Abstract
Background:
A reliable prediction of outcome for the victims of traumatic brain injury (TBI) on admission is possible from concurrent data analysis from any systematic real-time registry.
Objective:
To determine the clinical relevance of the findings from our TBI registry to develop prognostic futuristic models with readily available traditional and novel predictors.
Materials and Methods:
Prospectively collected data using predesigned pro forma were analyzed from the first phase of a trauma registry from a South Indian Trauma Centre, compatible with computerized management system at electronic data entry and web data entry interface on demographics, clinical, management, and discharge status.
Statistical Analysis:
On univariate analysis, the variables with P < 0.15 were chosen for binary logistic model. On regression model, variables were selected with test of coefficient 0.001 and with Nagelkerke R2 with alpha error of 5%.
Results:
From 337 cases, predominantly males from rural areas in their productive age, road traffic injuries accounted for two-thirds cases, one-fourths occurred during postmonsoon while two-wheeler was the most common prerequisite. Fifty percent of patients had moderate to severe brain injury; the most common finding was unconsciousness followed by vomiting, ear bleed, seizures, and traumatic amnesia. Fifteen percent required intracranial surgery. Patients with severe Glasgow coma scale score were 4.5 times likely to have the fatal outcome (P = 0.003). Other important clinical variables accountable for fatal outcomes were oral bleeds and cervical spine injury while imperative socio-demographic risk correlates were age and seasons.
Conclusion:
TBI registry helped us finding predictors of clinical relevance for the outcomes in victims of TBI in search of prognostic futuristic models in TBI victims.
Keywords: Age, Glasgow coma scale score, oral bleed, registry, regression model, season, traumatic brain injury, univariate analysis
INTRODUCTION
India has deficiencies in current trauma management systems with growing burden compared to nontraumatic morbidities. To augment optimum and favorable outcomes in trauma care, systematic studies with holistic approaches are warranted for insight into the prevailing reality.[1,2,3] Traumatic brain injury (TBI) is a leading cause of death and disability for which reliable factors for the outcome prediction on admission is clinically relevant as is captured in age old hippocratic aphorism, “no head injury is too severe to despair of, nor too trivial to ignore.” Glasgow coma scale (GCS) and the Glasgow outcome scale help us with confident predictions after 24 h following the injury, but not on admission.[4] Global experts estimated that TBI will become the third most common cause of death and disability globally by the year 2020 and is expected to surpass other noncommunicable diseases in mortality and morbidity by next decade involving neurosurgical emergencies requiring specialized neurosurgical care.[4,5,6,7] Prognostic models on admission are critical for early clinical decision-making and future research based abstraction of data on the variation in vital clinical observations.[8,9,10] Each country needs to find the load and demographic characteristics of TBI. A holistic approach embracing all disciplines is needed for effective primary prevention activities, policy improvement, and planning to guarantee satisfactory health care for people with TBI. This challenging effort will be capable to enumerate and evaluate numerous potential predictor variables of outcomes of victims of TBI Inclusion of abundant predictors in the TBI registry with unpredictable predictive power may be counterproductive; yet they are needed in developing countries like India where nationally representative data is yet to be evolved.[11,12] This study was conducted to identify the core variables on demographic factors, clinical course, management, and outcome of TBI cases in search of an electronic data entry interface (including web-based data entry interface) in resource-limited settings.
MATERIALS AND METHODS
The data for this study were sliced out from the first phase of a trauma registry prospectively being carried out at Narayana Medical College and Hospital, Nellore, Andhra Pradesh, India. This study was conducted at a center that is earmarked for exclusive emergency trauma care. The study was approved by Institute Ethical Board. Informed consents were obtained from all participants or their caregivers as well as bystanders before enrolling the TBI victims into the study.
The data were concurrently collected on a predesigned pro forma that is compatible with computerized management system by researchers not involved in patient care. The electronic data entry interface for this TBI registry was developed by FileMaker Pro Advanced 13 (Copyright© 1994–2015, FileMaker, Inc.) and the web data entry interface Drupal CMS (http://www.neuropractices.com/node/add/tbi-registry).
