fed high fat/high cholesterol (HF/HC) exhibit high levels of toxic oxysterols, such as triol, and oxidative stress and mitochondrial dysfunction associated with NASH. Accordingly, Huh7 and primary rat hepatocytes co-exposed to triol and palmitic or oleic acid, undergo apoptosis, mediated by impaired mitochondrial respiratory chain [116]. Finally, besides the effects on liver, cholesterol contributes to NASH pathogenesis also by stimulating inflammatory reactions in other tissues, such as adipose tissue and arterial wall, representing a key factor in the multiparallel scenario concurring to NASH [117,118].
5. Mitochondrial Dysfunction and Apoptosis
Oxidative stress has been recognized as a major factor in the pathogenesis of NASH. Based on the evidence that a high amount of intracellular ROS are generated in mitochondria and ROS overproduction is elicited in the presence of respiratory chain disruption, mitochondrial impairment has been suggested as a main event in NASH development [83,119,120]. Along these lines, structural and functional defects in mitochondria have been reported in patients with NASH [121,122].
Several mechanisms contribute to mitochondrial impairment and subsequent hepatic cell injury during NASH, mainly associated with lipotoxicity. It has been shown that, following lipid accumulation, water and calcium influx in mitochondria is increased, due to lower phosphorylation of the voltage dependent anion channel (VDAC) in the mitochondrial outer membrane, resulting in cytochrome c release and cell death [123]. Lipotoxic effects in mitochondria are also mediated by JNK; high concentrations of palmitate cause mitochondrial dysfunction and apoptosis through phosphorylation of Sab (SH3BP5), a mitochondrial outer membrane substrate of JNK [124], whereas free cholesterol accumulation in the liver of NASH mice induces mitochondrial permeability, ROS production and apoptosis through JNK1. An emerging role for NAD+ in mitochondrial stress induction during NASH development has been recently shown. Gariani et al. demonstrated that mice fed high-fat/high-sucrose exhibit impaired mitochondrial function associated with lower hepatic NAD+ levels [125]. Conversely, NAD+ repletion displays a protective effect against NAFLD, probably mediated by the induction of mitochondrial unfolded protein response (UPRmt), an adaptive mechanism dependent on the histone deacetylases SIRT1 and SIRT3, aimed to enhance mitochondrial activity and hepatic β-oxidation [126]. Furthermore, recent studies have suggested a role for coenzyme Q (CoQ), which is essential for mitochondrial respiration, in NAFLD development and progression to NASH [127,128,129,130]. Abnormal concentrations of CoQ have been found in plasma and liver of NAFLD patients [131] and perturbation in CoQ metabolism was observed in experimental NAFLD during disease progression [132,133].
Other key inducers of mitochondrial dysfunction are lysosomal permeabilization, which is frequently observed in NAFLD patients and associated with caspase activation [134], and ROS generation. CYP2E1 promotes oxidative stress, inflammation and protein modifications, by hydrolyzing molecules such as fatty acids and ethanol into toxic metabolites, including ROS, which cause respiratory chain disruption and mitochondrial damage [135], resulting in hepatocyte injury and progression to NASH [136].
6. Necroptosis
Necroptosis is a recently described cell death mechanism, morphologically comparable to necrosis, but consisting in definite biochemical pathways that occur in a programmed mode [137] and are potentially involved in inflammatory disorders, including liver diseases. Necroptosis can be initiated by activation of multiple signals, such as toll-like receptors, death receptors and others, which lead to the assembly of the necrosome, a multiprotein complex consisting in caspase-8, Fas-Associated protein with Death Domain (FADD), cellular FLICE/caspase 8-like inhibitory protein (cFLIP), and receptor-interacting proteins 1 and 3 (RIP1 and RIP3) [138]. RIP1–RIP3 interaction initiates necroptotic signaling [139]; RIP3 phosphorylates mixed lineage kinase domain-like protein (MLKL), which oligomerizes and translocates to the plasma membrane causing irreversible membrane damage and consequent cell death [140]. In specific cell setting, RIP3 can mediate necroptosis independently of RIP1 [141,142,143]. In other cell contexts, a RIP3 dependent ROS production may play an additional role [144,145].
Recently, necroptosis has been proposed as a novel mechanism in the pathogenesis of NAFLD both in humans and experimental models. Gautheron et al. found that RIP3 was overexpressed and mediated liver inflammation, activation of hepatic progenitor cells/cholangiocytes and liver fibrosis in NASH patients and in the methionine/choline-deficient (MCD) mouse model of steatohepatitis. They observed that RIP3 induces JNK activation, leading to release of pro-inflammatory mediators, such as CCL2, that further sustain RIP3-dependent signaling, cell death, and liver fibrosis. RIP3-induced pathways were blocked by caspase-8. [146]. A study by Afonso et al. [147] confirmed that hepatic levels of RIP3 are significantly augmented in steatohepatitis and showed that RIP3-dependent MLKL activation is increased in the liver of NAFLD patients as well as in MCD-induced experimental NASH. Moreover, lack of RIP3 ameliorates liver injury, steatosis, inflammation and fibrosis in experimental NASH.
7. Endoplasmic Reticulum Stress
ER stress has been implicated in a number of liver diseases, including NASH. ER dysfunction, ATP depletion or other stimuli induce the unfolded protein response (UPR), an adaptive mechanism directed to avoid luminal accumulation of defective proteins and apoptosis initiation. In NAFLD, a cross-talk between insulin signaling and UPR has been reported, involving XBP–1/PI3K interaction and consequent XBP-1 nuclear translocation [148]. Other pathways activated by cellular response to ER stress involve JNK, an activator of inflammation and apoptosis implicated in NAFLD progression to NASH [90] and SREBP-1c, which induces liver fat accumulation, worsening ER stress [149]. In vitro studies show that exposure of hepatic cells to a lipotoxic concentration of palmitate, a saturated fatty acid (SFA), is associated with ER calcium depletion, ROS accumulation and apoptosis [92,150,151]. In fact, increased SFA incorporation in ER membrane, as well as altered phosphatidylcholine/phosphatidylethanolamine ratio, induces disruption of ER membrane and impairment of sarcoendoplasmic reticulum calcium ATPase (SERCA) function, causing a net calcium efflux from ER stores and its subsequent translocation to the mitochondria, with dysregulation of mitochondrial metabolism and oxidative stress. Accordingly SERCA activity is impaired in obese livers [152] and overexpression of SERCA in obese mice improve hepatic ER stress, indicating that SERCA plays a crucial role in lipotoxic-induced ER stress and, indirectly, in mitochondrial dysfunction [152].
8. Hypoxia
In experimental NASH, hypoxia causes alterations in lipid homeostasis, upregulating genes involved in lipogenesis, such as SREBP-1c, PPARγ, ACC1 or 2 and downregulating genes implied in lipid metabolism, such as PPARα and carnitine palmitoyltransferase-1 (CPT-1) [153]. Besides lipid metabolism, insulin signaling is also affected and under hypoxic conditions hepatic upregulation of inflammatory cytokines and profibrogenic genes was observed [154]. Moreover, reduced oxygen availability induces secretion of adipokines and inflammatory cytokines in adipose tissue [155], contributing to alter lipid metabolism and glucose homeostasis [156,157]. These effects are mediated by hypoxia-inducible transcription factors (HIF-1α and HIF-2α) that regulate cellular response to oxygen deficiency and can be also activated by other stimuli, including oxidative stress or inflammatory signals [158]. In particular, HIF-1α transcription is induced by nuclear factor kappa-B (NF-κB), and NF-κB activity is crucial for HIF-1α accumulation under oxygen deprivation [159]. Furthermore, hypoxia has been reported to modulate inflammation by regulating TLR expression and function through HIF-1 [160,161]. Along these lines, it is conceivable that the proinflammatory state observed in obese NAFLD patients may be enhanced by hypoxia, due to a positive feedback mechanism involving HIF-1α and NF-κB, explaining the exacerbation of liver injury in NAFLD subjects in the presence of obstructive sleep apnea-hypopnea syndrome (OSAHS) [162].
9. Inflammation
Inflammation represents a crucial aspect in NASH pathogenesis. Overload of toxic lipids, mainly FFA, causes cellular stress and induces specific signals that trigger hepatocyte apoptosis, the prevailing mechanism of cell death in NASH, correlating with the degree of liver inflammation and fibrosis [163]. Signaling pathways induced by key death receptors, such as TNF-related apoptosis-inducing ligand (TRAIL-R), Fas and tumor necrosis factor receptor (TNFR), are upregulated in NASH, indicating they may have a role in promoting inflammation and chemokine secretion. Although the precise role of Fas and TNFR in NASH in vivo is still controversial, it has been shown that lack of TRAIL-R is protective, as TRAIL-R-deficient mice display reduced steatosis, inflammation and fibrosis in association with lower hepatocyte apoptosis [164]. Moreover, prolonged ER stress and mitochondrial dysfunction, two critical events in NAFLD, have been reported to induce apoptosis through TRAIL-R/caspase 8 [165].
Different types of immune cells are recruited and/or activated to the site of injury, contributing to NAFLD development and progression. Kupffer Cell (KC) activation is critical in NASH and precedes the recruitment of other cells [166]. Lanthier et al. [167] have shown that KC depletion increases insulin sensitivity and ameliorates inflammation and fibrosis. Depending on the settings, different polarization forms have been described for KCs, mainly classified in two phenotypes: M1, pro-inflammatory and M2, considered primarily immunoregulatory [168]. However, markers of both M1 and M2 forms can be expressed at once [169]. Differentiation of KCs towards a M1 phenotype is principally driven by pathogen-associated molecular patterns (PAMPs) that, interacting with TLRs, induce the secretion of various cytokines, such as IL-1β, IL-12, TNF-α, CCL2 and CCL5, concurring to further hepatocyte damage and release of damage-associated molecular patterns (DAMPs). DAMPs, in turn, act on TLRs amplifying KCs activation and inflammation. In addition, some cytokines (i.e., CCL2 and CCL5), induce HSC activation, initiating a fibrogenic response [170]. Activation of KCs in NAFLD is also triggered by toxic lipids, that upregulate TLRs and augment the response to lipopolysaccharide (LPS) [171]. KCs displaying the M2 phenotype produce several factors with anti-inflammatory properties, as IL-4, IL-10, IL-13 and TGF-α [168,169], but different subtypes have been identified with diverse actions. Although it has been reported that induction of peroxisome proliferator-activated receptor delta (PPARδ) drives KCs toward the M2 form, reducing obesity-induced insulin resistance in mice [172], the role of M2 KCs in NAFLD is still not elucidated [168].
Despite potent antimicrobial and phagocytic properties, neutrophils display scarce specificity. Excess of neutrophil recruitment in NASH crucially contributes to hepatocyte damage, inflammation and fibrosis, through the release of different factors [173,174], including cytotoxic enzymes as myeloperoxidase and elastase. Myeloperoxidase-deficient mice show moderated NASH, associated with lower hepatic secretion of inflammatory cytokines [175]. Similarly, deletion of neutrophil elastase attenuates liver inflammation in experimental NAFLD [176].
Dendritic Cells (DCs) counteract sterile inflammation acting as antigen-presenting cells and eliminating cell debris and apoptotic cells. Studies aimed to establish DCs’ function in NASH have shown controversial results [177]. An anti-inflammatory and antifibrotic role of DCs in NASH is suggested by the fact that liver depletion of these cells exacerbates inflammation and fibrosis. According to the study by Henning et al liver infiltrating DCs activate and secrete IL-6, TNF-α and CCL2 [178]. In contrast, other findings report that avoiding the accumulation of DCs subtypes expressing high levels of inflammatory factors limits liver injury in experimental NASH [179].
Natural Killer (NK) cells in the liver are stimulated through several receptors upon interaction with other hepatic cells. In NASH, activation of NK can be achieved by a broad number of ligands and cytokines, but the role of these cells in NAFLD pathogenesis is still controversial [180,181]. Two different phenotypes of NKT cells have been recently associated with liver disease, acting in opposite modes during sterile inflammation: proinflammatory type I and protective type II cells [182]. Although NKT type I cells can be activated by lipids, suggesting their possible involvement in NAFLD, NKT-deficient mice fed HFD are more prone to steatosis and weight gain than wild type mice [183]. In addition, adoptive transfer of NKT cells in leptin-deficient mice ameliorates glucose metabolism and diminishes fatty liver [184]. Furthermore, depletion of NKT can result in activation of KC and secretion of IL-12 [184]. Conversely, clinical studies performed in patients with different stages of NAFLD demonstrate that NKT cells tend to increase in the liver during disease progression [185]. According to these data, NKT cells seem to be depleted in early NAFLD to enhance in the later phases, participating in inflammation and fibrosis [186].
10. Hedgehog
Hedgehog (Hh) is a well-characterized factor implied in the fibrogenic process of several organs, including the liver. Hh pathway activation is proportional to the severity and persistence of injury [187], induces a cascade of events concurring to wound healing response and involves various cell types, including damaged ballooned hepatocytes, inflammatory cells (mainly NKT cells and macrophages), ductular/progenitor cells and HSCs [188].
The Hh pathway was associated with severe NASH in a gene profiling study where patients with different severity of the disease were included [189]. In experimental NASH, the Hh pathway leads to proliferation and activation of ductular progenitor cells and HSC, that, in turn, produce Hh ligands and, consequently, soluble mediators such as osteopontin and CXCL-16, responsible for immune cells recruitment and damage progression [190,191]. Moreover, Patched-heterozygous deficient mice, characterized by hyperactivation of the Hh pathway, show exacerbation of the disease following a NASH-inducing diet, whereas liver-specific inhibition of Smo prevents diet-induced liver damage and fibrosis, despite hepatic lipid accumulation [190].
Caspase-2 has been recently identified as a critical factor in NASH pathogenesis, mediating hepatocyte lipoapoptosis. Hepatic caspase-2 was found to be increased both in human and experimental NASH, in association with profibrogenic factors, such as Hh-related genes. When challenged with a HF diet or fed a MCD diet, caspase-2 knockout mice showed lipid-induced hepatic apoptosis, together with decreased activation of Hh signaling and fibrosis [192].
In NAFLD patients, Hh activity and Hh ligands’ expression correlates with the degree of fibrosis [193] and elevated Hh activation is associated with hepatocyte ballooning, high presence of progenitor cells and myofibroblasts and portal inflammation [187]. In agreement with these findings, the Pioglitazone vs. Vitamin E vs. Placebo for treatment of NASH (PIVENS) trial demonstrated that amelioration of NASH in response to treatment was associated with a marked decrease of Sonic Hh ligand (Shh) expressing hepatocytes [194].
11. Nuclear Receptors
Nuclear receptors are ligand-dependent transcription factors that regulate glucose and lipid metabolism in the liver. Nuclear receptors are divided into seven subfamilies named as NR0-NR6 [195] and NR1 subfamily is of particular importance in NAFLD. This latter group of nuclear receptors is retained in the nucleus and heterodimerizes with the retinoid X receptor (RXRα) [195,196] and includes: NR1C1-3 (the peroxisome proliferator-activated receptors, PPARα, β, γ), NR1H2-3 (the liver X receptors, LXRα, β), NR1H4 (the farnesoid X receptor, FXRα), NR1I2 (the constitutive androstane receptor, CAR), and NR113 (the pregnane X receptor, PXR). PPARs inhibit inflammation in the obese state acting on NF-κB and AP1 transcription factor and regulate metabolism by inducing transcription of adiponectin (PPARγ) and fibroblast growth factor-21 (FGF21) (PPARα and FXR) [195]. PPARα regulates β-oxidation and cholesterol removal during the fasting state or when metabolism increases in adipose and/or muscle tissues [195]. Hepatic PPARα expression decreases in NAFLD leading to steatosis, but is enhanced following diet and exercise [197,198].
In animal models of steatosis and steatohepatitis, the use of PPARα activators improves the disease [199,200]. In addition, several studies in mice suggest that induction of both PPARβ/δ and PPARγ ameliorates steatosis [201,202]. Indeed, animals treated with PPARα activators show less weight gain than controls, lower levels of epididymal fat, and are protected from atherosclerosis [203]. PPAR activation may also ameliorate fibrosis, since NASH patients treated with pioglitazone (a PPARγ agonist) had improved fibrosis biomarkers [204]. Recent studies show that PPARγ downregulates adipocyte endothelial nitric oxide synthase (eNOS), a molecule that contributes to IR and development of NASH [205]. Since the use of selective PPARα agonists has proven quite ineffective against NAFLD [197] the use of mixed receptor agonists (PPARα and PPARβ/γ) is underway in the therapy for NASH patients and recent results have been reported [206].
PXR, expressed in many tissues but mainly in the liver [207], is released not only by hepatocytes, but also by Kupffer and stellate cells [208]. Two polymorphisms of this gene have been associated with augmented severity of NAFLD: rs7643645/G and rs2461823 [209], whereas a variant encoding a short dominant negative PXR isoform, which inhibits the full-length isoform activity, has been recently described [210]. PXR regulates various genes involved in xenobiotic and drug metabolism, including enzymes [211] that play a role in the oxidative metabolism of lipophilic compounds such as steroids, fatty acids, bile acids, drugs, retinoids, and xenobiotics. PXR activation has been associated with increased severity of steatosis, obesity, insulin resistance and hypercholesterolemia as it enhances hepatic fatty acid uptake and lipogenesis, while it decreases β-oxidation [212,213]. The role of PXR in experimental NAFLD is more complex. While PXR knockout mice are resistant to obesity, they show impaired glucose tolerance, hyperleptinemia and hypoadiponectinemia, together with elevated fasting glucose levels [212]. Recently, it was shown that PXR activation inhibits the production of many NF-κB target genes and increases the production of secreted interleukin-1 receptor antagonist (IL-1RA), reducing the effects of LPS-induced inflammation [214].
