Abstract
Purpose
Lenalidomide, thalidomide, and pomalidomide (LTP) are immunomodulatory agents approved for use in multiple myeloma, but in some settings, especially with alkylating agents, an increase in Hodgkin’s lymphoma (HL) and other secondary primary malignancies (SPM) has been noted. Some of these malignancies have been linked to Epstein-Barr virus (EBV), raising the possibility that immunomodulatory drugs disrupt latent EBV infection.
Experimental Design
We studied the ability of LTP to reactivate latently infected EBV-positive cell lines in vitro and in vivo, and evaluated the EBV viral load in archived serum samples from patients who received a lenalidomide, thalidomide and dexamethasone (LTD) combination.
Results
Treatment of EBV-infected B-cell lines with LTP at physiologically relevant concentrations induced the immediate early gene BZLF1, the early gene BMRF1, and the late proteins VCA and BCFR1. This occurred in the potency order pomalidomide>lenalidomide>thalidomide, and the nucleoside analogue ganciclovir enhanced the cytotoxic effects of lenalidomide and pomalidomide in Burkitt’s lymphoma cells in vitro and in vivo. EBV reactivation was related to phosphatidylinositol-3 kinase (PI3K) stimulation and Ikaros suppression, and blocked by the PI3K-δ inhibitor idelalisib. Combinations of lenalidomide with dexamethasone or rituximab increased EBV reactivation compared to lenalidomide alone and, importantly, lenalidomide with melphalan produced even greater reactivation
Conclusions
We conclude LTP may reactivate EBV-positive resting memory B-cells thereby enhancing EBV lytic cycle and host immune suppression.
Keywords: EBV, lenalidomide, thalidomide, pomalidomide
Introduction
The immunomodulatory drugs lenalidomide (LEN), thalidomide (THAL), and pomalidomide (POM) (together, LTP) have contributed to an improvement in survival in multiple myeloma (MM) patients (1). Consequently, they have become part of the backbone of many therapeutic regimens in the upfront, relapsed, and relapsed/refractory settings. Moreover, LEN is now included in maintenance therapy (MT) in both transplant-eligible and -ineligible populations (2–4).
While the efficacy of LTP is without question, concern has arisen about a possible increase in secondary primary malignancies (SPMs). This has been seen with maintenance after melphalan-based high-dose chemotherapy and autologous stem cell transplant (SCT)(2, 3), or following melphalan-based induction therapy (4). Interestingly, LEN maintenance increased the incidence of Hodgkin’s lymphoma (HL) in two studies, an uncommon SPM seen in MM patients. Indeed, Attal and colleagues reported four HL cases in MM patients who had undergone SCT and none in the placebo group (2), whilst McCarthy reported one case (3). Moreover, a retrospective analysis of three phase III trials in relapsed MM patients demonstrated an SPM incidence of 4% in patients who received LEN versus 1.4% in those who received placebo (5).
One possible reason for the development of HL as an SPM is reactivation of Epstein-Barr virus (EBV). This oncogenic gamma herpes virus is associated with, and contributes to the development and maintenance of a variety of human malignancies, including HL, Burkitt’s lymphoma (BL), and post-transplant lymphoproliferative disease (PTLD)(6). Primary infection occurs during childhood, and lifelong infection is maintained latently in resting memory B-cells, with occasional viral reactivation. In the absence of immune control, such as in patients who undergo SCT, loss of EBV control can give rise to PTLD (7). The use of HYPER-CVAD regimens in leukemia and lymphoma patients, and methotrexate (MTX) use in patients with autoimmune disease, increases the incidence of EBV-positive lymphomas (8, 9). It is also interesting to note that LEN-MT in relapsed/refractory MM patients following allograft SCT induced herpes virus reactivation (EBV and herpes simplex virus) requiring acyclovir prophylaxis (10). In contrast, chemotherapeutics such as doxorubicin (DOX) or gemcitabine have been shown to reactivate EBV from a latent infection in EBV-positive malignancies to a lytic infection, which has led to clinically significant regression of EBV-positive tumors (11). Hence the ability of chemotherapy agents to induce lytic EBV infection can be a therapeutic modality for EBV-positive malignancies in combination with the nucleoside analogue ganciclovir (GCV), or it could give rise to secondary EBV-positive malignancies in immunocompromised hosts. These possibilities drove us to determine whether LEN reactivates the EBV lytic cycle, which could sensitize tumor cells to the effects of GCV and/or contribute to the development of HL as an SPM.
Here we show that LTP reactivated lytic EBV infection in latently infected BL cell lines. This reactivation was responsible for sensitization of the cells to GCV and enhanced the efficacy of LEN in a BL xenograft. LTP reactivated EBV through the stimulation of phosphatidylinositol 3-kinase (PI3K) and suppression of Ikaros, whilst the combination of LEN with dexamethasone (DEX) and rituximab (RTX), as well as with melphalan, enhanced EBV-reactivation. Taken together, these data provide a potential mechanism through which LEN can drive reactivation of EBV to a lytic form, and this may contribute to the increased incidence of HL in the post-SCT/LEN maintenance setting.
Materials and Methods
Reagents
LEN was from Celgene (Summit, NJ), whilst THAL, POM, idelalisib, LY294002, SB202190, PD98059, and DEX were purchased from Selleck Chemicals (Houston, TX). DOX, melphalan (MLPH), and GCV were purchased from Sigma-Aldrich (St. Louis, MO) as were MTX and bortezomib (BZB). RTX was from The MD Anderson Cancer Center Pharmacy (Houston, TX). All drugs were dissolved in DMSO, except for MLPH, which was dissolved in ethanol, and RTX, which was in 0.9% sodium chloride.
Cell culture and patient samples
MUTU-I and KEM-I (gifts from Alan Rickinson and Jeff Sample, UK) are EBV+ BL cell lines. The EBV+ BL cell line DAUDI and the lymphoblastoid cell line (LCL) B95.8 were from the ATCC (Manassas, VA), while the donor 4 (D4-WT) LCL and BZLF-1 deleted LCL (D4-ZKO) were described previously (12). All lines were validated through The MD Anderson Cancer Center Characterized Cell Line Core Facility. Cells were grown in RPMI-1640 (Life Technologies; Carlsbad, CA) with 10% fetal bovine serum, 100 U/mL penicillin, and 100 µg/mL streptomycin (Sigma-Aldrich). Archived serum samples were sourced from myeloma patients enrolled in a phase I/II clinical trial (13) which was in compliance with the Declaration of Helsinki according to an Institutional Review Board-approved protocol.
Immunoblotting
Protein expression was measured by immunoblot analysis as previously described (14). The antibody to BZLF-1 was from Santa Cruz Biotechnologies (Santa Cruz, CA), while the anti-AKT, phospho (p)-GSK3α/βSer21/9, p-AKTSer473, FoxO1 and Ikaros antibodies were from Cell Signaling Technology (Danvers, MA). Antibody to BMRF1 was obtained from Millipore (Billerica, MA), anti-β-actin from Sigma-Aldrich, and anti-VCA p18 antibodies were from Thermo-Scientific (Waltham, MA). Total AKT and pAKTSER473 levels were also measured using sandwich ELISA kit as recommended by the manufacturer Cell Signaling Technology.
Cell proliferation assay
The WST-1 tetrazolium reagent from Roche (Indianapolis, IN) was used to determine effects on cell proliferation. Viable cell numbers (Annexin-V- and TO-PRO-3-negative) were measured using Annexin-V-Pacific Blue and TO-PRO-3 (Life Technologies; Grand Island, NY) in combination with Count Bright Beads on a Fortessa flow cytometer (Becton-Dickson; Franklin Lakes, NJ) using FlowJo, version 10 (Tree Star, Inc.; Ashland, OR).
Blockade of PI3K signaling
DAUDI cells were pretreated for 1 hour with DMSO alone or with LY294002, PD98059, SB202190, idelalisib and in combination with LTP for 48 hours.
Lentiviral overexpression of Ikaros
MUTU-I cells were infected with a Lentivirus encoding Ikaros or a control virus as previously described (15).
In vivo xenograft
Experiments were performed in accordance with protocols approved by the institutional Animal Care and Use Facility. CB-17 severe combined immunodeficiency (SCID) mice (Harlan Laboratories, Inc.; Indianapolis, IN) were inoculated in the right flank subcutaneously with 5 × 106 MUTU-I cells. When tumor burdens reached ~100 mm3 in volume, mice were randomized into groups of 5 mice to receive intraperitoneal vehicle (phosphate-buffered-saline (PBS)) daily, LEN daily, GCV thrice weekly, or both agents.
Quantitative real time PCR (qPCR) and semi-quantitative reverse-transcription PCR (RT-PCR) analysis
Total RNA harvested from cells was reverse transcribed as previously described (16). cDNA was subjected to PCR using primers and conditions for BZLF1, BCRF1, and β2M as previously published (16, 17). qPCR for BGLF-4 was performed on a StepOne PCR analyzer (Applied Biosystems) using SYBR Green master mix (Life Technologies) with sense primer 5’-TGACGGAGCTGTATCACGAG-3’ and antisense primer 5’-CCAGGGGCTCAATACTACCA-3’ based on the GenBank EBV sequence: AJ507799.2. EBV viral load in serum samples was measured using the EBV R-gene™ kit (Argene; Lombard, IL) according to the manufacturer’s instructions.