The pro forma questionnaire consisted of demographics variables such as age, gender, residence, and hospital district; time of injury and arrival; GCS score for head injuries TBIs; mode and intent of injury; preexisting conditions; vital signs on arrival (blood pressure, heart and respiratory rate); management aspects and discharge status (alive or dead).
Statistical analysis
The collected data was analyzed using StatsDirect version 3.0.150 (StatsDirect statistical software (http://www.statsdirect.com. England: 2015). Percentages were calculated for categorical data, and mean ± standard deviation was calculated for continuous data. The significance among categorical data was calculated using Chi-square test with an alpha error at 5%.
Logistic regression model
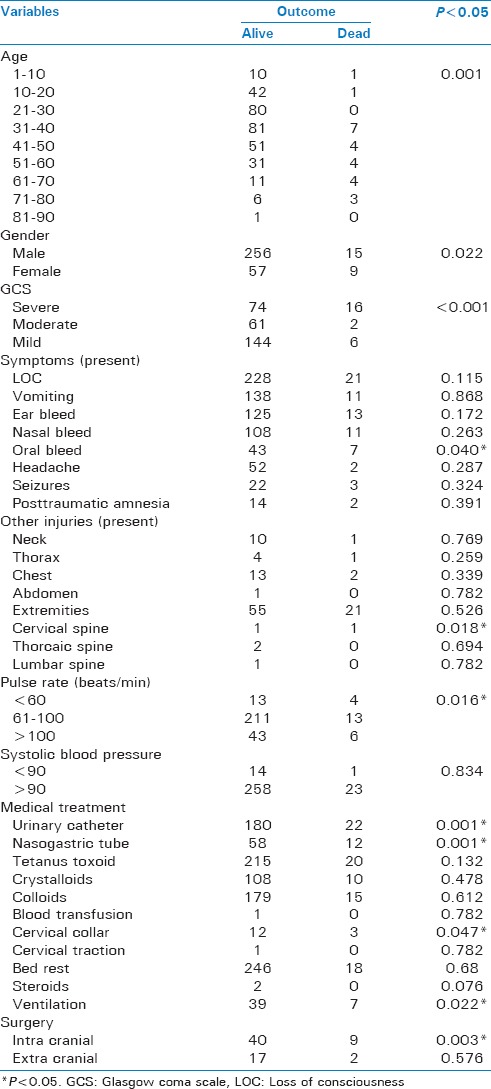
All the variables were analyzed using univariate test (variables with P < 0.15 were chosen). Binary logistic regression was used to identify the possible risk factors responsible for discharge outcome alive or death (dependent variables). The variables that entered logistic regression model are demographic variables are age, gender, season, place of injury, and time of admission; clinical variables are severity of injury, loss of consciousness, oral bleed, airway, breathing, cervical spine injury, and injury mechanism; management variables are intracranial surgery, urinary catheter, nasogastric tube, and ventilation. For more details refer Table 1, test of coefficient for the model was 0.001 and with Nagelkerke R2 with an alpha error at 5%.
Table 1.
Details of demographic, clinical and management variables of traumatic brain injury patients
RESULTS
In this study, identification of risk factors and their relationship to outcome were explored on 337 patients with a mean age of 36.26 ± 15.86 years; nearly half of the participants belonged to the third and fourth decade of age group; victims from male gender and rural sites were >80%. Prehospital care was received by 67.42% only, while private or public transportation (75.67%) was the most common mode of transportation. Road traffic injuries (RTIs) accounted for 63.20%. Seasonal variation was less though the highest cases noted during postmonsoon season (28.49%). Among injury risk correlates two-wheeler vehicular injuries were most common mode (60.83%), followed by falls (13.95%) and pedestrian injuries (13.65%) [Table 1].
