Abstract
Background:
Between November 2011 and November 2012, an Inuit village in Nunavik, Quebec experienced a surge in the occurrence of active TB; contact investigations showed that TB infection was highly prevalent (62.6%), particularly among those over age 14 years (78.8%). A nested case-control study showed that nutritional inadequacy was associated with acquisition of infection but not progression to disease. We performed a study to determine whether characteristics of one's dwelling were associated with 1) acquisition of newly diagnosed TB infection and 2) progression to confirmed or probable disease among those with TB infection.
Methods:
In this nested case-control study, we enrolled 200 people who were household or social contacts of at least 1 person with active TB or had received a diagnosis of active TB and assessed whether characteristics of their dwellings were associated with their odds of having newly diagnosed TB infection and/or odds of progression to disease between November 2011 and November 2012. For our first objective, we compared participants with newly diagnosed TB infection (regardless of their disease status) to a control group of contacts who were uninfected. For the second objective, we compared participants with confirmed or probable disease to a control group consisting of those with infection but no disease. We used information collected during investigation of the contacts and from study questionnaires to determine whether participants may have been exposed to TB in their own home (if they had shared a dwelling with someone who had smear-positive TB during the outbreak) or in other dwellings that they visited at least weekly.
Results:
The participants lived in 79 dwellings. The mean number of people per room was 1.1 (standard deviation [SD] 0.5). The mean room size and ventilation level of the common living space (kitchen and living/dining rooms) were 67.9 (SD 9.4) m3 and 1.69 (SD 0.26) air changes per hour, respectively. After adjustment for potential confounders, the number of people per room was positively associated with the odds of newly diagnosed infection and odds of disease, but only among participants who lived with someone with smear-positive TB (the minority of participants). Other dwelling characteristics were not associated with either outcome.
Interpretation:
Reducing household crowding may contribute to TB prevention. Overall, our investigations have not identified associations that explain the elevated disease risk in this village. In light of our results and considering the high prevalence of TB infection, treatment of latent infection is an essential intervention for long-term reduction of TB incidence in this village.
During the period 2008-2012, the average annual tuberculosis (TB) incidence among Canadian Inuit was 190 per 100 000, compared with the national average of 5 per 100 000.1-5 The reasons for this dramatic difference are unclear, although major disparities in socioeconomic status6 and general health7,8 are thought to contribute.
Housing has been a concern for Inuit communities for several years owing to the high prevalence of overcrowding and disrepair of dwellings.9,10 Although housing is widely regarded as an important determinant of TB,11,12 there is surprisingly little evidence supporting a causal association between housing conditions and TB infection or disease. Associations between crowded housing and TB have mostly been reported in ecologic studies,13-15 but these community-level associations may have been due to confounding by other social, environmental or biological determinants of TB that are often coprevalent with crowded households. An association between low ventilation - the exchange of indoor air with outdoor air - and the risk of TB infection has been shown in health care settings,16 but its role in TB transmission in homes has not been established.
Between November 2011 and November 2012, an Inuit village in Nunavik, Quebec experienced a surge in the occurrence of active TB.17 Culture-confirmed TB was diagnosed in 5.4% of the village's 933 inhabitants and clinically probable TB disease in another 2.0%. As part of an intensified medical and public health response, 695 villagers were evaluated for TB infection or disease during this period. Our study was motivated by 2 observations: the elevated rate of newly diagnosed TB infection among villagers evaluated as contacts during this period (27.0%) and the high rate of active disease in this group (28.2%). Although similar rates of TB disease have been reported in outbreaks of multidrug-resistant strains18 and among people with HIV,19 neither of these were contributing factors in this village.
By November 2012, TB notifications had returned to baseline; hence, we planned an intensive investigation of the association between demographic, economic, housing, dietary and lifestyle factors and the acquisition of infection or development of disease that had occurred during the period of elevated incidence. In parallel, whole-genome sequencing of all isolates from culture-positive cases showed that the surge in incidence was not related to the introduction of a new strain or the emergence of a more transmissable or virulent organism.17 Sequencing also showed that the surge had resulted from the contemporaneous occurrence of at least 6 independent reactivation events with multiple chains of transmission rather than a single point-source outbreak.17 A detailed evaluation of dietary and lifestyle factors identified inadequate intake of fruits, vegetables and carbohydrates as nutritional factors associated with infection.20 These variables were not associated with disease.
This paper focuses on the relation between TB outcomes and housing characteristics. Our 2 main objectives were to determine whether characteristics of one's dwelling were associated with 1) acquisition of newly diagnosed TB infection and 2) progression to confirmed or probable disease among those with TB infection.
Methods
Between November 2011 and November 2012, 695 of the village's 933 inhabitants were identified as a household or social contact of at least 1 person with active TB or had received a diagnosis of active TB.17,20 The evaluation of these 695 people has been previously reported in detail.17,20 It included tuberculin skin testing (TST) performed and interpreted per the Canadian Tuberculosis Standards,21 in those who did not have a documented prior positive TST result. All those in whom TB disease was suspected on the basis of radiographic or clinical findings submitted 3 spontaneous or induced sputum samples, which were sent for acid-fast microscopic examination, liquid culture and nucleic acid amplification testing. As the village has little in-migration, 1 clinic and a single public health authority, villagers' medical records provided complete information on lifelong past investigations for TB infection or disease.
