Abstract
Recent developments in sequencing methods and bioinformatics analysis tools have greatly enabled the culture-independent analysis of complex microbial communities associated with environmental samples, plants, and animals. This has led to a spectacular increase in the number of studies on both membership and functionalities of these hitherto invisible worlds, in particular those of the human microbiome. The wide variety in available microbiome tools and platforms can be overwhelming, and making sound conclusions from scientific research can be challenging. Here, I will review 1) the methodological and analytic hoops a good microbiome study has to jump through, including DNA extraction and choice of bioinformatics tools, 2) the hopes this field has generated for diseases such as autism and inflammatory bowel diseases, and 3) some of the hypes that it has created, e.g., by confusing correlation and causation, and the recent pseudoscientific commercialization of microbiome research.
Keywords: microbiome, microbiota, microbial ecology, DNA extraction, sequencing
Introduction
Our bodies are home to complex communities of microbes that live on our skin, in our mouths, and in our guts. These microbial consortia consist of many different bacterial, archaeal, and fungal species, collectively called the human microbiome or microbiota, and are the most dense in the colon [1]. An often-used but now obsolete statement claimed that the human body contains 10 times more microbial cells than human cells. However, a recent paper has revisited these calculations and it is now estimated that the number of bacteria associated with a human body is about the same as human body cells, i.e. 40 trillion [2]. Microbial communities are not exclusively found in humans, however. Almost every plant or animal studied so far has been found to live in close association with microbes. In addition, microbial communities are found in a wide range of environmental niches as well, including soil, seawater, glacier ice, and walls and floors of homes [3-6].
Spectacular advances in amplification and sequencing technologies accomplished in the past 20 years have led to large amounts of new studies of these microbial communities [1]. Many microbial ecology studies rely on the amplification of a marker gene, usually the gene encoding for the structural RNA of the small ribosomal subunit, called the 16S rRNA gene. This gene is present in all living organisms, and consists of a unique mosaic structure including both conserved regions that can be used as the targets of broad-range primers, as well as variable regions that can be used for sequence-based strain typing. Since its first use of a marker gene to investigate bacterial and archaeal phylogeny [7], it has become the gene of choice for the analysis of microbial communities [8-10], with currently over 1.4 million bacterial and 53,000 archaeal sequences available [11]. Amplification of the 16S rRNA gene and the rapid development of high-throughput sequencing platforms have allowed microbiologists to analyze complex microbial communities without the need to culture them. However, this approach is limited by the lack of phylogenetic resolution, especially with short read lengths, and distinct bacterial species or strains often contain nearly identical 16S rRNA gene sequences [12]. In addition to sequencing of marker genes to identify the members of a microbial community, it became technically possible to sequence all genomic DNA within a single sample (“metagenomics”), thus allowing to determine the genetic capacities within a community and to better identify differences between closely related microbial strains [13]. Finally, functional community profiling by transcriptomics, proteomics, and metabolomics is providing us with novel insights into the genes that are being expressed under certain circumstances in a variety of sample types [13].
After many decades of being dependent on culturing techniques to study pathogenic bacteria and viruses, microbiology could shift towards the study of yet unexplored microbial diversity and functionality, allowing novel insights into a hitherto hidden world [14]. Among the many new environments to explore were the microbial populations found in the human mouth [15-18], distal gut [19-21], and skin [22]. It was revealed that human-associated microbial communities varied primarily between anatomical sites, but also per individual and over time [23]. Soon after these first exploratory studies, two large-scale sequence-based human microbiome projects were launched in 2008 to study these consortia in more depth. The European MetaHit consortium focused on the metagenomic analysis of stool samples from 124 subjects with various health conditions, while the United States-based Human Microbiome Project (HMP) analyzed multiple body sits from 242 healthy adults [24,25]. Together, these projects greatly enhanced our knowledge of the constituents, functionalities, and boundaries of variation within the human microbiome.
The combined genomes of the microbes living in the human gut can be viewed as a functional expansion of our own genome, because they add to the variety of enzymes that the human genome does not encode, e.g., for the breakdown of complex polysaccharides. Functions of the human intestinal microbiome include the extraction of energy from food, fermentation of fiber and production of short-chain fatty acids, structuring anatomical features of the distal gut, modulation of the immune system, vitamin synthesis, and occupying niches to prevent pathogens from colonizing [21,24,26,27]. Bidirectional communication routes between the gastrointestinal tract and the central nervous system have led to the postulation of a “brain-gut-axis” mediated by the gut microbiome [28].
Within the same individual, the human gut microbiome is relatively stable over time, but responds rapidly to changes in food, gastrointestinal illness, or travel [29,30]. To further explore the influence of geography, diet, and culture on our gut commensals, recent microbiome studies have analyzed fecal specimens from non-Western human subjects living in traditional communities in Africa and South-America [31-34]. A huge influence of lifestyle and diet on the human gut microbiome was revealed, with hunter-gatherers, traditional agriculturalists, and urban-industrial populations all displaying very different microbiomes with decreasing amounts of bacterial diversity.
A wide variety of diseases have now been found associated with changes in the human microbiome, in particular that of the gut. Many of these associations might be correlations, not causations, with cause and effect often hard to distinguish. However, the ever increasing amount of microbiota studies is creating excitement among the general public with overly optimistic expectations that knowledge of the human-associated microbiome will solve nearly all medical problems. Unfortunately, some of this over-enthusiastic interpretation of data has been found in scientific papers as well, and it is not always easy to separate the wheat from the chaff.
Here, I will review some of the challenges that a good microbiome study will need to overcome, some of the new insights and expectations that this field has generated, as well some examples where microbiome research or the popular press has potentially over-interpreted or exaggerated findings.