Of 337 cases, nearly half (45.40%) had moderate to severe brain injury as assessed by GCS. All patients presented with symptoms - most common was a loss of consciousness (73.89%) followed by vomiting (40.21%), ear bleed (40.95%), and nasal bleed (35.31%). TBI-associated injuries were present in 157 (46.6%) of patients. Extremities were majorly affected (17.2%). Abnormal vitals were noted in quite a good number of cases in the pupils (3.26%), pulse (19.58%), systolic (39.17%), and diastolic blood pressure (24.33%). Abnormal airway and breathing was present in > 40% of patients. Colloids were needed by 57.57% of injured cases on admission; 20.77% required nasogastric intubation for external feeding. Among TBI victims, 14.54% of cases were seriously injured to require intracranial surgery for evacuation of accumulated blood, while only 7.12% of enrolled TBI cases expired during the study period [Table 1].
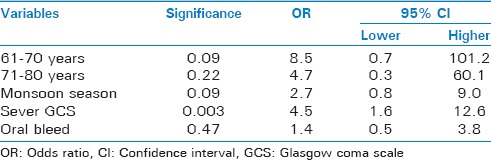
The demographic, clinical, and management variables discussed elsewhere were entered into binary logistic regression. The model reveals that among clinical variables oral bleed and GCS were found to be risk factor. Severe GCS patients are 4.5 times likely to die with reference to mild (P = 0.003). Oral bleed patients are 1.4 times likely to die (P = 0.475). Among demographic variables age and seasons were found to be risk factors. The patients in age range of 61–70 years are 8.5 (P = 0.09) times and 71–80 years are 4.7 (P = 0.225) times likely to die with reference to <10 years age group. In monsoon season patients are 2.7 (P = 0.96) and in winter 1.3 (P = 0.63) times likely to die with reference to postmonsoon. Among managements, no variables were found to be significant [Table 2].
Table 2.
Binary logistic regression with variables of >1 odds ratio
DISCUSSION
Internationally clinical guidelines are being proposed with the aim to guide decisions in TBI treatment.[13] In the light of current evidence, we have indigenously generated the TBI registry that is user-friendly as well as applicable at any healthcare facility with minimum infrastructure in India. In this prospective observational study, the clinical relevance of abnormal findings and identification of risk factors were analyzed to bring out relationship to the outcome by a systematic TBI registry.
Prehospital care
In our study, the prehospital care was received by 67.42% and private or public transportation (75.67%) was the most common mode of transportation. Other studies also reported that TBI cases were brought to hospital largely by known person or reached on their own arrangements rather than accompanied by police or by ambulance in needed hours.[14,15] Yet, literature concluded in their study that optimum prehospital care can ensure to reduce morbidity and mortality due to TBI in particular and trauma in general.[16,17,18]
Demographic variables
Overall, the role of age as demographic risk factor in TBI outcome has been noted to be vital risk factors in our registry. In our study, mortality was significant in the age group 60 years above presenting with TBI that was a significant problem in older adults. Older age is known to negatively influence outcome after TBI was also noted by others.[18] Elderly trauma patients present unique challenges and face more significant obstacles to recovery than their younger counterparts.[17] The effect of head injury is disproportionately severe in elderly and for a given severity of head injury; more patients require admissions and neurosurgical care.[19] In a study from central India, mean reported age of TBI cases were 32–64 years.[20] The International Mission for Prognosis and Clinical Trial (IMPACT) database on TBI through merging individual patient data from eight RCTs and three observational surveys observed that increasing age was strongly related to worse outcome in a continuous linear trend.[21] Males gender were >80% in our TBI registry. Other studies also reported male preponderance in their case series; the reason may be exposure of male gender to more risky as well as outdoor jobs for longer hours.[14,15,22,23] Cases from rural areas were >80% in our study. Literature reported a state level surveillance system to identify cases of TBI that showed higher rates of severe cases in rural areas.[24] We noted seasonal variations in the occurrence of TBI cases. TBI admissions experienced a bimodal peak, during the months of March to June and from October to November in a Maharashtra study.[25]
Cause of injury
In our registry data set, RTIs accounted for 63.20%. Two-wheeler motorized vehicular injuries were most common mode, followed by pedestrian, four and three wheelers and bicycle injuries in our study. Other Indian researchers also noted similar findings from Indian studies that majority of cases of TBI are due to RTI and significant number of two-wheeler users and pedestrians were hit by some motorized vehicle on the road leading to RTI.[14,15] The most common mechanism of injury of TBI was road traffic crashes (46.8%) in the rural Maharashtra.[26] Published global literature also reported that motorbikes as major causes of TBI with an incremental role in developing countries though other risk factors are reported going lesser in recent times.[24]
Clinical presentation