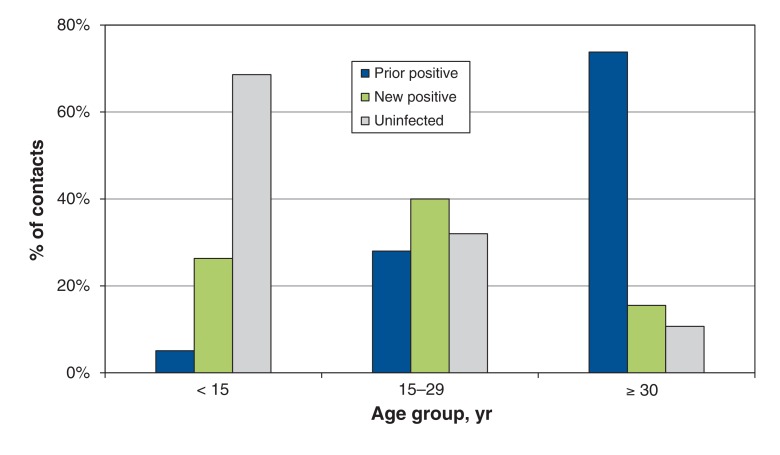
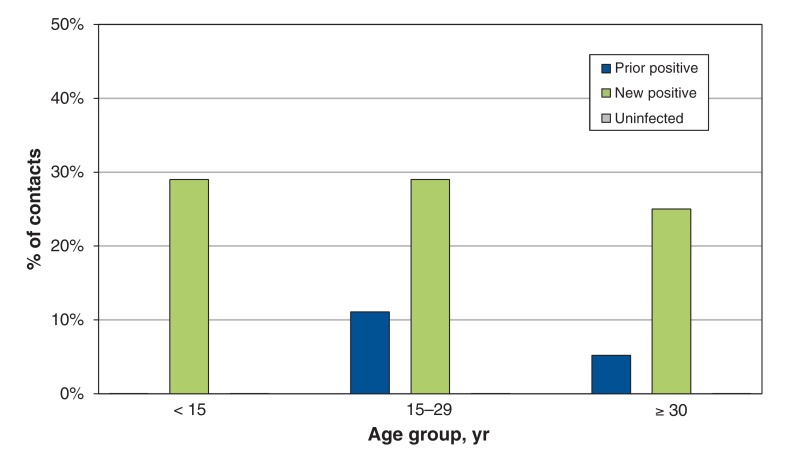
By November 2012, of the 695 people investigated, 92 (13.2%) had been treated for active TB. Of the 695, 50 (7.2%) had culture-confirmed disease, and 19 (2.7%) had clinically probable disease (defined below); 23 people (3.3%) treated during the outbreak were later considered to not have had active TB. There were no cases of confirmed or clinically probable TB among villagers with a negative TST result. Of the 695 people investigated, 247 (35.5%) had been documented as having a positive TST result before November 2011, and 188 (27.0%) were documented to have a new positive TST result or TST conversion between November 2011 and November 2012 (Figure 1). The prevalence of infection was 89.3% (208/233) among those aged 30 years or more, 67.8% (152/224) among those 15-29 years old and 31.6% (75/237) among those under 15 years. Across all age groups, the rate of disease was highest among newly infected contacts (Figure 2). All TST and treatment for TB disease or latent infection were performed according to Canadian standards.21 By November 2012, among contacts who were not treated for active TB, treatment for latent infection had been started in 89.6% (121/135) of those with a new positive TST result or TST conversion.
Figure 1.
Proportion of contacts (n = 695) investigated between November 2011 and November 2012 who were uninfected, newly infected or previously infected with tuberculosis (TB). "Prior positive" and "new positive" categories include contacts with disease and contacts in whom disease did not develop between November 2011 and November 2012. Confirmed or probable TB disease did not develop in any contact with a negative result of tuberculin skin testing.
Figure 2.
Proportion of contacts in whom microbiologically confirmed or probable active tubercular disease developed, by tuberculin skin test status and age group.
Study definitions
Based on detailed clinical information collected between November 2011 and November 2012, we grouped all investigated contacts into one of 3 categories: those with newly diagnosed TB infection, defined as a new positive TST result or TST conversion; those with a prior positive TST result, defined as a positive TST result documented before November 2011; and those who were uninfected, defined as at least 1 negative TST result between November 2011 and November 2012, with no prior positive TST result and no TB disease. We categorized villagers treated for active TB as having confirmed TB disease if they had at least 1 positive culture for Mycobacterium tuberculosis, or probable TB disease if there were typical clinical and radiological features, including response to therapy, but without culture confirmation. This designation was made by 2 experienced chest physicians, who independently reviewed all clinical and radiological information.
Design
We conducted a case-control study nested within the 695 people who were identified and investigated between November 2011 and November 2012. The study was carried out between February and July 2013. For our first objective, we compared participants with newly diagnosed TB infection (regardless of their disease status) to a control group of contacts who were uninfected. For the second objective, we compared participants with confirmed or probable disease to a control group consisting of those with infection but no disease.
People were eligible for inclusion if, between November 2011 and November 2012, they had resided in the village and had received a diagnosis of confirmed or probable TB disease, or they had been investigated as contacts of a villager with confirmed or probable disease (at least 1 TST performed during this period or documented prior positive TST result).
For the first objective, we aimed to recruit people with newly diagnosed infection to serve as cases and an equal number of uninfected people to serve as control subjects. For the second objective, we planned to recruit as many people with confirmed or probable active TB as possible, and aimed to recruit twice as many people without disease but with TB infection to serve as control subjects.