Human CAR1-3, expressed mainly in liver and intestine and to a lower extent in other tissues [215], is implicated in protection against toxic food or contaminants [216]. CAR is also associated with lipid metabolism and inflammation in NAFLD. CAR increases in the liver in the fed state, reducing hepatic steatosis, inflammation, insulin resistance and hypercholesterolemia [217]. In animal models, treatment with an agonist of CAR ameliorates diet-induced obesity, hepatic steatosis and diabetes [218]. Moreover, in knockout mice for the low density lipoprotein receptor (LDLR), activation of CAR reduces triglycerides and cholesterol plasma levels [219]. Recently, it has been reported that activated CAR translocates into the nucleus and functions as an adaptor protein to recruit PGC1α to the Cullin1 E3 ligase complex for ubiquitination. The interaction between CAR and PGC1α also induces the degradation of PGC1α and suppression of gluconeogenesis both in vitro and in vivo [220]. CAR can induce carcinogenesis in mice, although this effect has not observed in humans [221]. Indeed, CAR activation in humans may have antiproliferative effects, as demonstrated by a recent report showing that CAR-deficient HepaRG cells have increased expression of proliferative genes [222].
FXR, highly expressed in liver, kidney, intestine, and adrenals, inhibits the expression of CYP7A1 and sterol 12-α-hydroxylase (CYP8B1), genes involved in bile acid synthesis from cholesterol. Besides its central role in bile acid metabolism, FXR activation also regulates the expression of various genes involved in glucose, lipid, and lipoprotein metabolism, crucial in NAFLD [223]. Hepatic FXR inhibits fatty acid synthesis and uptake and upregulates beta oxidation, regulating lipid homeostasis [224]. In NAFLD patients and in animal models, activation of FXR by obeticholic acid (OCA) decreases both steatosis and obesity [225,226]. In HF/HC diet-treated mice, the FXR agonist GW4064 decreased the expression of the hepatic lipid transporter CD36, reducing hepatic steatosis and weight gain [227]. FXR can regulate insulin resistance as recently demonstrated in NASH patients treated with OCA, which improves insulin sensitivity [228]. Similarly, OCA treatment in Zucker (fa/fa) rats improves insulin sensitivity, and GW4064 treatment, in HF/HC diet mice, reduces hyperinsulinemia and hyperglycemia [226]. Besides OCA and GW4064, further potential novel therapeutic targets in NASH are currently in phase II clinical development [229].
Intestinal activation of FXR reduces weight gain, liver glucose production and steatosis, stimulating human fibroblast growth factor-19 (FGF19). This factor inhibits CYP7A1 resulting in an inhibition of liver bile acid synthesis. Indeed, administration of FGF19 in mice and rats animal models increases fat oxidation and decreases liver triglycerides and glucose levels [230,231]. Recent studies show that activation of intestinal FXR by feraxamine inhibits weight gain induced by diet, hepatic glucose production and steatosis. These effects are mediated by fibroblast growth factor-15 signaling, without interfering with hepatic FXR activation [232]. Intestinal FXR agonism promotes adipose tissue browning and reduces obesity and insulin resistance, suggesting that tissue-specific activation of FXR may be a novel approach to treat NAFLD. Activation of intestinal FXR affords hepatoprotection by restoring hepatic homeostasis, regulating cellular proliferation and decreasing hepatic fibrosis and inflammation [233].
12. Pattern Recognition Receptors and the Inflammasomes
Toll-like receptors are highly conserved receptors that recognize endogenous danger signals, such as molecules released by damaged cells (damage-associated molecular patterns, DAMPs) or exogenous danger signals, as gut-derived pathogen-associated molecules (pathogen-associated molecular patterns, PAMPs) [234,235]. Due to the high liver exposure to danger signals via the portal system, TLR-induced pathways play a central role in activation of hepatic cells, primarily Kupffer cells, but also hepatocytes and HSC. As pattern recognition receptors (PRR), TLRs act as defense mechanism, but are also implicated in the pathogenesis of NASH [236,237]. Among NAFLD-related TLRs, TLR2 interacts with a broad range of PAMPs, including peptidoglycan, a surface component of Gram-positive bacteria [238], which appears to be increased in NAFLD [239]. Importantly, inhibition of TLR2 signaling prevents insulin resistance in HFD mice [240], whereas TLR2-deficient mice fed HFD display reduced levels of inflammatory cytokines and do not develop NASH [241].
The role of TLR5 in NAFLD pathogenesis is still unclear, as only a correlation with dysbiosis and metabolic syndrome has been reported [242,243]. TLR9, an intracellular receptor, is activated by unmethylated DNA, typically express in viruses and bacteria but rare in mammalian cells. TLR9 downstream signaling involves IL-1, and is associated with NASH severity and fibrosis [244]. A study conducted in an experimental model of colitis, with high portal levels of LPS, shows increased TLR9 liver expression, associated with hepatic steatosis, inflammation, and fibrosis [245].
The crucial role of TLR4 in NAFLD pathogenesis has been demonstrated in TLR4-deficient mice, that display lower levels of inflammatory mediators and fail to develop NAFLD or insulin resistance [246]. TLR4 plays a major role in linking innate immunity with inflammatory response and the function of TLR4 in Kupffer cells is well characterized [247]. TLR4 is primarily activated by Gram-negative bacterial lipopolysaccharides (LPS), leading to overexpression of cytokines, chemokines and antimicrobial molecules [248,249]. LPS/TLR4 interaction, that requires LPS-binding protein and two co-receptors (CD14 and myeloid differentiation protein 2, MD2), activates downstream pathways in a myeloid differentiation factor (MyD)88-dependent or independent fashion [250]. The MyD88-dependent pathway signals through IκB kinase (IKK)/NF-κB and mitogen activated protein kinase (MAPK)/AP-1, inducing the expression of pro-inflammatory cytokines (TNF-α, IL-1β, IL-6 and IL-12) and genes implicated in the immune response [250]. The MyD88-independent cascade involves IFNs [250]. ROS production and subsequent activation of the unfolded protein response are also induced in TLR4-activated Kupffer cells, representing an additional mechanism triggered by TLRs in NAFLD progression [251].
Besides Kupffer cells, TLR4 is expressed by other hepatic cells, including HSCs, hepatocytes and cholangiocytes and LPS/TLR4 axis plays a critical role in the pathogenesis and progression of fatty liver diseases, as demonstrated by increased levels of portal endotoxins and TLR4 hepatic expression in experimental NASH [252,253]. Based on its expression in HSC, a direct role of TLR4 in liver fibrogenesis has been suggested. According to this hypothesis, the expression of chemokines and adhesion molecules, as well as TGF-β-mediated signaling, are positively modulated by TLR4 [254], while two TLR4 polymorphisms, protective against fibrosis, are associated with a lower apoptotic threshold for HSC [255].
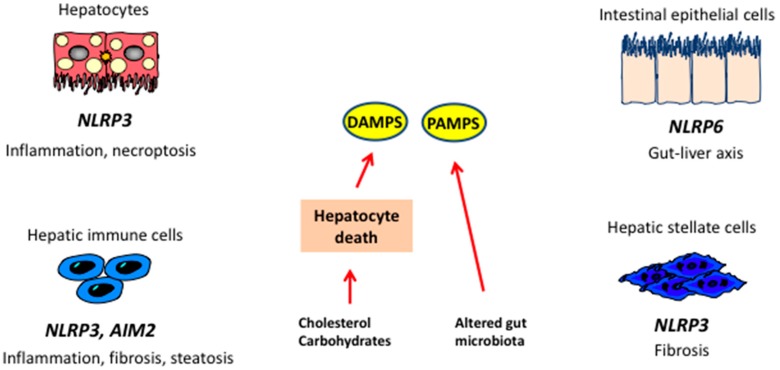
TLR4-mediated inflammatory response can also be elicited by DAMPs released by necrotic cells, such as high mobility group box 1 (HMGB1) or phospholipids. These molecules stimulate monocyte and Kupffer cells to secrete inflammatory mediators (Figure 3). It is noteworthy that, in the presence of high glucose, TLR4 activation and downstream signaling can be triggered by FFA [256], clarifying, at least in part, the mechanism by which saturated fatty acids, frequently enhanced in plasma of obese patients, have toxic effects [257].
Figure 3.
Inflammasomes and the liver. In steatosis, hepatic damage leads to generation of damage-associated molecular pattern (DAMPs), while alterations in microbiota lead to increased availability of pathogen-associated molecular patterns (PAMPs). DAMPs and PAMPs act on receptors localized on liver cells leading to activation of different inflammasomes and release of cytokines implicated in NASH. NLRP3: NOD-like receptor family, pyrin domain containing 3; AIM2: Abscent in melanoma 2.
An important role in NASH pathogenesis has been recently ascribed to the nucleotide oligomerization domain (NOD)-like receptors (NLRs). NLR activation in response to DAMPs or PAMPs leads to the assembly of inflammasome, a multiprotein complex required for caspase-1 activity and initiation of inflammatory signals. Full activation of inflammasome, mediated by PRRs via NF-κB, can be induced by a broad spectrum of signals, such as uric acid, ROS, ATP [258] and mitochondrial DNA [259], and results in secretion of mature IL-1 and IL-18 [260,261]. These cytokines, acting on different cell types, elicit inflammatory signals in liver as well as in the adipose tissue and intestine, triggering steatosis, insulin resistance, inflammation and cell death [262]. A role for inflammasomes in NAFLD development and progression to NASH has been shown both in humans and animal models [263,264]. Activation of NLRP3 inflammasome has been reported in MCD diet-induced steatohepatitis [265], as well following protracted HF/HC/HS feeding [266]. Moreover, NLRP3 gain of function correlates with liver fibrosis. Conversely, absence of this receptor appears to improve metabolic activity [267] and diet-induced steatohepatitis [268], although a study by Henao-Mejia et al. [269] demonstrated that lack of NLP3 promotes gut dysbiosis and chronic inflammation. Activation of NLRP3 inflammasome has been associated with hepatocyte pyroptosis, a recently described, inflammasome-mediated cell death mechanism [268,270].
Hepatocyte damage leads to secretion of intracellular molecules, DAMPs, acting as danger signals capable to recruit and/or activate immune cells and initiate an inflammatory response in the absence of pathogens, a mechanism referred as sterile inflammation [271,272]. Several DAMPs have been identified, including nuclear and mitochondrial DNA, purine nucleotides (ATP, UTP), nuclear factors as HMGB1 and uric acid [180,273]. Besides mitochondrial DNA, which activates TLR9, a number of mitochondrial components have been shown to play a part in sterile inflammation [274,275], including formyl-peptides, ATP and ROS, that act by inducing inflammasome activation [276,277,278]. High concentrations of extracellular ATP, as a consequence of cell death, result in inflammasome activation and IL-1β production, via P2X7 receptor [279]. As binding of ATP to P2X7 provokes pore formation in the plasma membrane, allowing bacterial products to enter the cells, ATP plays a role also in pathogen-associated molecular pattern-induced inflammation [280].
HMGB1 is a constitutively expressed nuclear protein that induces transcriptional activation [281], and is released in response to different stimuli, such as PAMPs and DAMPs [282,283]. HMGB1 interacts with a broad spectrum of receptors (TLR4, TLR2, TLR9, and RAGE) exerting proinflammatory actions in complex with other factors, as single stranded DNA, LPS and IL-1β [284].
In its crystal form, uric acid induce inflammatory response by inflammasome activation in a receptor-independent manner, causing phagosome burst and spill of cytosolic proteases [285]. In some settings, DAMPs can be also secreted independently of apoptosis. HMGB1 production can occur by activated macrophages in response to LPS, TNF, and TGFβ [286]. Moreover, secondary necrosis, due to impaired efferocytosis, may contribute to release of intracellular components amplifying the inflammatory response.
13. Adipokines
Adipose tissue is recognized as an endocrine organ that secretes adipokines, which are peptides with autocrine, paracrine and endocrine functions, controlling systemic metabolism and energy homeostasis [287]. Among these, leptin and adiponectin are involved in the pathogenesis of NAFLD and progression to NASH, leptin being identified as a profibrogenic adipokine [285,288]. Adipose tissue also produces other molecules (including classical cytokines), mostly released by endothelial or immune cells, such as TNF-α and IL-6 [289]. Adiponectin has in general a beneficial impact on NAFLD [290], while others, as resistin, TNF-α and IL-6 possibly have an adverse impact. In particular, adiponectin reduces IR and shows anti-steatotic and anti-inflammatory properties, while TNF-α increases IR and displays pro-inflammatory effects [291,292]. In physiologic conditions, cytokine-adipokine interplay is finely regulated, but in some setting, such as increased adipose tissue mass, the critical balance between cytokines and adipokines is compromised, leading to chronic inflammation, IR and NAFLD [292]. Leptin, an adipokine which plays a major role in energy homeostasis, is mainly produced by adipose tissue, but it is also synthesized in other organs [293]. Consequent to an increase in adipose tissue mass, leptin is upregulated, acting as compensatory factor in preserving insulin sensitivity and exerting anti-steatotic effects. Nevertheless, if adipose tissue continues to augment, the compensatory mechanism fails, with a sustained rise in IR and hepatic steatosis [294]. Leptin-mediated dual action has been demonstrated in experimental NAFLD, as in early disease leptin exerts a protective effect by inhibiting hepatic glucose production and de novo lipogenesis through stimulation of fatty acid oxidation, while as NAFLD proceeds, it acts as a pro-fibrogenic and inflammatory factor [294]. Novel evidence indicates that leptin-mediated nicotinamide adenine dinucleotide phosphate (NADPH) oxidase increases the levels of miR21, which is a key regulator of TGF-β signaling. The rise in miR21 increases TGF-β and SMAD2/3-SMAD4 nuclear colocalizations, whilst repressing SMAD7 [295]. In addition, leptin reduces PPAR-γ expression in HSCs, promoting hepatic fibrosis [296]. A recent study, conducted by Heinrich et al., shows that leptin resistance contributes to obesity in null mice mutated for carcinoembryonic antigen cell adhesion molecule 1 (CEACAM1) [297]. CEACAM1 is a molecule that induces insulin clearance [298] and reduces fatty acid synthesis in liver in the presence of insulin resistance, hepatic steatosis and visceral obesity [299]. Furthermore, (Cc1−/−) mice develop hyperleptinemia, firstly related to the augmented visceral obesity, followed by hyperphagia and reduced physical activity. These effects are possibly due to leptin resistance and elevated hypothalamic fatty acid synthase activity, that could, in turn, be mediated by both central and peripheral factors [297].
Adiponectin is one of the most abundant adipokines, and is also produced by hepatocytes in response to liver injury [300]. It exhibits anti-steatotic and antiapoptotic actions on hepatocytes and exerts anti-inflammatory and anti-fibrotic effects acting on HSC, Kupffer and sinusoidal cells [301]. Adiponectin amounts drop when adipose mass increases, but the underlying mechanism is not completely elucidated. It may involve adipose tissue hypoxia, oxidative stress [155,302] and increased inflammatory mediator levels [303]. Another potential factor linking adipocyte hypertrophy to reduced adiponectin synthesis is mitochondrial dysfunction [304]. Recent reports show that 11β-hydroxysteroid dehydrogenase type1 (11β-HSD1) expression increases in hypertrophic adipocytes and this could be responsible for mitochondrial dysfunction and reduced adiponectin synthesis.
After NASH progression towards cirrhosis, circulating adiponectin seems to increase [305], probably due to two main mechanisms: a decrease in hepatic clearance of adiponectin and/or a compensatory mechanism aimed to buffer the hyper-secretion of inflammatory cytokines. Recent studies show that in the compensated late stage of NASH, circulating adiponectin is associated with hepatic lipid loss [306]. These data reinforce the theory that adiponectin may be involved in the “burnt-out NASH”, characterized by the loss of hepatic lipids, often observed in advanced fibrosis and cirrhosis.
Adipose tissue (mainly visceral) and liver (mainly hepatocytes) are the principal producers of chemerin [307]. Chemerin concentrations, which are generally higher in obesity and IR and drop after weight loss, may modulate insulin resistance and inflammatory responses [308]. Animal models of obesity and IR (ob/ob and db/db mice) display increased chemerin expression [309,310]. A recent study conducted in NAFLD subjects show that circulating levels of chemerin positively correlate with body mass index (BMI) and are also higher in individuals with impaired glucose tolerance (IGT) or type 2 diabetes. In MCD-induced NASH, hepatic levels of chemerin tend to increase. In human NASH, liver chemerin mRNA is upregulated in respect to healthy controls, but similar levels have been found also in steatosis [311].
14. Microbiota
Accumulating evidence indicates that dysregulation of microbiota components are involved in various liver diseases, including NAFLD and NASH, through obesity predisposition, metabolic alterations and liver inflammation. Gut microbiota produces extra energy for the host, processing polysaccharides to short-chain fatty acids (mainly acetate, propionate, and butyrate) [312] and stimulating lipogenesis. A potential role of specific gut microbiome has been suggested in the pathogenesis of NAFLD, as obese mouse models host 50% less Bacteroides and more Firmicutes compared to lean control [313], and germ-free mice show significantly greater increase in body fat following colonization with an “obese microbiome” [313]. Conversely, a recently described bacterium, Akkermansia muciniphila, has been associated with a non-obese phenotype both in humans and animal models, and HFD mice administered with Akkermansia show reduced adipose tissue inflammation and increased glucose tolerance [314,315]. The intestinal microflora produces enzymes that metabolize dietary choline, a cell membrane component regulating lipid transport in liver, into methylamines, toxic compounds responsible for inflammation and liver injury [316]. Aberrant microbiota could induce triglyceride accumulation and promote NASH both reducing choline and increasing methylamines [317].
Alterations in bile acid metabolism have been reported during NAFLD development. Intestinal bacteria can modify bile acid pool through the conversion of cholic and chenodeoxycholic acid into secondary bile acids, influencing lipid and glucose homeostasis. In addition, abnormal microbiota can impair bile acid receptor signaling, such as FXR and the G-protein-coupled bile acid-activated receptor TGR5 [318,319], affecting hepatic de novo lipogenesis and very low-density lipoprotein VLDL export [320] as well as glucose metabolism [321,322].