Hoops to Jump Through
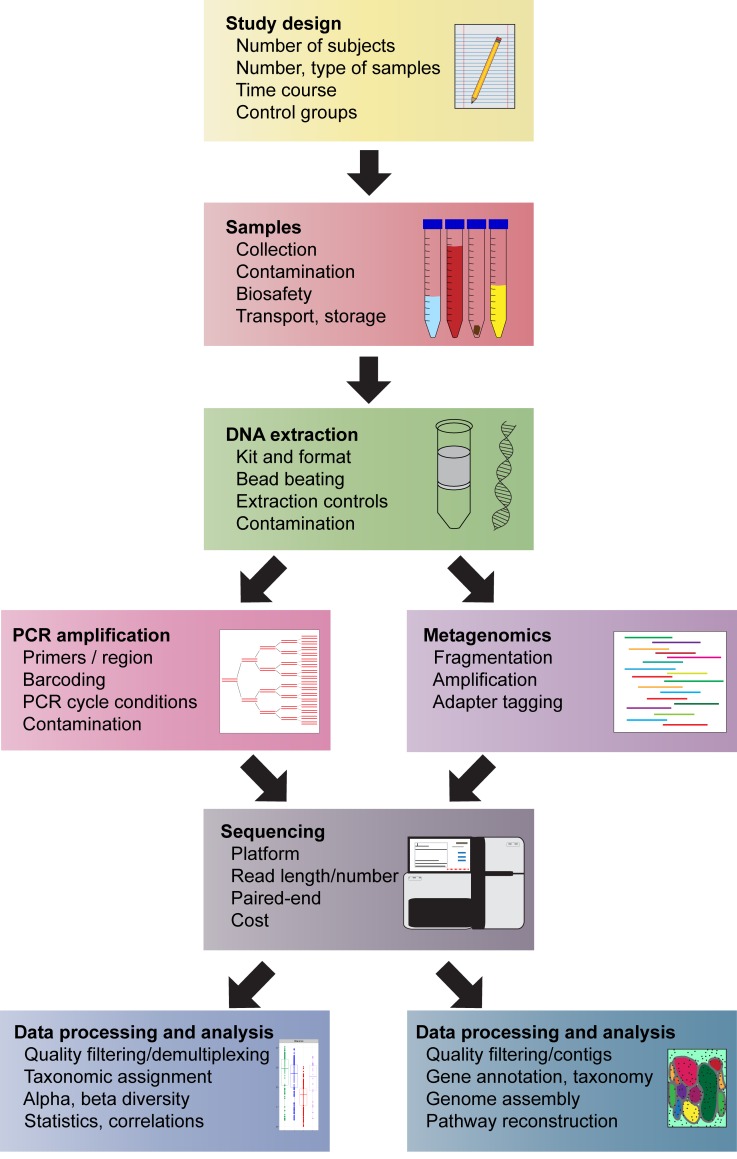
As with any other research study, a microbiome study is most likely to succeed when it is based on a carefully planned study design and smart choices of methods and analysis tools. Each choice with respect to extraction, amplification, sequencing, and ecological analysis can have a profound effect on the outcome of the study, and this is particularly important when comparing new results to previous studies. With so many research groups starting to apply microbiome methods to their own field, and the ever increasing new bioinformatics tools becoming available, it might be difficult and overwhelming to select the best options and parameters. This section will list some of these choices, with a focus on 16S rRNA gene amplification and metagenomics studies (Figure 1). Because this field is so rapidly evolving, the list of choices and parameters is not meant to be comprehensive, but rather a guide to make a new microbiome researcher aware of the range of options that are available.
Figure 1.
General overview of the workflow for 16S rRNA gene-based and metagenomic analysis of microbial communities, showing the most important steps and considerations for each stage of the process.
Study Design
A good microbiome study starts with estimating a useful number of study groups, subjects, and specimens. The type of sample or novelty of the study object will determine how many samples and experimental groups should be included. A low number of samples might be sufficient in the case of a new sample type, such as the indigenous microbial community of a host species or body site that has not previously been analyzed. In those situations, any new information about the microbes associated with those yet unexplored specimen types will offer new insights. In the early days of microbiome research, when many specimen types were yet unexplored, publications included relatively low numbers of samples. For example, a 2005 paper from our laboratory on the distal gut microbiome analyzed six distal gut sites from three healthy humans [19]. In contrast, the HMP project published in 2012 involved 4,788 specimens from 242 adults sampled at 15 to 18 different body sites [24]. Clearly, the publication requirements of studies involving human samples have been raised tremendously. On the other hand, it could currently still be very useful to perform a study on the microbiome of a handful of samples or individuals from a host species or health condition never before analyzed. Given the large variation of individuals found in most animal and plant species, it would always be wise to include more than one individual and sample type.
Given that the human microbiome in health has been extensively studied as of now, and given the high amount of inter-individual variation, most analyses of the human microbiome will require large numbers of samples to reveal underlying patterns of geography or health vs. diseases states. The number of samples per group often cannot be determined a priori and depends on how clearly two different populations differ.
Sampling and Storage
Before the start of the study, microbiome researchers should incorporate in their study design how samples will be collected, by whom and where, and how samples will be transported to the lab and stored. Collection of samples close to the laboratory where the samples will be stored and analyzed ensures short time intervals between collection and freezing. However, human subjects often are more comfortable if they can self-collect, and self-sampling can be simple and as effective as sampling by a physician [35]. Collection at home brings challenges in terms of transport to the laboratory, which can be hindered by distance, outside temperature, and transport regulations. For example, microbial communities from fecal samples stored for three days at room temperature differ significantly from fresh samples or those stored at -80°C or at 4°C [36]. The optimal choice of sampling must find the best balance between all of these considerations. For most applications and sample types, immediate freezing and storage at -80°C is optimal to preserve the microbial composition within the sample [36].
DNA Extraction
A third consideration of a microbiome study is the quality of the nucleic acids extracted from the specimens. A wide range of DNA extraction kits are available on the market, combining premade buffers, materials, and protocols for the disruption of cellular membranes, denaturation of proteins, and purification of nucleic acids thus ensuring reproducibility and reliability. Many of these commercial methods contain similar components such as guanidine-based chaotropic salts and silica-adsorption spin-columns, but kits might vary in the composition of the buffers and enzymes used for cell lysis and whether mechanical lysis steps such as bead-beating are incorporated or not. The QIAamp (Qiagen, Valencia, CA) and PowerSoil (MO BIO Laboratories, Carlsbad, CA) DNA extraction kits are currently among the most popular choices for microbiome analysis applications. Depending on the type of specimen to be extracted, the choice of nucleic acid extraction kit might have a considerable effect on both the yield as well as the bacterial ratios in the purified sample [37-40].
As long as all samples within a single study are processed with the same nucleic acid extraction technique, the choice of extraction method should not be too much cause of concern. However, problems might arise when results obtained with different types of extraction procedures are compared to each other, because the observed variation in bacterial communities might be driven by the DNA extraction method, not by a true underlying difference. However, particular sample types, e.g. containing hard-to-remove inhibitors, might benefit from an in-house developed specific extraction protocol
Contamination
An important point to address is the possible introduction of contaminating DNA during sample preparation. Contamination might occur during several stages of the sample processing by cross-contamination from adjacent samples, the operator, or the presence of amplicon residues in the laboratory. Important measures to reduce these types of contamination are the use of biosafety cabinets, gloves, filter tips, and separate areas for DNA extraction and PCR [41]. In addition, several studies have reported the presence of low amounts of contaminant DNA in sample collection materials such as paper points used for the collection of oral samples [42], DNA extraction buffers or columns [43,44], or PCR reagents [45], a problem that is much harder to avoid. The concern for contamination becomes increasingly important when extracting or amplifying low-yield clinical samples, such as blood, where the signal-to-noise ratio is low. In an elegant study, Salter et al. showed that most DNA extraction reagents contain non-negligible amounts of contaminating DNA that could progressively be more detected in samples with a low amount of microbial biomass [46]. An increasing number of studies attempt to detect microbial DNA in near-sterile environments such as amniotic fluid or blood from healthy individuals. Without the inclusion of carefully selected extraction and amplification controls, the interpretation of the results of such studies becomes very difficult.
DNA Amplification Primers and Parameters
Although metagenomics studies are on the rise, many microbiome analyses still rely on the amplification of the 16S rRNA gene, by using PCR primers that fit on conserved regions of this mosaic gene, and sequencing on the interposed variable regions. The choice of primer pairs and thus of the variable regions to be amplified and analyzed is partly dictated by the read length of the selected sequencing platform (also see discussion below). For example, nearly the entire length of the 1.5 kb 16S rRNA gene can be analyzed by paired-end 800-nt reads obtained with classical Sanger sequencing, while the shorter read length of newer high-throughput sequencing platforms is better suitable for amplification of only one to three variable regions. Amplification of the V4 variable region in combination with Illumina sequencing is currently a popular and solid choice.