Drug synergy assays
To detect the presence of synergistic interactions, the methods of Chou and Talalay were used (18). Data were analyzed using CalcuSyn Version 2 software (Biosoft), and combination indices (CIs) calculated.
Statistical analyses
Data were subjected to statistical analyses using the standard error of the mean (SEM). The significance of drug-effect relationships was determined by one-tailed unpaired t tests using Excel software (Microsoft Corporation; Redmond, WA), and results were considered significant when p<0.05. For in vivo studies, an analysis of co-operative effects of LEN and GCV on tumor growth was performed using a Bayesian bootstrapping approach (19). Linear mixed-effect models were used to study the change of EBV viral load over time in patient serum samples and the effects of valacyclovir (VTX) treatment. An unstructured covariance model was used to account for inter-patient variability and the longitudinal nature of the data. The transformation of logarithm to the base 10 of the EBV viral load was used in the analyses to satisfy the normality assumption of the models. SAS version 9.2 and S-Plus version 8.04 (SAS Institute; Cary, NC) were used to carry out the computations for all analyses.
Results
Immunomodulatory agents reactivate latent EBV infection
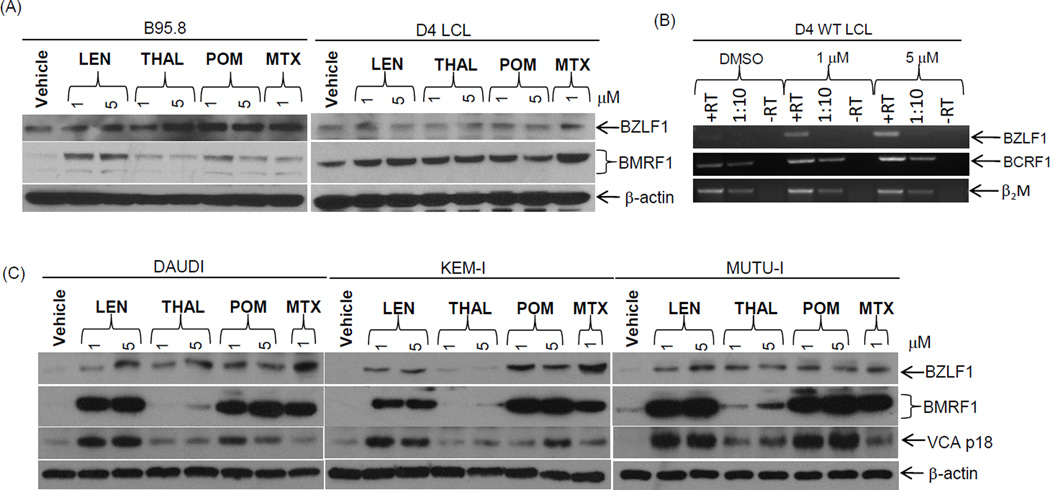
We sought to determine if LTP induced EBV reactivation in latently infected LCL and BL cell lines. Clinically relevant concentrations (20–22) of LTP weakly enhanced expression of the immediate early gene product BZLF1, and the early viral gene product BMRF1 in B95.8 and D4 LCL cells (Figure 1A). RT-PCR analysis also showed a dose-dependent increase in BZLF1 transcription and induction of BCRF1 (viral IL-10), a marker of the late stages of EBV replication with LEN treatment (Figure 1B). In contrast, the BL cell lines DAUDI, KEM-I, and MUTU-1 showed robust BMRF1 and BZLF1 induction, along with the expression of the late protein, VCA (Figure 1C). BMRF1 induction was similar with 1 and 5 µM LEN and POM, and equivalent to MTX, a known EBV reactivation inducer (9). POM was particularly effective in DAUDI and KEM-I, followed by LEN and THAL (Figure 1C). This potency in reactivating EBV parallels the known clinical efficacy of these agents in multiple myeloma(23).
Figure 1. Immunomodulatory agents reactivate lytic EBV infection.
(A) B95.8 and D4 LCL cell lines were treated for 48 hours with vehicle, LTP, or MTX as a positive control, and extracts were immunoblotted with the indicated antibodies. (B) Reverse-transcriptase (RT) PCR on D4 LCLs following treatment with LEN for 48 hours with primers for BZLF1, BCRF1, and a loading control using β2M or a 1:10 dilution of the cDNA. (C) The EBV+ BL cell lines DAUDI, KEM-I and MUTU-I were treated as above. Protein levels of BZLF1, BMRF1 and VCA, along with β-actin as a loading control, were determined. Representative images are shown from 1 of 3 independent experiments.
EBV lytic cycle induction by LEN and POM enhances their activity in BL and LCL cells
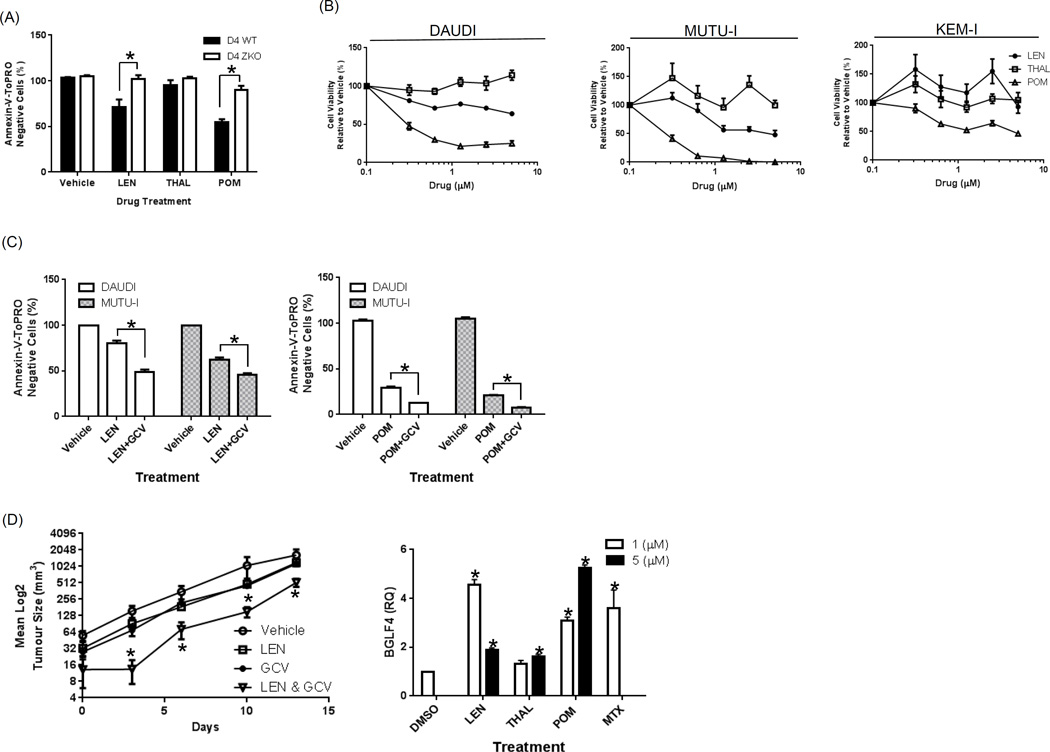
To determine the contribution of the EBV lytic cycle to the cytotoxic effects of immunomodulatory drugs, we evaluated D4 cells bearing wild-type (WT) EBV or D4 cells transformed using a BZLF1 gene-deleted (D4-ZKO) EBV, rendering them incapable of entering lytic cycle. Treatment of WT LCLs with LTP reduced the viable cell number to 60% with LEN, 90% with THAL, and 50% with POM (Figure 2A), but the ZKO LCL cells displayed little to no change in viability with LEN and THAL, whilst POM only reduced viability 10% (Figure 2A). We next evaluated the effect of LTP on DAUDI, MUTU-I and KEM-I. POM was the most effective in suppressing DAUDI and MUTU-I proliferation, with IC50’s of 0.3 and 0.25 µM, respectively, while the KEM-I IC50 plateaued at approximately 1–3 µM (Figure 2B). LEN in the three lines did not achieve an IC50, but did reduce proliferation to 75% in DAUDI at 0.6 µM and 53% in MUTU-I cells at 1 µM (Figure 2B). LEN had no significant effect in KEM-I, whilst THAL had no significant effect in any of them (Figure 2B).
Figure 2. EBV lytic cycle enhances growth inhibition in response to LEN and POM and synergize with GCV in SCID mice.
