Abstract
Background:
Instrument assisted soft tissue mobilization (IASTM) is a popular treatment for myofascial restriction. IASTM uses specially designed instruments to provide a mobilizing effect to scar tissue and myofascial adhesions. Several IASTM tools and techniques are available such as the Graston® technique. Currently, there are no systematic reviews that have specifically appraised the effects of IASTM as a treatment or to enhance joint range of motion (ROM).
Purpose:
The purpose of this study was to systematically appraise the current evidence assessing the effects of IASTM as an intervention to treat a musculoskeletal pathology or to enhance joint ROM.
Methods:
A search of the literature was conducted during the month of December 2015 which included the following databases: PubMed, PEDro, Science Direct, and the EBSCOhost collection. A direct search of known journals was also conducted to identify potential publications. The search terms included individual or a combination of the following: instrument; assisted; augmented; soft-tissue; mobilization; Graston®; and technique.
Results:
A total of 7 randomized controlled trials were appraised. Five of the studies measured an IASTM intervention versus a control or alternate intervention group for a musculoskeletal pathology. The results of the studies were insignificant (p>.05) with both groups displaying equal outcomes. Two studies measured an IASTM intervention versus a control or alternate intervention group on the effects of joint ROM. The IASTM intervention produced significant (P<.05) short term gains up to 24 hours.
Conclusion:
The literature measuring the effects of IASTM is still emerging. The current research has indicated insignificant results which challenges the efficacy of IASTM as a treatment for common musculoskeletal pathology, which may be due to the methodological variability among studies. There appears to be some evidence supporting its ability to increase short term joint ROM.
Keywords: chiropractic, Graston®; myofascial; massage
Abstract
Contexte:
La mobilisation des tissus mous assistée par instrument (MTMAI) est un traitement populaire pour la restriction des tissus myofasciaux. La MTMAI utilise des instruments spécialement conçus pour fournir un effet de mobilisation sur les tissus cicatriciels et les adhérences myofasciales. Plusieurs outils et techniques de MTMAI sont disponibles, comme la technique GrastonMD. Actuellement, il n’y a aucun examen systématique ayant notamment évalué les effets de la MTMAI comme traitement ou pour améliorer l’amplitude articulaire.
Objectif:
Cette étude visait à évaluer systématiquement les données actuelles évaluant les effets de la MTMAI comme méthode d’intervention pour traiter une pathologie musculo-squelettique ou pour améliorer l’amplitude articulaire.
Méthodologie:
Une recherche des publications scientifiques a été réalisée au cours du mois de décembre 2015, incluant les bases de données suivantes : PubMed, PEDro, Science Direct, et la collection EBSCOhost. Une recherche directe a également été réalisée dans les revues connues pour relever les publications possibles. La recherche était basée sur les termes ou combinaisons de termes suivants : instrument; assistée; accrue; tissu mou; mobilisation; GrastonMD; technique.
Résultats:
Au total, sept essais contrôlés randomisés ont été évalués. Cinq des études mesuraient une intervention de MTMAI par rapport à un groupe de contrôle ou une intervention différente pour l’évaluation de la pathologie musculo-squelettique. Les résultats des études étaient négligeables (p > ,05) les deux groupes affichant des résultats égaux. Deux études mesuraient une intervention de MTMAI par rapport à un groupe de contrôle ou une intervention différente sur les effets de l’amplitude articulaire. L’intervention de MTMAI a produit des gains à court terme significatifs (P < ,05) allant jusqu’à 24 heures.
Conclusion:
Les publications scientifiques sur la mesure des effets de la MTMAI sont encore à leur début. La recherche actuelle a indiqué des résultats négligeables qui mettent en question l’efficacité de la MTMAI comme traitement de la pathologie musculo-squelettique courante, ce qui peut être dû à la variabilité de la méthodologie entre les études. Il semble y avoir des preuves soutenant sa capacité à augmenter l’amplitude articulaire à court terme.
Keywords: chiropratique, GrastonMD, myofascial, massage
Introduction
Instrument assisted soft tissue mobilization (IASTM) is a popular treatment for myofascial restriction based upon the rationale introduced by James Cyriax.1,2 Unlike the Cyriax approach utilizing digital cross friction, IASTM is applied using specially designed instruments to provide a mobilizing effect to soft tissue (e.g., scar tissue, myofascial adhesion) to decrease pain and improve range of motion (ROM) and function.2 The use of the instrument is thought to provide a mechanical advantage for the clinician by allowing deeper penetration and more specific treatment, while also reducing imposed stress on the hands (Figure 1).2–4 Using instruments for soft tissue mobilization is theorized to increase vibration sense by the clinician and patient. The increased perception of vibration may facilitate the clinician’s ability to detect altered tissue properties (e.g., identify tissue adhesions) while facilitating the patient’s awareness of altered sensations within the treated tissues.2,5
Figure 1.

Example of IASTM treatment.
The IASTM treatment is thought to stimulate connective tissue remodeling through resorption of excessive fibrosis, along with inducing repair and regeneration of collagen secondary to fibroblast recruitment.6,7 In turn, this will result in the release and breakdown of scar tissue, adhesions, and fascial restrictions.6–8 In laboratory studies using a rat model, the use of instruments resulted in increased fibroblast proliferation and collagen repair (e.g., synthesis, alignment, and maturation) in cases of enzyme-induced tendinitis.9,10 Many of these benefits were also found in a laboratory study on ligament healing using the rat model which further provided supporting evidence that instrument massage produces a significant short-term (e.g., 4 weeks) increase in ligament strength and stiffness compared to the contralateral control limb.11 While these findings provide initial support for IASTM stimulating connective tissue remodeling, these physiological changes are still being studied and have not been confirmed in human trials.