Despite the presence of multiple conserved regions within the 16S rRNA gene and a multiple published “universal” PCR primer sequences, no primer combination will be perfect. Most primers need to contain degeneracies in order to amplify a wide range of bacterial taxa, and no matter which primer pairs or ambiguities are chosen, the amplification ratios of the different bacterial groups present in the original sample will be biased [47,48]. In addition to this bias in taxonomic coverage, the choice of the variable region will influence how well certain bacterial taxa can be distinguished from each other [47,48].
The PCR cycle number is worth some consideration too. Cycle numbers that are too high will lead to increased risk of chimera formation, and older datasets contain many chimeras [49]. Depending on the expected amount of target DNA in the sample, keeping the cycle number below 30 is recommended [49].
Sequencing Technology
DNA sequencing has undergone dramatic changes in the past decade. A wide variety of established and recently developed high-throughput technologies is currently available, and choice of the appropriate sequence platform needs to take into account read length, read yield, error rate, number of samples, and cost. The first microbiome studies were based on Sanger sequencing, which yields long and high-quality reads that were very valuable in precise phylogenetic and taxonomic assignments [10]. However, this methodology was cumbersome and costly, limiting its use to analyze complex microbial communities.
The development of high-throughput sequencing platforms has quickly revolutionized the study of microbial communities, both for amplicon based sequencing as well as for metagenomic analysis [50,51]. The first technique that became commonly used was 454 pyrosequencing, but its usefulness for taxonomic purposes is hindered by its high error rate of ~1 percent, and support for this platform has stopped in 2013. Illumina-based sequencing platforms provide much lower error rates and higher read numbers than pyrosequencing, and have proven to be extremely effective and successful for high-throughput microbial community analysis. Even newer sequencing technologies have entered the microbial ecology field and are rapidly winning terrain, such as the Ion Torrent, PacBio, and the MinIon sequence platforms [50,52,53]; it is still unclear which of these will become the most popular. Each technology generates a different balance between output, read length, and error rate, making it hard to compare datasets generated with multiple platforms [47,54].
Bioinformatics
The newer sequencing platforms generate millions of reads which are impossible to process and analyze without the use of bioinformatics tools. Several packages are available for both marker as well as shotgun reads.
For the processing and analysis of amplified 16S rRNA gene reads, the current most commonly used packages are mothur [55] and QIIME [56]. Each tool comes with a wide range of options and parameters that are not always reported in published studies, making these choices difficult to make for non-experienced users. Quality of the alignment, distance calculation methods, sequence filtering and many other parameters all have significant impacts on community structure outcomes, suggesting that extreme caution must be taken when comparing results from different labs [57].
An even wider selection of bioinformatics tools for the assembly and analysis of metagenomic shotgun reads are available. In general, better results are expected when short reads are first assembled into larger contigs, allowing better taxonomic and functional assessments of the microbial communities. In some cases, nearly complete genomes can be assembled [51,58,59]. The choices of tools and parameters in metagenomics analysis are even more overwhelming and less standardized than with marker gene data. Metagenomic analysis involves a large number of specific steps, such as contig assembly, taxonomic and functional assignment, pathway reconstruction, and genome assembly, and specialized laboratories might use in-house developed algorithms and pipelines that are not easy to implement for other researchers. Some commonly used metagenomic analysis tools include MetaPhlAn2 [60] and HUMAnN [61], both developed by the Huttenhower laboratory.
Finally, there is a whole range of tools developed for data not based on DNA sequencing, such as transcriptomics, proteomics, and metabolomics, that provide measures for the functional activity with a microbial community [13]. In contrast to DNA-based studies, which can only detect the potential for biochemical pathways, such studies provide new insights into the genes that are actively being expressed and the community proteins and other compounds that are synthesized under specific circumstances [13].
Hopes for the Best
The novel world that opened up for scientists after the first human microbiome studies were published has offered many new insights in the members and functions of our indigenous communities, as well as hopes that this new scientific knowledge could be applied for diagnostics tests or ways to modulate our microbiota to cure diseases. Indeed, the human microbiome field has generated several success stories and hopes for future treatment options, some of which are highlighted here.
Effect of Diet
Not surprisingly, the composition of the gut microbiome is in part determined by what we eat. As noted above, although the human gut microbiome is relatively stable over time within the same individual, it will respond quickly to dietary changes [29,30]. Studies on non-Western human stool samples have shown that the gut communities from hunter-gatherers and traditional agriculturalists contain many more bacterial species than those from urban dwellers. It has been proposed that the different microbial consortia are a reflection of different amounts of fiber consumed by their hosts, and that the typical Western diet low in fiber and high in simple carbohydrates might be associated with a “loss” of microbial diversity [31-33]. This hypothesis has been strengthened by animal experiments, in which mice fed a low fiber diet for several generations showed a progressive loss of gut microbiota diversity [62]. These new insights might help evolve therapeutic strategies to increase the microbial diversity in Western guts and possibly decrease metabolic diseases such as obesity and diabetes, both of which are associated with decreased diversity of the gut microbiome [63,64]. Promising treatment options include the consumption of more fiber and less simple carbohydrates in our food, and the addition of probiotic supplements (food items containing live organisms with a postulated positive effect on our health) [65].
Effect of Antibiotics
One of the most compelling findings of the microbiome field are the damaging effects of antibiotics on the human gut microbiome. Antibiotics used to treat an infection elsewhere in the body can also generate “collateral damage” on the distal gut communities, despite any lack of noticeable side effects by the patient. In volunteer studies, a single course of antibiotics rapidly changes and decreases the number of bacterial species in stool communities, often followed by incomplete recovery even after several months [66,67]. The mouth microbiome however, is much more resilient to these changes, possibly because of the pharmacokinetics of antibiotics [67]. These results, together with those from animal experiments, have led to the hypothesis that multiple perturbations by antibiotic use early in life might lead to adult gut microbiotas that contain fewer bacterial species than those of subjects who have never had antibiotics [68]. The prevalent use of antibiotics in children and the putative resulting decreased microbial diversity might be related to the increased prevalence of diseases such as obesity and diabetes [68]. These associations could lead to new treatment or prevention options for these morbidities, e.g., by the use of probiotics after antibiotic use, as well as reduced use of antibiotics for the treatment of non-life-threatening infections or in the food industry [68].
Clostridium difficile Infections and Stool Transplants
Related to new insights in the effects of antibiotics on the human gut microbiome are the success stories of treating Clostridium difficile infections (CDI). Treatment of patients with antibiotics is the main risk factor for CDI, which is characterized by diarrhea and fever [69]. C. difficile is a spore-forming and toxin-producing bacterium that is present in low numbers in the gut microbiota of about 10 percent of the healthy population, where it causes no apparent problems [70]. However, antibiotic use – which kills off many other bacterial species in the gut – can lead to a disturbance of this balance and to a higher relative abundance of this bacterium [71]. Cases of CDI are difficult to treat, and recurrent infections often occur. The burden of CDI is very high, with almost half a million cases and 30,000 deaths per year in the United States [72]. Fecal microbiota transplantation (FMT), in which a stool sample from a healthy donor is transplanted into the intestinal tract of a recipient, has proven to be very successful in CDI cases, with cure rates over 85 percent and very few complications [73,74]. The high success rate of FMT for CDI has created high expectations for the application of this technique to other gastrointestinal diseases.
