Abstract
Intermediate filaments together with actin filaments and microtubules form the cytoskeleton, which is a complex and highly dynamic 3D network. Intermediate filaments are the major mechanical stress protectors but also affect cell growth, differentiation, signal transduction, and migration. Using intermediate filament-mitochondrial crosstalk as a prominent example, this review emphasizes the importance of intermediate filaments as crucial organizers of cytoplasmic space to support these functions. We summarize observations in different mammalian cell types which demonstrate how intermediate filaments influence mitochondrial morphology, subcellular localization, and function through direct and indirect interactions and how perturbations of these interactions may lead to human diseases.
Keywords: mitochondrion, mitochondria-associated membrane, intermediate filament, neurofilament, desmin, keratin, vimentin
1. Introduction
In this review we will summarize current knowledge on the interactions between intermediate filaments and mitochondria in different tissues. This topic has been subject of multiple publications in the recent past but has not been systematically reviewed since 2005 [1].
1.1. Intermediate Filaments as Organizers of Cytoplasmic Space
Intermediate filaments are part of the cytoskeleton along with microtubules and actin filaments. They form three-dimensional scaffolds that are arranged in context-dependent networks to provide mechanical resilience. Intermediate filaments can be divided into cytoplasmic intermediate filaments and nuclear lamins. The constitutive intermediate filament proteins are expressed in a cell type- and differentiation-specific manner [2]. Based on their sequence homology, encoding gene structure, charge, assembly mechanism, and expression pattern the following types can be distinguished: epithelial type I and type II keratins; the type III intermediate filament proteins including vimentin, typically expressed in cells of mesenchymal origin, glial fibrillary acidic protein (GFAP) of glial cells, peripherin expressed mainly in neurons of the peripheral nervous system and desmin, which is found in muscle cells; the type IV intermediate filament proteins of neurons such as the three neurofilament proteins; the nuclear type V lamins; and the unusual type VI intermediate filament proteins phakinin and filensin, which form beaded filaments in the lens [2,3,4,5,6].
In addition to the established role of intermediate filaments as major mechanical integrators of cells and tissues, a variety of novel functions have been identified. These include regulation of apoptosis and cell growth, differentiation, signal transduction, and migration. The emerging view is that these functions are a consequence of intermediate filaments acting as organizers of cytoplasmic space. In accordance, intermediate filaments have been shown to determine nuclear shape and to affect the positioning of the Golgi apparatus, mitochondria, transport vesicles, lysosomes, melanosomes, centrosomes, ribosomes, lipid droplets, and junctions between cells and to the extracellular matrix [7,8,9,10,11,12,13,14,15,16]. Very little is known about the mechanistic and molecular nature of these interactions and how their perturbation contributes to the phenotypes of more than 80 human diseases that are caused by mutations in intermediate filament genes [17]. The scheme in Figure 1 portrays three major scenarios: (i) binding of intermediate filaments to cellular components through molecular linkage; (ii) confinement of cellular components by intermediate filament networks; and (iii) bidirectional signaling between cellular components and intermediate filaments.
Figure 1.
Schematic representation of different modes of interaction between intermediate filaments and mitochondria.
1.2. Mitochondrial Trafficking and Shape Changes
Constant ATP supply is essential for virtually all cellular functions. In order to achieve local ATP production, mitochondria accumulate at regions of high-energy demand. Additionally, stationary mitochondria serve as calcium buffers to avoid harmful intracellular calcium spikes. Therefore, not only directed transport but also docking and anchoring mechanisms are needed to achieve the correct distribution of mitochondria. In the past, the contribution of actin filaments and microtubules to mitochondrial transport has been extensively examined [18,19]. For example, mitochondrial movement has been shown to depend on microtubule-associated motor proteins: plus-end-directed kinesin superfamily proteins (KIFs) and minus-end-directed cytoplasmic dynein [20]. Mitochondria attach to motor proteins via motor adaptors (TRAK1/2 or Milton) that are linked to mitochondrial membrane anchors (RhoT1/2 or Miro) [21,22]. Since intermediate filaments are intrinsically apolar they cannot provide directional cues to mitochondrial transport [23].
Immobilized mitochondria are likely anchored to the cytoskeleton. For both, microtubules and actin, mitochondrial docking mechanisms have been described that include mitochondrial membrane anchoring receptors. Anchoring of mitochondria to microtubules via the outer membrane protein syntaphilin arrests them and is regulated by the dynein light chain LC8 [24,25]. In Drosophila, tethering of mitochondria to the actin cytoskeleton reduces their motility and involves the association of myosin V and VI [26]. An increasing number of reports show that intermediate filaments also influence mitochondrial motility that will be discussed in more detail below.
In addition to mitochondrial motility, the mitochondrial shape is critical for mitochondrial function and seems to be influenced by intermediate filament proteins [1,27]. Mitochondrial morphology is determined by the balance between fusion and fission events. The key determinant of mitochondrial fission is the cytoplasmic GTPase Drp1 that can be recruited to mitochondria by several outer mitochondrial membrane proteins such as Fis1 and Mff1 [28,29,30]. Fusion events are mediated by the outer mitochondrial membrane proteins mitofusin 1 and 2 (Mfn1/2) and the inner mitochondrial membrane protein OPA1 [31,32]. Mitochondrial morphology changes in response to alterations in energy demand and nutrient availability. While elongated mitochondria are associated with a sustained and more-efficient ATP production, fragmented mitochondria produce less ATP [33].
2. Interactions of Intermediate Filaments and Mitochondria in Different Cell Types
Almost 40 years ago, several groups described a close spatial association between intermediate filaments and mitochondria in multiple cell types based on electron microscopy studies [34,35,36,37]. It was suggested that the intermediate filament network can serve as an anchorage site for mitochondria [38]. More generally, it was proposed that organelle distribution requires intermediate filaments [39]. Since then, many reports provided further insight how intermediate filaments contribute to mitochondrial localization and function in different cell types (summarized in Table 1).
Table 1.
List of mitochondrial phenotypes observed in cells and tissues harboring intermediate filament network modifications.
| Intermediate Filament Protein | Modification | Cell Type | Mitochondrial Phenotype | Reference |
|---|---|---|---|---|
| NF-L | Knock-Out | Neurons | Decreased length and fusion rate, increased motility | [40] |
| Peripherin | Overexpression | NFL knock-out neurons | Increased retrograde transport of mitochondria | [41] |
| Vimentin | Knock-Out | Fibroblasts | Decreased membrane potential, altered distribution, increased motility | [42,43] |
| Vimentin | Knock-Down | Cos7 cell line | Fragmentation, altered distribution | [44] |
| Desmin | Knock-Out | Cardiac and skeletal muscle | Abnormal shape and positioning, decreased maximal respiration rate, decreased oxygen consumption | [45] |
| Keratin 5 | P24L mutation | Epidermis | Intracellular clustering | [46] |
| Keratin | Knock-Out | Epidermis | Altered lipid composition and activity | [47] |
| Keratin 18 | R89C mutation | Liver-derived cell lines | Fragmentation | [48] |
| Keratin 19 | Knock-Out | Muscle | Mitochondrial disorganization | [49] |
2.1. Lessons Learned from Neurons: Intermediate Filaments Determine Mitochondrial Motility
Neurofilaments are the major intermediate filament proteins in neuronal cells. They are divided into light (NF-L), medium (NF-M), and heavy (NF-H) neurofilament proteins. NF-L associates with either NF-M or NF-H into the 10–12 nm intermediate filaments [50]. Positioning of mitochondria is especially important in axons where they produce not only ATP but also buffer Ca2+ to regulate neurotransmission in associated nerve terminals [51]. Axonal mitochondria can either be transported via microtubules or actin filaments. Only cells lacking both cytoskeletal components show complete mitochondrial arrest [18].
