Abstract
Inequalities in women's mortality between U.S. states are large and growing. It is unknown whether they reflect differences between states in their population characteristics, contextual characteristics, or both. This study systematically examines the large inequalities in women's mortality between U.S. states using a multilevel approach. It focuses on “fundamental” social determinants of mortality at the individual and state levels as potential explanations. We analyze data from the 2013 public-use National Longitudinal Mortality Study on women aged 45–89 years and estimate multilevel logistic regression models. The models include women's personal characteristics (age, race/ethnicity, education, employment, income, and marriage) and states’ contextual characteristics (economic environment, social cohesion, sociopolitical orientation, physical infrastructure, and tobacco environment). We found that variation in women's mortality across states was significant (p<0.001). Adjusting for women's personal characteristics explained 30% of the variation. Additionally adjusting for states’ contextual characteristics explained 62% of the variation; the most important characteristics were social cohesion and economic conditions. No significant mortality differences between any two states remained after accounting for individual and contextual characteristics. Supplementary analyses of men indicate that state contexts have stronger and more pernicious consequences for women than men. Taken together, the findings underscore the importance of ‘bringing context back in’ and taking a multilevel approach when investigating geographic inequalities in U.S. mortality.
Keywords: Mortality, Gender, Inequality, Social determinants, U.S. states, Multilevel
Highlights
-
•
Variation in adult women's mortality risk across U.S. states is significant.
-
•
Differences in both women's and states’ characteristics account for the variation.
-
•
Most important state characteristics are social cohesion and economic conditions.
-
•
States may have stronger and more pernicious consequences for women than men.
1. Introduction
Life expectancy differs markedly across geographic areas of the United States. These differences have been growing since the 1980s—particularly among women—across regions (Montez & Berkman, 2014), divisions (Fenelon, 2013), states (Wilmoth, Boe, & Barbieri, 2011), and counties (Ezzati, Friedman, Kulkarni, & Murray, 2008). The differences between U.S. states are especially striking when put in international context. In 2000 the range in life expectancy at birth across U.S. states was 7.4 years compared to a range of only 4.7 years across similar high-income countries including Canada, Australia, New Zealand, Japan, and non-Eastern European countries (Wilmoth et al., 2011). The reasons for the differences across U.S. states are poorly understood and a growing area of research (Wilmoth et al., 2011, Patel et al., 2014, Tencza et al., 2014). The present study adds to the research on adult mortality differences across states using a powerful-yet-underutilized dataset, a multilevel perspective, and an extensive array of states’ characteristics.
1.1. Prior research
Prior studies aiming to explain geographic inequalities in U.S. adult mortality generally share two characteristics: (1) they focus on spatially-patterned characteristics of the population and (2) they use an ecological approach (i.e., data aggregated at the county level). For instance, an analysis of U.S. counties found that gains in longevity after the early 1980s were associated with county income and proportion of non-black residents, but unrelated to income inequality and the proportion graduating high school (Ezzati et al., 2008). Another county-level study of mortality trends examined population characteristics such as county-level estimates of race, education, single-parent households, and access to medical care (Kindig & Cheng, 2013). The characteristics most predictive of mortality trends during the 1990s were Hispanic ethnicity, education, population density, median household income, and percent smokers (for women), while access to medical care was not a significant predictor. Another study examined eight empirically-derived areas of the United States. It concluded that disparities in longevity among them were not explained by aggregate measures of race, income, or health-care access and utilization (Murray et al., 2006).
In addition to focusing on population characteristics, prior studies are largely ecological analyses of aggregate measures. This partly reflects data limitations, as researchers have had to rely on vital statistics data to investigate subnational mortality. However, as Subramanian, Kawachi, and Kennedy (2001) point out, geographic inequalities in health and mortality reflect an intrinsically multilevel phenomenon. They are influenced by individual and contextual characteristics, and thus “…when we restrict our focus only on one level of analysis (be it individual or ecological [contextual]), rather than use both levels, we obtain a distorted picture of the potential multilevel processes at play” (Subramanian, Jones, Kaddour, & Krieger, 2009: p. 348). The 2013 release of the public-use National Longitudinal Mortality Study has made multilevel analyses possible by unmasking respondents’ state of residence. The current study uses this data.
1.2. Geography and gender
Although there is no ideal geographic level for examining health inequalities, there is a long and prominent tradition of focusing on states (e.g., Wilmoth et al., 2011, Patel et al., 2014, Tencza et al., 2014). States are semi-sovereign areas that construct many of their own laws, policies, and programs. These structures filter down and shape mortality through myriad pathways, such as income tax, tobacco tax, and Medicaid generosity. Many studies find that states shape population health (see review in Borrell, Paléncia, Muntaner, Urquía, and Maimusi (2014)). For instance, Kawachi and colleagues (1999) found that state indices of women's status had “detrimental consequences” for women's and men's mortality and morbidity. Similarly, state-level income inequality can have pernicious consequences for morbidity and mortality (Wilkinson, 1996), while state-level social capital can have salubrious consequences (e.g., Herian et al., 2014, Kawachi et al., 1997). The importance of states is also underscored by a spatial analysis of U.S. life expectancy in 1999 that found roughly one-half of the variation in longevity across counties was attributable to the state within which they are located (Arcaya, Brewster, Zigler, & Subramanian, 2012).
We focus on state differences in women's mortality for two reasons. First, although geographic variation in U.S. mortality has historically been larger among men, women are rapidly catching up (Wilmoth et al., 2011). Since the early 1980s—a time of social and economic change, growing income inequality, and devolution to the states—the variation has grown more among women (Wilmoth et al., 2011, Ezzati et al., 2008, Kindig and Cheng, 2013). The growing geographic inequality in women's mortality is especially alarming because it reflects mortality increases in some areas alongside declines in others (Kindig & Cheng, 2013).
A second reason why we focus on women is that their mortality may be more strongly affected than men's mortality by state laws, policies, and programs. These contextual factors (for example, Medicaid generosity, abortion regulations that impact a broad array of health care services targeting women, and availability of affordable housing) may be more salient to women's lives in part because women are more likely than men to be economically disadvantaged and raising children. The few prior studies that have examined gender differences in contextual effects on health have found some support for this conjecture. A multilevel study of body mass index (BMI) across U.S. census tracts found that tract-level socioeconomic conditions predicted women's BMI, net of individual characteristics, but not men's BMI (Robert & Reither, 2004). A multilevel study of U.K. neighborhoods found that several neighborhood characteristics—trust, integration, political climate, unemployment rate, and the quality of the physical environment—were more strongly related to women's than men's health (Stafford, Cummins, Macintyre, Ellaway, & Marmot, 2005). We replicate our main analysis for men to glean insights into the extent to which state contexts may have unique consequences for women.
1.3. Hypothesized explanations for inequalities in women's mortality between U.S. States
We focus on “fundamental” social determinants of mortality (Link & Phelan, 1995) at the individual and state levels. Our approach reflects both the social determinants framework proposed by the World Health Organization (Solar & Irwin, 2010) and the socio-ecological framework developed by Macintyre and colleagues (Macintyre, Ellaway, & Cummins, 2002). The WHO framework posits that socioeconomic and demographic characteristics are the most important structural determinants of health and mortality, and that they are causally prior to downstream behavioral and biological risk factors.
1.3.1. Individual explanations
The personal characteristics that we examine reflect women's socioeconomic resources. These resources are considered “fundamental causes” of health and mortality disparities (Link & Phelan, 1995). They provide access to safe neighborhoods, fulfilling jobs, social ties, healthy lifestyles, et cetera—intervening mechanisms on the pathway between socioeconomic resources and health. Consistent with other studies, we focus on socioeconomic resources rather than intervening mechanisms because including the latter “stacks the deck” in favor of individual sources of inequality by over-specifying the individual portion of the multilevel model (Macintyre et al., 2002).
