Abstract
Background: A high prevalence of dieting has been reported among preadolescent females. It is important to understand factors influencing the emergence of dieting because dieting is associated with increased likelihood of overeating, greater weight gain over time, and other chronic health problems. Previous studies suggest that mothers' own dieting behavior influences their daughters' dieting (i.e., modeling). Because it is not possible to randomly assign girls to a mother who is dieting versus not dieting, causal inference regarding the effects of mothers' modeling behaviors on daughters' dieting is not straightforward.
Methods: In an observational study, data were collected on four occasions of measurement across a 6-year period, with 2-year intervals between assessments on 181 girls and their parents. Propensity score methods were used to estimate the causal effects of mothers' dieting on the emergence of daughters' dieting between ages 7 and 11, examining the moderating effect of weight status.
Results: Girls whose mothers were currently dieting were significantly more likely to diet before age 11 than those whose mothers were not currently dieting, and this effect did not vary by girls' or mothers' weight status.
Conclusions: We conclude by discussing the implications of the effects of mothers' dieting on daughters' early dieting as well as the potential of propensity score methods in the field of obesity compared with traditional methodology such as regression analysis.
Introduction
Dieting to maintain or lose weight is prevalent among both normal weight and overweight female children1,2 and adolescents3; estimates suggest that one-third of preadolescent children report dieting.4 There is some evidence that early self-initiated dieting attempts increase the likelihood of disordered eating,5 depressive symptoms,6 overeating, and greater weight gain over time.7–10 The emergence of daughters' dieting has been associated with maternal dieting (i.e., modeling),11 parental encouragement to diet,4,11 and the use of controlling feeding practices such as restriction.12 Both restriction13 and encouragement to diet have been shown to lead to weight gain over time in children,4 suggesting that these practices may be counterproductive. Thus, understanding the emergence of early self-initiated dieting has important implications for public health and obesity prevention and can be used to design interventions to prevent unhealthy eating behaviors and excess weight gain.
A randomized controlled trial (RCT) would guarantee that daughters randomly assigned to maternal dieting and those who are not, are on average, equivalent (i.e., balanced) on measured and unmeasured confounders (e.g., weight concerns). However, as is often the case, randomization is not possible or ethical. Recent advances in statistical methods and software have provided new tools for strengthening causal effect estimates using observational longitudinal data. These methods use propensity scores: the predicted probability of the exposure given measured confounders.14 Confounders are variables that affect both the exposure and outcome and may bias causal effect estimates if not properly accounted for. Propensity scores balance the distributions of measured confounders such that differences in outcomes between exposed and unexposed individuals with similar propensity scores can be used to estimate the causal effect of the exposure. The primary assumption underlying the use of propensity scores is that all confounders have been measured and included in the propensity model. The more measured confounders that are included in the propensity model, the more plausible the assumption. Thus, when using propensity score methods in an observational study, it is critical to measure as many potential confounders as possible. In addition, if there is an unmeasured confounder that is highly correlated with a measured confounder, including the measured confounder in the propensity model will mitigate the bias of the causal effect estimate to the degree that they are correlated.
This article describes and applies both a propensity score method, inverse propensity weighting (IPW), and a standard regression method using observational longitudinal data from the Early Dieting in Girls study to estimate the effect of mothers' dieting at daughters' age 7 on the emergence of daughters' early dieting, operationally defined as emergence of dieting between ages 7 and 11, and whether this effect varies by daughters' baseline weight status. Based on previous studies,11,15 we expect mothers' dieting to have an effect on daughters' dieting. Furthermore, based on previous findings that overweight girls are more likely to diet,4 we expect to observe a stronger effect among girls who were overweight at age 5 than among girls who were normal weight.
Subjects and Methods
Participants included non-Hispanic White families living in central Pennsylvania recruited as part of an observational longitudinal study of the health and development of young girls with one of the primary aims to identify familial predictors of dieting behavior.16 At baseline, participants included 197 five-year-old girls (mean age = 5.4 ± 0.4) and their mothers. Eligibility criteria for girls' participation at baseline included living with the biological parents, the absence of severe food allergies or chronic medical problems affecting food intake, and the absence of dietary restrictions involving animal products. The sample was not recruited based on weight status. Daughters and mothers were also assessed at daughters' ages 7 (n = 193), 9 (n = 184), and 11 (n = 178). Attrition was primarily due to family relocation outside of the study area.
