Abstract
During life, many personal changes occur. These include changing house, school, work, and even friends and partners. However, the daily experience shows clearly that, in some situations, subjects are unable to change even if they want to. The recent advances in psychology and neuroscience are now providing a better view of personal change, the change affecting our assumptive world: (a) the focus of personal change is reducing the distance between self and reality (conflict); (b) this reduction is achieved through (1) an intense focus on the particular experience creating the conflict or (2) an internal or external reorganization of this experience; (c) personal change requires a progression through a series of different stages that however happen in discontinuous and non-linear ways; and (d) clinical psychology is often used to facilitate personal change when subjects are unable to move forward. Starting from these premises, the aim of this paper is to review the potential of virtuality for enhancing the processes of personal and clinical change. First, the paper focuses on the two leading virtual technologies – augmented reality (AR) and virtual reality (VR) – exploring their current uses in behavioral health and the outcomes of the 28 available systematic reviews and meta-analyses. Then the paper discusses the added value provided by VR and AR in transforming our external experience by focusing on the high level of personal efficacy and self-reflectiveness generated by their sense of presence and emotional engagement. Finally, it outlines the potential future use of virtuality for transforming our inner experience by structuring, altering, and/or replacing our bodily self-consciousness. The final outcome may be a new generation of transformative experiences that provide knowledge that is epistemically inaccessible to the individual until he or she has that experience, while at the same time transforming the individual’s worldview.
Keywords: virtual reality, augmented reality, personal change, anxiety disorders, eating disorders, acute pain, post-traumatic stress disorder, body swapping
Introduction: Understanding Personal Change
How can we use technologies like virtual reality or augmented reality to support personal and clinical change? A meaningful answer to this question requires an in-depth examination of the process of change. During our life, we undergo many personal changes: we change our house, our school, our work, and even our friends and partners. However, in this paper, we will focus on a peculiar type of change – personal change – whose main effect is a change in the conceptual system of the subject (assumptive world), derived from perceptions of one’s own behavior or experience, or other incoming information (1). Personal change plays an adaptive role in managing symptoms of distress produced by life transitions and traumatic events (1, 2). Moreover, high levels of personal change are associated with psychological well-being (2).
Our daily experience shows clearly that, in some situations, subjects are unable to change even if they want to. To help these subjects, clinical psychology is often used to facilitate personal change. However, as noted by Higginson and Mansell (3): “The mechanism of change is not fully understood. This is clear in research demonstrating the efficacy of different therapeutic approaches and the significant rates of natural recovery” (p. 326). On one side different studies suggest the lack of differential effectiveness between therapies – many therapies have equivalently positive outcomes – despite manifestly non-equivalent theories and techniques (4, 5). On the other side, some people experience personal change without the help of any form of psychotherapeutic treatment.
The recent advances in psychology and neuroscience are now providing a better view of personal change that help us in understanding the potential of these technologies. The main tenets are:
change is contextual: depending on the person, the issues, and the situation (6);
the self can be both a barrier and a catalyst to change: people are motivated to maintain self-integrity (7);
change is a process: it happens in discontinuous and non-linear ways, following life transitions and traumatic events (8).
We will deepen these points in the following section.
The starting point for our exploration of the process of change is the perceptual control theory (PCT) (9, 10). According to this vision, the process of control is the critical feature of human nature (9): “life is a constant process of comparing how things are with how we want things to be, and if they do not match doing something to get closer to how we want things to be” (p. 250).
Generally, control is a defined as the process of reducing the distance between what we want and what we are (error). Interestingly, the source of errors is both within and between individuals (9, 11). Specifically, PCT suggests that a possible source of error is internal: the coherence between goals and subgoals of the individual (conflict).
To eliminate a conflict, the individual must direct his or her awareness to the experience that is creating the conflict. Then, a reorganization is required: a trial and error process, which modifies the characteristics or the conflicting goals (3).
The PCT can be integrated with the vision of a second theory: self-affirmation theory (SAT) (12, 13). According to this view, individuals are motivated to maintain their self-integrity, defined as (7) “a sense of global efficacy, an image of oneself as able to control important adaptive and moral outcomes in one’s life” (p. 336). On one side, any threat to it evokes self-defense and psychological stress. On the other side, subjects can import into a critical domain the sense of personal integrity that they feel in another. In the concept of self-integrity, a critical role is played by self-efficacy, the strength of one’s belief in one’s own ability to complete tasks and reach goals (14, 15). As noted by Bandura (16, 17), self-efficacy determines whether the process of change will be initiated, how much effort will be expended toward it, and how long it will be sustained in the face of obstacles and aversive experiences.
The process of change is also the focus of another vision: the TransTheoretical Model of Behavior Change (18–20). This model describes personal change as a progression through a series of five stages: precontemplation, contemplation, determination, action, and maintenance. These stages represent a temporal dimension that allows both the individuals and the persons supporting them to understand when particular shifts in attitudes, intentions, and behaviors occur.
However, not all personal changes occur in a linear or gradual manner. As noted by Miller and C’de Baca (21), individuals may have “transformative experiences” able to produce a deep and enduring restructuration of one or more personal dimension. According to Mezirow’s Transformative Learning Theory (22, 23), these experiences can be triggered by a “disorienting dilemma” usually related to a life crisis or major life transition (e.g., death, illness, separation, or divorce), which forces individuals to critically examine and eventually revise their core assumptions and beliefs. The outcome of a transformative experience is a significant and permanent change in the expectations – mindsets, perspectives and habits of mind – through which we filter and make sense of the world.
As noted by Kottler (6) and Riva (24), by merging these theories, we can identify some important properties of personal change:
the focus of personal change is reducing the distance between self and reality (conflict);
this reduction is achieved through: (a) an intense focus on the particular experience creating the conflict and (b) an internal or external reorganization of this experience;
-
this process can be the outcome of either a sudden transformative experience or a progression through a series of different stages:
selfhood is affected by a crisis, trauma, or developmental transition;
a level of pain and discomfort is reached that cannot any longer be ignored or denied;
there is an awareness or insight that something different must be done (change);
there is a process of applying what was realized or learned into new meanings and/or constructive action;
if a sufficient level of action is achieved, it alters the perception of the environment and sets new goals; and
there is recovery from inevitable relapses.
The critical steps in this process are three: the emergence of transformative experiences, the passage between stage c and d and the one between stage d and e.
As noted by Gaggioli (25), transformative experiences provide knowledge that is epistemically inaccessible to the individuals until they have that experience. For this reason, transformative experiences cannot be planned in advance but happen suddenly in individuals’ lives without a prior control on their contents and their effects.
Instead, the passage between stage c and d requires self-reflectiveness: an intense focus on the particular instance or experience creating the conflict (26). By exploring this experience as thoroughly as possible, the individual can relive and identify all of the significant elements associated with it (e.g., conceptual, behavioral, emotional, and motivational) facilitating their reorganization (24).
Finally, the passage between stage d and e requires the belief of personal efficacy (16, 17): individuals have to believe that they have the power to effect changes through their actions. Without it there, they are not willing to act, or to keep on acting in the face of problems and difficulties.
Starting from these premises, the paper wants to review the potential of virtuality for enhancing the process of personal change. First, the paper will explore the two leading virtual technologies – augmented reality (AR) and virtual reality (VR) – assessing their current uses in behavioral health and the outcomes of the available systematic reviews and meta-analyses. Then the paper will discuss their added value in transforming our external experience by focusing on the elevated level of personal efficacy and self-reflectiveness generated by their sense of presence and emotional engagement. Finally, it will outline the potential future use of virtuality for transforming our inner experience by structuring, altering, and/or replacing our bodily self-consciousness (BSC).
The Virtual Technologies: Augmented Reality and Virtual Reality
Experiential Learning through Augmented Reality
Augmented reality can be described as an interactive visualization system (a head-mounted display, a computer, a game console, a smartphone, or a tablet) allowing the merging of digital contents with the real environment surrounding the user (27, 28). In simpler words, AR allows the augmentation of our real experience blending both “real-world elements” and “virtual elements,” which may involve not only the view but also hearing, touch, and smell (29). For this reason, within the reality–virtuality continuum (see Figure 1) introduced by Milgram and Kishino (30) to describe all the possible combinations of real and virtual objects, AR is the step just after the real environment.
Figure 1.
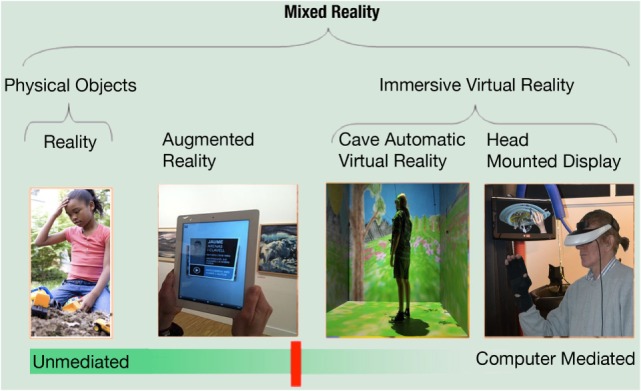
The reality–virtuality continuum [adapted from Milgram and Kishino (30)].
In fact, the most important feature of AR is that the synthetic objects and data provide the real world with remarkable and valuable information for its user. van Krevelen and Poelman describe this opportunity in the following way (31): “Imagine a technology with which you could see more than others see, hear more than others hear, and perhaps even touch, smell, and taste things that others cannot. What if we had technology to perceive completely computational elements and objects within our real world experience… that help us in our daily activities, while interacting almost unconsciously through mere gestures and speech?” (p. 1).
The additional information offered by AR can be a powerful tool for personal change, because it can support and improve the sense of self-reflectiveness and personal efficacy of its users.
For these features, AR seems to be a promising and useful tool for intervention in the treatment of specific phobias (29, 32), as also supported by a recent systematic review (28) (see Table 1) and a narrative review (33).
Table 1.