Endogenous ethanol is produced by several microbiome species. Ethanol induces hepatotoxicity stimulating Kupffer cells to produce nitric acid and cytokines, whereas ethanol metabolites promote triglyceride accumulation and oxidative stress in the liver. In addition, ethanol impairs gut mucosal permeability inducing endotoxemia. Enhanced breath ethanol content was found in ob/ob mice and it was abolished by antibiotic treatment [323]. Increased ethanol levels were also detected in obese individuals and in children with NASH [324].
The gut microflora plays an important role in the development and function of the host immune system [325]. Through the portal circulation, liver is directly exposed to gut-derived products, being the first line of defense against bacterial toxins. Enhanced levels of circulating LPS and endotoxins have been detected in rodents with diet-induced NAFLD and in NASH patients, respectively. LPS, the active component of endotoxins, interacts with LPS-binding protein and the CD14 receptor, activating TLRs and, consequently, the inflammatory cascade that involves stress-activated protein kinases, JNK, p38, interferon regulatory factor-3 (IRF-3) and NF-κB, pathways implicated in insulin resistance and triglycerides synthesis [252,325].
Finally, a correlation between small intestinal bacterial overgrowth (SIBO) and NAFLD has been observed in clinical and experimental studies [237,326,327]. Bacterial overgrowth in the small intestine, as well as qualitative microbiome abnormalities can impair the barrier functions of the intestinal mucosa, leading to enhanced mucosa permeability and subsequent translocation of endotoxin to the bloodstream [328,329]. Therefore, increased gut permeability represents an additional mechanism in NASH pathogenesis, acting through the accumulation of endotoxin and bacterial metabolites in liver and subsequent induction of inflammatory responses, via activation of pattern recognition receptors.
15. Perspectives
Extensive information has accumulated in the past few years on the molecular mechanisms underlying the development of steatohepatitis. This has been paralleled by a number of clinical trials exploring novel approaches, in part derived from preclinical data. Continuing research in this field will be instrumental in providing new targets and biomarkers for the management of this very prevalent condition.
Acknowledgments
Work on steatohepatitis in Marra’s laboratory is supported by grants from the Italian Ministry for Research (Projects PRIN and FIRB), the European Community (projects FLIP and EPoS), and the CARIPLO Foundation.
Author Contributions
Alessandra Caligiuri and Alessandra Gentilini searched the literature, contributed to manuscript organization and wrote the text. Fabio Marra defined manuscript organization and reviewed the final version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Satapathy S.K., Sanyal A.J. Epidemiology and natural history of nonalcoholic fatty liver disease. Semin. Liver Dis. 2015;35:221–235. doi: 10.1055/s-0035-1562943. [DOI] [PubMed] [Google Scholar]
- 2.Vernon G., Baranova A., Younossi Z.M. Systematic review: The epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment. Pharmacol. Ther. 2011;34:274–285. doi: 10.1111/j.1365-2036.2011.04724.x. [DOI] [PubMed] [Google Scholar]
- 3.Williams C.D., Stengel J., Asike M.I., Torres D.M., Shaw J., Contreras M., Landt C.L., Harrison S.A. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: A prospective study. Gastroenterology. 2011;140:124–131. doi: 10.1053/j.gastro.2010.09.038. [DOI] [PubMed] [Google Scholar]
- 4.Browning J.D., Horton J.D. Molecular mediators of hepatic steatosis and liver injury. J. Clin. Investig. 2004;114:147–152. doi: 10.1172/JCI200422422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brunt E.M., Kleiner D.E., Wilson L.A., Belt P., Neuschwander-Tetri B.A., Network N.C.R. Nonalcoholic fatty liver disease (NAFLD) activity score and the histopathologic diagnosis in NAFLD: Distinct clinicopathologic meanings. Hepatology. 2011;53:810–820. doi: 10.1002/hep.24127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pais R., Charlotte F., Fedchuk L., Bedossa P., Lebray P., Poynard T., Ratziu V. A systematic review of follow-up biopsies reveals disease progression in patients with non-alcoholic fatty liver. J. Hepatol. 2013;59:550–556. doi: 10.1016/j.jhep.2013.04.027. [DOI] [PubMed] [Google Scholar]
- 7.McPherson S., Hardy T., Henderson E., Burt A.D., Day C.P., Anstee Q.M. Evidence of NAFLD progression from steatosis to fibrosing-steatohepatitis using paired biopsies: Implications for prognosis and clinical management. J. Hepatol. 2015;62:1148–1155. doi: 10.1016/j.jhep.2014.11.034. [DOI] [PubMed] [Google Scholar]
- 8.Angulo P. Long-term mortality in nonalcoholic fatty liver disease: Is liver histology of any prognostic significance? Hepatology. 2010;51:373–375. doi: 10.1002/hep.23521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ekstedt M., Franzen L.E., Mathiesen U.L., Thorelius L., Holmqvist M., Bodemar G., Kechagias S. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. 2006;44:865–873. doi: 10.1002/hep.21327. [DOI] [PubMed] [Google Scholar]
- 10.Adams L.A., Lymp J.F., St Sauver J., Sanderson S.O., Lindor K.D., Feldstein A., Angulo P. The natural history of nonalcoholic fatty liver disease: A population-based cohort study. Gastroenterology. 2005;129:113–121. doi: 10.1053/j.gastro.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 11.Ludwig J., Viggiano T.R., McGill D.B., Oh B.J. Nonalcoholic steatohepatitis: Mayo clinic experiences with a hitherto unnamed disease. Mayo Clin. Proc. 1980;55:434–438. [PubMed] [Google Scholar]
- 12.Day C.P., James O.F. Steatohepatitis: A tale of two “hits”? Gastroenterology. 1998;114:842–845. doi: 10.1016/S0016-5085(98)70599-2. [DOI] [PubMed] [Google Scholar]
- 13.Cusi K. Role of obesity and lipotoxicity in the development of nonalcoholic steatohepatitis: Pathophysiology and clinical implications. Gastroenterology. 2012;142:711–725. doi: 10.1053/j.gastro.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Neuschwander-Tetri B.A. Hepatic lipotoxicity and the pathogenesis of nonalcoholic steatohepatitis: The central role of nontriglyceride fatty acid metabolites. Hepatology. 2010;52:774–788. doi: 10.1002/hep.23719. [DOI] [PubMed] [Google Scholar]
- 15.Tilg H., Moschen A.R. Evolution of inflammation in nonalcoholic fatty liver disease: The multiple parallel hits hypothesis. Hepatology. 2010;52:1836–1846. doi: 10.1002/hep.24001. [DOI] [PubMed] [Google Scholar]
- 16.Marra F., Lotersztajn S. Pathophysiology of NASH: Perspectives for a targeted treatment. Curr. Pharm. Des. 2013;19:5250–5269. doi: 10.2174/13816128113199990344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Loomba R., Schork N., Chen C.H., Bettencourt R., Bhatt A., Ang B., Nguyen P., Hernandez C., Richards L., Salotti J., et al. Heritability of hepatic fibrosis and steatosis based on a prospective twin study. Gastroenterology. 2015;149:1784–1793. doi: 10.1053/j.gastro.2015.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anstee Q.M., Seth D., Day C.P. Genetic factors that affect risk of alcoholic and nonalcoholic fatty liver disease. Gastroenterology. 2016;150:1728–1744. doi: 10.1053/j.gastro.2016.01.037. [DOI] [PubMed] [Google Scholar]
- 19.Dongiovanni P., Donati B., Fares R., Lombardi R., Mancina R.M., Romeo S., Valenti L. PNPLA3 I148M polymorphism and progressive liver disease. World J. Gastroenterol. 2013;19:6969–6978. doi: 10.3748/wjg.v19.i41.6969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Romeo S., Kozlitina J., Xing C., Pertsemlidis A., Cox D., Pennacchio L.A., Boerwinkle E., Cohen J.C., Hobbs H.H. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat. Genet. 2008;40:1461–1465. doi: 10.1038/ng.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Speliotes E.K., Butler J.L., Palmer C.D., Voight B.F., Consortium G., Consortium M.I., Nash C.R.N., Hirschhorn J.N. PNPLA3 variants specifically confer increased risk for histologic nonalcoholic fatty liver disease but not metabolic disease. Hepatology. 2010;52:904–912. doi: 10.1002/hep.23768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pirazzi C., Adiels M., Burza M.A., Mancina R.M., Levin M., Stahlman M., Taskinen M.R., Orho-Melander M., Perman J., Pujia A., et al. Patatin-like phospholipase domain-containing 3 (PNPLA3) I148M (RS738409) affects hepatic VLDL secretion in humans and in vitro. J. Hepatol. 2012;57:1276–1282. doi: 10.1016/j.jhep.2012.07.030. [DOI] [PubMed] [Google Scholar]
- 23.Kumari M., Schoiswohl G., Chitraju C., Paar M., Cornaciu I., Rangrez A.Y., Wongsiriroj N., Nagy H.M., Ivanova P.T., Scott S.A., et al. Adiponutrin functions as a nutritionally regulated lysophosphatidic acid acyltransferase. Cell Metab. 2012;15:691–702. doi: 10.1016/j.cmet.2012.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen W., Chang B., Li L., Chan L. Patatin-like phospholipase domain-containing 3/adiponutrin deficiency in mice is not associated with fatty liver disease. Hepatology. 2010;52:1134–1142. doi: 10.1002/hep.23812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smagris E., BasuRay S., Li J., Huang Y., Lai K.M., Gromada J., Cohen J.C., Hobbs H.H. PNPLA3 I148M knockin mice accumulate PNPLA3 on lipid droplets and develop hepatic steatosis. Hepatology. 2015;61:108–118. doi: 10.1002/hep.27242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mondul A., Mancina R.M., Merlo A., Dongiovanni P., Rametta R., Montalcini T., Valenti L., Albanes D., Romeo S. PNPLA3 I148M variant influences circulating retinol in adults with nonalcoholic fatty liver disease or obesity. J. Nutr. 2015;145:1687–1691. doi: 10.3945/jn.115.210633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kovarova M., Konigsrainer I., Konigsrainer A., Machicao F., Haring H.U., Schleicher E., Peter A. The genetic variant I148M in PNPLA3 is associated with increased hepatic retinyl-palmitate storage in humans. J. Clin. Endocrinol. Metab. 2015;100:E1568–E1574. doi: 10.1210/jc.2015-2978. [DOI] [PubMed] [Google Scholar]
- 28.Pirazzi C., Valenti L., Motta B.M., Pingitore P., Hedfalk K., Mancina R.M., Burza M.A., Indiveri C., Ferro Y., Montalcini T., et al. PNPLA3 has retinyl-palmitate lipase activity in human hepatic stellate cells. Hum. Mol. Genet. 2014;23:4077–4085. doi: 10.1093/hmg/ddu121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kozlitina J., Smagris E., Stender S., Nordestgaard B.G., Zhou H.H., Tybjaerg-Hansen A., Vogt T.F., Hobbs H.H., Cohen J.C. Exome-wide association study identifies a TM6SF2 variant that confers susceptibility to nonalcoholic fatty liver disease. Nat. Genet. 2014;46:352–356. doi: 10.1038/ng.2901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu Y.L., Reeves H.L., Burt A.D., Tiniakos D., McPherson S., Leathart J.B., Allison M.E., Alexander G.J., Piguet A.C., Anty R., et al. TM6SF2 RS58542926 influences hepatic fibrosis progression in patients with non-alcoholic fatty liver disease. Nat. Commun. 2014;5 doi: 10.1038/ncomms5309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mahdessian H., Taxiarchis A., Popov S., Silveira A., Franco-Cereceda A., Hamsten A., Eriksson P., van’t Hooft F. TM6SF2 is a regulator of liver fat metabolism influencing triglyceride secretion and hepatic lipid droplet content. Proc. Natl. Acad. Sci. USA. 2014;111:8913–8918. doi: 10.1073/pnas.1323785111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dongiovanni P., Valenti L., Rametta R., Daly A.K., Nobili V., Mozzi E., Leathart J.B., Pietrobattista A., Burt A.D., Maggioni M., et al. Genetic variants regulating insulin receptor signalling are associated with the severity of liver damage in patients with non-alcoholic fatty liver disease. Gut. 2010;59:267–273. doi: 10.1136/gut.2009.190801. [DOI] [PubMed] [Google Scholar]
- 33.Beer N.L., Tribble N.D., McCulloch L.J., Roos C., Johnson P.R., Orho-Melander M., Gloyn A.L. The P446L variant in GCKR associated with fasting plasma glucose and triglyceride levels exerts its effect through increased glucokinase activity in liver. Hum. Mol. Genet. 2009;18:4081–4088. doi: 10.1093/hmg/ddp357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Santoro N., Zhang C.K., Zhao H., Pakstis A.J., Kim G., Kursawe R., Dykas D.J., Bale A.E., Giannini C., Pierpont B., et al. Variant in the glucokinase regulatory protein (GCKR) gene is associated with fatty liver in obese children and adolescents. Hepatology. 2012;55:781–789. doi: 10.1002/hep.24806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tonjes A., Scholz M., Loeffler M., Stumvoll M. Association of Pro12Ala polymorphism in peroxisome proliferator-activated receptor γ with pre-diabetic phenotypes: Meta-analysis of 57 studies on nondiabetic individuals. Diabetes Care. 2006;29:2489–2497. doi: 10.2337/dc06-0513. [DOI] [PubMed] [Google Scholar]
- 36.Nelson J.E., Bhattacharya R., Lindor K.D., Chalasani N., Raaka S., Heathcote E.J., Miskovsky E., Shaffer E., Rulyak S.J., Kowdley K.V. HFE C282Y mutations are associated with advanced hepatic fibrosis in caucasians with nonalcoholic steatohepatitis. Hepatology. 2007;46:723–729. doi: 10.1002/hep.21742. [DOI] [PubMed] [Google Scholar]
- 37.Bugianesi E., Manzini P., D’Antico S., Vanni E., Longo F., Leone N., Massarenti P., Piga A., Marchesini G., Rizzetto M. Relative contribution of iron burden, HFE mutations, and insulin resistance to fibrosis in nonalcoholic fatty liver. Hepatology. 2004;39:179–187. doi: 10.1002/hep.20023. [DOI] [PubMed] [Google Scholar]
- 38.Valenti L., Fracanzani A.L., Bugianesi E., Dongiovanni P., Galmozzi E., Vanni E., Canavesi E., Lattuada E., Roviaro G., Marchesini G., et al. HFE genotype, parenchymal iron accumulation, and liver fibrosis in patients with nonalcoholic fatty liver disease. Gastroenterology. 2010;138:905–912. doi: 10.1053/j.gastro.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 39.Raszeja-Wyszomirska J., Kurzawski G., Lawniczak M., Miezynska-Kurtycz J., Lubinski J. Nonalcoholic fatty liver disease and HFE gene mutations: A polish study. World J. Gastroenterol. 2010;16:2531–2536. doi: 10.3748/wjg.v16.i20.2531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Al-Serri A., Anstee Q.M., Valenti L., Nobili V., Leathart J.B., Dongiovanni P., Patch J., Fracanzani A., Fargion S., Day C.P., et al. The SOD2 C47T polymorphism influences NAFLD fibrosis severity: Evidence from case-control and intra-familial allele association studies. J. Hepatol. 2012;56:448–454. doi: 10.1016/j.jhep.2011.05.029. [DOI] [PubMed] [Google Scholar]
- 41.Mancina R.M., Dongiovanni P., Petta S., Pingitore P., Meroni M., Rametta R., Boren J., Montalcini T., Pujia A., Wiklund O., et al. The MBOAT7-TMC4 variant rs641738 increases risk of nonalcoholic fatty liver disease in individuals of European descent. Gastroenterology. 2016;150:1219–1230. doi: 10.1053/j.gastro.2016.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sun C., Fan J.G., Qiao L. Potential epigenetic mechanism in non-alcoholic fatty liver disease. Int. J. Mol. Sci. 2015;16:5161–5179. doi: 10.3390/ijms16035161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang L.J., Zhang H.W., Zhou J.Y., Liu Y., Yang Y., Chen X.L., Zhu C.H., Zheng R.D., Ling W.H., Zhu H.L. Betaine attenuates hepatic steatosis by reducing methylation of the MTTP promoter and elevating genomic methylation in mice fed a high-fat diet. J. Nutr. Biochem. 2014;25:329–336. doi: 10.1016/j.jnutbio.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 44.Iacobazzi V., Castegna A., Infantino V., Andria G. Mitochondrial DNA methylation as a next-generation biomarker and diagnostic tool. Mol. Genet. Metab. 2013;110:25–34. doi: 10.1016/j.ymgme.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 45.Tryndyak V.P., Han T., Muskhelishvili L., Fuscoe J.C., Ross S.A., Beland F.A., Pogribny I.P. Coupling global methylation and gene expression profiles reveal key pathophysiological events in liver injury induced by a methyl-deficient diet. Mol. Nutr. Food Res. 2011;55:411–418. doi: 10.1002/mnfr.201000300. [DOI] [PubMed] [Google Scholar]
