Abstract
Arterial stiffness is an independent risk factor for stroke and myocardial infarction. This study was designed to investigate the role of SIRT1, an important deacetylase, and its relationship with Klotho, a kidney-derived aging-suppressor protein, in the pathogenesis of arterial stiffness and hypertension. We found that the serum level of Klotho was decreased by nearly 45% in patients with arterial stiffness and hypertension. Interestingly, Klotho haplodeficiency caused arterial stiffening and hypertension, as evidenced by significant increases in pulse wave velocity (PWV) and blood pressure (BP) in Klotho-haplodeficient (KL+/−) mice. Notably, the expression and activity of SIRT1 were decreased significantly in aortic endothelial and smooth muscle cells in KL+/− mice, suggesting that Klotho deficiency downregulates SIRT1. Treatment with SRT1720 (15 mg/kg/day, IP), a specific SIRT1 activator, abolished Klotho deficiency-induced arterial stiffness and hypertension in KL+/− mice. Klotho deficiency was associated with significant decreases in activities of AMP-activated protein kinase alpha (AMPKα) and endothelial nitric oxide synthase (eNOS) in aortas, which were abolished by SRT1720. Furthermore, Klotho deficiency upregulated NADPH oxidase activity and superoxide production, increased collagen expression, and enhanced elastin fragmentation in the media of aortas. These Klotho deficiency-associated changes were blocked by SRT1720. In conclusion, this study provides the first evidence that Klotho deficiency downregulates SIRT1 activity in arterial endothelial and smooth muscle cells. Pharmacological activation of SIRT1 may be an effective therapeutic strategy for arterial stiffness and hypertension.
Keywords: Klotho, AMPKα, eNOS, SIRT1, arterial stiffness, hypertension
Introduction
Aortic stiffness and hypertension are generally regarded as common aging-related disorders, as the prevalences of these disorders increase with age.1–2 According to the Seventh Report of the Joint National Committee,3 more than two thirds of individuals over aged 65 years suffer from hypertension. Arterial stiffening reflects gradual fragmentation and loss of elastin fibers and accumulation of stiffer collagen fibers in the media of large arteries. It occurs independently of atherosclerosis4 and is an independent predictor of cardiovascular outcomes.5 It has been reported that aortic stiffness predicts an increase in systolic blood pressure (BP) and incident hypertension,6 indicating a close relationship between large artery stiffness and the development of hypertension.4 Our recent study revealed that haplodeficiency of the Klotho gene causes aortic stiffness prior to the elevation of BP.7 However, the underlying mechanism is not fully understood.
Of the human sirtuins, SIRT1 is the closest homologue to yeast silent information regulator 2 (Sir2) protein and functions as a NAD+-dependent protein and histone deacetylase. An accumulation of evidence has shown that SIRT1 has anti-inflammatory, anti-oxidant, and anti-apoptotic effects in the endothelium, thus preventing endothelial senescence and dysfunction.8–9 Since the first report showing that SIRT1 activates endothelial nitric oxide synthase (eNOS),10 several studies using gene mutant mouse models have demonstrated that SIRT1 has atheroprotective effects.8–11 Angiotensin II-induced vascular remodeling and hypertension in mice were attenuated by overexpression of SIRT1.12 However, whether SIRT1 plays a role in the pathogenesis of arterial stiffening is not clear.
AMP-activated protein kinase (AMPK) is a serine/threonine protein kinase that serves as an energy sensor in the regulation of cellular metabolism. AMPKα is a catalytic subunit of AMPK, and its activity is regulated via phosphorylation.13–14 Activation of AMPKα improves endothelial function by suppressing oxidative stress.15–16 Some reports have indicated that SIRT1 regulates AMPKα activity,17,18 while others have shown that AMPK can also function as a SIRT1 activator by increasing the NAD+/NADH ratio.17,19 Endothelial nitric oxide synthase (eNOS) is a major source of nitric oxide (NO) in the vascular system20–21 and plays a critical role in regulating NO bioavailability and endothelial function. AMPK may mediate eNOS activity by regulating phosphorylation of eNOS22–23. Nevertheless, the regulation of SIRT1, AMPKα, and eNOS in the development of Klotho deficiency-induced aortic stiffening has not yet been assessed.
Klotho is an aging-suppressor gene that extends lifespan when overexpressed and shortens life span when disrupted.24–25 Klotho is predominately expressed in kidneys. In humans, the circulatory Klotho level declines with age.26 By age 70, the level of circulatory Klotho is about 50% of what it was at age 4026. In this study, we used a Klotho-haplodeficient mouse model for studying the underlying mechanism of arterial stiffness and hypertension. Specifically, we investigated the relationship of Klotho and SIRT1 in the pathogenesis of arterial stiffness and hypertension.
Methods
A detailed Methods section is available in the online Supplemental Methods and Data.
Clinical and laboratory data collection
We prospectively enrolled 14 essential hypertensive patients during their routine health screening. All patients were in a non-therapy situation (never having received any antihypertensive drug or had been under drug withdrawal for at least 1 week). Normotensive healthy control participants (systolic BP < 130 and diastolic BP < 80 mmHg) were also prospectively recruited and matched with hypertensive patients according to age, gender, and body mass index (BMI). Clinical data collected by physical examination included age, sex, height, weight, history of hypertension, systolic BP, and diastolic BP. Total cholesterol (TC), low-density lipoprotein (LDL), high-density lipoprotein (HDL), total triglyceride (TG), fasting blood glucose, and serum creatinine were determined by standard procedures. All clinical data were obtained from the First Affiliated Hospital of Chongqing Medical University (Chongqing, China). This study was approved by the Ethics Committee of The First Affiliated Hospital of Chongqing Medical University (Chongqing, China).
Circulatory Klotho measurement in human blood samples
Serum Klotho was measured using a commercial ELISA kit (Shanghai yuanye Bio-Technology Co., Ltd) by following the manufacturer’s protocol.
Animal study protocols
Briefly, 24 KL+/− mice and 24 wild-type (WT) mice (12 months old) in the 129Sv background were used. BP was measured biweekly at the age of 12–15 months by the tail-cuff method. At the age of 15 months, each group was divided into two subgroups. One subgroup received SRT1720 (15 mg/kg per day intraperitoneally; Medchem Express HY-15145), whereas the other group received an equal dose of vehicle (normal saline) and served as a control. During treatment, BP was measured twice a week using the tail-cuff method, and PWV was measured once a week by Doppler. On the 19th day of treatment, direct BP was assessed by direct intra-arterial cannulation, and plasma was collected for measuring circulatory Klotho. After perfusion, the aorta was collected and separated into three parts. One part was saved at −80°C for molecular assays, and the others were embedded in paraffin or optimal cutting temperature (OCT) compound for histological and immunohistochemical analysis.