Meta-analyses and systematic reviews related to the use of AR in the different areas of behavioral health.
| Review type | Reference | Included studies | Conclusions (from papers) | |
|---|---|---|---|---|
| Anxiety disorders | Systematic review | (28) | 13 studies | “In general, the presented studies show that the AR seems to be a promising and useful tool for intervention in the treatment of specific phobias. Nevertheless, the small sample of subjects examined, and the lack of control group and randomized controlled studies necessitate more randomized controlled experiments for exploring the AR efficacy in the clinical treatments” |
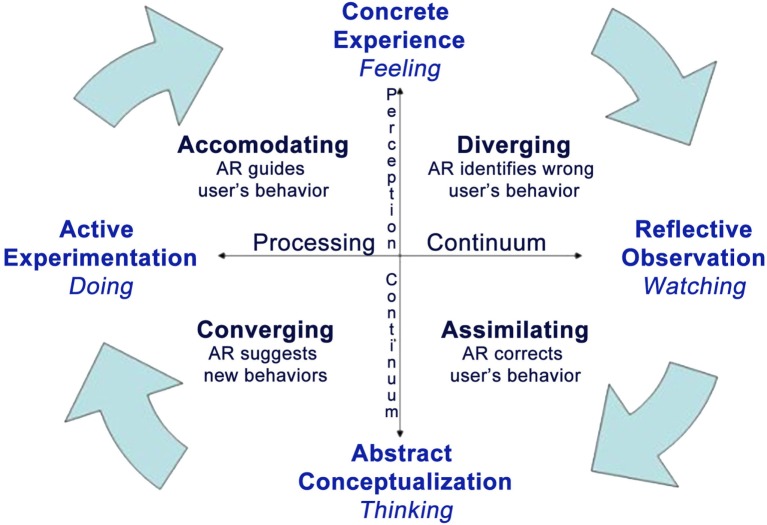
However, its potential in supporting personal change is wider as demonstrated by different emerging applications: from post-stroke (34) and physical rehabilitation (35, 36), social (37) and emotional (38) training for children with autism, to pain reduction (39). Here, we suggest that the added value of AR is related to the support it offers to all the stages of the experiential learning cycle (40) (see Figure 2).
Figure 2.
The role of AR in the experiential cycle [adapted from Kolb (40)].
According to the influential model introduced by David Kolb, experiential learning is a process consisting of four stages: experience, observation and reflection, abstract reconceptualization, and experimentation (40, 41). The individual starts the learning process from his/her experience, which leads to observations and reflections on its contents. Specifically, abstract conceptualization is used to create a generalization of the experience that is evaluated, integrated with the available knowledge, and converted into recommendations. These recommendations activate new actions and strategies, which can be tested and explored, to adjust the original experience.
A possible example of how AR can be used to support experiential learning in relation to clinical change is the treatment of a specific phobia, for example cockroach phobia (32, 42, 43). In the “concrete experience” stage, the patient observes the cockroaches in the “here-and-now” offered by AR. This experience is the “basis for observation and reflection” (reflective observation): the patient has the opportunity to consider the actions – e.g., avoidance – and emotions – e.g., irritability and fear – experienced and to think about his/her behavior in previous similar experiences (generalization). At this stage, the role of the therapist is important: generalization questions – e.g., individual is asked to compare the performance in earlier exposures and to identify the pros and cons of the different behaviors – can be used to facilitate abstract conceptualization and to identify recommendations supporting the next exposure. During the new exposure, AR can support, in real time, the patient, offering real-time information about his/her status – e.g., the level of emotional arousal – and practical suggestions – e.g., to keep their hands closer to the ones of the therapist. Moreover, AR can enhance the process of change throughout the entire treatment, for instance, Botella and colleagues (44) used an AR-based serious game in a mobile phone in order to facilitate the exposure treatment. The goal of this game was reducing the level of fear and avoidance before the AR exposure session and promoting the over-learning after the AR exposure session as a homework assignment.
In this way, AR facilitates personal change through a cyclical interaction of experience, thought, and reflection (active experimentation).
In other words, AR is the perfect experiential learning tool. On one side, it allows real-time interactivity in an ecological setting improving concentration and motivation (45). On the other side, it provides targeted and non-directive suggestions and guidelines that help users to develop skills and knowledge in a more effective way (46). Finally, as suggested by Baus and Bouchard (32), AR can be used in the actual places the subject encounters his difficulties, facilitating the transfer of the acquired skills to the real world.
Virtual Reality as Simulative Technology
Within the reality–virtuality continuum (see Figure 1) introduced by Milgram and Kishino (30), VR is the final step, in opposition to reality: if AR adds digital information to the real-world environment, VR completely replaces it with a virtual one. But what is VR?
In computer sciences, VR is usually described as a set of fancy technologies (47, 48): an interactive 3D visualization system (a computer, a game console, or a smartphone) supported by one or more position trackers and head-mounted display. The trackers sense the movements of the individual and report the collected data to the visualization system, which updates the scene in real time.
However, in psychology and neuroscience, VR is instead defined as (49) “an advanced form of human–computer interface that allows the user to interact with and become immersed in a computer-generated environment in a naturalistic fashion” (p. 82). From a psychological perspective, VR is a subjective experience cheating the individual out of the illusion that he/she is there, that this experience is real (50). Specifically, VR is different from other media because it induces the sense of “presence”: the feeling of “being there” inside the virtual experience produced by the technology (51, 52).
While still is lacking a general consensus about the definition and the etiology of presence [for an introduction to this topic see Ref. (53–66)], most researchers agree about what it is not (65). As underlined by Riva and colleagues (54) “Presence is not the degree of technological immersion, it is not the same thing as emotional engagement, it is not absorption or attention or action; but all of these have a potential role in understanding the experience of presence in interaction – the experience of interacting with presence” (p. 1).
The sense of presence offered by VR can be a powerful tool for personal change because it offers a world where the individual can stay and live a specific experience (47, 67, 68). Following the model of personal change discussed before, VR allows a level of self-reflectiveness that is higher than the one provided by memory and imagination, and it is more controlled than the one offered by direct “real” experience. In fact, VR can also be defined as an “advanced imaginal system” (69–71): an experiential form of imagery that is as effective as reality in inducing emotional responses.
As underlined by Glantz and colleagues (72) “One reason it is so difficult to get people to update their assumptions is that change often requires a prior step – recognizing the distinction between an assumption and a perception. Until revealed to be fallacious, assumptions constitute the world; they seem like perceptions, and as long as they do, they are resistant to change” (p. 96). Using the sense of presence induced by VR, it is easier to develop new, realistic, credible, and informative experiences regarding the surrounding world or the self demonstrating to the individual that what is assumed to be true – e.g., my team disapproves me – in fact is a result of his/her mind. Once this has been understood, it is easier to identify all of the elements supporting the assumption and make them available for reorganization (73).
These features clearly explain the increasing use of VR in behavioral health and, in particular, in the treatment of anxiety disorders. In Table 2, we reported all the available systematic reviews and meta-analyses related to the use of VR in behavioral health. To select them, a computer-based search in several databases was performed for relevant publications. Databases used for the search were PsycINFO, PubMed/Medline, and Web of Science (Web of Knowledge). We searched using the string “Virtual Reality” AND (“review” OR “systematic review” OR “meta-analysis” OR “meta-analysis”). English, French, and German were used as language limits. More, we hand-searched the reference lists of all relevant articles to find additional studies (snowball technique).
Table 2.
Meta-analyses and systematic reviews related to the use of VR in the different areas of behavioral health.
| Review type | Reference | Included studies | Conclusions (from papers) | |
|---|---|---|---|---|
| Addictions | Systematic review | Bordnick et al. (90) | 14 studies | “Research using VR has shown that drug-dependent people react with strong craving to specific cues (e.g., cigarette packs and liquor bottles) as well as environments or settings (e.g., bar and party) associated with drug use. Virtual reality has also been used to enhance learning and generalization of relapse prevention skills in smokers by reinforcing these skills in lifelike environments” |
| Systematic review | Hone-Blanchet et al. (91) | 21 studies | “VR enhances ecological validity of traditional craving-induction measurement. Specifically, findings indicate that VR can successfully increase craving. Studies combining cue-exposure therapy with virtual environment, however, reported mitigated success so far” | |
| Meta-analysis | Pericot-Valverde et al. (94) | 18 studies | “Presentations of smoking cues through virtual reality can produce strong increases in craving among cigarette smokers. This strong cue-reactivity effect, which was comparable in magnitude to the craving effect sizes, found with more conventional modes of cue presentation, supports the use of virtual reality for the generation of robust cue-specific craving in cue-reactivity research” | |
| Anxiety disorders | Meta-analysis | Parsons and Rizzo (74) | 21 studies | “Although meta-analysis revealed large declines in anxiety symptoms following VRET, moderator analyses were limited due to inconsistent reporting in the VRET literature” |
| Meta-analysis | Powers and Emmelkamp (75) | 13 studies | “Analysis showed a large mean effect size for VRET compared to control conditions, Cohen’s d = 1.11 (SE = 0.15, 95% CI: 0.82–1.39). This finding was consistent across secondary outcome categories as well (domain-specific, general subjective distress, cognition, behavior, and psychophysiology). Also, as expected, in vivo treatment was not significantly more effective than VRET. In fact, there was a small effect size favoring VRET over in vivo conditions, Cohen’s d = 0.35 (SE = 0.15, 95% CI: 0.05–0.65)” | |
| Systematic review | Meyerbroker and Emmelkamp (76) | 20 studies | “Only in fear of flying and acrophobia, there is considerable evidence that VRET indeed is effective. In more complex anxiety disorders as panic disorder and social phobia, which form the core clinical groups, first results of VRET are promising, but more and better controlled studies are needed before the status of empirically supported treatment is reached. More severe cases of panic disorder with agoraphobia and social phobia are often not reached with existing treatments” | |
| Meta-analysis | Opris et al. (77) | 23 studies | “The results show that VR does far better than the waitlist control, and similar efficacy between the behavioral and the cognitive behavioral interventions incorporating a VR exposure component and the classical evidence-based interventions. VR has a powerful real-life impact, similar to that of the classical evidence-based treatments, and a good stability of results over time, similar to that of the classical evidence-based treatments. There is a dose–response relationship for VRET, and there is no difference in the dropout rate between the VR exposure and the in vivo exposure” | |
| Systematic review | McCann et al. (78) | 27 studies | “VRET may be an effective method of treatment but caution should be exercised in interpreting the existing body of literature supporting VRET relative to existing standards of care. The need for well-designed VRET research is discussed” | |
| Meta-analysis | Ling et al. (66) | 33 studies | “Analysis showed a medium effect size for the correlation between sense of presence and anxiety (r = 0.28; 95% CI: 0.18–0.38). Moderation analyses revealed that the effect size of the correlation differed across different anxiety disorders, with a large effect size for fear of animals (r = 0.50; 95% CI: 0.30–0.66) and a no to small effect size for social anxiety disorder (r = 0.001; 95% CI: −0.19 to 0.19). Further, the correlation between anxiety and presence was stronger in studies with participants who met criteria for an anxiety disorder than in studies with a non-clinical population” | |
| Systematic review | Diemer et al. (62) | 38 studies | “Despite several limitations, this review provides evidence that VR exposure elicits psychophysiological fear reactions in patients and healthy subjects, rendering VR a promising treatment for anxiety disorders, and a potent research tool for future investigations of psychophysiological processes and their significance during exposure treatment” | |
| Stress-related disorders | Systematic review | Goncalves et al. (80) | 10 studies | “The results suggest the potential efficacy of VRET in the treatment of PTSD for different types of trauma. VRET proved to be as efficacious as exposure therapy. VRET can be particularly useful in the treatment of PTSD that is resistant to traditional exposure because it allows for greater engagement by the patient and, consequently, greater activation of the traumatic memory, which is necessary for the extinction of the conditioned fear” |