1.3.2. Contextual explanations
Macintyre and colleagues (Macintyre et al., 2002) offer a useful conceptual framework that allows us to develop hypotheses about the ways in which U.S. states shape their population's mortality. The framework was originally developed to categorize characteristics of small geographic areas, but can be easily adapted to larger areas. It rests on two primary contextual features—material and infrastructural resources, and collective social functioning. Material and infrastructural resources refer to socially patterned features of the physical and social environment which can shape health, such as education spending, transportation, and social services (Macintyre et al., 2002). Collective social functioning refers to social capital and cohesion, and speaks to how shared norms and values may shape health. Macintyre and colleagues (Macintyre et al., 2002) also posit that contextual factors may differ in importance across population groups.
These contextual features can be assessed using integral or derived measures (Diez Roux, 2003). Integral measures capture the characteristics of areas, such as public transportation, that persist even if the residents change. Derived measures capture aggregate characteristics of individuals that shape everyone's health. For example, median household income corresponds with school quality, recreational facilities, environmental conditions, and safe public spaces that affect everyone's health (Diez Roux, 2003). Adapting the Macintyre and colleagues (Macintyre et al., 2002) framework to U.S. states, we hypothesize that the following five features of states contribute to the degree to which their populations are able to lead a healthy life: the economic environment, social cohesion, sociopolitical orientation, physical infrastructure, and the tobacco environment.
The importance of the economic environment is illustrated by the finding that states with a high median household income and gross state product tend to have low mortality (Morgan & Morgan, 2013). An area's unemployment level also predicts adult mortality, even after accounting for adult's employment status (Osler et al., 2003), particularly for women (Stafford et al., 2005). Income inequality also matters. High income inequality in a state is associated with higher mortality (e.g., Kennedy, Kawachi, & Prothrow-Stith, 1996).
States also differ in the degree of social cohesion within their populations. Indeed, one indicator of cohesion—social capital—is a well-established predictor of a state's mortality (e.g., Kawachi et al., 1997). Social capital can influence mortality through mechanisms such as information flows, norms of reciprocity, collective actions, and solidarity (Putnam, 2000). State-level social capital predicts individual health, net of sociopolitical context (Herian et al., 2014) and income inequality (Subramanian et al., 2001).
A state's sociopolitical orientation can also affect mortality. For instance, regressive tax structures disproportionately hurt poor residents and may elevate mortality (Newman & O’Brien, 2011). Sociopolitical orientation can influence social expenditures, of which education is a key component. Dunn, Burgess, and Ross (2005) found that public expenditures on education had a greater impact on a state's mortality rate than did other expenditures, such as welfare, health, and hospitals. In addition, the generosity of a state's Medicaid program corresponds with its sociopolitical orientation (Ramírez de Arellano & Wolfe, 2007), and differentials in access and quality of care can be expected to influence mortality.
The physical infrastructure of a state shapes access to resources such as housing and transportation. A state's housing infrastructure can indirectly affect mortality when rental costs are a substantial portion of household income, leaving less money for other basic needs. Housing can directly affect mortality, for example, in states with a high share of housing built before lead-based paint was banned. In addition, access to public transportation can indirectly shape health through the ability to commute to work, and directly via exposure to pollutants and traffic fatalities. The proportion of the population living in urban areas may also be important.
State differences in policies related to tobacco may also be critical. States with a high presence of tobacco manufacturing impose less restrictive controls (e.g., smoking in public areas) and have a higher prevalence of tobacco consumption. Residents of such states may be at greater risk of exposure to second-hand smoke and an environment conducive to unhealthy lifestyles, regardless of personal smoking behavior.
Although we selected the individual and contextual characteristics based on theory and prior evidence, the conceptual distinction between the two types of characteristics is not entirely clear cut because “people create places, and places create people” (Macintyre & Ellaway, 2003: p. 20). Despite this complexity, a multilevel framework can be judiciously used. One way to do this (e.g., Subramanian et al., 2001) is to focus on partitioning the variation in mortality into individual and contextual sources, rather than building a causal model requiring strong temporal assumptions. Such assumptions are unnecessary for partitioning because, once constituted, the two sources can independently shape mortality. For instance, one's education provides personal resources for health while the average education in the state shapes community resources for health, and both sources can independently influence mortality. We return to this complexity in the discussion section.
1.4. Aims
The questions guiding this study are: (1) to what extent do individual characteristics and states’ contextual characteristics account for variation in women's mortality between states, (2) which contextual characteristics contribute most to the variation, and (3) do contextual characteristics similarly contribute to the variation among men? Our study extends prior work by: (a) distinguishing the contribution of individual characteristics from contextual features of their state of residence using a multilevel approach, (b) using data from a large nationally-representative survey, and (c) merging data on states’ contextual features collected from external sources, (d) including a wide range of contextual features, and (e) focusing on states and women. Our ultimate aim is to glean insights into potential policies and strategies to reduce geographic inequalities in mortality.
2. Materials and method
2.1. Data
Our analysis is based on the U.S. National Longitudinal Mortality Study (NLMS: Rogot, Sorlie & Johnson, 1992). The NLMS provides a random sample of the non-institutionalized population for the purpose of examining demographic and socioeconomic differentials in adult mortality. It was created by linking respondents in multiple waves of the Current Population Survey and a subset of the 1980 Census to death certificate information provided by the National Center for Health Statistics. We analyze the public-use version of the NLMS. It contains survey data collected during the 1980s and 1990s, with mortality follow-up through December 31, 2002. It provides six years of mortality follow-up for each respondent. It is the best data for our study because of its size, coverage, and information on state of residence.
2.2. Analytic sample
The analytic sample includes U.S.-born women aged 45–89 years during their six years of mortality follow-up. We had complete information for 94% of respondents (6% were excluded). The women represent all 50 states, excluding the District of Columbia.
The NLMS provides duration of follow-up from interview until death or six years for survivors (it masks other temporal information). We first created a person-quarter file that contains a record for every quarter a U.S.-born woman 35–89 years of age was alive from the interview until death or six years. Respondent's age is incremented every fourth quarter. We then selected person-quarter records when respondents were ages 45–89, our target age range. Thus, respondents can “age-in” and “age-out” of the analytic sample (e.g., see Montez and Zajacova (2013)). The final dataset contains 5,959,576 person-quarter observations and 24,754 deaths.
2.3. Analytic strategy
We estimate a series of multilevel, discrete-time event history models. The models account for the two-level hierarchical structure of the data, with respondents (level 1) nested within states (level 2). A multilevel model adjusted for age is shown below; subscript “i” identifies respondents and “j” identifies states.
The coefficient β0 is the overall intercept. It can be interpreted as the log-odds of death when ageij=0 and uj=0. Age is centered in our analysis, so ageij=0 reflects an actual age of 62.5 years. The term uj is the random effect of state. It will be greater (or less) than 0 depending on whether the state has a higher (or lower) than average log-odds of death. The intercept for state “j” is β0+ uj. Finally, the between-state variance in the log-odds of death, adjusted for age, is . We refer to the standard deviation, , as the state-level residual. After estimating the age-adjusted model, we progressively add the individual and contextual variables. We assess their contribution to the variation in state mortality by monitoring the attenuation of the state-level residual. All models are estimated with xtmelogit in Stata 14.0.