Interestingly, injection of excess neurofilament proteins into cultured neurons also leads to mitochondrial arrest [52]. It was not shown, however, whether this effect is specific to either neurofilament polypeptide. It was later demonstrated that mitochondrial distribution was not affected in neurons of mice expressing a tail-less NF-H mutant, while the full length NF-H induced perinuclear aggregation of mitochondria upon overexpression in cultivated cells [53,54]. The mutant NF-H lacks the highly phosphorylated end domain that is known to form extended sidearms that are involved in axonal intermediate filament arrangement [55,56]. Furthermore, it was shown that this domain of NF-H and also of NF-M competes with microtubule-associated protein 2 (MAP2) for binding to the voltage-dependent anion channel (VDAC) in the outer mitochondrial membrane and may thus affect the mitochondrial membrane potential [57]. Of note, stationary mitochondria have a higher membrane potential than motile mitochondria leading to a higher metabolic activity [58]. Furthermore, stationary mitochondria with higher membrane potential show increased binding to phosphorylated NF-L [59]. Taken together, the experimental findings support the notion that neurofilament binding to mitochondria affects their activity which appears to be linked to reduced mitochondrial mobility. Furthermore, NF-L knock-out mice display not only an increased mitochondrial motility with a reduced frequency of stops but also decreased overall length and fusion rate of mitochondria [40,41]. Overexpression of peripherin in a NF-L deficient background in turn results in a net retrograde transport of mitochondria, probably contributing to the pathology of neurodegenerative disorders with intermediate filament aggregate formation [41].
Moreover, mutations in NF-L lead to a misassembly of neurofilaments and cause devastating Charcot-Marie-Tooth (CMT) neuronal muscular dystrophy disease types 1 and 2 that are characterized by degeneration of long peripheral axons. Mutant NF-L was shown to perturb axonal transport of mitochondria, resulting in accumulation of mitochondria in cell bodies and subsequent impairment of energy supply in distal regions of axons [60]. Interestingly, most of the CMT type 2A cases are caused by mutations of Mfn2 leading to reduced fusion as well as a decline in mitochondrial motility [61,62]. The decrease is explained by the interaction of Mfn2 with the Miro/Milton complex, which has been implicated in the regulation of mitochondrial transport [62]. These findings suggest that NF-L is upstream of Mfn2 and may exert its disease-causing function through perturbed Mfn2 activity.
2.2. Lessons Learned from Mesenchymal Cells: Intermediate Filaments Bind to Mitochondria
The intermediate filament protein vimentin is mainly expressed in cells of mesenchymal origin. Vimentin has been reported to co-localize with mitochondria in several different cell lines [44,63,64,65]. Similar to neurofilaments, vimentin filaments are able to modulate the motile behavior and shape of mitochondria [66].
Intermediate filaments might either bind directly to mitochondria or via intermediate filament-associated proteins. One of the most likely bridging molecules is plectin, a large cytolinker protein that is ubiquitously expressed [67]. Its isoform 1b was shown to mediate vimentin linkage to mitochondria [68]. Plectin 1b knock-out resulted in mitochondrial shape changes with increased elongation but did not affect mitochondrial motility [69]. The latter shows that only some intermediate filament-dependent mitochondrial functions are mediated through plectin.
Interestingly, direct plectin-independent mitochondrial binding was demonstrated for vimentin. This binding is restricted to mitochondria with functional respiratory chain activity [43]. The binding activity was localized to the non-α-helical N-terminal domain of vimentin [42]. This domain meets the requirements for sequences targeted to the outer mitochondrial membrane [70]. As described above, mitochondrial anchoring sites are needed to ensure localized ATP production. Vimentin binding results in arrested mitochondria [42]. Of note, stationary mitochondria possess a higher membrane potential than motile mitochondria. Yet, reducing mitochondrial motility by disruption of actin filaments or microtubules does not change the membrane potential [71]. On the other hand, vimentin-null cells display not only more motile mitochondria but also mitochondria with lower membrane potential, which could be reversed by re-introducing vimentin [71]. Thus, the mitochondrial membrane potential may be regulated by the interaction of the N-terminal domain of vimentin with a still unknown receptor in the outer mitochondrial membrane [43]. The resulting elevation in the mitochondrial membrane potential then leads to enhanced ATP production.
A possible regulatory mechanism of the vimentin-mitochondrial interaction is suggested by findings of the Minin laboratory implicating the GTPase Rac1. They showed that activation of Rac1 induces phosphorylation of vimentin either directly or indirectly via PAK1 [72]. Phosphorylation of vimentin at the mitochondrial binding site, which lies in the most extensively phosphorylated vimentin subdomain, may thereby release motile mitochondria with a decreased membrane potential resulting in reduced ATP production [73].
The pathological relevance of vimentin for mitochondrial motility was recently elucidated in fibroblasts that were derived from patients carrying a mutation in gigaxonin, an E3 ligase adapter that targets intermediate filament proteins for degradation. The vimentin network is collapsed into cytoplasmic aggregates in these cells, leading to the accumulation of mitochondria near the vimentin-containing aggregates. In addition, mitochondrial motility is considerably reduced [74]. The mechanisms by which gigaxonin mutations in gigaxonin lead to these profound effects are not understood.
2.3. Lessons Learned from Muscle Cells: Intermediate Filaments Affect Mitochondrial Calcium Handling and Energy Production
The major intermediate filament protein in muscle cells is desmin. The three-dimensional filamentous desmin cytoskeleton provides highly flexible links between myofibrils and connects them to other intracellular components and the extracellular matrix through specialized contact sites [75]. Ablation of desmin leads to defects in the architecture of the contractile apparatus resulting in myopathy [76]. Desmin intermediate filaments are tethered to the nucleus and mitochondria to maintain their subcellular localization during and after contraction [77]. Desmin null mice helped to further delineate the relationship between intermediate filaments and mitochondria [15,45,78]. The nuclear as well as mitochondrial morphology and localization are disturbed in the absence of desmin [45,79]. Mitochondria of cardiac and skeletal muscle cells showed reduced cristae density along with vacuolization of the mitochondrial matrix and formation of giant mitochondria. Furthermore, extensive mitochondrial proliferation was observed in muscle cells of desmin null mice, especially after work overload [45]. The described mitochondrial phenotypes are recapitulated in patients harboring desmin mutations [80,81].
Altered spatial organization of mitochondria goes along with altered distance to the endo(sarco)plasmic reticulum (ER). Close contacts between mitochondria and ER are referred to as mitochondria-associated membranes (MAMs) [82]. They are involved in lipid traffic between both organelles and in transfer of Ca2+ from the ER to mitochondria through a complex formed by the voltage-dependent anion channel (VDAC) and inositol 1,4,5-trisphophate receptors (IP3Rs) [83,84,85]. Proteomic analysis of mitochondria isolated from heart tissue has shown that several key pathways, including apoptosis, calcium homeostasis, and different metabolic pathways are perturbed in desmin knock-out mice. One of the differentially expressed proteins is VDAC, suggesting a relationship between the desmin-determined structural organization of the cell and mitochondrial functions [86]. In accordance, transgenic mice expressing the aggregation-prone desmin mutant L345P displayed severe alterations of mitochondrial morphology and Ca2+ handling in skeletal and cardiac muscle [79]. Mitochondrial Ca2+ uptake was increased, whereas release was reduced resulting in mitochondrial Ca2+ overload ([79] for contradictory in vitro results see, however, [87]).