Sources of data
The online supplement (Appendix 1, available at www.cmajopen.ca/content/4/3/E496/suppl/DC1) provides details about questionnaires, definitions of socioeconomic variables and housing characteristics, the methods for measuring and extrapolating ventilation levels and our approach to multivariate analyses.
Trained study staff administered questionnaires assessing housing, nutrition, socioeconomic and lifestyle factors.20 Parents or guardians provided responses for children aged up to 12 years. Informed consent was obtained from each participant or the parent/guardian before the questionnaires were administered. For the housing assessment, consent was obtained from the individual identified as the head of the household.
We used information collected during investigation of the contacts and from the study questionnaires to determine whether participants may have been exposed to TB in their own home (if they had shared a dwelling with someone who had smear-positive TB during the outbreak) or in other dwellings that they visited at least weekly. Community members had raised concerns that people were at greater risk for contracting TB if they had visited a subset of dwellings that had been used for social activities. To address these concerns, we specifically evaluated whether visiting these dwellings at least once weekly was associated with each study outcome.
The dwelling of each participant was visited by study personnel to administer questionnaires and perform a standardized walk-through assessment (for enumerating rooms and assessing need for major repairs). The kitchen, living/dining area and bedrooms were counted as rooms.22
We measured ventilation in air changes per hour in the rooms where participants slept and in the common living area (living, dining and kitchen area, which were contiguous in all dwellings) using carbon dioxide as a tracer gas.23,24 In dwellings with forced-air heating systems, which blow heated outdoor air into rooms, measurements were taken with the heating both on and off. Because the design and construction of many dwellings were identical (dwellings in this community are grouped into 5 main construction types that share the same design and layout), ventilation was not directly measured in all dwellings of the same type. Rather, these were assigned the weighted average air changes per hour measured in dwellings of the same construction model and layout; we estimated these average values using multilevel linear regression (Appendix 1).
To determine the occupancy level (i.e., "crowdedness") that each participant had been exposed to between November 2011 and November 2012, we used a list created for the public health response that enumerated each of the village's dwellings and its occupants during the period of the outbreak. We divided the total number of occupants by the number of rooms in each dwelling to obtain our measure of occupancy, number of people per room. We defined "overcrowding" as more than 1 person per room in the dwelling.22
Statistical analysis
The level of analysis was the individual. We used the method of generalized estimating equations for logistic regression, with clustering at the dwelling level, to identify associations between each outcome of interest and housing characteristics, potential TB exposures in dwellings and factors recognized as important determinants of TB (e.g., smoking tobacco). To analyze ventilation as a risk factor for TB, we used the ventilation level in the common living area of participants' dwellings, given that all household occupants shared these areas and many slept in these areas. We used interaction terms to test the hypothesis that occupancy level would be associated with TB transmission in dwellings where someone with smear-positive TB lived. Because our results supported this hypothesis, we used the same approach to analyze the impact of occupancy on disease. Additional details are found in Appendix 1. The multivariate models in this report do not adjust for measures of nutritional inadequacy; a detailed evaluation of nutritional factors is reported elsewhere.20
The study was approved by the Nunavik Nutrition and Health Committee, the mayor and municipal council of the village and the Institutional Review Board of McGill University.
Results
Study population
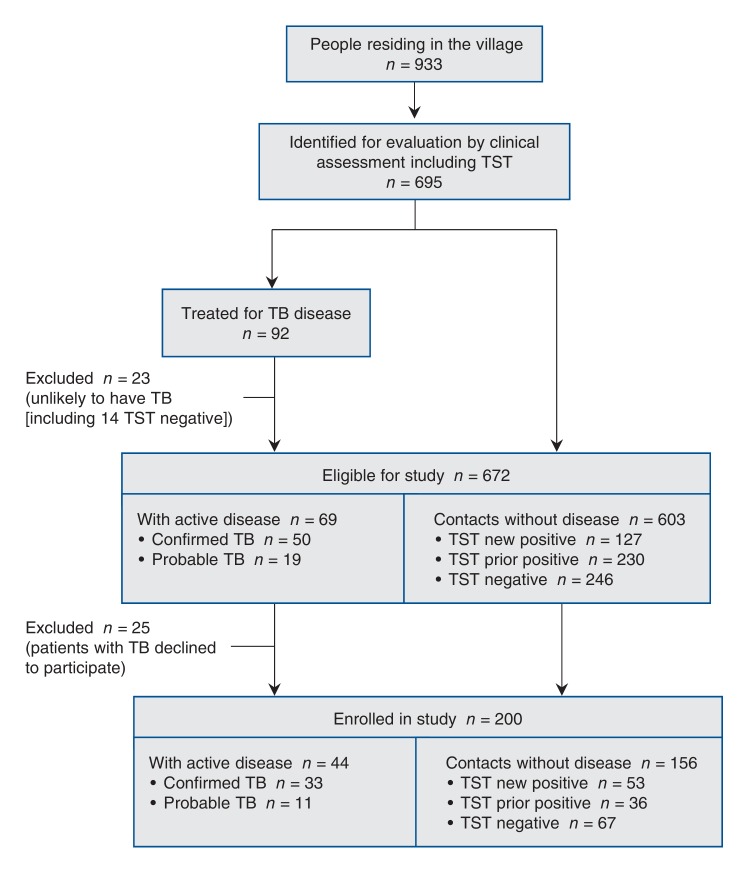
Details about enrolment and comparisons between participants and nonparticipants have been previously reported.20 Of the 695 eligible villagers, 200 were enrolled in the study (Figure 3). Within each TST category, age and sex distributions were similar among participants and nonparticipants (Table S1, Appendix 1). Similarly, among villagers with confirmed or probable TB, participants and nonparticipants had similar age and sex distributions as well as proportions in each TST category (Table S1, part B, Appendix 1).