2.4. Individual characteristics
Measures of individuals’ demographic characteristics and socioeconomic resources are used to characterize their personal risks of death. Age refers to age in years during follow-up. It ranges from 45 to 89 and is centered at its mean of 62.5 years. Race/ethnicity is a three-category variable indicating non-Hispanic white (omitted reference); non-Hispanic black; other. Education is a three-category variable indicating 0–11 years of education; 12 years (omitted reference); 13 or more years. Employment status is a binary indicator of whether the respondent was employed at the time of interview. Family income-to-poverty ratio indicates whether family income was below 100% of the federal poverty level. Incomes are adjusted for inflation to 1990 dollars and compared to the 1990 poverty level. We also include legal marital status (married versus unmarried (omitted reference) respondents).
2.5. Contextual characteristics
State of residence includes the 50 U.S. states. In preliminary analyses, we collected 21 state-level variables that reflect various dimensions of the states’ economic environments, sociopolitical orientations, social cohesion, physical infrastructures, and tobacco environments. The values reflect circa 1990 to center the data on the approximate midpoint of the mortality follow-up. Variables based on the U.S. Census are taken from the 1990 census; variables from annual surveys are averaged across 1988–1992 to minimize annual fluctuation in these estimates.
We condensed the information in the 21 state-level variables into latent factors using exploratory (EFA) and confirmatory (CFA) factor analysis in Mplus (Muthén & Muthén, 2012). We chose this strategy because: (a) the variables tend to cluster, (b) we wanted a holistic measure of each underlying factor, and (c) summary measures avoid overestimating the impact of a single variable, over-specifying the model, and stacking the deck in favor of the contextual portion of the model. Our strategy is guided by Subramanian et al. (2009) who warn against using specific state variables for this type of analysis, as well as Navarro and Shi (2001) who assert that each contextual variable is part of an interrelated set, and it is the set that is both meaningful and actionable.
First, we used EFA to examine how the 21 variables cluster. We then used the EFA results, combined with theory-based choices for variables whose EFA clustering was ambiguous, to develop the five latent factors. The five factors were then validated using CFA. Model fit indices for each factor (available on request) showed adequate to excellent model fit, using standard thresholds. The five latent factors and the variables associated with them are described below and listed in Appendix Table A.1 with their sources.
2.5.1. Economic environment
This latent factor taps the absolute level of economic well-being. It is comprised of: (1) gross state product per capita (GSP), (2) education expenditures per capita, (3) percent of state's total tax revenue from sales tax, (4) median household income, (5) percent of individuals below poverty line, (6) percent of female-householder families below poverty line, and (7) percent of adults 25 years and older with a bachelor's degree or higher.
2.5.2. Social cohesion
This factor describes the level of social and economic integration and equality within a state. It is comprised of four variables: (1) Gini coefficient of income inequality, (2) unemployment rate, (3) violent crime rate, and (4) the state-level social capital index developed by Putnam (2000). The index includes 14 components such as involvement in community organizations and social trust. The fact that income inequality and unemployment cluster with crime and social capital more so than with the variables in the economic environment latent factor indicates that these measures capture social and economic integration, and relative well-being, more so than absolute economic well-being.
2.5.3. Sociopolitical orientation
This factor captures the states' political orientation, particularly with respect to social safety nets. The four variables include: (1) percent of federal Earned Income Tax Credit offered by the state (among states offering it before 1990), an indicator of progressive taxation, (2) per capita public welfare expenditures (e.g., social services), (3) percent of presidential elections from 1960 through 1992 in which voters favored a Republican candidate, and (4) an overall score of the state's Medicaid program.
2.5.4. Physical infrastructure
This factor describes the housing, transportation, and population distribution in a state. It includes: (1) the percent of population living in a metropolitan statistical area, (2) the percent of workers using public transportation, and (3) housing affordability, which is the percent of renter-occupied units with monthly costs <35% of household income.
2.5.5. Tobacco environment
This factor captures the state's consumption, regulation, and production of tobacco. It includes the: (1) number of cigarette pack sales per capita, (2) percent of the retail price of a pack of cigarettes comprised of state taxes, and (3) percent contribution of tobacco manufacturing to the gross state product.
3. Results
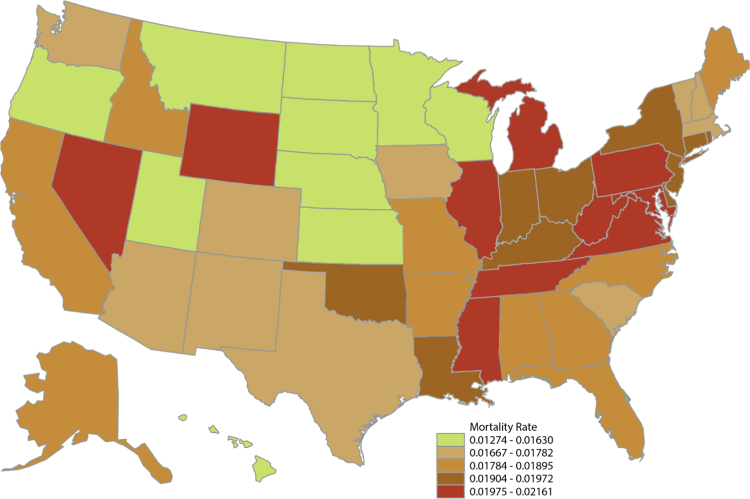
Fig. 1 shows the age-standardized annual probability of death among U.S-born women aged 45–89 years by U.S. state, where the NLMS data is centered on approximately 1990. It displays the well-documented geographic clustering of especially-high mortality states in the Appalachian and southeastern areas, and especially-low mortality states in the upper plains. The patterns are similar to maps of life expectancy at age 50 using vital statistics data (e.g., Wilmoth et al., 2011); slight discrepancies will result from the NLMS sampling frame, which excludes the institutionalized population, and our focus on U.S.-born individuals.
Fig. 1.
Age-standardized annual probability of death among U.S.-born women aged 45–89 years.
A summary of the individual and contextual variables used in our analysis is provided in Table 1. The individual variables are age-standardized. The contextual latent factors are Z-scores. For parsimony the table shows the 10 states with the lowest mortality and the 10 with the highest mortality among women aged 45–89 years (all states are shown in appendix Table A.2). The age-standardized annual probability of death during the study period ranges from a low of 1.27% in Hawaii (followed by 1.37% in South Dakota and 1.48% in North Dakota) to a high of 2.16% in Nevada (right after 2.10% in West Virginia and 2.06% in Tennessee). The disparity is substantial; the probability of death in Nevada is 1.7 times greater than Hawaii.
Table 1.