| Systematic review | Serino et al. (81) | 10 studies | “VR-based cyber-SIT cyber-SIT may play an important role in the future clinical psychology, but it is crucial to enhance the validation of this approach from a methodological point of view: controlled trials testing a greater number of participants are needed” | |
| Systematic review | Motraghi et al. (82) | 9 studies | “Although preliminary findings suggest some positive results for VRET as a form of exposure treatment for PTSD, additional research using well-specified randomization procedures, assessor blinding, and monitoring of treatment adherence is warranted. Movement toward greater standardization of treatment manuals, virtual environments, and equipment would further facilitate interpretation and consolidation of this literature” | |
| Systematic review | Botella et al. (83) | 12 studies | “Results suggest VR is effective in the treatment of PTSD. Not all studies reported having followed the clinical guidelines for evidence-based interventions in the treatment of PTSD. Few studies evaluated acceptability, however, the findings are very promising, and patients reported high satisfaction and acceptability regarding the inclusion of VR in the treatment of PTSD. The main weaknesses identified focus on the need for more controlled studies, the need to standardize treatment protocols using VR, and the need to include assessments of acceptability and related variables” | |
| Autism | Systematic review | Aresti-Bartolome and Garcia-Zapirain (96) | 11 studies | “Virtual reality makes it possible to create safe environments where they can learn rules and repeat the tasks. Furthermore, interacting with avatars where social situations are replicated enables patients to work on these situations and find more flexible solutions. This means that virtual environments may be good instruments to work on social skills with ASD sufferers” |
| Systematic review | den Brok and Sterkenburg (97) | 28 studies | “Specific kinds of technologies can be used to learn specific kinds of skills (e.g., videos on computers or handheld devices for daily living skills; virtual reality for time perception and emotions of others). For attaining cognitive concepts, advanced technologies such as virtual reality are effective” | |
| Depression | Systematic review and meta-analysis | Li et al. (105) | 19 studies | “The unique experience of virtual reality exposure therapy was reported to be particularly effective for reducing depression caused by fear. The meta-analysis revealed a moderate effect size of the game interventions for depression therapy at posttreatment [d = −0.47 (95% CI −0.69 to −0.24)]” |
| Eating disorders and obesity | Systematic review | Ferrer-Garcia and Gutierrez-Maldonado (114) | 12 studies | “Although examined results suggest that VR-based therapy is an effective intervention for treating body image disturbances, more controlled studies with larger clinical samples are needed” |
| Systematic review | Koskina et al. (116) | 4 studies | “Data indicate that using virtual environments provide alternative ways of delivering exposure therapy that has promising outcomes. Overall, it is possible that VR may be a useful intervention for ED, and its implementation is recommended either as a stand alone treatment or as an intermediary step prior to in vivo exposure” | |
| Systematic review | Ferrer-Garcia et al. (115) | 17 studies | “Although several methodological deficiencies were detected in the reviewed studies, there is fair evidence for the effectiveness of VR-based treatments in ED and obesity. VR-based interventions usually combine exposure to VR environments with cognitive therapies. The VR component seems to be especially suitable for reducing body image disturbances and for increasing self-esteem and self-efficacy” | |
| Pain reduction | Systematic review | Morris et al. (109) | 9 studies | “VR, in conjunction with pharmacologic analgesics, significantly reduced pain experienced by burn injury patients during wound dressing changes and physiotherapy. There is equivocal evidence for the effect of VR in conjunction with pharmacologic analgesics on reducing anxiety in burn injury patients during wound dressing changes and physiotherapy” |
| Systematic review | Malloy and Milling (110) | 11 studies | “VR distraction was shown to be effective for reducing experimental pain, as well as the discomfort associated with burn injury care. Studies of needle-related pain provided less consistent findings” | |
| Systematic review | Triberti et al. (112) | 11 studies | “Results suggest the importance of different psychological factors in the effectiveness of the analgesic distraction. While sense of presence influences the effectiveness of VR as a distraction tool, anxiety as well as positive emotions directly affect the experience of pain” | |
| Systematic review | Garrett et al. (111) | 17 studies | “There was strong overall evidence for immediate and short-term pain reduction after VR, whereas moderate evidence was found for short-term effects on physical function. Little evidence exists for longer-term benefits” | |
| Psychosis | Systematic review | Valmaggia et al. (106) | 16 studies | “The review identified studies investigating the effect of interpersonal sensitivity, childhood bullying victimization, physical assault, perceived ethnic discrimination, social defeat, population density, and ethnic density on the real-time appraisal of VR social situations. Further studies demonstrated the potential of VR to investigate paranoid ideation, anomalous experiences, self-confidence, self-comparison, physiological activation, and behavioral response. The reviewed studies suggest that VR can be used to investigate psychological processes and mechanisms associated with psychosis” |
| Schizophrenia | Meta-analysis | Välimäki et al. (107) | 3 studies | “There is no clear good quality evidence for or against using virtual reality for treatment compliance among people with schizophrenia. If virtual reality is used, the experimental nature of the intervention should be clearly explained. High-quality studies should be undertaken in this area to explore any effects of this novel intervention and variations of approach” |
| Systematic review | Veling et al. (108) | 4 studies | “There is a small but expanding literature on interventions for delusions, hallucinations, neurocognition, social cognition, and social skills; preliminary results are promising. VR applications for assessment and treatment of psychotic disorders are in their infancy but appear to have a great potential for increasing our understanding of psychosis and expanding the therapeutic toolbox” | |
We have included only articles on VR used for supporting personal and clinical change. Excluded from the analysis were studies related to the use of VR in surgery, physical and cognitive rehabilitation, and review articles lacking basic information about the selection of the discussed papers.
Our initial search yielded 918 non-duplicate citations screened via PsycINFO, PubMed/Medline, and Web of Science (Web of Knowledge). After the application of inclusion/exclusion criteria, papers have been reduced to 67 articles. A more in-depth investigation of the full papers resulted in an exclusion of 40 articles. Twenty-seven of them were excluded because their specific focus was not VR, while the remaining 13 were excluded, because they lacked a clear description of the process used to select the discussed papers. In the end, 27 studies met full criteria and were included in Table 2.
As expected, the highest number of papers – four meta-analyses and seven systematic reviews – is related to the use of VR in the treatment of emotion-related disorders: anxiety disorders (four meta-analyses and three systematic reviews) (66, 74–79) and stress-related disorders (four systematic reviews) (80–83). The results support the use of VR in the treatment of phobias (66, 74, 75, 79), stress management (81), post-traumatic stress disorders (80, 82, 83), and panic disorders with or without agoraphobia (77). No definitive evidence is available for the treatment of social phobia (66, 75, 76). More, as underlined by most studies (84), and specifically by McCann and colleagues (78), the quality of future research has to be improved using well-specified randomization procedures, assessing treatment adherence, and providing a better standardization of clinical protocols.
As noted by Riva and Mantovani (85), the rationale behind the use VR in anxiety disorders is simple “…in VR, the patient is intentionally confronted with the feared stimuli while allowing the anxiety to attenuate. Avoiding a dreaded situation, reinforces a phobia, and each successive exposure to it reduces the anxiety” (p. 21). In other words, VR is a versatile tool that permits to develop multiple environments that can be presented to the user in many different forms (66, 86). Recent studies show that VR exposure to multiple contexts reduces the recurrence of fear to a greater extent than exposure to only one scenario (87); in the same way, return of fear at posttreatment was significantly reduced by the use of multiple stimuli contexts during exposure (33, 88). Therefore, exposure to different virtual contexts can be an effective way to generalize the results. More, as suggested by Diemer and colleagues (62), VR can be used to induce emotional reactions via different routes (perceptual vs. conceptual), with additive effects if combined.
These studies are in agreement with the results obtained by Craske et al. (89) on the inhibitory learning approach presenting exposure optimization strategies such as (a) “deepened extinction,” where multiple fear stimuli are first extinguished separately before being combined during extinction; (b) “variability,” using different stimuli, levels of intensity, and durations; or (c) “exposure to multiple contexts,” different in terms of colors and textures. These kinds of effects are not easy to obtain in the “real world” but easier to achieve by using VR.
A similar process can be used in addiction. As underlined by two systematic review by Bordnick and colleagues (90) and Hone-Blanchet and colleagues (91), VR stimuli (e.g., liquor bottles and cigarette packs) and VR environments (e.g., bar and party) are effective in inducing strong craving in cocaine/alcohol/smoking-dependent subjects. It is supposed that the reactions induced by VR cues support motivational processes reducing relapse in addicts attempting to remain abstinent (92, 93). The same result is reported in the recent meta-analysis by Pericot-Valverde and colleagues exploring the use of VR in cigarette craving assessment. The paper confirms the potential of VR “for the generation of robust cue-specific craving in cue-reactivity research” (94). As discussed before, the use of VR exposure allows patients to experience arousal and reactivity in a controlled setting, and to develop new coping skills through repeated exposures and practice (95).
The use of VR as a controlled setting in which to develop new skills through trials and errors is also effective with persons with autistic spectrum disorder. The two systematic reviews support the use of VR to learn how to cope with social situations (96, 97), in particular to learn communication and imitation skills.
In summary, as underlined by Pla-Sanjuanelo and colleagues (98) “the capability of developing a large amount of realistic controlled stimuli and, simultaneously, of monitoring the responses generated by the user offers a considerable advantage over real experiences” (p. 145). For example, if an individual experiences a significant fear when exposed to heights, using a virtual elevator simulation, the therapist can assure him/her that this threat will be experienced only when he/she is prepared to cope with it. The same can be said for all the elements that are present in the situation, which can make it more or less threatening (99, 100). For instance, the height of the spaces, the presence of protecting elements, and the duration of a determined situation.
More, VR allows the construction of “virtual adventures” in which subjects experience themselves as competent and efficacious (47, 101, 102). Specifically, it is possible to design targeted VR experiences with different difficulty levels – from easy performances to very difficult ones – that offer an important source of personal efficacy. Interacting with them individuals discover that the conflicts and/or feared situations can be overcome through confrontation and effort (85).
Finally, as recently suggested by Gaggioli (25), a further opportunity offered by VR is the possibility of simulating impossible worlds – that is, worlds that do not conform to the fundamental laws of logic and nature. For example, Friedman and colleagues used VR to give people the illusion of backwards time travel allowing them to relive a sequence of events in which they can intervene and change history. In this view, time alterations and time paradoxes (e.g., the possibility of changing and restructuring the history) represent a kind of impossible manipulation of physical reality that is feasible in virtual reality and that can be used to elicitate transformative experiences (103).
