Abstract
Objective To investigate the practice, experiences and views of motivated and trained family physicians as they attempt to implement informed and shared decision making (ISDM) in routine practice and to identify and understand the barriers they encounter.
Background Patient involvement in decision making about their health care has been the focus of much academic activity. Although significant conceptual and experimental work has been done, ISDM rarely occurs. Physician attitudes and lack of training are identified barriers.
Design Qualitative analysis of transcripts of consultations and key informant group interviews.
Settings and participants Six family physicians received training in the ISDM competencies. Audiotapes of office consultations were made before and after training. Transcripts of consultations were examined to identify behavioural markers associated with each competency and the range of expression of the competencies. The physicians attended group interviews at the end of the study to explore experiences of ISDM.
Results The physicians liked the ISDM model and thought that they should put it into practice. Evidence from transcripts indicated they were able to elicit concerns, ideas and expectations (although not about management) and agree an action plan. They did not elicit preferences for role or information. They sometimes offered choices. They had difficulty achieving full expression of any of the competencies and integrating ISDM into their script for the medical interview. The study also identified a variety of competency‐specific barriers.
Conclusion A major barrier to the practice of ISDM by motivated physicians appears to be the need to change well‐established patterns of communication with patients.
Keywords: Canada, family medicine, patient participation, physician–patient communication, shared decision making
Introduction
The rationale for the involvement of patients in making decisions about their health care arises from the ethical imperative of patient autonomy. 1 Law, 2 government policy 3 and the governing bodies of the medical profession 4 are moving from paternalism in the direction of informed choice. Informing patients and involving them in decisions seems to be the physician's duty and the topic has been the focus of much academic activity, especially over the past decade. 5 Although significant conceptual and experimental work has taken place, it has also been documented that informed and shared decision making or its fundamental constituents such as offering treatment options, rarely occurs in practice. 6 , 7 , 8 , 9 This has been attributed, at least in part, to the fact that physicians are not trained in the communication skills required for sharing decisions about management with patients, the so‐called ‘second half of the consultation’. 10 , 11
We have published a set of competencies (knowledge, skills and abilities) that are a framework for the teaching, learning, practice and investigation of informed shared decision making (ISDM) based on a review of the literature and interviews and focus groups with physicians, patient educators and patients (Table 1). 12 These things that a physician ought to be able to do are the elements of the ISDM model. Lists of similar competencies, competences, elements or steps that define the characteristics of shared decision making have been published by other authors. 13 , 14
Table 1.
Competencies for informed and shared decision making (ISDM): what the doctor should be able to do* 12
| 1 Develop a partnership with the patient [PARTNERSHIP] |
| 2 Establish or review the patient's preferences for information (such as amount or format) [INFORMATION] |
| 3 Establish or review the patient's preferences for role in decision making (such as risk taking and degree of involvement of self and others), and the existence and nature of any uncertainty about the course of action to take (decisional conflict) [ROLE] |
| 4 Ascertain and respond to patient's ideas, concerns and expectations (such as about disease management options) [IDEAS] |
| 5 Identify choices (including ideas and information patient may have) and evaluate the research evidence in relation to the individual patient [CHOICES] |
| 6 Present (or direct patient to) evidence taking into account 2 and 3 above, framing effects (how presentation of the information may influence decision making), etc. Help patient to reflect upon and assess the impact of alternative decisions with regard to his or her values and lifestyles [EVIDENCE] |
| 7 Make or negotiate a decision in partnership and resolve conflict [DECISION] |
| 8 Agree upon an action plan and complete arrangements for follow up [PLAN] |
ISDM may also: involve a team of health professionals; involve significant others (partners, family); differ across cultural, social and age groups. We have created a one‐word summary of each competency for brevity in the text.
*Notes: although the competencies are numbered, there is no intent that they should be practiced in this, or any other sequence in the context of the medical interview.
We developed a workshop for general practitioners (GPs) based on the ISDM framework to provide an opportunity for the learning and practice of the competencies. We had anecdotal evidence that the physicians who came to the workshops tried to put ISDM into practice but we had not systematically recorded in detail what those behaviours were, nor what barriers they would experience.