There are various IASTM tools and companies such as Graston®, Técnica Gavilán®, Hawk Grips®, Functional and Kinetic Treatment and Rehab (FAKTR)®, Adhesion Breakers® and Fascial Abrasion Technique™ that have their own approach to treatment and instrument design (e.g., instrument materials, instrument shape). Anecdotally, the Graston® technique contains a protocol for treatment that contains several components: examination, warm-up, IASTM treatment (e.g., 30–60 seconds per lesion), post treatment stretching, strengthening, and ice (only when subacute inflammation is of concern).12 Despite the variations in treatment approaches and design, the general premise of IASTM is to enhance myofascial mobility with limited adverse effects such as discomfort during treatment or bruising (e.g. petechiae) after treatment.13–17
To date, there have been no systematic reviews appraising the body of IASTM literature. For many years, the efficacy of IASTM was described through case series2,18–21 and reports1,6,8,22–32 (level 4 evidence) which are limited due to their subjectivity. Most of the case reports described successful treatment of tendinopathies8,19,21,22,24–27,30,32 and arthrofibrosis31,33. Recently, higher level controlled investigations14,32,34–38 have been published assessing the efficacy of IASTM treatment for various conditions but have not been appraised. The goal of this systematic review was to appraise the current IASTM literature to provide a current update for the clinician.
Methods
Search Strategy
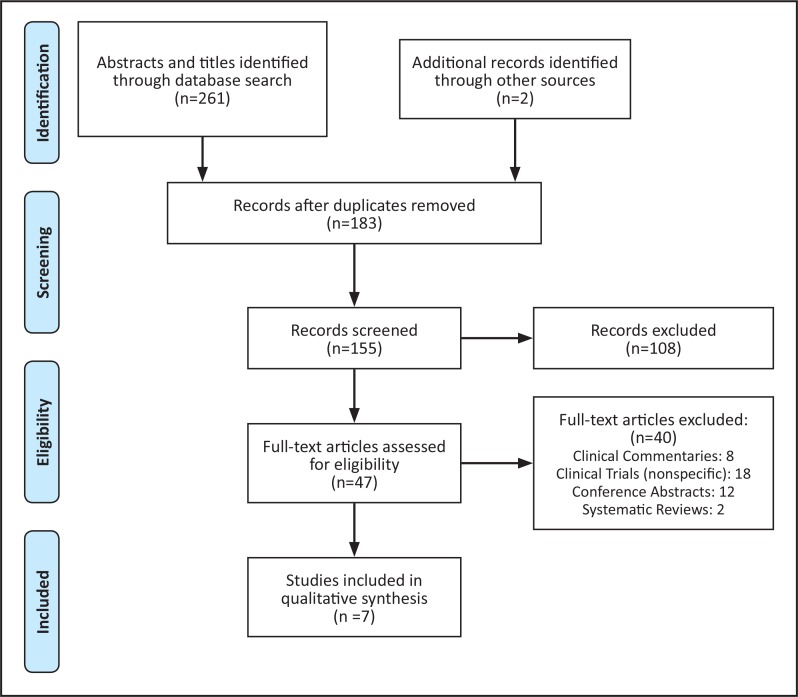
A systematic search strategy was conducted according the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for reporting systematic reviews.39,40 The following databases were searched during the month of December 2015: PubMed, PEDro, Science Direct, and the EBSCOhost collection. A direct search of known journals was also conducted to identify potential publications. The search terms included individual or a combination of the following: instrument; assisted; augmented; soft-tissue; mobilization; Graston®; and technique.
The terms Gua sha and ASTYM® were omitted from this search. Gua sha is a popular Asian medical treatment that uses a smooth edged instrument (e.g. water buffalo horn, honed jade, soup spoon) to scrape the skin until a red blemish appears.41 The red ecchymosis caused by the scraping is believed to be blood stasis. The Gua sha treatment is supposed to relieve blood stagnation and reduce pain.15 Clinicians may consider the Gua sha approach a form of IASTM but the treatment rationale, goals, and application differs from the other IASTM approaches.41 Another form of myofascial treatment called augmented soft tissue mobilization (ASTYM®) is often considered a type of IASTM.42 The creators and proponents of ASTYM® do not consider it a form of IASTM due to their unique treatment approach which uses a combination of instruments, stretching, and strengthening.32,42,43 Both Gua sha and ASTYM® have their own body of evidence including literature reviews.15,17,32,41–44 Due to these variations, Gua sha and ASTYM® were not included in this review since the focus of this review was to appraise the literature on IASTM.
Study Selection
Two reviewers (MC and ML) independently searched the databases and selected studies. A third independent reviewer (SC) was available to resolve any disagreements. Studies considered for inclusion met the following criteria:
Peer reviewed, English language publications
Controlled clinical trials that compared pretest and posttest measurements for an intervention program using IASTM
Investigations that compared an intervention program using IASTM
Investigations that compared two intervention programs using IASTM.