(A) LCL cells bearing a wild-type EBV (D4 WT) or a BZLF1-deleted EBV (D4 ZKO) were treated with LTP (1 µM) or vehicle for 1 week. Flow cytometric analysis was then performed after staining with Annexin-V/TO-PRO-3 and Count Bright beads, from which the viable cell number was calculated and normalized to the vehicle control group. (B) BL cell lines were treated for 4 days with LEN, THAL, POM or vehicle, cell viability was determined using the WST-1 reagent, and results were expressed as the percentage viability relative to the vehicle control, which was arbitrarily set at 100%. (C) DAUDI and MUTU-I cells were treated for 1 week with either LEN (1 µM) or POM (0.25 µM) alone, or in combination with GCV (50 µM). Annexin-V/TO-PRO-3 and Count Bright bead flow cytometry were used to determine the viable cell numbers. Values represent the mean +/− the standard error of the mean from 3 independent experiments. An unpaired t-test was performed to evaluate for significance and “*” denotes p values of <0.01. (D) SCID mice were inoculated with MUTU-I cells subcutaneously and monitored until tumors were established. Five mice per group were injected intraperitoneally with vehicle, LEN (50 mg/kg) daily, GCV (50 mg/kg) three times per week, or the combination. Tumor volumes were measured and are plotted as a function of time for each group. Statistically significant differences comparing the combination to the single agents were determined using an unpaired t-test, and a p value of <0.02 is indicated by “*”. MUTU-I was treated with DMSO, LTP at 1 or 5 µM or 1 µM MTX as a positive control for 48 hours. RNA was harvested and cDNA synthesized and qPCR performed for BGLF-4 with RQ values normalized to the DMSO control. An unpaired t-test was performed to evaluate for significance and “*” denotes p values of <0.05 relative to the DMSO control.
As we cannot introduce a BZLF1-deleted EBV into BL cells because these cells harbor an endogenous WT EBV, we next evaluated whether LEN and POM stimulated the lytic cycle enough to result in conversion of GCV to its active triphosphate form. This can then compete with deoxyguanosine triphosphate (dGTP) and be inserted into the cellular DNA, leading to apoptosis of the infected cells (24). DAUDI and MUTU-I cells were treated with LEN (Figure 2C, left panel) or POM (Figure 2C, right panel) alone or in combination with 50 µM GCV, and the live cell number determined using Annexin-V/TO-PRO-3 exclusion fluorescence-activated cell sorting. LEN alone reduced the DAUDI live cell population to 80%, but LEN with GCV reduced the live cell number to 49%. In MUTU-I cells, LEN reduced the live cell number to 62% alone, and to 45% with GCV (Figure 2C, left panel). Similarly, the combination of POM and GCV in DAUDI cells reduced the live cell fraction to 12% versus 30% with POM alone. MUTU-I cells were even more sensitive to the combination, with a reduction of the live cells to 8% versus 21% for POM alone (Figure 2C, right panel).
To determine the presence of any synergistic interactions with varying LTP and GCV concentrations, we performed synergy assays with DAUDI, MUTU-I and KEM-I treated with LTP or GCV alone, or in combination with GCV. DAUDI cells demonstrated an enhanced suppression of cell growth with LTP in combination with GCV with concentrations as low as 0.4 µM LEN or POM and 4 µM GCV. In comparison, 10 µM THAL with 100 µM GCV actually overcame the stimulation of growth observed with THAL (Supplemental Figure 1A). KEM-I cells demonstrated less growth suppression, with LEN and POM both requiring 10 µM in combination with 100 µM GCV, while no activity was present with THAL and GCV (Supplemental Figure 1B). MUTU-I cells, in contrast, showed an enhanced suppression of cell growth with LTP and GCV at a range of concentrations, with POM and GCV being particularly effective, whilst THAL and GCV overcame the growth stimulation of THAL (Supplemental Figure 1C). Isobologram analysis was performed to determine if these interactions were synergistic as defined by Chou and Talalay (18). MUTU-I treated with LEN and GCV demonstrated synergy at all the concentrations used, with CI values ranging from 0.031 to 0.314. Similarly, POM and GCV were also highly synergistic across the concentrations, with CIs of 0.02–0.55. In comparison, only 0.4 µM THAL and 4 µM GCV showed synergy, with a CI of 0.141 (Supplemental Table 1). POM and GCV were also synergistic against KEM-I across the concentration ranges used, with CIs of 0.03–0.2 (Supplemental Table 1). In DAUDI cells, POM with GCV at the lowest concentrations were synergistic, with CIs of 0.027–0.670, whereas LEN and GCV were synergistic to additive, with CIs of 0.417–1.154. Note that no CIs are shown for LEN and THAL with KEM-I, or THAL with DAUDI, as the single agents had no change in viability or stimulated growth (i.e. cell viability over 100%), which precludes isobologram analysis (Supplemental Table 1). These data show that EBV lytic cycle induction is in part responsible for the anti-proliferative effects of LEN and POM in LCLs, and to a greater extent in BL cell lines.
LEN in combination with GCV enhances the therapeutic effect in vivo
In order to determine if EBV lytic cycle induction is sufficient to result in effects in vivo, we established MUTU-I xenografts and treated them with vehicle, LEN daily, GCV thrice weekly, or the combination. LEN and GCV alone each had a slight effect on suppressing MUTU-I tumor growth (Figure 2D), but statistical analysis showed this effect was not significant. In contrast, the LEN and GCV combination inhibited tumor growth, with tumor volumes from day 3 of treatment onwards being significantly smaller compared to the vehicle, or LEN or GCV alone (Figure 2D). For each time point comparing the LEN & GCV combination to single agents, p values were <0.02 (Supplemental Table 2), with no significant differences between LEN or GCV alone. An analysis of the cooperative effects of LEN and GCV found, from day 3 onwards, the posterior probability of co-operative effect was equal to 1, meaning there was a 0 in 10,000 chance that the combination did not have a cooperative effect. To confirm that LTP stimulate the BGLF-4 kinase responsible for phosphorylating GCV to its active form in EBV-positive cells (25), we treated MUTU-I for 48 hours with LTP or MTX and performed qPCR for BGLF-4. LEN and POM at concentrations as low as 1 µM stimulated a four- and five-fold increase in BGLF-4, respectively. Interestingly, the 5 µM concentration actually induced less BGLF-4 with both LEN and POM, whilst THAL induced minimal BGLF-4 at the two concentrations used (Figure 2D, right panel).
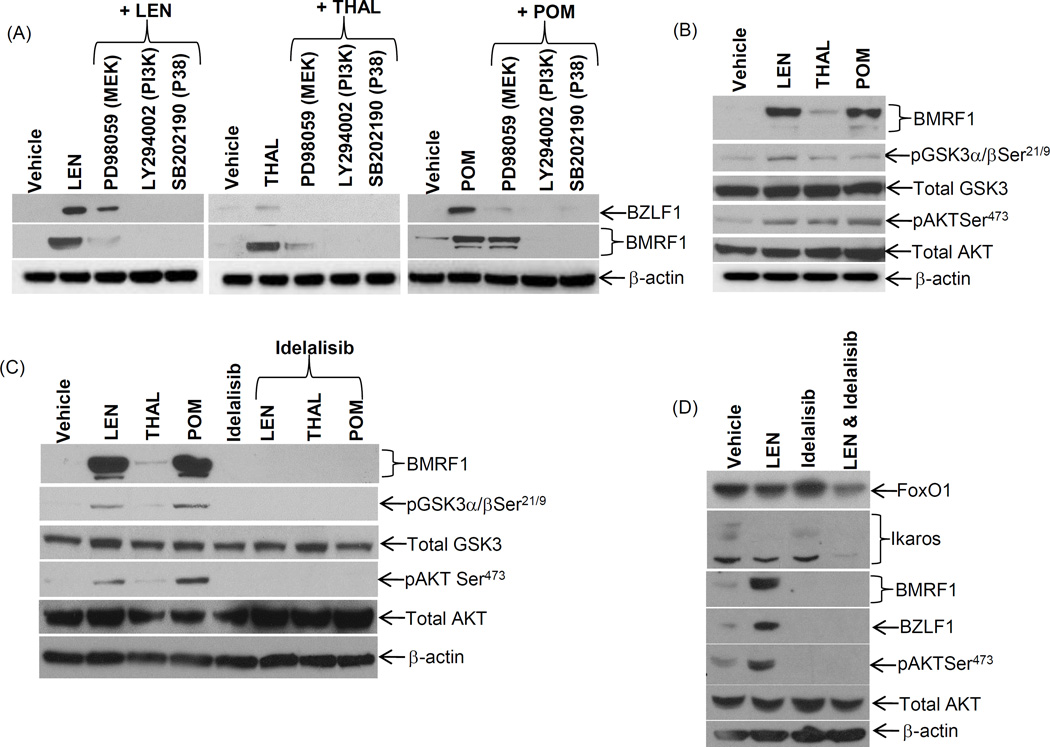
Blockade of PI3K signaling suppresses LEN-induced EBV reactivation
EBV-reactivation by chemotherapy agents is mediated through stimulation of PI3K, mitogen-activated protein kinase (MAPK) kinase (MEK), and p38-MAPK signaling (26–28). We therefore assessed the effects of MEK, PI3K, and p38-MAPK inhibitors in combination with LTP on EBV-reactivation. LTP were unable to consistently induce BMRF1 or BZLF1 in the presence of LY294002 or SB202190, whereas the MEK inhibitor had a limited effect on reactivation (Figure 3A). The induction of the EBV lytic cycle by LTP also coincided with stimulation of PI3K signaling, as evidenced by enhanced expression of phospho-Glycogen synthase kinase (GSK) 3α/βSer21/9 and Protein kinase B/AKTSer473 (Figure 3B).