Measurements of BP
BP was monitored by the volume-pressure recording (VPR) tail-cuff method as we described previously.7, 27–29 At the end of the experiment, BP was assessed from the arcus aortae via direct cannulation of a carotid artery under anesthesia (1% isoflurane) before euthanasia.
Measurement of pulse wave velocity (PWV)
Brachial-ankle pulse wave velocity (baPWV) was obtained in hypertensive patients and normotensive control (NC) participants in the supine position using an automated device (BP-203RPE III BP Monitor; Omron Healthcare, Inc. Japan).
Aortic PWV was assessed in mice as described previously.7, 27
Immunohistochemical analysis and histological examination of aortas
The procedures were described in our previous studies.30–31,32,33–34 For details, refer to the online Supplemental Methods and Data.
Western blots
Standardized protocols were used as we described recently,35–42 with details available in the online Supplemental Methods and Data.
Measurement of in situ superoxide production
In situ superoxide production was measured in aortas using the oxidation-sensitive dye dihydroethidium (DHE).34, 39, 43 For details, see the online Supplemental Methods and Data.
Quantification of NADPH oxidase activity
NADPH oxidase activity in aortas was assessed using the lucigenin chemiluminescence method. 39,44 The detailed procedure can be found in the online Supplemental Methods and Data.
Statistical analyses
BP was analyzed using one-way ANOVA repeated over time. All other data were analyzed by one-way ANOVA. The unpaired t-test was used for comparisons between two groups. The significance was set at a 95% confidence limit.
Results
Serum Klotho was decreased in patients with arterial stiffness and hypertension
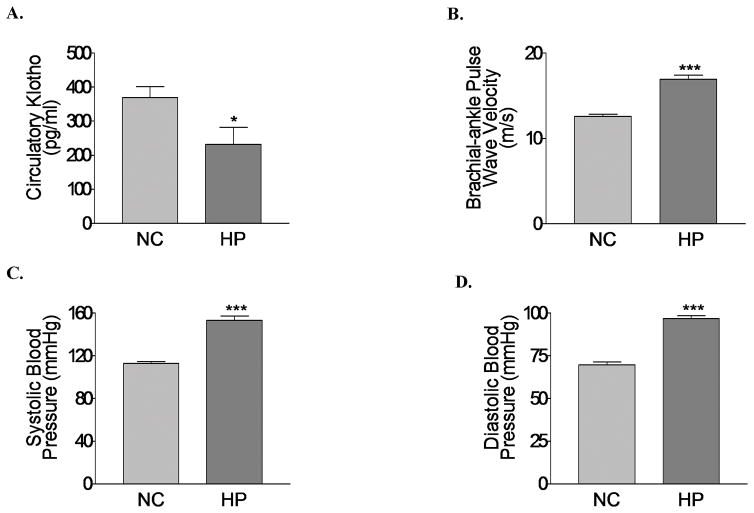
Serum Klotho levels were decreased by approximately 45% in patients with essential hypertension relative to those of healthy participants (Fig. 1A). The baPWV was increased significantly in hypertensive patients (Fig. 1B), which is associated with a significant elevation of BP compared with normal controls (Fig. 1C, D). This result suggests that a decrease in serum Klotho was associated with a significant increase in BP and baPWV in human. There were no significant differences in blood levels of TG, TC, LDL, HDL, glucose, and creatinine between hypertensive patients and healthy controls (Supplemental Table S1).
Figure 1. Serum Klotho was decreased in patients with arterial stiffness and hypertension.
(A) Serum levels of Klotho. (B) Brachial-ankle pulse wave velocity (baPWV) in hypertensive patients and normal controls. (C) Systolic blood pressure (SBP). (D) Diastolic blood pressure (DBP) in hypertensive patients and normal controls. NC, normal control; HP, hypertensive patients. n=13–14 participants/group. Data=means±SEM. *P<0.05, **P<0.01, *** P<0.001, ****P<0.0001 vs. NC.
Klotho deficiency caused arterial stiffness and spontaneous hypertension, which were associated with decreased expression and activity of SIRT1 in aorta
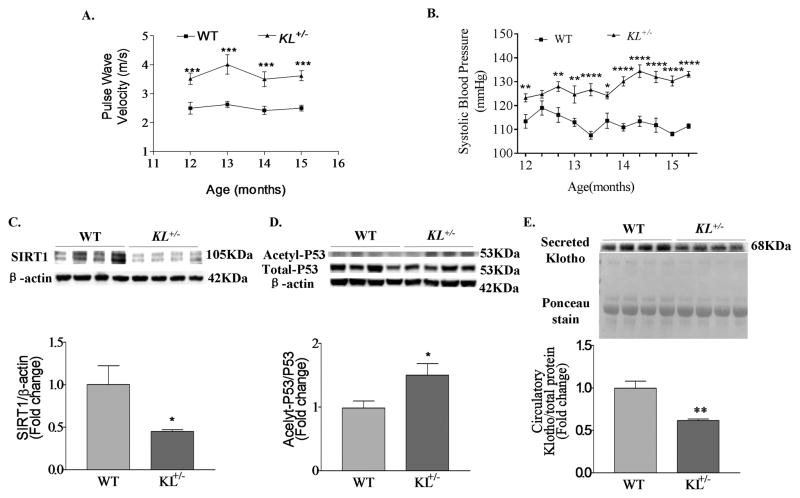
PWV, an important and reliable measure of arterial stiffness, was increased significantly in KL+/− mice by the age of 12–15 months (Fig. 2A). Systolic and diastolic BP were also elevated significantly in KL+/− mice compared with WT mice (Fig. 2B, Fig. S1). Interestingly, SIRT1 protein expression was decreased significantly in the aortas of KL+/− mice (Fig. 2C). p53 is a known downstream target of SIRT1, and the ratio of acetyl-p53 to total p53 is an index of SIRT1 activity. This ratio was increased significantly in the aortas of KL+/− mice (Fig. 2D), suggesting that Klotho deficiency suppresses SIRT1 activity. Western blot analysis confirmed a significant decrease in the plasma level (by ~45%) of Klotho protein in KL+/− mice (Fig. 2E). These results reveal, for the first time, that SIRT1 expression and activity are down-regulated in aorta due to Klotho deficiency during the development of arterial stiffness and hypertension.