Low GCS and oral bleed were notable risk factors for the outcome (alive or dead) in our study and unconsciousness was common clinical presentation. Associated clinical findings suggestive of basal skull fractures were vomiting (40.21%), ear bleed (40.95%), nasal bleed (35.31%), etc. Others researchers worldwide also noted the history of loss of consciousness mostly in TBI victims with nasal bleed, ear bleed among associated injuries.[14,15,27] Conventionally, we assessed severity of TBI by GCS score. Yet researchers historically are not having unanimous opinion on the positive predictability of GCS on outcome analysis as it does not follow a normal distribution.[27,28] Common clinical finding in TBI patient was vomiting, ear, and nose bleed also reported by others.[14,15,27] Associated injuries play an additive role in TBI on the outcome apart from age, sex, severity of injury, intracranial pathology, intracranial pressure, etc.[20] In an Indian hospital based study, two-thirds of TBI cases had a local injury on head and neck region and in suspected polytrauma, radiological evaluation of other body parts revealed evidence of injury was noted one in ten.[14]
Abnormal signs
Unequal pupil size is potentially a sign of a serious brain injury.[29] In our TBI registry, we observed pupillary asymmetry in 3.26%; Delhi study noted in 14%.[14] In our study, pulse (19.58%), systolic (39.17%), and diastolic blood pressure (24.33%) with weird airway and breathing (>40%) were also noted with TBI cases.
Other risk factors
Researchers in different parts of the world had observed other significant risk factors for TBI which we could not find and would like to include in our registry modifications. These were provision of first aid by trained personal, distance covered by patients to reach hospital, prehospital requirement of resuscitation, presence of local injury on head and face, radiological injuries of other body parts among others.[14] IMPACT study outcome remained to be closely related with the impact of primary injury as shown by the initial GCS by exploiting the ordinal nature of the Glasgow Outcome Scale and by relating the outcome obtained in individual patients to their baseline prognostic risk.[20,30,31]
Management
We did not find noteworthy role of aggressive interventions on outcome as only 14.54% intracranial surgery for evacuation of accumulated blood, 7.12% expired. Globally researchers also noted that a positive change in TBI intervention outlook is possible as majority of TBI patients do not require costly neurosurgical intervention and can be conservatively managed with excellent outcome, even in the dearth of state-of-art neurosurgical facilities; insertion of ventriculostomies or ICP monitors can be successfully performed by dedicated capacity building that is proved to be cost-effective approach. Despite these questions arise on the domain of basic care of TBI versus specialized care of a neurosurgeon interpreting risk as well as management.[6,14,21,32,33,34]
An ambitious national plan has identified health-care facilities across highways to establish life support ambulance system with communication links and trauma referral system and to develop a national trauma registry to improvise, monitor and evaluate the efficiency of the trauma care system to widen the scope of injury science to the global standard.[1,35]
Death from traumatic brain injury
In Delhi study, the patient who required resuscitation (6% of total admission) on reaching the hospital, among these 60% expired; among severe grade (15% of TBI cases) 73.5% died.[14] Overall, mortality in a TBI intervention series was 8.69% in Jaipur study[15] and 6.4% in the rural Maharashtra study.[26] Associated injuries like compound fracture pelvis, hemoperitoneum, and blunt/perforating trauma chest lead trail of death in severe TBI as seen in Jaipur study.[15] In a North-Indian study on geriatric head-injury, the mortality rate increased with age: the highest mortality was observed in patients aged above 70 years (28.6%). The mortality rate was 27% in patients with age group of 66–70 years, while it was 24% in patients with age group of 60–65 years.[36]
Need of registry-based continuous data collection
Experts have opined that in India, majority of the data available is based either on postmortem, forensic analysis, or medico-legal reports; thus, it may not reveal the true picture. That was in our back of mind to initiate a real time TBI registry. From the analysis of this first phase of data, we strongly feel that for a reliable prediction of outcome of TBI from systematic real-time registry is a promising tool. TBI registry also helped us finding predictors of clinical relevance for the outcomes in victims of TBI in search of prognostic futuristic models. Researchers from India feel that, by strengthening trauma care system with improved documentation, it is possible to decrease the risk factors of TBI as well as their timely interventions for better outcome.[14]
Strengths of the study
We are trying hard to develop an indigenous TBI registry within the existing challenges to TBI management secondary to the limited resources designated to our center as we strongly feel it, as an under-assessed crisis. Furthermore, there is a wide scope of research on the development of facilities available to treat neurosurgical cases in the developing world.