Figure 3.
Selection of study participants. Screening comprised chest radiography, clinical assessment and tuberculin skin testing (TST) to determine disease and infection status. TB = tuberculosis. Adapted from Fox and colleagues20 with permission of the American Thoracic Society. Copyright © 2016 American Thoracic Society.
Of the 200 villagers enrolled, 67 (33.5%) were uninfected, 88 (44.0%) had newly diagnosed TB infection, and 45 (22.5%) had a prior positive TST result (Figure 3). Among the 133 participants with TB infection, 44/200 (22.0%) had confirmed (33) or probable (11) TB disease, and 89/200 (44.5%) had TB infection with no disease. The mean age of the participants was 21.5 (standard deviation 14.1) years, 107 (53.5%) were female, 118 (59.0%) were current smokers, and 118 (59.0%) had an annual personal income less than $20 000 (for participants under 18 years of age, this was the income of their parent or guardian).
Housing characteristics
The characteristics of 78 of the 79 dwellings where the 200 participants resided between November 2011 and November 2012 are shown in Table 1. We could not determine the characteristics for 1 dwelling because the participant had moved before the study and research staff could not gain access to the residence. The 78 dwellings accounted for 40% of all dwellings in the village. Five dwellings were studio apartments without separate bedrooms. Most dwellings used forced-air heating systems; in these dwellings, air changes per hour were higher when the heating was on.
Table 1: Characteristics of the 78 dwellings where study participants lived between November 2011 and November 2012.
| Characteristic | Mean ± SD* |
|---|---|
| Years since dwelling was built | 19.3 ± 8.2 |
| Heating method, no. (%) | |
| Forced air | 70 (90) |
| Radiator | 8 (10) |
| Dwelling occupancy | |
| No. of occupants | 6.1 ± 3.0 |
| No. of people per room† | 1.1 ± 0.5 |
| Overcrowded,‡ no. (%) | 39 (50) |
| Ventilation | |
| Air changes per hour | |
| With heating off | |
| Living area | 0.67 ± 0.28 |
| Bedrooms | 0.31 ± 0.28 |
| With heating on | |
| Living area | 1.69 ± 0.26 |
| Bedrooms | 1.29 ± 0.29 |
| Volume of room, m3 | |
| Living area | 67.9 ± 9.4 |
| Bedrooms | 27.7 ± 4.4 |
Note: SD = standard deviation.
*Except where noted otherwise.
†Calculated by dividing the number of occupants by the total number of rooms in the dwelling.
‡Occupancy exceeding 1 person per room.22
Community members identified 18 dwellings that had been used for social activities. These dwellings' characteristics were similar to those of the other 178 dwellings in the village (Table S2, Appendix 1).
Determinants of newly diagnosed TB infection
In univariate analyses, participants with newly diagnosed TB infection were significantly more likely than uninfected participants to have visited at least once weekly a dwelling that was used for social activities (Table 2). Newly infected participants were also more likely than uninfected participants to have lived in a dwelling with someone who had smear-positive TB.
Table 2: Associations between acquisition of TB infection and potential exposure to villagers with active TB when visiting other dwellings or at home.
| Variable | No. (%) of participants | p value† | |
|---|---|---|---|
| Newly infected* (n = 88) | Uninfected (n = 67) | ||
| No. of participants who visited at least once weekly ≥ 1 dwelling | 84 (95) | 64 (96) | 1.0 |
| No. of participants who visited at least once weekly dwelling that was not used for social activities (178 dwellings) | |||
| Any of these dwellings | 77 (88) | 63 (94) | 0.17 |
| Dwelling where villager with TB disease lived or visited | 53 (60) | 49 (73) | 0.09 |
| No. of participants who visited at least once weekly dwelling used for social activities (18 dwellings) | |||
| Any of these dwellings | 47 (53) | 16 (24) | < 0.01 |
| Dwelling where villager with TB disease lived or visited | 34 (39) | 11 (16) | < 0.01 |
| No. of participants who lived with someone with TB | |||
| Lived with someone with TB disease | 42 (48) | 26 (39) | 0.34 |
| Lived with someone with smear-positive TB | 20 (23) | 2 (3) | < 0.01 |
| Lived with someone with smear-negative TB | 36 (41) | 25 (37) | 0.77 |
Note: TB = tuberculosis.
*Included 53 people without disease and 35 people with disease.
†Pearson's χ2 test or Fisher's exact test.
The method of heating, level of ventilation and volume of the living area were not associated with infection and did not meet the criteria for inclusion in multivariate analyses (Table 3). Age greater than 14 years and visiting at least once weekly dwellings used for social activities were associated with newly diagnosed infection. The effect of occupancy on infection was dependent on living with someone with smear-positive TB: among participants who had lived with someone with smear-positive TB, the odds of newly diagnosed infection increased as the number of people per room increased (Table 3); this association was not seen among those who had not lived with someone with smear-positive TB. This interaction also meant that the association between living with someone with smear-positive TB and infection was stronger in dwellings with more people per room (the odds ratio for this association corresponds to living in a dwelling with 1.2 people per room, the median value for this variable).