At each assessment, mothers completed questionnaires during a scheduled visit to the laboratory. Each girl was individually interviewed by a trained staff member about her eating behavior and attitudes, weight concerns, perceptions of maternal feeding practices, body satisfaction, and peer relationships. Anthropometric measures were collected on both mother and daughter at all assessments. At baseline, reported income was <$50,000 for 64% of households. Mothers' mean baseline BMI was 26.4 (standard deviation = 6.07). The Institutional Review Board approved all study procedures. Mothers provided consent for their family's participation in the study before the initiation of data collection.
Measures
Variables considered in this study include the exposure (mother's self-report of dieting, at age 7), the outcome (daughter's self-reported dieting between ages 7 and 11), the baseline (age 5) moderator, and numerous baseline covariates that are potential confounders included in the propensity model. In this study, designed to assess the effects of parent influence, on girls dieting, growth, and development, more than 200 covariates were assessed at age 5. We selected variables that we thought would be related to both the exposure and the outcome (i.e., confounders). Table 1 lists and provides details about these baseline covariates.
Table 1.
Descriptive Statistics before and after Weighting for Confounders Included in the Propensity Model by Mothers' Dieting Behavior
| Before weighting | After weighting | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Confounders | Mean: dieters | Mean: nondieters | SD: dieters | SD: nondieters | Std. effect size | Mean: dieters | Mean: nondieters | SD: dieters | SD: nondieters | Std. effect size |
| Family history of diabetes | 0.51 | 0.47 | 0.50 | 0.50 | 0.05 | 0.49 | 0.48 | 0.50 | 0.50 | 0.02 |
| Mother's age | 35.82 | 35.18 | 4.17 | 5.03 | 0.10 | 35.64 | 35.19 | 4.07 | 5.00 | 0.07 |
| Mother's BMI | 28.56 | 25.42 | 7.29 | 5.19 | 0.35 | 27.92 | 25.58 | 7.03 | 5.17 | 0.27 |
| Mother's depressiona | 11.87 | 8.76 | 8.29 | 7.04 | 0.29 | 10.54 | 8.75 | 8.03 | 6.95 | 0.17 |
| Mother's self-esteemb | 31.89 | 33.60 | 4.98 | 4.42 | 0.26 | 32.28 | 33.45 | 4.68 | 4.36 | 0.18 |
| Mother's exercise behavior | 1.56 | 1.76 | 0.68 | 0.75 | 0.20 | 1.57 | 1.75 | 0.68 | 0.74 | 0.17 |
| Mother's weight concerns | 2.05 | 1.41 | 0.67 | 0.68 | 0.67 | 1.93 | 1.48 | 0.67 | 0.69 | 0.47 |
| Mother's years of education | 14.38 | 14.66 | 2.02 | 2.31 | 0.09 | 14.39 | 14.65 | 1.93 | 2.29 | 0.09 |
| Mother's hours worked outside the home/week | 18.43 | 18.30 | 16.78 | 17.72 | 0.01 | 17.93 | 18.45 | 16.65 | 17.58 | 0.02 |
| Mother currently dieting to lose weight | 0.55 | 0.10 | 0.50 | 0.31 | 0.77 | 0.43 | 0.14 | 0.49 | 0.35 | 0.47 |
| Mother currently dieting to maintain weight | 0.31 | 0.13 | 0.46 | 0.33 | 0.33 | 0.29 | 0.14 | 0.45 | 0.35 | 0.27 |
| Mother's satisfaction with daughter's current body | 1.33 | 1.18 | 0.66 | 0.52 | 0.18 | 1.31 | 1.18 | 0.64 | 0.52 | 0.16 |
| Mother's conflict about mother's weight | 1.51 | 1.40 | 0.61 | 0.57 | 0.14 | 1.46 | 1.42 | 0.59 | 0.59 | 0.05 |
| Mother's conflict about daughter's weight | 1.08 | 1.07 | 0.26 | 0.20 | 0.05 | 1.07 | 1.06 | 0.22 | 0.20 | 0.01 |
| Mother's external locus of control | 2.29 | 2.21 | 0.56 | 0.54 | 0.11 | 2.27 | 2.22 | 0.55 | 0.54 | 0.06 |
| Mother's weight-related teasing | 2.54 | 2.38 | 2.16 | 2.02 | 0.06 | 2.39 | 2.45 | 2.16 | 2.03 | 0.02 |