- 46.Kalhan S.C., Edmison J., Marczewski S., Dasarathy S., Gruca L.L., Bennett C., Duenas C., Lopez R. Methionine and protein metabolism in non-alcoholic steatohepatitis: Evidence for lower rate of transmethylation of methionine. Clin. Sci. 2011;121:179–189. doi: 10.1042/CS20110060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zivkovic A.M., Bruce German J., Esfandiari F., Halsted C.H. Quantitative lipid metabolomic changes in alcoholic micropigs with fatty liver disease. Alcohol. Clin. Exp. Res. 2009;33:751–758. doi: 10.1111/j.1530-0277.2008.00892.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cordero P., Campion J., Milagro F.I., Martinez J.A. Transcriptomic and epigenetic changes in early liver steatosis associated to obesity: Effect of dietary methyl donor supplementation. Mol. Genet. Metab. 2013;110:388–395. doi: 10.1016/j.ymgme.2013.08.022. [DOI] [PubMed] [Google Scholar]
- 49.Sookoian S., Rosselli M.S., Gemma C., Burgueno A.L., Fernandez Gianotti T., Castano G.O., Pirola C.J. Epigenetic regulation of insulin resistance in nonalcoholic fatty liver disease: Impact of liver methylation of the peroxisome proliferator-activated receptor γ coactivator 1α promoter. Hepatology. 2010;52:1992–2000. doi: 10.1002/hep.23927. [DOI] [PubMed] [Google Scholar]
- 50.Wolff G.L., Kodell R.L., Moore S.R., Cooney C.A. Maternal epigenetics and methyl supplements affect agouti gene expression in Avy/a mice. FASEB J. 1998;12:949–957. [PubMed] [Google Scholar]
- 51.Pruis M.G., Lendvai A., Bloks V.W., Zwier M.V., Baller J.F., de Bruin A., Groen A.K., Plosch T. Maternal western diet primes non-alcoholic fatty liver disease in adult mouse offspring. Acta Physiol. 2014;210:215–227. doi: 10.1111/apha.12197. [DOI] [PubMed] [Google Scholar]
- 52.Chen G., Broseus J., Hergalant S., Donnart A., Chevalier C., Bolanos-Jimenez F., Gueant J.L., Houlgatte R. Identification of master genes involved in liver key functions through transcriptomics and epigenomics of methyl donor deficiency in rat: Relevance to nonalcoholic liver disease. Mol. Nutr. Food Res. 2015;59:293–302. doi: 10.1002/mnfr.201400483. [DOI] [PubMed] [Google Scholar]
- 53.Carabelli J., Burgueno A.L., Rosselli M.S., Gianotti T.F., Lago N.R., Pirola C.J., Sookoian S. High fat diet-induced liver steatosis promotes an increase in liver mitochondrial biogenesis in response to hypoxia. J. Cell. Mol. Med. 2011;15:1329–1338. doi: 10.1111/j.1582-4934.2010.01128.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pirola C.J., Gianotti T.F., Burgueno A.L., Rey-Funes M., Loidl C.F., Mallardi P., Martino J.S., Castano G.O., Sookoian S. Epigenetic modification of liver mitochondrial DNA is associated with histological severity of nonalcoholic fatty liver disease. Gut. 2013;62:1356–1363. doi: 10.1136/gutjnl-2012-302962. [DOI] [PubMed] [Google Scholar]
- 55.Aagaard-Tillery K.M., Grove K., Bishop J., Ke X., Fu Q., McKnight R., Lane R.H. Developmental origins of disease and determinants of chromatin structure: Maternal diet modifies the primate fetal epigenome. J. Mol. Endocrinol. 2008;41:91–102. doi: 10.1677/JME-08-0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bricambert J., Miranda J., Benhamed F., Girard J., Postic C., Dentin R. Salt-inducible kinase 2 links transcriptional coactivator p300 phosphorylation to the prevention of ChREBP-dependent hepatic steatosis in mice. J. Clin. Investig. 2010;120:4316–4331. doi: 10.1172/JCI41624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jun H.J., Kim J., Hoang M.H., Lee S.J. Hepatic lipid accumulation alters global histone H3 Lysine 9 and 4 trimethylation in the peroxisome proliferator-activated receptor α network. PLoS ONE. 2012;7:1575. doi: 10.1371/annotation/eff6e471-306a-41bd-88e3-13857af094af. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li J., Huang J., Li J.S., Chen H., Huang K., Zheng L. Accumulation of endoplasmic reticulum stress and lipogenesis in the liver through generational effects of high fat diets. J. Hepatol. 2012;56:900–907. doi: 10.1016/j.jhep.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 59.Colak Y., Yesil A., Mutlu H.H., Caklili O.T., Ulasoglu C., Senates E., Takir M., Kostek O., Yilmaz Y., Yilmaz Enc F., et al. A potential treatment of non-alcoholic fatty liver disease with SIRT1 activators. J. Gastrointest. Liver Dis. 2014;23:311–319. doi: 10.15403/jgld.2014.1121.233.yck. [DOI] [PubMed] [Google Scholar]
- 60.Colak Y., Ozturk O., Senates E., Tuncer I., Yorulmaz E., Adali G., Doganay L., Enc F.Y. SIRT1 as a potential therapeutic target for treatment of nonalcoholic fatty liver disease. Med. Sci. Monit. 2011;17:HY5–HY9. doi: 10.12659/MSM.881749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Suter M.A., Chen A., Burdine M.S., Choudhury M., Harris R.A., Lane R.H., Friedman J.E., Grove K.L., Tackett A.J., Aagaard K.M. A maternal high-fat diet modulates fetal SIRT1 histone and protein deacetylase activity in nonhuman primates. FASEB J. 2012;26:5106–5114. doi: 10.1096/fj.12-212878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hirschey M.D., Shimazu T., Jing E., Grueter C.A., Collins A.M., Aouizerat B., Stancakova A., Goetzman E., Lam M.M., Schwer B., et al. SIRT3 deficiency and mitochondrial protein hyperacetylation accelerate the development of the metabolic syndrome. Mol. Cell. 2011;44:177–190. doi: 10.1016/j.molcel.2011.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rottiers V., Naar A.M. MicroRNAs in metabolism and metabolic disorders. Nat. Rev. Mol. Cell Biol. 2012;13:239–250. doi: 10.1038/nrm3313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Williams M.D., Mitchell G.M. MicroRNAs in insulin resistance and obesity. Exp. Diabetes Res. 2012;2012 doi: 10.1155/2012/484696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ferreira D.M., Simao A.L., Rodrigues C.M., Castro R.E. Revisiting the metabolic syndrome and paving the way for microRNAs in non-alcoholic fatty liver disease. FEBS J. 2014;281:2503–2524. doi: 10.1111/febs.12806. [DOI] [PubMed] [Google Scholar]
- 66.Cheung O., Puri P., Eicken C., Contos M.J., Mirshahi F., Maher J.W., Kellum J.M., Min H., Luketic V.A., Sanyal A.J. Nonalcoholic steatohepatitis is associated with altered hepatic MicroRNA expression. Hepatology. 2008;48:1810–1820. doi: 10.1002/hep.22569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Castro R.E., Ferreira D.M., Afonso M.B., Borralho P.M., Machado M.V., Cortez-Pinto H., Rodrigues C.M. miR-34a/SIRT1/p53 is suppressed by ursodeoxycholic acid in the rat liver and activated by disease severity in human non-alcoholic fatty liver disease. J. Hepatol. 2013;58:119–125. doi: 10.1016/j.jhep.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 68.Li T., Francl J.M., Boehme S., Chiang J.Y. Regulation of cholesterol and bile acid homeostasis by the cholesterol 7α-hydroxylase/steroid response element-binding protein 2/microRNA-33a axis in mice. Hepatology. 2013;58:1111–1121. doi: 10.1002/hep.26427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Guo Y., Xiong Y., Sheng Q., Zhao S., Wattacheril J., Flynn C.R. A micro-RNA expression signature for human NAFLD progression. J. Gastroenterol. 2016 doi: 10.1007/s00535-016-1178-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Soronen J., Yki-Jarvinen H., Zhou Y., Sadevirta S., Sarin A.P., Leivonen M., Sevastianova K., Perttila J., Laurila P.P., Sigruener A., et al. Novel hepatic microRNAs upregulated in human nonalcoholic fatty liver disease. Physiol. Rep. 2016;4 doi: 10.14814/phy2.12661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Esau C., Davis S., Murray S.F., Yu X.X., Pandey S.K., Pear M., Watts L., Booten S.L., Graham M., McKay R., et al. miR-122 regulation of lipid metabolism revealed by in vivo antisense targeting. Cell Metab. 2006;3:87–98. doi: 10.1016/j.cmet.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 72.Li Z., Xu G., Qin Y., Zhang C., Tang H., Yin Y., Xiang X., Li Y., Zhao J., Mulholland M., et al. Ghrelin promotes hepatic lipogenesis by activation of mtor-PPARγ signaling pathway. Proc. Natl. Acad. Sci. USA. 2014;111:13163–13168. doi: 10.1073/pnas.1411571111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Promrat K., Kleiner D.E., Niemeier H.M., Jackvony E., Kearns M., Wands J.R., Fava J.L., Wing R.R. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatology. 2010;51:121–129. doi: 10.1002/hep.23276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wong V.W., Chan R.S., Wong G.L., Cheung B.H., Chu W.C., Yeung D.K., Chim A.M., Lai J.W., Li L.S., Sea M.M., et al. Community-based lifestyle modification programme for non-alcoholic fatty liver disease: A randomized controlled trial. J. Hepatol. 2013;59:536–542. doi: 10.1016/j.jhep.2013.04.013. [DOI] [PubMed] [Google Scholar]
- 75.Charlton M., Krishnan A., Viker K., Sanderson S., Cazanave S., McConico A., Masuoko H., Gores G. Fast food diet mouse: Novel small animal model of nash with ballooning, progressive fibrosis, and high physiological fidelity to the human condition. Am. J. Physiol. Gastrointest. Liver Physiol. 2011;301:G825–G834. doi: 10.1152/ajpgi.00145.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Garbow J.R., Doherty J.M., Schugar R.C., Travers S., Weber M.L., Wentz A.E., Ezenwajiaku N., Cotter D.G., Brunt E.M., Crawford P.A. Hepatic steatosis, inflammation, and ER stress in mice maintained long term on a very low-carbohydrate ketogenic diet. Am. J. Physiol. Gastrointest. Liver Physiol. 2011;300:G956–G967. doi: 10.1152/ajpgi.00539.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Haas J.T., Miao J., Chanda D., Wang Y., Zhao E., Haas M.E., Hirschey M., Vaitheesvaran B., Farese R.V., Jr., Kurland I.J., et al. Hepatic insulin signaling is required for obesity-dependent expression of SREBP-1c mRNA but not for feeding-dependent expression. Cell Metab. 2012;15:873–884. doi: 10.1016/j.cmet.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Schmid A.I., Szendroedi J., Chmelik M., Krssak M., Moser E., Roden M. Liver ATP synthesis is lower and relates to insulin sensitivity in patients with type 2 diabetes. Diabetes Care. 2011;34:448–453. doi: 10.2337/dc10-1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lee A.H., Scapa E.F., Cohen D.E., Glimcher L.H. Regulation of hepatic lipogenesis by the transcription factor XBP1. Science. 2008;320:1492–1496. doi: 10.1126/science.1158042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nakagawa T., Hu H., Zharikov S., Tuttle K.R., Short R.A., Glushakova O., Ouyang X., Feig D.I., Block E.R., Herrera-Acosta J., et al. A causal role for uric acid in fructose-induced metabolic syndrome. Am. J. Physiol. Ren. Physiol. 2006;290:F625–F631. doi: 10.1152/ajprenal.00140.2005. [DOI] [PubMed] [Google Scholar]
- 81.Lanaspa M.A., Sanchez-Lozada L.G., Choi Y.J., Cicerchi C., Kanbay M., Roncal-Jimenez C.A., Ishimoto T., Li N., Marek G., Duranay M., et al. Uric acid induces hepatic steatosis by generation of mitochondrial oxidative stress: Potential role in fructose-dependent and -independent fatty liver. J. Biol. Chem. 2012;287:40732–40744. doi: 10.1074/jbc.M112.399899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lim J.S., Mietus-Snyder M., Valente A., Schwarz J.M., Lustig R.H. The role of fructose in the pathogenesis of NAFLD and the metabolic syndrome. Nat. Rev. Gastroenterol. Hepatol. 2010;7:251–264. doi: 10.1038/nrgastro.2010.41. [DOI] [PubMed] [Google Scholar]
- 83.Kohli R., Pan X., Malladi P., Wainwright M.S., Whitington P.F. Mitochondrial reactive oxygen species signal hepatocyte steatosis by regulating the phosphatidylinositol 3-kinase cell survival pathway. J. Biol. Chem. 2007;282:21327–21336. doi: 10.1074/jbc.M701759200. [DOI] [PubMed] [Google Scholar]
- 84.Ishimoto T., Lanaspa M.A., Rivard C.J., Roncal-Jimenez C.A., Orlicky D.J., Cicerchi C., McMahan R.H., Abdelmalek M.F., Rosen H.R., Jackman M.R., et al. High-fat and high-sucrose (western) diet induces steatohepatitis that is dependent on fructokinase. Hepatology. 2013;58:1632–1643. doi: 10.1002/hep.26594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ohashi K., Munetsuna E., Yamada H., Ando Y., Yamazaki M., Taromaru N., Nagura A., Ishikawa H., Suzuki K., Teradaira R., et al. High fructose consumption induces DNA methylation at PPARα and CPT1A promoter regions in the rat liver. Biochem. Biophys. Res. Commun. 2015;468:185–189. doi: 10.1016/j.bbrc.2015.10.134. [DOI] [PubMed] [Google Scholar]
- 86.Yamazaki M., Munetsuna E., Yamada H., Ando Y., Mizuno G., Murase Y., Kondo K., Ishikawa H., Teradaira R., Suzuki K., et al. Fructose consumption induces hypomethylation of hepatic mitochondrial DNA in rats. Life Sci. 2016;149:146–152. doi: 10.1016/j.lfs.2016.02.020. [DOI] [PubMed] [Google Scholar]
- 87.Handa P., Morgan-Stevenson V., Maliken B.D., Nelson J.E., Washington S., Westerman M., Yeh M.M., Kowdley K.V. Iron overload results in hepatic oxidative stress, immune cell activation, and hepatocellular ballooning injury, leading to nonalcoholic steatohepatitis in genetically obese mice. Am. J. Physiol. Gastrointest. Liver Physiol. 2016;310:G117–G127. doi: 10.1152/ajpgi.00246.2015. [DOI] [PubMed] [Google Scholar]
- 88.Tallino S., Duffy M., Ralle M., Cortes M.P., Latorre M., Burkhead J.L. Nutrigenomics analysis reveals that copper deficiency and dietary sucrose up-regulate inflammation, fibrosis and lipogenic pathways in a mature rat model of nonalcoholic fatty liver disease. J. Nutr. Biochem. 2015;26:996–1006. doi: 10.1016/j.jnutbio.2015.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Peverill W., Powell L.W., Skoien R. Evolving concepts in the pathogenesis of nash: Beyond steatosis and inflammation. Int. J. Mol. Sci. 2014;15:8591–8638. doi: 10.3390/ijms15058591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Puri P., Mirshahi F., Cheung O., Natarajan R., Maher J.W., Kellum J.M., Sanyal A.J. Activation and dysregulation of the unfolded protein response in nonalcoholic fatty liver disease. Gastroenterology. 2008;134:568–576. doi: 10.1053/j.gastro.2007.10.039. [DOI] [PubMed] [Google Scholar]
- 91.Tandra S., Yeh M.M., Brunt E.M., Vuppalanchi R., Cummings O.W., Unalp-Arida A., Wilson L.A., Chalasani N., Network N.C.R. Presence and significance of microvesicular steatosis in nonalcoholic fatty liver disease. J. Hepatol. 2011;55:654–659. doi: 10.1016/j.jhep.2010.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Leamy A.K., Egnatchik R.A., Young J.D. Molecular mechanisms and the role of saturated fatty acids in the progression of non-alcoholic fatty liver disease. Prog. Lipid Res. 2013;52:165–174. doi: 10.1016/j.plipres.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cheung O., Sanyal A.J. Abnormalities of lipid metabolism in nonalcoholic fatty liver disease. Semin. Liver Dis. 2008;28:351–359. doi: 10.1055/s-0028-1091979. [DOI] [PubMed] [Google Scholar]
- 94.Alkhouri N., Dixon L.J., Feldstein A.E. Lipotoxicity in nonalcoholic fatty liver disease: Not all lipids are created equal. Expert Rev. Gastroenterol. Hepatol. 2009;3:445–451. doi: 10.1586/egh.09.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Pagadala M., Kasumov T., McCullough A.J., Zein N.N., Kirwan J.P. Role of ceramides in nonalcoholic fatty liver disease. Trends Endocrinol. Metab. 2012;23:365–371. doi: 10.1016/j.tem.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Brenner C., Galluzzi L., Kepp O., Kroemer G. Decoding cell death signals in liver inflammation. J. Hepatol. 2013;59:583–594. doi: 10.1016/j.jhep.2013.03.033. [DOI] [PubMed] [Google Scholar]
- 97.Chaurasia B., Summers S.A. Ceramides—Lipotoxic inducers of metabolic disorders. Trends Endocrinol. Metab. 2015;26:538–550. doi: 10.1016/j.tem.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 98.Yamaguchi K., Yang L., McCall S., Huang J., Yu X.X., Pandey S.K., Bhanot S., Monia B.P., Li Y.X., Diehl A.M. Inhibiting triglyceride synthesis improves hepatic steatosis but exacerbates liver damage and fibrosis in obese mice with nonalcoholic steatohepatitis. Hepatology. 2007;45:1366–1374. doi: 10.1002/hep.21655. [DOI] [PubMed] [Google Scholar]