Perceived barriers to shared decision making and the closely related evidence‐based patient choice (EBPC) consultation have been documented. Ford et al. interviewed professionals anticipated to have an interest in the EBPC consultation and found the following perceived barriers: limitations of available evidence, doctor attitudes, patient factors, resource constraints, time constraints and disruption of the doctor–patient relationship. 15 Elwyn et al. studied a group of registrars for whom the concept of shared decision making was novel and who had no communication skills training that addressed this part of the doctor–patient interaction. 16 Following experience with three simulated consultations they anticipated various barriers to sharing decisions: lack of information; time and timing; contextual modifiers (e.g. patient age and education); and nature of the decision.
A questionnaire survey of GPs who had participated in a trial of shared decision making and risk communication for four chronic conditions found positive attitudes to the training and towards involving patients. 17 Time constraints were given as a reason for not implementing the approach more widely. Following the trial the frequency with which they applied the new skills and tools in routine practice was limited. 18 They acknowledged that they were selective, often incorrectly, about when they felt greater patient involvement was appropriate and feasible rather than seeking to apply the approaches to the majority of consultations. The decision to engage in shared decision making was influenced by patient sociodemographic characteristics, nature of patient's problem and perceived time constraints.
In contrast to studies that have enquired about the barriers that physicians anticipate will be important in practice or that they experienced with a limited set of patients, our qualitative exploratory study investigated the barriers that were reported and independently identified while motivated and trained family physicians attempted to implement ISDM in routine practice with unselected patients. The practice, experiences and views of these physicians and the identification of barriers was done through analysis of transcripts of actual doctor–patient consultations and through key informant discussion groups 19 with the physicians.
Method
Recruitment
Family physicians who were ‘lead tutors’ in the Department of Family Practice at the University of British Columbia, Vancouver, Canada, were invited to participate in the study. This group was selected as they are experienced preceptors of undergraduate medical students with a known high standard of practice and commitment to patient‐centred care. Six physicians were recruited, all of whom confirmed their interest in involving patients in decision making. The physicians represented a range of typical urban Vancouver solo and group family practice.
Training
The physicians attended a 3‐h workshop at which they were introduced to the rationale for shared decision making and the ISDM model comprising the eight competencies. They then viewed and discussed a videotape of a doctor–patient encounter that demonstrated the competencies in practice. Finally they were challenged to practice the competencies themselves in encounters with three different standardized (simulated) patients representing a range of common decision‐making situations and types of patients found in primary care. After each encounter they received feedback from the standardized patients, workshop facilitators and peers.
Office data collection
Two half‐day visits were made to their offices prior to the workshop to collect baseline data. Consultations of all consenting patients were audiotaped and transcribed. Each patient completed a short questionnaire after the consultation to collect basic demographic and satisfaction data. The physicians completed a simple log for each patient to assess opportunities for and perceived success of putting ISDM into practice. Post‐workshop, four half‐day visits were made to each office and data were collected as before. There were 206 consenting encounters yielding 198 complete data sets (physician logs, patient questionnaires and transcribed audiotapes). Eighty‐one were collected pre‐workshop (average 13/physician) and 117 post‐workshop (average 20/physician).
Analysis of consultations
Four members of the research team each independently read 10 randomly selected transcripts to identify the presence of individual ISDM competencies. A simple scheme was developed to classify the transcripts based on the opportunity for, or presence of, ISDM. Each transcript was classified independently by the research team and discussed to reach agreement on the markers to be used for each category. The offering of choices was agreed to be the key marker for ISDM and was easily identifiable in the transcripts. The final classification scheme comprised four categories:
-
1
Category 0: No opportunity for ISDM (doctor choice only, e.g. emergency management or patient attending for a procedure, e.g. flu shot).
-
2
Category 1: Opportunity for ISDM present but not demonstrated (physician managed problem without offering or discussing options with the patient).
-
3
Category 2: Some ISDM present (physician appeared to be trying to put ISDM into practice (choices offered) but expression of other competencies was rudimentary.
-
4
Category 3: ISDM present (choices offered and had many elements of the other competencies also present).
The remaining interviews were classified independently by two of the researchers. There was good agreement between the raters and discrepancies were resolved by discussion.