While a slight increase in mitochondrial Ca2+ increases ATP production, mitochondrial Ca2+ overload leads to autophagy and apoptosis [88,89]. Members of the Bcl-2 protein family are known to regulate apoptosis [90]. They bind to VDAC and thereby regulate mitochondrial membrane potential and cytochrome c release during apoptosis [91]. The anti-apoptotic Bcl-2 rendered mitochondria more resistant to exposure of high levels of calcium, while desmin knock-out rendered mitochondria more susceptible to high levels of calcium [92]. Bcl-2 expression prevents calcium induced swelling of mitochondria, subsequent cytochrome c release and hence apoptosis induction [93]. Consequently and quite remarkably, Bcl-2 overexpression in desmin null cardiomyocytes of transgenic mice rescued the mitochondrial defects and ameliorated the overall cardiomyopathy [94].
In mitochondria of desmin null heart, creatine kinase activity was elevated [95]. Creatine phosphate, an important cellular energy source, is produced by mitochondrial creatine kinase that resides in the mitochondrial intermembrane space to buffer high ATP levels in cells with high and fluctuating energy requirements. Creatine phosphate is processed by cytosolic creatine kinases to ensure sufficient ATP supply in situations of sudden energy demands. Mitochondrial creatine kinase is near to VDAC that is localized in the outer mitochondrial membrane and the adenine nucleotide translocator (ANT) of the inner mitochondrial membrane. The complex of the three proteins is essential for facilitating the transport of ATP from the mitochondrial matrix to the mitochondrial intermembrane space and, conversely, the transport of ADP from the mitochondrial intermembrane space into the mitochondrial matrix which is referred to as metabolite channeling or functional coupling [96]. In soleus muscle, desmin ablation leads to an uncoupling of mitochondrial creatine kinase and ANT [45]. As a consequence ADP is reduced in the mitochondrial matrix leading to a lower ADP-stimulated respiratory rate and, hence, reduced ATP production. Accordingly, the number of mitochondria with lower ADP-stimulated respiratory rates is increased in striated muscles of desmin knock-out animals resulting in an overall decrease in respiratory capacity [97].
2.4. Lessons Learned in Epithelia: Intermediate Filaments Affect Mitochondrial Lipid Metabolism and Communicate through Signaling with Mitochondria
The expression of keratin intermediate filament proteins is a hallmark of epithelial differentiation. Keratins are subdivided into type I and type II proteins that form obligate heteropolymers in a cell type-, differentiation-, and tissue-specific manner. Simple epithelia, as found in liver, pancreas, and intestine, express the keratin pair keratin 8 and 18 or 19, whereas the stratified epithelium of the skin, the epidermis, expresses a more complex pattern of different keratin pairs depending on the epidermal layer and the status of the keratinocytes [98]. Patients harboring mutations in keratins 5 and 14, the major keratins in the basal layer of the epidermis, develop epidermolysis bullosa simplex (EBS). EBS is characterized by severe blistering due to impaired mechanical stress resilience [99]. Mitochondria of these keratinocytes are abnormally concentrated around the nucleus [46,100].
The lipid composition of keratin-depleted keratinocytes has been shown to be considerably altered [47]. The nonbilayer-forming lipids cardiolipin and phosphatidyl ethanolamine, which are produced in mitochondria, are elevated. The precursors for both lipids are imported from the ER through mitochondria-associated membranes (MAMs) [82,83,101]. An interesting observation in this context is the finding that the keratin-binding protein trichoplein/mitostatin has been shown to function as a regulator of ER-mitochondrium tethering [102,103]. This may be the reason why mitochondrial lipid homeostasis is severely perturbed in the absence of keratins and may also explain the other observed alterations in mitochondrial structure and function [47,104,105].
When livers of keratin 8 knock-out mice were compared to wild type controls changes in mitochondrial morphology were readily detectable. Mitochondria were significantly smaller and irregularly distributed [106]. One possible mechanism by which the distribution of mitochondria is modulated is the formation of a complex consisting of Pirh2 and keratins 8 and 18. Pirh2 is a RING-H2-type ubiquitin E3 ligase, that targets p53 for degradation and was shown to regulate intermediate filament organization [107,108]. Knock-down of either keratin 8/18 or Pirh2 leads to an abnormal juxtanuclear clustering of mitochondria as well as enhanced apoptosis. Expression of the mutant keratin 18 R89C in liver epithelial cells leads to mitochondrial fragmentation, a hallmark of apoptosis [48,109].
The influence of keratin-mediated mitochondrial changes also extends to alterations of mitochondrial hexokinase expression [110]. Keratin-deficient hepatocytes display increased levels of mitochondrial hexokinase leading to increased glycogen content. A possible explanation is that loss of keratins releases PKC which is bound through RACK1 [111]. The released PKC may then phosphorylate VDAC. Phosphorylated VDAC in turn recruits hexokinase [112].
3. Conclusions and Future Directions
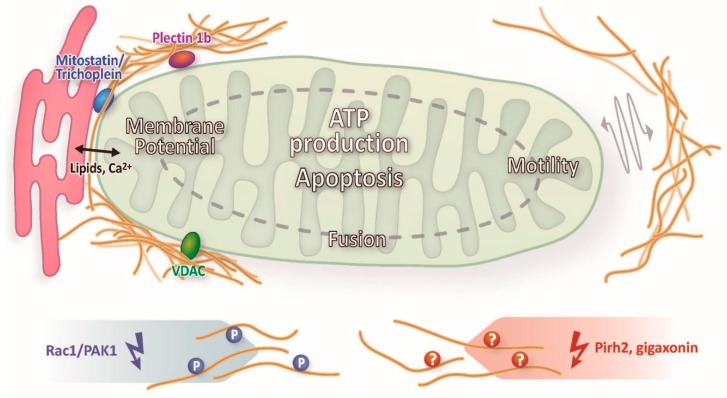
Taken together, convincing evidence has accumulated over the years that intermediate filaments influence the motility, shape and, more importantly, function of mitochondria in different cell types. The scheme in Figure 2 summarizes the described modes of interaction of intermediate filaments and mitochondria and their consequences. Yet, an overall concept of the mechanistic details is still lacking.
Figure 2.
Schematic synopsis of different modes of interaction between intermediate filaments and mitochondria and their consequences as described in this review.
For example, we would like to know whether intermediate filament proteins other than vimentin bind directly to mitochondria. If so, what are the mitochondrial binding sites? Are they mitochondrial-associated membrane components such as VDAC? Are other molecules involved such as plectin and trichoplein/mitostatin? This scenario would provide an explanation how intermediate filaments affect lipid metabolism and Ca2+ signaling. In addition, intermediate filaments could control the opening of the mitochondrial permeability transition pore through the same or other interactions and thereby affect apoptosis. In the same vein, it has been suggested recently that mitochondria-associated membranes function as hubs for neurodegeneration, notably in Charcot-Marie-Tooth disease [113].
One would also like to know more about the details of mitochondrial motility control through intermediate filaments and the resulting metabolic alterations. Do intermediate filaments merely provide an inert 3D scaffold or do they represent adjustable docking stations? How do these interactions affect mitochondrial shape? What role do posttranslational intermediate filament protein modifications play in this context [114]?