Virtual Reality as Embodied and Transformative Technology
However, VR is more than a tool to provide exposure, training, and desensitization (104), as evidenced by the other areas of behavioral health in which VR systematic reviews have been found: depression, psychosis, schizophrenia, pain management, obesity, and eating disorders.
The first three applicative areas are still in their infancy. The systematic review discussing the use of VR in depression (105) and psychosis (106) suggests that VRET may be effective both for reducing depression caused by fear and for investigating psychological processes and mechanisms associated with psychosis. However, actual studies are not conclusive (105, 106). A similar picture is provided by the two systematic reviews assessing the use of VR in schizophrenia (107, 108): there is no clear good quality evidence for or against using VR for treatment compliance among people with schizophrenia (107), even if existing studies suggest a potential for increasing our understanding of psychosis (108). The situation is different for pain management and the treatment of obesity and eating disorders.
The four systematic reviews related to the use of VR in pain management support its use in the treatment of acute pain (109–112) and, in particular, in reducing the pain experienced by burn injury patients during wound dressing changes (109, 110). A strong overall evidence has been found for immediate and short-term pain reduction after VR, while moderate one for short-term effects on physical function. A recent systematic review tried to shed some light on the rationale of this approach (112). The results suggest that if on one side, the sense of presence influences the effectiveness of VR as a distraction tool, on the other side anxiety as well as positive emotions directly affect the experience of pain. The potential of VR in the treatment of pain was recently confirmed by “The Italian Consensus Conference on Pain in Neurorehabilitation” (113). In their analysis of the psychological interventions and psychotherapies that can be used within an integrated approach for patients undergoing neurological rehabilitation for pain, authors included the use of VR (grade of recommendation: D) for acute pain management (113).
A similar outcome is provided by the three systematic reviews related to the use of VR in the treatment of obesity and eating disorders (114–116): both VR cue exposure to food stimuli (115–117) and VR body image treatments (114, 115) are effective. A recent narrative review (117) confirms these data concluding that “VR has, for the past two decades, proven to be a useful adjunctive tool for both assessment and treatment of patients with eating disorders and obesity” (p. 71). In particular, as underlined by Gutiérrez-Maldonado and colleagues (118): “Recent studies indicate that … VR can integrate and extend existing treatments for eating and weight disorders. Future possibilities for VR to improve actual approaches include its use for altering in real time the experience of the body (embodiment) and as a cue exposure tool for reducing food craving” (p. 148).
But what is the link between the use of VR in pain and eating/weight disorders? Both are effective in modifyng the experience of the body of their users. Let us try to deepen this claim.
Virtual reality can be defined as an “embodied technology” for “its ability of modifying the feeling of presence” (119–121): in VR, subjects can experience the synthetic environment as if it was “their surrounding world” (incarnation: the physical body is within a virtual environment) or can experience their synthetic avatars as if they were “their own body” (embodiment: the physical body is replaced by the virtual one). In other words, the VR user is present in a virtual world or in a virtual body through the alteration of the cognitive factors regulating our experience of body and space [for an in-depth analysis of this claim, see Ref. (119)]. The side effect of this alteration is the experience of simulation sickness experienced by some VR users: the conflict between the visually perceived movement in the virtual world and the vestibular system’s sense of movement (I stand still) may produce negative effect like vomiting, discomfort, disorientation, and fatigue (122).
The increasing interest of cognitive science and social psychology for the experience of the body – Bodily Self-Consciousness – BSC – is providing a better picture of these processes.
First, BSC is apparently experienced by the subject as a single and coherent experience. However, neuroimaging and clinical data suggest that BSC is the outcome of different experiential layers (123–127). Specifically, we become aware of our bodies through exteroceptive signals arising outside the body (e.g., vision, and touch) and through proprioceptive (e.g., skeletal joints/muscles) and interoceptive (e.g., heart rate) signals arising inside the body (128, 129).
Second, the above studies support also the idea that body representations play a central role in structuring cognition and the self (124, 130–132). As underlined by Blanke (124) in his paper for Nature Reviews Neuroscience: “Human adults experience a “real me” that “resides” in “my” body and is the subject (or “I”) of experience and thought. This aspect of self-consciousness, namely the feeling that conscious experiences are bound to the self and are experiences of a unitary entity (“I”), is often considered to be one of the most astonishing features of the human mind” (p. 556). For this reason, the experience of the body is strictly connected to processes like cognitive development and autobiographical memory.
Third, we use the “feelings” from the body to sense both our physical condition and emotional state. These feelings range from bodily changes both visible (e.g., posture, touch, and facial expressions) and invisible (e.g., heart rate, endocrine release, and muscle contractions) to an external observer (133).
Fourth, the characteristics of BSC evolve over time following the ontogenetic development of the subject. As suggested by Riva (134), we expand over time our BSC by progressively including new experiences – minimal selfhood, self-location, agency, body ownership, third-person perspective, and body satisfaction – based on different and more sophisticated bodily representations that progressively integrate.
Fifth, bodily representations are usually produced and modulated by sensory inputs, but they can exist and produce qualitatively rich bodily experiences even in the absence of any input signal (e.g., phantom limb syndrome) (135). In this view, the experience of our bodily self is the outcome of a multimodal simulation. As underlined by Wilson (136): “The human perceptual system incorporates an emulator… that is isomorphic to the human body…the emulator draws on body-schematic knowledge derived from the observer’s representation of his own body” (p. 221).
Starting from these premises in 2007, two European teams of cognitive neuroscientists independently reported in Science how VR could be used for altering BSC (producing an out-of-body experience) in healthy volunteers (137, 138). Since then, the rapid development of immersive VR environments has allowed a new research line – virtual embodiment – (139–142) whose results are discussed in two recent reviews (143, 144). But how the experience of “being” in a synthetic body is achieved in these studies? These experiments are an evolution of the trick used in the low-tech rubber-hand illusion (145): the cross-modal congruence between what a person feels via the somatosensory pathways (touch) and what (s)he sees in VR. Using VR, different authors induced the illusion of a fake hand (146) or a fake limb (147) and produced an out-of-body experience (137) by modifying the normal association between touch and vision. Slater and colleagues even used VR to induce a body transfer illusion (147): they transferred a group of male subjects in a life-sized virtual human female body. Interestingly, altering the experience of the body has significant effects also on social cognition: for example, the transfer illusion in a body of different race produced a significant reduction of the implicit bias against that race (148).
But, how can these research data drive a new generation of VR tools aimed at supporting personal and clinical change? Up to now, VR has been used to simulate external reality, which is to make people feel “real” what is actually not really there. The next step is the use of VR for the simulation of our internal reality, including the way we perceive our body, control it, and affectively react to what happens to it. The final outcome is a new generation of transformative experiences that provide knowledge that is epistemically inaccessible to the individual until he or she has that experience, while at the same time transforming the individual’s worldview (25).
This opportunity may also open a radically new research field in medicine – Embodied Medicine – allowing new clinical solutions for the treatment of neurological and psychiatric disorders where our BSC seems to be altered (119). Considerable evidence suggests that the etiology of different disorders – including PTSD, eating disorders, depression, chronic pain, phantom limb pain, autism, schizophrenia, Parkinson’s and Alzheimer’s – may be related to an impaired/altered BSC. More, it may offer a scientific path to improve the level of well-being in non-clinical subjects by inducing positive emotions, improving attitudes, and helping individuals in understanding and controlling the signals of their body.
In general, it is possible to modify our BSC in three different ways (see Table 1) (25, 119, 120, 149, 150):
-
•
By structuring BSC through the focus and reorganization of its contents (mindful embodiment): individuals have different levels of body awareness is the extent of sensitivity and attentiveness to bodily signals and sensations (151). VR, if integrated with other technologies like biosensors, can be applied for improving body awareness. For example, in integration with biofeedback, training can be used to assess and control specific body signals like heart rate, galvanic skin response, electromyography, or electroencephalography (152, 153).
-
•
By augmenting BSC to achieve enhanced and extended experiences by altering/extending its boundaries (augmented embodiment): by integrating VR with biosensors, stimulation, and haptic devices, it is possible to map the contents of a sensory channel to a different one – e.g., vision to touch or to hearing – for augmenting its sensibility and replacing the impaired channels (150).
-
•
By replacing the contents of BSC with synthetic ones (synthetic embodiment): as we have seen before, VR allows different type of synthetic bodily experiences. The most advanced is the “full body swapping” in which the individual’s body is substituted by a virtual body (154). In other words, as in the movie Being John Malkovich, using VR, individuals can experience the perspective of another individual by seeing what the other see, hearing what the other hear, and touching what the other touch (155, 156). In a recent attempt of applying this method, Serino and colleagues (157) successfully used the illusion of body ownership over a body different to current one (a virtual body with a skinny belly) with a non-operable extreme obese patient (e.g., body mass index >60 kg/m2). Their data show that, after body swapping, the patient reduced the levels of body dissatisfaction and body distortion. More, she increased her motivation for undertaking healthy behavior and decreased the level of anxiety feelings associated with her clinical condition.
Conclusion
This paper claimed that virtual technologies – AR and VR – have the potential for supporting personal and clinical change: if AR adds virtual information to the real world, VR completely replaces the real environment with a virtual one. Specifically, both AR and VR can transform our external experience through the high level of personal efficacy and self-reflectiveness generated by their sense of presence and emotional engagement. Moreover, VR can also modify our inner experience by structuring, altering, and/or replacing our BSC.
In the first part of the paper, we explored the characteristics of the process of change. By integrating the available literature, we identified three critical steps that may slow down or block the process.
First, the process of change requires self-reflectiveness: an intense focus on the particular instance or experience creating the conflict (26). By focusing on this experience as much as possible, the individual can relive and identify any significant element (e.g., conceptual, behavioral, emotional, and motivational) facilitating its reorganization (24).
Second, the process of change requires personal efficacy (16, 17): individuals have to believe that they have the power to effect changes through their actions. Without it there, they are not willing to act or to keep on acting in the face of problems and difficulties.
Finally, the process of change can be dramatically boosted by transformative experiences (22, 23), forcing individuals to critically examine and eventually revise their core assumptions and beliefs. The key advantage of these experiences is that they are epochal (158): “a sudden, dramatic, and reorienting insight” (p. 86) pushing the individual to an immediate and irreversible change. Unfortunately, most transformative experiences cannot be planned in advance, but happen suddenly in individuals’ lives, without a prior control on their contents and their effects.
In the second part of the paper, we analyzed the outcomes of the available systematic reviews and meta-analyses related to the use of virtual technologies in behavioral health to identify and discuss the added values offered by them.
The only available systematic review for AR support its use in the treatment of phobias. Moreover, it also outlines the value of AR as experiential learning tool. On one side, it offers real-time interactivity in an ecological setting improving concentration and motivation (45). On the other side, it provides targeted and non-directive suggestions and guidelines helping individuals to develop skills and knowledge in a more effective way (46). Finally, AR can be used in the actual places where the subject encounter his difficulties, facilitating the transfer of the acquired skills to the real world (32).