The transcripts coded in categories 2 and 3 were examined in detail to identify behavioural markers associated with each competency, i.e. competencies were identified by the presence of explicit statements in the transcripts that reflected a close reading of the wording of the competencies. For example:
PARTNERSHIP: Is the patient encouraged to be involved in decisions? Does there appear to be an explicit attempt to enhance the autonomy of the patient? INFORMATION: Does the doctor ask the patient how much or about the form in which she would like to receive information? ROLE: Does the doctor establish the patient's preference for involvement in decisions or enquire if others should be involved? IDEAS: Does the doctor ask the patient for his thoughts about the choices? CHOICE: Is it clear that there may be more than one possible management choice? Does the doctor reserve her preferences until the patient has responded to the choices? EVIDENCE: Does the doctor direct the patient to sources of information or present information based on current evidence? DECISION: Do both the doctor and the patient contribute to the decision? PLAN: Is it clear who does what and by when?
For each competency examples were collected from the transcripts to illustrate the markers or range of expression.
Key informant discussion groups
At the end of the office data collection period, the study physicians attended one of two key informant discussion groups with the research team to share their experiences in attempting to use the ISDM model. The first group also sought physicians’ views on questions arising from our analysis of the transcripts and logs to validate or provide explanations for our findings. In the second group, physicians and four members of research team went through two transcripts (of interviews in category 3) and independently identified the competencies present. The group then stepped through the transcripts and discussed the examples of the competencies that had been identified by the physicians to probe their understanding of the competencies. The discussion groups were audiotaped and transcribed.
Transcripts were analysed using the Framework method of analysis developed by the National Centre for Social Research (http://www.natcen.ac.uk/natcen/pages/hw_qualitative.htm), a method in which themes are developed both from the research questions and from the accounts of research participants. The data presented include both key informant and transcribed consultation data organized by the eight ISDM competencies. Key issues and themes were identified by the members of the research team through careful reading of the transcripts. They were grouped into categories related to the ISDM model overall and to each specific competency and further refined upon re‐reading of the data. The key issues emerging from the data are presented with illustrative quotes.
From our observations of how the competencies were operationalized in the transcripts, through answers to specific questions asked of the key informants and through review of the transcripts at the key informant discussion group, competency‐specific barriers to the implementation of ISDM were identified.
Ethics approval for the study was granted by the University of British Columbia Behavioural Research Ethics Board.
Results
Of the 198 complete data sets, 69% (range 17–90%) of the patients had been seeing this physician for a year or more. An average of 1.6 problems was discussed in each encounter (range 1–5, 59% a single issue). The median length of the interview (transcription) was 8.1 min (range 2.2–40 min); 65% of patients were female; all age groups were represented (from children to elderly); 69% had education beyond high school.
From the patient questionnaires, 76% said the doctor provided choices for treatment, 90% felt they and the doctor made the decision together, 94% felt able to share information they brought and 95% felt better informed.
Physician views of ISDM
The physicians had very positive attitudes towards ISDM and the model presented in the workshop. They said the model felt consistent with their practice; the workshop and the experience of being in the study had made them more conscious of their communication and helped them to formalize their approach to ISDM.
For me that's, I find that's the only way I can be effective. I mean it's not my style to be of the more traditional older style physician. I don't have much experience with that. So I can't use that. But I just think that, I find the ISDM just very natural.
Well, um, in fact I've been using for several years now, I just didn't call it ISDM… So when actually, you know, you people came along I jumped at it because I really want to kind of crystallize and gel, you know, what was happening…
Responses at the discussion group showed that situations not considered appropriate for ISDM were situations where they perceived no choices: emergencies and when simple procedures were being done. Patient characteristics affected their practice of ISDM. Some physicians determined whether their patients would want ISDM or not; others took the view that if patients were resistant to getting involved (e.g. wanted the physician to make the decision), then ISDM was a process which would take time. Patients perceived to be least likely to want ISDM were the elderly and certain cultural groups.
A positive patient response encouraged physicians to continue their efforts with certain competencies even though it may take more time. For example, an anecdote about the offering of choices:
And, and so I said to her, ‘What do you want to do?’ And she said, ‘I don't know.’ And this was a beautiful case to say alright, here are your options… And then she got up and she said to me, ‘Do you know I now have a totally clear picture in my head of what my choices are and now I have to go and sit down with [Name] and have this talk.’ And to me that conversation took us 25 minutes, it was worth every minute because she went away feeling very empowered and I didn't make any decision for her.