What role does intermediate filament-dependent subcellular localization of mitochondria play for cellular function? Obvious examples include the local production and availability of ATP in striated muscle cells, neuronal synapses, or migrating cells [60,97,115,116,117]. The relevance may well extend to multiple disease situations such as metastatic tumor cell migration [118,119].
Acknowledgments
Our work is supported by the German Research Council (DFG), the EU, and IZKF RWTH Aachen University. The authors thank Adam Breitscheidel for designing the schemes in Figure 1 and Figure 2.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Toivola D.M., Tao G.-Z., Habtezion A., Liao J., Omary M.B. Cellular integrity plus: organelle-related and protein-targeting functions of intermediate filaments. Trends Cell Biol. 2005;15:608–617. doi: 10.1016/j.tcb.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 2.Herrmann H., Strelkov S.V., Burkhard P., Aebi U. Intermediate filaments: Primary determinants of cell architecture and plasticity. J. Clin. Investig. 2009;119:1772–1783. doi: 10.1172/JCI38214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coulombe P.A., Wong P. Cytoplasmic intermediate filaments revealed as dynamic and multipurpose scaffolds. Nat. Cell Biol. 2004;6:699–706. doi: 10.1038/ncb0804-699. [DOI] [PubMed] [Google Scholar]
- 4.Moll R., Divo M., Langbein L. The human keratins: biology and pathology. Histochem. Cell Biol. 2008;129:705–733. doi: 10.1007/s00418-008-0435-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bragulla H.H., Homberger D.G. Structure and functions of keratin proteins in simple, stratified, keratinized and cornified epithelia. J. Anat. 2009;214:516–559. doi: 10.1111/j.1469-7580.2009.01066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karantza V. Keratins in health and cancer: More than mere epithelial cell markers. Oncogene. 2011;30:127–138. doi: 10.1038/onc.2010.456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bauer C., Traub P. Interaction of intermediate filaments with ribosomes in vitro. Eur. J. Cell Biol. 1995;68:288–296. [PubMed] [Google Scholar]
- 8.Chang L., Barlan K., Chou Y.-H., Grin B., Lakonishok M., Serpinskaya A.S., Shumaker D.K., Herrmann H., Gelfand V.I., Goldman R.D. The dynamic properties of intermediate filaments during organelle transport. J. Cell Sci. 2009;122:2914–2923. doi: 10.1242/jcs.046789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guo Y., Zheng Y. Lamins position the nuclear pores and centrosomes by modulating dynein. Mol. Biol. Cell. 2015;26:3379–3389. doi: 10.1091/mbc.E15-07-0482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kumemura H., Harada M., Omary M.B., Sakisaka S., Suganuma T., Namba M., Sata M. Aggregation and loss of cytokeratin filament networks inhibit Golgi organization in liver-derived epithelial cell lines. Cell Motil. Cytoskeleton. 2004;57:37–52. doi: 10.1002/cm.10152. [DOI] [PubMed] [Google Scholar]
- 11.Mayerson P.L., Brumbaugh J.A. Lavender, a chick melanocyte mutant with defective melanosome translocation: A possible role for 10 nm filaments and microfilaments but not microtubules. J. Cell Sci. 1981;51:25–51. doi: 10.1242/jcs.51.1.25. [DOI] [PubMed] [Google Scholar]
- 12.Sarria A.J., Lieber J.G., Nordeen S.K., Evans R.M. The presence or absence of a vimentin-type intermediate filament network affects the shape of the nucleus in human SW-13 cells. J. Cell Sci. 1994;107:1593–1607. doi: 10.1242/jcs.107.6.1593. [DOI] [PubMed] [Google Scholar]
- 13.Styers M.L., Salazar G., Love R., Peden A.A., Kowalczyk A.P., Faundez V. The Endo-Lysosomal Sorting Machinery Interacts with the Intermediate Filament Cytoskeleton. Mol. Biol. Cell. 2004;15:5369–5382. doi: 10.1091/mbc.E04-03-0272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seltmann K., Roth W., Kröger C., Loschke F., Lederer M., Hüttelmaier S., Magin T.M. Keratins Mediate Localization of Hemidesmosomes and Repress Cell Motility. J. Investig. Dermatol. 2013;133:181–190. doi: 10.1038/jid.2012.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Milner D.J., Weitzer G., Tran D., Bradley A., Capetanaki Y. Disruption of muscle architecture and myocardial degeneration in mice lacking desmin. J. Cell Biol. 1996;134:1255–1270. doi: 10.1083/jcb.134.5.1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lieber J.G., Evans R.M. Disruption of the vimentin intermediate filament system during adipose conversion of 3T3-L1 cells inhibits lipid droplet accumulation. J. Cell Sci. 1996;109:3047–3058. doi: 10.1242/jcs.109.13.3047. [DOI] [PubMed] [Google Scholar]
- 17.Omary M.B. “IF-pathies”: A broad spectrum of intermediate filament-associated diseases. J. Clin. Investig. 2009;119:1756–1762. doi: 10.1172/JCI39894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morris R.L., Hollenbeck P.J. Axonal transport of mitochondria along microtubules and F-actin in living vertebrate neurons. J. Cell Biol. 1995;131:1315–1326. doi: 10.1083/jcb.131.5.1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sheng Z.-H., Cai Q. Mitochondrial transport in neurons: Impact on synaptic homeostasis and neurodegeneration. Nat. Rev. Neurosci. 2012;13:77–93. doi: 10.1038/nrn3156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sheng Z.-H. Mitochondrial trafficking and anchoring in neurons: New insight and implications. J. Cell Biol. 2014;204:1087–1098. doi: 10.1083/jcb.201312123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stowers R.S., Megeath L.J., Górska-Andrzejak J., Meinertzhagen I.A., Schwarz T.L. Axonal Transport of Mitochondria to Synapses Depends on Milton, a Novel Drosophila Protein. Neuron. 2002;36:1063–1077. doi: 10.1016/S0896-6273(02)01094-2. [DOI] [PubMed] [Google Scholar]
- 22.Glater E.E., Megeath L.J., Stowers R.S., Schwarz T.L. Axonal transport of mitochondria requires milton to recruit kinesin heavy chain and is light chain independent. J. Cell Biol. 2006;173:545–557. doi: 10.1083/jcb.200601067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Herrmann H., Aebi U. Intermediate Filaments: Molecular Structure, Assembly Mechanism, and Integration into Functionally Distinct Intracellular Scaffolds. Annu. Rev. Biochem. 2004;73:749–789. doi: 10.1146/annurev.biochem.73.011303.073823. [DOI] [PubMed] [Google Scholar]