| Mother's CFQ responsibility for feeding daughterc | 4.12 | 4.19 | 0.72 | 0.63 | 0.07 | 4.17 | 4.19 | 0.71 | 0.63 | 0.02 |
| Mother's CFQ restriction of daughter's dietc | 3.05 | 2.90 | 0.87 | 0.85 | 0.13 | 3.01 | 2.92 | 0.85 | 0.85 | 0.08 |
| Mother's CFQ report of daughter picky eatingd | 2.38 | 2.25 | 1.20 | 1.27 | 0.08 | 2.34 | 2.27 | 1.16 | 1.27 | 0.04 |
| Mother's disinhibited eatingd | 8.04 | 6.45 | 3.54 | 3.91 | 0.30 | 7.71 | 6.67 | 3.56 | 3.95 | 0.19 |
| Mother's hungerd | 6.09 | 5.60 | 2.95 | 3.07 | 0.11 | 6.00 | 5.74 | 2.94 | 3.09 | 0.06 |
| Mother's restrained eatingd | 13.20 | 7.41 | 5.13 | 5.46 | 0.77 | 12.26 | 8.00 | 5.25 | 5.69 | 0.55 |
| Daughter's weight concerns | 0.82 | 0.57 | 0.48 | 0.44 | 0.38 | 0.80 | 0.59 | 0.48 | 0.44 | 0.32 |
| Daughter's weight-related teasing | 2.27 | 1.64 | 3.66 | 2.69 | 0.14 | 2.10 | 1.72 | 3.54 | 2.73 | 0.09 |
| Daughter's % fat masse | 21.07 | 20.71 | 4.90 | 4.23 | 0.06 | 21.22 | 20.74 | 4.95 | 4.24 | 0.07 |
| Father's perception of mother's current size | −0.70 | −0.64 | 1.19 | 0.86 | 0.04 | −0.64 | −0.67 | 1.17 | 0.87 | 0.02 |
All constructs were measured at daughters' age 5 (i.e., baseline). Superscripts indicate how constructs were assessed.
Center for Epidemiological Studies Depression Scale.
Self-Esteem Scale.
Child Feeding Questionnaire (CFQ).
Eating Inventory.
DEXA and skinfold thickness measures.
SD, standard deviation; Std., standardized.
Exposure
Mothers were asked, “Are you currently dieting to lose weight?” at daughters' age 7. To provide clarification for participants, dieting was defined as eating less or exercising more to lose weight. One hundred thirty-four mothers answered no, 59 answered yes.
Outcome
Girls were asked, “Have you ever dieted to lose or maintain weight?” Girls who responded positively to this question at baseline (n = 13) were removed from the sample because we cannot infer whether mothers' dieting occurred before or after these girls began dieting. Forty-six girls reported dieting between ages 7 and 11.
Moderator
Girls' height and weight were measured in triplicate by a trained staff member following procedures outlined by Lohman et al.17 and were used to calculate BMI (kg/m2). BMI was converted to age- and sex-specific percentiles using CDC 2000 growth charts; overweight was defined as BMI ≥85th percentile based on standardized reference criteria.18 At baseline, 37 girls were categorized as overweight.
Statistical Analysis
First, we describe propensity score estimation, creation of weights, and balance assessment without moderators. Second, we modify estimation and weight creation to include a moderator (e.g., daughters' baseline weight status). Finally, we describe the weighted outcome analysis.
Estimating propensity scores
Propensity scores have typically been estimated by logistic regression of the exposure on the potential confounders. The propensity score estimates are the model-predicted probabilities. However, logistic regression requires specification of a parametric form (i.e., linear in the logit) and it can be difficult to decide which interactions or nonlinear terms to include, especially when there are many potential confounders. This drawback has led to the use of nonparametric machine-learning methods for estimating propensity scores,19,20 such as generalized boosted modeling (GBM21), which often performs better22 than logistic regression in terms of obtaining balance.