The ISDM competencies in practice
Based on the physicians’ logs, 163 consultations (82%) were viewed as opportunities for ISDM. Of these, physicians rated their success at ISDM as high in 42 (21%) and moderately high in 86 (43%) consultations. Classification of the transcripts by the research team identified 181 as opportunities for ISDM. Some ISDM (category 2) was demonstrated in 27 (14%); and ISDM was judged present (category 3) in 25 (13%) (see Fig. 1). There were no obvious important differences in the presence of ISDM in the transcripts pre‐ and post‐workshop and the data have been pooled. Two physicians had significantly more transcripts in categories 2 and 3 than their colleagues both before and after the workshops.
Figure 1.
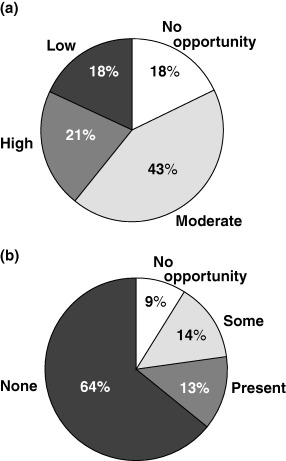
(a) Physicians’ post‐encounter self assessment of the presence of informed and shared decision making (ISDM). (b) Analysis of transcripts by research team for markers of the elements of ISDM.
Based on careful reading of the transcripts and identification of the behavioural markers for each competency, we identified three categories: routinely present, sometimes present and never present.
Competencies that were routinely present but not necessarily associated with the presence of ISDM (necessary but not sufficient) were PARTNERSHIP, IDEAS, DECISION and PLAN. Some elements of these competencies were observed in most transcripts, independent of whether or not ISDM actually occurred (as exemplified by the offering of choices). They represent those ISDM competencies that are most likely to be done routinely as elements of the standard short office interview. Competencies PARTNERSHIP and IDEAS were most often done within the context of the first part of the interview (problem identification) rather than subsequent problem management.
Competencies that were sometimes present and were specific to ISDM were CHOICES and EVIDENCE. By definition CHOICES was present in interviews in categories 2 and 3. Presentation of EVIDENCE was present in some of these transcripts. Both competencies were specific to the treatment decision‐making part of the interview.
The competencies that were not explicitly seen were INFORMATION and ROLE.
Partnership
Partnership is a specific kind of relationship that goes beyond rapport and is derived from the mutual participation and contractual model of doctor–patient relationships. 20 It is a relationship that is characterized by mutual co‐operation, trust and responsibility for the achievement of a specified goal. Most of the examples of relationship building that we found in the transcripts were primarily rapport‐building communication and not related to shared decision making. For example, the interview usually began with a social interaction and the relationship was developed through enquiry into the patient's story and might be further consolidated during the physical examination. Once the patient's problem was identified, relationship communication was carried on through the other competencies and we were not able to identify specific partnership development behaviours associated with decision making.
Two difficulties with the practice of this competency as defined in the context of shared decision making were identified from the key informant discussion group. First, there was an ambivalence towards the idea of mutual responsibility inherent in partnership. Despite positive attitudes towards ISDM, the physicians’ statements revealed, on the one hand, a sense of responsibility for the patient and, on the other, a lack of trust in the patient's ability to behave responsibly.
It's our job to be responsible for the patient, the patient's health…I mean that's, we go to work every day to do that. But the patient doesn't come to us with a job to be healthy, you know. They, they come to us, we give them advice, how compliant are patients? Sometimes they think just by going to the doctor they've done their job and they're not going to follow through with what, what we asked of them.
A second difficulty was that partnership building may require an effort over time to get the patient to a place where they are ready to make shared decisions.
It takes me several visits to engage them in being a partner and not everyone wants to and if you, you use this model and you feel as a physician that this is something you're comfortable with, and you feel that this is good practice, then you have to educate them on being a person involved in this partnership and it may take six or seven visits with a farm worker to let him feel comfortable with the idea that he can actually think about what he wants to do, and he has to, you'll give him the knowledge, you'll teach him about his body and then you teach him about, uh, investigation. So as he's receiving this information then he may a year later start being a partner.