- 24.Kang J.-S., Tian J.-H., Pan P.-Y., Zald P., Li C., Deng C., Sheng Z.-H. Docking of Axonal Mitochondria by Syntaphilin Controls Their Mobility and Affects Short-Term Facilitation. Cell. 2008;132:137–148. doi: 10.1016/j.cell.2007.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen Y.-M., Gerwin C., Sheng Z.-H. Dynein Light Chain LC8 Regulates Syntaphilin-Mediated Mitochondrial Docking in Axons. J. Neurosci. 2009;29:9429–9438. doi: 10.1523/JNEUROSCI.1472-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pathak D., Sepp K.J., Hollenbeck P.J. Evidence That Myosin Activity Opposes Microtubule-Based Axonal Transport of Mitochondria. J. Neurosci. 2010;30:8984–8992. doi: 10.1523/JNEUROSCI.1621-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Campello S., Scorrano L. Mitochondrial shape changes: Orchestrating cell pathophysiology. EMBO Rep. 2010;11:678–684. doi: 10.1038/embor.2010.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smirnova E., Griparic L., Shurland D.-L., van der Bliek A.M. Dynamin-related Protein Drp1 Is Required for Mitochondrial Division in Mammalian Cells. Mol. Biol. Cell. 2001;12:2245–2256. doi: 10.1091/mbc.12.8.2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.James D.I., Parone P.A., Mattenberger Y., Martinou J.-C. hFis1, a Novel Component of the Mammalian Mitochondrial Fission Machinery. J. Biol. Chem. 2003;278:36373–36379. doi: 10.1074/jbc.M303758200. [DOI] [PubMed] [Google Scholar]
- 30.Gandre-Babbe S., van der Bliek A.M. The Novel Tail-anchored Membrane Protein Mff Controls Mitochondrial and Peroxisomal Fission in Mammalian Cells. Mol. Biol. Cell. 2008;19:2402–2412. doi: 10.1091/mbc.E07-12-1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Santel A., Fuller M.T. Control of mitochondrial morphology by a human mitofusin. J. Cell Sci. 2001;114:867–874. doi: 10.1242/jcs.114.5.867. [DOI] [PubMed] [Google Scholar]
- 32.Cipolat S., de Brito O.M., Zilio B.D., Scorrano L. OPA1 requires mitofusin 1 to promote mitochondrial fusion. Proc. Natl. Acad. Sci. USA. 2004;101:15927–15932. doi: 10.1073/pnas.0407043101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rossignol R., Gilkerson R., Aggeler R., Yamagata K., Remington S.J., Capaldi R.A. Energy Substrate Modulates Mitochondrial Structure and Oxidative Capacity in Cancer Cells. Cancer Res. 2004;64:985–993. doi: 10.1158/0008-5472.CAN-03-1101. [DOI] [PubMed] [Google Scholar]
- 34.Lehto V.-P., Virtanen I. Association of intermediate filaments with other cell organelles in carcinoid tumor of the colon. Experientia. 1979;35:35–36. doi: 10.1007/BF01917860. [DOI] [PubMed] [Google Scholar]
- 35.Toh B.H., Lolait S.J., Mathy J.P., Baum R. Association of mitochondria with intermediate filaments and of polyribosomes with cytoplasmic actin. Cell Tissue Res. 1980;211:163–169. doi: 10.1007/BF00233731. [DOI] [PubMed] [Google Scholar]
- 36.David-Ferreira K.L., David-Ferreira J.F. Association between intermediate-sized filaments and mitochondria in rat Leydig cells. Cell Biol. Int. Rep. 1980;4:655–662. doi: 10.1016/0309-1651(80)90204-0. [DOI] [PubMed] [Google Scholar]
- 37.Hirokawa N. Cross-linker system between neurofilaments, microtubules and membranous organelles in frog axons revealed by the quick-freeze, deep-etching method. J. Cell Biol. 1982;94:129–142. doi: 10.1083/jcb.94.1.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mose-Larsen P., Bravo R., Fey S.J., Small J.V., Celis J.E. Putative association of mitochondria with a subpopulation of intermediate-sized filaments in cultured human skin fibroblasts. Cell. 1982;31:681–692. doi: 10.1016/0092-8674(82)90323-3. [DOI] [PubMed] [Google Scholar]
- 39.Eckert B.S. Alteration of the distribution of intermediate filaments in PtK1 cells by acrylamide II: Effect on the organization of cytoplasmic organelles. Cell Motil. Cytoskeleton. 1986;6:15–24. doi: 10.1002/cm.970060104. [DOI] [PubMed] [Google Scholar]
- 40.Gentil B.J., Minotti S., Beange M., Baloh R.H., Julien J.-P., Durham H.D. Normal role of the low-molecular-weight neurofilament protein in mitochondrial dynamics and disruption in Charcot-Marie-Tooth disease. FASEB J. 2012;26:1194–1203. doi: 10.1096/fj.11-196345. [DOI] [PubMed] [Google Scholar]
- 41.Perrot R., Julien J.-P. Real-time imaging reveals defects of fast axonal transport induced by disorganization of intermediate filaments. FASEB J. 2009;23:3213–3225. doi: 10.1096/fj.09-129585. [DOI] [PubMed] [Google Scholar]
- 42.Nekrasova O.E., Mendez M.G., Chernoivanenko I.S., Tyurin-Kuzmin P.A., Kuczmarski E.R., Gelfand V.I., Goldman R.D., Minin A.A. Vimentin intermediate filaments modulate the motility of mitochondria. Mol. Biol. Cell. 2011;22:2282–2289. doi: 10.1091/mbc.E10-09-0766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chernoivanenko I.S., Matveeva E.A., Gelfand V.I., Goldman R.D., Minin A.A. Mitochondrial membrane potential is regulated by vimentin intermediate filaments. FASEB J. 2015;29:820–827. doi: 10.1096/fj.14-259903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tang H.L., Lung H.L., Wu K.C., Le A.-H.P., Tang H.M., Fung M.C. Vimentin supports mitochondrial morphology and organization. Biochem. J. 2008;410:141–146. doi: 10.1042/BJ20071072. [DOI] [PubMed] [Google Scholar]
- 45.Milner D.J., Mavroidis M., Weisleder N., Capetanaki Y. Desmin Cytoskeleton Linked to Muscle Mitochondrial Distribution and Respiratory Function. J. Cell Biol. 2000;150:1283–1298. doi: 10.1083/jcb.150.6.1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Uttam J., Hutton E., Coulombe P.A., Anton-Lamprecht I., Yu Q.C., Gedde-Dahl T., Fine J.D., Fuchs E. The genetic basis of epidermolysis bullosa simplex with mottled pigmentation. Proc. Natl. Acad. Sci. USA. 1996;93:9079–9084. doi: 10.1073/pnas.93.17.9079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kumar V., Bouameur J.-E., Bär J., Rice R.H., Hornig-Do H.-T., Roop D.R., Schwarz N., Brodesser S., Thiering S., Leube R.E., et al. A keratin scaffold regulates epidermal barrier formation, mitochondrial lipid composition, and activity. J. Cell Biol. 2015;211:1057–1075. doi: 10.1083/jcb.201404147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kumemura H., Harada M., Yanagimoto C., Koga H., Kawaguchi T., Hanada S., Taniguchi E., Ueno T., Sata M. Mutation in keratin 18 induces mitochondrial fragmentation in liver-derived epithelial cells. Biochem. Biophys. Res. Commun. 2008;367:33–40. doi: 10.1016/j.bbrc.2007.12.116. [DOI] [PubMed] [Google Scholar]