- 99.McClain C.J., Barve S., Deaciuc I. Good fat/bad fat. Hepatology. 2007;45:1343–1346. doi: 10.1002/hep.21788. [DOI] [PubMed] [Google Scholar]
- 100.Sanyal A.J. Reply: To PMID 24818764. Gastroenterology. 2015;148:262–263. doi: 10.1053/j.gastro.2014.11.030. [DOI] [PubMed] [Google Scholar]
- 101.Provenzano A., Milani S., Vizzutti F., Delogu W., Navari N., Novo E., Maggiora M., Maurino V., Laffi G., Parola M., et al. N-3 polyunsaturated fatty acids worsen inflammation and fibrosis in experimental nonalcoholic steatohepatitis. Liver Int. 2014;34:918–930. doi: 10.1111/liv.12500. [DOI] [PubMed] [Google Scholar]
- 102.Puri P., Baillie R.A., Wiest M.M., Mirshahi F., Choudhury J., Cheung O., Sargeant C., Contos M.J., Sanyal A.J. A lipidomic analysis of nonalcoholic fatty liver disease. Hepatology. 2007;46:1081–1090. doi: 10.1002/hep.21763. [DOI] [PubMed] [Google Scholar]
- 103.Caballero F., Fernandez A., De Lacy A.M., Fernandez-Checa J.C., Caballeria J., Garcia-Ruiz C. Enhanced free cholesterol, SREBP-2 and star expression in human nash. J. Hepatol. 2009;50:789–796. doi: 10.1016/j.jhep.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 104.Mari M., Caballero F., Colell A., Morales A., Caballeria J., Fernandez A., Enrich C., Fernandez-Checa J.C., Garcia-Ruiz C. Mitochondrial free cholesterol loading sensitizes to TNF- and FAS-mediated steatohepatitis. Cell Metab. 2006;4:185–198. doi: 10.1016/j.cmet.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 105.Savard C., Tartaglione E.V., Kuver R., Haigh W.G., Farrell G.C., Subramanian S., Chait A., Yeh M.M., Quinn L.S., Ioannou G.N. Synergistic interaction of dietary cholesterol and dietary fat in inducing experimental steatohepatitis. Hepatology. 2013;57:81–92. doi: 10.1002/hep.25789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Van Rooyen D.M., Larter C.Z., Haigh W.G., Yeh M.M., Ioannou G., Kuver R., Lee S.P., Teoh N.C., Farrell G.C. Hepatic free cholesterol accumulates in obese, diabetic mice and causes nonalcoholic steatohepatitis. Gastroenterology. 2011;141:1393–1403. doi: 10.1053/j.gastro.2011.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wouters K., van Gorp P.J., Bieghs V., Gijbels M.J., Duimel H., Lutjohann D., Kerksiek A., van Kruchten R., Maeda N., Staels B., et al. Dietary cholesterol, rather than liver steatosis, leads to hepatic inflammation in hyperlipidemic mouse models of nonalcoholic steatohepatitis. Hepatology. 2008;48:474–486. doi: 10.1002/hep.22363. [DOI] [PubMed] [Google Scholar]
- 108.Min H.K., Kapoor A., Fuchs M., Mirshahi F., Zhou H., Maher J., Kellum J., Warnick R., Contos M.J., Sanyal A.J. Increased hepatic synthesis and dysregulation of cholesterol metabolism is associated with the severity of nonalcoholic fatty liver disease. Cell Metab. 2012;15:665–674. doi: 10.1016/j.cmet.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Simonen P., Kotronen A., Hallikainen M., Sevastianova K., Makkonen J., Hakkarainen A., Lundbom N., Miettinen T.A., Gylling H., Yki-Jarvinen H. Cholesterol synthesis is increased and absorption decreased in non-alcoholic fatty liver disease independent of obesity. J. Hepatol. 2011;54:153–159. doi: 10.1016/j.jhep.2010.05.037. [DOI] [PubMed] [Google Scholar]
- 110.Cortes V.A., Busso D., Maiz A., Arteaga A., Nervi F., Rigotti A. Physiological and pathological implications of cholesterol. Front. Biosci. 2014;19:416–428. doi: 10.2741/4216. [DOI] [PubMed] [Google Scholar]
- 111.Walenbergh S.M., Koek G.H., Bieghs V., Shiri-Sverdlov R. Non-alcoholic steatohepatitis: The role of oxidized low-density lipoproteins. J. Hepatol. 2013;58:801–810. doi: 10.1016/j.jhep.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 112.Hendrikx T., Walenbergh S.M., Hofker M.H., Shiri-Sverdlov R. Lysosomal cholesterol accumulation: Driver on the road to inflammation during atherosclerosis and non-alcoholic steatohepatitis. Obes. Rev. 2014;15:424–433. doi: 10.1111/obr.12159. [DOI] [PubMed] [Google Scholar]
- 113.Tomita K., Teratani T., Suzuki T., Shimizu M., Sato H., Narimatsu K., Okada Y., Kurihara C., Irie R., Yokoyama H., et al. Free cholesterol accumulation in hepatic stellate cells: Mechanism of liver fibrosis aggravation in nonalcoholic steatohepatitis in mice. Hepatology. 2014;59:154–169. doi: 10.1002/hep.26604. [DOI] [PubMed] [Google Scholar]
- 114.Chalasani N., Younossi Z., Lavine J.E., Diehl A.M., Brunt E.M., Cusi K., Charlton M., Sanyal A.J. The diagnosis and management of non-alcoholic fatty liver disease: Practice guideline by the American association for the study of liver diseases, American college of gastroenterology, and the American gastroenterological association. Hepatology. 2012;55:2005–2023. doi: 10.1002/hep.25762. [DOI] [PubMed] [Google Scholar]
- 115.Spolding B., Connor T., Wittmer C., Abreu L.L., Kaspi A., Ziemann M., Kaur G., Cooper A., Morrison S., Lee S., et al. Rapid development of non-alcoholic steatohepatitis in psammomys obesus (Israeli Sand Rat) PLoS ONE. 2014;9:1575. doi: 10.1371/journal.pone.0092656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Bellanti F., Mitarotonda D., Tamborra R., Blonda M., Iannelli G., Petrella A., Sanginario V., Iuliano L., Vendemiale G., Serviddio G. Oxysterols induce mitochondrial impairment and hepatocellular toxicity in non-alcoholic fatty liver disease. Free Radic. Biol. Med. 2014;75:S16–S17. doi: 10.1016/j.freeradbiomed.2014.10.594. [DOI] [PubMed] [Google Scholar]
- 117.Tall A.R., Yvan-Charvet L. Cholesterol, inflammation and innate immunity. Nat. Rev. Immunol. 2015;15:104–116. doi: 10.1038/nri3793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Chung S., Cuffe H., Marshall S.M., McDaniel A.L., Ha J.H., Kavanagh K., Hong C., Tontonoz P., Temel R.E., Parks J.S. Dietary cholesterol promotes adipocyte hypertrophy and adipose tissue inflammation in visceral, but not in subcutaneous, fat in monkeys. Arterioscler. Thromb. Vasc. Biol. 2014;34:1880–1887. doi: 10.1161/ATVBAHA.114.303896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Serviddio G., Bellanti F., Vendemiale G., Altomare E. Mitochondrial dysfunction in nonalcoholic steatohepatitis. Expert Rev. Gastroenterol. Hepatol. 2011;5:233–244. doi: 10.1586/egh.11.11. [DOI] [PubMed] [Google Scholar]
- 120.Tessari P., Coracina A., Cosma A., Tiengo A. Hepatic lipid metabolism and non-alcoholic fatty liver disease. Nutr. Metab. Cardiovasc. Dis. 2009;19:291–302. doi: 10.1016/j.numecd.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 121.Nassir F., Ibdah J.A. Role of mitochondria in nonalcoholic fatty liver disease. Int. J. Mol. Sci. 2014;15:8713–8742. doi: 10.3390/ijms15058713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Mailloux R.J., Florian M., Chen Q., Yan J., Petrov I., Coughlan M.C., Laziyan M., Caldwell D., Lalande M., Patry D., et al. Exposure to a northern contaminant mixture (NCM) alters hepatic energy and lipid metabolism exacerbating hepatic steatosis in obese JCR rats. PLoS ONE. 2014;9:1575. doi: 10.1371/journal.pone.0106832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Martel C., Allouche M., Esposti D.D., Fanelli E., Boursier C., Henry C., Chopineau J., Calamita G., Kroemer G., Lemoine A., et al. Glycogen synthase kinase 3-mediated voltage-dependent anion channel phosphorylation controls outer mitochondrial membrane permeability during lipid accumulation. Hepatology. 2013;57:93–102. doi: 10.1002/hep.25967. [DOI] [PubMed] [Google Scholar]
- 124.Win S., Than T.A., Le B.H., Garcia-Ruiz C., Fernandez-Checa J.C., Kaplowitz N. Sab (Sh3bp5) dependence of JNK mediated inhibition of mitochondrial respiration in palmitic acid induced hepatocyte lipotoxicity. J. Hepatol. 2015;62:1367–1374. doi: 10.1016/j.jhep.2015.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Penke M., Larsen P.S., Schuster S., Dall M., Jensen B.A., Gorski T., Meusel A., Richter S., Vienberg S.G., Treebak J.T., et al. Hepatic nad salvage pathway is enhanced in mice on a high-fat diet. Mol. Cell. Endocrinol. 2015;412:65–72. doi: 10.1016/j.mce.2015.05.028. [DOI] [PubMed] [Google Scholar]
- 126.Gariani K., Menzies K.J., Ryu D., Wegner C.J., Wang X., Ropelle E.R., Moullan N., Zhang H., Perino A., Lemos V., et al. Eliciting the mitochondrial unfolded protein response by nicotinamide adenine dinucleotide repletion reverses fatty liver disease in mice. Hepatology. 2016;63:1190–1204. doi: 10.1002/hep.28245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bentinger M., Brismar K., Dallner G. The antioxidant role of coenzyme Q. Mitochondrion. 2007;7:S41–S50. doi: 10.1016/j.mito.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 128.Nowicka B., Kruk J. Occurrence, biosynthesis and function of isoprenoid quinones. Biochim. Biophys. Acta. 2010;1797:1587–1605. doi: 10.1016/j.bbabio.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 129.Laredj L.N., Licitra F., Puccio H.M. The molecular genetics of coenzyme Q biosynthesis in health and disease. Biochimie. 2014;100:78–87. doi: 10.1016/j.biochi.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 130.Bentinger M., Tekle M., Dallner G. Coenzyme Q—Biosynthesis and functions. Biochem. Biophys. Res. Commun. 2010;396:74–79. doi: 10.1016/j.bbrc.2010.02.147. [DOI] [PubMed] [Google Scholar]
- 131.Yesilova Z., Yaman H., Oktenli C., Ozcan A., Uygun A., Cakir E., Sanisoglu S.Y., Erdil A., Ates Y., Aslan M., et al. Systemic markers of lipid peroxidation and antioxidants in patients with nonalcoholic fatty liver disease. Am. J. Gastroenterol. 2005;100:850–855. doi: 10.1111/j.1572-0241.2005.41500.x. [DOI] [PubMed] [Google Scholar]
- 132.Huertas J.R., Battino M., Lenaz G., Mataix F.J. Changes in mitochondrial and microsomal rat liver coenzyme Q9 and Q10 content induced by dietary fat and endogenous lipid peroxidation. FEBS Lett. 1991;287:89–92. doi: 10.1016/0014-5793(91)80022-U. [DOI] [PubMed] [Google Scholar]
- 133.Bravo E., Palleschi S., Rossi B., Napolitano M., Tiano L., D’Amore E., Botham K.M. Coenzyme Q metabolism is disturbed in high fat diet-induced non-alcoholic fatty liver disease in rats. Int. J. Mol. Sci. 2012;13:1644–1657. doi: 10.3390/ijms13021644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Feldstein A.E., Werneburg N.W., Canbay A., Guicciardi M.E., Bronk S.F., Rydzewski R., Burgart L.J., Gores G.J. Free fatty acids promote hepatic lipotoxicity by stimulating TNF-α expression via a lysosomal pathway. Hepatology. 2004;40:185–194. doi: 10.1002/hep.20283. [DOI] [PubMed] [Google Scholar]
- 135.Aubert J., Begriche K., Knockaert L., Robin M.A., Fromenty B. Increased expression of cytochrome P450 2E1 in nonalcoholic fatty liver disease: Mechanisms and pathophysiological role. Clin. Res. Hepatol. Gastroenterol. 2011;35:630–637. doi: 10.1016/j.clinre.2011.04.015. [DOI] [PubMed] [Google Scholar]
- 136.Abdelmegeed M.A., Banerjee A., Yoo S.H., Jang S., Gonzalez F.J., Song B.J. Critical role of cytochrome P450 2E1 (CYP2E1) in the development of high fat-induced non-alcoholic steatohepatitis. J. Hepatol. 2012;57:860–866. doi: 10.1016/j.jhep.2012.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Guicciardi M.E., Malhi H., Mott J.L., Gores G.J. Apoptosis and necrosis in the liver. Compr. Physiol. 2013;3:977–1010. doi: 10.1002/cphy.c120020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hirsova P., Gores G.J. Death receptor-mediated cell death and proinflammatory signaling in nonalcoholic steatohepatitis. Cell. Mol. Gastroenterol. Hepatol. 2015;1:17–27. doi: 10.1016/j.jcmgh.2014.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Li J., McQuade T., Siemer A.B., Napetschnig J., Moriwaki K., Hsiao Y.S., Damko E., Moquin D., Walz T., McDermott A., et al. The RIP1/RIP3 necrosome forms a functional amyloid signaling complex required for programmed necrosis. Cell. 2012;150:339–350. doi: 10.1016/j.cell.2012.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Wang H., Sun L., Su L., Rizo J., Liu L., Wang L.F., Wang F.S., Wang X. Mixed lineage kinase domain-like protein MLKL causes necrotic membrane disruption upon phosphorylation by RIP3. Mol. Cell. 2014;54:133–146. doi: 10.1016/j.molcel.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 141.Zhang D.W., Shao J., Lin J., Zhang N., Lu B.J., Lin S.C., Dong M.Q., Han J. RIP3, an energy metabolism regulator that switches TNF-induced cell death from apoptosis to necrosis. Science. 2009;325:332–336. doi: 10.1126/science.1172308. [DOI] [PubMed] [Google Scholar]
- 142.Upton J.W., Kaiser W.J., Mocarski E.S. Virus inhibition of RIP3-dependent necrosis. Cell Host Microbe. 2010;7:302–313. doi: 10.1016/j.chom.2010.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Moujalled D.M., Cook W.D., Okamoto T., Murphy J., Lawlor K.E., Vince J.E., Vaux D.L. TNF can activate RIPK3 and cause programmed necrosis in the absence of RIPK1. Cell Death Dis. 2013;4 doi: 10.1038/cddis.2012.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Degterev A., Huang Z., Boyce M., Li Y., Jagtap P., Mizushima N., Cuny G.D., Mitchison T.J., Moskowitz M.A., Yuan J. Chemical inhibitor of nonapoptotic cell death with therapeutic potential for ischemic brain injury. Nat. Chem. Biol. 2005;1:112–119. doi: 10.1038/nchembio711. [DOI] [PubMed] [Google Scholar]
- 145.Zhao J., Jitkaew S., Cai Z., Choksi S., Li Q., Luo J., Liu Z.G. Mixed lineage kinase domain-like is a key receptor interacting protein 3 downstream component of TNF-induced necrosis. Proc. Natl. Acad. Sci. USA. 2012;109:5322–5327. doi: 10.1073/pnas.1200012109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Gautheron J., Vucur M., Reisinger F., Cardenas D.V., Roderburg C., Koppe C., Kreggenwinkel K., Schneider A.T., Bartneck M., Neumann U.P., et al. A positive feedback loop between RIP3 and JNK controls non-alcoholic steatohepatitis. EMBO Mol. Med. 2014;6:1062–1074. doi: 10.15252/emmm.201403856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Afonso M.B., Rodrigues P.M., Carvalho T., Caridade M., Borralho P., Cortez-Pinto H., Castro R.E., Rodrigues C.M. Necroptosis is a key pathogenic event in human and experimental murine models of non-alcoholic steatohepatitis. Clin. Sci. 2015;129:721–739. doi: 10.1042/CS20140732. [DOI] [PubMed] [Google Scholar]
- 148.Park S.W., Zhou Y., Lee J., Lu A., Sun C., Chung J., Ueki K., Ozcan U. The regulatory subunits of PI3K, p85α and p85β, interact with XBP-1 and increase its nuclear translocation. Nat. Med. 2010;16:429–437. doi: 10.1038/nm.2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Kapoor A., Sanyal A.J. Endoplasmic reticulum stress and the unfolded protein response. Clin. Liver Dis. 2009;13:581–590. doi: 10.1016/j.cld.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 150.Padilla A., Descorbeth M., Almeyda A.L., Payne K., de Leon M. Hyperglycemia magnifies Schwann cell dysfunction and cell death triggered by PA-induced lipotoxicity. Brain Res. 2011;1370:64–79. doi: 10.1016/j.brainres.2010.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Wei Y., Wang D., Topczewski F., Pagliassotti M.J. Saturated fatty acids induce endoplasmic reticulum stress and apoptosis independently of ceramide in liver cells. Am. J. Physiol. Endocrinol. Metab. 2006;291:E275–E281. doi: 10.1152/ajpendo.00644.2005. [DOI] [PubMed] [Google Scholar]
- 152.Fu S., Yang L., Li P., Hofmann O., Dicker L., Hide W., Lin X., Watkins S.M., Ivanov A.R., Hotamisligil G.S. Aberrant lipid metabolism disrupts calcium homeostasis causing liver endoplasmic reticulum stress in obesity. Nature. 2011;473:528–531. doi: 10.1038/nature09968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Arias-Loste M.T., Fabrega E., Lopez-Hoyos M., Crespo J. The crosstalk between hypoxia and innate immunity in the development of obesity-related nonalcoholic fatty liver disease. BioMed Res. Int. 2015;2015 doi: 10.1155/2015/319745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Qu A., Taylor M., Xue X., Matsubara T., Metzger D., Chambon P., Gonzalez F.J., Shah Y.M. Hypoxia-inducible transcription factor 2α promotes steatohepatitis through augmenting lipid accumulation, inflammation, and fibrosis. Hepatology. 2011;54:472–483. doi: 10.1002/hep.24400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Ye J., Gao Z., Yin J., He Q. Hypoxia is a potential risk factor for chronic inflammation and adiponectin reduction in adipose tissue of ob/ob and dietary obese mice. Am. J. Physiol. Endocrinol. Metab. 2007;293:E1118–E1128. doi: 10.1152/ajpendo.00435.2007. [DOI] [PubMed] [Google Scholar]