Figure 2. Klotho deficiency caused arterial stiffness and spontaneous hypertension, which were associated with decreased expression and activity of SIRT1 in aorta.
(A) Time course of pulse wave velocity (PWV) and (B) systolic blood pressure (SBP) in WT and KL+/− mice, n=10–12 mice/group. (C) Representative western blot bands and quantitative analysis of SIRT1 protein expression in aortas. (D) Representative western blot bands and quantitative analysis of Acetyl-p53 and total p53 in aortas. SIRT1 activity is expressed as the relative ratio of Acetyl-p53/total P53. (E) Representative western blot bands and quantitative analysis of plasma Klotho. Total protein with Ponceau staining served as loading control. Protein expression was normalized to the loading control, and the relative expression calculated as the fold change relative to the experimental control (WT). n=6 animals/group for western blot analysis. Data=means±SEM.*P<0.05, **P<0.01, ***P<0.001, ****P<0.0001 vs. WT.
Activation of SIRT1 by SRT1720 attenuated arterial stiffening and hypertension in KL+/− mice without affecting circulatory Klotho levels
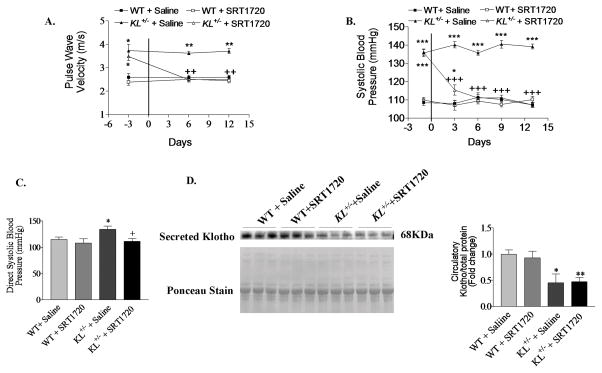
We next assessed wither pharmacological activation of SIRT1 affects arterial stiffness and hypertension in KL+/− mice. Daily intraperitoneal injection of SRT1720 (15 mg/kg), an activator of SIRT1, attenuated Klotho deficiency-induced elevation of PWV and BP to the control level within one week (Fig. 3A–B, Fig. S2A). SRT1720 did not affect PWV and BP significantly in WT mice, and direct BP measured by intra-arterial cannulation confirmed these results (Fig. 3C, Fig. S2B). On the other hand, body weights were not affected by treatment with SRT1720 (data not shown). The plasma Klotho level was not altered by SRT1720 treatment in either WT or KL+/− mice (Fig. 3D), indicating that Klotho activity lies upstream of SIRT1. These results suggest that downregulation of SIRT1 is involved in Klotho deficiency-induced arterial stiffness and hypertension.
Figure 3. Activation of SIRT1 attenuated arterial stiffening and hypertension in KL+/− mice without affecting levels of circulatory Klotho.
(A) PWV and (B) Systolic BP in KL+/− mice. (C) Direct BP measured by intra-arterial cannulation under anesthesia. (D) Representative western blot bands and quantitative analysis of plasma Klotho. Protein expression was normalized to the loading control, and the relative expression calculated as the fold change relative to the experimental control (WT+ Saline). n=10–12 animals/group. Data=means±SEM. *P<0.05, ** P<0.01, ***P<0.001 vs. WT + Saline; +P<0.05, ++ P<0.01, +++P<0.001 vs. KL+/− + Saline.
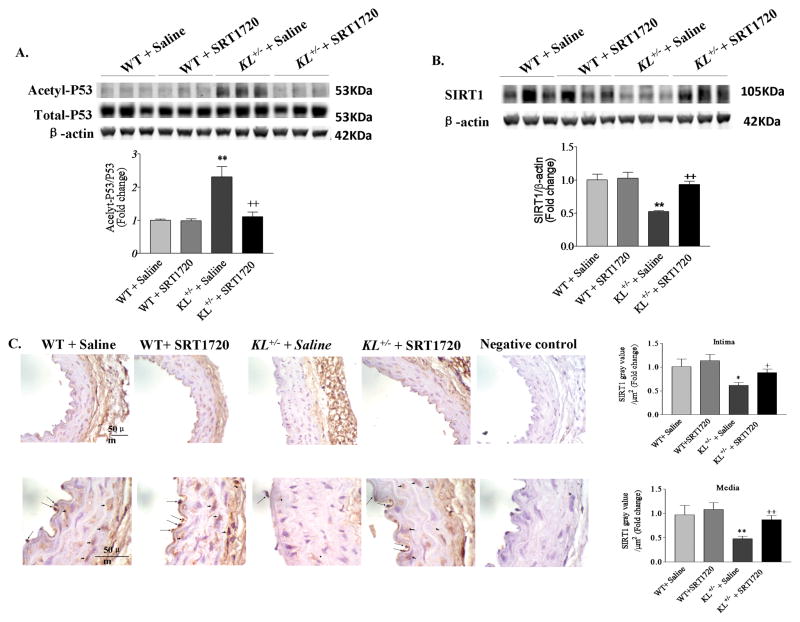
Activation of SIRT1 by SRT1720 rescued the downregulation of SIRT1 activity and protein expression in the aortas of KL+/− mice
Treatment with SRT1720 attenuated the ratio of acetyl-p53 to total p53 in the aortas of KL+/− mice to the control level, indicating that SRT1720 rescues the Klotho deficiency-induced downregulation of SIRT1 activity (Fig. 4A). Unexpectedly, SRT1720 also abolished downregulation of SIRT1 protein expression in the aortas of KL+/− mice (Fig. 4B), while SRT1720 did not alter SIRT1 expression or activity in the aortas of WT mice. To gain a better understanding of the cell types that express SIRT1, we assessed the localization of SIRT1 in the aorta using immunohistochemistry. SIRT1 was abundantly and predominantly expressed in the nuclei of both endothelial cells (ECs) and smooth muscle cells (SMCs, Fig. 4C). The results show that SRT1720 effectively activated SIRT1 by increasing the abundance of SIRT1 expression in both SMCs and ECs in the aortas of Klotho-deficient mice.
Figure 4. SRT1720 rescued the downregulation of SIRT1 activity and protein expression in the aortas of KL+/− mice.