The 27 meta-analyses and systematic reviews available for VR support the use of this technology in the treatment of anxiety disorders, stress-related disorders, obesity and eating disorders, and pain management. But still, there is no clear good quality evidence for or against using VR for the treatment of depression and schizophrenia.
In most pathologies, VR is used as simulative tool for controlled exposure to critical/fearful situations. The possibility of presenting realistic controlled stimuli and, simultaneously, of monitoring the responses generated by the user offers a considerable advantage over real experiences. More, the possibility of designing targeted VR experiences with different difficulty levels – from easy performances to very difficult ones – offers an important source of personal efficacy.
However, the use of VR in pain management and in the treatment of obesity and eating disorders suggest a different rationale: VR can also be used as an embodied technology able to alter our experience of the body and space. If most VR applications to date have been used to simulate external reality, it is also possible to use VR for the simulation of our internal reality including the perception and ownership of our body. The final outcome may be a new generation of transformative experiences that provide knowledge that is epistemically inaccessible to the individual until he or she has that experience, while at the same time transforming the individual’s worldview and pushing him/her to an immediate and irreversible personal or clinical change (25, 159). More, it may offer a scientific path to improve the level of well-being in non-clinical subjects by inducing positive emotions, improving attitudes, and helping individuals in understanding and controlling the signals of their body.
At the end, the contents of this review offer a sound foundation and rationale for researchers interested in using virtual technologies for improving personal and clinical change.
Author Contributions
GR performed the literature review and drafted the first version of the manuscript. RB, CB, FM, and AG supervised the rationale and the scientific contributions. All authors read and approved the final manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding
This paper was funded by the research project “Tecnologia Positiva e Healthy Ageing” funded by Università Cattolica del Sacro Cuore (D3.2, Ricerche di interesse d’Ateneo 2014).
References
- 1.Janoff-Bulman R, Schwartzberg SS. Chapter 24. Toward a general model of personal change. In: Snyder CR, Forsyth DR, editors. Handbook of Social and Clinical Psychology: The Health Perspective. New York: Pergamon Press; (1991). p. 488–508. [Google Scholar]
- 2.Blackie L, Jayawickreme E, Forgeard M, Jayawickreme N. The protective function of belief in personal change among genocide survivors in Rwanda. Pers Individ Dif (2014) 60(S1):S15–6. 10.1016/j.paid.2013.07.369 [DOI] [Google Scholar]
- 3.Higginson S, Mansell W. What is the mechanism of psychological change? A qualitative analysis of six individuals who experienced personal change and recovery. Psychol Psychother (2008) 81:309–28. 10.1348/147608308X320125 [DOI] [PubMed] [Google Scholar]
- 4.Stiles WB, Shapiro DA, Elliott R. Are all psychotherapies equivalent. Am Psychol (1986) 41(2):165–80. 10.1037/0003-066X.41.2.165 [DOI] [PubMed] [Google Scholar]
- 5.Stiles WB, Barkham M, Twigg E, Mellor-Clark J, Cooper M. Effectiveness of cognitive-behavioural, person-centred and psychodynamic therapies as practised in UK National Health Service settings. Psychol Med (2006) 36(4):555–66. 10.1017/S0033291706007136 [DOI] [PubMed] [Google Scholar]
- 6.Kottler JA. Change: What Really Leads to Lasting Personal Transformation. New York, NY: Oxford University Press; (2014). [Google Scholar]
- 7.Cohen GL, Sherman DK. The psychology of change: self-affirmation and social psychological intervention. Annu Rev Psychol (2014) 65:333–71. 10.1146/annurev-psych-010213-115137 [DOI] [PubMed] [Google Scholar]
- 8.Hayes AM, Laurenceau JP, Feldman G, Strauss JL, Cardaciotto L. Change is not always linear: the study of nonlinear and discontinuous patterns of change in psychotherapy. Clin Psychol Rev (2007) 27(6):715–23. 10.1016/j.cpr.2007.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Higginson S, Mansell W, Wood AM. An integrative mechanistic account of psychological distress, therapeutic change and recovery: the Perceptual Control Theory approach. Clin Psychol Rev (2011) 31(2):249–59. 10.1016/j.cpr.2010.01.005 [DOI] [PubMed] [Google Scholar]
- 10.Vancouver JB, Putka DJ. Analyzing goal-striving processes and a test of the generalizability of perceptual control theory. Organ Behav Hum Decis Process (2000) 82(2):334–62. 10.1006/obhd.2000.2901 [DOI] [PubMed] [Google Scholar]
- 11.Gianakis M, Carey TA. An interview study investigating experiences of psychological change without psychotherapy. Psychol Psychother (2011) 84(4):442–57. 10.1111/j.2044-8341.2010.02002.x [DOI] [PubMed] [Google Scholar]
- 12.Sherman DK, Cohen GL. The psychology of self-defense: self-affirmation theory. Adv Exp Soc Psychol (2006) 38:183–242. 10.1016/S0065-2601(06)38004-5 [DOI] [Google Scholar]
- 13.Aronson J, Cohen G, Nail PR. Self-affirmation theory: an update and appraisal. In: Harmon-Jones E, Mills J, editors. Cognitive Dissonance: Progress on a Pivotal Theory in Social Psychology. Washington, DC: American Psychological Association; (1999). p. 127–147. [Google Scholar]
- 14.Bandura A. Exercise of control through self-belief – a citation classic commentary on self-efficacy – toward a unifying theory of behavioral-change by Bandura, A. Cc/Soc Behav Sci (1989) 20:14–14. [Google Scholar]
- 15.Bandura A. Self-efficacy – toward a unifying theory of behavioral change. Psychol Rev (1977) 84(2):191–215. 10.1037/0033-295X.84.2.191 [DOI] [PubMed] [Google Scholar]
- 16.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol (2001) 52:1–26. 10.1146/annurev.psych.52.1.1 [DOI] [PubMed] [Google Scholar]
- 17.Bandura A. Toward a psychology of human agency. Perspect Psychol Sci (2006) 1(2):164–80. 10.1111/j.1745-6916.2006.00011.x [DOI] [PubMed] [Google Scholar]
- 18.Prochaska JO, DiClemente CC. Transtheoretical therapy: toward a more integrative model of change. Psychother Theory Res Pract (1982) 19(3):212–6. 10.1037/h0088437 [DOI] [Google Scholar]
- 19.Prochaska JO, DiClemente CC. Stages and processes of self-change in smoking toward an integrative model of change. J Consult Clin Psychol (1983) 5:390–5. 10.1037/0022-006X.51.3.390 [DOI] [PubMed] [Google Scholar]
- 20.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Am Psychol (1992) 47(9):1102–14. 10.1037/0003-066X.47.9.1102 [DOI] [PubMed] [Google Scholar]
- 21.Miller WR, C’de Baca J. Quantum Change: When Epiphanies and Sudden Insights Transform Ordinary Lives. New York: Guilford Press; (2001). [Google Scholar]
- 22.Mezirow J. Learning as Transformation: Critical Perspectives on a Theory in Progress. San Francisco, CA: Jossey-Bass; (2000). [Google Scholar]
- 23.Mezirow J. Transformative Dimensions of Adult Learning. San Francisco, CA: Jossey-Bass; (1991). [Google Scholar]
- 24.Riva G. Phenomenology of positive change: personal growth. In: Inghilleri P, Riva G, Riva E, editors. Enabling Positive Change Flow and Complexity in Daily Experience. Berlin: De Gruyter; (2014). p. 15–28. [Google Scholar]
- 25.Gaggioli A. Transformative experience design. In: Gaggioli A, Ferscha A, Riva G, Dunne S, Viaud-Delmon I, editors. Human Computer Confluence: Transforming Human Experience Through Symbiotic Technologies. Warsaw: De Gruyter Open; (2015). p. 97–121. [Google Scholar]
- 26.Wolfe BE. The role of lived experience in self- and relational observation: a commentary on Horowitz (2002). J Psychother Integr (2002) 12(2):147–53. 10.1037/1053-0479.12.2.147 [DOI] [Google Scholar]
- 27.Hugues O, Fuchs P, Nannipieri O. New Augmented Reality Taxonomy: Technologies and Features of Augmented Environment. Heidelberg: Springer; (2011). [Google Scholar]
- 28.Chicchi Giglioli IA, Pallavicini F, Pedroli E, Serino S, Riva G. Augmented reality: a brand new challenge for the assessment and treatment of psychological disorders. Comput Math Methods Med (2015) 862942:1–13. 10.1155/2015/862942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Juan MC, Alcaniz M, Monserrat C, Botella C, Banos RM, Guerrero B. Using augmented reality to treat phobias. IEEE Comput Graph Appl (2005) 25(6):31–7. 10.1109/MCG.2005.143 [DOI] [PubMed] [Google Scholar]
- 30.Milgram P, Kishino F. A taxonomy of mixed reality visual displays. IEICE Trans Inf Syst (1994) 12:1321–9. [Google Scholar]
- 31.van Krevelen DWF, Poelman R. A survey of augmented reality technologies, applications and limitations. Int J Virtual Real (2010) 9(2):1–20. [Google Scholar]
- 32.Baus O, Bouchard S. Moving from virtual reality exposure-based therapy to augmented reality exposure-based therapy: a review. Front Hum Neurosci (2014) 8:112. 10.3389/fnhum.2014.00112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shiban Y, Schelhorn I, Pauli P, Muhlberger A. Effect of combined multiple contexts and multiple stimuli exposure in spider phobia: a randomized clinical trial in virtual reality. Behav Res Ther (2015) 71:45–53. 10.1016/j.brat.2015.05.014 [DOI] [PubMed] [Google Scholar]
- 34.Trojan J, Diers M, Fuchs X, Bach F, Bekrater-Bodmann R, Foell J, et al. An augmented reality home-training system based on the mirror training and imagery approach. Behav Res Methods (2014) 46(3):634–40. 10.3758/s13428-013-0412-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lin CY, Chang YM. Interactive augmented reality using Scratch 2.0 to improve physical activities for children with developmental disabilities. Res Dev Disabil (2015) 37:1–8. 10.1016/j.ridd.2014.10.016 [DOI] [PubMed] [Google Scholar]