Summary of individual and contextual characteristics by U.S. state, circa 1990.
| State | Annual p(death) | Age-standardized characteristics of female respondents (%) |
State contextual characteristics |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-Hispanic White | Less than high school | Employed | Poverty | Married | Economic environment | Social cohesion | Socio-political orientation | Physical infra-structure | Tobacco environment | ||
| 10 lowest-mortality states | |||||||||||
| HI | 0.01274 | 31.4 | 30.0 | 47.7 | 9.0 | 63.4 | 1.37 | −1.22 | −0.67 | 0.70 | −1.30 |
| SD | 0.01367 | 95.4 | 30.4 | 46.9 | 17.0 | 68.5 | −1.49 | −1.95 | 0.91 | −1.63 | −0.38 |
| ND | 0.01476 | 97.6 | 32.0 | 43.3 | 15.8 | 69.1 | −0.76 | −1.61 | 0.78 | −1.31 | −0.96 |
| NE | 0.01488 | 96.5 | 26.0 | 46.9 | 12.4 | 67.0 | −0.54 | −1.28 | 0.31 | −0.97 | −0.85 |
| MN | 0.01498 | 98.0 | 27.3 | 46.5 | 11.7 | 66.0 | 0.23 | −1.06 | −3.48 | 0.29 | −1.81 |
| UT | 0.01520 | 96.3 | 19.0 | 40.1 | 10.8 | 69.9 | 0.34 | −1.22 | 0.28 | 0.22 | −0.10 |
| KS | 0.01536 | 92.8 | 25.6 | 46.9 | 12.0 | 66.5 | −0.31 | −0.33 | 0.24 | −0.64 | −0.47 |
| WI | 0.01555 | 96.0 | 29.1 | 44.9 | 10.5 | 64.9 | 0.46 | −1.11 | −1.00 | 0.06 | −1.12 |
| MT | 0.01577 | 96.0 | 25.3 | 42.1 | 13.9 | 64.9 | −1.14 | −0.89 | 0.33 | −1.52 | 0.49 |
| OR | 0.01630 | 97.6 | 23.5 | 41.5 | 10.5 | 65.0 | −0.29 | −0.39 | −0.33 | 0.25 | −0.73 |
| 10 highest-mortality states | |||||||||||
| MD | 0.01975 | 79.1 | 33.0 | 42.3 | 11.7 | 59.5 | 2.12 | −0.17 | −1.37 | 1.22 | 0.89 |
| IL | 0.01980 | 86.9 | 33.5 | 42.8 | 12.1 | 59.5 | 0.39 | 0.72 | −0.00 | 1.23 | −0.31 |
| MI | 0.01988 | 87.3 | 32.2 | 37.5 | 12.7 | 61.4 | 1.18 | 0.44 | −0.07 | 0.86 | −0.67 |
| PA | 0.02012 | 92.2 | 35.3 | 38.1 | 12.5 | 60.5 | −0.07 | 0.22 | −0.09 | 1.03 | 0.31 |
| MS | 0.02025 | 70.4 | 44.5 | 37.8 | 27.4 | 59.0 | −1.19 | 1.83 | 1.18 | −1.17 | 0.24 |
| VA | 0.02030 | 80.8 | 36.3 | 42.7 | 13.9 | 60.8 | 0.81 | −0.11 | 0.78 | 0.28 | 2.43 |
| WY | 0.02035 | 95.5 | 22.6 | 44.1 | 10.9 | 67.2 | 0.09 | −1.17 | 1.29 | −1.54 | 1.40 |
| TN | 0.02059 | 82.6 | 46.8 | 38.5 | 21.7 | 58.8 | −0.97 | 1.11 | 0.44 | −0.13 | 0.94 |
| WV | 0.02098 | 96.6 | 46.8 | 30.5 | 17.8 | 60.9 | −1.37 | 1.11 | −0.26 | −0.93 | 0.44 |
| NV | 0.02161 | 89.6 | 22.1 | 44.8 | 10.7 | 57.5 | 0.16 | 0.50 | 0.46 | 0.76 | −0.29 |
| (A) # of the lowest mortality states that scored in top 10 of each characteristic (underlined) | |||||||||||
| 3 | 4 | 5 | 2 | 7 | 2 | 7 | 3 | 4 | 4 | ||
| (B) # of the highest mortality states that scored in bottom 10 of each characteristic (bolded) | |||||||||||
| 1 | 3 | 5 | 2 | 3 | 3 | 3 | 3 | 3 | 4 | ||
| Difference between (A) and (B) | |||||||||||
| 2 | 1 | 0 | 0 | 4 | −1 | 4 | 0 | 1 | 0 | ||
Notes: N=5,959,576 person-quarter observations. The individual characteristics of female respondents are from the public-use NLMS. The estimates are weighted using the NLMS sample weights and age-standardized to the 2000 U.S. female population. The state characteristics are latent factor scores from a confirmatory factor analysis. Each latent factor is standardized as a Z-score. We underline low-mortality states if they were among the 10 “best” scores for each characteristic associated with a healthy life (e.g., low proportion of women without a high school credential), and we bold high-mortality states if they were among the 10 “worst” scores for each characteristic (e.g., high proportion without credential).
To illustrate the associations between the variables and women's mortality, we underline low-mortality states if they were among the 10 “best” scores for each characteristic associated with a healthy life (e.g., low proportion of women without a high school credential), and we bold high-mortality states if they were among the 10 “worst” scores for each characteristic (e.g., high proportion without a credential). An intriguing finding, also suggested by Macintyre et al. (2002), is that if a characteristic is associated with low mortality in a state, the lack of that characteristic does not necessarily correspond with high mortality, and vice versa. This is most pronounced for social cohesion. A high degree of cohesion strongly corresponds to low mortality (among the 10 states with the “best” scores for cohesion, 7 were among the lowest-mortality states), but low cohesion does not strongly correspond to high mortality (among the 10 states with the “worst” scores for cohesion, just 3 were among the highest mortality states).
3.1. Contribution of individual characteristics to mortality inequalities between states
Next we assess the extent to which women's personal characteristics account for variation in mortality between states. We estimate a series of multilevel logistic regression models shown in Table 2. The baseline model includes age and the state-level random effect. The model coefficients indicate that, on average, each year of age is associated with a 0.087 increase in the log-odds of death, or a 9.1% [100(e0.087−1)] increase in the odds of death. Adjusting for age, the between-state standard deviation, or “state residual,” in the log-odds of death is 0.091 (p<0.001).
Table 2.
Multilevel logistic regression coefficients estimating the log-odds of death among U.S-born women aged 45–89 years.