(A) Representative western blot bands of Acetyl-P53 and total P53 and the quantification of SIRT1 activity. Data were expressed as the ratio of Acetyl-p53/total P53. (B) Representative western blot bands and quantitative analysis of SIRT1 protein expression in aortas. Protein expression was normalized to β-actin, and the relative expression calculated as the fold change relative to the control (WT+ Saline). (C) Representative photomicrographs of immunohistochemical analysis of SIRT1 expression in aortic sections. The negative control was sample in the absence of the primary antibody. Brown staining indicates positive SIRT1 staining, arrows indicate positively stained endothelial cells (ECs), and arrowheads indicate positively stained smooth muscle cells (SMCs). Semi-quantitative analysis of SIRT1-positive staining in the intima and media of the aortic wall (data were calculated as fold changes of the WT + Saline group). n=6 animals/group. Data=means±SEM. *P<0.05, **P<0.01 vs. WT + Saline; +P<0.05, ++P<0.01 vs. KL+/− + Saline.
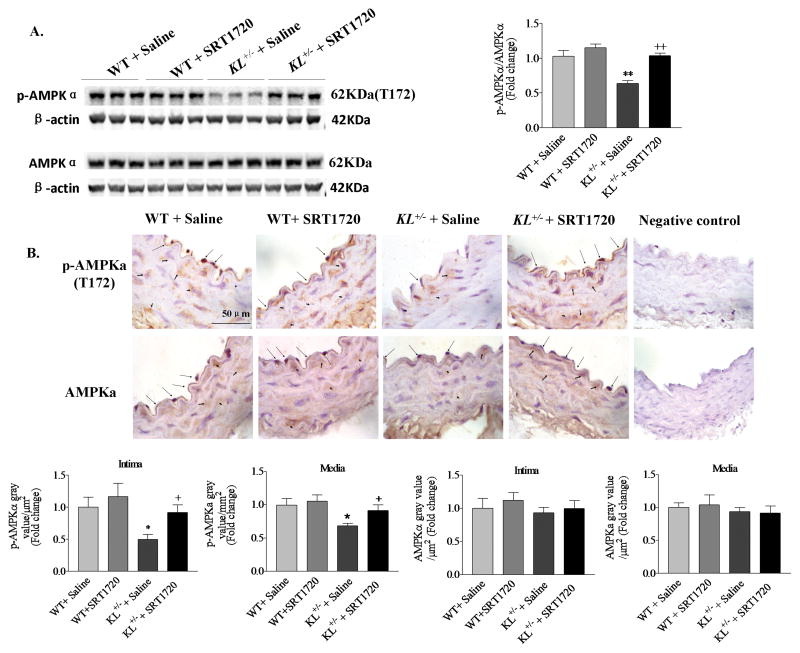
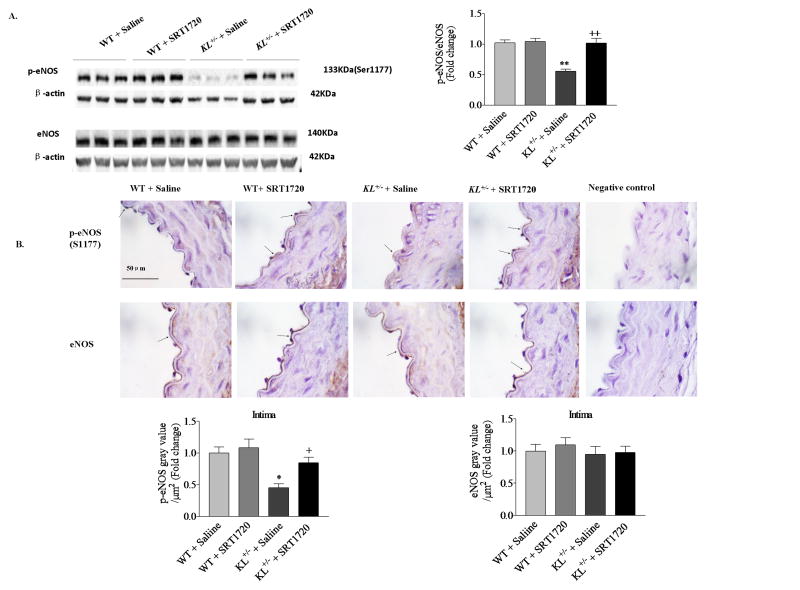
Activation of SIRT1 by SRT1720 abolished downregulation of AMPKα and eNOS activities in the aortas of KL+/− mice
We assessed protein expression and activity of AMP-activated protein kinase α (AMPKα) and endothelial nitric oxide synthase (eNOS). Protein expression of phosphorylated AMPKα (p-AMPKα) and phosphorylated eNOS (p-eNOS) were decreased significantly, while total protein expression of AMPKα and eNOS were not altered in the aortas of KL+/− mice (Fig. 5A, B), suggesting that Klotho deficiency downregulates AMPKα and eNOS activities. Interestingly, treatment with SRT1720 abolished the downregulation of AMPKα and eNOS activity in KL+/− mice, suggesting that the Klotho deficiency-induced downregulation of AMPKα and eNOS activities is due to suppression of SIRT1. SRT1720 treatment did not affect the expression or activity of AMPKα or eNOS in WT mice (Fig. 5A, B).
Figure 5. Activation of SIRT1 by SRT1720 enhanced AMPKα activity in aortas.
(A) Representative western blot bands and quantitative analysis of p-AMPKα and AMPKα in aortas. Protein expression was normalized to β-actin, and the relative expression was calculated as the fold change relative to the control (WT+Saline). (B) Representative photomicrographs of immunohistochemical analysis of p-AMPKα and AMPKα in aortic sections. Brown staining indicates positive staining, arrows indicate positively stained endothelial cells (ECs), and arrowheads indicate positively stained smooth muscle cells (SMCs). Semi-quantitative analysis of p-AMPKα- and AMPKα-positive staining in the intima and media of aortas (data were calculated as fold changes of the WT + Saline group). n=6 animals/group. Data=means±SEM. *P<0.05, *P<0.01 vs. WT + Saline; +P<0.05, ++P<0.01 vs. KL+/− + Saline.