Table 3: Factors associated with acquisition of TB infection between November 2011 and November 2012.
| Variable† | No. (%) of participants* | Crude OR (95% CI)‡ | Adjusted OR (95% CI)‡§ | |
|---|---|---|---|---|
| Newly infected(n = 88) | Uninfected (n = 67) | |||
| Age, yr | ||||
| < 15 | 30 (34) | 45 (67) | Reference | Reference |
| 15-29 | 44 (50) | 17 (25) | 3.9 (2.1-7.1) | 5.5 (2.8-10.7) |
| ≥ 30 | 14 (16) | 5 (8) | 4.2 (1.5-12.0) | 5.2 (1.5-18.0) |
| Sex | ||||
| Male | 40 (45) | 31 (46) | Reference | Reference |
| Female | 48 (54) | 36 (54) | 1.0 (0.6-1.9) | 0.8 (0.4-1.8) |
| Tobacco smoking | ||||
| Not current smoker | 30 (34) | 40 (60) | Reference | Not in model |
| Current smoker | 58 (66) | 27 (40) | 2.9 (1.5-5.4) | |
| Annual personal income, $ | ||||
| < 20 000 | 55 (66) | 36 (56) | Reference | Not in model |
| ≥ 20 000 | 28 (34) | 28 (44) | 0.7 (0.3-1.5) | |
| Heating method | ||||
| Forced air | 81 (92) | 64 (97) | Reference | Not in model |
| Radiator | 7 (8) | 2 (3) | 2.8 (0.8-10.2) | |
| No. of people per room,¶ mean ± SD | ||||
| Among participants living with smear-positive person | 1.7 ± 0.6 | 1.1 ± 0.7 | 1.5 (0.9-2.3) | 1.8 (1.1-2.9) |
| Among participants not living with smear-positive person | 1.2 ± 0.5 | 1.3 ± 0.4 | 0.9 (0.7-1.1) | 0.9 (0.7-1.1) |
| Ventilation with heating on relative to median (1.66 air changes per hour)** | ||||
| < Median | 68 (77) | 51 (76) | Reference | Not in model |
| ≥ Median | 20 (23) | 15 (22) | 1.0 (0.4-2.6) | |
| Volume of living area relative to median (65.5 m3) | ||||
| < Median | 32 (36) | 31 (47) | Reference | Not in model |
| ≥ Median | 56 (64) | 35 (53) | 1.6 (0.7-3.6) | |
| Visited dwelling used for social activities | 47 (53) | 16 (24) | 3.7 (1.7-7.9) | 4.2 (1.8-10.1) |
| Lived with smear-positive person†† | 20 (23) | 2 (3) | 9.6 (2.4-38.0) | 4.7 (0.95-23.2) |
Note: CI = confidence interval, OR = odds ratio, SD = standard deviation, TB = tuberculosis.
*Except where noted otherwise. One participant who had moved after the outbreak and whose dwelling could not be accessed was excluded from multivariate analysis.
†Data missing on income (n = 8), heating type (n = 1), ventilation (n = 1) and volume of living area (n = 1).
‡CIs where OR excludes 1.0 are in bold.
§Final multivariate model included all listed variables, except where indicated, plus an interaction term between occupancy and living with a smear-positive person that was statistically significant (p = 0.006).
¶Interaction term between occupancy and living with a smear-positive person was significant in univariate analysis (p < 0.05). The crude and adjusted ORs are per 0.2-unit increment in the number of people per room. This scale was chosen because it corresponds to an increment of 1 occupant in a dwelling with 5 rooms (the median number of rooms). As an example of interpretation: among those living with a smear-positive person in a dwelling with 5 rooms, if we were to compare 2 participants who did not live together and whose dwellings differed in occupancy by 1 person, the unadjusted odds of newly diagnosed infection would be 50% higher (as the OD is 1.5) for the participant living in the home with the greater number of people per room.
**In the living area. Lowest ventilation measured in the living area was also not associated with infection (data not shown).
††Adjusted OR shows association between living with someone with smear-positive TB and newly diagnosed infection if living in a dwelling with 1.2 persons per room (chosen because it was the median number of people per room).
Determinants of TB disease among participants with TB infection
In univariate analyses among participants with TB infection, active TB was not associated with visiting dwellings used for social activities or with having lived with someone with TB disease (Table 4).
Table 4: Association between active TB disease among participants with TB infection and potential exposure to villagers with active TB when visiting other dwellings or at home.
| Variable | No. (%) of participants | p value | |
|---|---|---|---|
| Disease (n = 44) | No disease (n = 89) | ||
| No. of participants who visited at least once weekly ≥ 1 dwelling | 41 (93) | 83 (93) | 0.37 |
| No. of participants who visited at least once weekly dwelling that was not used for social activities (178 dwellings) | |||
| Any of these dwellings | 37 (84) | 80 (90) | 0.33 |
| Dwelling where villager with TB disease lived or visited | 27 (61) | 55 (62) | 0.96 |
| No. of participants who visited at least once weekly dwelling used for social activities (18 dwellings) | |||
| Any of these dwellings | 21 (48) | 50 (56) | 0.46 |
| Dwelling where villager with TB disease lived or visited | 14 (32) | 33 (37) | 0.57 |
| No. of participants who lived with someone with TB | |||
| Lived with someone with TB disease | 21 (48) | 44 (49) | 1.00 |
| Lived with someone with smear-positive TB | 13 (30) | 16 (18) | 0.20 |
| Lived with someone with smear-negative TB | 17 (39) | 42 (47) | 0.45 |
Note: TB = tuberculosis.
*Pearson's χ2 test or Fisher's exact test.