| Characteristics of women |
Characteristics of states |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Race | Education | Economic well-being | Marital status | Economic environment | Social cohesion | Socio-political orientation | Physical infra-structure | Tobacco environment | Full model | State only | |
| Intercept | −6.000⁎⁎⁎ | −6.032⁎⁎⁎ | −6.061⁎⁎⁎ | −5.895⁎⁎⁎ | −5.703⁎⁎⁎ | −5.704⁎⁎⁎ | −5.705⁎⁎⁎ | −5.703⁎⁎⁎ | −5.707⁎⁎⁎ | −5.702⁎⁎⁎ | −5.705⁎⁎⁎ | −6.003⁎⁎⁎ |
| Level 1: Individual | ||||||||||||
| Age | 0.087⁎⁎⁎ | 0.088⁎⁎⁎ | 0.085⁎⁎⁎ | 0.077⁎⁎⁎ | 0.072⁎⁎⁎ | 0.072⁎⁎⁎ | 0.072⁎⁎⁎ | 0.072⁎⁎⁎ | 0.072⁎⁎⁎ | 0.072⁎⁎⁎ | 0.072⁎⁎⁎ | 0.087⁎⁎⁎ |
| Race/ethnicity (NHW) | ||||||||||||
| NHB | 0.353⁎⁎⁎ | 0.296⁎⁎⁎ | 0.274⁎⁎⁎ | 0.248⁎⁎⁎ | 0.249⁎⁎⁎ | 0.240⁎⁎⁎ | 0.248⁎⁎⁎ | 0.247⁎⁎⁎ | 0.245⁎⁎⁎ | 0.234⁎⁎⁎ | ||
| Other | −0.003 | |||||||||||
| Education (HS) | ||||||||||||
| Less than HS | 0.178⁎⁎⁎ | 0.130⁎⁎⁎ | 0.121⁎⁎⁎ | 0.121⁎⁎⁎ | 0.119⁎⁎⁎ | 0.121⁎⁎⁎ | 0.121⁎⁎⁎ | 0.120⁎⁎⁎ | 0.120⁎⁎⁎ | |||
| More than HS | −0.118⁎⁎⁎ | −0.089⁎⁎⁎ | −0.098⁎⁎⁎ | −0.097⁎⁎⁎ | −0.098⁎⁎⁎ | −0.098⁎⁎⁎ | −0.097⁎⁎⁎ | −0.098⁎⁎⁎ | −0.098⁎⁎⁎ | |||
| Employed | −0.532⁎⁎⁎ | −0.571⁎⁎⁎ | −0.572⁎⁎⁎ | −0.571⁎⁎⁎ | −0.571⁎⁎⁎ | −0.571⁎⁎⁎ | −0.571⁎⁎⁎ | −0.570⁎⁎⁎ | ||||
| Income−to-poverty<1 | 0.146⁎⁎⁎ | 0.080⁎⁎⁎ | 0.082⁎⁎⁎ | 0.079⁎⁎⁎ | 0.080⁎⁎⁎ | 0.082⁎⁎⁎ | 0.080⁎⁎⁎ | 0.081⁎⁎⁎ | ||||
| Married | −0.253⁎⁎⁎ | −0.253⁎⁎⁎ | −0.254⁎⁎⁎ | −0.253⁎⁎⁎ | −0.253⁎⁎⁎ | −0.254⁎⁎⁎ | −0.253⁎⁎⁎ | |||||
| Level 2: State | ||||||||||||
| Economic environment | 0.022† | 0.027⁎ | 0.029⁎ | |||||||||
| Social cohesion | 0.035⁎⁎⁎ | 0.026⁎ | 0.063⁎⁎⁎ | |||||||||
| Sociopolitical orientation | 0.007 | 0.014 | 0.007 | |||||||||
| Physical infrastructure | 0.029⁎⁎ | 0.018 | 0.007 | |||||||||
| Tobacco environment | 0.019† | 0.020† | 0.036⁎⁎ | |||||||||
| State residual | 0.091⁎⁎⁎ | 0.076⁎⁎⁎ | 0.073⁎⁎⁎ | 0.071⁎⁎⁎ | 0.064⁎⁎⁎ | 0.059⁎⁎⁎ | 0.052⁎⁎⁎ | 0.063⁎⁎⁎ | 0.052⁎⁎⁎ | 0.062⁎⁎⁎ | 0.035⁎⁎ | 0.043⁎⁎⁎ |
Notes: Reference groups in parentheses. In all models, the number of deaths=24,754 and number of person-quarter records=5,959,576. NHW=non-Hispanic white; NHB=non-Hispanic black; HS=high school. Models are not weighted. In the state economics model, the p-value for economic environment is 0.052; in the tobacco environment model, the p-value for tobacco is 0.090; in full model the p-value for tobacco environment is 0.060.
p<0.05.
p<0.01.
p<0.001.
p<0.10.
The next four models in Table 2 progressively add the personal characteristics. Adjusting for women's race/ethnicity reduces the state residual from 0.091 to 0.076, a 16% reduction. The residual is further reduced to 0.073 after accounting for education and then to 0.071 after adding employment and poverty to the model. Including marital status attenuates the state residual to 0.064, a 30% reduction from the baseline model. In other words, 30% of the variation in women's mortality across states is accounted for by the individual characteristics we examined.
3.2. Contribution of contextual characteristics to mortality inequalities between states
The next six models add the contextual latent factors. We first examine each factor separately. Among the five factors, states’ social cohesion (p<0.001) is the most strongly associated with women's mortality. States’ physical infrastructure (p<0.01) and economic environment (p=0.052) are also significant predictors of women's mortality. The tobacco environment is marginally significant (p=0.090) while sociopolitical orientation is not significant (p=0.555). Comparing the magnitude of the coefficients is also informative (recall the latent factors are standardized to Z-scores). For instance, the cohesion coefficient is roughly twice as large as the tobacco coefficient. Comparing the latent factors to women's characteristics is not as straightforward but illuminating nonetheless. The social cohesion model shows that moving across the range of states’ social cohesion scores (±3σ=6×0.035=0.210) has a similar effect as moving across the range of women's education levels (0.119−(−0.098)=0.217).
The full model includes all individual and contextual characteristics. Two of the five contextual factors—social cohesion and economic environment—remain statistically significant. In the full model the state residual is reduced to just 0.035, a 62% reduction from the baseline model. In other words, 62% of the variation in women's mortality across states is accounted for by the individual and contextual characteristics that we examined.
In the last column of Table 2 we only include age and the contextual factors in order to examine the sensitivity of the findings to considering contextual factors alone. We find that 53% of the variation in women's mortality across states reflects these contextual factors alone compared with 30% by the individual factors alone.
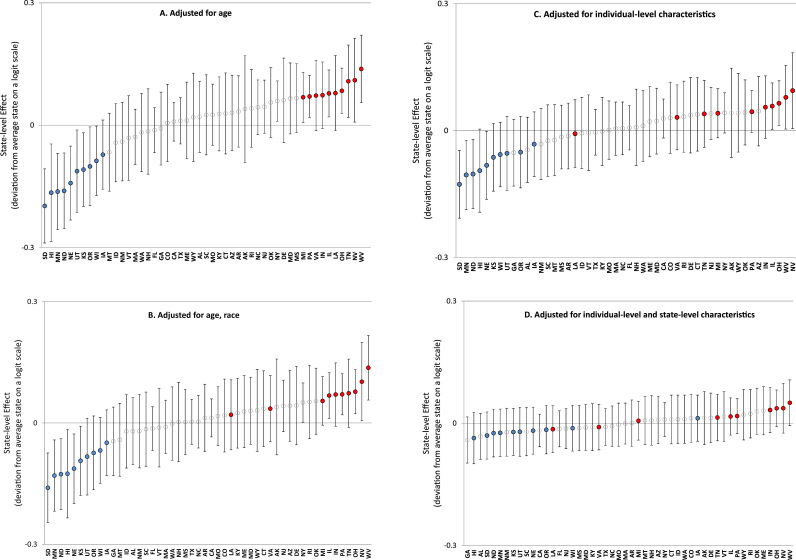
3.3. Differences in women's mortality between specific states
To visualize the contribution of the individual and contextual characteristics to differences in mortality between states, we plot the state-level effects in Fig. 2. These effects are the difference in the log-odds of death between each state and the average state. Panel A in Fig. 2 displays the state-level effects and their 95% confidence intervals estimated from the age-adjusted model in Table 2. It shows that women's mortality in states such as South Dakota, Hawaii, and Minnesota is significantly lower than the statistically average state and significantly lower than many other states such as West Virginia, Nevada, and Tennessee. To more easily track how adjusting for individual and state characteristics accounts for mortality differences between specific states, we identify the 10 lowest mortality states with blue dots and the 10 highest with red dots. Interestingly, panel A also illustrates a modest curvilinear pattern. Low-mortality states have exceptionally low mortality. Beyond this group of states, the incremental state-to-state increase in mortality is much smaller than it is among these states.
Fig. 2.
State-level effects on mortality of U.S. women aged 45–89 years.
As shown in panel B, controlling for women's race/ethnicity attenuates the state effects. Two of the ten highest mortality states—Louisiana and Virginia—break away from the pack and now exhibit average mortality. Panel C shows the state effects after controlling for all individual characteristics. As expected the effects are further attenuated. However, the overall curvilinear pattern persists, as do significant differences between low and high mortality states.