IHC analysis showed that AMPKα and p-AMPKα proteins were abundantly expressed in both ECs and SMCs throughout the intima and tunica media (Fig. 5B). p-AMPKα was expressed in both the cytoplasm and nucleus in ECs and mainly in the cytoplasm in SMCs. Semi-quantitative analysis further confirmed that p-AMPKα expression was downregulated in both ECs and SMCs in KL+/− mice, and this effect was eliminated by SRT1720 (Fig. 5B). By contrast, eNOS and p-eNOS were found only in ECs but not in SMCs (Fig. 6B). p-eNOS was decreased in the ECs of KL+/− mice, and this effect was abolished by SRT1720 (Fig. 6B). These results suggest that activation of SIRT1 by SRT1720 rescues the Klotho deficiency-induced downregulation of AMPKα and eNOS activities in aortas.
Figure 6. Activation of SIRT1 by SRT1720 enhanced eNOS activity in aortas.
(A) Representative western blot bands and quantitative analysis of p-eNOS and eNOS in aortas. Protein expression was normalized to β-actin, and the relative expression calculated as the fold change relative to the control (WT + Saline). (B) Representative photomicrographs of immunohistochemical analysis of p-eNOS and eNOS in aortic sections. Brown staining indicates positive staining, and arrows indicate positively stained endothelial cells (ECs). Semi-quantitative analysis of p-eNOS- and eNOS-positive staining in aortic intima (data were calculated as fold change of the WT + Saline group). n=6 mice/group. Data=means±SEM. *P<0.05, **P<0.01 vs. WT + Saline; +P<0.05, ++P<0.01 vs. KL+/− + Saline.
Activation of SIRT1 by SRT1720 attenuated in situ superoxide levels in the aortas of KL+/− mice
Arterial stiffness is associated with increased generation of reactive oxygen species (ROS) in the vasculature.45 To determine whether SIRT1 activation affects NADPH oxidase activity and superoxide levels, we assessed NADPH oxidase activity and in situ dihydroethidium (DHE) staining in aortas. Superoxide production (red fluorescence, DHE staining, Fig. S3A) and NADPH oxidase activity (Fig. S3B) were increased in the aortas of KL+/− mice relative to WT mice. Interestingly, NADPH oxidase activity and vascular superoxide levels were significantly decreased in the aortas of KL+/− mice treated with SRT1720, suggesting that upregulation of NADPH oxidase activity and superoxide levels are likely due to suppression of SIRT1.
Activation of SIRT1 by SRT1720 attenuated Klotho-deficiency-induced collagen deposition and elastin fragmentation in aortas
Passive aortic stiffness largely depends on the matrix composition within the vascular medial layer46. Masson’s trichrome staining showed that collagen deposition (blue) was increased in the medial layer of the aortas in KL+/− mice, and this effect was abolished by SRT1720 (Fig. S4A). Elastin staining showed that the number of elastic fiber breaks was increased in the aortic walls of KL+/− mice, and this was significantly attenuated by activation of SIRT1 (Fig. S4B).
Western blot analysis confirmed the enhanced expression of collagen I in the aortas of KL+/− mice, which was eliminated by treatment with SRT1720 (Fig. S4C). Conversely, the elastin level was significantly decreased in the aortas of Klotho-deficient mice, and this level which was restored by activation of SIRT1 (Fig. S4D).
Discussion
Aortic stiffness is an independent risk factor for hypertension, stroke, and myocardial infarction.4 However, the etiology and pathogenesis of aortic stiffness remains largely unknown. Klotho was originally discovered as an aging-suppressor gene,47 and mutation of the Klotho gene results in multiple premature aging phenotypes and shortened lifespan24. In this study, we provided the first evidence that aortic stiffness and hypertension are associated with a significant decrease in circulatory Klotho protein levels in humans (Fig. 1). We further demonstrated in an animal model that Klotho deficiency is likely to be an important factor that contributes to the pathogenesis of arterial stiffening and hypertension, because haplodeficiency of Klotho (KL+/−) induces significant increases in PWV and BP (Fig. 2). This finding is significant, because it points to a new direction for understanding the pathogenesis of arterial stiffening and hypertension. A recent Framingham study showed that large-artery stiffness precedes the development of hypertension, suggesting that arterial stiffening may be the cause of hypertension.6 Several longitudinal studies have demonstrated that arterial stiffness predicts an increase in systolic blood pressure and incident hypertension.48–49
Arterial stiffness is one of the earliest detectable manifestations of adverse structural and functional changes within the vessel wall, which eventually leads to stroke and ischemic heart disease50. The prevalence of arterial stiffness and hypertension continues to increase, especially in the aged population1–2. Unfortunately, there is no cure for the disease, due to its unknown etiology. The currently available antihypertensive drugs were mainly designed to reduce peripheral resistance and are not adequate to alter the pathological processes of vascular remodeling or stiffening. Our study suggests that Klotho may be an important etiological factor and a potential interventional target for arterial remodeling and stiffness. Our findings also provide a strong rationale for further investigating whether Klotho supplements can attenuate arterial stiffening and associated cardiovascular mortality.
The Klotho gene is primarily expressed in the distal tubular epithelial cells of the kidneys and the choroid plexus of the brain.47 One of the interesting findings of this study is that a Klotho gene haplodeficiency (KL+/−) suppresses SIRT1 expression and activity in aortas (Fig. 4). This result is interesting, because, although Klotho is not expressed in the vasculature,25,47 Klotho deficiency downregulated vascular SIRT1 expression and activity. This finding supports the notion that Klotho functions as a hormone.30,47 Indeed, the circulatory Klotho level was decreased by ~50% in KL+/− mice (Fig. 2), which was not affected by activation of SIRT1 (Fig. 3). Therefore, Klotho likely serves as an upstream regulator of vascular SIRT1 in the vasculature. The circulatory Klotho level is important in the regulation of cardiovascular function, because it has direct access to vascular endothelial and smooth muscle cells.30 It is noteworthy that the Klotho deficiency-induced decrease in SIRT1 activity is proportional to that of SIRT1 protein expression in aortas (Fig. 4), suggesting that Klotho regulates SIRT1 activity partially by regulating its protein expression. The limitation of this in vivo study is that it does not address how Klotho regulates SIRT1 protein expression. On the other hand, the Klotho protein entails the property of glycosylation,47 and this moiety may functionally interact with SIRT1 and regulate its activity. This hypothesis, however, needs to be validated. Nevertheless, this study reveals, for the first time, that Klotho regulates SIRT1 expression and activity.