Inflammatory Bowel Diseases
Inflammatory bowel diseases (IBD) include both Crohn’s Disease and Ulcerative Colitis, the etiology of which are still poorly understood. Several studies have reported a decreased overall bacterial diversity of the intestinal microbiota in IBD, as well as changes in the abundance of specific bacterial groups [75,76]. However, it remains unclear whether this dysbiosis is the cause of the disease, or the result of the prolonged disease pathology or medications or dietary modifications that are commonly found in IBD patients. Although IBD are unlikely caused by a single microbial pathogen, and are more likely to be triggered by a complex combination of genetics, microbiota disturbances, and immune defects, restoring the microbial diversity of the gut has been proposed as an interesting new therapy. Despite variable success rates so far (30 to 60 percent in a series of trials reviewed in [77]), both probiotic supplements as well as FMT are currently being considered to treat IBD [75].
Autism
Autism spectrum disorders (ASD) are another family of conditions where the expectations with regards to microbiome research are high, although actual treatment options have been lacking so far. Autistic children have more gastrointestinal problems such as constipation and diarrhea than healthy controls [78]. Recent studies on the stool microbiota of ASD patients have reported conflicting findings with respect to stool samples from healthy controls with different studies reporting distinct increased or decreased microbial groups [28,79]. In addition, altered gut microbial communities in ASD children might be related to the behavioral problems found in these patients, which are often accompanied by strong food preferences for e.g. starchy, processed foods [78]. The diets of ASD patients therefore might lack certain nutrients which could be correlated to changes in their gut microbial communities [78]. Although the relationship between the gut microbiome and disease is still unclear, prebiotics, probiotics, and FMT are gaining popularity as therapy options in ASD [79].
Pregnancy and Birth
The birth of every child marks the beginning of a new symbiosis between microbes and human. Microbial ecology research has greatly improved our knowledge on how babies are colonized [80,81], and the important roles of mode of delivery and feeding [82-84]. Babies born by cesarean section or fed with sterile formula might follow a perturbed path of microbial colonization [85]. This has led to recent practices where newborns delivered by cesarean section are “seeded” with the vaginal microbiome of their mother [86]. In addition to the effect of delivery mode or feeding practices, the presence of pets or siblings in their household and the composition of their family’s gut microbiomes all play significant roles on the development of a child’s microbiome [87]. Interestingly, growing up with dogs or farm animals decreases a child’s risk to develop asthma [88], which fits into the “hygiene hypothesis” which proposes that exposure to many microbes early in live is needed to properly educate the immune system and make it more tolerant to environmental antigens [89].
Microbiome research has provided new insights in the complex processes preceding birth as well. Vaginal microbiomes cluster into several community types [90], in which Lactobacillus-dominated microbiotas are associated with health, while another, more diverse community type with fewer lactic acid bacteria is associated with bacterial vaginosis and poorer pregnancy outcomes [91,92]. Modulation of the vaginal microbiome by probiotics or other therapeutics is currently being investigated as treatment options for bacterial vaginosis [93].
Hypes to Bust
It is clear that studies on the human-associated microbial communities have generated large amounts of new data and interesting findings, but many of the high expectations expressed around the launch of the HMP and Metahit studies have not yet come true. We cannot clearly define a healthy microbiome yet; there is too much variation between the gut microbiomes of people living on different diets or in different populations all around the world. In addition, microbiome research has brought us better understanding but yet no clear cause or cure for complex gastrointestinal or other disorders such as IBD, autism, or multiple sclerosis. Not withstanding this relative lack of therapeutic or diagnostic applications, many scientists in non-microbiology medical fields such as neurology, psychology, and dermatology have started to incorporate and execute microbiome studies to their own specialties in the hopes to find cures for hard-to-treat or diagnose diseases.
Disturbingly, the recent large amounts of microbiome articles by popular science media and general news outlets have generated feelings of exaggerated excitement among the public which is led to believe that the microbiome is connected to all human organs and diseases. Many of these proposed connections are interesting hypotheses some of which might turn out to be correct, but most of these hypes are not, or only poorly, founded by scientific findings. This section will review some causes and concerning effects of these hypes.
Correlation is not Causation
Altered microbiomes have been reported in a wide variety of health conditions, including IBD [75,76], autism [28,79], and anorexia nervosa [94,95]. However, correlation does not mean causation. It can often not be determined whether differences in the microbiome are causing the disease, or if they are caused by the disease. For example, many people with gastrointestinal diseases such as IBD have been on various medications and might have excluded certain food components, and people with anorexia nervosa have decreased caloric intake than healthy controls; these confounding factors could have caused the reported changes in microbial communities. Similarly, it has been reported that rugby players have a different, more diverse, microbiome than age-matched controls [96]. This was interpreted both by the authors as well as by the popular press as proof that exercise has a beneficial impact on the gut microbiome diversity. However, several other confounding factors, such as different diets for these athletes or more contact with soil, could have caused the microbial changes as well. In these examples, and many other studies, correlations of a certain health condition to changes in the microbiome should not be interpreted as causal relationships without further evidence to support those claims.
Animals are not Humans
Without doubt, animal models such as germ-free (GF) mice, born and raised in sterile laboratory environments, have proven invaluable for microbiome research. They have shown the importance of intestinal microorganisms for development of a correctly structured gut lining, immune system, and important roles in gut-brain signaling [97]. Colonization of GF animals with simple communities of specific microorganisms or human-derived microbiota have brought new insights on how bacterial strains co-exist and communicate with each other [98,99], and spectacular images of the spatial organization of the murine gut microbiota [100]. However, results obtained in mouse or other animal models have to be interpreted with caution. Mice and humans are quite different with respect to body sizes, diet, gut anatomy and functions [101]. Findings from a mouse model therefore are not necessarily applicable to humans. In addition, several animal models of human digestive tract diseases such as colitis, obesity, or diabetes are only superficially related to their human counterparts. Although the symptoms of these animal model diseases might ostensibly resemble the human equivalent, their origin or development is quite different. Some of these models have underlying genetic mutations not corresponding to human genes, while in others the disease is artificially induced with chemical treatment. Any findings of altered microbial communities or effects of treatments must be viewed in this light, and might not simply transfer to human physiology [101].
Microbial Detection is not the Same as a Microbiome
Another area where experimental findings could easily be over-interpreted is the analysis of microbial communities found at anatomical sites that are traditionally thought to be sterile or near-sterile in health, such as blood, amniotic fluid, placenta, or urine. Infections of these specimen types are often associated with detectable bacterial counts, either by culture or by amplification of a marker gene, [102-104]. However, stories about “rich” microbiomes in these types of samples in health without clinical evidence of infection or any other underlying disease are harder to accept, especially if they are not accompanied by adequate numbers of thoughtfully planned extraction controls. These reports on the presence of microorganisms in previously believed to be sterile sites might be correct, but could also represent detection of circulating non-viable lysed microbial cell remnants or transient bacteremia, e.g., after dental flossing [105]. Alternatively, as discussed above, some of these communities might reflect contaminants introduced during specimen sampling, DNA extraction, or amplification [46]. No matter what scenario, interpreting these low-abundance and possibly transient microorganisms as evidence for a microbiome appears farfetched. A true microbiome is more than a random selection of detectable microbes; it refers to the combined microorganisms adapted to live within a particular environment.
