Abstract
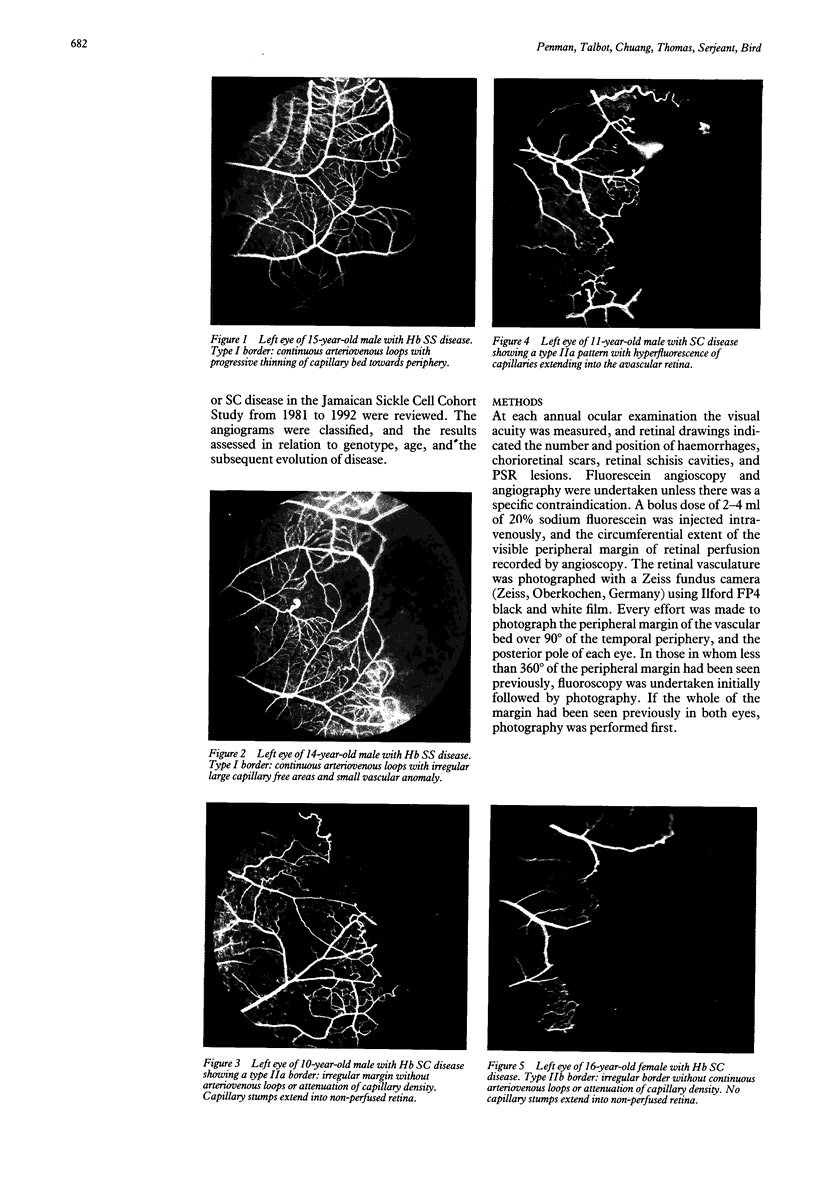
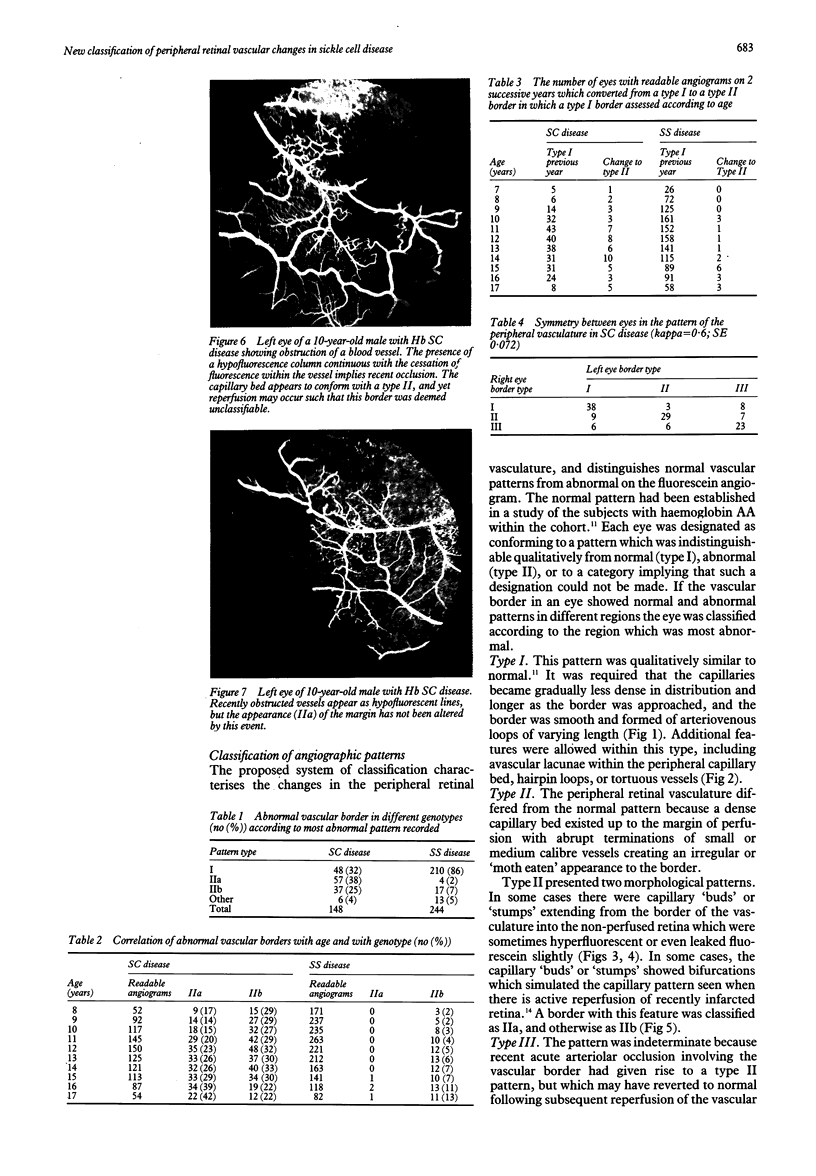
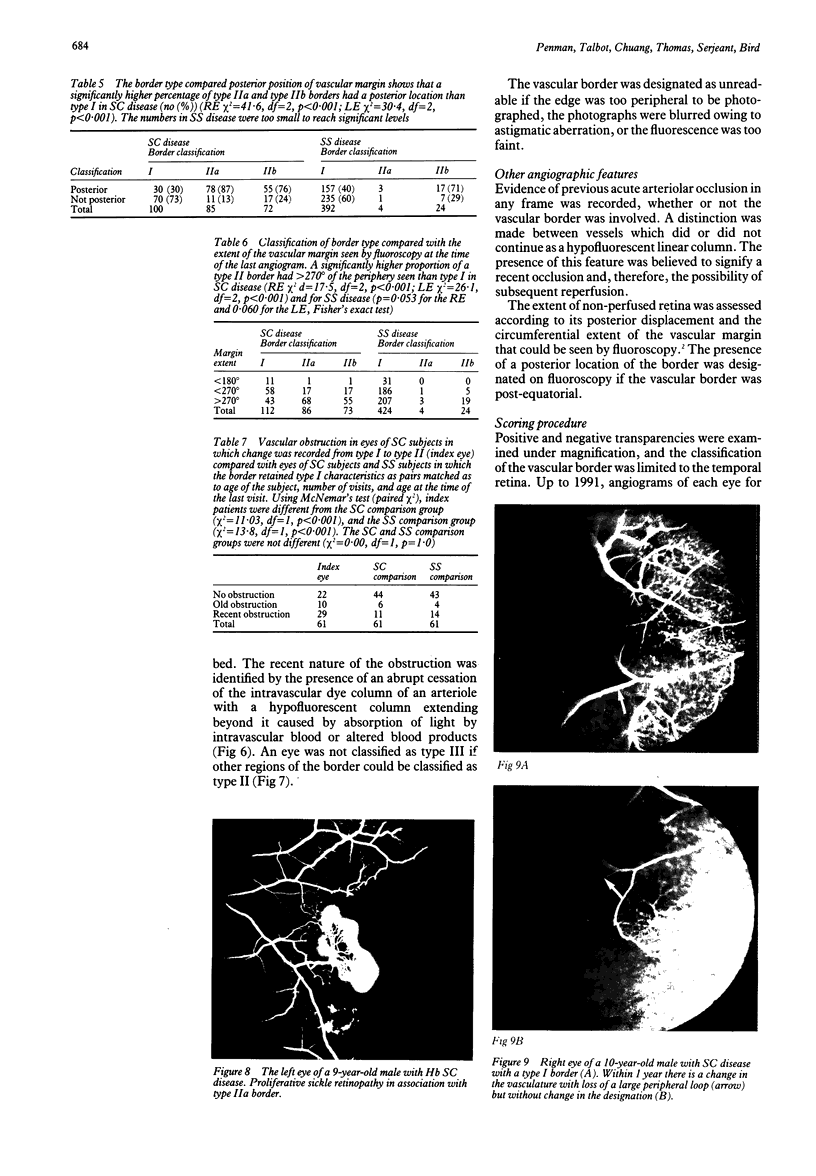
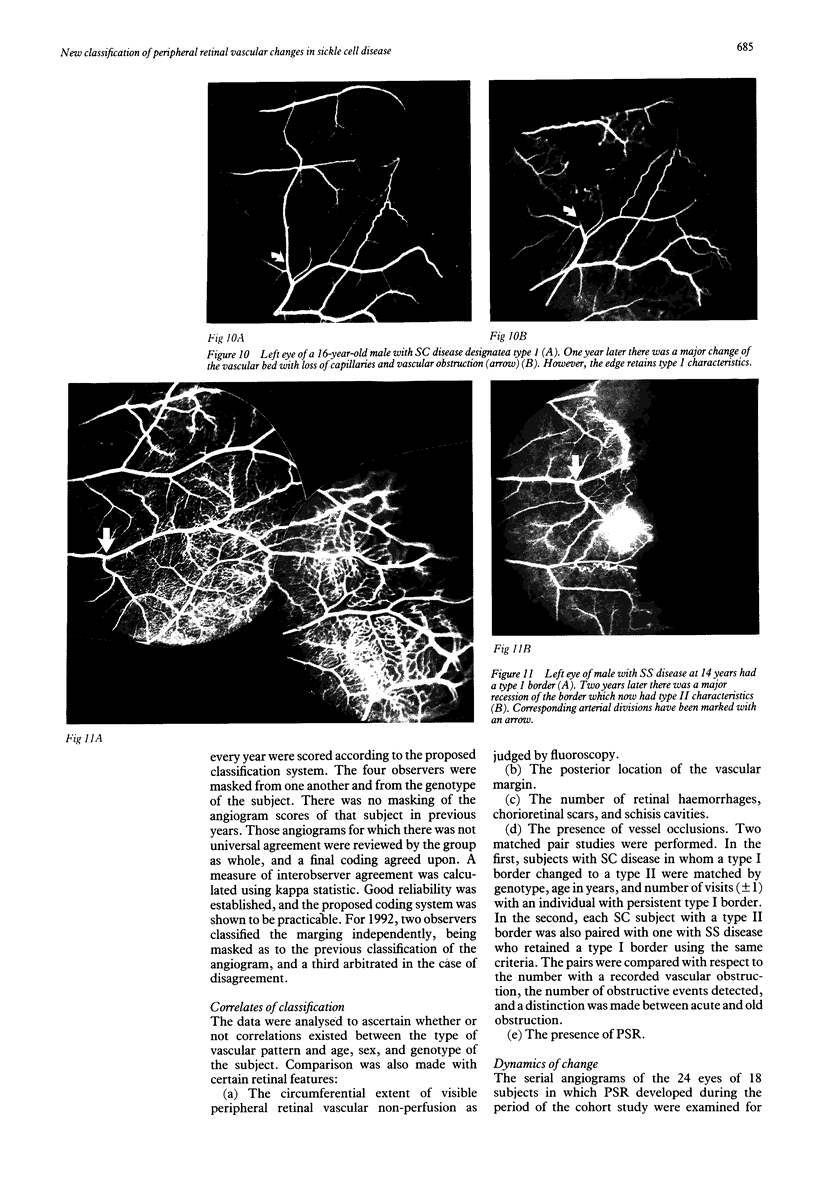
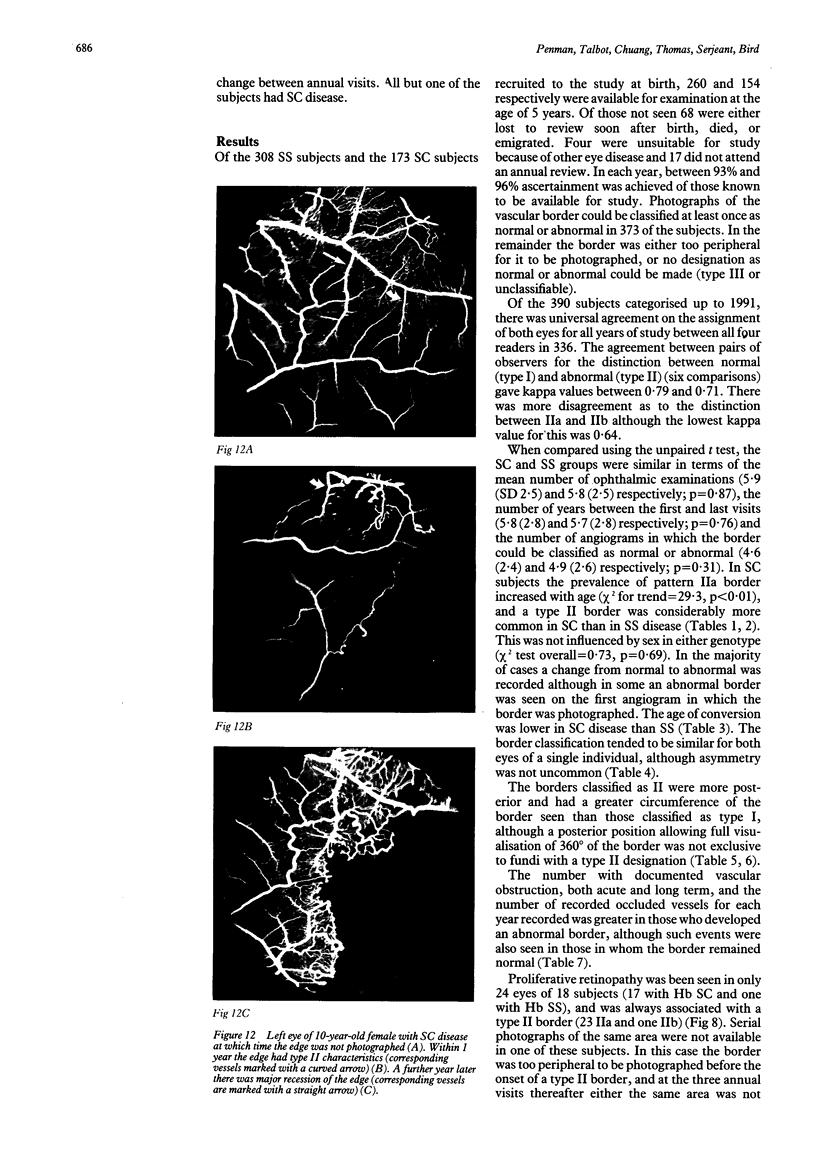
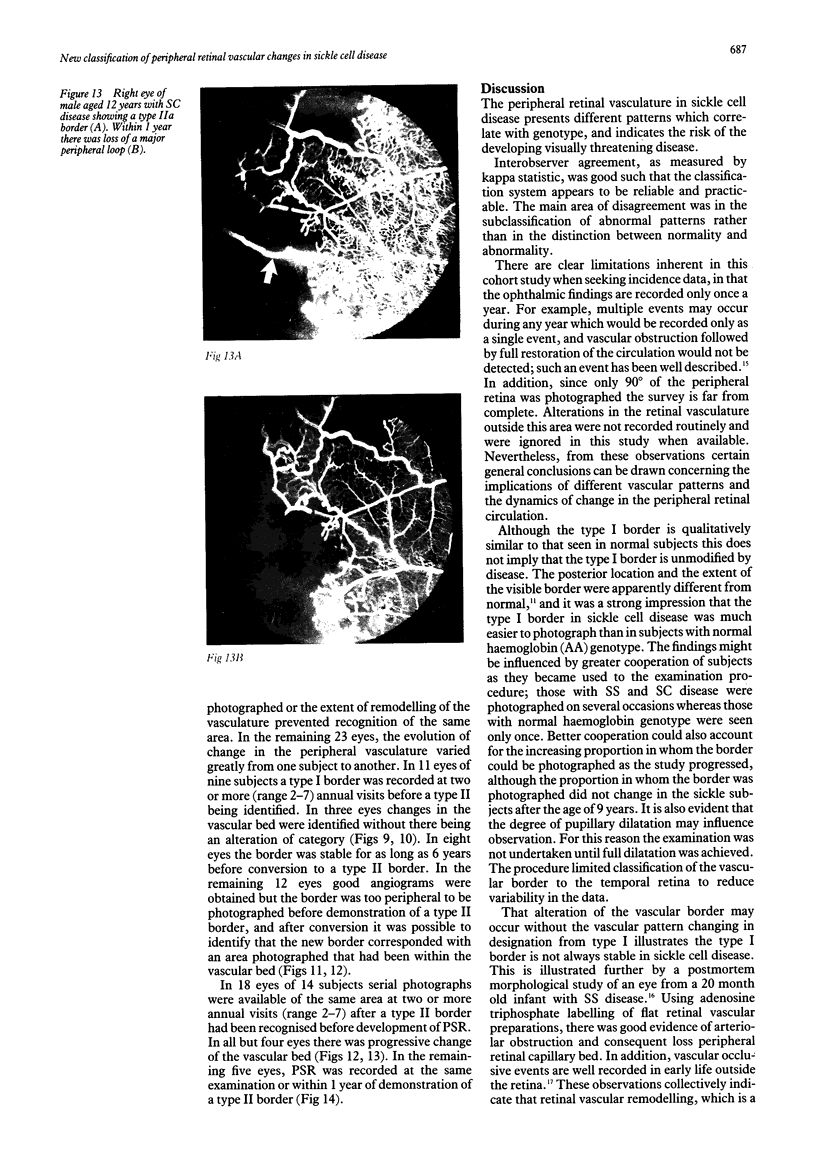
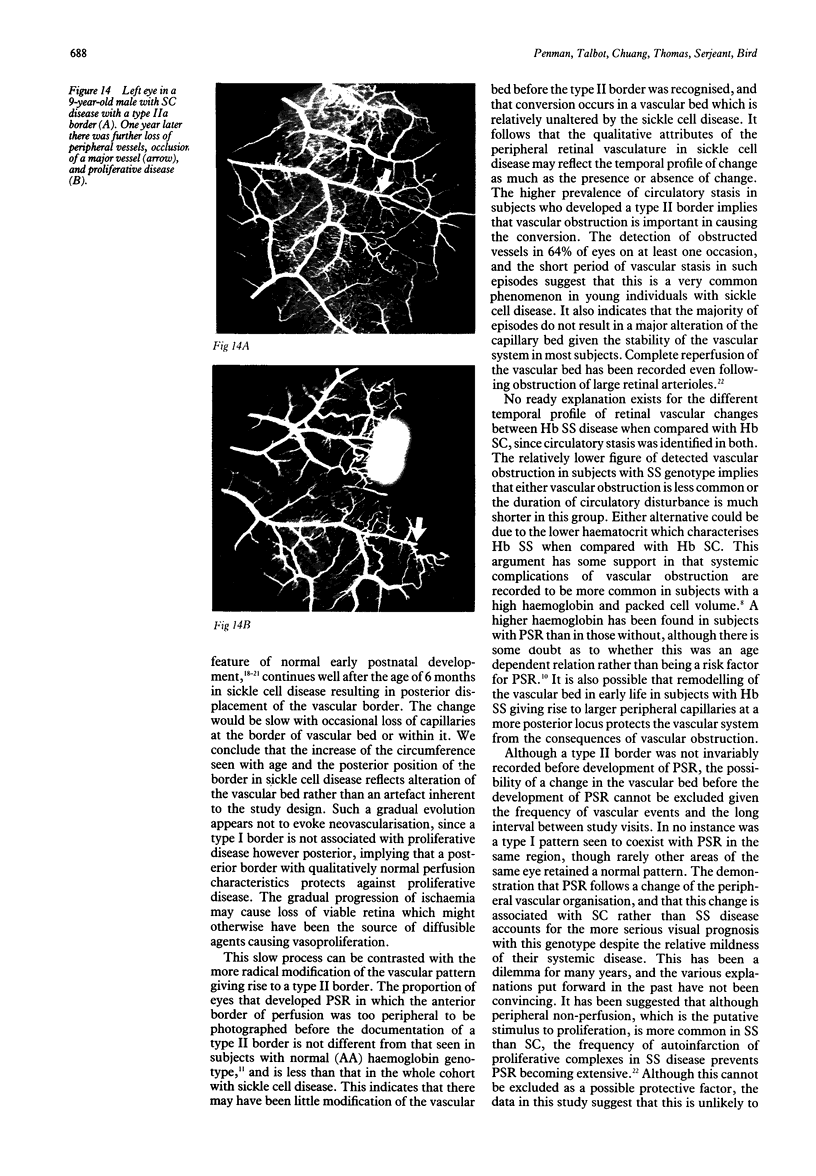
The systemic complications of homozygous sickle cell disease (SS) are more severe than in sickle cell haemoglobin C (SC) disease, and yet visual loss due to proliferative retinopathy is more common in the latter. This anomaly is unexplained. It is believed that proliferative disease occurs in response to closure of the peripheral retinal vasculature, yet a systematic longitudinal survey of the peripheral retinal vascular bed has not been undertaken. In the Jamaica Sickle Cohort study all subjects are scheduled to receive annual ocular examination and fluorescein angiography. The results have now been analysed in subjects with SS and SC disease using a new classification