Klotho deficiency led to a decreased elastin/collagen ratio, which is apparently due to an enhanced degradation of elastin and increased accumulation of collagen (Fig. S4), which is stiffer than elastin, and this structural remodeling contributes to the pathogenesis of arterial stiffening. One of the major findings of this study is that activation of SIRT1 by SRT1720 reverses Klotho deficiency-induced elevation of PWV and BP (Fig. 3A, B), suggesting for the first time that downregulation of SIRT1 activity mediates Klotho deficiency-induced arterial stiffening and hypertension. The beneficial effects of SRT1720 are manifested by a largely attenuated arterial collagen deposition and elastin degradation (Fig. S4).
It is noteworthy that pharmacological activation of SIRT1 decreased arterial stiffening and hypertension within one week of treatment (Fig. 3), which is sooner than we expected. The early and quick drop in PWV and BP may be partially attributed to the relaxation of blood vessels. Indeed, diastolic BP, which largely reflects vascular resistance, was effectively attenuated by SRT1720. This result suggests that there may also be a functional component of arterial stiffness, i.e., increased vascular tension in KL+/− mice which may be attributed to decreased AMPKα and eNOS activities (Figs. 5 and 6). Consistent with this interpretation, the Klotho deficiency-induced downregulation of AMPKα and eNOS activities in ECs were largely rescued by treatment with SRT1720. Therefore, this study demonstrates that activation of SIRT1 functionally interacts with AMPKα and upregulates its activity (phosphorylation), which, in turn, activates eNOS22–23, leading to vasorelaxation (Fig. S5). By contrast, the structural recovery of blood vessels is a relatively slow process, although it contributes to attenuation of arterial stiffening and hypertension by SRT1720. It should be mentioned that although activation of SIRT1 increases AMPKα and eNOS activity and decreases NADPH oxidase activity, we cannot exclude the possibility that changes in the downstream factors of SIRT1 may also be partially secondary to reduction of hypertension.
The recovery of structural remodeling by SRT1720 may be partially attributed to the attenuation of superoxide upregulation in the aortas of KL+/− mice (Fig. S3, Fig. S4), because increased ROS and oxidative stress contribute to vascular remodeling. It is noteworthy that NADPH oxidase activity and superoxide levels were increased in aortas due to Klotho deficiency (KL+/−, Fig. S3). Interestingly, SIRT1 may be involved in Klotho deficiency-induced upregulation of NADPH oxidase activity and superoxide generation in aortas, which were both blocked by SIRT1 activation. The effects of SIRT1 activation on NADPH oxidase activity may be mediated by AMPKα (Fig. S5), because AMPKα regulates NADPH oxidase activity.15–16 Knockout of AMPKα upregulates NADPH oxidase activity, leading to endothelial dysfunction.15–16
We used Klotho+/− mice which mimics a half Klotho reduction in hypertensive patients (Fig. 1). Klotho homozygous (−/−) mice develop extensive aging phenotypes and die before the age of 8 weeks.47 Klotho homozygous mice also demonstrate severe hyperphosphatemia, emphysema, and soft tissue calcification.25, 47 As a result, klotho homozygous mice were not used for this study.
Perspective
To our knowledge, this is the first study demonstrating that Klotho deficiency downregulates SIRT1 expression and activity in aortic endothelial and smooth muscle cells, which may mediate Klotho deficiency-induced arterial stiffness and hypertension. This finding is significant, as it points to a new direction for understanding the pathogenesis of arterial stiffening. Supplementing anti-aging Klotho protein or pharmacological activation of SIRT1 may be effective therapeutic approaches for arterial remodeling and hypertension.
Supplementary Material
Novelty and Significance.
1. What is new?
It is new and interesting that haplodeficiency of Klotho gene downregulates SIRT1 activity in vascular endothelial and smooth muscle cells.
This study demonstrates, for the first time, that activation of SIRT1 attenuates Klotho deficiency-induced arterial stiffness and hypertension.
2. What is relevant?
It is significant that a decrease in plasma Klotho is associated with arterial stiffening in hypertensive patients.
This study reveals that pharmacological activation of SIRT1 may be an effective therapeutic strategy for arterial stiffness, an independent risk factor for cardiovascular mortality and morbidity.
3. Summary
This study provides the first evidence that Klotho deficiency downregulates SIRT1 activity in arterial endothelial and smooth muscle cells. Pharmacological activation of SIRT1 may be an effective therapeutic strategy for arterial stiffness and hypertension.
Acknowledgments
Source of Funding
This work was supported by NIH grants R01 HL118558, DK093403, HL122166, HL116863, HL105302, HL102074, and AG049780. This publication was made possible by NIH Grant Number 9P20GM104934-06 from the Center of Biomedical Research Excellence (COBRE) Program of the National Institute of General Medical Sciences.
Footnotes
Disclosures
None.
References
- 1.AlGhatrif M, Strait JB, Morrell CH, Canepa M, Wright J, Elango P, Scuteri A, Najjar SS, Ferrucci L, Lakatta EG. Longitudinal trajectories of arterial stiffness and the role of blood pressure: The baltimore longitudinal study of aging. Hypertension. 2013;62:934–941. doi: 10.1161/HYPERTENSIONAHA.113.01445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rosano C, Watson N, Chang Y, Newman AB, Aizenstein HJ, Du Y, Venkatraman V, Harris TB, Barinas-Mitchell E, Sutton-Tyrrell K. Aortic pulse wave velocity predicts focal white matter hyperintensities in a biracial cohort of older adults. Hypertension. 2013;61:160–165. doi: 10.1161/HYPERTENSIONAHA.112.198069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC, Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT, Jr, Narva AS, Ortiz E. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the eighth joint national committee (jnc 8) JAMA. 2014;311:507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 4.Sun Z. Aging, arterial stiffness, and hypertension. Hypertension. 