Panel D shows the state-level effects after adjusting for all individual and contextual characteristics. Little difference in women's mortality rates remains. We also note that the social cohesion latent factor was the only factor that explained the exceptionally low mortality of states such as North Dakota and Minnesota (figures from models including each latent factor separately are available on request). Social cohesion was also the only factor that flattened the curvilinear pattern.
3.4. Sensitivity analyses
Given the importance of the social cohesion and economic latent factors, we examined each of their indicators in separate models, adjusting for individual factors (available on request). Although the indicators collectively reflect an underlying latent factor we wanted to confirm that our results were not unduly influenced by a single indicator. Our analyses confirmed this. We first assessed the four indicators reflecting social cohesion. From greatest to smallest contribution to state variation in mortality were social capital (adjusting for it reduced the state residual to 0.043), unemployment (0.049), crime (0.058), and income inequality (0.060). We then assessed the seven indicators within the economic latent factor. Adjusting for median household income or gross state product reduced the state residual by a slightly greater degree (0.058 or 0.059, respectively) than did adjusting for other indicators (0.062–0.064 depending on the indicator).
We also examined state variation in mortality for two broad age groups, as many state policies and programs target specific age groups. Due to sample size limitations we examined two age groups (45–69 and 70–89 years), and even then the model for the younger group is not very robust. In age-adjusted models, we found that state variation in mortality was 50% larger among the younger group (state residual=0.108) than the older group (state residual=0.072). However, state context appears to be more important among the older group. For instance, once we adjusted for all of the individual factors, we had accounted for 88% of the state variation in mortality among the younger group but just 18% among the older group.
3.5. A look at men's mortality
We replicated the analysis for men to assess how personal characteristics and state contexts shaped variation in men's mortality. Consistent with our expectation, the state-level mortality variation was less strongly associated with the contextual features among men than among women (gender difference not tested for statistical significance). As shown in Table 3, individual factors accounted for 34% of the state variation in men's mortality (vs. 30% for women) while individual and contextual factors jointly accounted for 41% of the variation in men's mortality (vs. 62% for women). Even more striking, adjusting only for contextual factors accounted for 23% of men's mortality variation compared with 53% of women's. We also found that the contextual factors that mattered most differed for men and women. While economic environments and social cohesion were most important for women, the tobacco environment was the main explanation for men.
Table 3.
Multilevel logistic regression coefficients estimating the log-odds of death among U.S-born men aged 45–89 years.
| Characteristics of men |
Characteristics of states |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Race | Education | Economic well-being | Marital status | Economic environment | Social cohesion | Socio-political orientation | Physical infra-structure | Tobacco environment | Full model | State only | |
| Intercept | −5.395⁎⁎⁎ | −5.412⁎⁎⁎ | −5.471⁎⁎⁎ | −5.092⁎⁎⁎ | −4.887⁎⁎⁎ | −4.886⁎⁎⁎ | −4.888⁎⁎⁎ | −4.887⁎⁎⁎ | −4.888⁎⁎⁎ | −4.886⁎⁎⁎ | −4.888⁎⁎⁎ | −5.396⁎⁎⁎ |
| Level 1: Individual | ||||||||||||
| Age | 0.086⁎⁎⁎ | 0.086⁎⁎⁎ | 0.083⁎⁎⁎ | 0.068⁎⁎⁎ | 0.067⁎⁎⁎ | 0.067⁎⁎⁎ | 0.067⁎⁎⁎ | 0.067⁎⁎⁎ | 0.067⁎⁎⁎ | 0.067⁎⁎⁎ | 0.067⁎⁎⁎ | 0.086⁎⁎⁎ |
| Race/ethnicity (NHW) | ||||||||||||
| NHB | 0.274⁎⁎⁎ | 0.191⁎⁎⁎ | 0.130⁎⁎⁎ | 0.098⁎⁎⁎ | 0.098⁎⁎⁎ | 0.094⁎⁎⁎ | 0.098⁎⁎⁎ | 0.098⁎⁎⁎ | 0.096⁎⁎⁎ | 0.093⁎⁎⁎ | ||
| Other | −0.058† | |||||||||||
| Education (HS) | ||||||||||||
| Less than HS | 0.192⁎⁎⁎ | 0.134⁎⁎⁎ | 0.126⁎⁎⁎ | 0.126⁎⁎⁎ | 0.126⁎⁎⁎ | 0.126⁎⁎⁎ | 0.126⁎⁎⁎ | 0.125⁎⁎⁎ | 0.125⁎⁎⁎ | |||
| More than HS | −0.224⁎⁎⁎ | −0.175⁎⁎⁎ | −0.176⁎⁎⁎ | −0.175⁎⁎⁎ | −0.176⁎⁎⁎ | −0.176⁎⁎⁎ | −0.176⁎⁎⁎ | −0.176⁎⁎⁎ | −0.177⁎⁎⁎ | |||
| Employed | −0.637⁎⁎⁎ | −0.627⁎⁎⁎ | −0.627⁎⁎⁎ | −0.626⁎⁎⁎ | −0.627⁎⁎⁎ | −0.627⁎⁎⁎ | −0.627⁎⁎⁎ | −0.626⁎⁎⁎ | ||||
| Income-to-Poverty<1 | 0.206⁎⁎⁎ | 0.153⁎⁎⁎ | 0.152⁎⁎⁎ | 0.152⁎⁎⁎ | 0.153⁎⁎⁎ | 0.153⁎⁎⁎ | 0.152⁎⁎⁎ | 0.152⁎⁎⁎ | ||||
| Married | −0.247⁎⁎⁎ | −0.247⁎⁎⁎ | −0.247⁎⁎⁎ | −0.247⁎⁎⁎ | −0.247⁎⁎⁎ | −0.248⁎⁎⁎ | −0.247⁎⁎⁎ | |||||
| Level 2: State | ||||||||||||
| Economic environment | −0.003 | −0.005 | −0.008 | |||||||||
| Social cohesion | 0.019† | 0.007 | 0.038⁎ | |||||||||
| Sociopolitical orientation | 0.0004 | −0.006 | −0.018 | |||||||||
| Physical infrastructure | 0.010 | 0.013 | −0.004 | |||||||||
| Tobacco environment | 0.018† | 0.022⁎ | 0.030⁎ | |||||||||
| State residual | 0.080⁎⁎⁎ | 0.062⁎⁎⁎ | 0.054⁎⁎⁎ | 0.053⁎⁎⁎ | 0.053⁎⁎⁎ | 0.053⁎⁎⁎ | 0.050⁎⁎⁎ | 0.053⁎⁎⁎ | 0.052⁎⁎⁎ | 0.050⁎⁎⁎ | 0.047⁎⁎⁎ | 0.062⁎⁎⁎ |
Notes: Reference groups in parentheses. In all models, the number of deaths=31,115 and number of person-quarter records=4,972,418. NHW = non-Hispanic white; NHB = non-Hispanic black; HS = high school. Models are not weighted. In the social cohesion model, the p-value for cohesion is 0.060. In the tobacco environment model, the p-value for tobacco is 0.064.
p<0.05. ⁎⁎p<0.01.
p<0.001.
p<0.10.
4. Discussion
Women's mortality varies dramatically between U.S. states. These inequalities are well-documented but poorly understood. Do they reflect differences between states in their residents, contexts, or both? In this study we used a multilevel approach to estimate the contribution of key individual and contextual characteristics to the inequality in women's mortality across states.