system based on a comparison of the peripheral retinal vascular bed with that recorded in the cohort with normal haemoglobin (AA) genotype. The vascular patterns could be classified as qualitatively normal (type I) or abnormal (type II). An abnormal vascular pattern was identified more commonly with age, in a significantly larger proportion of subjects with SC than SS disease, and was associated with the development of proliferative disease. In order to establish the dynamics of change, the angiograms were analysed in the 18 subjects (24 eyes) who developed proliferative disease. It is shown that a qualitatively normal vascular pattern may be retained despite loss of capillary bed and posterior displacement of the vascular border. A border which is qualitatively abnormal does not revert to normal, and once abnormal, continuous evolution may occur before development of proliferative lesions. The peripheral border of the retinal vasculature was too peripheral to photographed in 13 of the 24 eyes before it becoming qualitatively abnormal. It is concluded that a normal border, if posterior, results from gradual modification of the capillary bed and indicates low risk of proliferative disease. A qualitatively abnormal vascular border occurs as a radical alteration of retinal perfusion in subjects in whom little modification of the vascular bed occurred before the event, and signals risk of proliferative disease. This classification system is useful in identifying the likelihood of threat to vision in young Jamaicans with sickle cell disease, and the higher frequency of proliferative retinopathy in SC can be explained by the higher prevalence of a qualitatively abnormal peripheral retinal vasculature.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- COGAN D. G. DEVELOPMENT AND SENESCENCE OF THE HUMAN RETINAL VASCULATURE. Trans Ophthalmol Soc U K. 1963;83:465–489. [PubMed] [Google Scholar]
