Summary
This guideline aims to ensure that patients admitted to hospital for elective surgery are known to have blood pressures below 160 mmHg systolic and 100 mmHg diastolic in primary care. The objective for primary care is to fulfil this criterion before referral to secondary care for elective surgery. The objective for secondary care is to avoid spurious hypertensive measurements. Secondary care should not attempt to diagnose hypertension in patients who are normotensive in primary care. Patients who present to pre‐operative assessment clinics without documented primary care blood pressures should proceed to elective surgery if clinic blood pressures are below 180 mmHg systolic and 110 mmHg diastolic.
Recommendations
General practitioners should refer patients for elective surgery with mean blood pressures in primary care in the past 12 months less than 160 mmHg systolic and less than 100 mmHg diastolic.
Secondary care should accept referrals that document blood pressures below 160 mmHg systolic and below 100 mmHg diastolic in the past 12 months.
Pre‐operative assessment clinics need not measure the blood pressure of patients being prepared for elective surgery whose systolic and diastolic blood pressures are documented below 160/100 mmHg in the referral letter from primary care.
General practitioners should refer hypertensive patients for elective surgery after the blood pressure readings are less than 160 mmHg systolic and less than 100 mmHg diastolic. Patients may be referred for elective surgery if they remain hypertensive despite optimal antihypertensive treatment or if they decline antihypertensive treatment.
Surgeons should ask general practitioners to supply primary care blood pressure readings from the last 12 months if they are undocumented in the referral letter.
Pre‐operative assessment staff should measure the blood pressure of patients who attend clinic without evidence of blood pressures less than 160 mmHg systolic and 100 mmHg diastolic being documented by primary care in the preceding 12 months. (We detail the recommended method for measuring non‐invasive blood pressure accurately, although the diagnosis of hypertension is made in primary care.)
Elective surgery should proceed for patients who attend the pre‐operative assessment clinic without documentation of normotension in primary care if their blood pressure is less than 180 mmHg systolic and 110 mmHg diastolic when measured in clinic.
The disparity between the blood pressure thresholds for primary care (160/100 mmHg) and secondary care (180/110 mmHg) allows for a number of factors. Blood pressure reduction in primary care is based on good evidence that the rates of cardiovascular morbidity, in particular stroke, are reduced over years and decades. There is no evidence that peri‐operative blood pressure reduction affects rates of cardiovascular events beyond that expected in a month in primary care. Blood pressure measurements might be more accurate in primary care than secondary care, due to a less stressful environment and a more practised technique.
What other guideline statements are available on this topic?
There is detailed evidence‐based guidance on the diagnosis and treatment of hypertension in the community from, for example, the National Institute for Health and Care Excellence 1. There is little guidance on a ‘safe’ blood pressure for planned anaesthesia and surgery.
Why was this guideline developed?
There is no national guideline for the measurement, diagnosis or management of raised blood pressure before planned surgery. There is little evidence that raised pre‐operative blood pressure affects postoperative outcomes. Local guidelines vary from area to area. Hypertension is a common reason to cancel or postpone surgery. In our sprint audit, 1–3% of elective patients had further investigations precipitated by blood pressure measurement, of whom half had their surgery postponed. Across the UK this would equate to ~100 concerned and inconvenienced patients each day, with associated costs to the NHS and the national economy 2, 3.
This guideline is the first collaboration between the AAGBI and the British Hypertension Society; these two organisations have very different perspectives. Members of the British Hypertension Society are concerned with the long‐term reduction in rates of cardiovascular disease, particularly strokes. Anaesthetists are more focused on immediate complications, in the peri‐operative period. This guideline aims to prevent the diagnosis of hypertension being the reason that planned surgery is cancelled or delayed. As such, it should also be of interest to hospital managers and commissioners of hospital care.
How does this statement differ from existing guidelines?
This guideline serves, therefore, not to advise on treatment of hypertension, but rather to produce a common terminology in diagnosis and referral, explaining the impact of anaesthesia on blood pressure and vice versa to the wider, non‐anaesthetic community. At the same time, it will review current best practice on the measurement, diagnosis and treatment of hypertension.
Why does this statement differ from existing guidelines?
Pre‐operative blood pressure management involves many specialties and professions: primary care, general medicine, cardiology, endocrinology, pre‐operative assessment clinics and, of course, both anaesthetists and surgeons. This list is not exhaustive. This guideline should be a useful summary for all those clinicians and for patients. The guidance takes into account not just the best clinical evidence, but the particular pattern of referral for treatment within the NHS in all four countries of the UK.