The heating method and ventilation level were not associated with TB disease (Table 5). Living area size was associated with disease in univariate but not multivariate analysis. We again observed an interaction between occupancy and living with someone with smear-positive TB: the odds of disease increased with increasing number of people per room only among participants who had lived with someone with smear-positive TB. This analysis also showed that, after adjustment for potential confounders, the risk of disease was significantly higher among participants with new compared with previous TB infection.
Table 5: Factors associated with progression to TB disease from infection between November 2011 and November 2012.
| Variable | No. (%) of participants with new or prior TB infection* | Crude OR (95% CI)† | Adjusted OR (95% CI)†‡ | |
|---|---|---|---|---|
| Disease (n = 44) | No disease (n = 89) | |||
| Age, yr | ||||
| < 15 | 12 (27) | 19 (21) | Reference | Reference |
| 15-29 | 22 (50) | 39 (44) | 0.9 (0.4-2.3) | 1.0 (0.3-2.8) |
| ≥ 30 | 10 (23) | 31 (35) | 0.5 (0.2-1.3) | 1.0 (0.3-3.0) |
| Sex | ||||
| Male | 22 (50) | 40 (45) | Reference | Reference |
| Female | 22 (50) | 49 (55) | 0.8 (0.4-1.5) | 0.8 (0.4-1.7) |
| Tobacco smoking | ||||
| Not current smoker | 15 (34) | 26 (30) | Reference | Not in model |
| Current smoker | 29 (66) | 62 (70) | 0.8 (0.4-1.8) | |
| Annual personal income, $§ | ||||
| < 20 000 | 31 (77) | 51 (60) | Reference | Reference |
| ≥ 20 000 | 9 (23) | 34 (40) | 0.4 (0.2-1.05) | 0.4 (0.2-1.1) |
| Prior TB infection | ||||
| Not documented TST-positive before November 2011 | 35 (79) | 53 (60) | Reference | Reference |
| Documented TST-positive before November 2011 | 9 (21) | 36 (40) | 0.4 (0.2-0.8) | 0.4 (0.2-0.9) |
| Heating method | ||||
| Forced air | 41 (93) | 83 (93) | Reference | Not in model |
| Radiator | 3 (7) | 6 (7) | 1.0 (0.3-3.4) | |
| No. of people per room¶ | ||||
| Among participants living with a smear-positive person | 1.9 ± 0.4 | 1.6 ± 0.6 | 1.3 (1.1-1.6) | 1.3 (1.2-1.5) |
| Among participants not living with a smear-positive person | 1.2 ± 0.5 | 1.1 ± 0.5 | 1.1 (0.9-1.2) | 1.1 (0.9-1.3) |
| Ventilation with heating on relative to median (1.66 air changes per hour)** | ||||
| < Median | 36 (82) | 67 (75) | Reference | Not in model |
| ≥ Median | 8 (18) | 22 (25) | 0.7 (0.3-1.5) | |
| Volume of living area relative to median (65.5 m3) | ||||
| < Median | 13 (30) | 44 (49) | Reference | Not in model |
| ≥ Median | 27 (61) | 59 (66) | 2.3 (1.1-5.0) | |
| Visited any dwelling used for social activities | 21 (48) | 50 (56) | 0.7 (0.3-1.6) | Not in model |
| Lived with smear-positive person†† | 13 (30) | 16 (18) | 1.9 (0.9-4.1) | 0.8 (0.3-1.8) |
Note: CI = confidence interval, OR = odds ratio, TB = tuberculosis, TST = tuberculin skin testing.
*Except where stated otherwise.
†CIs where OR excludes 1.0 are in bold.
‡Adjusted OR from the model that included all variables, except where indicated, plus an interaction term between occupancy and living with a smear-positive person that was statistically significant (p = 0.04).
§Eight participants with missing data on income status were excluded from the final model.
¶Interaction term between occupancy and living with a smear-positive person was not statistically significant in univariate analysis (p = 0.1), and was significant in the multivariate model (p = 0.04). As an example of interpretation, if we were to compare 2 participants who did not live together and whose dwellings differed in occupancy by 1 person per room, the unadjusted odds of disease would be 30% higher (as the crude OR is 1.3) for the participant living in the home with the greater number of people per room.
**In the living area. Lowest ventilation measured in the living area also was not associated with disease (data not shown).
††Adjusted OR shows association between living with someone with smear-positive TB and disease if living in a dwelling with 1.2 persons per room (chosen because it was the median number of people per room).
Interpretation
During a 12-month period when the incidence of TB dramatically increased in this village, the number of people per room was the only housing characteristic associated with newly diagnosed TB infection, and it was associated only among participants who had lived with someone with smear-positive disease. Similarly, the number of people per room was the only housing characteristic associated with progression to TB disease among infected participants, and this association was also dependent on living with someone with smear-positive TB. Other factors associated with newly diagnosed TB infection were age over 14 years old, visiting a dwelling that was used for social activities and having lived with someone with smear-positive TB. Prior TB infection was the only other factor associated with disease (against which it was protective).
Our results suggest that crowding in houses negatively affects efforts to eliminate TB from Canada's northern communities. Our findings also suggest that crowding affects TB risk among those living in a household where someone has smear-positive TB. Interestingly, crowding was associated both with risk of infection and risk of progression from infection to disease. The latter association may have arisen if people living in crowded conditions were more likely to experience repeated infection. However, as most participants with active TB did not live in such households, crowding alone does not explain the elevated risk of disease in this village.