GBM is a flexible, nonparametric algorithm, in which a large number of classification or regression tree models are linearly combined to optimize predictive performance.21 GBM automatically considers all interactions and nonlinearities for the potential confounders. Through the use of a penalty term, unimportant interactions and nonlinearities are removed and important ones remain. The propensity score estimates are the model-predicted probabilities. R code for obtaining GBM propensity score estimates is included in the Supplementary Data (Supplementary Data are available online at www.liebertpub.com/chi).
Weights
To control for confounding, the propensity scores are used to weight the observed data such that it mimics data from an RCT. The basis for IPW23 is that there is an underrepresentation of those who are in the exposure group and have a low propensity score and an overrepresentation of those who are in the exposure group and have a high propensity score. Thus, a solution is to up-weight those who are underrepresented and down-weight those who are overrepresented.
Individuals in the exposed group are weighted by P[T = 1]/P[T = 1|X] and individuals in the unexposed group are weighted by (1−P[T = 1])/(1−P[T = 1|X]). The propensity score is P[T = 1|X], that is, the probability of being in the exposed group (i.e., T = 1) given the baseline covariates, denoted X. The value for the numerator of the weights can be obtained from an intercept-only model, which helps stabilize the weights24,25 to decrease their variability. After the weights are created, they are incorporated into the outcome model as if they were survey weights. If weights are extremely large, they may cause computational problems when fitting the outcome model. Therefore, it is necessary to check summary statistics of the weights, such as the range, percentiles, and mean, which should be ∼1.0 (see Cole and Hernan24).
Balance
Covariate balance across the exposure groups should be assessed, with a goal of determining whether differences remain after weighting. Balance is usually assessed using standardized mean differences (SMDs)26 for the unweighted and weighted samples. A general rule of thumb is that if the absolute value of the SMDs is less than 0.2 after weighting, then the exposure groups are considered balanced on the measured covariates.27 Alternatively, a more stringent rule of thumb would be 0.1. If there are a few variables on which adequate balance cannot be obtained, one option is that these variables may be included as covariates in the outcome model.28
Moderators
The computation of the weights can be modified to incorporate a moderator by including it as a predictor in both the numerator and denominator models for creating the weights. Individuals in the exposed group are given a weight of P[T = 1|Z]/P[T = 1|X,Z] and individuals in the unexposed group are given a weight of (1−P[T = 1|Z])/(1−P[T = 1|X,Z]), where the moderator is denoted as Z.25
Outcome analysis
Finally, a model for the outcome is fit using the weighted data. Because the outcome, daughters' early dieting, is binary, we fit weighted logistic regression models, in which the exposure, the moderator, and their interaction are predictors. It is not necessary to include the confounders as covariates in the weighted outcome model because the confounding is already adjusted for through IPW. However, covariates may be included if, for example, balance is not achieved for particular confounders.
Results
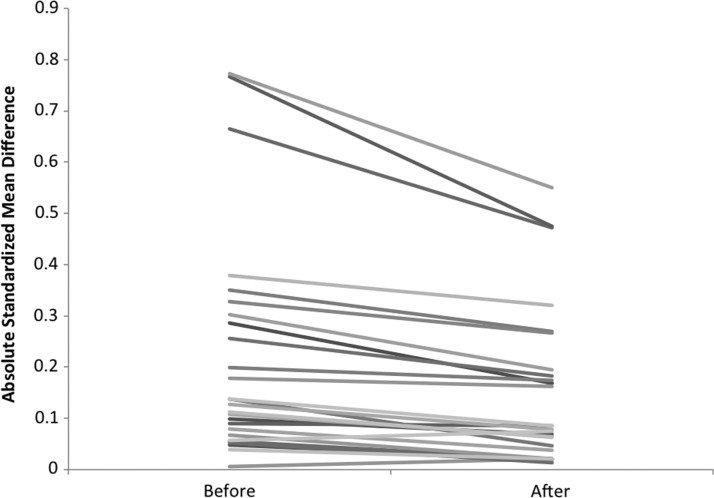
We used GBM to predict mothers' dieting at daughters' age 7 from the 26 baseline confounders listed in Table 1, computed the weights as already described, and assessed balance. The means and standard deviations for mothers' dieting and nondieting exposure groups are given in Table 1 for both the original and weighted data. Figure 1 presents the SMDs between exposure groups before and after weighting for each confounder. Each line represents a confounder and each point represents an SMD. The unweighted data are presented on the left and the weighted data on the right. The SMDs, given on the y-axis, decrease in the weighted data. The figure provides a visual assessment of the degree of balance between the exposure groups on the confounders before and after weighting. Six confounders still have moderately sized (i.e., |SMD| > 0.2) SMDs in the weighted data (Fig. 1 and Table 1). These six confounders are baseline measures of mothers' weight concerns, girls' weight concerns, mothers' dieting to lose weight, mothers' dieting to maintain weight, mothers' BMI, and mothers' dietary restriction. We included these confounders as covariates in the weighted outcome logistic regression model to further control for them.