Studies were excluded if they were non-English publications, clinical trials that included IASTM as an intervention but did not directly measure its effects, clinical trials that included Gua sha and ASTYM®, case reports, case series, clinical commentary, dissertations, and conference posters or abstracts.
Data Extraction and Synthesis
The following data were extracted from each article: subject demographics, intervention type, intervention parameters, and outcomes. The research design of each study was also identified by the reviewers. Qualifying manuscripts were assessed using the PEDro (Physiotherapy Evidence Database) scale for appraising the quality of literature.45,46 A PEDro score of 6 or more was considered moderate to high level evidence.47
Intra observer agreement was calculated using the Kappa statistic.48 Landis and Koch 49 provided the following interpretation to the Kappa values: <0 poor inter-rater agreement, 0.01 to 0.20 as slight agreement, 0.21 to 0.40 as fair agreement, 0.41 to 0.60 as moderate agreement, 0.61 to 0.80 is substantial agreement, and 0.81 to 1.0 as almost perfect agreement.
Results
A total of 261 articles were initially identified from the search and 106 articles were excluded due to duplication or not meeting the inclusion criteria. A total of 155 articles were screened and a total of 7 randomized controlled trials (RCTs) met the inclusion criteria for this analysis. A summary of the search strategy and reasons for exclusion of manuscripts are outlined in Figure 2. The reviewers Kappa value for the 7 articles was 1.0 (perfect agreement). Table 1 provides the PEDro score for each of the qualifying studies and Table 2 provide a description of each study.
Figure 2.
PRISMA search strategy.
Table 1.
PEDro score for the qualified studies.
| Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 | Item 11 | Total Score | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Blanchette and Normand32 | Y | Y | N | Y | Y | N | N | Y | Y | Y | Y | 8 |
| Burke et al35 | Y | Y | N | Y | Y | N | N | Y | Y | Y | Y | 8 |
| Gulick36 | Y | Y | N | Y | Y | N | N | Y | Y | Y | Y | 8 |
| Laudner et al37 | Y | Y | N | Y | Y | N | N | Y | Y | Y | Y | 8 |
| Markovic14 | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 7 |
| Schaefer and Sandrey38 | Y | Y | N | Y | Y | N | N | Y | Y | Y | Y | 8 |
| Brantingham et al34 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | 10 |
Pedro Criteria: Item 1(Eligibility criteria), Item 2 (Subjects randomly allocated), Item 3 (Allocation concealed), Item 4 (Intervention groups similar), Item 5 (subjects were blinded), Item 6 (Therapists administering therapy blinded), Item 7 (All assessors blinded), Item 8 (At least 1 key outcome obtained from more than 85% of subjects initially allocated), Item 9 (All subjects received treatment or control intervention or an Intention-to-treat analysis performed), Item 10 (Between group comparison reported for a least on variable), Item 11 (study provides both point measures and measures of variability for at least one key outcome)
Table 2.
Summary of qualifying studies.
| Author | Type of Study | Subjects | Technique | Pathology or Region | Outcome Measures | Intervention | Results |
|---|---|---|---|---|---|---|---|
| Blanchette and Normand32 | RCT | N=27 (12M, 15F) IASTM (N=15) Control (N=12) |
Graston® | Lateral Epicondylitis |
|
IASTM: received IASTM twice a week for 5 weeks. Dosage time not reported. Control: received education about the pathology, computer ergonomics, and stretching flexors and the extensors muscles of the wrist (hold 30 seconds, 6 times a day), ice and generic anti-inflammatory medications. |
Post-intervention and at a 3-month follow-up. Both groups showed improvements in pain-free grip strength, VAS, and Patient-Rated Tennis Elbow Evaluation. |
| Burke et al35 | RCT | N=22 (3M, 19F) IASTM (N=12) STM (N=10) |
Graston® | Carpel Tunnel Syndrome |
|
Both the IASTM and STM groups received the same treatment protocol: 2x/week for first 4 weeks and 1x/week for 2 weeks. Home program included stretching and strengthening the upper extremity. IASTM and STM dosage times not reported. Note: subjects were instructed to refrain from use of wrist splints and anti-inflammatory medications during the intervention period. |
Post-intervention and at a 3-month follow-up, both groups showed improvement in all outcomes measures. |
| Gulick36 | RCT |
Phase I (N=27, 13M, 14F) Phase II (N=22, 5M, 15F) IASTM (N=14) Control (N=8) |
Graston® | Myofascial Trigger points in upper back and |
|
Phase I: Two MTrPS were identified. One treated with IASTM for maximum of 5 minutes the other was control. 6 total treatments (2x/week for 3 weeks) Phase II: One MTrPS identified inIASTM and control group. IASTM group received a maximum treatment time of 5 minutes 2x/week for 3 weeks. Control group did not receive treatment. |
Post-intervention, both the IASTM and control groups showed improvement in the outcome measures. intervention. No secondary follow-up was reported. |
| Laudner et al37 | RCT | N=35M IASTM (N=17) Control (N=18) |
Graston® | Posterior Shoulder Muscles |
|