Limitations of the study
Our study had several limitations. First, we had done this study in a single center. Second, we are in search of predictors which are relevant for our sociodemographic and health infrastructure savvy though we know that inclusion of too many predictor variables that may result in lack of statistical significance of one or more of important predictor variables. Finally, trauma registry may not reflect correctly the quality of prehospital care in TBI cases with associated problems that demand concurrent evaluations, discussion, improvisation, and interventions as enormously essential to save life and prevent permanent disabilities.[14]
Future directions of the study
We are striving to include like-minded researchers in the lengths and breadths of our country for multicentric studies using this registry to increase validity. In the long run, the analysis will help improve TBI scenario with the implementation of newer algorithm. To address this significant public health issue, a refocusing of research efforts is justified to prevent TBI to discern unique care requirements to facilitate best patient outcomes.[37]
CONCLUSION
TBI registry has been bridging the gap of information in the understanding of risk factors, interventions, and outcomes. In absence of any national database, the policy makers could not be well sensitized regarding the socioeconomic and health impact of injury. The developed countries could have enhanced quality of injury care by identifying gaps in the trauma management system and find out opportunities of improvements using registry. We hope, believe and trust that this study will provide a cost-effective comprehensive data collection system on diverse parameters including configuration of present scenario of prehospital care in our country.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Pal R, Agarwal A, Galwankar S, Swaroop M, Stawicki SP, Rajaram L, et al. The 2014 Academic College of Emergency Experts in India's INDO-US Joint Working Group (JWG) White Paper on “Developing Trauma Sciences and Injury Care in India”. Int J Crit Illn Inj Sci. 2014;4:114–30. doi: 10.4103/2229-5151.134151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agrawal A, Kakani A, Baisakhiya N, Galwankar S, Dwivedi S, Pal R. Developing traumatic brain injury data bank: Prospective study to understand the pattern of documentation and presentation. Indian J Neurotrauma. 2012;9:87–92. [Google Scholar]
- 3.Pal R. Injury epidemiology: The neglected chapter. Nepal J Epidemiol. 2012;2:216–8. [Google Scholar]
- 4.Steyerberg EW, Mushkudiani N, Perel P, Butcher I, Lu J, McHugh GS, et al. Predicting outcome after traumatic brain injury: Development and international validation of prognostic scores based on admission characteristics. PLoS Med. 2008;5:e165. doi: 10.1371/journal.pmed.0050165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schuhmann MU, Rickels E, Rosahl SK, Schneekloth CG, Samii M. Acute care in neurosurgery: Quantity, quality, and challenges. J Neurol Neurosurg Psychiatry. 2001;71:182–7. doi: 10.1136/jnnp.71.2.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agrawal A, Kumar A, Agrawal CS, Pratap A. One year of neurosurgery in the Eastern region of Nepal. Surg Neurol. 2008;69:652–6. doi: 10.1016/j.surneu.2007.03.047. [DOI] [PubMed] [Google Scholar]