Figure 3. Inhibition of PI3 kinase suppresses LEN induced EBV reactivation.
(A) DAUDI cells were incubated with vehicle, LTP (5 µM), or in combination with inhibitors of MEK (PD98059; 50 µM), PI3K (LY294002; 15 µM), or p38 (SB202190; 20 µM) for 48 hours, and immunoblotted with the indicated sera. (B) Immunoblotting of DAUDI cells treated with LTP (5 µM) was performed for markers of PI3K activation and EBV reactivation. (C) DAUDI cells were treated with LTP (5 µM) alone or in combination with the PI3Kδ subunit inhibitor idelalisib (1 µM) for 48 hours, and lysates probed for PI3K activation markers and EBV reactivation markers. (D) DAUDI cells were treated with LEN (5 µM), idelalisib (1 µM) or the combination for 24 hours and immunoblotted for the markers of PI3K activation, EBV reactivation, FoxO1 and Ikaros. Representative images are shown from 1 of 3 independent experiments.
Suppression of EBV-reactivation using SB202190 or LY294002 may be an off-target effect as these inhibitors have a broad range of mechanisms, including suppression of casein kinase 1 and nuclear factor kappa B, which may influence EBV-reactivation. We therefore evaluated idelalisib, a highly specific PI3K-p110δinhibitor (29). Treatment of DAUDI cells with LEN and POM induced significant BMRF1 expression, and enhanced pGSK3α/βSer21/9 and pAKTSer473 levels (Figure 3C). In contrast, concomitant addition of a clinically relevant concentration of idelalisib completely suppressed stimulation of BMRF1, pGSK3α/βSer21/9, and pAKTSer427 (Figure 3C). LTP may also regulate EBV reactivation through PI3K-mediated suppression of the transcription factor Forkhead-box-O1 (FoxO1), which if suppressed leads to loss of Ikaros (30), an EBV latency regulator (15). Treatment of DAUDI cells with LEN slightly decreased FoxO1 and depleted Ikaros, leading to the enhancement of BZLF1 and BMRF1 and the induction of pAKTSer473 (Figure 3D). The addition of idelalisib with LEN led to a further depletion of Ikaros and greater suppression of FoxO1. This was in contrast to treatment with idelalisib alone, which actually enhanced FoxO1 and did not have any effect on Ikaros. These data confirm the role of PI3K stimulation by LTP in EBV reactivation.
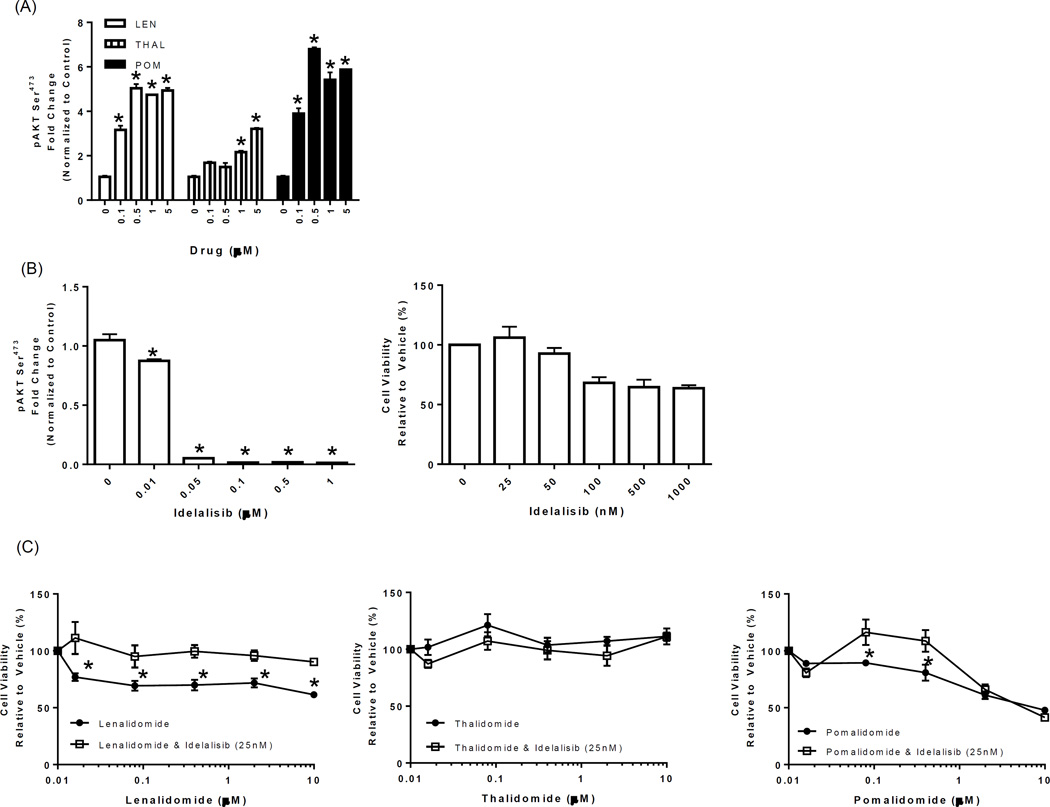
LTP display differential abilities to stimulate PI3K
To further understand the varying ability of LTP to stimulate EBV reactivation, we evaluated the ability of different LTP concentrations to increase PI3K signaling as measured by a pAKTSER473 ELISA and the effect of idelalisib on blocking the lytic cycle as it relates to cell viability. LEN and POM concentrations as low as 0.1 µM increased pAKTSER473 3- to 3.5-fold, respectively, compared with vehicle controls. At 0.5 µM, this effect increased to 5-fold with LEN and 7-fold with POM, remaining stable at concentrations of up to 5 µM (Figure 4A). In contrast, THAL did not increase pAKTSER473 significantly at low concentrations. At 1 µM, THAL resulted in a 2-fold increase, which increased to 3-fold at 5 µM. This pattern of induction of pAKTSER473 followed by a plateau directly reflected the induction of BMRF1 observed in Figure 1B.
Figure 4. Idelalisib blocks LTP-mediated stimulation of PI3K at nanomolar concentrations and reverses LTP-mediated inhibition of proliferation.
(A) DAUDI cells were incubated with vehicle or LTP (0.1–5 µM) for 24 hours, and PI3K activity evaluated in cell lysates using a pAKTSer473 ELISA. pAKTSer473 values were normalized to those of the total AKT (also determined by ELISA), and the fold change was compared to that with the vehicle control. (B) Idelalisib (0.01–1 µM) was added to DAUDI cells for 24 hours, the suppression of PI3K was measured using a pAKTSer473 ELISA (left panel), and normalization was as described above. DAUDI cells were treated with either vehicle or increasing concentrations of idelalisib (25–1000 nM) for 72 hours, cell viability was determined using the WST-1 reagent, and results were expressed as the percentage viability relative to the vehicle control, which was arbitrarily set at 100% (right panel). “*” denotes p values of <0.05 compared to the vehicle control in A and B. (C) DAUDI cells were treated with LTP (0.016–10 µM) alone or in combination with idelalisib (25 nM) for 72 hours, cell viability was determined using the WST-1 reagent, and results were expressed as the percentage viability relative to the vehicle control, which was arbitrarily set at 100%. “*” denotes p values of <0.05 comparing the single-agent LTP to the idelalisib combination.
As shown in Figure 3, idelalisib suppressed pAKTSER473 at the clinically relevant concentration of 1 µM. We next determined the optimal concentration in vitro at which idelalisib could suppress pAKTSER473. Treatment of DAUDI cells with concentrations of idelalisib as low as 50 nM led to a 95% decrease in the basal levels of pAKTSER473, with complete suppression at concentrations up to 1 µM (Figure 4B). We also determined that a concentration of idelalisib as low as 25 nM was in the effective range to suppress basal pAKTSER473 levels and had no effect on cell viability (Figure 4B, right panel). We therefore used idelalisib (25 nM) in combination with varying LTP concentrations to determine whether it could reverse the LTP-induced decrease in proliferation. Single-agent LEN suppressed the growth of DAUDI cells to 70% compared to the vehicle control, and this remained constant across the concentration range used; the addition of Idelalisib completely reversed this growth suppression at all concentrations used (p<0.05 compared with the control) (Figure 4C). POM as a single agent decreased the cell viability to 90% at 0.08 µM and to 80% at 0.4 µM, and this growth suppression was reversed by idelalisib (p<0.05). At POM concentrations of 2 and 10 µM, however, idelalisib was not able to reverse the cell growth suppression (Figure 4C, right panel). THAL did not induce any decrease in cell viability, as previously observed, and the addition of Idelalisib resulted in no significant change to the cell viability (Figure 4C, middle panel).