Little is known about the role of home ventilation in transmission of M. tuberculosis. Although the level of ventilation in health care settings has been shown to affect the risk of TB infection among health care workers, in our study, air exchange rates in participants' dwellings were not associated with infection. We speculate that exposure to M. tuberculosis-containing droplet particles was so intense during interactions in people's homes that air exchange rates within the range of values measured in our study were insufficient to produce an observable reduction in the probability of transmission. It is plausible that exposure intensity is greater in people's homes compared with other settings, owing to greater duration or closer physical proximity of interactions. This may apply to other airborne infections of the respiratory tract: a study of Inuit infants on Baffin Island also did not find an association between ventilation and lower respiratory tract infections.25 Given the lack of association in our study and the absence of other published data on the effects of residential ventilation on TB transmission, increasing air exchange rates in houses may not reduce the incidence of TB infection in this village or other Inuit communities.
Strengths and limitations
Strengths of our study include the availability of detailed medical records (usually lifelong records) for all participants, which allowed accurate categorization of people as having new or prior TB infection as well as probable or confirmed disease. This permitted a unique study of risk factors for acquisition of infection and for progression to disease among those infected within the same population. In addition, we conducted a thorough evaluation of housing, which included a standardized walk-through assessment, enumeration of occupancy and direct measurement of outdoor air exchange rates (ventilation) with the use of a validated protocol based on tracer gas techniques.23 To account for seasonal fluctuations in air exchange rates, we manipulated the heating system to simulate different conditions, although we were unable to account for all factors (e.g., outdoor temperature, indoor activities) that may influence ventilation.
This study had a number of limitations, including the timing of the study, which was begun a few months after public health authorities considered TB incidence to have returned to baseline. This delay was unavoidable, given the need to allow the health services to complete all necessary evaluations and start treatment for active and latent TB plus the complexities of arranging a scientific investigation in a remote community. However, bias due to this delay is unlikely as all participants but 1, even those who had moved, were assigned the characteristics of their original residence; furthermore, it is unlikely that the characteristics of the dwellings changed substantially before the study was carried out. A second limitation is the possibility of measurement error for air exchange rates, which could have arisen form our use of carbon dioxide as a tracer gas. However, we adjusted our analyses to account for carbon dioxide production by people present during the measurement (details in Appendix 1). Furthermore, the air exchange rates we reported with heating off were in keeping with those reported by other investigators who used perfluorocarbon methods.25 A third limitation is the possibility of selection bias: the distribution of risk factors among contacts who declined to participate may have differed from that among the participants. However, housing characteristics are unlikely to have been associated with selection probability, and hence those associations would have been less affected by selection bias. A fourth limitation is the potential for a false-positive TST result due to prior bacille Calmette-Guérin vaccination. The risk of this occurrence is less than 1% when vaccination occurs in infancy and TST is performed more than 10 years later.26 False-positive TST results are unlikely to have occurred in our study, as bacille Calmette-Guérin is administered in infancy in this village, and there were only 18 TST-positive participants under the age of 10, of whom 10 had active TB and 3 lived with a smear-positive person, leaving only 5 in whom a false-positive TST result due to bacille Calmette-Guérin was plausible. Last, we may have been underpowered to find associations between ventilation and our outcomes owing to the limited sample size and homogeneity in the distribution of exposure to air change levels. The small sample also meant that we were unable to control for all potential confounders, and hence it is possible that our lack of observed associations may have been partially attributable to residual confounding.
Conclusion
This is the third report from a series of investigations performed to investigate why an Inuit village experienced a surge in the occurrence of active TB between November 2011 and November 2012. Despite a rigorous evaluation that included whole-genome sequencing of all culture-positive isolates and study of the role of nutritional, lifestyle and housing characteristics, we have been unable to identify the factors that clearly explain the elevated disease rate. Our findings suggest that improved nutrition and less crowding in households may contribute to reducing the risk of TB infection. However, given that the impact of nutritional, lifestyle or housing interventions on the risk of active TB remains uncertain, similar events could happen in other villages where TB infection is highly prevalent. Hence treatment of latent TB infection should be even further emphasized to achieve a long-term reduction in TB incidence in this village and in other communities where TB infection is highly prevalent.
Supplemental information
For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/4/3/E496/suppl/DC1
Supplementary Material
Acknowledgements
The authors thank the following for their help during the conduct of this study: the residents, village council, Hilda Snowball (mayor of the village) and all staff of the village clinic; the wellness workers who helped with enrolment and data collection: Janice Baron, Nikita Etok and Louisa Etok; Elena Labranche and other members of the region's Inuit health authority (Nunavik Regional Board of Health and Social Services); Matthew German for work in data collection; and Watson A. Fournier for providing information on housing construction.
Footnotes
Funding: The study was made possible through funding from the Foundation of the Royal Victoria Hospital, Canadian Institutes of Health Research (Operating Grant MOP-125858) and the Public Health Agency of Canada. Faiz Ahmad Khan is the recipient of salary support from the Fonds de recherche du Québec - Santé.
References
- 1.Tuberculosis in Canada, 2009: pre-release. Ottawa: Public Health Agency of Canada. 2010. [Google Scholar]
- 2.Tuberculosis in Canada, 2010: pre-release. Ottawa: Public Health Agency of Canada. 2011. [Google Scholar]
- 3.Tuberculosis in Canada, 2008: pre-release. Ottawa: Public Health Agency of Canada. 2009. [Google Scholar]
- 4.Tuberculosis in Canada, 2011: pre-release. Ottawa: Public Health Agency of Canada. 2012. [Google Scholar]
- 5.Tuberculosis in Canada, 2012: pre-release. Ottawa: Public Health Agency of Canada. 2013. [Google Scholar]
- 6.Duhaime G, Édouard R. Mesures et taux de faible revenu dans l'Inuit Nunangat. Québec: Université Laval. 2012. [accessed 2016 Sept. 2]. Available www.chaireconditionautochtone.fss.ulaval.ca/documents/pdf/2012-Faible-Revenu-Note-Finale(1).pdf.