- 156.Hodson L. Adipose tissue oxygenation: Effects on metabolic function. Adipocyte. 2014;3:75–80. doi: 10.4161/adip.27114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Hodson L., Humphreys S.M., Karpe F., Frayn K.N. Metabolic signatures of human adipose tissue hypoxia in obesity. Diabetes. 2013;62:1417–1425. doi: 10.2337/db12-1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Eltzschig H.K., Carmeliet P. Hypoxia and inflammation. N. Engl. J. Med. 2011;364:656–665. doi: 10.1056/NEJMra0910283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Rius J., Guma M., Schachtrup C., Akassoglou K., Zinkernagel A.S., Nizet V., Johnson R.S., Haddad G.G., Karin M. NF-κB links innate immunity to the hypoxic response through transcriptional regulation of HIF-1α. Nature. 2008;453:807–811. doi: 10.1038/nature06905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kuhlicke J., Frick J.S., Morote-Garcia J.C., Rosenberger P., Eltzschig H.K. Hypoxia inducible factor (HIF)-1 coordinates induction of toll-like receptors TLR2 and TLR6 during hypoxia. PLoS ONE. 2007;2:1575. doi: 10.1371/journal.pone.0001364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kim S.Y., Choi Y.J., Joung S.M., Lee B.H., Jung Y.S., Lee J.Y. Hypoxic stress up-regulates the expression of toll-like receptor 4 in macrophages via hypoxia-inducible factor. Immunology. 2010;129:516–524. doi: 10.1111/j.1365-2567.2009.03203.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Aron-Wisnewsky J., Minville C., Tordjman J., Levy P., Bouillot J.L., Basdevant A., Bedossa P., Clement K., Pepin J.L. Chronic intermittent hypoxia is a major trigger for non-alcoholic fatty liver disease in morbid obese. J. Hepatol. 2012;56:225–233. doi: 10.1016/j.jhep.2011.04.022. [DOI] [PubMed] [Google Scholar]
- 163.Feldstein A.E., Canbay A., Angulo P., Taniai M., Burgart L.J., Lindor K.D., Gores G.J. Hepatocyte apoptosis and FAS expression are prominent features of human nonalcoholic steatohepatitis. Gastroenterology. 2003;125:437–443. doi: 10.1016/S0016-5085(03)00907-7. [DOI] [PubMed] [Google Scholar]
- 164.Idrissova L., Malhi H., Werneburg N.W., LeBrasseur N.K., Bronk S.F., Fingas C., Tchkonia T., Pirtskhalava T., White T.A., Stout M.B., et al. Trail receptor deletion in mice suppresses the inflammation of nutrient excess. J. Hepatol. 2015;62:1156–1163. doi: 10.1016/j.jhep.2014.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Lu M., Lawrence D.A., Marsters S., Acosta-Alvear D., Kimmig P., Mendez A.S., Paton A.W., Paton J.C., Walter P., Ashkenazi A. Opposing unfolded-protein-response signals converge on death receptor 5 to control apoptosis. Science. 2014;345:98–101. doi: 10.1126/science.1254312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Gadd V.L., Skoien R., Powell E.E., Fagan K.J., Winterford C., Horsfall L., Irvine K., Clouston A.D. The portal inflammatory infiltrate and ductular reaction in human nonalcoholic fatty liver disease. Hepatology. 2014;59:1393–1405. doi: 10.1002/hep.26937. [DOI] [PubMed] [Google Scholar]
- 167.Lanthier N. Targeting Kupffer cells in non-alcoholic fatty liver disease/non-alcoholic steatohepatitis: Why and how? World J. Hepatol. 2015;7:2184–2188. doi: 10.4254/wjh.v7.i19.2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Dixon L.J., Barnes M., Tang H., Pritchard M.T., Nagy L.E. Kupffer cells in the liver. Compr. Physiol. 2013;3:785–797. doi: 10.1002/cphy.c120026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Tacke F., Zimmermann H.W. Macrophage heterogeneity in liver injury and fibrosis. J. Hepatol. 2014;60:1090–1096. doi: 10.1016/j.jhep.2013.12.025. [DOI] [PubMed] [Google Scholar]
- 170.Marra F., Tacke F. Roles for chemokines in liver disease. Gastroenterology. 2014;147:577–594. doi: 10.1053/j.gastro.2014.06.043. [DOI] [PubMed] [Google Scholar]
- 171.Leroux A., Ferrere G., Godie V., Cailleux F., Renoud M.L., Gaudin F., Naveau S., Prevot S., Makhzami S., Perlemuter G., et al. Toxic lipids stored by Kupffer cells correlates with their pro-inflammatory phenotype at an early stage of steatohepatitis. J. Hepatol. 2012;57:141–149. doi: 10.1016/j.jhep.2012.02.028. [DOI] [PubMed] [Google Scholar]
- 172.Chinetti-Gbaguidi G., Staels B. Macrophage polarization in metabolic disorders: Functions and regulation. Curr. Opin. Lipidol. 2011;22:365–372. doi: 10.1097/MOL.0b013e32834a77b4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Xu R., Huang H., Zhang Z., Wang F.S. The role of neutrophils in the development of liver diseases. Cell. Mol. Immunol. 2014;11:224–231. doi: 10.1038/cmi.2014.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Ibusuki R., Uto H., Arima S., Mawatari S., Setoguchi Y., Iwashita Y., Hashimoto S., Maeda T., Tanoue S., Kanmura S., et al. Transgenic expression of human neutrophil peptide-1 enhances hepatic fibrosis in mice fed a choline-deficient, l-amino acid-defined diet. Liver Int. 2013;33:1549–1556. doi: 10.1111/liv.12203. [DOI] [PubMed] [Google Scholar]
- 175.Rensen S.S., Bieghs V., Xanthoulea S., Arfianti E., Bakker J.A., Shiri-Sverdlov R., Hofker M.H., Greve J.W., Buurman W.A. Neutrophil-derived myeloperoxidase aggravates non-alcoholic steatohepatitis in low-density lipoprotein receptor-deficient mice. PLoS ONE. 2012;7:1575. doi: 10.1371/journal.pone.0052411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Talukdar S., Oh da Y., Bandyopadhyay G., Li D., Xu J., McNelis J., Lu M., Li P., Yan Q., Zhu Y., et al. Neutrophils mediate insulin resistance in mice fed a high-fat diet through secreted elastase. Nat. Med. 2012;18:1407–1412. doi: 10.1038/nm.2885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Tacke F., Yoneyama H. From NAFLD to NASH to fibrosis to HCC: Role of dendritic cell populations in the liver. Hepatology. 2013;58:494–496. doi: 10.1002/hep.26405. [DOI] [PubMed] [Google Scholar]
- 178.Henning J.R., Graffeo C.S., Rehman A., Fallon N.C., Zambirinis C.P., Ochi A., Barilla R., Jamal M., Deutsch M., Greco S., et al. Dendritic cells limit fibroinflammatory injury in nonalcoholic steatohepatitis in mice. Hepatology. 2013;58:589–602. doi: 10.1002/hep.26267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Sutti S., Locatelli I., Bruzzi S., Jindal A., Vacchiano M., Bozzola C., Albano E. CX3CR1-expressing inflammatory dendritic cells contribute to the progression of steatohepatitis. Clin. Sci. 2015;129:797–808. doi: 10.1042/CS20150053. [DOI] [PubMed] [Google Scholar]
- 180.Ganz M., Szabo G. Immune and inflammatory pathways in NASH. Hepatol. Int. 2013;7:771–781. doi: 10.1007/s12072-013-9468-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Tian Z., Chen Y., Gao B. Natural killer cells in liver disease. Hepatology. 2013;57:1654–1662. doi: 10.1002/hep.26115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Kumar V. NKT-cell subsets: Promoters and protectors in inflammatory liver disease. J. Hepatol. 2013;59:618–620. doi: 10.1016/j.jhep.2013.02.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Martin-Murphy B.V., You Q., Wang H., De La Houssaye B.A., Reilly T.P., Friedman J.E., Ju C. Mice lacking natural killer T cell are more susceptible to metabolic alterations following high fat diet feeding. PLoS ONE. 2014;9:1575. doi: 10.1371/journal.pone.0080949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Kremer M., Thomas E., Milton R.J., Perry A.W., van Rooijen N., Wheeler M.D., Zacks S., Fried M., Rippe R.A., Hines I.N. Kupffer cell and interleukin-12-dependent loss of natural killer T cell in hepatosteatosis. Hepatology. 2010;51:130–141. doi: 10.1002/hep.23292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Syn W.K., Oo Y.H., Pereira T.A., Karaca G.F., Jung Y., Omenetti A., Witek R.P., Choi S.S., Guy C.D., Fearing C.M., et al. Accumulation of natural killer T cells in progressive nonalcoholic fatty liver disease. Hepatology. 2010;51:1998–2007. doi: 10.1002/hep.23599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Tajiri K., Shimizu Y. Role of NKT cells in the pathogenesis of NAFLD. Int. J. Hepatol. 2012;2012 doi: 10.1155/2012/850836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Guy C.D., Suzuki A., Zdanowicz M., Abdelmalek M.F., Burchette J., Unalp A., Diehl A.M., Nash C.R.N. Hedgehog pathway activation parallels histologic severity of injury and fibrosis in human nonalcoholic fatty liver disease. Hepatology. 2012;55:1711–1721. doi: 10.1002/hep.25559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Verdelho Machado M., Diehl A.M. Role of Hedgehog Signaling Pathway in NASH. Int. J. Mol. Sci. 2016;17 doi: 10.3390/ijms17060857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Moylan C.A., Pang H., Dellinger A., Suzuki A., Garrett M.E., Guy C.D., Murphy S.K., Ashley-Koch A.E., Choi S.S., Michelotti G.A., et al. Hepatic gene expression profiles differentiate presymptomatic patients with mild versus severe nonalcoholic fatty liver disease. Hepatology. 2014;59:471–482. doi: 10.1002/hep.26661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Kwon H., Song K., Han C., Chen W., Wang Y., Dash S., Lim K., Wu T. Inhibition of hedgehog signaling ameliorates hepatic inflammation in mice with nonalcoholic fatty liver disease. Hepatology. 2015;63:1155–1169. doi: 10.1002/hep.28289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Syn W.K., Choi S.S., Liaskou E., Karaca G.F., Agboola K.M., Oo Y.H., Mi Z., Pereira T.A., Zdanowicz M., Malladi P., et al. Osteopontin is induced by hedgehog pathway activation and promotes fibrosis progression in nonalcoholic steatohepatitis. Hepatology. 2011;53:106–115. doi: 10.1002/hep.23998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Machado M.V., Michelotti G.A., Pereira T., Boursier J., Swiderska-Syn M., Karaca G., Xie G., Guy C.D., Bohinc B., Lindblom K.R., et al. Reduced lipoapoptosis, hedgehog pathway activation and fibrosis in caspase-2 deficient mice with non-alcoholic steatohepatitis. Gut. 2015;64:1148–1157. doi: 10.1136/gutjnl-2014-307362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Machado M.V., Michelotti G.A., Pereira T.A., Xie G., Premont R., Cortez-Pinto H., Diehl A.M. Accumulation of duct cell with activated YAP parallels fibrosis progression in non-alcoholic fatty liver disease. J. Hepatol. 2015;63:962–970. doi: 10.1016/j.jhep.2015.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Guy C.D., Suzuki A., Abdelmalek M.F., Burchette J.L., Diehl A.M. Treatment response in the PIVENS trial is associated with decreased hedgehog pathway activity. Hepatology. 2015;61:98–107. doi: 10.1002/hep.27235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Evans R.M., Mangelsdorf D.J. Nuclear receptors, RXR, and the big bang. Cell. 2014;157:255–266. doi: 10.1016/j.cell.2014.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Fuchs C.D., Traussnigg S.A., Trauner M. Nuclear receptor modulation for the treatment of nonalcoholic fatty liver disease. Semin. Liver Dis. 2016;36:69–86. doi: 10.1055/s-0036-1571296. [DOI] [PubMed] [Google Scholar]
- 197.Tailleux A., Wouters K., Staels B. Roles of PPARs in NAFLD: Potential therapeutic targets. Biochim. Biophys. Acta. 2012;1821:809–818. doi: 10.1016/j.bbalip.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 198.Francque S., Verrijken A., Caron S., Prawitt J., Paumelle R., Derudas B., Lefebvre P., Taskinen M.R., Van Hul W., Mertens I., et al. PPARα gene expression correlates with severity and histological treatment response in patients with non-alcoholic steatohepatitis. J. Hepatol. 2015;63:164–173. doi: 10.1016/j.jhep.2015.02.019. [DOI] [PubMed] [Google Scholar]
- 199.Reddy J.K., Rao M.S. Lipid metabolism and liver inflammation. II. Fatty liver disease and fatty acid oxidation. Am. J. Physiol. Gastrointest. Liver Physiol. 2006;290:G852–G858. doi: 10.1152/ajpgi.00521.2005. [DOI] [PubMed] [Google Scholar]
- 200.Ip E., Farrell G., Hall P., Robertson G., Leclercq I. Administration of the potent PPARα agonist, Wy-14,643, reverses nutritional fibrosis and steatohepatitis in mice. Hepatology. 2004;39:1286–1296. doi: 10.1002/hep.20170. [DOI] [PubMed] [Google Scholar]
- 201.Shan W., Nicol C.J., Ito S., Bility M.T., Kennett M.J., Ward J.M., Gonzalez F.J., Peters J.M. Peroxisome proliferator-activated receptor-β/δ protects against chemically induced liver toxicity in mice. Hepatology. 2008;47:225–235. doi: 10.1002/hep.21925. [DOI] [PubMed] [Google Scholar]
- 202.Kawaguchi K., Sakaida I., Tsuchiya M., Omori K., Takami T., Okita K. Pioglitazone prevents hepatic steatosis, fibrosis, and enzyme-altered lesions in rat liver cirrhosis induced by a choline-deficient l-amino acid-defined diet. Biochem. Biophys. Res. Commun. 2004;315:187–195. doi: 10.1016/j.bbrc.2004.01.038. [DOI] [PubMed] [Google Scholar]
- 203.Stienstra R., Duval C., Muller M., Kersten S. PPARs, obesity, and inflammation. PPAR Res. 2007;2007 doi: 10.1155/2007/95974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Lutchman G., Modi A., Kleiner D.E., Promrat K., Heller T., Ghany M., Borg B., Loomba R., Liang T.J., Premkumar A., et al. The effects of discontinuing pioglitazone in patients with nonalcoholic steatohepatitis. Hepatology. 2007;46:424–429. doi: 10.1002/hep.21661. [DOI] [PubMed] [Google Scholar]
- 205.Yamada Y., Eto M., Ito Y., Mochizuki S., Son B.K., Ogawa S., Iijima K., Kaneki M., Kozaki K., Toba K., et al. Suppressive role of PPARγ-regulated endothelial nitric oxide synthase in adipocyte lipolysis. PLoS ONE. 2015;10:1575. doi: 10.1371/journal.pone.0136597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Ratziu V., Harrison S.A., Francque S., Bedossa P., Lehert P., Serfaty L., Romero-Gomez M., Boursier J., Abdelmalek M., Caldwell S., et al. Elafibranor, an agonist of the peroxisome proliferator-activated receptor-α and -β, induces resolution of nonalcoholic steatohepatitis without fibrosis worsening. Gastroenterology. 2016;150:1147–1159. doi: 10.1053/j.gastro.2016.01.038. [DOI] [PubMed] [Google Scholar]
- 207.Lamba V., Yasuda K., Lamba J.K., Assem M., Davila J., Strom S., Schuetz E.G. PXR (NR1I2): Splice variants in human tissues, including brain, and identification of neurosteroids and nicotine as PXR activators. Toxicol. Appl. Pharmacol. 2004;199:251–265. doi: 10.1016/j.taap.2003.12.027. [DOI] [PubMed] [Google Scholar]
- 208.Haughton E.L., Tucker S.J., Marek C.J., Durward E., Leel V., Bascal Z., Monaghan T., Koruth M., Collie-Duguid E., Mann D.A., et al. Pregnane X receptor activators inhibit human hepatic stellate cell transdifferentiation in vitro. Gastroenterology. 2006;131:194–209. doi: 10.1053/j.gastro.2006.04.012. [DOI] [PubMed] [Google Scholar]
- 209.Sookoian S., Castano G.O., Burgueno A.L., Gianotti T.F., Rosselli M.S., Pirola C.J. The nuclear receptor PXR gene variants are associated with liver injury in nonalcoholic fatty liver disease. Pharmacogenet. Genom. 2010;20:1–8. doi: 10.1097/FPC.0b013e328333a1dd. [DOI] [PubMed] [Google Scholar]
- 210.Breuker C., Planque C., Rajabi F., Nault J.C., Couchy G., Zucman-Rossi J., Evrard A., Kantar J., Chevet E., Bioulac-Sage P., et al. Characterization of a novel PXR isoform with potential dominant-negative properties. J. Hepatol. 2014;61:609–616. doi: 10.1016/j.jhep.2014.04.030. [DOI] [PubMed] [Google Scholar]
- 211.Monostory K., Dvorak Z. Steroid regulation of drug-metabolizing cytochromes P450. Curr. Drug Metab. 2011;12:154–172. doi: 10.2174/138920011795016854. [DOI] [PubMed] [Google Scholar]