IASTM: One treatment to the posterior shoulder musculature for a total treatment time of 40 seconds. Control: No treatment. |
Post-intervention, the IASTM group demonstrated greater acute improvements in ROM when compared to the control group. No secondary follow-up was reported. |
| Markovic14 | RCT | N-20M IASTM (N=10) Foam Roll (N=10) |
Fascial AbrasionTechnique® | Quadriceps and Hamstrings |
|
IASTM: One treatment to the quadriceps and hamstring for a total of 2 minutes to each region. Foam Rolling: One session to the quadriceps and hamstrings for 2x/1 minute per muscle group. Note: Both groups performed awarm-up up before each session. They cycled for 5 minutes and did dynamic movements (2–5 sets each leg) of walking lunges, walkingknee to chest, side squats, deep squats, and standing toe-touches. Static stretching of quadriceps and hamstring muscles was also done (2 sets of 30 seconds each). |
Post intervention, both groups showed improvement in joint ROM At the 24-hour follow-up, the IASTM group preserved the most joint ROM. |
| Schaefer and Sandrey38 | RCT | N=36 (31 M, 5F) Balance/IASTM (N=13) Balance/Sham IASTM (N=12) Balance only (N=11) |
Graston® | Chronic Ankle Instability |
|
Balance: 4-week program based upon the work of McKeon et al. Exercises included: single-limb hops to stabilization, hop to stabilization and reach, unanticipated hop to stabilization, and single-limb-stance activities. IASTM: 2x/week for a maximum of 8 minutes |
Post-intervention, all groups showed improvement in all outcome measures. No longer term follow-up was reported. |
| Brantingham et al34 | RCT | N=31 Group A (N=13) Group B(N=18) |
Graston® | Patellofemoral Pain Syndrome |
|
Group A: chiropractic manipulative therapy, exercise, and IASTM toknee joints only. Group B: chiropractic manipulative therapy, exercise, and IASTM tolumbosacral, hip, knee, ankle, and foot Both groups received treatment 1–3x/week for 2–6 weeks for a total of 6 treatments Note: IASTM was performed on both groups for a maximum of 3 minutes at each site. The exerciseprogram included isometrics for hip and knee muscles, supine straight leg raise, short arc quadriceps extensions, double and single leg squats, and stretching of the hamstrings and quadriceps. The home program consisted of similar exercises that that subjects continued until the 2-month follow-up. |
Post-intervention and at the 2-month follow-up, both groups showed improvement in all outcome measures. |
IASTM: Instrument Assisted Soft-Tissue Mobilization
STM: Soft Tissue Massage
VAS: Visual analog scale
MTrPS: Myofascial Trigger Points
ROM: Range of motion
Study Quality and Patient Characteristics
All qualified studies were RCTs and scored a 7 or higher on the PEDro scale (Table 1). This is higher than the reported mean PEDro scores of musculoskeletal studies (5.08 ±1.7) and sports physiotherapy studies (4.46 ±1.61).50,51 All seven manuscripts yielded a total of 220 subjects (Male-144, Female-76) (Mean age 28.6 ± 4.17 years). Five studies32,34–36,38 investigated IASTM treatment on subjects with a musculoskeletal pathology and two studies14,37 measured the effects of IASTM on joint ROM in healthy individuals. None of the studies 14,32,34–38 reported any adverse effects or subject attrition from the IASTM intervention. Three studies34,35,38 reported subjects (N=24) dropping out for unrelated reasons. The qualifying studies were grouped into two sections: IASTM treatment for pathology and IASTM treatment for joint ROM.
IASTM Treatment for Pathology
Five studies measured the effects of IASTM on subjects with musculoskeletal pathology which included: lateral epicondylitis32, carpel tunnel syndrome35, myofascial trigger points36, chronic ankle instability38, and patellofemoral pain syndrome34. All studies32,34–36,38 reported using the Graston® technique but varied in their treatment protocol.
For the intervention program, two studies32,36 compared IASTM with a control group, one study35 compared IASTM to soft-tissue massage, one study34 compared two intervention programs that included either IASTM, strengthening exercises, stretching, and chiropractic manipulative therapy, and one study38 compared three intervention programs that included either IASTM, dynamic strengthening (e.g., single leg hops), or proprioception exercises. The time frame for the all the interventions ranged from 2 to 6 weeks (average 2 sessions per week).32,34–36,38
All studies32,34–36,38 used the Graston® technique but only three studies34,36,38 reported the treatment time. One study34 reported a maximum 3 minutes per site and two studies36,38 reported a total treatment times of 5 and 8 minutes. Two studies32,35 did not report any specific IASTM treatment times. Only one study35 followed the recommended Graston® treatment protocol. All other studies14,32,34,36–38 either modified the protocol or did not include all intervention components. Due to the variations in treatment protocols and the lack of homogeneity in treatment application, it is difficult to utilize the results to assess the effect of the Graston® protocol or IASTM effectiveness in general.