- 36.Kaber D, Tupler LA, Clamann M, Gil GH, Zhu B, Swangnetr M, et al. Evaluation of an augmented virtual reality and haptic control interface for psychomotor training. Assist Technol (2014) 26(1):51–60. 10.1080/10400435.2013.800923 [DOI] [PubMed] [Google Scholar]
- 37.Chung PJ, Vanderbilt DL, Soares NS. Social behaviors and active videogame play in children with autism spectrum disorder. Games Health J (2015) 4(3):225–34. 10.1089/g4h.2014.0125 [DOI] [PubMed] [Google Scholar]
- 38.Chen CH, Lee IJ, Lin LY. Augmented reality-based self-facial modeling to promote the emotional expression and social skills of adolescents with autism spectrum disorders. Res Dev Disabil (2014) 36C:396–403. 10.1016/j.ridd.2014.10.015 [DOI] [PubMed] [Google Scholar]
- 39.Mott J, Bucolo S, Cuttle L, Mill J, Hilder M, Miller K, et al. The efficacy of an augmented virtual reality system to alleviate pain in children undergoing burns dressing changes: a randomised controlled trial. Burns (2008) 34(6):803–8. 10.1016/j.burns.2007.10.010 [DOI] [PubMed] [Google Scholar]
- 40.Kolb DA. Experiential Learning as the Science of Learning and Development. Englewood Cliffs, NJ: Prentice Hall; (1984). [Google Scholar]
- 41.Konak A, Clark TK, Nasereddin M. Using Kolb’s experiential learning cycle to improve student learning in virtual computer laboratories. Comput Educ (2014) 72:11–22. 10.1016/j.compedu.2013.10.013 [DOI] [Google Scholar]
- 42.Botella C, Breton-Lopez J, Quero S, Banos R, Garcia-Palacios A. Treating cockroach phobia with augmented reality. Behav Ther (2010) 41(3):401–13. 10.1016/j.beth.2009.07.002 [DOI] [PubMed] [Google Scholar]
- 43.Breton-Lopez J, Quero S, Botella C, Garcia-Palacios A, Banos RM, Alcaniz M. An augmented reality system validation for the treatment of cockroach phobia. Cyberpsychol Behav Soc Netw (2010) 13(6):705–10. 10.1089/cyber.2009.0170 [DOI] [PubMed] [Google Scholar]
- 44.Botella C, Breton-Lopez J, Quero S, Banos RM, Garcia-Palacios A, Zaragoza I, et al. Treating cockroach phobia using a serious game on a mobile phone and augmented reality exposure: a single case study. Comput Human Behav (2011) 27(1):217–27. 10.1016/j.chb.2010.07.043 [DOI] [Google Scholar]
- 45.Di Serio A, Ibanez MB, Kloos CD. Impact of an augmented reality system on students’ motivation for a visual art course. Comput Educ (2013) 68:586–96. 10.1016/j.compedu.2012.03.002 [DOI] [Google Scholar]
- 46.Wu HK, Lee SWY, Chang HY, Liang JC. Current status, opportunities and challenges of augmented reality in education. Comput Educ (2013) 62:41–9. 10.1016/j.compedu.2012.10.024 [DOI] [Google Scholar]
- 47.Riva G, Botella C, Baños R, Mantovani F, García-Palacios A, Quero S, et al. Presence-inducing media for mental health applications. In: Lombard M, Biocca F, Freeman J, Ijsselsteijn W, Schaevitz RJ, editors. Immersed in Media. New York: Springer International Publishing; (2015). p. 283–332. [Google Scholar]
- 48.Riva G, Gamberini L. Virtual reality in telemedicine. Telemed J E Health (2004) 6(3):327–40. 10.1089/153056200750040183 [DOI] [PubMed] [Google Scholar]
- 49.Schultheis MT, Rizzo AA. The application of virtual reality technology in rehabilitation. Rehabil Psychol (2001) 46(3):296–311. 10.1037/0090-5550.46.3.296 [DOI] [Google Scholar]
- 50.Riva G. Virtual environments in neuroscience. IEEE Trans Inf Technol Biomed (1998) 2(4):275–81. 10.1109/4233.737583 [DOI] [PubMed] [Google Scholar]
- 51.Riva G, Waterworth JA. Presence and the self: a cognitive neuroscience approach. Presence Connect (2003) 3(3). Available from: http://www8.informatik.umu.se/~jwworth/Riva-Waterworth.htm [Google Scholar]
- 52.Gorini A, Capideville CS, De Leo G, Mantovani F, Riva G. The role of immersion and narrative in mediated presence: the virtual hospital experience. Cyberpsychol Behav Soc Netw (2011) 14(3):99–105. 10.1089/cyber.2010.0100 [DOI] [PubMed] [Google Scholar]
- 53.Zahoric P, Jenison RL. Presence as being-in-the-world. Presence (Camb) (1998) 7(1):78–89. 10.1162/105474698565541 [DOI] [Google Scholar]
- 54.Riva G, Waterworth JA, Murray D, editors. Interacting with Presence: HCI and the Sense of Presence in Computer-Mediated Environments. Berlin: De Gruyter Open; (2014). Available from: http://www.presence-research.com [Google Scholar]
- 55.Riva G, Davide F, IJsselsteijn WA, editors. Being There: Concepts, effects and Measurements of User Presence in Synthetic Environments. Amsterdam: Ios Press; (2003). [Google Scholar]
- 56.Lee KM. Presence, explicated. Commun Theory (2004) 14(1):27–50. 10.1111/j.1468-2885.2004.tb00302.x [DOI] [Google Scholar]
- 57.Lombard M, Biocca F, Freeman J, IJsselsteijn W, Schaevitz RJ, editors. Immersed in Media. Telepresence Theory, Measurement & Technology. Heidelberg: Springer; (2015). [Google Scholar]
- 58.Waterworth JA, Riva G. Feeling Present in the Physical World and in Computer-Mediated Environments. London: Palgrave Macmillan; (2014). [Google Scholar]
- 59.Banos RM, Botella C, Alcaniz M, Liano V, Guerrero B, Rey B. Immersion and emotion: their impact on the sense of presence. Cyberpsychol Behav (2004) 7(6):734–41. 10.1089/cpb.2004.7.734 [DOI] [PubMed] [Google Scholar]
- 60.Banos RM, Botella C, Rubio I, Quero S, Garcia-Palacios A, Alcaniz M. Presence and emotions in virtual environments: the influence of stereoscopy. Cyberpsychol Behav (2008) 11(1):1–8. 10.1089/cpb.2007.9936 [DOI] [PubMed] [Google Scholar]
- 61.Pillai JS, Schmidt C, Richir S. Achieving presence through evoked reality. Front Psychol (2013) 4:86. 10.3389/fpsyg.2013.00086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Diemer J, Alpers GW, Peperkorn HM, Shiban Y, Muhlberger A. The impact of perception and presence on emotional reactions: a review of research in virtual reality. Front Psychol (2015) 6:26. 10.3389/fpsyg.2015.00026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sethi AK, Suzuki K, Critchley HD. An interoceptive predictive coding model of conscious presence. Front Psychol (2012) 3:395. 10.3389/fpsyg.2011.00395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Riva G. Neuroscience and eating disorders: the allocentric lock hypothesis. Med Hypotheses (2012) 78:254–7. 10.1016/j.mehy.2011.10.039 [DOI] [PubMed] [Google Scholar]
- 65.Riva G. Is presence a technology issue? Some insights from cognitive sciences. Virtual Real (2009) 13(3):59–69. 10.1007/s10055-009-0121-6 [DOI] [Google Scholar]
- 66.Ling Y, Nefs HT, Morina N, Heynderickx I, Brinkman WP. A meta-analysis on the relationship between self-reported presence and anxiety in virtual reality exposure therapy for anxiety disorders. PLoS One (2014) 9(5):e96144. 10.1371/journal.pone.0096144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Baños RM, Botella C, Guerrero B, Liaño V, Alcañiz M, Rey B. The third pole of the sense of presence: comparing virtual and imagery spaces. PsychNol J (2005) 3(1):90–100. Available from: http://www.psychnology.org/index.php?page=abstract---volume-3---banos [Google Scholar]
- 68.Riva G, Bacchetta M, Cesa G, Conti S, Molinari E. Six-month follow-up of in-patient experiential-cognitive therapy for binge eating disorders. Cyberpsychol Behav (2003) 6(3):251–8. 10.1089/109493103322011533 [DOI] [PubMed] [Google Scholar]
- 69.North MM, North SM, Coble JR. Virtual reality therapy: an effective treatment for psychological disorders. Stud Health Technol Inform (1997) 44:59–70. [PubMed] [Google Scholar]
- 70.Vincelli F. From imagination to virtual reality: the future of clinical psychology. Cyberpsychol Behav (1999) 2(3):241–8. 10.1089/cpb.1999.2.241 [DOI] [PubMed] [Google Scholar]
- 71.Vincelli F, Molinari E, Riva G. Virtual reality as clinical tool: immersion and three-dimensionality in the relationship between patient and therapist. Stud Health Technol Inform (2001) 81:551–3. 10.3233/978-1-60750-925-7-551 [DOI] [PubMed] [Google Scholar]
- 72.Glantz K, Durlach NI, Barnett RC, Aviles WA. Virtual reality (VR) and psychotherapy: opportunities and challenges. Presence (Camb) (1997) 6(1):87–105. 10.1162/pres.1997.6.1.87 [DOI] [PubMed] [Google Scholar]
- 73.Riva G, Mantovani F, Gaggioli A. Presence and rehabilitation: toward second-generation virtual reality applications in neuropsychology. J Neuroeng Rehabil (2004) 1(1):9. 10.1186/1743-0003-1-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Parsons TD, Rizzo AA. Affective outcomes of virtual reality exposure therapy for anxiety and specific phobias: a meta-analysis. J Behav Ther Exp Psychiatry (2008) 39(3):250–61. 10.1016/j.jbtep.2007.07.007 [DOI] [PubMed] [Google Scholar]
- 75.Powers MB, Emmelkamp PM. Virtual reality exposure therapy for anxiety disorders: a meta-analysis. J Anxiety Disord (2008) 22(3):561–9. 10.1016/j.janxdis.2007.04.006 [DOI] [PubMed] [Google Scholar]
- 76.Meyerbroker K, Emmelkamp PM. Virtual reality exposure therapy in anxiety disorders: a systematic review of process-and-outcome studies. Depress Anxiety (2010) 27(10):933–44. 10.1002/da.20734 [DOI] [PubMed] [Google Scholar]
- 77.Opris D, Pintea S, Garcia-Palacios A, Botella C, Szamoskozi S, David D. Virtual reality exposure therapy in anxiety disorders: a quantitative meta-analysis. Depress Anxiety (2012) 29(2):85–93. 10.1002/da.20910 [DOI] [PubMed] [Google Scholar]
- 78.McCann RA, Armstrong CM, Skopp NA, Edwards-Stewart A, Smolenski DJ, June JD, et al. Virtual reality exposure therapy for the treatment of anxiety disorders: an evaluation of research quality. J Anxiety Disord (2014) 28(6):625–31. 10.1016/j.janxdis.2014.05.010 [DOI] [PubMed] [Google Scholar]
- 79.Diemer J, Muhlberger A, Pauli P, Zwanzger P. Virtual reality exposure in anxiety disorders: impact on psychophysiological reactivity. World J Biol Psychiatry (2014) 15(6):427–42. 10.3109/15622975.2014.892632 [DOI] [PubMed] [Google Scholar]