However, there are several examples of studies on low-yield specimen types that carefully considered contamination or the presence of transient microbial DNA. Most of these provided additional proof of the presence and viability of these microorganisms, such as traditional cultivation, adenosine triphosphate and propidium monoazide PCR assays, or microscopy with fluorescent probes to estimate viable microbial populations [106-108]. Without such controls, reports on rich microbiomes at unlikely anatomical sites need to be interpreted with caution.
Microbes are Unlikely to Determine our Partner Choice
Recent claims in the popular media have stated that our microbes can determine our behavior, including choosing a partner. Statements like these are often based on extreme extrapolations of scientific findings. For example, there are several examples from the animal world in which particular microbes can modify behavior or influence mate choice, as reviewed in [109]. A study in humans showed that the composition of the oral microbiome can be shaped by kissing [110], but there is no scientific evidence yet that microbes determine with whom we kiss.
Commercialization of the Microbiome
An area of recent concern is the commercialization of human microbiome research. As written above, the human microbiome has been implicated in a wide range of human health issues, and our diets have been shown to have an immediate effect on the microbial composition of our gut [30]. The idea that our microbiome can be modulated through food has created a whole new branch within the “functional foods” industry. Unfortunately, dietary supplements are poorly regulated in most countries. Many of these products such as yogurts or fermented drinks with live bacteria are sold in supermarkets but vary widely in manufacturing processes, amount of microorganisms, quality control, and proven success [111]. In addition, there has been a recent surge of pseudoscientific websites run by self-proclaimed “microbiome experts”, often without professional education or scientific background, who promote overpriced probiotic or fiber-rich food items or wellness books and videos. Some of these also cater to patients suffering from chronic conditions, raising several ethical and legal concerns [111].
Conclusions and Outlook
The invisible world that opened up to microbiologists after the introduction of culture-independent microbial community analysis and high-throughput sequencing tools has offered novel insights into the members and functions of our bodies’ indigenous communities, as well as hopes that this new scientific knowledge can be applied for diagnostics tests or ways to modulate our microbiota and cure diseases. So far we have learned that the microbiome is an important and intricate part of our physiology which appears to be disturbed in a wide range of disease conditions. Our gut microbiota fares best on a diet rich in vegetables and fiber, and can possibly be enhanced with probiotics and fermented foods. In some instances, microbiome studies have led to treatment options, e.g. FMT in CDI, while there is still much to learn for many others conditions.
The hopes generated around 2010 when the first HMP and MetaHit papers were published are reminiscent of the excitement expressed when the first draft of the human genome was released in 2001. The sequencing of the human genome was viewed as a huge step in the advancement of clinical medicine [112], generating high expectations for the treatment of diseases with a genetic origin and novel insights into basic human physiology. However, the authors recognized that the human genome project was not more than another step in the continuing research of human genetics, and only the start of many new projects, noting “(T)he more we learn about the human genome, the more there is to explore.” [112]. Similarly, the datasets generated on the human microbiome are only the start of our understanding which microbes we are host to, the functions of these consortia, and how small variations are associated with geographical differences, diet, or health status.
Glossary
- ASD
Autism spectrum disorders
- CDI
Clostridium difficile infections
- FMT
fecal microbiome transplantation
- HMP
Human Microbiome Project
- IBD
Inflammatory Bowel Diseases
- PCR
polymerase chain reaction
- rRNA
ribosomal RNA
References
- Grice EA, Segre JA. The human microbiome: our second genome. Annu Rev Genomics Hum Genet. 2012;13:151–170. doi: 10.1146/annurev-genom-090711-163814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sender R, Fuchs S, Milo R. Are We Really Vastly Outnumbered? Revisiting the Ratio of Bacterial to Host Cells in Humans. Cell. 2016;164(3):337–340. doi: 10.1016/j.cell.2016.01.013. [DOI] [PubMed] [Google Scholar]
- Sunagawa S, Coelho LP, Chaffron S. et al. Ocean plankton. Structure and function of the global ocean microbiome. Science. 2015;348(6237):1261359. doi: 10.1126/science.1261359. [DOI] [PubMed] [Google Scholar]
- Choudhari S, Smith S, Owens S. et al. Metagenome sequencing of prokaryotic microbiota collected from Byron Glacier, Alaska. Genome Announc. 2013;1(2):e0009913. doi: 10.1128/genomeA.00099-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz-Calderon JF, Cavallin H, Song SJ. et al. Walls talk: Microbial biogeography of homes spanning urbanization. Science Advances. 2016;2(2):e1501061. doi: 10.1126/sciadv.1501061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramirez KS, Leff JW, Barberán A. et al. Biogeographic patterns in below-ground diversity in New York City’s Central Park are similar to those observed globally. Proc Biol Sci. 2014;281(1795) doi: 10.1098/rspb.2014.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woese CR, Fox GE. Phylogenetic structure of the prokaryotic domain: the primary kingdoms. Proc Natl Acad Sci U S A. 1977;74(11):5088–5090. doi: 10.1073/pnas.74.11.5088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woese CR, Kandler O, Wheelis ML. Towards a natural system of organisms: proposal for the domains Archaea, Bacteria, and Eucarya. Proc Natl Acad Sci U S A. 1990;87(12):4576–4579. doi: 10.1073/pnas.87.12.4576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace NR. A molecular view of microbial diversity and the biosphere. Science. 1997;276(5313):734–740. doi: 10.1126/science.276.5313.734. [DOI] [PubMed] [Google Scholar]