All studies32,34–36,38 included a combination of patient related outcome measures and clinical tests. The most common patient related outcome measure was the visual analog scale for pain.32,34–36,38 Three32,34,35 studies included clinical tests such as joint ROM and muscle strength as part of their outcome measures. All studies measured outcomes pre-intervention and immediately post-intervention.32,34–36,38 Only three studies32,34,35 reported a second follow-up assessment that ranged from 2 to 3 months’ post treatment. The overall results among studies were insignificant (p>.05) with the IASTM group displaying equal improvement as the control or comparison groups.32,34–36,38
IASTM Treatment for joint ROM
Two RCT studies14,37 measured the effects of IASTM on joint ROM of the shoulder and knee in healthy subjects. One study37 measured the effects of a single session (40 seconds) of the Graston® technique on glenohumeral ROM and compared it to a non-intervention control group. The Graston® protocol was not followed. Another study14 compared the effects of one session (2 minutes) of the IASTM Fascial Abrasion Technique (FAT™) to one session of foam rolling (2 minutes) on hip and knee ROM. Subjects performed a comprehensive warm-up prior to the FAT™ intervention and 24-hour follow-up. The warm-up consisted of cardiovascular activity, closed chain movements, and lower extremity statistic stretching. No specific IASTM protocol was used in the study.14
Both studies14,37 used joint ROM as the primary outcome measure and did not use any patient related outcome measures. Both studies14,37 measured pre-intervention and immediately post-intervention outcomes with only the FAT™ study14 conducting a follow-up at 24-hours post-intervention. The results of the study37 using Graston® revealed a significant (p<.05) acute increase in joint ROM when compared to the control group. The study14 using FAT™ reported equal improvement between groups immediately post-intervention but the FAT™ group preserved the most joint ROM (p<.05) at the 24-hour follow-up.
Discussion
To the authors’ knowledge, this is the first systematic review to appraise the IASTM literature. Seven RCTs met the search criteria (Table 2) and were mainly comprised of intervention studies followed by joint ROM investigations. The body of knowledge regarding IASTM is still emerging. The current research has indicated insignificant results which challenges the efficacy of IASTM as a treatment, which may be due to the methodological variability among studies. The clinical implications of the investigations will be discussed in the following sections.
IASTM Treatment for Pathology
Five studies32,34–36,38 were appraised but varied in their study populations, methodology, and outcomes measures preventing a direct comparison. The common variable among all the studies was the reported use of the Graston® technique; however, there were several potential methodological issues that may have led to the insignificant results among all studies. First, only one study35 followed the recommended Graston® treatment protocol which includes examination, warm-up, IASTM treatment, post treatment stretching, strengthening, and ice.13 The other four studies32,34,36,38 either modified or excluded parts of the protocol. It is problematic to compare studies with different IASTM protocols and attempt to draw conclusions regarding its efficacy in clinical practice. The varied protocols also make it difficult to determine the effectiveness of the Graston® technique when their specified protocols are not followed. Second, the IASTM treatment times varied among studies. Three studies34,36,38 reported different treatment times and two studies failed to report any treatment times. Third, several of the studies seem to have methodological issues with their intervention programs. Blanchette and Norman32 measured the effects of IASTM for lateral epicondylitis in a group of 27 subjects. The researchers randomized the groups into an experimental and control group. The experimental group received IASTM treatment only and the control group received education, forearm stretching, strengthening exercises, ice, and generic anti-inflammatory medication during the intervention phase. Upon completion of the study, the researchers found that both groups improved but no significant difference in outcomes were found. Perhaps, the difference in group interventions (e.g., not including other components of IASTM protocol) may have led to the insignificant treatment outcomes.32 Schaefer and Sandrey38 measured the effects of a 4-week dynamic balance program combined with IASTM on subjects with a history chronic ankle instability. The researchers randomized the 36 healthy subjects with a history of ankle instability into 3 groups: balance/IASTM (N=13), balance/sham IASTM (N=12), and balance only (N=11). Upon completion of the study, the researchers found that all groups improved with no significant difference between groups. Perhaps, the IASTM had no effect because the subjects did not have a current injury, the therapy was not provided for a long enough duration to initiate tissue remodeling for chronic scar tissue following injury, or the treatment application was not directed at the appropriate anatomical area. Thus, the dynamic balance training program would have been the only effective intervention.38 Brantingham et al.34 conducted a feasibility study comparing two chiropractic protocols in the treatment of patellofemoral pain syndrome. Protocol A consisted of chiropractic manipulative therapy, exercise, and IASTM to the knees only. Protocol B consisted of chiropractic manipulative therapy, exercise, and IASTM to lumbosacral, hip, knee, ankle, and foot. The researchers reported that the study was conducted over a 1-year period with several different treating clinicians and blinded assessors (total not reported).34 The researchers did not report any formal training or reliability measures for these clinicians. The subjects were also instructed to continue with a prescribed home program until a 2 month follow-up. The researchers did not report any procedure to ensure the subjects were following the home program correctly.34 These variables may have influenced the overall outcomes of the study. Upon completion, the researchers found that all groups improved with no significant difference between groups.