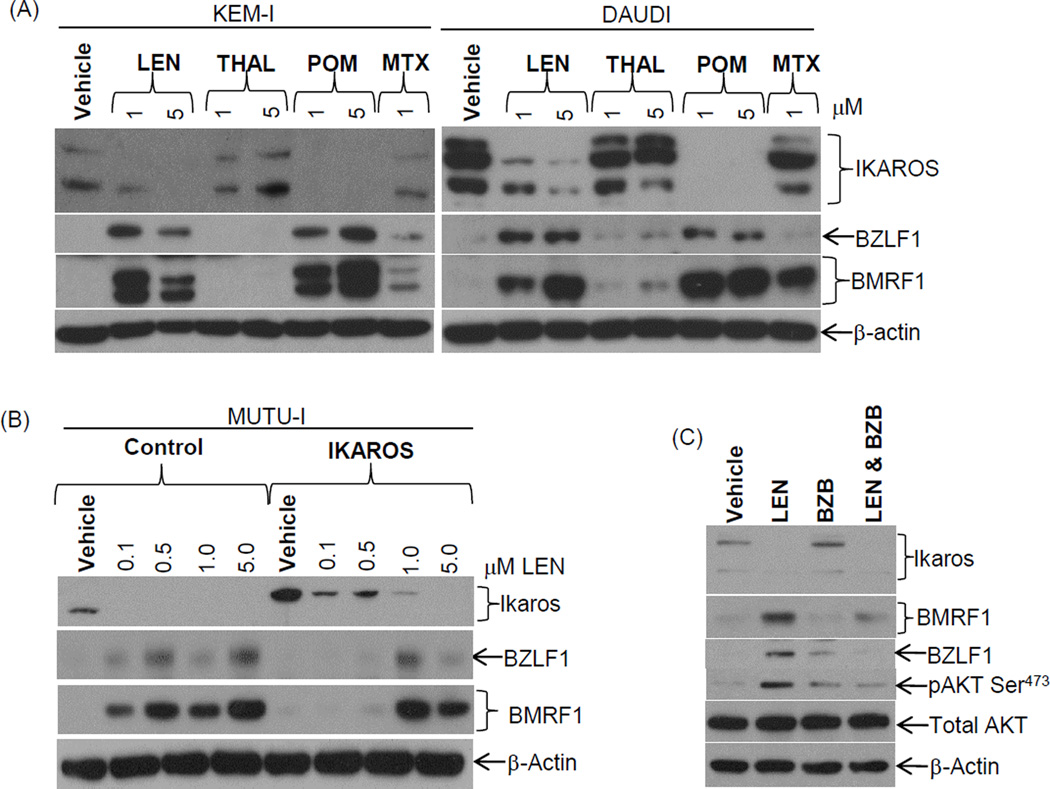
Overexpression of Ikaros attenuates LEN-induced EBV reactivation
LEN induces proteasome-mediated degradation of the Ikaros family of proteins (31), and Ikaros suppresses EBV-reactivation in BL cells (15). We therefore evaluated whether LTP-mediated Ikaros degradation is associated with EBV-reactivation. While exposure of DAUDI and KEM-I cells to 1 µM of LEN or POM strongly induced Ikaros degradation, coinciding with strong BMRF1 and BZLF1 induction, no change was seen with THAL (Figure 5A). Overexpression of Ikaros in MUTU-I cells attenuated both BZLF1 and BMRF1 induction by LEN at low concentrations (0.1–0.5 µM), compared to the control virus (Figure 5B). However, this effect was lost at higher concentrations (1–5 µM) of LEN, with complete loss of the overexpressed Ikaros at 5 µM (Figure 5B). We also evaluated the ability of the proteasome inhibitor BZB to block Ikaros-mediated degradation by LEN. While LEN alone induced loss of Ikaros, with accompanying increases in BMRF1, BZLF1, and pAKTSER473 (Figure 5C), addition of a low concentration of BZB (5 nM) with LEN suppressed the induction of BMRF1, BZLF1, and pAKTSER473 but failed to rescue Ikaros expression (Figure 5C).
Figure 5. Ikaros overexpression attenuates EBV reactivation by LEN.
(A) KEM-I and DAUDI were treated with either vehicle, various concentrations of LTP (1–5 µM) or MTX (1 µM) for 48 hours, and cell lysates were immunoblotted for Ikaros, BZLF1, BMRF1, and β-actin. (B) MUTU-I cells were infected with a control Lentivirus or a Lentivirus inducing expression of Ikaros for 48 hours, and then treated with LEN (0.1–5 µM) for 48 hours. Cell lysates were immunoblotted for Ikaros, BZLF1, BMRF1, and β-Actin as a loading control. (C) DAUDI cells were treated with LEN (1 µM), BZB (5 nM), or both for 24 hours, and cell lysates were immunoblotted with the indicated sera.
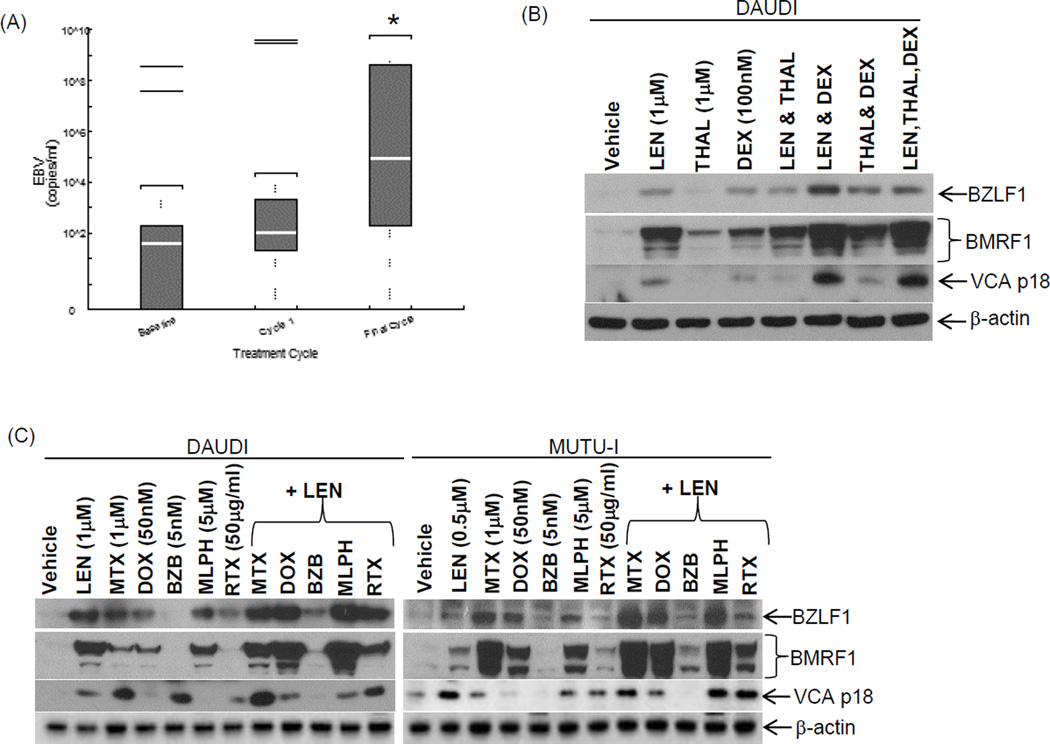
Combinations of LEN with chemotherapy agents enhance EBV reactivation
A combination of LEN and THAL with DEX in LEN resistant/refractory myeloma patients may to some extent overcome LEN resistance (13). This combination could also result in enhanced EBV-reactivation, since corticosteroid use with MTX enhanced EBV-reactivation, raising the risk of development of EBV lymphomas (9). We therefore examined the EBV viral load in 18 archived serum samples from patients who received a LEN, THAL, and DEX combination (Supplemental Figure 2A and Figure 6A) (13) and for whom a serum sample was available at baseline and after the first and last cycles of therapy (number of cycles, 3–15). qPCR evaluation of the baseline pretreatment serum indicated that most patients had no or low levels of virus, with a median load of 3.5 × 101 copies/mL (note: 2 patients had a high titer of virus at baseline) and a range of 0 to 3.7 × 108 copies/ml (Figure 6A and Supplemental Table 3). After 1 cycle of the treatment combination, the median viral load increased to 1.0 × 102 copies/mL with a range of 0 to 3.9 × 109 copies/mL, but this increase was not significant when compared to the baseline serum value (p=0.08). However, analysis after the final cycle for the 18 patients demonstrated an increase in the median viral load to 2.3 ×105 copies/mL, with a range of 0 to 4.0 × 108, which was highly significant compared with the baseline (p=0.0016) (Figure 6A and Supplemental Table 3). Six patients received VTX for varicella zoster infection at intermittent times (and not continuously) throughout the trial. To account for any differences in treatment outcome due to VTX, we compared the 6 patients receiving VTX to the 12 who did not and did not observe any statistical difference in the EBV viral load (p=0.3628) (Supplemental Figure 2B).
Figure 6. LEN and commonly used chemotherapy agents enhance EBV reactivation.
(A) Archived serum samples from a trial with myeloma patients receiving THAL and LEN continuously with weekly DEX in a 28-day cycle were evaluated for their EBV viral load by qPCR. EBV viral load copies per ml was calculated for the baseline and first and last cycles of therapy for each patient. “*” denotes p values of <0.01 comparing the final cycle to the baseline viral load. (B) DAUDI cells were treated with LEN, THAL (1µM), or DEX (100 nM), or in two- or three-drug combinations for 48 hours, and cell lysates were immunoblotted with the indicated sera. (C) MUTU-I and DAUDI cells were treated with LEN, MTX, DOX, BZB, MLPH, or RTX alone or in combination with LEN at the indicated concentrations. Protein lysates were immunoblotted with the indicated sera. Representative images are shown from 1 of 3 independent experiments.