- 80.Goncalves R, Pedrozo AL, Coutinho ES, Figueira I, Ventura P. Efficacy of virtual reality exposure therapy in the treatment of PTSD: a systematic review. PLoS One (2012) 7(12):e48469. 10.1371/journal.pone.0048469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Serino S, Triberti S, Villani D, Cipresso P, Gaggioli A, Riva G. Toward a validation of cyber-interventions for stress disorders based on stress inoculation training: a systematic review. Virtual Real (2014) 18(1):73–87. 10.1007/s10055-013-0237-6 [DOI] [Google Scholar]
- 82.Motraghi TE, Seim RW, Meyer EC, Morissette SB. Virtual reality exposure therapy for the treatment of posttraumatic stress disorder: a methodological review using CONSORT guidelines. J Clin Psychol (2014) 70(3):197–208. 10.1002/jclp.22051 [DOI] [PubMed] [Google Scholar]
- 83.Botella C, Serrano B, Baños R, García-Palacios A. Virtual reality exposure-based therapy for the treatment of posttraumatic stress disorder. A review of its efficacy, the adequacy of the treatment protocol, and its acceptability. Neuropsychiatr Dis Treat (2015) 15:2533–45. 10.2147/NDT.S89542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Choi YH, Vincelli F, Riva G, Wiederhold BK, Lee JH, Park KH. Effects of group experiential cognitive therapy for the treatment of panic disorder with agoraphobia. Cyberpsychol Behav (2005) 8(4):387–93. 10.1089/cpb.2005.8.387 [DOI] [PubMed] [Google Scholar]
- 85.Riva G, Mantovani F. Being there: understanding the feeling of presence in a synthetic environment and its potential for clinical change. In: Eichenberg C, editor. Virtual Reality in Psychological, Medical and Pedagogical Applications. New York: InTech; (2012). p. 3–34. Available from: http://www.intechopen.com/books/virtual-reality-in-psychological-medical-and-pedagogical-applications/being-there-understanding-the-feeling-of-presence-in-a-synthetic-environment-and-its-potential-for-c [Google Scholar]
- 86.Gorini A, Riva G. Virtual reality in anxiety disorders: the past and the future. Expert Rev Neurother (2008) 8(2):215–33. 10.1586/14737175.8.2.215 [DOI] [PubMed] [Google Scholar]
- 87.Shiban Y, Pauli P, Muhlberger A. Effect of multiple context exposure on renewal in spider phobia. Behav Res Ther (2013) 51(2):68–74. 10.1016/j.brat.2012.10.007 [DOI] [PubMed] [Google Scholar]
- 88.Dunsmoor JE, Ahs F, Zielinski DJ, LaBar KS. Extinction in multiple virtual reality contexts diminishes fear reinstatement in humans. Neurobiol Learn Mem (2014) 113:157–64. 10.1016/j.nlm.2014.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Craske MG, Treanor M, Conway CC, Zbozinek T, Vervliet B. Maximizing exposure therapy: an inhibitory learning approach. Behav Res Ther (2014) 58:10–23. 10.1016/j.brat.2014.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Bordnick PS, Carter BL, Traylor AC. What virtual reality research in addictions can tell us about the future of obesity assessment and treatment. J Diabetes Sci Technol (2011) 5(2):265–71. 10.1177/193229681100500210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hone-Blanchet A, Wensing T, Fecteau S. The use of virtual reality in craving assessment and cue-exposure therapy in substance use disorders. Front Hum Neurosci (2014) 8:844. 10.3389/fnhum.2014.00844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bordnick PS, Graap KM, Copp HL, Brooks J, Ferrer M. Virtual reality cue reactivity assessment in cigarette smokers. Cyberpsychol Behav (2005) 8(5):487–92. 10.1089/cpb.2005.8.487 [DOI] [PubMed] [Google Scholar]
- 93.Bordnick PS, Traylor A, Copp HL, Graap KM, Carter B, Ferrer M, et al. Assessing reactivity to virtual reality alcohol based cues. Addict Behav (2008) 33(6):743–56. 10.1016/j.addbeh.2007.12.010 [DOI] [PubMed] [Google Scholar]
- 94.Pericot-Valverde I, Germeroth LJ, Tiffany ST. The use of virtual reality in the production of cue-specific craving for cigarettes: a meta-analysis. Nicotine Tob Res (2016) 18(5):538–46. 10.1093/ntr/ntv216 [DOI] [PubMed] [Google Scholar]
- 95.Riva G. Virtual reality for health care: the status of research. Cyberpsychol Behav (2002) 5(3):219–25. 10.1089/109493102760147213 [DOI] [PubMed] [Google Scholar]
- 96.Aresti-Bartolome N, Garcia-Zapirain B. Technologies as support tools for persons with autistic spectrum disorder: a systematic review. Int J Env Res Pub He (2014) 11(8):7767–802. 10.3390/ijerph110807767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.den Brok W, Sterkenburg P. Self-controlled technologies to support skill attainment in persons with an autism spectrum disorder and/or an intellectual disability: a systematic literature review. Disabil Rehabil Assist Technol (2014) 10(1):1–10. 10.3109/17483107.2014.921248 [DOI] [PubMed] [Google Scholar]
- 98.Riva G, Wiederhold BK. The new dawn of virtual reality in health care: medical simulation and experiential interface. Annu Rev Cybertherapy Telemed (2015) 13:3–6. [PubMed] [Google Scholar]
- 99.Pla-Sanjuanelo J, Ferrer-Garcia M, Gutiérrez-Maldonado J, Vilalta-Abella F, Andreu-Gracia A, Dakanalis A, et al. Trait and state craving as indicators of validity of VR-based software for binge eating treatment. Annu Rev Cybertherapy Telemed (2015) 13:141–6. [PubMed] [Google Scholar]
- 100.Ferrer-Garcia M, Gutiérrez-Maldonado J, Pla-Sanjuanelo J, Vilalta-Abella F, Andreu-Gracia A, Dakanalis A, et al. External eating as a predictor of cue-reactivity to food-related virtual environments. Annu Rev Cybertherapy Telemed (2015) 13:117–22. [PubMed] [Google Scholar]
- 101.Botella C, Quero S, Banos RM, Perpina C, Garcia Palacios A, Riva G. Virtual reality and psychotherapy. Stud Health Technol Inform (2004) 99:37–54. 10.3233/978-1-60750-943-1-37 [DOI] [PubMed] [Google Scholar]
- 102.Riva G, Gaggioli A, Villani D, Preziosa A, Morganti F, Corsi R, et al. NeuroVR: an open source virtual reality platform for clinical psychology and behavioral neurosciences. Stud Health Technol Inform (2007) 125:394–9. [PubMed] [Google Scholar]
- 103.Friedman D, Pizarro R, Or-Berkers K, Neyret S, Pan X, Slater M. A method for generating an illusion of backwards time travel using immersive virtual reality-an exploratory study. Front Psychol (2014) 5:943. 10.3389/fpsyg.2014.00943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Riva G. Medical clinical uses of virtual worlds. In: Grimshaw M, editor. The Oxford Handbook of Virtuality. New York: Oxford University Press; (2014). p. 649–65. [Google Scholar]
- 105.Li J, Theng YL, Foo S. Game-based digital interventions for depression therapy: a systematic review and meta-analysis. Cyberpsychol Behav Soc Netw (2014) 17(8):519–27. 10.1089/cyber.2013.0481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Valmaggia LR, Day F, Rus-Calafell M. Using virtual reality to investigate psychological processes and mechanisms associated with the onset and maintenance of psychosis: a systematic review. Soc Psychiatry Psychiatr Epidemiol (2016) 51(7):921–36. 10.1007/s00127-016-1245-0 [DOI] [PubMed] [Google Scholar]
- 107.Välimäki M, Hatonen HM, Lahti ME, Kurki M, Hottinen A, Metsaranta K, et al. Virtual reality for treatment compliance for people with serious mental illness. Cochrane Database Syst Rev (2014) 10:CD009928. 10.1002/14651858.CD009928.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Veling W, Moritz S, van der Gaag M. Brave new worlds – review and update on virtual reality assessment and treatment in psychosis. Schizophr Bull (2014) 40(6):1194–7. 10.1093/schbul/sbu125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Morris LD, Louw QA, Grimmer-Somers K. The effectiveness of virtual reality on reducing pain and anxiety in burn injury patients: a systematic review. Clin J Pain (2009) 25(9):815–26. 10.1097/AJP.0b013e3181aaa909 [DOI] [PubMed] [Google Scholar]
- 110.Malloy KM, Milling LS. The effectiveness of virtual reality distraction for pain reduction: a systematic review. Clin Psychol Rev (2010) 30(8):1011–8. 10.1016/j.cpr.2010.07.001 [DOI] [PubMed] [Google Scholar]
- 111.Garrett B, Taverner T, Masinde W, Gromala D, Shaw C, Negraeff M. A rapid evidence assessment of immersive virtual reality as an adjunct therapy in acute pain management in clinical practice. Clin J Pain (2014) 30(12):1089–98. 10.1097/AJP.0000000000000064 [DOI] [PubMed] [Google Scholar]
- 112.Triberti S, Repetto C, Riva G. Psychological factors influencing the effectiveness of virtual reality-based analgesia: a systematic review. Cyberpsychol Behav Soc Netw (2014) 17(6):335–45. 10.1089/cyber.2014.0054 [DOI] [PubMed] [Google Scholar]
- 113.Castelnuovo G, Giusti EM, Manzoni GM, Saviola D, Gatti A, Gabrielli S, et al. Psychological treatments and psychotherapies in the neurorehabilitation of pain: evidences and recommendations from the italian consensus conference on pain in neurorehabilitation. Front Psychol (2016) 7:115. 10.3389/fpsyg.2016.00115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ferrer-Garcia M, Gutierrez-Maldonado J. The use of virtual reality in the study, assessment, and treatment of body image in eating disorders and nonclinical samples: a review of the literature. Body Image (2012) 9(1):1–11. 10.1016/j.bodyim.2011.10.001 [DOI] [PubMed] [Google Scholar]
- 115.Ferrer-Garcia M, Gutiérrez-Maldonado J, Riva G. Virtual reality based treatments in eating disorders and obesity: a review. J Contemp Psychol (2013) 43(4):207–21. 10.1007/s10879-013-9240-1 [DOI] [Google Scholar]
- 116.Koskina A, Campbell IC, Schmidt U. Exposure therapy in eating disorders revisited. Neurosci Biobehav Rev (2013) 37(2):193–208. 10.1016/j.neubiorev.2012.11.010 [DOI] [PubMed] [Google Scholar]