- Amann RI, Ludwig W, Schleifer KH. Phylogenetic identification and in situ detection of individual microbial cells without cultivation. Microbiol Rev. 1995;59(1):143–169. doi: 10.1128/mr.59.1.143-169.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schloss PD, Girard RA, Martin T. et al. Status of the Archaeal and Bacterial Census: an Update. MBio. 2016;7(3) doi: 10.1128/mBio.00201-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poretsky R, Rodriguez-R LM, Luo C. et al. Strengths and limitations of 16S rRNA gene amplicon sequencing in revealing temporal microbial community dynamics. PLoS One. 2014;9(4):e93827. doi: 10.1371/journal.pone.0093827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franzosa EA, Hsu T, Sirota-Madi A. et al. Sequencing and beyond: integrating molecular “omics” for microbial community profiling. Nat Rev Microbiol. 2015;13(6):360–372. doi: 10.1038/nrmicro3451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schloss PD, Handelsman J. Status of the microbial census. Microbiol Mol Biol Rev. 2004;68(4):686–691. doi: 10.1128/MMBR.68.4.686-691.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroes I, Lepp PW, Relman DA. Bacterial diversity within the human subgingival crevice. Proc Natl Acad Sci U S A. 1999;96(25):14547–14552. doi: 10.1073/pnas.96.25.14547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paster BJ, Boches SK, Galvin JL. et al. Bacterial diversity in human subgingival plaque. J Bacteriol. 2001;183(12):3770–3783. doi: 10.1128/JB.183.12.3770-3783.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bik EM, Long CD, Armitage GC. et al. Bacterial diversity in the oral cavity of 10 healthy individuals. ISME J. 2010;4(8):962–974. doi: 10.1038/ismej.2010.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aas JA, Paster BJ, Stokes LN. et al. Defining the normal bacterial flora of the oral cavity. J Clin Microbiol. 2005;43(11):5721–5732. doi: 10.1128/JCM.43.11.5721-5732.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckburg PB, Bik EM, Bernstein CN. et al. Diversity of the human intestinal microbial flora. Science. 2005;308(5728):1635–1638. doi: 10.1126/science.1110591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turnbaugh PJ, Hamady M, Yatsunenko T. et al. A core gut microbiome in obese and lean twins. Nature. 2009;457(7228):480–484. doi: 10.1038/nature07540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill SR, Pop M, Deboy RT. et al. Metagenomic analysis of the human distal gut microbiome. Science. 2006;312(5778):1355–1359. doi: 10.1126/science.1124234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grice EA, Kong HH, Conlan S. et al. Topographical and temporal diversity of the human skin microbiome. Science. 2009;324(5931):1190–1192. doi: 10.1126/science.1171700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EK, Lauber CL, Hamady M. et al. Bacterial community variation in human body habitats across space and time. Science. 2009;326(5960):1694–1697. doi: 10.1126/science.1177486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Human Microbiome Project Consortium. Structure, function and diversity of the healthy human microbiome. Nature. 2012;486(7402):207–214. doi: 10.1038/nature11234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin J, Li R, Raes J. et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature. 2010;464(7285):59–65. doi: 10.1038/nature08821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kau AL, Ahern PP, Griffin NW. et al. Human nutrition, the gut microbiome and the immune system. Nature. 2011;474(7351):327–336. doi: 10.1038/nature10213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bik EM. Composition and function of the human-associated microbiota. Nutr Rev. 2009;67(2):S164–S171. doi: 10.1111/j.1753-4887.2009.00237.x. [DOI] [PubMed] [Google Scholar]
- O’Mahony SM, Stilling RM, Dinan TG. et al. The microbiome and childhood diseases: Focus on brain-gut axis. Birth Defects Res C Embryo Today. 2015;105(4):296–313. doi: 10.1002/bdrc.21118. [DOI] [PubMed] [Google Scholar]
- David LA, Materna AC, Friedman J. et al. Host lifestyle affects human microbiota on daily timescales. Genome Biol. 2014;15(7):R89. doi: 10.1186/gb-2014-15-7-r89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David LA, Maurice CF, Carmody RN. et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505(7484):559–563. doi: 10.1038/nature12820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnorr SL, Candela M, Rampelli S. et al. Gut microbiome of the Hadza hunter-gatherers. Nat Commun. 2014;5:3654. doi: 10.1038/ncomms4654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez A, Petrzelkova KJ, Burns MB. et al. Gut Microbiome of Coexisting BaAka Pygmies and Bantu Reflects Gradients of Traditional Subsistence Patterns. Cell Rep. 2016;14(9):2142–2153. doi: 10.1016/j.celrep.2016.02.013. [DOI] [PubMed] [Google Scholar]
- Obregon-Tito AJ, Tito RY, Metcalf J. et al. Subsistence strategies in traditional societies distinguish gut microbiomes. Nat Commun. 2015;6:6505. doi: 10.1038/ncomms7505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yatsunenko T, Rey FE, Manary MJ. et al. Human gut microbiome viewed across age and geography. Nature. 2012;486(7402):222–227. doi: 10.1038/nature11053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forney LJ, Gajer P, Williams CJ. et al. Comparison of self-collected and physician-collected vaginal swabs for microbiome analysis. J Clin Microbiol. 2010;48(5):1741–1748. doi: 10.1128/JCM.01710-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choo JM, Leong LE, Rogers GB. Sample storage conditions significantly influence faecal microbiome profiles. Sci Rep. 2015;5:16350. doi: 10.1038/srep16350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesolowska-Andersen A, Bahl MI, Carvalho V. et al. Choice of bacterial DNA extraction method from fecal material influences community structure as evaluated by metagenomic analysis. Microbiome. 2014;2:19. doi: 10.1186/2049-2618-2-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner Mackenzie B, Waite DW, Taylor MW. et al. Evaluating variation in human gut microbiota profiles due to DNA extraction method and inter-subject differences. Front Microbiol. 2015;6:130. doi: 10.3389/fmicb.2015.00130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wüst PK, Nacke H, Kaiser K. et al. Estimates of the bacterial ribosome content and diversity in soils are significantly affected by different nucleic acid extraction methods. Appl Environ Microbiol. 2016;82(9):2595–2607. doi: 10.1128/AEM.00019-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burbach K, Seifert J, Pieper DH. et al. Evaluation of DNA extraction kits and phylogenetic diversity of the porcine gastrointestinal tract based on Illumina sequencing of two hypervariable regions. Microbiologyopen. 2015;5(1):70–82. doi: 10.1002/mbo3.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheils OM, Finn S, O’Leary JJ. et al. Quality-control issues for PCR-based assays in the molecular laboratory. Current diagnostic pathology. 2003;9(3):165–172. [Google Scholar]
- Van der Horst J, Buijs MJ, Laine ML. et al. Sterile paper points as a bacterial DNA-contamination source in microbiome profiles of clinical samples. J Dent. 2013;41(12):1297–1301. doi: 10.1016/j.jdent.2013.10.008. [DOI] [PubMed] [Google Scholar]
- Van der Zee A, Peeters M, de Jong C. et al. Qiagen DNA extraction kits for sample preparation for legionella PCR are not suitable for diagnostic purposes. J Clin Microbiol. 2002;40(3):1126. doi: 10.1128/JCM.40.3.1126.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naccache SN, Greninger AL, Lee D. et al. The perils of pathogen discovery: origin of a novel parvovirus-like hybrid genome traced to nucleic acid extraction spin columns. J Virol. 2013;87(22):11966–11977. doi: 10.1128/JVI.02323-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilburg JJ, Nabuurs-Franssen MH, van Hannen EJ. et al. Contamination of commercial PCR master mix with DNA from Coxiella burnetii. J Clin Microbiol. 2010;48(12):4634–4635. doi: 10.1128/JCM.00464-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salter SJ, Cox MJ, Turek EM. et al. Reagent and laboratory contamination can critically impact sequence-based microbiome analyses. BMC Biol. 2014;12:87. doi: 10.1186/s12915-014-0087-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremblay J, Singh K, Fern A. et al. Primer and platform effects on 16S rRNA tag sequencing. Front Microbiol. 2015;6:771. doi: 10.3389/fmicb.2015.00771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczynski J, Lauber CL, Walters WA. et al. Experimental and analytical tools for studying the human microbiome. Nat Rev Genet. 