- 7.Zitnay G. Re-Engineering of the Damaged Brain and Spinal Cord. Vienna: Springer; 2005. Lessons from national and international TBI societies and funds like NBIRTT; pp. 131–3. [DOI] [PubMed] [Google Scholar]
- 8.Hernández AV, Steyerberg EW, Butcher I, Mushkudiani N, Taylor GS, Murray GD, et al. Adjustment for strong predictors of outcome in traumatic brain injury trials: 25% reduction in sample size requirements in the IMPACT study. J Neurotrauma. 2006;23:1295–303. doi: 10.1089/neu.2006.23.1295. [DOI] [PubMed] [Google Scholar]
- 9.Hernández AV, Steyerberg EW, Taylor GS, Marmarou A, Habbema JD, Maas AI. Subgroup analysis and covariate adjustment in randomized clinical trials of traumatic brain injury: A systematic review. Neurosurgery. 2005;57:1244–53. doi: 10.1227/01.neu.0000186039.57548.96. [DOI] [PubMed] [Google Scholar]
- 10.Machado SG, Murray GD, Teasdale GM. Evaluation of designs for clinical trials of neuroprotective agents in head injury. European Brain Injury Consortium. J Neurotrauma. 1999;16:1131–8. doi: 10.1089/neu.1999.16.1131. [DOI] [PubMed] [Google Scholar]
- 11.CDC. Traumatic Brain Injury in the United States: The Future of Registries and Data Systems. [Last accessed on 2016 Feb 06]. Available from: http://www.cdc.gov/traumaticbraininjury/pdf/Future_of_Registries-a.pdf .
- 12.Yuh EL, Mukherjee P, Lingsma HF, Yue JK, Ferguson AR, Gordon WA, et al. Magnetic resonance imaging improves 3-month outcome prediction in mild traumatic brain injury. Ann Neurol. 2013;73:224–35. doi: 10.1002/ana.23783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maas AI, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008;7:728–41. doi: 10.1016/S1474-4422(08)70164-9. [DOI] [PubMed] [Google Scholar]
- 14.Shekhar C, Gupta LN, Premsagar IC, Sinha M, Kishore J. An epidemiological study of traumatic brain injury cases in a trauma centre of New Delhi (India) J Emerg Trauma Shock. 2015;8:131–9. doi: 10.4103/0974-2700.160700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gupta P, Singh J, Sharma A, et al. Epidemiological analysis and clinical characteristics of traumatic brain injuries in rural Jaipur: The first single centre experience. Journal of Evidence Based Medicine and Healthcare. 2015;2(52):8686–91. [Google Scholar]
- 16.Bhatoe HS. Brain injury and prehospital care: Reachable goals in India. Indian J Neurotrauma. 2009;6:5–10. [Google Scholar]
- 17.Callaway DW, Wolfe R. Geriatric trauma. Emerg Med Clin North Am. 2007;25:837–60, x. doi: 10.1016/j.emc.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 18.Thompson HJ, McCormick WC, Kagan SH. Traumatic brain injury in older adults: Epidemiology, outcomes, and future implications. J Am Geriatr Soc. 2006;54:1590–5. doi: 10.1111/j.1532-5415.2006.00894.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maurice-Williams RS. Head injuries in the elderly. Br J Neurosurg. 1999;13:5–8. doi: 10.1080/02688699944104. [DOI] [PubMed] [Google Scholar]
- 20.Bhole AM, Potode R, Agrawal A, Joharapurkar S. Demographic profile, clinical presentation, management options in cranio cerebral trauma: An experience of a rural hospital in central India. Pak J Med Sci. 2007;23:724. [Google Scholar]