IASTM Treatment for joint ROM
Two studies were appraised that measured the effects of IASTM on joint ROM. Both studies reported favourable outcomes but only applied a one session dose of treatment with a short term follow-up. Both studies contained some potential methodological issues that may have influenced the results. First, the IASTM treatment times were different between studies. Laudner et al.37 reported using the Graston® technique which helped determine their treatment time of 40 seconds but the protocol was not completely followed. Markovic14 used the FAT™ technique, but did not report any specific IASTM guidelines. The treatment time of 2 minutes was based upon the comparison intervention of foam rolling which has been found in the literature to enhance hip and knee joint ROM with shorter intervention times.52 Perhaps, a more structured IASTM intervention protocol would have enhanced the outcomes. Second, both studies14,37 measured the immediate post-intervention outcomes with only Markovic14 performing a second ROM assessment 24-hours later which showed that the IASTM group maintained more joint ROM. It is important to note that Markovic14 performed the comprehensive warm-up prior to the 24-hour follow-up which may have influenced the favourable outcomes found. Perhaps, a longer post-intervention assessment period using pre-established time points and more stringent guidelines may have helped to better determined the lasting effects of the IASTM. In comparison, several studies have measured the effects of self-myofascial release using a foam roll or roller massage bar on lower extremity joint ROM.52 The studies measured the post-intervention effects at several pre-established time points and determined that foam rolling and roller massage have positive short-term effects (<10 minutes) on joint ROM.52
Limitations
The main limitation of this systematic review is the paucity and heterogeneity of evidence surrounding IASTM. For example, it is difficult to compare the results of studies utilizing only IASTM therapy versus those utilizing IASTM as part of a treatment protocol with other adjunct therapies (e.g., ultrasound, stretching, exercise, etc.). This problem is further compounded when the IASTM application is used with patient populations who may theoretically respond to IASTM therapy without adjunct therapy (e.g., tendinopathy) and those who likely require adjunct therapy (e.g., chronic ankle instability). Additionally, it is challenging to assess IASTM treatment effectiveness, even when used in isolation, given the inconsistent methodology (e.g., treatment time variation, application of static versus dynamic IASTM treatment, etc.) used across studies. A second limitation is the search criteria for this review which excluded lower level evidence (e.g., case reports) and focused on higher level clinical trials. A third limitation is the literature search only included English language publications which may not have represented all the available evidence from non-English studies or studies currently submitted for publication. Another potential limitation may be the search criteria focusing on IASTM methods utilizing the most homogenous rationale and treatment approach which led to the exclusion Gua sha and ASTYM® for comparison.
Clinical Implications
The heterogeneity among the current IASTM investigations makes it a challenge when attempting to translate the results into clinical practice. The variability in study protocols including the study population, type of IASTM intervention, dosage time, and outcome measures make it difficult to determine the optimal treatment protocol. Five studies 32,34,36–38 reported using the Graston® technique but modified or excluded parts of the protocol. This creates a challenge for the clinician because the Graston® technique is based upon a sequential protocol and the current evidence failed to use this treatment strategy.12 Perhaps, future studies should further define the intervention protocol by stating if the Graston® protocol was followed or just the tools were used. To date, the best available evidence for the Graston® technique is the RCT by Burke et al.35 which followed the complete protocol.
Clinicians may also benefit from reading related research on the myofascial system in order to further understand the postulated physiological mechanisms that occur with the different myofascial therapies. Several authors have contributed to the existing body of knowledge through their research. Notable authors such as Findley53, Stecco54, Langevin55, and Schleip56 have helped to increase our knowledge of this complex system. The reader is referred to the reference section which provides the citations for these authors.
Conclusion
The current evidence of RCTs does not support the efficacy of IASTM for treating certain musculoskeletal pathologies. There is weak evidence supporting the efficacy of IASTM for increasing lower extremity joint ROM for a short period of time. IASTM is a popular form of myofascial therapy but its efficacy has not been fully determined due to the paucity and heterogeneity of evidence. There is a gap between the current research and clinical practice. A consensus has not been established regarding the optimal IASTM program, type of instrument, dosage time, and outcomes measures. Future studies are needed to assess the different IASTM tools and IASTM protocols such as Graston® using strict methodology and fully powered controlled trials. The current evidence seems to lack the methodological rigours necessary to validate the efficacy of IASTM itself or any of the IASTM protocols.
References:
- 1.Baker RT, Hansberger BL, Warren L, et al. A novel approach for the reversal of chronic apparent hamstring tightness: a case report. Int J Sports Phys Ther. 2015;10(5):723–733. [PMC free article] [PubMed] [Google Scholar]
- 2.Baker RT, Nasypany A, Seegmiller JG, et al. Instrument-assisted soft tissue mobilization treatment for tissue extensibility dysfunction. Int J Athl Ther Training. 2013;18(5):16–21. [Google Scholar]
- 3.Loghmani MT, Warden SJ. Instrument-assisted cross fiber massage increases tissue perfusion and alters microvascular morphology in the vicinity of healing knee ligaments. BMC Complem Alternat Med. 2013;13:240. doi: 10.1186/1472-6882-13-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hammer WI. The effect of mechanical load on degenerated soft tissue. J Bodyw Mov Ther. 2008;12(3):246–256. doi: 10.1016/j.jbmt.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 5.Lee JJ, Lee JJ, Kim do H, et al. Inhibitory effects of instrument-assisted neuromobilization on hyperactive gastrocnemius in a hemiparetic stroke patient. Biomed Mater Eng. 2014;24(6):2389–2394. doi: 10.3233/BME-141052. [DOI] [PubMed] [Google Scholar]
- 6.Howitt S, Jung S, Hammonds N. Conservative treatment of a tibialis posterior strain in a novice triathlete: a case report. J Can Chiropr Assoc. 2009;53(1):23–31. [PMC free article] [PubMed] [Google Scholar]
- 7.Strunk RG, Pfefer MT, Dube D. Multimodal chiropractic care of pain and disability for a patient diagnosed with benign joint hypermobility syndrome: a case report. J Chiropr Med. 2014;13(1):35–42. doi: 10.1016/j.jcm.2014.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Papa JA. Conservative management of De Quervain’s stenosing tenosynovitis: a case report. J Can Chiropr Assoc. 2012;56(2):112–120. [PMC free article] [PubMed] [Google Scholar]
- 9.Davidson CJ, Ganion LR, Gehlsen GM, et al. Rat tendon morphologic and functional changes resulting from soft tissue mobilization. Med Sci Sports Exerc. 1997;29(3):313–319. doi: 10.1097/00005768-199703000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Gehlsen GM, Ganion LR, Helfst R. Fibroblast responses to variation in soft tissue mobilization pressure. Med Sci Sports Exerc. 1999;31(4):531–535. doi: 10.1097/00005768-199904000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Loghmani MT, Warden SJ. Instrument-assisted cross-fiber massage accelerates knee ligament healing. J Orthop Sports Phys Ther. 2009;39(7):506–514. doi: 10.2519/jospt.2009.2997. [DOI] [PubMed] [Google Scholar]
- 12.Technique G. Graston Technique: Frequently Asked Qustions. Graston Technique Website. 2016. available at: http://www.grastontechnique.com/FAQs.html. Accessed 1/21/16.