- 117.Wiederhold BK, Riva G, Gutiérrez-Maldonado J. Virtual reality in the assessment and treatment of weight-related disorders. Cyberpsychol Behav Soc Netw (2016) 19(2):67–73. 10.1089/cyber.2016.0012 [DOI] [PubMed] [Google Scholar]
- 118.Gutiérrez-Maldonado J, Wiederhold BK, Riva G. Future directions: how virtual reality can further improve the assessment and treatment of eating disorders and obesity. Cyberpsychol Behav Soc Netw (2016) 19:148–53. 10.1089/cyber.2015.0412 [DOI] [PubMed] [Google Scholar]
- 119.Riva G, Dakanalis A, Mantovani F. Leveraging psychology of virtual body for health and wellness. In: Sundar SS, editor. The Handbook of the Psychology of Communication Technology. Chichester, UK: John Wiley & Sons, Ltd; (2015). p. 528–47. [Google Scholar]
- 120.Riva G, Mantovani F. Extending the self through the tools and the others: a general framework for presence and social presence in mediated interactions. In: Riva G, Waterworth JA, Murray D, editors. Interacting with Presence: HCI and the Sense of Presence in Computer-Mediated Environments. Berlin: De Gruyter Open; (2014). p. 12–34. Available from: http://www.presence-research.com [Google Scholar]
- 121.Riva G, Mantovani F. From the body to the tools and back: a general framework for presence in mediated interactions. Interact Comput (2012) 24(4):203–10. 10.1016/j.intcom.2012.04.007 [DOI] [Google Scholar]
- 122.Regan EC, Price KR. Some Side-Effects of Immersion Virtual Reality: The Effects of Increasing Head Movements, of Rapid Interaction, and of Seated Subjects. Farnborough, UK: Army Personnel Research Establishment; (1993). Report 93R022. [Google Scholar]
- 123.Pfeiffer C, Lopez C, Schmutz V, Duenas JA, Martuzzi R, Blanke O. Multisensory origin of the subjective first-person perspective: visual, tactile, and vestibular mechanisms. PLoS One (2013) 8(4):e61751. 10.1371/journal.pone.0061751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Blanke O. Multisensory brain mechanisms of bodily self-consciousness. Nat Rev Neurosci (2012) 13(8):556–71. 10.1038/nrn3292 [DOI] [PubMed] [Google Scholar]
- 125.Vogeley K, Fink GR. Neural correlates of the first-person-perspective. Trends Cogn Sci (2003) 7(1):38–42. 10.1016/S1364-6613(02)00003-7 [DOI] [PubMed] [Google Scholar]
- 126.Shilling C. The Body & Social Theory. London: SAGE; (2012). [Google Scholar]
- 127.Crossley N. The Social Body: Habit, Identity and Desire. London: SAGE; (2001). [Google Scholar]
- 128.Durlik C, Cardini F, Tsakiris M. Being watched: the effect of social self-focus on interoceptive and exteroceptive somatosensory perception. Conscious Cogn (2014) 25:42–50. 10.1016/j.concog.2014.01.010 [DOI] [PubMed] [Google Scholar]
- 129.Garfinkel SN, Critchley HD. Interoception, emotion and brain: new insights link internal physiology to social behaviour. Commentary on: “anterior insular cortex mediates bodily sensibility and social anxiety” by Terasawa et al. (2012). Soc Cogn Affect Neurosci (2013) 8(3):231–4. 10.1093/scan/nss140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Tsakiris M, Longo MR, Haggard P. Having a body versus moving your body: neural signatures of agency and body-ownership. Neuropsychologia (2010) 48(9):2740–9. 10.1016/j.neuropsychologia.2010.05.021 [DOI] [PubMed] [Google Scholar]
- 131.Slaughter V, Brownell C, editors. Early Development of Body Representations. Cambridge, UK: Cambridge University Press; (2012). [Google Scholar]
- 132.Gallagher S. How the Body Shapes the Mind. Oxford: Oxford University; (2005). [Google Scholar]
- 133.Bechara A, Damasio A. The somatic marker hypothesis: a neural theory of economic decision. Games Econ Behav (2005) 52:336–72. 10.1016/j.geb.2004.06.010 [DOI] [Google Scholar]
- 134.Riva G. Out of my real body: cognitive neuroscience meets eating disorders. Front Hum Neurosci (2014) 8:236. 10.3389/fnhum.2014.00236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Melzack R. Evolution of the neuromatrix theory of pain. The Prithvi Raj Lecture: presented at the Third World Congress of World Institute of Pain, Barcelona 2004. Pain Pract (2005) 5(2):85–94. 10.1111/j.1533-2500.2005.05203.x [DOI] [PubMed] [Google Scholar]
- 136.Wilson M. Covert imitation. In: Knoblich G, Thornton IM, Grosjean M, Shiffrar M, editors. Human Body Perception from the Inside Out. New York: Oxford University Press; (2006). p. 211–28. [Google Scholar]
- 137.Lenggenhager B, Tadi T, Metzinger T, Blanke O. Video ergo sum: manipulating bodily self-consciousness. Science (2007) 317(5841):1096–9. 10.1126/science.1143439 [DOI] [PubMed] [Google Scholar]
- 138.Ehrsson HH. The experimental induction of out-of-body experiences. Science (2007) 5841(317):1048. 10.1126/science.1142175 [DOI] [PubMed] [Google Scholar]
- 139.Bergouignan L, Nyberg L, Ehrsson HH. Out-of-body-induced hippocampal amnesia. Proc Natl Acad Sci U S A (2014) 111(12):4421–6. 10.1073/pnas.1318801111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Olive I, Berthoz A. Combined induction of rubber-hand illusion and out-of-body experiences. Front Psychol (2012) 3:128. 10.3389/fpsyg.2012.00128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Pomes A, Slater M. Drift and ownership toward a distant virtual body. Front Hum Neurosci (2013) 7:908. 10.3389/fnhum.2013.00908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Maselli A, Slater M. Sliding perspectives: dissociating ownership from self-location during full body illusions in virtual reality. Front Hum Neurosci (2014) 8:693. 10.3389/fnhum.2014.00693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Costantini M. Body perception, awareness, and illusions. Wiley Interdiscip Rev Cogn Sci (2014) 5(5):551–60. 10.1002/wcs.1309 [DOI] [PubMed] [Google Scholar]
- 144.Gallace A, Spence C. Outside the boundaries of our bodies: the relationship between touch and the representation of the body in our mind. In: Gallace A, Spence C, editors. In Touch with the Future: The Sense of Touch from Cognitive Neuroscience to Virtual Reality. Oxford: Oxford University Press; (2014). p. 102–24. [Google Scholar]
- 145.Tsakiris M, Haggard P. The rubber hand illusion revisited: visuotactile integration and self-attribution. J Exp Psychol Hum Percept Perform (2005) 31(1):80–91. 10.1037/0096-1523.31.1.80 [DOI] [PubMed] [Google Scholar]
- 146.Perez-Marcos D, Slater M, Sanchez-Vives MV. Inducing a virtual hand ownership illusion through a brain-computer interface. Neuroreport (2009) 20(6):589–94. 10.1097/WNR.0b013e32832a0a2a [DOI] [PubMed] [Google Scholar]
- 147.Slater M, Perez-Marcos D, Ehrsson HH, Sanchez-Vives MV. Inducing illusory ownership of a virtual body. Front Neurosci (2009) 3(2):214–20. 10.3389/neuro.01.029.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Maister L, Slater M, Sanchez-Vives MV, Tsakiris M. Changing bodies changes minds: owning another body affects social cognition. Trends Cogn Sci (2015) 19(1):6–12. 10.1016/j.tics.2014.11.001 [DOI] [PubMed] [Google Scholar]
- 149.Riva G, Banos RM, Botella C, Wiederhold BK, Gaggioli A. Positive technology: using interactive technologies to promote positive functioning. Cyberpsychol Behav Soc Netw (2012) 15(2):69–77. 10.1089/cyber.2011.0139 [DOI] [PubMed] [Google Scholar]
- 150.Waterworth JA, Waterworth EL. Altered, expanded and distributed embodiment: the three stages of interactive presence. In: Riva G, Waterworth JA, Murray D, editors. Interacting with Presence: HCI and the Sense of Presence in Computer-Mediated Environments. Berlin: De Gruyter Open; (2014). p. 36–50. Available from: http://www.presence-research.com [Google Scholar]
- 151.Ginzburg K, Tsur N, Barak-Nahum A, Defrin R. Body awareness: differentiating between sensitivity to and monitoring of bodily signals. J Behav Med (2014) 37(3):564–75. 10.1007/s10865-013-9514-9 [DOI] [PubMed] [Google Scholar]
- 152.Gaggioli A, Pallavicini F, Morganti L, Serino S, Scaratti C, Briguglio M, et al. Experiential virtual scenarios with real-time monitoring (interreality) for the management of psychological stress: a block randomized controlled trial. J Med Internet Res (2014) 16(7):e167. 10.2196/jmir.3235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Repetto C, Gorini A, Algeri D, Vigna C, Gaggioli A, Riva G. The use of biofeedback in clinical virtual reality: the intrepid project. Stud Health Technol Inform (2009) 144:128–32. [PubMed] [Google Scholar]
- 154.Petkova VI, Ehrsson HH. If i were you: perceptual illusion of body swapping. PLoS One (2008) 3(12):e3832. 10.1371/journal.pone.0003832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Serino S, Pedroli E, Keizer A, Triberti S, Dakanalis A, Pallavicini F, et al. Virtual reality body swapping: a tool for modifying the allocentric memory of the body. Cyberpsychol Behav Soc Netw (2016) 19(2):127–33. 10.1089/cyber.2015.0229 [DOI] [PubMed] [Google Scholar]
- 156.Oliveira ECD, Bertrand P, Lesur MER, Palomo P, Demarzo M, Cebolla A, et al., editors. Virtual body swap: a new feasible tool to be explored in health and education. 2016 XVIII Symposium on Virtual and Augmented Reality (SVR). (2016). p. 81–89. [Google Scholar]
- 157.Serino S, Scarpina F, Keizer A, Pedroli E, Dakanalis A, Castelnuovo G, et al. A novel technique for improving bodily experience in a non-operable super-super obesity case. Front Psychol (2016) 7:837. 10.3389/fpsyg.2016.00837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Mezirow J. Learning to think like an adult: core concepts of transformation theory. In: Taylor EW, Cranton P, editors. The Handbook of Transformative Learning: Theory, Research, AND Practice. San Francisco, CA: Jossey-Bass; (2012). p. 73–95. [Google Scholar]
- 159.Riva G, Wiederhold BK, Gaggioli A. Being different. The transfomative potential of virtual reality. Annu Rev Cybertherapy Telemed (2016) 14:1–4. [Google Scholar]