Figure 1.
Absolute standardized mean differences between dieting and nondieting exposure groups for each of 26 confounders in the unweighted and weighted samples.
Results from the outcome model for estimating the effect of mothers' dieting are summarized in Table 2. The effect of mothers' dieting on girls' early dieting was statistically significant such that if the mother was dieting, daughters were 2.89 times more likely to diet by age 11. Next, we examined the moderating effect of girls' baseline weight status on the effect of mothers' dieting on daughters' early dieting. Results revealed no significant interaction. However, girls who were overweight at baseline were 6.05 times more likely to diet by age 11 compared with those of normal weight. Finally, none of the potential confounders included as covariates in the weighted logistic regression outcome model had statistically significant effects on daughters' early dieting.
Table 2.
Logistic Regression Outcome Model Estimates Using Propensity Weights
| Estimate | Odds ratio | Std. error | p Value | |
|---|---|---|---|---|
| Mothers' current dieting to lose weight at daughter's age 7 (i.e., exposure) | 1.06 | 2.89 | 0.51 | 0.037 |
| Girls' baseline overweight status | 1.80 | 6.05 | 0.57 | 0.002 |
| Mothers' dieting by girls' weight status interaction | −1.71 | 0.18 | 1.14 | 0.134 |
| Mothers' baseline dieting to lose weight | 0.40 | 1.49 | 0.58 | 0.471 |
| Mothers' baseline dieting to maintain weight | 0.28 | 1.32 | 0.47 | 0.551 |
| Mothers' baseline weight concerns | −0.34 | 0.71 | 0.39 | 0.386 |
| Mothers' baseline restraint | 0.03 | 1.03 | 0.05 | 0.532 |
| Mothers' baseline BMI | 0.07 | 1.07 | 0.04 | 0.090 |
| Girls' baseline weight concerns | 0.59 | 1.80 | 0.50 | 0.233 |
Baseline measures assessed at daughters' age 5.
For comparison, we fit a regression model that adjusted for the six unbalanced confounders. The only difference between this regression model and the propensity score weighted outcome model described previously is that it did not include the weights. Thus, there is no adjustment for the other 20 confounders at all and the 6 unbalanced confounders are adjusted for only once as opposed to the propensity score weighted outcome model, in which these 6 confounders are adjusted for twice—once through the propensity scores and again as covariates in the weighted outcome model. This regression model is the most “fair” comparison with the propensity score weighted results, as most researchers would adjust for some small number of confounders, but would not likely fit a regression model that included 26 covariates. For this unweighted model, the main effect of mothers' dieting was 1.28, in comparison with 1.06 (Table 2), the main effect of daughters' baseline weight was 1.74 in comparison with 1.80, and the interaction effect was −1.9 in comparison with −1.71. As in the propensity weighted outcome model, the main effects were statistically significant but the interaction effect was not. Note that although the estimate of the main effect of daughters' baseline weight was not very different, the estimate of the main effect of mothers' dieting was (odds ratio of 3.60 in the regression model as compared with 2.89 in the propensity weighted outcome model). The reason is because the propensity weighted model adjusted for many more confounders of mothers' dieting than the nonweighted regression model, but neither model attempted to adjust for confounders of the moderator because neither model attempts to estimate a causal effect of it.
Discussion
Results revealed an effect of mothers' dieting behavior at daughters' age 7 on the emergence of daughters' early dieting by age 11. Girls of mothers who reported dieting were almost three times more likely to attempt dieting by age 11. This effect was not moderated by daughters' weight status at age 5, despite previous findings that body weight promotes risk factors for eating pathology such as dieting,16 potentially suggesting that weight may play more of a role later in childhood and adolescence. The relatively small sample may have limited the ability to detect significant interactions: only 37 girls were categorized as overweight at baseline. Because six of our covariates were not balanced after weighing, additional research is needed before inferring causality. The propensity weighted results can, however, be interpreted as less biased estimates than analyses presented using a traditional regression approach, which only adjusted for 6 confounders (compared with 26 potential confounders in the weighted model). However, the discussion focuses primarily on methodological considerations because further research is needed before asserting that mothers' dieting causes the emergence of daughters' dieting.