Information
We did not observe in the transcripts explicit enquiry into the patient's preferences for amount and type of information. There were examples of indirect methods of enquiry about information preferences (a doctor may ask if the patient has read anything) and patients sometimes mentioned their preferences, at least indirectly (a patient might mention having read something or spoken to someone about their problem). The doctors agreed that this competency was not present in the transcripts (i.e. they did not think it was there when it was not).
Direct and indirect questioning of the physicians revealed the following reasons why this competency is not done:
-
1
It is not part of the interview model that they learned and therefore does not currently have a natural place in the interview structure. As a consequence they perceive that they have managed fine during all their years of training and practice without having asked about it. In addition, they are not sure how it would be done and feel awkward about the idea of asking the patient directly (the patient might be taken aback and not know how to respond).
Um, so I just find that difficult and to be honest in 16 years I've never asked a patient, ‘how would you like your information?’
-
2
They regard themselves as the most important source of information and that patients want their information verbally. They consider other sources of information of minor importance and needed only on specific occasions, although they said they were more likely to offer choices in format when there was a lot of information available (e.g. menopause).
Isn't that the way most people want their information? They want, they assume their doctor is well informed.
-
3
They think they already know their patients’ preferences or think it is implicit in the way patients respond when the doctor offers information or options.
If you have a good awareness of a patient's context and you develop a partnership where there is a free flow of communication then you don't have to ask because it is implicit.
Role
There were no examples in the transcripts of explicit discussion of the patient's role. We found three indirect markers of this competency.
-
1
Indications about role preference given by patients, e.g. ‘What I am doing is not working and we need to find a different course of action.’
-
2
Doctors testing the patient's degree of active participation in their health care, for example by enquiry about whether the patient would be prepared to take their own blood pressure measurements over a trial period.
-
3
Doctors gauging the patient's wish to be involved by offering choices and then asking ‘What do you think?’
The reasons why this competency is not done explicitly were similar to those for information preference. The physicians felt that they could intuit this either for individual patients or on specific visits, particularly when they had a long standing relationship with a patient.
And there are times when like as a doctor you can sense that the patient needs and wants guidance and not, and not, uh, you know, a visit where you provide them options and they, you know, give their input.
Alternatively, they thought that the patient's preferred role was implicit in the way they responded when offered options.
If you're saying these are the options we have and they sit there and say nothing and you then, you say ‘what do you think about it?’, they'll say ‘well I don't know, what do you want?’ or ‘what do you think? You tell me what to do’. It's implicit. They've said to you, ‘I want you to make a decision for me’.
Ideas
Most interviews appeared to have this competency present, at least to some degree, but it seemed to exist on a very large continuum. The physicians were obviously able to elicit and respond to patients’ ideas, concerns and expectations, although this was most often done in relation to the patient's story and problem rather than in relation to treatment. Its fullest expression was contingent upon the offering of choices. Rarely were the three distinct concepts of ideas, concerns and expectations explicitly addressed.
There were two difficulties with the practice of this competency. First, the physicians did not relate it specifically to the patient's ideas, concerns and expectations about treatment options. When they were asked to identify this competency in the transcripts they noted it as present when the patient was spontaneously telling their story during the history taking part of the interview, rather than something the physician was actively doing by ascertaining and responding.
Secondly, physicians made a conscious decision whether to do this or not. They gave the following reasons when asked why the competency was sometimes present and sometimes not:
-
1
Lack of time – patients backed up in waiting room.
-
2
Fatigue or stress of physician.
-
3
Expectation that it will only lead to repetition of a previous story.
-
4
Discomfort in dealing with patients’ fears and emotional state.
-
5
Concern that asking will be the equivalent of opening Pandora's box.
I paused and thought, do I want to go there? I actually, I can recognize there was half a second where I went through this whole process in my mind… So in this whole time I, I actually had to think if I consciously wanted to open that box. And I chose to.
Choices
The offering of choices was the easiest competency to identify in the interviews (there was no doubt about whether choices were offered or not). There were distinct and explicit verbal markers such as ‘choices’, ‘options’‘other things we can do’. In the transcripts there were clearly opportunities for offering choices that were not taken; when offered, choices were rarely provided in a complete, coherent or unbiased manner.
The physicians indicated that they also thought that choices were at the heart of ISDM. They said they found this the most natural part of the ISDM model and linked choices with patient autonomy and partnership building.