- 13.Stow R. Instrument-assisted soft tissue mobilization. Int J Athl Ther Train. 2011;16(3):5–8. [Google Scholar]
- 14.Markovic G. Acute effects of instrument assisted soft tissue mobilization vs. foam rolling on knee and hip range of motion in soccer players. J Bodyw Mov Ther. 2015;19(4):690–696. doi: 10.1016/j.jbmt.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 15.Lee MS, Choi T-Y, Kim J-I, et al. Using Guasha to treat musculoskeletal pain: A systematic review of controlled clinical trials. Chinese Med. 2010;5:5. doi: 10.1186/1749-8546-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Amshel CE, Caruso DM. Vietnamese “coining”: a burn case report and literature review. J Burn Care Rehabil. 2000;21(2):112–114. [PubMed] [Google Scholar]
- 17.Odhav A, Patel D, Stanford CW, et al. Report of a case of Gua Sha and an awareness of folk remedies. Int J Dermatol. 2013;52:892–898. doi: 10.1111/j.1365-4632.2011.05063.x. [DOI] [PubMed] [Google Scholar]
- 18.Looney B, Srokose T, Fernandez-de-las-Penas C, et al. Graston instrument soft tissue mobilization and home stretching for the management of plantar heel pain: a case series. J Manipulative Physiol Ther. 2011;34(2):138–142. doi: 10.1016/j.jmpt.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 19.White KE. High hamstring tendinopathy in 3 female long distance runners. J Chiropr Med. 2011;10(2):93–99. doi: 10.1016/j.jcm.2010.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCrea EC, George SZ. Outcomes following augmented soft tissue mobilization for patients with knee pain: a case series. Orthop Phys The Pract. 2010;22(2):69–74. [Google Scholar]
- 21.Papa JA. Two cases of work-related lateral epicondylopathy treated with Graston Technique(R) and conservative rehabilitation. J Can Chiropr Assoc. 2012;56(3):192–200. [PMC free article] [PubMed] [Google Scholar]
- 22.Papa JA. Conservative management of Achilles tendinopathy: a case report. J Can Chiropr Assoc. 2012;56(3):216–224. [PMC free article] [PubMed] [Google Scholar]
- 23.Papa JA. Conservative management of a lumbar compression fracture in an osteoporotic patient: a case report. J Can Chiropr Assoc. 2012;56(1):29–39. [PMC free article] [PubMed] [Google Scholar]
- 24.Hudes K. Conservative management of a case of medial epicondylosis in a recreational squash player. J Can Chiropr Assoc. 2011;55:26–29. [PMC free article] [PubMed] [Google Scholar]
- 25.Howell ER. Conservative care of De Quervain’s tenosynovitis/tendinopathy in a warehouse worker and recreational cyclist: a case report. J Can Chiropr Assoc. 2012;56:121–125. [PMC free article] [PubMed] [Google Scholar]
- 26.Miners AL, Bougie TL. Chronic Achilles tendinopathy: a case study of treatment incorporating active and passive tissue warm-up, Graston Technique, ART, eccentric exercise, and cryotherapy. J Can Chiropr Assoc. 2011;55(4):269–279. [PMC free article] [PubMed] [Google Scholar]
- 27.Daniels CJ, Morrell AP. Chiropractic management of pediatric plantar fasciitis: a case report. J Chiropr Med. 2012;11(1):58–63. doi: 10.1016/j.jcm.2011.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Solecki TJ, Herbst EM. Chiropractic management of a postoperative complete anterior cruciate ligament rupture using a multimodal approach: a case report. J Chiropr Med. 2011;10(1):47–53. doi: 10.1016/j.jcm.2010.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hammer WI, Pfefer MT. Treatment of a case of subacute lumbar compartment syndrome using the Graston technique. J Manipulative Physiol Ther. 2005;28(3):199–204. doi: 10.1016/j.jmpt.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 30.Bayliss AJ, Klene FJ, Gundeck EL, et al. Treatment of a patient with post-natal chronic calf pain utilizing instrument-assisted soft tissue mobilization: a case study. J Man Manip Ther. 2011;19(3):127–134. doi: 10.1179/2042618611Y.0000000006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Black DW. Treatment of knee arthrofibrosis and quadriceps insufficiency after patellar tendon repair: a case report including use of the graston technique. Int J Ther Mass Bodyw. 2010;3(2):14–21. [PMC free article] [PubMed] [Google Scholar]
- 32.Blanchette MA, Normand MC. Augmented soft tissue mobilization vs natural history in the treatment of lateral epicondylitis: a pilot study. J Manipulative Physiol Ther. 2011;34(2):123–130. doi: 10.1016/j.jmpt.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 33.Henry P, Panwitz B, Wilson JK. Treatment of a bilateral total knee replacement using augmented soft tissue mobilization. Phys Ther Case Reports. 1999;2(1):27–30. [Google Scholar]