- 212.Spruiell K., Richardson R.M., Cullen J.M., Awumey E.M., Gonzalez F.J., Gyamfi M.A. Role of pregnane X receptor in obesity and glucose homeostasis in male mice. J. Biol. Chem. 2014;289:3244–3261. doi: 10.1074/jbc.M113.494575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Li L., Li H., Garzel B., Yang H., Sueyoshi T., Li Q., Shu Y., Zhang J., Hu B., Heyward S., et al. SLC13A5 is a novel transcriptional target of the pregnane X receptor and sensitizes drug-induced steatosis in human liver. Mol. Pharmacol. 2015;87:674–682. doi: 10.1124/mol.114.097287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Sun M., Cui W., Woody S.K., Staudinger J.L. Pregnane X receptor modulates the inflammatory response in primary cultures of hepatocytes. Drug Metab. Dispos. 2015;43:335–343. doi: 10.1124/dmd.114.062307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Nishimura M., Naito S., Yokoi T. Tissue-specific MRNA expression profiles of human nuclear receptor subfamilies. Drug Metab. Pharmacokinet. 2004;19:135–149. doi: 10.2133/dmpk.19.135. [DOI] [PubMed] [Google Scholar]
- 216.Beilke L.D., Aleksunes L.M., Holland R.D., Besselsen D.G., Beger R.D., Klaassen C.D., Cherrington N.J. Constitutive androstane receptor-mediated changes in bile acid composition contributes to hepatoprotection from lithocholic acid-induced liver injury in mice. Drug Metab. Dispos. 2009;37:1035–1045. doi: 10.1124/dmd.108.023317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Fisher C.D., Lickteig A.J., Augustine L.M., Ranger-Moore J., Jackson J.P., Ferguson S.S., Cherrington N.J. Hepatic cytochrome P450 enzyme alterations in humans with progressive stages of nonalcoholic fatty liver disease. Drug Metab. Dispos. 2009;37:2087–2094. doi: 10.1124/dmd.109.027466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Gao J., He J., Zhai Y., Wada T., Xie W. The constitutive androstane receptor is an anti-obesity nuclear receptor that improves insulin sensitivity. J. Biol. Chem. 2009;284:25984–25992. doi: 10.1074/jbc.M109.016808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Sberna A.L., Assem M., Xiao R., Ayers S., Gautier T., Guiu B., Deckert V., Chevriaux A., Grober J., Le Guern N., et al. Constitutive androstane receptor activation decreases plasma apolipoprotein B-containing lipoproteins and atherosclerosis in low-density lipoprotein receptor-deficient mice. Arterioscler. Thromb. Vasc. Biol. 2011;31:2232–2239. doi: 10.1161/ATVBAHA.110.222497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Gao J., Yan J., Xu M., Ren S., Xie W. CAR suppresses hepatic gluconeogenesis by facilitating the ubiquitination and degradation of PGC1α. Mol. Endocrinol. 2015;29:1558–1570. doi: 10.1210/me.2015-1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Dong B., Lee J.S., Park Y.Y., Yang F., Xu G., Huang W., Finegold M.J., Moore D.D. Activating CAR and β-catenin induces uncontrolled liver growth and tumorigenesis. Nat. Commun. 2015;6 doi: 10.1038/ncomms6944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Li D., Mackowiak B., Brayman T.G., Mitchell M., Zhang L., Huang S.M., Wang H. Genome-wide analysis of human constitutive androstane receptor (CAR) transcriptome in wild-type and CAR-knockout HepaRG cells. Biochem. Pharmacol. 2015;98:190–202. doi: 10.1016/j.bcp.2015.08.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Kunne C., Acco A., Duijst S., de Waart D.R., Paulusma C.C., Gaemers I., Oude Elferink R.P. FXR-dependent reduction of hepatic steatosis in a bile salt deficient mouse model. Biochim. Biophys. Acta. 2014;1842:739–746. doi: 10.1016/j.bbadis.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 224.Pineda Torra I., Claudel T., Duval C., Kosykh V., Fruchart J.C., Staels B. Bile acids induce the expression of the human peroxisome proliferator-activated receptor α gene via activation of the farnesoid X receptor. Mol. Endocrinol. 2003;17:259–272. doi: 10.1210/me.2002-0120. [DOI] [PubMed] [Google Scholar]
- 225.Neuschwander-Tetri B.A., Loomba R., Sanyal A.J., Lavine J.E., van Natta M.L., Abdelmalek M.F., Chalasani N., Dasarathy S., Diehl A.M., Hameed B., et al. Farnesoid X nuclear receptor ligand obeticholic acid for non-cirrhotic, non-alcoholic steatohepatitis (FLINT): A multicentre, randomised, placebo-controlled trial. Lancet. 2015;385:956–965. doi: 10.1016/S0140-6736(14)61933-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Cipriani S., Mencarelli A., Palladino G., Fiorucci S. FXR activation reverses insulin resistance and lipid abnormalities and protects against liver steatosis in zucker (FA/FA) obese rats. J. Lipid Res. 2010;51:771–784. doi: 10.1194/jlr.M001602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Ma Y., Huang Y., Yan L., Gao M., Liu D. Synthetic FXR agonist GW4064 prevents diet-induced hepatic steatosis and insulin resistance. Pharm. Res. 2013;30:1447–1457. doi: 10.1007/s11095-013-0986-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Mudaliar S., Henry R.R., Sanyal A.J., Morrow L., Marschall H.U., Kipnes M., Adorini L., Sciacca C.I., Clopton P., Castelloe E., et al. Efficacy and safety of the farnesoid x receptor agonist obeticholic acid in patients with type 2 diabetes and nonalcoholic fatty liver disease. Gastroenterology. 2013;145:574–582. doi: 10.1053/j.gastro.2013.05.042. [DOI] [PubMed] [Google Scholar]
- 229.Jahn D., Rau M., Wohlfahrt J., Hermanns H.M., Geier A. Non-alcoholic steatohepatitis: From pathophysiology to novel therapies. Dig. Dis. 2016;34:356–363. doi: 10.1159/000444547. [DOI] [PubMed] [Google Scholar]
- 230.Tomlinson E., Fu L., John L., Hultgren B., Huang X., Renz M., Stephan J.P., Tsai S.P., Powell-Braxton L., French D., et al. Transgenic mice expressing human fibroblast growth factor-19 display increased metabolic rate and decreased adiposity. Endocrinology. 2002;143:1741–1747. doi: 10.1210/endo.143.5.8850. [DOI] [PubMed] [Google Scholar]
- 231.Fu L., John L.M., Adams S.H., Yu X.X., Tomlinson E., Renz M., Williams P.M., Soriano R., Corpuz R., Moffat B., et al. Fibroblast growth factor 19 increases metabolic rate and reverses dietary and leptin-deficient diabetes. Endocrinology. 2004;145:2594–2603. doi: 10.1210/en.2003-1671. [DOI] [PubMed] [Google Scholar]
- 232.Fang S., Suh J.M., Reilly S.M., Yu E., Osborn O., Lackey D., Yoshihara E., Perino A., Jacinto S., Lukasheva Y., et al. Intestinal FXR agonism promotes adipose tissue browning and reduces obesity and insulin resistance. Nat. Med. 2015;21:159–165. doi: 10.1038/nm.3760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Degirolamo C., Modica S., Vacca M., Di Tullio G., Morgano A., D’Orazio A., Kannisto K., Parini P., Moschetta A. Prevention of spontaneous hepatocarcinogenesis in farnesoid X receptor-null mice by intestinal-specific farnesoid x receptor reactivation. Hepatology. 2015;61:161–170. doi: 10.1002/hep.27274. [DOI] [PubMed] [Google Scholar]
- 234.Seki E., Brenner D.A. Toll-like receptors and adaptor molecules in liver disease: Update. Hepatology. 2008;48:322–335. doi: 10.1002/hep.22306. [DOI] [PubMed] [Google Scholar]
- 235.Strowig T., Henao-Mejia J., Elinav E., Flavell R. Inflammasomes in health and disease. Nature. 2012;481:278–286. doi: 10.1038/nature10759. [DOI] [PubMed] [Google Scholar]
- 236.Vanni E., Bugianesi E. The gut-liver axis in nonalcoholic fatty liver disease: Another pathway to insulin resistance? Hepatology. 2009;49:1790–1792. doi: 10.1002/hep.23036. [DOI] [PubMed] [Google Scholar]
- 237.Miele L., Valenza V., La Torre G., Montalto M., Cammarota G., Ricci R., Masciana R., Forgione A., Gabrieli M.L., Perotti G., et al. Increased intestinal permeability and tight junction alterations in nonalcoholic fatty liver disease. Hepatology. 2009;49:1877–1887. doi: 10.1002/hep.22848. [DOI] [PubMed] [Google Scholar]
- 238.Akira S., Uematsu S., Takeuchi O. Pathogen recognition and innate immunity. Cell. 2006;124:783–801. doi: 10.1016/j.cell.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 239.Raman M., Ahmed I., Gillevet P.M., Probert C.S., Ratcliffe N.M., Smith S., Greenwood R., Sikaroodi M., Lam V., Crotty P., et al. Fecal microbiome and volatile organic compound metabolome in obese humans with nonalcoholic fatty liver disease. Clin. Gastroenterol. Hepatol. 2013;11:868–875. doi: 10.1016/j.cgh.2013.02.015. [DOI] [PubMed] [Google Scholar]
- 240.Douhara A., Moriya K., Yoshiji H., Noguchi R., Namisaki T., Kitade M., Kaji K., Aihara Y., Nishimura N., Takeda K., et al. Reduction of endotoxin attenuates liver fibrosis through suppression of hepatic stellate cell activation and remission of intestinal permeability in a rat non-alcoholic steatohepatitis model. Mol. Med. Rep. 2015;11:1693–1700. doi: 10.3892/mmr.2014.2995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Ehses J.A., Meier D.T., Wueest S., Rytka J., Boller S., Wielinga P.Y., Schraenen A., Lemaire K., Debray S., van Lommel L., et al. Toll-like receptor 2-deficient mice are protected from insulin resistance and β cell dysfunction induced by a high-fat diet. Diabetologia. 2010;53:1795–1806. doi: 10.1007/s00125-010-1747-3. [DOI] [PubMed] [Google Scholar]
- 242.Vijay-Kumar M., Aitken J.D., Carvalho F.A., Cullender T.C., Mwangi S., Srinivasan S., Sitaraman S.V., Knight R., Ley R.E., Gewirtz A.T. Metabolic syndrome and altered gut microbiota in mice lacking toll-like receptor 5. Science. 2010;328:228–231. doi: 10.1126/science.1179721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Al-Daghri N.M., Clerici M., Al-Attas O., Forni D., Alokail M.S., Alkharfy K.M., Sabico S., Mohammed A.K., Cagliani R., Sironi M. A nonsense polymorphism (R392X) in TLR5 protects from obesity but predisposes to diabetes. J. Immunol. 2013;190:3716–3720. doi: 10.4049/jimmunol.1202936. [DOI] [PubMed] [Google Scholar]
- 244.Miura K., Kodama Y., Inokuchi S., Schnabl B., Aoyama T., Ohnishi H., Olefsky J.M., Brenner D.A., Seki E. Toll-like receptor 9 promotes steatohepatitis by induction of interleukin-1β in mice. Gastroenterology. 2010;139:323–334. doi: 10.1053/j.gastro.2010.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Gabele E., Dostert K., Hofmann C., Wiest R., Scholmerich J., Hellerbrand C., Obermeier F. DSS induced colitis increases portal LPS levels and enhances hepatic inflammation and fibrogenesis in experimental NASH. J. Hepatol. 2011;55:1391–1399. doi: 10.1016/j.jhep.2011.02.035. [DOI] [PubMed] [Google Scholar]
- 246.Csak T., Velayudham A., Hritz I., Petrasek J., Levin I., Lippai D., Catalano D., Mandrekar P., Dolganiuc A., Kurt-Jones E., et al. Deficiency in myeloid differentiation factor-2 and toll-like receptor 4 expression attenuates nonalcoholic steatohepatitis and fibrosis in mice. Am. J. Physiol. Gastrointest. Liver Physiol. 2011;300:G433–G441. doi: 10.1152/ajpgi.00163.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Dolganiuc A., Norkina O., Kodys K., Catalano D., Bakis G., Marshall C., Mandrekar P., Szabo G. Viral and host factors induce macrophage activation and loss of toll-like receptor tolerance in chronic HCV infection. Gastroenterology. 2007;133:1627–1636. doi: 10.1053/j.gastro.2007.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Beutler B. Inferences, questions and possibilities in toll-like receptor signalling. Nature. 2004;430:257–263. doi: 10.1038/nature02761. [DOI] [PubMed] [Google Scholar]
- 249.Kawasaki T., Kawai T. Toll-like receptor signaling pathways. Front. Immunol. 2014;5 doi: 10.3389/fimmu.2014.00461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Guo J., Friedman S.L. Toll-like receptor 4 signaling in liver injury and hepatic fibrogenesis. Fibrogenes. Tissue Repair. 2010;3 doi: 10.1186/1755-1536-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Ye D., Li F.Y., Lam K.S., Li H., Jia W., Wang Y., Man K., Lo C.M., Li X., Xu A. Toll-like receptor-4 mediates obesity-induced non-alcoholic steatohepatitis through activation of X-box binding protein-1 in mice. Gut. 2012;61:1058–1067. doi: 10.1136/gutjnl-2011-300269. [DOI] [PubMed] [Google Scholar]
- 252.Rivera C.A., Adegboyega P., van Rooijen N., Tagalicud A., Allman M., Wallace M. Toll-like receptor-4 signaling and Kupffer cells play pivotal roles in the pathogenesis of non-alcoholic steatohepatitis. J. Hepatol. 2007;47:571–579. doi: 10.1016/j.jhep.2007.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Szabo G., Bala S. Alcoholic liver disease and the gut-liver axis. World J. Gastroenterol. 2010;16:1321–1329. doi: 10.3748/wjg.v16.i11.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Seki E., de Minicis S., Osterreicher C.H., Kluwe J., Osawa Y., Brenner D.A., Schwabe R.F. TLR4 enhances TGF-β signaling and hepatic fibrosis. Nat. Med. 2007;13:1324–1332. doi: 10.1038/nm1663. [DOI] [PubMed] [Google Scholar]
- 255.Guo J., Loke J., Zheng F., Hong F., Yea S., Fukata M., Tarocchi M., Abar O.T., Huang H., Sninsky J.J., et al. Functional linkage of cirrhosis-predictive single nucleotide polymorphisms of toll-like receptor 4 to hepatic stellate cell responses. Hepatology. 2009;49:960–968. doi: 10.1002/hep.22697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Dasu M.R., Jialal I. Free fatty acids in the presence of high glucose amplify monocyte inflammation via toll-like receptors. Am. J. Physiol. Endocrinol. Metab. 2011;300:E145–E154. doi: 10.1152/ajpendo.00490.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Shi H., Kokoeva M.V., Inouye K., Tzameli I., Yin H., Flier J.S. TLR4 links innate immunity and fatty acid-induced insulin resistance. J. Clin. Investig. 2006;116:3015–3025. doi: 10.1172/JCI28898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Dostert C., Petrilli V., van Bruggen R., Steele C., Mossman B.T., Tschopp J. Innate immune activation through NALP3 inflammasome sensing of asbestos and silica. Science. 2008;320:674–677. doi: 10.1126/science.1156995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Shimada K., Crother T.R., Karlin J., Dagvadorj J., Chiba N., Chen S., Ramanujan V.K., Wolf A.J., Vergnes L., Ojcius D.M., et al. Oxidized mitochondrial DNA activates the NLRP3 inflammasome during apoptosis. Immunity. 2012;36:401–414. doi: 10.1016/j.immuni.2012.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Martinon F., Burns K., Tschopp J. The inflammasome: A molecular platform triggering activation of inflammatory caspases and processing of proil-β. Mol. Cell. 2002;10:417–426. doi: 10.1016/S1097-2765(02)00599-3. [DOI] [PubMed] [Google Scholar]
- 261.Szabo G., Csak T. Inflammasomes in liver diseases. J. Hepatol. 2012;57:642–654. doi: 10.1016/j.jhep.2012.03.035. [DOI] [PubMed] [Google Scholar]
- 262.Dixon L.J., Flask C.A., Papouchado B.G., Feldstein A.E., Nagy L.E. Caspase-1 as a central regulator of high fat diet-induced non-alcoholic steatohepatitis. PLoS ONE. 2013;8:1575. doi: 10.1371/journal.pone.0056100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Stienstra R., Joosten L.A., Koenen T., van Tits B., van Diepen J.A., van den Berg S.A., Rensen P.C., Voshol P.J., Fantuzzi G., Hijmans A., et al. The inflammasome-mediated caspase-1 activation controls adipocyte differentiation and insulin sensitivity. Cell Metab. 2010;12:593–605. doi: 10.1016/j.cmet.2010.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Membrez M., Ammon-Zufferey C., Philippe D., Aprikian O., Monnard I., Mace K., Darimont C. Interleukin-18 protein level is upregulated in adipose tissue of obese mice. Obesity. 2009;17:393–395. doi: 10.1038/oby.2008.535. [DOI] [PubMed] [Google Scholar]