[I offer choices] because I, its for me the way I practice is for patients to take ownership of their health and be responsible and accountable for their health and if I say do this I'm taking that role away from them and I'm discouraging that.
Direct and indirect questioning revealed the following reasons why the physicians did not offer choices:
-
1
They have already made up their mind (prior experience of what works and does not).
-
2
They do not perceive any choices (emergency or procedural).
-
3
They may not consider that a patient is receptive to choices on a particular day.
-
4
They perceive the patient needs a definite course of action to be specified by the physician (e.g. to relieve uncertainty; an example given was a diagnostic test for suspected breast cancer).
-
5
Constraints of practice guidelines (can be used both for and against offering choices).
-
6
They had a limited view of the choices available, e.g. may view the only decision to be made as whether something happens (no choice) and not explore other decisions such as when (for which there may be choices).
Evidence
The presentation of evidence was seldom observed and when it did occur, it existed on a wide continuum from a brief statement of how a proposed treatment works, to anecdotal evidence about the doctor's experience with the drug/management option, to sometimes a mention that ‘some studies have shown that…’ The specific results of studies or figures were rarely mentioned. Concepts like relative risk or numbers needed to treat were not referred to. The application of the results of studies to the individual patient was rare and rudimentary.
In attempting to identify this competency from the transcripts the physicians (i) identified the patient giving information (history) as part of presenting evidence and (ii) equated the doctor providing any information to the patient with providing evidence. It therefore appears there is some confusion about the meaning of the competency and it is not clearly identified with treatment decision‐making or evidence‐based information.
Other barriers to this competency being done effectively that were inferred from the discussion (and transcripts) included: physicians do not know the evidence; they do not have time; they do not think patients want or will understand the evidence.
Decision
Expression of this competency ranged from telling the patient what is going to happen, to agreeing with the patient's stated request. It was often combined with formulating an action plan. There were few cases where overt conflict was observed. Negotiation of conflict when the doctor and patient wanted different things appeared to be a time consuming and non‐linear process as evidenced by the length and complexity of the interview. The strategies used by the doctor to negotiate conflict appeared to be: deferral of a decision until more information has been gathered, referral to a third party (specialist) and persistence in presenting his/her opinion. The key informants had little to add about this competency.
Plan
This competency was always done in some way simply because it gives closure to the interview. Some physicians did it very thoroughly after they had summed up everything about the interview, others did it only in passing. In only a handful of interviews was it done in such a way that was consistent with partnership (explicit agreement about mutual roles and responsibilities following the visit). The key informants had little to add about this competency.
Discussion
All the physicians in this study liked the ISDM model and thought that they (and other physicians) put it into practice. However, the evidence from the transcripts indicated that their practice of ISDM was limited. These physicians were skilled in the teaching and practice of patient‐centred interviewing. Wensing et al. noted that attention to patients’ needs and emotions seems to be a fairly consistent working style of physicians and perhaps one of the competencies that doctors bring to their work from their qualification period. 21 Once established it is hard to influence and a self‐perception of competence will mean that there is little motivation to change. The physicians in our study were not able to take the list of competencies presented at the workshop and easily internalize them into their working model for the medical interview. The established communication patterns of competent physicians are difficult to change.
There were fundamental differences in the physicians’ and researchers’ understanding of the precise meaning of the competencies. Most of the competencies sounded intuitively obvious to the physicians and close to what they already do or try to do. They quickly identified transcript text which they thought illustrated the competencies. Wensing et al. found little correlation between patient‐centred communication and shared decision making and that skills associated with shared decision making were less consistently demonstrated. 21 We found that the ISDM competencies that are superficially similar to those routinely taught as part of good interviewing technique and that occur in most good short medical interviews were the ones most likely to be misunderstood. For example, the physicians equated rapport building (being nice to the patient) with partnership; they did not differentiate the patients’ volunteering ideas about their problems during history taking from the physicians’ ascertaining ideas, concerns and expectations about management; they counted as ‘evidence’ any information giving by the doctor or patient.