- 34.Brantingham JW, Globe GA, Jensen ML, et al. A feasibility study comparing two chiropractic protocols in the treatment of patellofemoral pain syndrome. J Manipulative Physiol Ther. 2009;32(7):536–548. doi: 10.1016/j.jmpt.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 35.Burke J, Buchberger DJ, Carey-Loghmani MT, et al. A pilot study comparing two manual therapy interventions for carpal tunnel syndrome. J Manipulative Physiol Ther. 2007;30(1):50–61. doi: 10.1016/j.jmpt.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 36.Gulick DT. Influence of instrument assisted soft tissue treatment techniques on myofascial trigger points. J Bodyw Mov Ther. 2014;18(4):602–607. doi: 10.1016/j.jbmt.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 37.Laudner K, Compton BD, McLoda TA, et al. Acute effects of instrument assisted soft tissue mobilization for improving posterior shoulder range of motion in collegiate baseball players. Int J Sports Phys Ther. 2014;9(1):1–7. [PMC free article] [PubMed] [Google Scholar]
- 38.Schaefer JL, Sandrey MA. Effects of a 4-week dynamic-balance-training program supplemented with Graston instrument-assisted soft-tissue mobilization for chronic ankle instability. J Sport Rehabil. 2012;21(4):313–326. doi: 10.1123/jsr.21.4.313. [DOI] [PubMed] [Google Scholar]
- 39.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. w264. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 40.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nielsen A. Gua sha research and the language of integrative medicine. J Bodyw Mov Ther. 2009;13(1):63–72. doi: 10.1016/j.jbmt.2008.04.045. [DOI] [PubMed] [Google Scholar]
- 42.Kivlan BR, Carcia CR, Clemente FR, et al. The effect of Astym(R) Therapy on muscle strength: a blinded, randomized, clinically controlled trial. BMC Musculoskelet Disord. 2015;16:325. doi: 10.1186/s12891-015-0778-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McCormack JR. The management of bilateral high hamstring tendinopathy with ASTYM(R) treatment and eccentric exercise: a case report. J Man Manip Ther. 2012;20(3):142–146. doi: 10.1179/2042618612Y.0000000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sevier TL, Stegink-Jansen CW. Astym treatment vs. eccentric exercise for lateral elbow tendinopathy: a randomized controlled clinical trial. Peer J. 2015;3:e967. doi: 10.7717/peerj.967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maher CG, Sherrington C, Herbert RD, et al. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–721. [PubMed] [Google Scholar]
- 46.Macedo LG, Elkins MR, Maher CG, et al. There was evidence of convergent and construct validity of Physiotherapy Evidence Database quality scale for physiotherapy trials. J Clin Epidemiol. 2010;63(8):920–925. doi: 10.1016/j.jclinepi.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 47.Foley NC, Bhogal SK, Teasell RW, et al. Estimates of quality and reliability with the physiotherapy evidence-based database scale to assess the methodology of randomized controlled trials of pharmacological and nonpharmacological interventions. Phys Ther. 2006;86(6):817–824. [PubMed] [Google Scholar]
- 48.Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37(5):360–363. [PubMed] [Google Scholar]
- 49.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 50.Moseley AM, Elkins MR, Janer-Duncan L, et al. The quality of reports of randomized controlled trials varies between subdisciplines of physiotherapy. Physiother Can. 2014;66(1):36–43. doi: 10.3138/ptc.2012-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sherrington C, Moseley AM, Herbert RD, et al. Ten years of evidence to guide physiotherapy interventions: Physiotherapy Evidence Database (PEDro) Br J Sports Med. 2010;44(12):836–837. doi: 10.1136/bjsm.2009.066357. [DOI] [PubMed] [Google Scholar]
- 52.Cheatham SW, Kolber MJ, Cain M, et al. The effects of self-myofascial release using a foam roll or roller massager on joint range of motion, muscle recovery, and performance: a systematic review. Int J Sports Phys Ther. 2015;10(6):827–838. [PMC free article] [PubMed] [Google Scholar]
- 53.Findley TW. Fascia research from a clinician/scientist’s perspective. Int J Ther Massage Bodywork. 2011;4(4):1–6. doi: 10.3822/ijtmb.v4i4.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Langevin HM, Churchill DL, Cipolla MJ. Mechanical signaling through connective tissue: a mechanism for the therapeutic effect of acupuncture. Faseb J. 2001;15(12):2275–2282. doi: 10.1096/fj.01-0015hyp. [DOI] [PubMed] [Google Scholar]
- 55.Stecco C, Day JA. The fascial manipulation technique and its biomechanical model: a guide to the human fascial system. Int J Ther Massage Bodywork. 2010;3(1):38–40. doi: 10.3822/ijtmb.v3i1.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Stecco C, Schleip R. A fascia and the fascial system. J Bodywork Move Ther. 2016;20(1):139–140. doi: 10.1016/j.jbmt.2015.11.012. [DOI] [PubMed] [Google Scholar]