Four findings are noteworthy. First, inequalities in women's mortality across states appear to reflect the differential distribution of both individual and contextual characteristics. The individual characteristics we examined accounted for 30%, and the contextual characteristics accounted for 53%, of the variation in women's mortality among states. Accounting for both characteristics explained 62% of the variation and no significant differences between any two states remained. To be clear, this does not imply that the remaining variance in state mortality is zero. As in effectively all empirical analyses, there remains some residual variance in the outcome, which potentially reflects measurement errors and unmeasured factors. When interpreting these percentages, it is important to remember that individual and contextual factors are interrelated in complex ways: individuals and contexts can shape each other. Nonetheless, the results provide compelling evidence that inequalities in women's mortality cannot be reduced to women's personal choices and characteristics; instead, the influence of socioeconomic and political contexts must be considered.
Another important finding is that two of the five contextual features that we examined—social cohesion and economic environment—are particularly important predictors of women's mortality and the between-state variation in women's mortality. Similarly, a multilevel analysis of neighborhoods in England and Scotland (Stafford et al., 2005) found that indicators of social cohesion were especially important for women's self-rated health, followed by economic indicators, with a much smaller role for sociopolitical and physical environments.
Third, the strongest explanation for the cluster of very-low mortality states was a high degree of social cohesion. Interestingly, while states with high cohesion generally had the lowest mortality rates, states with low cohesion did not necessarily have high mortality. In contrast, economic environments may be a better predictor of high mortality.
Fourth, the contextual features we examined appear to have unique and pernicious consequences for women. While differences between states in the personal characteristics of women and men contributed to state variation in mortality to a similar degree, the contextual features explained more than twice the variation in women's mortality than men's mortality. We also found that the specific contextual features that matter most differed between men and women. The states’ social cohesion and economic environment were especially important contributors to mortality inequalities among women, whereas the tobacco environment was most important for men. These findings corroborate extant studies that find social structural factors play a larger role in shaping women's than men's health, while behavioral factors are crucial for men's health (e.g., (Denton & Walters, 1999). They also make sense given that many state policies are inherently more relevant for women. For example, state policies that shape access to health care, prenatal care, affordable housing, children's health care, subsidized school lunches, family leave, and financial safety nets are especially important for women given that they are more likely than men to be socioeconomically-disadvantaged, raising children, caring for aging parents, interfacing with the health care system, and employed in unstable and low-paying jobs. Our finding that state contexts appear to be relatively more important for women than men is consistent with several studies examining gender differences in contextual effects on health (e.g., Robert & Reither, 2004; Stafford et al., 2005).
One interpretation of our findings is that raising social cohesion may be a promising way to lower mortality rates and inequalities, particularly among women. This idea is not far-fetched. In recent decades, Canada and Australia have launched efforts to enhance social cohesion. Raising cohesion may require coordinated efforts at state and local levels. It may require multiple strategies, such as lowering unemployment and income inequality (although debate persists about the causal influence of income inequality on health and mortality (Pickett & Wilkinson, 2015)), reducing commute times, and building safe public spaces. In addition, expanding opportunities for individuals to acquire personal resources, such as education, may be needed. Furthermore, because individuals and contexts can shape each other, strategies that focus on both states and individuals may be most effective. As others have noted (Macintyre et al., 2002), while focusing exclusively on one “level” may be sufficient in certain situations, most evidence suggests it is counter-productive.
4.1. Limitations
Our study has some limitations. First, the NLMS does not contain life course information such as employment and marital histories. It also masks temporal information, such as survey year, and does not contain mortality information after 2002. Third, it does not contain respondents’ migration histories. However, prior studies find that interstate migration is unrelated to older women's health and education (Halliday & Kimmitt, 2008) and that migration does not bias estimates of area-level health and mortality (Ezzati et al., 2008, Geronimus et al., 2014). To the extent that migration occurred among our sample, it would likely cause our state-level estimates to be conservative. Nonetheless, the strengths of the NLMS greatly outweigh its limitations for addressing our aims.
We did not include intervening mechanisms, such as health behaviors, on the pathway between socioeconomic resources and mortality. This strategy reflects our focus on “fundamental” socioeconomic determinants of mortality (Link & Phelan, 1995). Their importance is reflected in our finding that no significant differences in women's mortality between any two states remained after adjusting for the factors in our study. Similarly, a multilevel U.K. study found that individuals’ socioeconomic characteristics and neighborhood characteristics fully explained neighborhood variation in health (Stafford et al., 2005). Ultimately, socioeconomic resources shape mortality through myriad, proximate risks such as health behaviors and biological mechanisms. These are beyond the scope of our study and not available in the NLMS.
Despite the compelling reasons for examining the state level, one drawback is that our analysis does not capture heterogeneity within states. A complete explanation for the inequalities will require triangulating results across levels of analysis. It is important to note that smaller geographic levels have drawbacks as well. For instance, inter-county migration is more frequent than inter-state migration, and adults often live and work in different counties.
Future studies should examine whether the importance of states’ characteristics depends on personal characteristics. While extant evidence for interactions between contextual and individual characteristics on mortality rates is modest and inconsistent (Subramanian et al., 2001, Chetty et al., 2016), understanding how the two levels of factors interact is important for designing interventions and policy changes.
4.2. Conclusions
Large inequalities in mortality between U.S. states are well-documented but poorly understood. Our findings highlight the importance of ‘bringing context back in’ (Diez-Roux, 1998) when investigating these inequalities. Geographic inequalities in women's mortality cannot be reduced to women's personal characteristics; the influence of socioeconomic and political contexts must be considered. Our findings imply that divergent social and economic policies across states have played an important role in shaping the inequalities in women's mortality.
Acknowledgments
This study was funded in part by the Fund for the Advancement of the Discipline Award supported by the American Sociological Association and the National Science Foundation (PI: Jennifer Karas Montez); grants R24AG045061 (PI: James P. House) and 1 R01 AG040248-02 (PI: Lisa F. Berkman) from the National Institute on Aging; and grant 5 R24 HD042849 (PI: Mark D. Hayward) awarded to the Population Research Center at The University of Texas at Austin by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The authors thank three anonymous reviewers for their helpful and insightful comments.
Footnotes
Supplementary data associated with this article can be found in the online version at http://dx.doi.org/10.1016/j.ssmph.2016.07.004.
Contributor Information
Jennifer Karas Montez, Email: jmontez@maxwell.syr.edu.
Anna Zajacova, Email: zajacova@uwyo.edu.
Mark D. Hayward, Email: mhayward@prc.utexas.edu.