Offering choices was the most straightforward competency to recognize in the transcripts and was clearly related to decision making. A decision that appropriately involves a patient requires viable options. 22 It is difficult to imagine that shared decision making could occur without an offering of choices. It was the only competency for which there was, from the start, a shared understanding of its meaning between the physicians and the research team. It may offer the best starting point for the teaching of ISDM. 23 It is easy to understand and leads naturally to the other competencies.
In addition to a lack of clarity about the meaning and implications of some of the competencies, specific barriers were identified in relation to many of the competencies. Discussion of evidence‐based information was not observed and may require specific risk communication aids and be unrealistic in routine practice. It has been noted in other studies that explicit enquiry into the patient's preference for information and role in decision making is very rarely seen. 6 , 9 This study sheds insight into why that is so: the physicians felt uncomfortable with the idea of asking, did not think it was necessary and could not see how it would naturally fit into the structure of their interviews. However, a lengthy explanation given in one of the key informant discussion groups did stimulate at least one of the doctors to say she would try it out with her patients in the future.
The findings of this study have implications for the design of effective training programmes for ISDM. Our experience and the very limited success of others reinforces the fact that these are difficult and unfamiliar ideas and skills for physicians that are not currently learned in undergraduate or specialist training, a time when they are developing their medical identity. 24 The complexity of the barriers to ISDM means that a single educational intervention is unlikely to be effective in changing behaviour even among predisposed physicians. It was not surprising to us that there were no important differences in the presence of ISDM between the pre‐ and post‐workshop interviews. In a 3‐h workshop we were able to provide physicians with a coherent and explicit framework for ISDM and an immediate opportunity to try it out. It was insufficient to help them to acquire and comfortably use new phrases in their routine interview scripts. Transcript review by the physicians helped them to identify expression of the competencies and clarify their meaning. It also confronted them with discrepancies between subjective assessments of the presence of ISDM (their own and the perceptions of their patients) and the evidence of the actual words in the transcripts. This discrepancy between perception and reality is noted in the communications literature. 25 , 26 Transcript review as part of the feedback process for ISDM training would be a simple method to demonstrate this gap to promote behavioural change.
The strength of this study was that the physicians were selected for their known high standard of care, interest in education, peer status as excellent communicators and predisposition towards ISDM. They provided informed and high‐quality reflections on their practice of ISDM. The limitation is that they were a small sample and we do not have data to gauge the relative importance of the barriers uncovered or generalizability to the larger community of family physicians. This would require a much larger sample and different design. In retrospect it seems that the experimental design may have been more efficient with fewer office visits and more frequent discussion of transcripts and experiences.
Although some competencies are more frequently and naturally practised than others, full expression of the competencies was not observed. Clearly there are major barriers to putting ISDM into practice beyond the ones that have already been identified in the literature such as physician motivation, time, contextual modifiers (e.g. patient characteristics) and training. The additional barriers identified in this research relate to the practice of ISDM as a whole (lack of an overall framework in which to put the ISDM competencies within the familiar short office interview) and competency‐specific barriers. A major barrier to the practice of ISDM by motivated physicians appears to be the need to change well‐established patterns of communication with patients.
Acknowledgements
We thank the six physicians who took part in the study and standardized patient trainers and advisors, Sheila Dyer and Sabine Clifford. Assistance with data collection was provided by Stephanie Calvert, Jennifer Manklow, Jordan McCurrach, Amy Patterson, Holly Weisinger and Crispin Wye. This project was funded by the Vancouver Foundation, British Columbia Medical Services Foundation.