- 49.Stone M.R., O’Neill A., Lovering R.M., Strong J., Resneck W.G., Reed P.W., Toivola D.M., Ursitti J.A., Omary M.B., Bloch R.J. Absence of keratin 19 in mice causes skeletal myopathy with mitochondrial and sarcolemmal reorganization. J. Cell Sci. 2007;120:3999–4008. doi: 10.1242/jcs.009241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Scott D., Smith K.E., O’Brien B.J., Angelides K.J. Characterization of mammalian neurofilament triplet proteins. Subunit stoichiometry and morphology of native and reconstituted filaments. J. Biol. Chem. 1985;260:10736–10747. [PubMed] [Google Scholar]
- 51.David G., Barrett J.N., Barrett E.F. Evidence that mitochondria buffer physiological Ca2+ loads in lizard motor nerve terminals. J. Physiol. 1998;509:59–65. doi: 10.1111/j.1469-7793.1998.059bo.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Straube-West K., Loomis P.A., Opal P., Goldman R.D. Alterations in neural intermediate filament organization: functional implications and the induction of pathological changes related to motor neuron disease. J. Cell Sci. 1996;109:2319–2329. doi: 10.1242/jcs.109.9.2319. [DOI] [PubMed] [Google Scholar]
- 53.Rao M.V., Garcia M.L., Miyazaki Y., Gotow T., Yuan A., Mattina S., Ward C.M., Calcutt N.A., Uchiyama Y., Nixon R.A., et al. Gene replacement in mice reveals that the heavily phosphorylated tail of neurofilament heavy subunit does not affect axonal caliber or the transit of cargoes in slow axonal transport. J. Cell Biol. 2002;158:681–693. doi: 10.1083/jcb.200202037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Szebenyi G., Smith G.M., Li P., Brady S.T. Overexpression of neurofilament H disrupts normal cell structure and function. J. Neurosci. Res. 2002;68:185–198. doi: 10.1002/jnr.10212. [DOI] [PubMed] [Google Scholar]
- 55.Julien J.P., Mushynski W.E. The distribution of phosphorylation sites among identified proteolytic fragments of mammalian neurofilaments. J. Biol. Chem. 1983;258:4019–4025. [PubMed] [Google Scholar]
- 56.Hisanaga S., Hirokawa N. Structure of the peripheral domains of neurofilaments revealed by low angle rotary shadowing. J. Mol. Biol. 1988;202:297–305. doi: 10.1016/0022-2836(88)90459-7. [DOI] [PubMed] [Google Scholar]
- 57.Leterrier J.F., Rusakov D.A., Nelson B.D., Linden M. Interactions between brain mitochondria and cytoskeleton: Evidence for specialized outer membrane domains involved in the association of cytoskeleton-associated proteins to mitochondria in situ and in vitro. Microsc. Res. Tech. 1994;27:233–261. doi: 10.1002/jemt.1070270305. [DOI] [PubMed] [Google Scholar]
- 58.Overly C.C., Rieff H.I., Hollenbeck P.J. Organelle motility and metabolism in axons vs. dendrites of cultured hippocampal neurons. J. Cell Sci. 1996;109:971–980. doi: 10.1242/jcs.109.5.971. [DOI] [PubMed] [Google Scholar]
- 59.Wagner O.I., Lifshitz J., Janmey P.A., Linden M., McIntosh T.K., Leterrier J.-F. Mechanisms of Mitochondria-Neurofilament Interactions. J. Neurosci. 2003;23:9046–9058. doi: 10.1523/JNEUROSCI.23-27-09046.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Brownlees J. Charcot-Marie-Tooth disease neurofilament mutations disrupt neurofilament assembly and axonal transport. Hum. Mol. Genet. 2002;11:2837–2844. doi: 10.1093/hmg/11.23.2837. [DOI] [PubMed] [Google Scholar]
- 61.Züchner S., Mersiyanova I.V., Muglia M., Bissar-Tadmouri N., Rochelle J., Dadali E.L., Zappia M., Nelis E., Patitucci A., Senderek J., et al. Mutations in the mitochondrial GTPase mitofusin 2 cause Charcot-Marie-Tooth neuropathy type 2A. Nat. Genet. 2004;36:449–451. doi: 10.1038/ng1341. [DOI] [PubMed] [Google Scholar]
- 62.Misko A., Jiang S., Wegorzewska I., Milbrandt J., Baloh R.H. Mitofusin 2 Is Necessary for Transport of Axonal Mitochondria and Interacts with the Miro/Milton Complex. J. Neurosci. 2010;30:4232–4240. doi: 10.1523/JNEUROSCI.6248-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Summerhayes I.C., Wong D., Chen L.B. Effect of microtubules and intermediate filaments on mitochondrial distribution. J. Cell Sci. 1983;61:87–105. doi: 10.1242/jcs.61.1.87. [DOI] [PubMed] [Google Scholar]
- 64.Almahbobi G., Williams L.J., Han X.-G., Hall P.F. Binding of lipid droplets and mitochondria to intermediate filaments in rat Leydig cells. J. Reprod. Fertil. 1993;98:209–217. doi: 10.1530/jrf.0.0980209. [DOI] [PubMed] [Google Scholar]
- 65.Collier N.C., Sheetz M.P., Schlesinger M.J. Concomitant changes in mitochondria and intermediate filaments during heat shock and recovery of chicken embryo fibroblasts. J. Cell. Biochem. 1993;52:297–307. doi: 10.1002/jcb.240520306. [DOI] [PubMed] [Google Scholar]
- 66.Tolstonog G.V., Belichenko-Weitzmann I.V., Lu J.-P., Hartig R., Shoeman R.L., Taub U., Traub P. Spontaneously Immortalized Mouse Embryo Fibroblasts: Growth Behavior of Wild-Type and Vimentin-Deficient Cells in Relation to Mitochondrial Structure and Activity. DNA Cell Biol. 2005;24:680–709. doi: 10.1089/dna.2005.24.680. [DOI] [PubMed] [Google Scholar]
- 67.Wiche G., Krepler R., Artlieb U., Pytela R., Denk H. Occurrence and immunolocalization of plectin in tissues. J. Cell Biol. 1983;97:887–901. doi: 10.1083/jcb.97.3.887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rezniczek G.A., Abrahamsberg C., Fuchs P., Spazierer D., Wiche G. Plectin 5′-transcript diversity: short alternative sequences determine stability of gene products, initiation of translation and subcellular localization of isoforms. Hum. Mol. Genet. 2003;12:3181–3194. doi: 10.1093/hmg/ddg345. [DOI] [PubMed] [Google Scholar]
- 69.Winter L., Abrahamsberg C., Wiche G. Plectin isoform 1b mediates mitochondrion-intermediate filament network linkage and controls organelle shape. J. Cell Biol. 2008;181:903–911. doi: 10.1083/jcb.200710151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rapaport D. Finding the right organelle: Targeting signals in mitochondrial outer-membrane proteins. EMBO Rep. 2003;4:948–952. doi: 10.1038/sj.embor.embor937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chernoivanenko I.S., Matveeva E.A., Minin A.A. Vimentin intermediate filaments increase mitochondrial membrane potential. Biochem. Mosc. Suppl. Ser. Membr. Cell Biol. 2011;5:21–28. doi: 10.1134/S1990747811010041. [DOI] [Google Scholar]