- 265.Csak T., Pillai A., Ganz M., Lippai D., Petrasek J., Park J.K., Kodys K., Dolganiuc A., Kurt-Jones E.A., Szabo G. Both bone marrow-derived and non-bone marrow-derived cells contribute to AIM2 and NLRP3 inflammasome activation in a MyD88-dependent manner in dietary steatohepatitis. Liver Int. 2014;34:1402–1413. doi: 10.1111/liv.12537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Ganz M., Bukong T.N., Csak T., Saha B., Park J.K., Ambade A., Kodys K., Szabo G. Progression of non-alcoholic steatosis to steatohepatitis and fibrosis parallels cumulative accumulation of danger signals that promote inflammation and liver tumors in a high fat-cholesterol-sugar diet model in mice. J. Transl. Med. 2015;13 doi: 10.1186/s12967-015-0552-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Vandanmagsar B., Youm Y.H., Ravussin A., Galgani J.E., Stadler K., Mynatt R.L., Ravussin E., Stephens J.M., Dixit V.D. The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Nat. Med. 2011;17:179–188. doi: 10.1038/nm.2279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Wree A., McGeough M.D., Pena C.A., Schlattjan M., Li H., Inzaugarat M.E., Messer K., Canbay A., Hoffman H.M., Feldstein A.E. NLRP3 inflammasome activation is required for fibrosis development in NAFLD. J. Mol. Med. 2014;92:1069–1082. doi: 10.1007/s00109-014-1170-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Henao-Mejia J., Elinav E., Jin C., Hao L., Mehal W.Z., Strowig T., Thaiss C.A., Kau A.L., Eisenbarth S.C., Jurczak M.J., et al. Inflammasome-mediated dysbiosis regulates progression of NAFLD and obesity. Nature. 2012;482:179–185. doi: 10.1038/nature10809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Wree A., Eguchi A., McGeough M.D., Pena C.A., Johnson C.D., Canbay A., Hoffman H.M., Feldstein A.E. NLRP3 inflammasome activation results in hepatocyte pyroptosis, liver inflammation, and fibrosis in mice. Hepatology. 2014;59:898–910. doi: 10.1002/hep.26592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Seki E., Schwabe R.F. Hepatic inflammation and fibrosis: Functional links and key pathways. Hepatology. 2015;61:1066–1079. doi: 10.1002/hep.27332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Luedde T., Kaplowitz N., Schwabe R.F. Cell death and cell death responses in liver disease: Mechanisms and clinical relevance. Gastroenterology. 2014;147:765–783. doi: 10.1053/j.gastro.2014.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Huebener P., Pradere J.P., Hernandez C., Gwak G.Y., Caviglia J.M., Mu X., Loike J.D., Jenkins R.E., Antoine D.J., Schwabe R.F. The HMGB1/RAGE axis triggers neutrophil-mediated injury amplification following necrosis. J. Clin. Investig. 2015;125:539–550. doi: 10.1172/JCI76887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Zhang Q., Raoof M., Chen Y., Sumi Y., Sursal T., Junger W., Brohi K., Itagaki K., Hauser C.J. Circulating mitochondrial damps cause inflammatory responses to injury. Nature. 2010;464:104–107. doi: 10.1038/nature08780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Tschopp J. Mitochondria: Sovereign of inflammation? Eur. J. Immunol. 2011;41:1196–1202. doi: 10.1002/eji.201141436. [DOI] [PubMed] [Google Scholar]
- 276.Carp H. Mitochondrial N-formylmethionyl proteins as chemoattractants for neutrophils. J. Exp. Med. 1982;155:264–275. doi: 10.1084/jem.155.1.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Iyer S.S., Pulskens W.P., Sadler J.J., Butter L.M., Teske G.J., Ulland T.K., Eisenbarth S.C., Florquin S., Flavell R.A., Leemans J.C., et al. Necrotic cells trigger a sterile inflammatory response through the NLRP3 inflammasome. Proc. Natl. Acad. Sci. USA. 2009;106:20388–20393. doi: 10.1073/pnas.0908698106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Nakahira K., Haspel J.A., Rathinam V.A., Lee S.J., Dolinay T., Lam H.C., Englert J.A., Rabinovitch M., Cernadas M., Kim H.P., et al. Autophagy proteins regulate innate immune responses by inhibiting the release of mitochondrial DNA mediated by the NALP3 inflammasome. Nat. Immunol. 2011;12:222–230. doi: 10.1038/ni.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Coddou C., Yan Z., Obsil T., Huidobro-Toro J.P., Stojilkovic S.S. Activation and regulation of purinergic P2X receptor channels. Pharmacol. Rev. 2011;63:641–683. doi: 10.1124/pr.110.003129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Di Virgilio F. Liaisons dangereuses: P2X7 and the inflammasome. Trends Pharmacol. Sci. 2007;28:465–472. doi: 10.1016/j.tips.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 281.Stros M. HMGB proteins: Interactions with DNA and chromatin. Biochim. Biophys. Acta. 2010;1799:101–113. doi: 10.1016/j.bbagrm.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 282.Scaffidi P., Misteli T., Bianchi M.E. Release of chromatin protein HMGB1 by necrotic cells triggers inflammation. Nature. 2002;418:191–195. doi: 10.1038/nature00858. [DOI] [PubMed] [Google Scholar]
- 283.Tsung A., Klune J.R., Zhang X., Jeyabalan G., Cao Z., Peng X., Stolz D.B., Geller D.A., Rosengart M.R., Billiar T.R. HMGB1 release induced by liver ischemia involves toll-like receptor 4 dependent reactive oxygen species production and calcium-mediated signaling. J. Exp. Med. 2007;204:2913–2923. doi: 10.1084/jem.20070247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Bianchi M.E. HMGB1 loves company. J. Leukoc. Biol. 2009;86:573–576. doi: 10.1189/jlb.1008585. [DOI] [PubMed] [Google Scholar]
- 285.Hornung V., Bauernfeind F., Halle A., Samstad E.O., Kono H., Rock K.L., Fitzgerald K.A., Latz E. Silica crystals and aluminum salts activate the NALP3 inflammasome through phagosomal destabilization. Nat. Immunol. 2008;9:847–856. doi: 10.1038/ni.1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Lotze M.T., Tracey K.J. High-mobility group box 1 protein (HMGB1): Nuclear weapon in the immune arsenal. Nat. Rev. Immunol. 2005;5:331–342. doi: 10.1038/nri1594. [DOI] [PubMed] [Google Scholar]
- 287.Bluher M. Clinical relevance of adipokines. Diabetes Metab. J. 2012;36:317–327. doi: 10.4093/dmj.2012.36.5.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Marra F., Bertolani C. Adipokines in liver diseases. Hepatology. 2009;50:957–969. doi: 10.1002/hep.23046. [DOI] [PubMed] [Google Scholar]
- 289.Polyzos S.A., Kountouras J., Zavos C. Nonalcoholic fatty liver disease: The pathogenetic roles of insulin resistance and adipocytokines. Curr. Mol. Med. 2009;9:299–314. doi: 10.2174/156652409787847191. [DOI] [PubMed] [Google Scholar]
- 290.Polyzos S.A., Kountouras J., Zavos C., Tsiaousi E. The role of adiponectin in the pathogenesis and treatment of non-alcoholic fatty liver disease. Diabetes Obes. Metab. 2010;12:365–383. doi: 10.1111/j.1463-1326.2009.01176.x. [DOI] [PubMed] [Google Scholar]
- 291.Polyzos S.A., Kountouras J., Zavos C. The multi-hit process and the antagonistic roles of tumor necrosis factor-α and adiponectin in non alcoholic fatty liver disease. Hippokratia. 2009;13:127. [PMC free article] [PubMed] [Google Scholar]
- 292.Tilg H., Hotamisligil G.S. Nonalcoholic fatty liver disease: Cytokine-adipokine interplay and regulation of insulin resistance. Gastroenterology. 2006;131:934–945. doi: 10.1053/j.gastro.2006.05.054. [DOI] [PubMed] [Google Scholar]
- 293.Moon H.S., Dalamaga M., Kim S.Y., Polyzos S.A., Hamnvik O.P., Magkos F., Paruthi J., Mantzoros C.S. Leptin’s role in lipodystrophic and nonlipodystrophic insulin-resistant and diabetic individuals. Endocr. Rev. 2013;34:377–412. doi: 10.1210/er.2012-1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Polyzos S.A., Kountouras J., Mantzoros C.S. Leptin in nonalcoholic fatty liver disease: A narrative review. Metabolism. 2015;64:60–78. doi: 10.1016/j.metabol.2014.10.012. [DOI] [PubMed] [Google Scholar]
- 295.Dattaroy D., Pourhoseini S., Das S., Alhasson F., Seth R.K., Nagarkatti M., Michelotti G.A., Diehl A.M., Chatterjee S. Micro-RNA 21 inhibition of SMAD7 enhances fibrogenesis via leptin-mediated NADPH oxidase in experimental and human nonalcoholic steatohepatitis. Am. J. Physiol. Gastrointest. Liver Physiol. 2015;308:G298–G312. doi: 10.1152/ajpgi.00346.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Zhou Q., Guan W., Qiao H., Cheng Y., Li Z., Zhai X., Zhou Y. Gata binding protein 2 mediates leptin inhibition of PPARγ1 expression in hepatic stellate cells and contributes to hepatic stellate cell activation. Biochim. Biophys. Acta. 2014;1842:2367–2377. doi: 10.1016/j.bbadis.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 297.Heinrich G., Russo L., Castaneda T.R., Pfeiffer V., Ghadieh H.E., Ghanem S.S., Wu J., Faulkner L.D., Ergun S., McInerney M.F., et al. Leptin resistance contributes to obesity in mice with null mutation of carcinoembryonic antigen-related cell adhesion molecule 1. J. Biol. Chem. 2016;291:11124–11132. doi: 10.1074/jbc.M116.716431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Poy M.N., Yang Y., Rezaei K., Fernstrom M.A., Lee A.D., Kido Y., Erickson S.K., Najjar S.M. CEACAM1 regulates insulin clearance in liver. Nat. Genet. 2002;30:270–276. doi: 10.1038/ng840. [DOI] [PubMed] [Google Scholar]
- 299.DeAngelis A.M., Heinrich G., Dai T., Bowman T.A., Patel P.R., Lee S.J., Hong E.G., Jung D.Y., Assmann A., Kulkarni R.N., et al. Carcinoembryonic antigen-related cell adhesion molecule 1: A link between insulin and lipid metabolism. Diabetes. 2008;57:2296–2303. doi: 10.2337/db08-0379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Yoda-Murakami M., Taniguchi M., Takahashi K., Kawamata S., Saito K., Choi-Miura N.H., Tomita M. Change in expression of GBP28/adiponectin in carbon tetrachloride-administrated mouse liver. Biochem. Biophys. Res. Commun. 2001;285:372–377. doi: 10.1006/bbrc.2001.5134. [DOI] [PubMed] [Google Scholar]
- 301.Heiker J.T., Kosel D., Beck-Sickinger A.G. Molecular mechanisms of signal transduction via adiponectin and adiponectin receptors. Biol. Chem. 2010;391:1005–1018. doi: 10.1515/bc.2010.104. [DOI] [PubMed] [Google Scholar]
- 302.Jiang C., Qu A., Matsubara T., Chanturiya T., Jou W., Gavrilova O., Shah Y.M., Gonzalez F.J. Disruption of hypoxia-inducible factor 1 in adipocytes improves insulin sensitivity and decreases adiposity in high-fat diet-fed mice. Diabetes. 2011;60:2484–2495. doi: 10.2337/db11-0174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Otani H. Oxidative stress as pathogenesis of cardiovascular risk associated with metabolic syndrome. Antioxid. Redox Signal. 2011;15:1911–1926. doi: 10.1089/ars.2010.3739. [DOI] [PubMed] [Google Scholar]
- 304.Kusminski C.M., Scherer P.E. Mitochondrial dysfunction in white adipose tissue. Trends Endocrinol. Metab. 2012;23:435–443. doi: 10.1016/j.tem.2012.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Polyzos S.A., Kountouras J., Zavos C. Nonlinear distribution of adiponectin in patients with nonalcoholic fatty liver disease limits its use in linear regression analysis. J. Clin. Gastroenterol. 2010;44:229–230. doi: 10.1097/MCG.0b013e3181b5ce68. [DOI] [PubMed] [Google Scholar]
- 306.Van der Poorten D., Samer C.F., Ramezani-Moghadam M., Coulter S., Kacevska M., Schrijnders D., Wu L.E., McLeod D., Bugianesi E., Komuta M., et al. Hepatic fat loss in advanced nonalcoholic steatohepatitis: Are alterations in serum adiponectin the cause? Hepatology. 2013;57:2180–2188. doi: 10.1002/hep.26072. [DOI] [PubMed] [Google Scholar]
- 307.Bozaoglu K., Bolton K., McMillan J., Zimmet P., Jowett J., Collier G., Walder K., Segal D. Chemerin is a novel adipokine associated with obesity and metabolic syndrome. Endocrinology. 2007;148:4687–4694. doi: 10.1210/en.2007-0175. [DOI] [PubMed] [Google Scholar]
- 308.Sell H., Divoux A., Poitou C., Basdevant A., Bouillot J.L., Bedossa P., Tordjman J., Eckel J., Clement K. Chemerin correlates with markers for fatty liver in morbidly obese patients and strongly decreases after weight loss induced by bariatric surgery. J. Clin. Endocrinol. Metab. 2010;95:2892–2896. doi: 10.1210/jc.2009-2374. [DOI] [PubMed] [Google Scholar]
- 309.Ernst M.C., Issa M., Goralski K.B., Sinal C.J. Chemerin exacerbates glucose intolerance in mouse models of obesity and diabetes. Endocrinology. 2010;151:1998–2007. doi: 10.1210/en.2009-1098. [DOI] [PubMed] [Google Scholar]
- 310.Yoshimura T., Oppenheim J.J. Chemerin reveals its chimeric nature. J. Exp. Med. 2008;205:2187–2190. doi: 10.1084/jem.20081736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Krautbauer S., Wanninger J., Eisinger K., Hader Y., Beck M., Kopp A., Schmid A., Weiss T.S., Dorn C., Buechler C. Chemerin is highly expressed in hepatocytes and is induced in non-alcoholic steatohepatitis liver. Exp. Mol. Pathol. 2013;95:199–205. doi: 10.1016/j.yexmp.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 312.Topping D.L., Clifton P.M. Short-chain fatty acids and human colonic function: Roles of resistant starch and nonstarch polysaccharides. Physiol. Rev. 2001;81:1031–1064. doi: 10.1152/physrev.2001.81.3.1031. [DOI] [PubMed] [Google Scholar]
- 313.Turnbaugh P.J., Ley R.E., Mahowald M.A., Magrini V., Mardis E.R., Gordon J.I. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–1031. doi: 10.1038/nature05414. [DOI] [PubMed] [Google Scholar]
- 314.Shin N.R., Lee J.C., Lee H.Y., Kim M.S., Whon T.W., Lee M.S., Bae J.W. An increase in the Akkermansia spp. population induced by metformin treatment improves glucose homeostasis in diet-induced obese mice. Gut. 2014;63:727–735. doi: 10.1136/gutjnl-2012-303839. [DOI] [PubMed] [Google Scholar]
- 315.Karlsson C.L., Onnerfalt J., Xu J., Molin G., Ahrne S., Thorngren-Jerneck K. The microbiota of the gut in preschool children with normal and excessive body weight. Obesity. 2012;20:2257–2261. doi: 10.1038/oby.2012.110. [DOI] [PubMed] [Google Scholar]
- 316.Zeisel S.H., Wishnok J.S., Blusztajn J.K. Formation of methylamines from ingested choline and lecithin. J. Pharmacol. Exp. Ther. 1983;225:320–324. [PubMed] [Google Scholar]
- 317.Spencer M.D., Hamp T.J., Reid R.W., Fischer L.M., Zeisel S.H., Fodor A.A. Association between composition of the human gastrointestinal microbiome and development of fatty liver with choline deficiency. Gastroenterology. 2011;140:976–986. doi: 10.1053/j.gastro.2010.11.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Sinal C.J., Tohkin M., Miyata M., Ward J.M., Lambert G., Gonzalez F.J. Targeted disruption of the nuclear receptor FXR/BAR impairs bile acid and lipid homeostasis. Cell. 2000;102:731–744. doi: 10.1016/S0092-8674(00)00062-3. [DOI] [PubMed] [Google Scholar]
- 319.Hylemon P.B., Zhou H., Pandak W.M., Ren S., Gil G., Dent P. Bile acids as regulatory molecules. J. Lipid Res. 2009;50:1509–1520. doi: 10.1194/jlr.R900007-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Tremaroli V., Backhed F. Functional interactions between the gut microbiota and host metabolism. Nature. 2012;489:242–249. doi: 10.1038/nature11552. [DOI] [PubMed] [Google Scholar]
- 321.Prawitt J., Abdelkarim M., Stroeve J.H., Popescu I., Duez H., Velagapudi V.R., Dumont J., Bouchaert E., van Dijk T.H., Lucas A., et al. Farnesoid X receptor deficiency improves glucose homeostasis in mouse models of obesity. Diabetes. 2011;60:1861–1871. doi: 10.2337/db11-0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Thomas C., Gioiello A., Noriega L., Strehle A., Oury J., Rizzo G., Macchiarulo A., Yamamoto H., Mataki C., Pruzanski M., et al. TGR5-mediated bile acid sensing controls glucose homeostasis. Cell Metab. 2009;10:167–177. doi: 10.1016/j.cmet.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Cope K., Risby T., Diehl A.M. Increased gastrointestinal ethanol production in obese mice: Implications for fatty liver disease pathogenesis. Gastroenterology. 2000;119:1340–1347. doi: 10.1053/gast.2000.19267. [DOI] [PubMed] [Google Scholar]
- 324.Zhu L., Baker S.S., Gill C., Liu W., Alkhouri R., Baker R.D., Gill S.R. Characterization of gut microbiomes in nonalcoholic steatohepatitis (NASH) patients: A connection between endogenous alcohol and NASH. Hepatology. 2013;57:601–609. doi: 10.1002/hep.26093. [DOI] [PubMed] [Google Scholar]
- 325.Noverr M.C., Huffnagle G.B. Does the microbiota regulate immune responses outside the gut? Trends Microbiol. 2004;12:562–568. doi: 10.1016/j.tim.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 326.Sabate J.M., Jouet P., Harnois F., Mechler C., Msika S., Grossin M., Coffin B. High prevalence of small intestinal bacterial overgrowth in patients with morbid obesity: A contributor to severe hepatic steatosis. Obes. Surg. 2008;18:371–377. doi: 10.1007/s11695-007-9398-2. [DOI] [PubMed] [Google Scholar]
- 327.Wigg A.J., Roberts-Thomson I.C., Dymock R.B., McCarthy P.J., Grose R.H., Cummins A.G. The role of small intestinal bacterial overgrowth, intestinal permeability, endotoxaemia, and tumour necrosis factor α in the pathogenesis of non-alcoholic steatohepatitis. Gut. 2001;48:206–211. doi: 10.1136/gut.48.2.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Minemura M., Shimizu Y. Gut microbiota and liver diseases. World J. Gastroenterol. 2015;21:1691–1702. doi: 10.3748/wjg.v21.i6.1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Fukui H. Gut-liver axis in liver cirrhosis: How to manage leaky gut and endotoxemia. World J. Hepatol. 2015;7:425–442. doi: 10.4254/wjh.v7.i3.425. [DOI] [PMC free article] [PubMed] [Google Scholar]