Appendix A. Supplementary material
Supplementary material
References
- Arcaya M., Brewster M., Zigler C.M., Subramanian S.V. Area variations in health: a spatial multilevel modeling approach. Health Place. 2012;18:824–831. doi: 10.1016/j.healthplace.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrell C., Paléncia L., Muntaner C., Urquía M., Maimusi D. Influence of macrosocial policies on women’s health and gender inequalities in health. Epidemiologic Reviews. 2014;36:31–48. doi: 10.1093/epirev/mxt002. [DOI] [PubMed] [Google Scholar]
- Chetty R., Stepner M., Abraham S., Lin S., Scuderi B. The association between income and life expectancy in the United States, 2001–2014. JAMA. 2016;315:1750–1766. doi: 10.1001/jama.2016.4226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denton M., Walters V. Gender differences in structural and behavioral determinants of health: an analysis of the social production of health. Social Science & Medicine. 1999;48:1221–1235. doi: 10.1016/s0277-9536(98)00421-3. [DOI] [PubMed] [Google Scholar]
- Diez Roux A.V. The examination of neighborhood effects on health: Conceptual and methodological issues related to the presence of multiple levels of organization. In: Kawachi I., Berkman L.F., editors. Neighborhoods and health. Oxford University Press, Inc.; New York: 2003. pp. 45–64. [Google Scholar]
- Diez-Roux A.V. Bringing context back into epidemiology: a variables and fallacies in multilevel analysis. American Journal of Public Health. 1998;88:216–222. doi: 10.2105/ajph.88.2.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn J.R., Burgess B., Ross N.A. Income distribution, public services expenditures, and all cause mortality in U.S. states. Journal of Epidemiology & Community Health. 2005;59:768–774. doi: 10.1136/jech.2004.030361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezzati M., Friedman A.B., Kulkarni S.C., Murray C.J.L. The reversal of fortunes: trends in county mortality and cross-county mortality disparities in the United States. PLoS Medicine. 2008;5:0557–0568. doi: 10.1371/journal.pmed.0050066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenelon A. Geographic divergence in mortality in the United States. Population and Development Review. 2013;39:611–634. doi: 10.1111/j.1728-4457.2013.00630.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus A.T., Bound J., Ro A. Residential mobility across local areas in the United States and the geographic distribution of the healthy population. Demography. 2014;51:777–809. doi: 10.1007/s13524-014-0299-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halliday T.J., Kimmitt M.C. Selective migration and health in the USA, 1984-93. Population Studies. 2008;62:321–334. doi: 10.1080/00324720802339806. [DOI] [PubMed] [Google Scholar]
- Herian M.N., Tay L., Hamm J.A., Diener E. Social capital, ideology, and health in the United States. Social Science & Medicine. 2014;105:30–37. doi: 10.1016/j.socscimed.2014.01.003. [DOI] [PubMed] [Google Scholar]
- Kawachi I., Kennedy B.P., Lochner K., Prothro-Stith D. Social capital, income inequality, and mortality. American Journal of Public Health. 1997;87:1491–1498. doi: 10.2105/ajph.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I., Kennedy B.P., Gupta V., Prothrow-Stith D. Women’s status and the health of women and men: a view from the states. Social Science & Medicine. 1999;48:21–32. doi: 10.1016/s0277-9536(98)00286-x. [DOI] [PubMed] [Google Scholar]
- Kennedy B.P., Kawachi I., Prothrow-Stith D. Income distribution and mortality: Cross sectional ecological study of the Robin Hood Index in the United States. British Medical Journal. 1996;312:1004–1007. doi: 10.1136/bmj.312.7037.1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kindig D.A., Cheng E.R. Even as mortality fell in most U.S. counties, female mortality nonetheless rose in 42.8 percent of counties from 1992 to 2006. Health Affairs. 2013;32:451–458. doi: 10.1377/hlthaff.2011.0892. [DOI] [PubMed] [Google Scholar]
- Link B.G., Phelan J.C. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995:80–94. (extra issue) [PubMed] [Google Scholar]
- Macintyre S., Ellaway A. Neighborhoods and health: an overview. In: Kawachi I., Berkman L.F., editors. Neighborhoods and health. Oxford University Press; New York: 2003. [Google Scholar]
- Macintyre S., Ellaway A., Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Social Science & Medicine. 2002;55:125–139. doi: 10.1016/s0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- Montez J.K., Berkman L.F. Trends in the educational gradient of mortality: Bringing regional context into the explanation. American Journal of Public Health. 2014;104:e82–e90. doi: 10.2105/AJPH.2013.301526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez J.K., Zajacova A. Explaining the widening education gap in mortality among U.S. White women. Journal of Health and Social Behavior. 2013;54:165–181. doi: 10.1177/0022146513481230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan K.O.L., Morgan S., editors. State rankings 2013. A statistical view of America. SAGE and CQ Press; Los Angeles: 2013. [Google Scholar]
- Murray C.J.L., Kulkarni S.C., Michaud C., Tomijima N., Bulzacchelli M.T. Eight Americas: investigating mortality disparities across race, counties, and race-counties in the United States. PLoS Medicine. 2006;3:e260. doi: 10.1371/journal.pmed.0030260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L. K., & Muthén B. O. (2012). Mplus Version 7.0. 〈http://www.statmodel.com/-2012〉.
- Navarro V., Shi L. The political context of social inequalities and health. Social Science & Medicine. 2001;52:481–491. doi: 10.1016/s0277-9536(00)00197-0. [DOI] [PubMed] [Google Scholar]
- Newman K.S., O’Brien R.L. University of California Press; Berkelely, Los Angeles, CA: 2011. Taxing the poor: Doing damage to the truly disadvantaged. [Google Scholar]
- Osler M., Christensen U., Lund R., Gamborg M., Godtfredsen N. High local unemployment and increased mortality in Danish adults: Results from a prospective multilevel study. Occupational and Environmental Medicine. 2003;60:e16. doi: 10.1136/oem.60.11.e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel S.A., Narayan K.M.V., Ali M.K., Mehta N.K. Interstate variation in modifiable risk factors and cadiovascular mortality in the United States. PLoS One. 2014;9:e101531. doi: 10.1371/journal.pone.0101531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett K.E., Wilkinson R.G. Income inequality and health: a causal review. Social Science & Medicine. 2015;128:316–326. doi: 10.1016/j.socscimed.2014.12.031. [DOI] [PubMed] [Google Scholar]
- Putnam R. D. (2000). Bowling alone. The collapse and revival of American community. New York: Simon & Schuster Paperbacks. Social Capital Index for U.S. States
- Ramírez de Arellano A.B., Wolfe S.M. Public Citizen Health Research Group; Washington DC: 2007. Unsettling scores: A ranking of state Medicaid programs. [Google Scholar]
- Robert S.A., Reither E.N. A multilevel analysis of race, community disadvantage, and body mass index among adults in the US. Social Science & Medicine. 2004;59:2421–2434. doi: 10.1016/j.socscimed.2004.03.034. [DOI] [PubMed] [Google Scholar]
- Rogot E., Sorlie P. D., & Johnson N. J. (1992). A mortality study of 1.3 million persons by demographic, social and economic factors: 1979-1985 follow-up. Second data book. NIH Publication No 92-3297 ed. National Institutes of Health, PHS, DHHS
- Solar O., Irwin A. World Health Organization; Geneva: 2010. A conceptual framework for action on the social determinants of health. Social determinants of health discussion paper 2 (policy and practice) [Google Scholar]
- Stafford M., Cummins S., Macintyre S., Ellaway A., Marmot M. Gender differences in the association between health and neighborhood environment. Social Science & Medicine. 2005;60:1681–1692. doi: 10.1016/j.socscimed.2004.08.028. [DOI] [PubMed] [Google Scholar]
- Subramanian S.V., Kawachi I., Kennedy B.P. Does the state you live in make a difference? Multilevel analysis of self-rated health in the US. Social Science & Medicine. 2001;53:9–19. doi: 10.1016/s0277-9536(00)00309-9. [DOI] [PubMed] [Google Scholar]
- Subramanian S.V., Jones K., Kaddour A., Krieger N. Revisting Robinson: the perils of individualistic and ecologic fallacy. International Journal of Epidemiology. 2009;38:342–360. doi: 10.1093/ije/dyn359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tencza C., Stokes A., Preston S. Factors responsible for mortality variation in the United States: a latent variable analysis. Demographic Research. 2014;31:27–70. doi: 10.4054/DemRes.2014.31.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson R.G. Routledge; London: 1996. Unhealthy societies: The afflictions of inequality. [Google Scholar]
- Wilmoth J.R., Boe C., Barbieri M. Geographic differences in life expectancy at age 50 in the United States compared with other high-income countries. In: Crimmins E.M., Preston S.H., Cohen B., editors. International differences in mortality at older ages: Dimensions and sources. The National Academies Press; Washington DC: 2011. pp. 333–366. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material