- 72.Matveeva E.A., Venkova L.S., Chernoivanenko I.S., Minin A.A. Vimentin is involved in regulation of mitochondrial motility and membrane potential by Rac1. Biol. Open. 2015;4:1290–1297. doi: 10.1242/bio.011874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Izawa I., Inagaki M. Regulatory mechanisms and functions of intermediate filaments: A study using site- and phosphorylation state-specific antibodies. Cancer Sci. 2006;97:167–174. doi: 10.1111/j.1349-7006.2006.00161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lowery J., Jain N., Kuczmarski E.R., Mahammad S., Goldman A., Gelfand V.I., Opal P., Goldman R.D. Abnormal Intermediate Filament Organization Alters Mitochondrial Motility in Giant Axonal Neuropathy Fibroblasts. Mol. Biol. Cell. 2015 doi: 10.1091/mbc.E15-09-0627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Capetanaki Y., Bloch R.J., Kouloumenta A., Mavroidis M., Psarras S. Muscle intermediate filaments and their links to membranes and membranous organelles. Exp. Cell Res. 2007;313:2063–2076. doi: 10.1016/j.yexcr.2007.03.033. [DOI] [PubMed] [Google Scholar]
- 76.Thornell L.-E., Carlsson L., Li Z., Mericskay M., Paulin D. Null Mutation in the Desmin Gene Gives Rise to a Cardiomyopathy. J. Mol. Cell. Cardiol. 1997;29:2107–2124. doi: 10.1006/jmcc.1997.0446. [DOI] [PubMed] [Google Scholar]
- 77.Stromer M.H., Bendayan M. Immunocytochemical identification of cytoskeletal linkages to smooth muscle cell nuclei and mitochondria. Cell Motil. Cytoskeleton. 1990;17:11–18. doi: 10.1002/cm.970170104. [DOI] [PubMed] [Google Scholar]
- 78.Li Z., Colucci-Guyon E., Pinçon-Raymond M., Mericskay M., Pournin S., Paulin D., Babinet C. Cardiovascular Lesions and Skeletal Myopathy in Mice Lacking Desmin. Dev. Biol. 1996;175:362–366. doi: 10.1006/dbio.1996.0122. [DOI] [PubMed] [Google Scholar]
- 79.Kostareva A., Sjöberg G., Bruton J., Zhang S.-J., Balogh J., Gudkova A., Hedberg B., Edström L., Westerblad H., Sejersen T. Mice expressing L345P mutant desmin exhibit morphological and functional changes of skeletal and cardiac mitochondria. J. Muscle Res. Cell Motil. 2008;29:25–36. doi: 10.1007/s10974-008-9139-8. [DOI] [PubMed] [Google Scholar]
- 80.Schröder R., Goudeau B., Simon M.C., Fischer D., Eggermann T., Clemen C.S., Li Z., Reimann J., Xue Z., Rudnik-Schöneborn S., et al. On noxious desmin: functional effects of a novel heterozygous desmin insertion mutation on the extrasarcomeric desmin cytoskeleton and mitochondria. Hum. Mol. Genet. 2003;12:657–669. doi: 10.1093/hmg/ddg060. [DOI] [PubMed] [Google Scholar]
- 81.Henderson M., Waele L.D., Hudson J., Eagle M., Sewry C., Marsh J., Charlton R., He L., Blakely E.L., Horrocks I., et al. Recessive desmin-null muscular dystrophy with central nuclei and mitochondrial abnormalities. Acta Neuropathol. (Berl.) 2013;125:917–919. doi: 10.1007/s00401-013-1113-x. [DOI] [PubMed] [Google Scholar]
- 82.Vance J.E. MAM (mitochondria-associated membranes) in mammalian cells: Lipids and beyond. Biochim. Biophys. Acta. 2014;1841:595–609. doi: 10.1016/j.bbalip.2013.11.014. [DOI] [PubMed] [Google Scholar]
- 83.Achleitner G., Gaigg B., Krasser A., Kainersdorfer E., Kohlwein S.D., Perktold A., Zellnig G., Daum G. Association between the endoplasmic reticulum and mitochondria of yeast facilitates interorganelle transport of phospholipids through membrane contact. Eur. J. Biochem. 1999;264:545–553. doi: 10.1046/j.1432-1327.1999.00658.x. [DOI] [PubMed] [Google Scholar]
- 84.Filippin L., Magalhães P.J., Benedetto G.D., Colella M., Pozzan T. Stable Interactions between Mitochondria and Endoplasmic Reticulum Allow Rapid Accumulation of Calcium in a Subpopulation of Mitochondria. J. Biol. Chem. 2003;278:39224–39234. doi: 10.1074/jbc.M302301200. [DOI] [PubMed] [Google Scholar]
- 85.Szabadkai G., Bianchi K., Várnai P., Stefani D.D., Wieckowski M.R., Cavagna D., Nagy A.I., Balla T., Rizzuto R. Chaperone-mediated coupling of endoplasmic reticulum and mitochondrial Ca2+ channels. J. Cell Biol. 2006;175:901–911. doi: 10.1083/jcb.200608073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Fountoulakis M., Soumaka E., Rapti K., Mavroidis M., Tsangaris G., Maris A., Weisleder N., Capetanaki Y. Alterations in the heart mitochondrial proteome in a desmin null heart failure model. J. Mol. Cell. Cardiol. 2005;38:461–474. doi: 10.1016/j.yjmcc.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 87.Smolina N., Bruton J., Sjoberg G., Kostareva A., Sejersen T. Aggregate-prone desmin mutations impair mitochondrial calcium uptake in primary myotubes. Cell Calcium. 2014;56:269–275. doi: 10.1016/j.ceca.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 88.McCormack J.G., Denton R.M. Intracellular calcium ions and intramitochondrial Ca in the regulation of energy metabolism in mammalian tissues. Proc. Nutr. Soc. 1990;49:57–75. doi: 10.1079/PNS19900009. [DOI] [PubMed] [Google Scholar]
- 89.Cárdenas C., Miller R.A., Smith I., Bui T., Molgó J., Müller M., Vais H., Cheung K.-H., Yang J., Parker I., et al. Essential Regulation of Cell Bioenergetics by Constitutive InsP3 Receptor Ca2+ Transfer to Mitochondria. Cell. 2010;142:270–283. doi: 10.1016/j.cell.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Siddiqui W.A., Ahad A., Ahsan H. The mystery of BCL2 family: Bcl-2 proteins and apoptosis: An update. Arch. Toxicol. 2015;89:289–317. doi: 10.1007/s00204-014-1448-7. [DOI] [PubMed] [Google Scholar]
- 91.Shimizu S., Narita M., Tsujimoto Y. Bcl-2 family proteins regulate the release of apoptogenic cytochrome c by the mitochondrial channel VDAC. Nature. 1999;399:483–487. doi: 10.1038/20959. [DOI] [PubMed] [Google Scholar]
- 92.Zhu L., Ling S., Yu X.-D., Venkatesh L.K., Subramanian T., Chinnadurai G., Kuo T.H. Modulation of Mitochondrial Ca2+ Homeostasis by Bcl-2. J. Biol. Chem. 1999;274:33267–33273. doi: 10.1074/jbc.274.47.33267. [DOI] [PubMed] [Google Scholar]
- 93.Pinton P., Ferrari D., Rapizzi E., Virgilio F.D., Pozzan T., Rizzuto R. The Ca2+ concentration of the endoplasmic reticulum is a key determinant of ceramide-induced apoptosis: Significance for the molecular mechanism of Bcl-2 action. EMBO J. 2001;20:2690–2701. doi: 10.1093/emboj/20.11.2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Weisleder N., Taffet G.E., Capetanaki Y. Bcl-2 overexpression corrects mitochondrial defects and ameliorates inherited desmin null cardiomyopathy. Proc. Natl. Acad. Sci. USA. 2004;101:769–774. doi: 10.1073/pnas.0303202101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lindén M., Li Z., Paulin D., Gotow T., Leterrier J.-F. Effects of Desmin Gene Knockout on Mice Heart Mitochondria. J. Bioenerg. Biomembr. 2001;33:333–341. doi: 10.1023/A:1010611408007. [DOI] [PubMed] [Google Scholar]