2012;13(1):47–58. doi: 10.1038/nrg3129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashelford KE, Chuzhanova NA, Fry JC. et al. New screening software shows that most recent large 16S rRNA gene clone libraries contain chimeras. Appl Environ Microbiol. 2006;72(9):5734–5741. doi: 10.1128/AEM.00556-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuter JA, Spacek DV, Snyder MP. High-throughput sequencing technologies. Mol Cell. 2015;58(4):586–597. doi: 10.1016/j.molcel.2015.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oulas A, Pavloudi C, Polymenakou P. et al. Metagenomics: tools and insights for analyzing next-generation sequencing data derived from biodiversity studies. Bioinform Biol Insights. 2015;9:75–88. doi: 10.4137/BBI.S12462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loman NJ, Constantinidou C, Chan JZ. et al. High-throughput bacterial genome sequencing: an embarrassment of choice, a world of opportunity. Nat Rev Microbiol. 2012;10(9):599–606. doi: 10.1038/nrmicro2850. [DOI] [PubMed] [Google Scholar]
- Di Bella JM, Bao Y, Gloor GB. et al. High throughput sequencing methods and analysis for microbiome research. J Microbiol Methods. 2013;95(3):401–414. doi: 10.1016/j.mimet.2013.08.011. [DOI] [PubMed] [Google Scholar]
- Salipante SJ, Kawashima T, Rosenthal C. et al. Performance comparison of Illumina and ion torrent next-generation sequencing platforms for 16S rRNA-based bacterial community profiling. Appl Environ Microbiol. 2014;80(24):7583–7591. doi: 10.1128/AEM.02206-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schloss PD, Westcott SL, Ryabin T. et al. Introducing mothur: open-source, platform-independent, community-supported software for describing and comparing microbial communities. Appl Environ Microbiol. 2009;75(23):7537–7541. doi: 10.1128/AEM.01541-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caporaso JG, Kuczynski J, Stombaugh J. et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. 2010;7(5):335–336. doi: 10.1038/nmeth.f.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schloss PD. The effects of alignment quality, distance calculation method, sequence filtering, and region on the analysis of 16S rRNA gene-based studies. PLoS Comput Biol. 2010;6(7):e1000844. doi: 10.1371/journal.pcbi.1000844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharon I, Morowitz MJ, Thomas BC. et al. Time series community genomics analysis reveals rapid shifts in bacterial species, strains, and phage during infant gut colonization. Genome Res. 2013;23(1):111–120. doi: 10.1101/gr.142315.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharpton TJ. An introduction to the analysis of shotgun metagenomic data. Front Plant Sci. 2014;5:209. doi: 10.3389/fpls.2014.00209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truong DT, Franzosa EA, Tickle TL. et al. MetaPhlAn2 for enhanced metagenomic taxonomic profiling. Nat Methods. 2015;12(10):902–903. doi: 10.1038/nmeth.3589. [DOI] [PubMed] [Google Scholar]
- Abubucker S, Segata N, Goll J. et al. Metabolic reconstruction for metagenomic data and its application to the human microbiome. PLoS Comput Biol. 2012;8(6):e1002358. doi: 10.1371/journal.pcbi.1002358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonnenburg ED, Smits SA, Tikhonov M. et al. Diet-induced extinctions in the gut microbiota compound over generations. Nature. 2016;529(7585):212–215. doi: 10.1038/nature16504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kostic AD, Gevers D, Siljander J. et al. The dynamics of the human infant gut microbiome in development and in progression toward type 1 diabetes. Cell Host Microbe. 2015;17(2):260–273. doi: 10.1016/j.chom.2015.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Chatelier E, Nielsen T, Qin J. et al. Richness of human gut microbiome correlates with metabolic markers. Nature. 2013;500(7464):541–546. doi: 10.1038/nature12506. [DOI] [PubMed] [Google Scholar]
- Patterson E, Ryan PM, Cryan JF. et al. Gut microbiota, obesity and diabetes. Postgrad Med J. 2016;92(1087):286–300. doi: 10.1136/postgradmedj-2015-133285. [DOI] [PubMed] [Google Scholar]
- Dethlefsen L, Relman DA. Incomplete recovery and individualized responses of the human distal gut microbiota to repeated antibiotic perturbation. Proc Natl Acad Sci U S A. 2011;108(1):4554–4561. doi: 10.1073/pnas.1000087107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaura E, Brandt BW, Teixeira de Mattos MJ. et al. ame Exposure but Two Radically Different Responses to Antibiotics: Resilience of the Salivary Microbiome versus Long-Term Microbial Shifts in Feces. MBio. 2015;6(6):e01693. doi: 10.1128/mBio.01693-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox LM, Blaser MJ. Antibiotics in early life and obesity. Nat Rev Endocrinol. 2015;11(3):182–190. doi: 10.1038/nrendo.2014.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassetti M, Villa G, Pecori D. et al. Epidemiology, diagnosis and treatment of Clostridium difficile infection. Expert Rev Anti Infect Ther. 2012;10(12):1405–1423. doi: 10.1586/eri.12.135. [DOI] [PubMed] [Google Scholar]
- Galdys AL, Nelson JS, Shutt KA. et al. Prevalence and duration of asymptomatic Clostridium difficile carriage among healthy subjects in Pittsburgh, Pennsylvania. J Clin Microbiol. 2014;52(7):2406–2409. doi: 10.1128/JCM.00222-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert AM, Rogers MA, Ring C. et al. Microbiome data distinguish patients with Clostridium difficile infection and non-C. difficile-associated diarrhea from healthy controls. MBio. 2014;5(3):e01021. doi: 10.1128/mBio.01021-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leffler DA, Lamont JT. Clostridium difficile infection. N Engl J Med. 2015;372(16):1539–1548. doi: 10.1056/NEJMra1403772. [DOI] [PubMed] [Google Scholar]
- Drekonja D, Reich J, Gezahegn S. et al. Fecal Microbiota Transplantation for Clostridium difficile Infection: A Systematic Review. Ann Intern Med. 2015;162(9):630–638. doi: 10.7326/M14-2693. [DOI] [PubMed] [Google Scholar]
- Van Nood E, Vrieze A, Nieuwdorp M. et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013;368(5):407–415. doi: 10.1056/NEJMoa1205037. [DOI] [PubMed] [Google Scholar]
- Kostic AD, Xavier RJ, Gevers D. et al. The microbiome in inflammatory bowel disease: current status and the future ahead. Gastroenterology. 2014;146(6):1489–1499. doi: 10.1053/j.gastro.2014.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalal SR, Chang EB. The microbial basis of inflammatory bowel diseases. J Clin Invest. 2014:1–7. doi: 10.1172/JCI72330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moayyedi P. Fecal transplantation: any real hope for inflammatory bowel disease? Curr Opin Gastroenterol. 2016;32(4):282–286. doi: 10.1097/MOG.0000000000000285. [DOI] [PubMed] [Google Scholar]
- McElhanon BO, McCracken C, Karpen S. et al. Gastrointestinal symptoms in autism spectrum disorder: a meta-analysis. Pediatrics. 2014;133(5):872–883. doi: 10.1542/peds.2013-3995. [DOI] [PubMed] [Google Scholar]
- Rosenfeld CS. Microbiome Disturbances and Autism Spectrum Disorders. Drug Metab Dispos. 2015;43(10):1557–1571. doi: 10.1124/dmd.115.063826. [DOI] [PubMed] [Google Scholar]