2015;65:252–256. doi: 10.1161/HYPERTENSIONAHA.114.03617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coutinho T, Turner ST, Kullo IJ. Aortic pulse wave velocity is associated with measures of subclinical target organ damage. JACC Cardiovas Imag. 2011;4:754–761. doi: 10.1016/j.jcmg.2011.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaess BM, Rong J, Larson MG, Hamburg NM, Vita JA, Levy D, Benjamin EJ, Vasan RS, Mitchell GF. Aortic stiffness, blood pressure progression, and incident hypertension. JAMA. 2012;308:875–881. doi: 10.1001/2012.jama.10503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen K, Zhou X, Sun Z. Haplodeficiency of klotho gene causes arterial stiffening via upregulation of scleraxis expression and induction of autophagy. Hypertension. 2015;66:1006–1013. doi: 10.1161/HYPERTENSIONAHA.115.06033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zu Y, Liu L, Lee MY, Xu C, Liang Y, Man RY, Vanhoutte PM, Wang Y. Sirt1 promotes proliferation and prevents senescence through targeting lkb1 in primary porcine aortic endothelial cells. Circ Res. 2010;106:1384–1393. doi: 10.1161/CIRCRESAHA.109.215483. [DOI] [PubMed] [Google Scholar]
- 9.Zarzuelo MJ, Lopez-Sepulveda R, Sanchez M, Romero M, Gomez-Guzman M, Ungvary Z, Perez-Vizcaino F, Jimenez R, Duarte J. Sirt1 inhibits nadph oxidase activation and protects endothelial function in the rat aorta: Implications for vascular aging. Biochem Pharmacol. 2013;85:1288–1296. doi: 10.1016/j.bcp.2013.02.015. [DOI] [PubMed] [Google Scholar]
- 10.Nisoli E, Tonello C, Cardile A, Cozzi V, Bracale R, Tedesco L, Falcone S, Valerio A, Cantoni O, Clementi E, Moncada S, Carruba MO. Calorie restriction promotes mitochondrial biogenesis by inducing the expression of enos. Science. 2005;310:314–317. doi: 10.1126/science.1117728. [DOI] [PubMed] [Google Scholar]
- 11.Stein S, Lohmann C, Schafer N, Hofmann J, Rohrer L, Besler C, Rothgiesser KM, Becher B, Hottiger MO, Boren J, McBurney MW, Landmesser U, Luscher TF, Matter CM. Sirt1 decreases lox-1-mediated foam cell formation in atherogenesis. Eur Heart J. 2010;31:2301–2309. doi: 10.1093/eurheartj/ehq107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gao P, Xu TT, Lu J, Li L, Xu J, Hao DL, Chen HZ, Liu DP. Overexpression of sirt1 in vascular smooth muscle cells attenuates angiotensin ii-induced vascular remodeling and hypertension in mice. J Mol Med. 2014;92:347–357. doi: 10.1007/s00109-013-1111-4. [DOI] [PubMed] [Google Scholar]
- 13.Ruderman NB, Carling D, Prentki M, Cacicedo JM. Ampk, insulin resistance, and the metabolic syndrome. J Clin Invest. 2013;123:2764–2772. doi: 10.1172/JCI67227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Srivastava RA, Pinkosky SL, Filippov S, Hanselman JC, Cramer CT, Newton RS. Amp-activated protein kinase: An emerging drug target to regulate imbalances in lipid and carbohydrate metabolism to treat cardio-metabolic diseases. J Lipid Res. 2012;53:2490–2514. doi: 10.1194/jlr.R025882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang S, Zhang M, Liang B, Xu J, Xie Z, Liu C, Viollet B, Yan D, Zou MH. Ampkalpha2 deletion causes aberrant expression and activation of nad(p)h oxidase and consequent endothelial dysfunction in vivo: Role of 26s proteasomes. Circ Res. 2010;106:1117–1128. doi: 10.1161/CIRCRESAHA.109.212530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zou MH, Wu Y. Amp-activated protein kinase activation as a strategy for protecting vascular endothelial function. Clin Exp Pharmacol Physiol. 2008;35:535–545. doi: 10.1111/j.1440-1681.2007.04851.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Canto C, Gerhart-Hines Z, Feige JN, Lagouge M, Noriega L, Milne JC, Elliott PJ, Puigserver P, Auwerx J. Ampk regulates energy expenditure by modulating nad+ metabolism and sirt1 activity. Nature. 2009;458:1056–1060. doi: 10.1038/nature07813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hou X, Xu S, Maitland-Toolan KA, Sato K, Jiang B, Ido Y, Lan F, Walsh K, Wierzbicki M, Verbeuren TJ, Cohen RA, Zang M. Sirt1 regulates hepatocyte lipid metabolism through activating amp-activated protein kinase. J Biol Chem. 2008;283:20015–20026. doi: 10.1074/jbc.M802187200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Canto C, Auwerx J. Pgc-1alpha, sirt1 and ampk, an energy sensing network that controls energy expenditure. Curr Opin Lipid. 2009;20:98–105. doi: 10.1097/MOL.0b013e328328d0a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Youn JY, Gao L, Cai H. The p47phox- and nadph oxidase organiser 1 (noxo1)-dependent activation of nadph oxidase 1 (nox1) mediates endothelial nitric oxide synthase (enos) uncoupling and endothelial dysfunction in a streptozotocin-induced murine model of diabetes. Diabetologia. 2012;55:2069–2079. doi: 10.1007/s00125-012-2557-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li Q, Youn JY, Cai H. Mechanisms and consequences of endothelial nitric oxide synthase dysfunction in hypertension. J Hypertens. 2015;33:1128–1136. doi: 10.1097/HJH.0000000000000587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen ZP, Mitchelhill KI, Michell BJ, Stapleton D, Rodriguez-Crespo I, Witters LA, Power DA, Ortiz de Montellano PR, Kemp BE. Amp-activated protein kinase phosphorylation of endothelial no synthase. FEBS Lett. 1999;443:285–289. doi: 10.1016/s0014-5793(98)01705-0. [DOI] [PubMed] [Google Scholar]
- 23.Youn JY, Wang T, Cai H. An ezrin/calpain/pi3k/ampk/enoss1179 signaling cascade mediating vegf-dependent endothelial nitric oxide production. Circ Res. 2009;104:50–59. doi: 10.1161/CIRCRESAHA.108.178467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuro-o M, Matsumura Y, Aizawa H, Kawaguchi H, Suga T, Utsugi T, Ohyama Y, Kurabayashi M, Kaname T, Kume E, Iwasaki H, Iida A, Shiraki-Iida T, Nishikawa S, Nagai R, Nabeshima YI. Mutation of the mouse klotho gene leads to a syndrome resembling ageing. Nature. 1997;390:45–51. doi: 10.1038/36285. [DOI] [PubMed] [Google Scholar]
- 25.Wang Y, Sun Z. Current understanding of klotho. Ageing Res Rev. 2009;8:43–51. doi: 10.1016/j.arr.2008.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xiao NM, Zhang YM, Zheng Q, Gu J. Klotho is a serum factor related to human aging. Chin Med J. 2004;117:742–747. [PubMed] [Google Scholar]