In order to see if we could model this effect in vitro we treated DAUDI cells with the agents alone or in dual or triplicate combinations. LEN alone stimulated strong BMRF1 expression along with BZLF1 and VCA, whereas a similar THAL concentration stimulated BMRF1 weakly (Figure 6B). As expected, a clinically relevant concentration of DEX also stimulated BMRF1, BZLF1, and VCA expression (Figure 6B). The LEN and THAL combination did not increase BMRF1 expression over either agent alone, whereas LEN and DEX or THAL and DEX combinations induced significantly higher BZLF1, BMRF1, and VCA expression. A combination of all three agents was no more efficacious at EBV-reactivation than the LEN and DEX combination (Figure 6B).
Finally, we sought to investigate the interplay of LEN with other drugs used to treat myeloma and lymphoma patients. In DAUDI cells, LEN, MTX, DOX, and MLPH all induced significant amounts of BMRF1, BZLF1, and VCA, whereas RTX induced BZLF1, VCA, and BMRF1 weakly, and a low concentration of the proteasome inhibitor, BZB, had no effect (Figure 6C, left panel). When LEN was combined with DOX or MLPH, enhanced reactivation was observed, whereas BZB suppressed the LEN induction of BMRF1 and VCA. In comparison, EBV reactivation was induced in MUTU-I cells by a low dose (0.5 µM) of LEN, and strongly induced by single-agent MTX, DOX, MLPH, and, to a lesser extent, by RTX (Figure 6C, right panel), while BZB again had no effect. However, when LEN was combined with MTX, DOX, MLPH, or RTX, enhanced BMRF1, BZLF1, and VCA induction was observed beyond the single agents alone.
Discussion
Incorporation of THAL, LEN, and POM into the myeloma therapeutic armamentarium has contributed substantially to patient survival. Given the contributory role EBV plays in approximately 50% of HL, and reports of HL in patients on LEN-MT, we hypothesized that LEN, and its analogues THAL and POM, may induce EBV-reactivation. This hypothesis was further supported by the fact that the immunosuppressant MTX in non-malignant diseases such as rheumatoid arthritis enhanced the risk of EBV-positive lymphomas (9). In this study, we found that LTP reactivated EBV in latently infected B-cell lines in the order of efficacy POM>LEN>THAL. LCL cells were weakly inducible into lytic cycle, whereas BL cells were readily induced (Figure 1). Combinations of GCV with LEN or POM enhanced the growth inhibitory effect in BL cells (Figure 2C and Supplemental Figure 1), and this was further borne out in a mouse model (Figure 2D). The ability of LTP to reactivate EBV and sensitize cells to the bystander effect of GCV indicates a potential use in EBV-reactivation therapies for EBV-positive B-cell malignancies. Notably, similar approaches were shown to be effective using in vitro and in vivo models (11, 32, 33), and clinically with combinations of gemcitabine, valproic acid and GCV in nasopharyngeal carcinoma patients, which produced disease stabilization (34).
One mechanism of action of LTP against MM is through induction of proteasomal degradation of Ikaros (31, 35, 36). We observed this effect with LEN and POM at concentrations as low as 1 µM, which correlated with EBV-reactivation (Figure 5A). Interestingly, the addition of a low concentration of BZB (5 nM) failed to rescue Ikaros but did suppress the lytic cycle along with PI3K signaling, as seen by the decrease in pAKTSer473 (Figure 5C). The inability of BZB to prevent proteasomal suppression of Ikraos mediated by LEN has been shown to be both dose and time dependent, requiring pretreatment for 1 hour with 100 nM BZB to prevent Ikaros loss (37). The low concentration range of 3–5 nM was shown to be less effective in that study, as in our experiments. The ability of low BZB concentrations to block induction of the lytic cycle is most likely due to its reported ability to suppress pAKTSer473 by decreasing upstream kinases in the PI3K signaling cascade (38).
Ikaros is known to suppress the EBV lytic cycle through regulation of Octamer transcription factor-2 and Paired Box-5, B-cell transcription factors which promote latency (15, 39, 40), leading to the assumption that LTP-mediated EBV-reactivation occurs through this mechanism. Indeed, we found that Ikaros overexpression attenuated LEN induction of the lytic cycle, but did not result in complete blockade (Figure 5B). This is likely due to our additional finding that PI3K played a role in lytic EBV induction. LEN is known to stimulate PI3K activity (41), and we also showed that LTP stimulated PI3K activity, coinciding with EBV reactivation (Figures 3 and 4). Importantly, this stimulation was reversed by PI3K inhibition with idelalisib, which led to complete suppression of EBV reactivation. Of note is the fact that LEN and POM at low concentrations (0.1 µM) can eliminate Ikaros and also stimulate significant PI3K signaling, as shown by significant pAKTSer473 upregulation (Figures 4A and 5B). This effect plateaued at 0.5 µM and did not increase further for both LEN and POM, thereby explaining why no significant changes in BMRF1 occurred between 1 and 5 µM in the BL and LCL cells (Figure 1). However, THAL did show a dose-dependent increase in pAKTSer473 at 5 µM but does not suppress Ikaros, which suggests that the ability of LTP to induce EBV reactivation is primarily due to the stimulation of PI3K signaling, which is enhanced by LEN and POM’s simultaneous suppression of Ikaros.
EBV reactivation by LTP, therefore, is likely due to several mechanisms. First, stimulation of PI3K suppresses FoxO1, whose function is required for proper Ikaros mRNA splicing and whose loss results in Ikaros suppression (30). This effect was apparent with LEN treatment (Figure 3D). Second, LTP binding to Cereblon induces Ikaros degradation, further suppressing Ikaros expression. Finally, direct PI3K stimulation by LTP results in lytic cycle activation and appears to be a primary mechanism. The weaker induction of lytic cycle in LCLs compared with BL cells is likely due to the fact that LCLs have EBV latency state III, with lower Ikaros levels compared to the BL cells, which are in latency state I (15).
Finally, we evaluated EBV-reactivation with LEN in combination with commonly used chemotherapeutics for myeloma and lymphoma in patient serum samples and cell lines. In a small number of samples from myeloma patients who received a LEN/THAL/DEX combination, we could see that multiple cycles of the combination resulted in a significant increase in the EBV load in the serum (Figure 6A and Supplemental Table 3), and this was reproduced in vitro using cell lines (Figure 6B). This was in line with previously reported data showing glucocorticoids stimulate EBV-reactivation (42), which we found was enhanced by addition of LEN or THAL. Furthermore, we demonstrated expression of the late protein VCA in LEN- and POM-exposed BL cells (Figure 6B) and by RT-PCR we detected the late protein BCRF1 in LCL’s (Figure 1), indicating full activation of the EBV lytic cycle, which will result in viral release. MLPH, DOX and MTX also reactivated EBV, which was enhanced with the LEN addition (Figure 6C). RTX did not induce EBV-reactivation, but as reported for RTX/DEX combinations (43), RTX/LEN increased EBV-reactivation.
Our findings that LTP reactivate EBV in latently infected B-cells raises several interesting questions, particularly in light of LEN being linked to induction of SPMs in myeloma patients on LEN-MT (44, 45). Though the most common hematologic SPMs were acute myeloid leukemia and myelodysplastic syndromes, two LEN maintenance phase III trials reported HL in the LEN arms, with four cases in Attal et al. (2) and one in McCarthy et al. (3), with no cases in the placebo arms. In the context of THAL, two case reports on myeloma patients found EBV-positive HL as an SPM after THAL-containing regimens. One patient received THAL maintenance for 2 years with prior MLPH therapy (46), and another received 3 cycles of vincristine, DOX and DEX, and 4 cycles of BZB, THAL and DEX salvage with development of HL 5 years later (47). A study examining SPM incidence in myeloma patients treated in the pre-LEN era (1997–2008) reported only one case of HL out of 589 patients (48). In contrast, four patients developed HL as an SPM on LEN-MT out of 306 patients treated by Attal et al.
Myeloma patients frequently display varying degrees of immunosuppression due to secondary hypogammaglobulinemia, high-dose chemotherapy, use of LTP, proteasome inhibitors, or corticosteroids. In the face of varying degrees of immunosuppression, LEN could reactivate dormant EBV-positive-B-cells, which would normally attract both humoral and cytotoxic T cell responses, resulting in killing of the EBV-positive-B-cells and elimination of infectious virions. Lack of immune surveillance in the face of continual EBV stimulation may eventually exhaust remaining protective immunity. This would increase the small pool of latently infected EBV-positive B-cells, estimated to be around 1 in 106 cells, which would then have the potential to become transformed and, potentially, malignant. Combinations of DEX with LEN could result in enhanced EBV-reactivation and immune suppression, and the “R2” regimen comprising LEN and RTX used in lymphoma patients (49) could have a similar effect. It has been reported that LEN-treated myeloma patients have an increased incidence of varicella zoster and herpes simplex virus infections (50), suggesting LTP may reactivate the herpes virus family per se. The potential relationship between LEN and EBV-reactivation should be a consideration for patients treated with LEN long-term. Further studies are needed to determine if reactivation contributes to LEN-mediated clinical toxicities, if there is a possible contribution to SPMs, and if the risk of this could be reduced by the addition of anti-herpes virus agents such as acyclovir or valacyclovir in high-risk patient groups.