- 7.Oliver LN, Peters PA, Kohen DE. Mortality rates among children and teenagers living in Inuit Nunangat, 1994 to 2008. Health Rep. 2012;23:17–22. [PubMed] [Google Scholar]
- 8.Peters PA. An age- and cause decomposition of differences in life expectancy between residents of Inuit Nunangat and residents of the rest of Canada, 1989 to 2008. Health Rep. 2013;24:3–9. [PubMed] [Google Scholar]
- 9.Anaya J. Report of the Special Rapporteur on the rights of indigenous peoples, James Anaya. Addendum: the situation of indigenous peoples in Canada. Report no. A/HRC/27/52/Add.2. Geneva: United Nations. 2014. [Google Scholar]
- 10.Backgrounder on Inuit and housing. Ottawa: Inuit Tapiriit Kanatami. 2004. [Google Scholar]
- 11.Hargreaves JR, Boccia D, Evans CA, et al. The social determinants of tuberculosis: from evidence to action. Am J Public Health. 2011;101:654–62. doi: 10.2105/AJPH.2010.199505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rasanathan K, Sivasankara Kurup A, Jaramillo E, et al. The social determinants of health: key to global tuberculosis control. Int J Tuberc Lung Dis. 2011;15(Suppl 2):S30–6. doi: 10.5588/ijtld.10.0691. [DOI] [PubMed] [Google Scholar]
- 13.Baker M, Das D, Venugopal K, et al. Tuberculosis associated with household crowding in a developed country. J Epidemiol Community Health. 2008;62:715–21. doi: 10.1136/jech.2007.063610. [DOI] [PubMed] [Google Scholar]
- 14.Stein L. Glasgow tuberculosis and housing. Tubercle. 1954;35:195–203. doi: 10.1016/s0041-3879(54)80204-2. [DOI] [PubMed] [Google Scholar]
- 15.Clark M, Riben P, Nowgesic E. The association of housing density, isolation and tuberculosis in Canadian First Nations communities. Int J Epidemiol. 2002;31:940–5. doi: 10.1093/ije/31.5.940. [DOI] [PubMed] [Google Scholar]
- 16.Menzies D, Fanning A, Yuan L, et al. Hospital ventilation and risk for tuberculous infection in Canadian health care workers. Canadian Collaborative Group in Nosocomial Transmission of TB. Ann Intern Med. 2000;133:779–89. doi: 10.7326/0003-4819-133-10-200011210-00010. [DOI] [PubMed] [Google Scholar]
- 17.Lee RS, Radomski N, Proulx JF, et al. Reemergence and amplification of tuberculosis in the Canadian arctic. J Infect Dis. 2015;211:1905–14. doi: 10.1093/infdis/jiv011. [DOI] [PubMed] [Google Scholar]
- 18.Edlin BR, Tokars JI, Grieco MH, et al. An outbreak of multidrug-resistant tuberculosis among hospitalized patients with the acquired immunodeficiency syndrome. N Engl J Med. 1992;326:1514–21. doi: 10.1056/NEJM199206043262302. [DOI] [PubMed] [Google Scholar]
- 19.Daley CL, Small PM, Schecter GF, et al. An outbreak of tuberculosis with accelerated progression among persons infected with the human immunodeficiency virus. An analysis using restriction-fragment-length polymorphisms. N Engl J Med. 1992;326:231–5. doi: 10.1056/NEJM199201233260404. [DOI] [PubMed] [Google Scholar]
- 20.Fox GJ, Lee RS, Lucas M, et al. Inadequate diet is associated with acquiring Mycobacterium tuberculosis infection in an Inuit community: a case-control study. Ann Am Thorac Soc. 2015;12:1153–62. doi: 10.1513/AnnalsATS.201503-156OC. [DOI] [PubMed] [Google Scholar]
- 21.Canadian Tuberculosis Standards. 6th ed. Toronto: Canadian Lung Association, Public Health Agency of Canada, Tuberculosis Prevention and Control. 2007. [Google Scholar]
- 22.Rooms of private dwelling. Ottawa: Statistics Canada. 2012. [accessed 2014 July 9]. Available www.statcan.gc.ca/concepts/definitions/dwelling-logement01-eng.htm.
- 23.Menzies R, Schwartzman K, Loo V, et al. Measuring ventilation of patient care areas in hospitals. Description of a new protocol. Am J Respir Crit Care Med. 1995;152:1992–9. doi: 10.1164/ajrccm.152.6.8520767. [DOI] [PubMed] [Google Scholar]
- 24.Persily AK. Evaluating building IAQ and ventilation with indoor carbon dioxide. ASHRAE Trans. 1997;103:193–204. [Google Scholar]
- 25.Kovesi T, Gilbert NL, Stocco C, et al. Indoor air quality and the risk of lower respiratory tract infections in young Canadian Inuit children. CMAJ. 2007;177:155–60. doi: 10.1503/cmaj.061574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Farhat M, Greenaway C, Pai M, et al. False-positive tuberculin skin tests: What is the absolute effect of BCG and non-tuberculous mycobacteria? Int J Tuberc Lung Dis. 2006;10:1192–204. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.