- Palmer C, Bik EM, DiGiulio DB. et al. Development of the human infant intestinal microbiota. PLoS Biol. 2007;5(7):e177. doi: 10.1371/journal.pbio.0050177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig JE, Spor A, Scalfone N. et al. Succession of microbial consortia in the developing infant gut microbiome. Proc Natl Acad Sci U S A. 2011;108(1):4578–4585. doi: 10.1073/pnas.1000081107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez JM, Murphy K, Stanton C. et al. The composition of the gut microbiota throughout life, with an emphasis on early life. Microb Ecol Health Dis. 2015;26:26050. doi: 10.3402/mehd.v26.26050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker WA, Iyengar RS. Breast milk, microbiota, and intestinal immune homeostasis. Pediatr Res. 2015;77(1-2):220–228. doi: 10.1038/pr.2014.160. [DOI] [PubMed] [Google Scholar]
- Dominguez-Bello MG, Costello EK, Contreras M. et al. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc Natl Acad Sci U S A. 2010;107(26):11971–11975. doi: 10.1073/pnas.1002601107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller NT, Bakacs E, Combellick J. et al. The infant microbiome development: mom matters. Trends Mol Med. 2015;21(2):109–117. doi: 10.1016/j.molmed.2014.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dominguez-Bello MG, De Jesus-Laboy KM, Shen N. et al. Partial restoration of the microbiota of cesarean-born infants via vaginal microbial transfer. Nat Med. 2016;22(3):250–253. doi: 10.1038/nm.4039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song SJ, Lauber C, Costello EK. et al. Cohabiting family members share microbiota with one another and with their dogs. elife. 2013;2:e00458. doi: 10.7554/eLife.00458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fall T, Lundholm C, Örtqvist AK. et al. Early Exposure to Dogs and Farm Animals and the Risk of Childhood Asthma. JAMA Pediatr. 2015;169(11):e153219. doi: 10.1001/jamapediatrics.2015.3219. [DOI] [PubMed] [Google Scholar]
- Brown EM, Arrieta MC, Finlay BB. et al. A fresh look at the hygiene hypothesis: how intestinal microbial exposure drives immune effector responses in atopic disease. Semin Immunol. 2013;25(5):378–387. doi: 10.1016/j.smim.2013.09.003. [DOI] [PubMed] [Google Scholar]
- Ravel J, Gajer P, Abdo Z. et al. Vaginal microbiome of reproductive-age women. Proc Natl Acad Sci U S A. 2011;108(1):4680–4687. doi: 10.1073/pnas.1002611107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romero R, Hassan SS, Gajer P. et al. The composition and stability of the vaginal microbiota of normal pregnant women is different from that of non-pregnant women. Microbiome. 2014;2(1):4. doi: 10.1186/2049-2618-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiGiulio DB, Callahan BJ, McMurdie PJ. et al. Temporal and spatial variation of the human microbiota during pregnancy. Proc Natl Acad Sci U S A. 2015;112(35):11060–11065. doi: 10.1073/pnas.1502875112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machado D, Castro J, Palmeira-de-Oliveira A. et al. Bacterial Vaginosis Biofilms: Challenges to Current Therapies and Emerging Solutions. Front Microbiol. 2015;6:1528. doi: 10.3389/fmicb.2015.01528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morita C, Tsuji J, Hata T. et al. Gut Dysbiosis in Patients with Anorexia Nervosa. PLoS One. 2015;10(12):e0145274. doi: 10.1371/journal.pone.0145274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiman SC, Watson HJ, Bulik-Sullivan EC. et al. The Intestinal Microbiota in Acute Anorexia Nervosa and During Renourishment: Relationship to Depression, Anxiety, and Eating Disorder Psychopathology. Psychosom Med. 2015;77(9):969–981. doi: 10.1097/PSY.0000000000000247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke SF, Murphy EF, O’Sullivan O. et al. Exercise and associated dietary extremes impact on gut microbial diversity. Gut. 2014;63(12):1913–1920. doi: 10.1136/gutjnl-2013-306541. [DOI] [PubMed] [Google Scholar]
- Luczynski P, McVey Neufeld KA, Seira Oriach C. et al. Growing up in a Bubble: Using Germ-Free Animals to Assess the Influence of the Gut Microbiota on Brain and Behaviour. Int J Neuropsychopharmacol. 2016;19(8) doi: 10.1093/ijnp/pyw020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macpherson AJ, McCoy KD. Standardised animal models of host microbial mutualism. Mucosal Immunol. 2014;8(3):476–486. doi: 10.1038/mi.2014.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz JV, Desai MS, Shah P. et al. From meta-omics to causality: experimental models for human microbiome research. Microbiome. 2013;1(1):14. doi: 10.1186/2049-2618-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earle KA, Billings G, Sigal M. et al. Quantitative Imaging of Gut Microbiota Spatial Organization. Cell Host Microbe. 2015;18(4):478–488. doi: 10.1016/j.chom.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen TL, Vieira-Silva S, Liston A. et al. How informative is the mouse for human gut microbiota research? Dis Model Mech. 2015;8(1):1–16. doi: 10.1242/dmm.017400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiGiulio DB, Romero R, Amogan HP. et al. Microbial prevalence, diversity and abundance in amniotic fluid during preterm labor: a molecular and culture-based investigation. PLoS One. 2008;3(8):e3056. doi: 10.1371/journal.pone.0003056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su G, Fu Z, Hu L. et al. 16S Ribosomal Ribonucleic Acid Gene Polymerase Chain Reaction in the Diagnosis of Bloodstream Infections: A Systematic Review and Meta-Analysis. PLoS One. 2015;10(5):e0127195. doi: 10.1371/journal.pone.0127195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nickel JC, Stephens A, Landis JR. et al. Assessment of the Lower Urinary Tract Microbiota during Symptom Flare in Women with Urologic Chronic Pelvic Pain Syndrome: A MAPP Network Study. J Urol. 2016;195(2):356–362. doi: 10.1016/j.juro.2015.09.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crasta K, Daly CG, Mitchell D. et al. Bacteraemia due to dental flossing. J Clin Periodontol. 209;36(4):323–362. doi: 10.1111/j.1600-051X.2008.01372.x. [DOI] [PubMed] [Google Scholar]
- Checinska A, Probst AJ, Vaishampayan P. et al. Microbiomes of the dust particles collected from the International Space Station and Spacecraft Assembly Facilities. Microbiome. 2015;3:50. doi: 10.1186/s40168-015-0116-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatt AS, Freeman SS, Herrera AF. et al. Sequence-based discovery of Bradyrhizobium enterica in cord colitis syndrome. N Engl J Med. 2013;369(6):517–528. doi: 10.1056/NEJMoa1211115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo SC, Hung GC, Li B. et al. Mixed group of Rhizobiales microbes in lung and blood of a patient with fatal pulmonary illness. Int J Clin Exp Pathol. 2015;8(11):13834–13852. [PMC free article] [PubMed] [Google Scholar]
- Sampson TR, Mazmanian SK. Control of brain development, function, and behavior by the microbiome. Cell Host Microbe. 2015;17(5):565–576. doi: 10.1016/j.chom.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kort R, Caspers M, van de Graaf A. et al. Shaping the oral microbiota through intimate kissing. Microbiome. 2014;2:41. doi: 10.1186/2049-2618-2-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slashinski MJ, McCurdy SA, Achenbaum LS. et al. “Snake-oil,” “quack medicine,” and “industrially cultured organisms:” biovalue and the commercialization of human microbiome research. BMC Med Ethics. 2012;13:38. doi: 10.1186/1472-6939-13-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lander ES, Linton LM, Birren B. et al. Initial sequencing and analysis of the human genome. Nature. 2001;409(6822):860–921. doi: 10.1038/35057062. [DOI] [PubMed] [Google Scholar]