- 96.Vendelin M., Lemba M., Saks V.A. Analysis of Functional Coupling: Mitochondrial Creatine Kinase and Adenine Nucleotide Translocase. Biophys. J. 2004;87:696–713. doi: 10.1529/biophysj.103.036210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kay L., Li Z., Mericskay M., Olivares J., Tranqui L., Fontaine E., Tiivel T., Sikk P., Kaambre T., Samuel J.-L., et al. Study of regulation of mitochondrial respiration in vivo: An analysis of influence of ADP diffusion and possible role of cytoskeleton. Biochim. Biophys. Acta BBA Bioenerg. 1997;1322:41–59. doi: 10.1016/S0005-2728(97)00071-6. [DOI] [PubMed] [Google Scholar]
- 98.Moll R., Franke W.W., Schiller D.L., Geiger B., Krepler R. The catalog of human cytokeratins: Patterns of expression in normal epithelia, tumors and cultured cells. Cell. 1982;31:11–24. doi: 10.1016/0092-8674(82)90400-7. [DOI] [PubMed] [Google Scholar]
- 99.Coulombe P.A., Kerns M.L., Fuchs E. Epidermolysis bullosa simplex: A paradigm for disorders of tissue fragility. J. Clin. Investig. 2009;119:1784–1793. doi: 10.1172/JCI38177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Chan Y.M., Yu Q.C., LeBlanc-Straceski J., Christiano A., Pulkkinen L., Kucherlapati R.S., Uitto J., Fuchs E. Mutations in the non-helical linker segment L1–2 of keratin 5 in patients with Weber-Cockayne epidermolysis bullosa simplex. J. Cell Sci. 1994;107:765–774. doi: 10.1242/jcs.107.4.765. [DOI] [PubMed] [Google Scholar]
- 101.Vance J.E. Newly made phosphatidylserine and phosphatidylethanolamine are preferentially translocated between rat liver mitochondria and endoplasmic reticulum. J. Biol. Chem. 1991;266:89–97. [PubMed] [Google Scholar]
- 102.Nishizawa M., Izawa I., Inoko A., Hayashi Y., Nagata K., Yokoyama T., Usukura J., Inagaki M. Identification of trichoplein, a novel keratin filament-binding protein. J. Cell Sci. 2005;118:1081–1090. doi: 10.1242/jcs.01667. [DOI] [PubMed] [Google Scholar]
- 103.Cerqua C., Anesti V., Pyakurel A., Liu D., Naon D., Wiche G., Baffa R., Dimmer K.S., Scorrano L. Trichoplein/mitostatin regulates endoplasmic reticulum-mitochondria juxtaposition. EMBO Rep. 2010;11:854–860. doi: 10.1038/embor.2010.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zhong Q., Gohil V.M., Ma L., Greenberg M.L. Absence of Cardiolipin Results in Temperature Sensitivity, Respiratory Defects, and Mitochondrial DNA Instability Independent of pet56. J. Biol. Chem. 2004;279:32294–32300. doi: 10.1074/jbc.M403275200. [DOI] [PubMed] [Google Scholar]
- 105.DeVay R.M., Dominguez-Ramirez L., Lackner L.L., Hoppins S., Stahlberg H., Nunnari J. Coassembly of Mgm1 isoforms requires cardiolipin and mediates mitochondrial inner membrane fusion. J. Cell Biol. 2009;186:793–803. doi: 10.1083/jcb.200906098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tao G.-Z., Looi K.S., Toivola D.M., Strnad P., Zhou Q., Liao J., Wei Y., Habtezion A., Omary M.B. Keratins modulate the shape and function of hepatocyte mitochondria: A mechanism for protection from apoptosis. J. Cell Sci. 2009;122:3851–3855. doi: 10.1242/jcs.051862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Leng R.P., Lin Y., Ma W., Wu H., Lemmers B., Chung S., Parant J.M., Lozano G., Hakem R., Benchimol S. Pirh2, a p53-Induced Ubiquitin-Protein Ligase, Promotes p53 Degradation. Cell. 2003;112:779–791. doi: 10.1016/S0092-8674(03)00193-4. [DOI] [PubMed] [Google Scholar]
- 108.Duan S., Yao Z., Zhu Y., Wang G., Hou D., Wen L., Wu M. The Pirh2–keratin 8/18 interaction modulates the cellular distribution of mitochondria and UV-induced apoptosis. Cell Death Differ. 2009;16:826–837. doi: 10.1038/cdd.2009.12. [DOI] [PubMed] [Google Scholar]
- 109.Youle R.J., van der Bliek A.M. Mitochondrial Fission, Fusion, and Stress. Science. 2012;337:1062–1065. doi: 10.1126/science.1219855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Mathew J., Loranger A., Gilbert S., Faure R., Marceau N. Keratin 8/18 regulation of glucose metabolism in normal versus cancerous hepatic cells through differential modulation of hexokinase status and insulin signaling. Exp. Cell Res. 2013;319:474–486. doi: 10.1016/j.yexcr.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 111.Kröger C., Loschke F., Schwarz N., Windoffer R., Leube R.E., Magin T.M. Keratins control intercellular adhesion involving PKC-α-mediated desmoplakin phosphorylation. J. Cell Biol. 2013;201:681–692. doi: 10.1083/jcb.201208162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Baines C.P., Song C.-X., Zheng Y.-T., Wang G.-W., Zhang J., Wang O.-L., Guo Y., Bolli R., Cardwell E.M., Ping P. Protein Kinase Cε Interacts With and Inhibits the Permeability Transition Pore in Cardiac Mitochondria. Circ. Res. 2003;92:873–880. doi: 10.1161/01.RES.0000069215.36389.8D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Krols M., van Isterdael G., Asselbergh B., Kremer A., Lippens S., Timmerman V., Janssens S. Mitochondria-associated membranes as hubs for neurodegeneration. Acta Neuropathol. (Berl.) 2016;131:505–523. doi: 10.1007/s00401-015-1528-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Snider N.T., Omary M.B. Post-translational modifications of intermediate filament proteins: Mechanisms and functions. Nat. Rev. Mol. Cell Biol. 2014;15:163–177. doi: 10.1038/nrm3753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Parysek L.M., Eckert B.S. Vimentin filaments in spreading, randomly locomoting, and f-met-leu-phe-treated neutrophils. Cell Tissue Res. 1984;235:575–581. doi: 10.1007/BF00226955. [DOI] [PubMed] [Google Scholar]
- 116.Campello S., Lacalle R.A., Bettella M., Mañes S., Scorrano L., Viola A. Orchestration of lymphocyte chemotaxis by mitochondrial dynamics. J. Exp. Med. 2006;203:2879–2886. doi: 10.1084/jem.20061877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Helfand B.T., Mendez M.G., Murthy S.N.P., Shumaker D.K., Grin B., Mahammad S., Aebi U., Wedig T., Wu Y.I., Hahn K.M., et al. Vimentin organization modulates the formation of lamellipodia. Mol. Biol. Cell. 2011;22:1274–1289. doi: 10.1091/mbc.E10-08-0699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Desai S.P., Bhatia S.N., Toner M., Irimia D. Mitochondrial Localization and the Persistent Migration of Epithelial Cancer cells. Biophys. J. 2013;104:2077–2088. doi: 10.1016/j.bpj.2013.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kidd M.E., Shumaker D.K., Ridge K.M. The Role of Vimentin Intermediate Filaments in the Progression of Lung Cancer. Am. J. Respir. Cell Mol. Biol. 2014;50:1–6. doi: 10.1165/rcmb.2013-0314TR. [DOI] [PMC free article] [PubMed] [Google Scholar]