- 27.Lin Y, Chen J, Sun Z. Antiaging gene klotho deficiency promoted high-fat diet-induced arterial stiffening via inactivation of amp-activated protein kinase. Hypertension. 2016;67:564–573. doi: 10.1161/HYPERTENSIONAHA.115.06825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhou X, Chen K, Lei H, Sun Z. Klotho gene deficiency causes salt-sensitive hypertension via monocyte chemotactic protein-1/cc chemokine receptor 2-mediated inflammation. J Am Soc Nephrol. 2015;26:121–132. doi: 10.1681/ASN.2013101033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhou X, Chen K, Wang Y, Schuman M, Lei H, Sun Z. Antiaging gene klotho regulates adrenal cyp11b2 expression and aldosterone synthesis. J Am Soc Nephrol. 2015 doi: 10.1681/ASN.2015010093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang Y, Sun Z. Klotho gene delivery prevents the progression of spontaneous hypertension and renal damage. Hypertension. 2009;54:810–817. doi: 10.1161/HYPERTENSIONAHA.109.134320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang X, Skelley L, Cade R, Sun Z. Aav delivery of mineralocorticoid receptor shrna prevents progression of cold-induced hypertension and attenuates renal damage. Gene Ther. 2006;13:1097–1103. doi: 10.1038/sj.gt.3302768. [DOI] [PubMed] [Google Scholar]
- 32.Sun Z, Bello-Roufai M, Wang X. Rnai inhibition of mineralocorticoid receptors prevents the development of cold-induced hypertension. Am J Physiol Heart Circ Physiol. 2008;294:H1880–1887. doi: 10.1152/ajpheart.01319.2007. [DOI] [PubMed] [Google Scholar]
- 33.Lin Y, Sun Z. In vivo pancreatic beta-cell-specific expression of antiaging gene klotho: A novel approach for preserving beta-cells in type 2 diabetes. Diabetes. 2015;64:1444–1458. doi: 10.2337/db14-0632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lin Y, Sun Z. Antiaging gene klotho attenuates pancreatic beta-cell apoptosis in type 1 diabetes. Diabetes. 2015;64:4298–4311. doi: 10.2337/db15-0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fan J, Sun Z. The antiaging gene klotho regulates proliferation and differentiation of adipose-derived stem cells. Stem Cells. 2016;34:1615–1625. doi: 10.1002/stem.2305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang Y, Sun Z. Antiaging gene klotho regulates endothelin-1 levels and endothelin receptor subtype b expression in kidneys of spontaneously hypertensive rats. J Hypertens. 2014;32:1629–1636. doi: 10.1097/HJH.0000000000000233. [DOI] [PubMed] [Google Scholar]
- 37.Lin Y, Kuro-o M, Sun Z. Genetic deficiency of anti-aging gene klotho exacerbates early nephropathy in stz-induced diabetes in male mice. Endocrinology. 2013;154:3855–3863. doi: 10.1210/en.2013-1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen J, Lin Y, Sun Z. Deficiency in the anti-aging gene klotho promotes aortic valve fibrosis through ampkalpha-mediated activation of runx2. Aging Cell. 2016 May 31; doi: 10.111/acel.1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Crosswhite P, Sun Z. Inhibition of phosphodiesterase-1 attenuates cold-induced pulmonary hypertension. Hypertension. 2013;61:585–592. doi: 10.1161/HYPERTENSIONAHA.111.00676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lin Y, Sun Z. Thyroid hormone promotes insulin-induced glucose uptake by enhancing akt phosphorylation and vamp2 translocation in 3t3-l1 adipocytes. J Cell Physiol. 2011;226:2625–2632. doi: 10.1002/jcp.22613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lin Y, Sun Z. Thyroid hormone potentiates insulin signaling and attenuates hyperglycemia and insulin resistance in a mouse model of type 2 diabetes. Br J Pharmacol. 2011;162:597–610. doi: 10.1111/j.1476-5381.2010.01056.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang X, Sun Z. Thyroid hormone induces artery smooth muscle cell proliferation: Discovery of a new tralpha1-nox1 pathway. J Cell Mol Med. 2010;14:368–380. doi: 10.1111/j.1582-4934.2008.00489.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang X, Skelley L, Wang B, Mejia A, Sapozhnikov V, Sun Z. Aav-based rnai silencing of nadph oxidase gp91(phox) attenuates cold-induced cardiovascular dysfunction. Hum Gene Ther. 2012;23:1016–1026. doi: 10.1089/hum.2012.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dammanahalli JK, Sun Z. Endothelin (et)-1 inhibits nicotinamide adenine dinucleotide phosphate oxidase activity in human abdominal aortic endothelial cells: A novel function of etb1 receptors. Endocrinology. 2008;149:4979–4987. doi: 10.1210/en.2008-0199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Harvey A, Montezano AC, Touyz RM. Vascular biology of ageing-implications in hypertension. J Mol Cell Cardiol. 2015;83:112–121. doi: 10.1016/j.yjmcc.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Raaz U, Schellinger IN, Chernogubova E, Warnecke C, Kayama Y, Penov K, Hennigs JK, Salomons F, Eken S, Emrich FC, Zheng WH, Adam M, Jagger A, Nakagami F, Toh R, Toyama K, Deng A, Buerke M, Maegdefessel L, Hasenfuss G, Spin JM, Tsao PS. Transcription factor runx2 promotes aortic fibrosis and stiffness in type 2 diabetes mellitus. Circ Res. 2015;117:513–524. doi: 10.1161/CIRCRESAHA.115.306341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Xu Y, Sun Z. Molecular basis of klotho: From gene to function in aging. Endocr Rev. 2015;36:174–193. doi: 10.1210/er.2013-1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liao D, Arnett DK, Tyroler HA, Riley WA, Chambless LE, Szklo M, Heiss G. Arterial stiffness and the development of hypertension. The aric study. Hypertension. 1999;34:201–206. doi: 10.1161/01.hyp.34.2.201. [DOI] [PubMed] [Google Scholar]
- 49.Najjar SS, Scuteri A, Shetty V, Wright JG, Muller DC, Fleg JL, Spurgeon HP, Ferrucci L, Lakatta EG. Pulse wave velocity is an independent predictor of the longitudinal increase in systolic blood pressure and of incident hypertension in the baltimore longitudinal study of aging. J Am Coll Cardiol. 2008;51:1377–1383. doi: 10.1016/j.jacc.2007.10.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cavalcante JL, Lima JA, Redheuil A, Al-Mallah MH. Aortic stiffness: Current understanding and future directions. J Am Coll Cardiol. 2011;57:1511–1522. doi: 10.1016/j.jacc.2010.12.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.