Supplementary Material
Translational Relevance.
The expanding use of immunomodulatory drugs in multiple myeloma, other hematological malignancies, and diseases other than cancer demonstrates the potential effectiveness of this class of agents. Their long-term use, such as in the maintenance therapy setting, however, may reveal previously unidentified downstream effects and toxicities. Our findings show the reactivation of the Epstein-Barr virus (EBV) into its lytic life-cycle from a previously latent state occurs primarily through the stimulation of PI3K signaling. This phenomenon has the potential to be a novel therapeutic strategy against EBV-positive malignancies in combination with ganciclovir. However, these findings also raise concern about the immune-suppressive effects of these drugs, and provides a possible link to EBV-related second primary malignancies.
Acknowledgments
Flow cytometry services were provided by the MD Anderson Flow Cytometry Core Facility, which is supported by the MD Anderson Cancer Center Support Grant (P30 CA016672). RZO would like to acknowledge support from the National Cancer Institute (P50 CA142509, R01s CA184464 and 194264, and U10 CA032102).
This study was funded in part by Celgene, and RZO has served on an advisory board for this entity.
Footnotes
Conflict of Interest Disclosure: The remaining authors declare no financial conflicts of interest.
Contribution: RJJ designed and performed most of the research and wrote the manuscript; TI designed and performed the Ikaros research and data analysis; XW performed some research; HCL provided helpful comments; SCK and JEM provided cells, reagents, and valuable suggestions; HL and VB performed statistical analyses; CWD provided cells, reagents and helpful manuscript comments; DW and JS consented patients and collected serum samples; and RZO supervised all the research completed herein.
References
- 1.Jagannath S. Introduction: addressing challenges in multiple myeloma management in an era of new therapeutics. Journal of the National Comprehensive Cancer Network : JNCCN. 2010;8(Suppl 1):S1–S3. doi: 10.6004/jnccn.2010.0111. [DOI] [PubMed] [Google Scholar]
- 2.Attal M, Lauwers-Cances V, Marit G, Caillot D, Moreau P, Facon T, et al. Lenalidomide maintenance after stem-cell transplantation for multiple myeloma. The New England journal of medicine. 2012;366:1782–1791. doi: 10.1056/NEJMoa1114138. [DOI] [PubMed] [Google Scholar]
- 3.McCarthy PL, Owzar K, Hofmeister CC, Hurd DD, Hassoun H, Richardson PG, et al. Lenalidomide after stem-cell transplantation for multiple myeloma. The New England journal of medicine. 2012;366:1770–1781. doi: 10.1056/NEJMoa1114083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Palumbo A, Hajek R, Delforge M, Kropff M, Petrucci MT, Catalano J, et al. Continuous lenalidomide treatment for newly diagnosed multiple myeloma. The New England journal of medicine. 2012;366:1759–1769. doi: 10.1056/NEJMoa1112704. [DOI] [PubMed] [Google Scholar]
- 5.Dimopoulos MA, Richardson PG, Brandenburg N, Yu Z, Weber DM, Niesvizky R, et al. A review of second primary malignancy in patients with relapsed or refractory multiple myeloma treated with lenalidomide. Blood. 2012;119:2764–2767. doi: 10.1182/blood-2011-08-373514. [DOI] [PubMed] [Google Scholar]
- 6.Jha HC, Banerjee S, Robertson ES. The Role of Gammaherpesviruses in Cancer Pathogenesis. Pathogens. 2016;5 doi: 10.3390/pathogens5010018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hislop AD, Taylor GS, Sauce D, Rickinson AB. Cellular responses to viral infection in humans: lessons from Epstein-Barr virus. Annual review of immunology. 2007;25:587–617. doi: 10.1146/annurev.immunol.25.022106.141553. [DOI] [PubMed] [Google Scholar]
- 8.Luskin MR, Roy DB, Wasik MA, Loren AW. Development of lymphomas containing Epstein-Barr virus after therapy with hyper-CVAD regimen. Clinical lymphoma, myeloma & leukemia. 2014;14:e55–e58. doi: 10.1016/j.clml.2013.11.010. [DOI] [PubMed] [Google Scholar]
- 9.Feng WH, Cohen JI, Fischer S, Li L, Sneller M, Goldbach-Mansky R, et al. Reactivation of latent Epstein-Barr virus by methotrexate: a potential contributor to methotrexate-associated lymphomas. Journal of the National Cancer Institute. 2004;96:1691–1702. doi: 10.1093/jnci/djh313. [DOI] [PubMed] [Google Scholar]
- 10.Kroger N, Zabelina T, Klyuchnikov E, Kropff M, Pfluger KH, Burchert A, et al. Toxicity-reduced, myeloablative allograft followed by lenalidomide maintenance as salvage therapy for refractory/relapsed myeloma patients. Bone marrow transplantation. 2013;48:403–407. doi: 10.1038/bmt.2012.142. [DOI] [PubMed] [Google Scholar]
- 11.Feng WH, Hong G, Delecluse HJ, Kenney SC. Lytic induction therapy for Epstein-Barr virus-positive B-cell lymphomas. Journal of virology. 2004;78:1893–1902. doi: 10.1128/JVI.78.4.1893-1902.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hong GK, Kumar P, Wang L, Damania B, Gulley ML, Delecluse HJ, et al. Epstein-Barr virus lytic infection is required for efficient production of the angiogenesis factor vascular endothelial growth factor in lymphoblastoid cell lines. Journal of virology. 2005;79:13984–13992. doi: 10.1128/JVI.79.22.13984-13992.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shah JJ, Orlowski RZ, Thomas SK, Alexanian R, Wang M, Qazilbash MH, et al. Final Results of a Phase I/II Trial of the Combination of Concurrent Lenalidomide, Thalidomide and Dexamethasone in Patients with Relapsed and/or Refractory Myeloma. ASH Annual Meeting Abstracts. 2012;120:75-. [Google Scholar]
- 14.Jones RJ, Dickerson S, Bhende PM, Delecluse HJ, Kenney SC. Epstein-Barr virus lytic infection induces retinoic acid-responsive genes through induction of a retinol-metabolizing enzyme, DHRS9. The Journal of biological chemistry. 2007;282:8317–8324. doi: 10.1074/jbc.M608667200. [DOI] [PubMed] [Google Scholar]
- 15.Iempridee T, Reusch JA, Riching A, Johannsen EC, Dovat S, Kenney SC, et al. Epstein-Barr virus utilizes Ikaros in regulating its latent-lytic switch in B cells. Journal of virology. 2014;88:4811–4827. doi: 10.1128/JVI.03706-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hong GK, Gulley ML, Feng WH, Delecluse HJ, Holley-Guthrie E, Kenney SC. Epstein-Barr virus lytic infection contributes to lymphoproliferative disease in a SCID mouse model. Journal of virology. 2005;79:13993–14003. doi: 10.1128/JVI.79.22.13993-14003.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jones DT, Monroy D, Ji Z, Atherton SS, Pflugfelder SC. Sjogren's syndrome: cytokine and Epstein-Barr viral gene expression within the conjunctival epithelium. Invest Ophthalmol Vis Sci. 1994;35:3493–3504. [PubMed] [Google Scholar]
- 18.Chou TC, Talalay P. Quantitative analysis of dose-effect relationships: the combined effects of multiple drugs or enzyme inhibitors. Adv Enzyme Regul. 1984;22:27–55. doi: 10.1016/0065-2571(84)90007-4. [DOI] [PubMed] [Google Scholar]
- 19.Jones RJ, Baladandayuthapani V, Neelapu S, Fayad LE, Romaguera JE, Wang M, et al. HDM-2 inhibition suppresses expression of ribonucleotide reductase subunit M2, and synergistically enhances gemcitabine-induced cytotoxicity in mantle cell lymphoma. Blood. 2011;118:4140–4149. doi: 10.1182/blood-2011-03-340323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen N, Wen L, Lau H, Surapaneni S, Kumar G. Pharmacokinetics, metabolism and excretion of [(14)C]-lenalidomide following oral administration in healthy male subjects. Cancer chemotherapy and pharmacology. 2012;69:789–797. doi: 10.1007/s00280-011-1760-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eriksson T, Bjorkman S, Hoglund P. Clinical pharmacology of thalidomide. European journal of clinical pharmacology. 2001;57:365–376. doi: 10.1007/s002280100320. [DOI] [PubMed] [Google Scholar]
- 22.Hoffmann M, Kasserra C, Reyes J, Schafer P, Kosek J, Capone L, et al. Absorption, metabolism and excretion of [14C]pomalidomide in humans following oral administration. Cancer chemotherapy and pharmacology. 2013;71:489–501. doi: 10.1007/s00280-012-2040-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nooka AK, Kastritis E, Dimopoulos MA, Lonial S. Treatment options for relapsed and refractory multiple myeloma. Blood. 2015;125:3085–3099. doi: 10.1182/blood-2014-11-568923. [DOI] [PubMed] [Google Scholar]