These findings demonstrate how advanced statistical approaches can be used to help strengthen causal inferences using observational data about the effect of maternal dieting on the emergence of daughter dieting, which is important considering the suggested role between dieting and later weight gain.4 Propensity score methods have several advantages over regression adjustment. One by-product of propensity score analysis is the ability to examine balance and overlap. For example, if we had not estimated the propensity scores and had instead done only the regression analysis, we would not know that we did not attain balance on six of the variables. Schafer and Kang28 suggest performing these diagnostics using propensity scores even if the final analysis uses a traditional regression adjustment rather than propensity scores. Another advantage is that propensity scores summarize a potentially large number of confounders into a single-number summary. Finally, propensity score methods do not make any assumptions about the parametric form of the effect of the covariates on the outcome as regression-based adjustment typically does. Although interaction terms or quadratic terms may be added to a regression model, doing so would increase the number of covariates in the regression model even further. Furthermore, using GBM to estimate the propensity scores automates the process of including important interactions and nonlinearities.
Of course, propensity score methods are not without limitations. These methods, like regression-based adjustment, assume that there are no unmeasured confounders, which is why an RCT is ideal. Nevertheless, propensity score methods, particularly in combination with a traditional regression-based adjustment, are a viable alternative when an RCT is not feasible. In addition, methods are being developed for assessing the sensitivity of the estimates to the presence of an unmeasured confounder; that is, the degree to which an unmeasured confounder may bias the results.
It is important that variables that may have been influenced by the exposure are not included in the propensity score model.29 Because of this, we used baseline covariates at age 5 as confounders in a propensity score model for mothers' dieting at daughters' age 7. We were also careful to maintain temporal order to determine directionality. Girls reporting dieting before age 5 were excluded because the outcome occurred before or concurrent to the exposure of interest. The disadvantage of this is that we could not examine the effect of mothers' dieting at daughters' age 5.
In conclusion, propensity score methods may be useful for estimating the causal effects of family and environmental exposures on obesity and obesity-related outcomes from observational data and studies in which RCTs are not feasible. However, diligence needs to be taken when designing these studies to maintain temporal order and to measure all potential covariates. A doubly robust approach, in which propensity score methods are used in combination with regression adjustment, is ideal, followed by a sensitivity analysis to unmeasured confounding.
Supplementary Material
Acknowledgments
Preparation of this article was supported by National Institute on Drug Abuse (NIDA) center grant P50 DA100075-16, National Institute on Diabetes and Digestive and Kidney Diseases (NIDDK) 5R21DK082858-02, and USDA Grant No. 2011-67001-30117. The Early Dieting in Girls study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) R01 HD32973-09. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIDA, NIDDK, NICHD, the NIH, or the United States Department of Agriculture (USDA). We thank Amanda Applegate for comments on a previous draft.
Author Disclosure Statement
Drs. Coffman and Savage were funded by NIH. Dr. Balantekin declares no potential conflict of interest.