References
- 1. Coulter A. The Autonomous Patient. Ending Paternalism in Medical Care. London: Nuffield Trust, 2002. [Google Scholar]
- 2. Fenwick P, Beran RG. Informed consent – should Bolam be rejected? Medical Law, 1996; 16: 215–223. [PubMed] [Google Scholar]
- 3. Department of Health . Patient and Public Involvement in the New NHS. London: Department of Health, 1999. [Google Scholar]
- 4. General Medical Council . Good Medical Practice. London: GMC, 2001. [Google Scholar]
- 5. Edwards A, Evans R, Elwyn G. Manufactured but not imported: new directions for research in shared decision making support and skills. Patient Education and Counseling, 2003; 50: 33–38. [DOI] [PubMed] [Google Scholar]
- 6. Braddock CH, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. Informed decision making in outpatient practice. Journal of the American Medical Association, 1999; 282: 2313–2320. [DOI] [PubMed] [Google Scholar]
- 7. Stevenson FA, Barry CA, Britten N, Barber N, Bradley CP. Doctor–patient communication about drugs: the evidence for shared decision making. Social Science and Medicine, 2000; 50: 829–840. [DOI] [PubMed] [Google Scholar]
- 8. Campion P, Foulkes J, Neighbour R, Tate P. Patient centredness in the MRCGP video examination: analysis of a large cohort. British Medical Journal, 2002; 325: 691–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Elwyn G, Edwards A, Wensing M, Hood K, Atwell A, Grol R. Shared decision making: developing the OPTION scale for measuring patient involvement. Quality and Safety in Health Care, 2003; 12: 93–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Elwyn G, Edwards A, Kinnersley P. Shared decision‐making in primary care: the neglected second half of the consultation. British Journal of General Practice, 1999; 49: 477–482. [PMC free article] [PubMed] [Google Scholar]
- 11. Thistlethwaite JE. Making and sharing decisions about management with patients: the views and experiences of pre‐registration house officers in general practice and hospital. Medical Education, 2002; 36: 49–55. [DOI] [PubMed] [Google Scholar]
- 12. Towle A, Godolphin W. Framework for teaching and learning informed shared decision making. British Medical Journal, 1999; 319: 766–769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Elwyn G, Edwards A, Kinnersley P, Grol R. Shared decision‐making and the concept of equipoise: the competences of involving patients in healthcare choices. British Journal of General Practice, 2000; 50: 892–899. [PMC free article] [PubMed] [Google Scholar]
- 14. Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Education and Counseling, 2006; 60: 310–312. [DOI] [PubMed] [Google Scholar]
- 15. Ford S, Schofield T, Hope T. Barriers to the evidence‐based patient choice (EBPC) consultation. Patient Education and Counseling, 2002; 47: 179–185. [DOI] [PubMed] [Google Scholar]
- 16. Elwyn G, Edwards A, Gwyn R, Grol R. Towards a feasible model for shared decision making: focus group study with general practice registrars. British Medical Journal, 1999; 319: 753–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Edwards A, Elwyn G. Involving patients in decision making and communicating risk: a longitudinal evaluation of doctors’ attitudes and confidence during a randomized trial. Journal of Evaluation in Clinical Practice, 2004; 10: 431–437. [DOI] [PubMed] [Google Scholar]
- 18. Edwards A, Elwyn G, Wood F, Atwell C, Prior L, Houston H. Shared decision making and risk communication in practice: a qualitative study of GPs’ experiences. British Journal of General Practice, 2005; 55: 6–13. [PMC free article] [PubMed] [Google Scholar]
- 19. Gilchrist VJ, Williams RL. Key informant interviews In: Crabtree BF, Miller WL. (eds) Doing Qualitative Research. Thousand Oaks, CA: Sage Publications Inc., 1999: 71–88. [Google Scholar]
- 20. Quill TE. Partnerships in patient care: a contractual approach. Annals of Internal Medicine, 1983; 98: 228–234. [DOI] [PubMed] [Google Scholar]
- 21. Wensing M, Elwyn G, Edwards A, Vingerhoets E, Grol R. Deconstructing patient centred communication and uncovering shared decision making: an observational study. BMC Medical Informatics and Decision Making, 2002; 2: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McNutt RA. Shared medical decision making. Problems, process, progress. Journal of the American Medical Association, 2004; 292: 2516–2518. [DOI] [PubMed] [Google Scholar]
- 23. Godolphin W. The role of risk communication in shared decision making. British Medical Journal, 2003; 327: 692–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. O'Flynn N, Britten N. Does the achievement of medical identity limit the ability of primary care practitioners to be patient‐centred? A qualitative study. Patient Education and Counseling, 2006; 60: 49–56. [DOI] [PubMed] [Google Scholar]
- 25. Makoul G, Arntson P, Schofield T. Health promotion in primary care: physician–patient communication and decision making about prescription medications. Social Science and Medicine, 1995; 41: 1241–1254. [DOI] [PubMed] [Google Scholar]
- 26. Waitzkin H. Information giving in medical care. Journal of the American Medical Association, 1984; 252: 2441–2446. 6481931 [Google Scholar]