- Condon P. I., Serjeant G. R. Behaviour of untreated proliferative sickle retinopathy. Br J Ophthalmol. 1980 Jun;64(6):404–411. doi: 10.1136/bjo.64.6.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Condon P. I., Serjeant G. R. Ocular findings in homozygous sickle cell anemia in Jamaica. Am J Ophthalmol. 1972 Apr;73(4):533–543. doi: 10.1016/0002-9394(72)90005-0. [DOI] [PubMed] [Google Scholar]
- Condon P. I., Whitelocke R. A., Bird A. C., Talbot J. F., Serjeant G. R. Recurrent visual loss in homozygous sickle cell disease. Br J Ophthalmol. 1985 Sep;69(9):700–706. doi: 10.1136/bjo.69.9.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox P. D., Dunn D. T., Morris J. S., Serjeant G. R. Risk factors for proliferative sickle retinopathy. Br J Ophthalmol. 1990 Mar;74(3):172–176. doi: 10.1136/bjo.74.3.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galinos S. O., Asdourian G. K., Woolf M. B., Stevens T. S., Lee C. B., Goldberg M. F., Chow J. C., Busse B. J. Spontaneous remodeling of the peripheral retinal vasculature in sickling disorders. Am J Ophthalmol. 1975 May;79(5):853–870. doi: 10.1016/0002-9394(75)90747-3. [DOI] [PubMed] [Google Scholar]
- Goldberg M. F. Classification and pathogenesis of proliferative sickle retinopathy. Am J Ophthalmol. 1971 Mar;71(3):649–665. doi: 10.1016/0002-9394(71)90429-6. [DOI] [PubMed] [Google Scholar]
- Hamilton A. M., Marshall J., Kohner E. M., Bowbyes J. A. Retinal new vessel formation following experimental vein occlusion. Exp Eye Res. 1975 Jun;20(6):493–497. doi: 10.1016/0014-4835(75)90216-x. [DOI] [PubMed] [Google Scholar]
- McLeod D. S., Goldberg M. F., Lutty G. A. Dual-perspective analysis of vascular formations in sickle cell retinopathy. Arch Ophthalmol. 1993 Sep;111(9):1234–1245. doi: 10.1001/archopht.1993.01090090086026. [DOI] [PubMed] [Google Scholar]
- Penman A., Talbot J. F., Chuang E. L., Bird A. C., Serjeant G. R. Peripheral retinal vasculature in normal Jamaican children. Br J Ophthalmol. 