References
- 1. Abramovitz BA, Birch LL. Five-year-old girls' ideas about dieting are predicted by their mothers' dieting. J Am Diet Assoc 2000; 100: 1157– 1163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance—United States, 2011. MMWR Surveill Summ 2012; 61: 1– 162 [PubMed] [Google Scholar]
- 3. Crow S, Eisenberg ME, Story M, et al. Psychosocial and behavioral correlates of dieting among overweight and non-overweight adolescents. J Adolesc Health 2006; 38: 569– 574 [DOI] [PubMed] [Google Scholar]
- 4. Balantekin KN, Savage JS, Marini ME, et al. Parental encouragement of dieting promotes daughters' early dieting. Appetite 2014; 80: 190– 196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Neumark-Sztainer D, Wall M, Guo J, et al. Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: How do dieters fare 5 years later? J Am Diet Assoc 2006; 106: 559– 568 [DOI] [PubMed] [Google Scholar]
- 6. Gillen MM, Markey CN, Markey PM. An examination of dieting behaviors among adults: Links with depression. Eat Behav 2012; 13: 88– 93 [DOI] [PubMed] [Google Scholar]
- 7. Field AE, Austin SB, Taylor CB, et al. Relation between dieting and weight change among preadolescents and adolescents. Pediatrics 2003; 112: 900– 906 [DOI] [PubMed] [Google Scholar]
- 8. Savage JS, Hoffman L, Birch LL. Dieting, restraint, and disinhibition predict women's weight change over 6 y. Am J Clin Nutr 2009; 90: 33– 40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Savage JS, Birch LL. Patterns of weight control strategies predict differences in women's 4-year weight gain. Obesity (Silver Spring) 2010; 18: 513– 520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Stice E, Presnell K, Shaw H, et al. Psychological and behavioral risk factors for obesity onset in adolescent girls: A prospective study. J Consult Clin Psychol 2005; 73: 195– 202 [DOI] [PubMed] [Google Scholar]
- 11. Benedikt R, Wertheim EH, Love A. Eating attitudes and weight-loss attempts in female adolescents and their mothers. J Youth Adolesc 1998; 27: 43– 57 [Google Scholar]
- 12. Costanzo PR, Woody EZ. Domain-specific parenting styles and their impact on the child's development of particular deviance: the example of obesity proneness. J Soc Clin Psychol 1985; 1: 425– 445 [Google Scholar]
- 13. Fisher JO, Birch LL. Restricting access to palatable foods affects children's behavioral response, food selection, and intake. Am J Clin Nutr 1999; 69: 1264– 1272 [DOI] [PubMed] [Google Scholar]
- 14. Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika 1983; 70: 41– 55 [Google Scholar]
- 15. Smolak L, Levine MP, Schermer F. Parental input and weight concerns among elementary school children. Int J Eat Disord 1999; 25: 263– 271 [DOI] [PubMed] [Google Scholar]
- 16. Balantekin KN, Birch LL, Savage JS. Patterns of weight‐control behavior among 15 year old girls. Int J Eat Dis 2015; 48: 589– 600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lohman T, Roche A, Martorell R. Anthropometric Standardization Reference Manual. Illinois: Human Kinetics Book, 1991. [Google Scholar]
- 18. Ogden C, Kuczmarski R, Flegal K. CDC growth charts: United States. Adv Data 2000: 1– 27 [PubMed] [Google Scholar]
- 19. Berk R. An introduction to ensemble methods for data analysis. Sociol Methods Res 2006.
- 20. Strobl C, Malley J, Tutz G. An introduction to recursive partitioning: Rationale, application, and characteristics of classification and regression trees, bagging, and random forests. Psychol Methods 2009; 14: 323– 348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McCaffrey DF, Ridgeway G, Morral AR. Propensity score estimation with boosted regression for evaluating causal effects in observational studies. Psychol Methods 2004; 9: 403– 425 [DOI] [PubMed] [Google Scholar]
- 22. Lee BK, Lessler J, Stuart EA. Improving propensity score weighting using machine learning. Stat Med 2010; 29: 337– 346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hirano K, Imbens GW. Estimation of causal effects using propensity score weighting: An application to data on right heart catherization. Health Serv Outcomes Res Methodol 2001; 2: 259– 278 [Google Scholar]
- 24. Cole SR, Hernan MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol 2008; 168: 656– 664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Robins JM, Hernan MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology 2000; 11: 550– 560 [DOI] [PubMed] [Google Scholar]
- 26. Rosenbaum PR, Rubin DB. Constructing a control-group using multivariate matched sampling methods that incorporate the propensity score. Am Stat Assoc 1985; 39: 33– 38 [Google Scholar]
- 27. Harder VS, Stuart EA, Anthony JC. Propensity score techniques and the assessment of measured covariate balance to test causal associations in psychological research. Psychol Methods 2010; 15: 234– 249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Schafer JL, Kang JDY. Average causal effects from non-randomized studies: A practical guide and simulated example. Psychol Methods 2008; 13: 279– 313 [DOI] [PubMed] [Google Scholar]
- 29. Rosenbaum PR. The consequences of adjustment for a concomitant variable that has been affected by the treatment. J R Stat Soc Ser A 1984; 147: 656– 666 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.