- 21.Mushkudiani NA, Engel DC, Steyerberg EW, Butcher I, Lu J, Marmarou A, et al. Prognostic value of demographic characteristics in traumatic brain injury: Results from the IMPACT study. J Neurotrauma. 2007;24:259–69. doi: 10.1089/neu.2006.0028. [DOI] [PubMed] [Google Scholar]
- 22.Yattoo G, Tabish A. The profile of head injuries and traumatic brain injury deaths in Kashmir. J Trauma Manag Outcomes. 2008;2:5. doi: 10.1186/1752-2897-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Verma PK, Tiwari K. Epidemiology of road traffic injuries in Delhi: Result of survey. Reg Health Forum. 2004;8:6–14. [Google Scholar]
- 24.Reilly P. The impact of neurotrauma on society: An international perspective. Prog Brain Res. 2007;161:3–9. doi: 10.1016/S0079-6123(06)61001-7. [DOI] [PubMed] [Google Scholar]
- 25.Gururaj G. Epidemiology of traumatic brain injuries: Indian scenario. Neurol Res. 2002;24:24–8. doi: 10.1179/016164102101199503. [DOI] [PubMed] [Google Scholar]
- 26.Agrawal A, Galwankar S, Kapil V, Coronado V, Basavaraju SV, McGuire LC, et al. Epidemiology and clinical characteristics of traumatic brain injuries in a rural setting in Maharashtra, India 2007-2009. Int J Crit Illn Inj Sci. 2012;2:167–71. doi: 10.4103/2229-5151.100915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Waxman K, Sundine MJ, Young RF. Is early prediction of outcome in severe head injury possible? Arch Surg. 1991;126:1237–41. doi: 10.1001/archsurg.1991.01410340079011. [DOI] [PubMed] [Google Scholar]
- 28.Gaddis GM, Gaddis ML. Non-normality of distribution of Glasgow Coma Scores and Revised Trauma Scores. Ann Emerg Med. 1994;23:75–80. doi: 10.1016/s0196-0644(94)70012-5. [DOI] [PubMed] [Google Scholar]
- 29.Ghajar J. Traumatic brain injury. Lancet. 2000;356:923–9. doi: 10.1016/S0140-6736(00)02689-1. [DOI] [PubMed] [Google Scholar]
- 30.Maas AI, Marmarou A, Murray GD, Teasdale SG, Steyerberg EW. Prognosis and clinical trial design in traumatic brain injury: The IMPACT study. J Neurotrauma. 2007;24:232–8. doi: 10.1089/neu.2006.0024. [DOI] [PubMed] [Google Scholar]
- 31.Marmarou A, Lu J, Butcher I, McHugh GS, Mushkudiani NA, Murray GD, et al. IMPACT database of traumatic brain injury: Design and description. J Neurotrauma. 2007;24:239–50. doi: 10.1089/neu.2006.0036. [DOI] [PubMed] [Google Scholar]
- 32.Bajracharya A, Agrawal A, Yam B, Agrawal C, Lewis O. Spectrum of surgical trauma and associated head injuries at a university hospital in Eastern Nepal. J Neurosci Rural Pract. 2010;1:2–8. doi: 10.4103/0976-3147.63092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shukla D, Devi BI. Mild traumatic brain injuries in adults. J Neurosci Rural Pract. 2010;1:82–8. doi: 10.4103/0976-3147.71723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Valadka AB. Fact and fiction of emergency surgical care in America: A neurosurgical perspective. Clin Neurosurg. 2007;54:153–6. [PubMed] [Google Scholar]
- 35.Pal R. Injury science in India: Call for the action. Indian J Prev Soc Med. 2012;43:229–32. [Google Scholar]
- 36.Sinha V, Gupta V, Singh DK, Chopra S, Gupta P, Bagaria H. Geriatric head injuries – Experience and expectations. Indian J Neurotrauma. 2008;5:69–73. [Google Scholar]
- 37.Balak N. A prospective and comparative study of referrals to neurosurgeons in an emergency department: Does use of guidelines for head trauma affect the assessment made by non-neurosurgeons? Ulus Travma Acil Cerrahi Derg. 2008;14:292–8. [PubMed] [Google Scholar]