1994 Aug;78(8):615–617. doi: 10.1136/bjo.78.8.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers D. W., Clarke J. M., Cupidore L., Ramlal A. M., Sparke B. R., Serjeant G. R. Early deaths in Jamaican children with sickle cell disease. Br Med J. 1978 Jun 10;1(6126):1515–1516. doi: 10.1136/bmj.1.6126.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serjeant G. R., Grandison Y., Lowrie Y., Mason K., Phillips J., Serjeant B. E., Vaidya S. The development of haematological changes in homozygous sickle cell disease: a cohort study from birth to 6 years. Br J Haematol. 1981 Aug;48(4):533–543. doi: 10.1111/j.1365-2141.1981.tb02750.x. [DOI] [PubMed] [Google Scholar]
- Serjeant G. R., Serjeant B. E., Forbes M., Hayes R. J., Higgs D. R., Lehmann H. Haemoglobin gene frequencies in the Jamaican population: a study in 100,000 newborns. Br J Haematol. 1986 Oct;64(2):253–262. doi: 10.1111/j.1365-2141.1986.tb04117.x. [DOI] [PubMed] [Google Scholar]
- Talbot J. F., Bird A. C., Maude G. H., Acheson R. W., Moriarty B. J., Serjeant G. R. Sickle cell retinopathy in Jamaican children: further observations from a cohort study. Br J Ophthalmol. 1988 Oct;72(10):727–732. doi: 10.1136/bjo.72.10.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talbot J. F., Bird A. C., Rabb L. M., Maude G. H., Serjeant G. R. Sickle cell retinopathy in Jamaican children: a search for prognostic factors. Br J Ophthalmol. 1983 Nov;67(11):782–785. doi: 10.1136/bjo.67.11.782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talbot J. F., Bird A. C., Serjeant G. R., Hayes R. J. Sickle cell retinopathy in young children in Jamaica. Br J Ophthalmol. 1982 Mar;66(3):149–154. doi: 10.1136/bjo.66.3.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Meurs J. C. Relationship between peripheral vascular closure and proliferative retinopathy in sickle cell disease. Graefes Arch Clin Exp Ophthalmol. 1991;229(6):543–548. doi: 10.1007/BF00203319. [DOI] [PubMed] [Google Scholar]