- 24.Rubsam LZ, Davidson BL, Shewach DS. Superior cytotoxicity with ganciclovir compared with acyclovir and 1-beta-D-arabinofuranosylthymine in herpes simplex virus-thymidine kinase-expressing cells: a novel paradigm for cell killing. Cancer research. 1998;58:3873–3882. [PubMed] [Google Scholar]
- 25.Meng Q, Hagemeier SR, Fingeroth JD, Gershburg E, Pagano JS, Kenney SC. The Epstein-Barr virus (EBV)-encoded protein kinase, EBV-PK, but not the thymidine kinase (EBV-TK), is required for ganciclovir and acyclovir inhibition of lytic viral production. Journal of virology. 2010;84:4534–4542. doi: 10.1128/JVI.02487-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adamson AL, Darr D, Holley-Guthrie E, Johnson RA, Mauser A, Swenson J, et al. Epstein-Barr virus immediate-early proteins BZLF1 and BRLF1 activate the ATF2 transcription factor by increasing the levels of phosphorylated p38 and c-Jun N-terminal kinases. Journal of virology. 2000;74:1224–1233. doi: 10.1128/jvi.74.3.1224-1233.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Darr CD, Mauser A, Kenney S. Epstein-Barr virus immediate-early protein BRLF1 induces the lytic form of viral replication through a mechanism involving phosphatidylinositol-3 kinase activation. Journal of virology. 2001;75:6135–6142. doi: 10.1128/JVI.75.13.6135-6142.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bryant H, Farrell PJ. Signal Transduction and Transcription Factor Modification during Reactivation of Epstein-Barr Virus from Latency. J Virol. 2002;76:10290–10298. doi: 10.1128/JVI.76.20.10290-10298.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lannutti BJ, Meadows SA, Herman SE, Kashishian A, Steiner B, Johnson AJ, et al. CAL-101, a p110delta selective phosphatidylinositol-3-kinase inhibitor for the treatment of B-cell malignancies, inhibits PI3K signaling and cellular viability. Blood. 2011;117:591–594. doi: 10.1182/blood-2010-03-275305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alkhatib A, Werner M, Hug E, Herzog S, Eschbach C, Faraidun H, et al. FoxO1 induces Ikaros splicing to promote immunoglobulin gene recombination. The Journal of experimental medicine. 2012;209:395–406. doi: 10.1084/jem.20110216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lu G, Middleton RE, Sun H, Naniong M, Ott CJ, Mitsiades CS, et al. The myeloma drug lenalidomide promotes the cereblon-dependent destruction of Ikaros proteins. Science. 2014;343:305–309. doi: 10.1126/science.1244917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gutierrez MI, Judde JG, Magrath IT, Bhatia KG. Switching viral latency to viral lysis: a novel therapeutic approach for Epstein-Barr virus-associated neoplasia. Cancer Res. 1996;56:969–972. [PubMed] [Google Scholar]
- 33.Westphal EM, Blackstock W, Feng W, Israel B, Kenney SC. Activation of lytic Epstein-Barr virus (EBV) infection by radiation and sodium butyrate in vitro and in vivo: a potential method for treating EBV-positive malignancies. Cancer research. 2000;60:5781–5788. [PubMed] [Google Scholar]
- 34.Wildeman MA, Novalic Z, Verkuijlen SA, Juwana H, Huitema AD, Tan IB, et al. Cytolytic virus activation therapy for Epstein-Barr virus-driven tumors. Clinical cancer research : an official journal of the American Association for Cancer Research. 2012;18:5061–5070. doi: 10.1158/1078-0432.CCR-12-0574. [DOI] [PubMed] [Google Scholar]
- 35.Kronke J, Udeshi ND, Narla A, Grauman P, Hurst SN, McConkey M, et al. Lenalidomide causes selective degradation of IKZF1 and IKZF3 in multiple myeloma cells. Science. 2014;343:301–305. doi: 10.1126/science.1244851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gandhi AK, Kang J, Havens CG, Conklin T, Ning Y, Wu L, et al. Immunomodulatory agents lenalidomide and pomalidomide co-stimulate T cells by inducing degradation of T cell repressors Ikaros and Aiolos via modulation of the E3 ubiquitin ligase complex CRL4(CRBN.) Br J Haematol. 2014;164:811–821. doi: 10.1111/bjh.12708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shi CX, Kortum KM, Zhu YX, Jedlowski P, Bruins L, Braggio E, et al. Proteasome inhibitors block Ikaros degradation by lenalidomide in multiple myeloma. Haematologica. 2015;100:e315–e317. doi: 10.3324/haematol.2015.124297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen KF, Yeh PY, Yeh KH, Lu YS, Huang SY, Cheng AL. Down-regulation of phospho-Akt is a major molecular determinant of bortezomib-induced apoptosis in hepatocellular carcinoma cells. Cancer research. 2008;68:6698–6707. doi: 10.1158/0008-5472.CAN-08-0257. [DOI] [PubMed] [Google Scholar]
- 39.Robinson AR, Kwek SS, Kenney SC. The B-cell specific transcription factor, Oct-2, promotes Epstein-Barr virus latency by inhibiting the viral immediate-early protein, BZLF1. PLoS pathogens. 2012;8:e1002516. doi: 10.1371/journal.ppat.1002516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Raver RM, Panfil AR, Hagemeier SR, Kenney SC. The B-cell-specific transcription factor and master regulator Pax5 promotes Epstein-Barr virus latency by negatively regulating the viral immediate early protein BZLF1. Journal of virology. 2013;87:8053–8063. doi: 10.1128/JVI.00546-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lapalombella R, Andritsos L, Liu Q, May SE, Browning R, Pham LV, et al. Lenalidomide treatment promotes CD154 expression on CLL cells and enhances production of antibodies by normal B cells through a PI3-kinase-dependent pathway. Blood. 2010;115:2619–2629. doi: 10.1182/blood-2009-09-242438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yang EV, Webster Marketon JI, Chen M, Lo KW, Kim SJ, Glaser R. Glucocorticoids activate Epstein Barr virus lytic replication through the upregulation of immediate early BZLF1 gene expression. Brain, behavior, and immunity. 2010;24:1089–1096. doi: 10.1016/j.bbi.2010.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Daibata M, Bandobashi K, Kuroda M, Imai S, Miyoshi I, Taguchi H. Induction of lytic Epstein-Barr virus (EBV) infection by synergistic action of rituximab and dexamethasone renders EBV-positive lymphoma cells more susceptible to ganciclovir cytotoxicity in vitro and in vivo. J Virol. 2005;79:5875–5879. doi: 10.1128/JVI.79.9.5875-5879.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thomas A, Mailankody S, Korde N, Kristinsson SY, Turesson I, Landgren O. Second malignancies after multiple myeloma: from 1960s to 2010s. Blood. 2012;119:2731–2737. doi: 10.1182/blood-2011-12-381426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Landgren O, Mailankody S. Update on second primary malignancies in multiple myeloma: a focused review. Leukemia. 2014;28:1423–1426. doi: 10.1038/leu.2014.22. [DOI] [PubMed] [Google Scholar]
- 46.Zago M, Adam P, Goldschmidt H, Fend F, Kanz L, Weisel K. Classical hodgkin lymphoma as de novo B-cell malignancy after treatment of multiple myeloma in the pre-lenalidomide era. Clinical lymphoma, myeloma & leukemia. 2014;14:e7–e11. doi: 10.1016/j.clml.2013.07.101. [DOI] [PubMed] [Google Scholar]
- 47.Chim CS, Choi PT, Lee WK. Hodgkin's lymphoma as a second cancer in multiple myeloma never exposed to lenalidomide. Annals of hematology. 2013;92:855–857. doi: 10.1007/s00277-012-1639-3. [DOI] [PubMed] [Google Scholar]
- 48.Hasskarl J, Ihorst G, De Pasquale D, Schrottner P, Zerweck A, Wasch R, et al. Association of multiple myeloma with different neoplasms: systematic analysis in consecutive patients with myeloma. Leuk Lymphoma. 2011;52:247–259. doi: 10.3109/10428194.2010.529207. [DOI] [PubMed] [Google Scholar]
- 49.Fowler NH, Davis RE, Rawal S, Nastoupil L, Hagemeister FB, McLaughlin P, et al. Safety and activity of lenalidomide and rituximab in untreated indolent lymphoma: an open-label, phase 2 trial. The Lancet Oncology. 2014;15:1311–1318. doi: 10.1016/S1470-2045(14)70455-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Konig C, Kleber M, Reinhardt H, Knop S, Wasch R, Engelhardt M. Incidence, risk factors, and implemented prophylaxis of varicella zoster virus infection, including complicated varicella zoster virus and herpes simplex virus infections, in lenalidomide-treated multiple myeloma patients. Annals of hematology. 2014;93:479–484. doi: 10.1007/s00277-013-1951-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.