Introduction
The National Institute for Health and Care Excellence (NICE) has described hypertension as ‘one of the most important preventable causes of premature morbidity and mortality in the UK’ 1. The Association of Anaesthetists of Great Britain and Ireland (AAGBI), together with the British Hypertension Society, felt there was a need for a nationally agreed policy statement on how to deal with raised blood pressure in the pre‐operative period. We have based this statement on a consensus view with the backing of graded evidence, where such evidence is available.
Hypertension is almost always asymptomatic and it is diagnosed following screening in general practice. Managing hypertension pre‐operatively is a complex matter of balancing the risks of anaesthesia, treatment and delay for the individual patient. Most cases of hypertension are primary, i.e. with no other medical cause. For the remainder, the cause for hypertension may be associated with the reason for the proposed operation.
Cancellations and postponements of planned surgical procedures have been a major and long‐standing problem for healthcare worldwide. The quantifiable loss of resource is pitted against unquantifiable and significant psychological, social and financial implications of postponement for patients and their families. Although guidelines exist for the treatment of elevated blood pressure, there remains a paucity of literature and accepted guidelines for the peri‐operative evaluation and care of the patient with hypertension who undergoes non‐cardiac surgery 4. Of particular importance is defining the patients most vulnerable to complications and the indications for immediate and rapid antihypertensive treatment and/or postponement of surgery to reduce these risks pre‐operatively, intra‐operatively and postoperatively. Peri‐operative hypertension often occurs in conjunction with sympathetic nociceptive stimulation during the induction of anaesthesia, during surgery and with acute pain in the early postoperative period. Hypertension may also accompany hypothermia, hypoxia or intravascular volume overload from excessive intra‐operative fluid therapy, particularly in the ensuing 24–48 h as fluid is mobilised from the extravascular space 4, 5, 6.
There are no nationally agreed guidelines for the diagnosis or management of raised blood pressure before elective surgery. The evidence regarding the effect of raised pre‐operative blood pressure is very limited. Local guidelines do exist but vary from area to area. Both the AAGBI and the British Hypertension Society recognised the need for a national guideline and consensus statement to address the various issues of concern. We have limited our deliberations to a specific scope. Only the period before planned surgery is covered. Blood pressures which may cause an immediate risk to health are specified, rather than those that may cause risk over the long‐term. The best method of taking accurate blood pressure measurements is examined. We considered how long blood pressure should be controlled before surgery is undertaken. Communication between different hospital departments, primary care and the patient are of importance. We hope that by providing national guidance the chances of a patient receiving conflicting advice will be minimised.
Scope
This guideline is aimed at adults presenting for planned surgery. The following groups of patients are specifically not studied, although many of the general points covered in the guideline may apply.
Emergency/urgent surgery
By definition, these patients have no or very limited time for investigation, treatment or postponement. Such surgery must almost always proceed, but all those involved, including the patient, must be aware of any associated increased risk.
Obstetrics
Most cases of hypertension in pregnancy will be directly related to the pregnancy (although with an ageing obstetric population with higher rates of obesity, this may be less so). The monitoring and treatment of blood pressure is a specific and integral part of obstetric care, regardless of the need for surgery, and even for ‘elective’ Caesarean section there may be very limited opportunity for delay.
Paediatrics
Childhood hypertension is relatively uncommon, and its epidemiology and natural history is relatively unclear and there are no definitive trials on screening. Thus, its diagnosis and management, including pre‐operatively, is a specialist area beyond the scope of the general guidance in this publication.
Cardiac surgery
Peri‐operative hypertension commonly complicates surgery for congenital and acquired cardiac disease. Management will be affected by many other factors including the planned procedure, the use or not of cardiopulmonary bypass and the other indications for vaso‐ and cardio‐active medication. We have thus considered it to be a specialist area beyond the scope of the general guidance in this publication.
Surgery for blood pressure management
This includes surgery for phaeochromocytoma and bariatric surgery; we have excluded this from our guidance for similar reasons to that of cardiac surgery.
Methods
We formed a Working Party consisting of four members from each society who were academics and clinicians with varied interests, including vascular anaesthesia, cardiology, elderly care medicine and general practice. We agreed on the scope of the guideline, and then carried out a systematic review with the quality of evidence described using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach 7, 8. The GRADE approach considers the quality of a body of evidence as high, moderate, low or very low. To achieve a full consensus document was important. Therefore, we consulted 20 general practitioners, including those with a specialist interest in cardiovascular medicine, as well as senior academics. A consultation guideline was then made available to members of both societies for comment. We specifically asked for and received comments from the patient group, Blood Pressure UK. The comments and responses have been made available online. The Council and Executive of the respective societies were given the task of final approval.
Blood pressure, hypertension and anaesthesia
The anaesthetist has two broad considerations in the hypertensive patient who presents for surgery. One is to be cognisant of the effect of chronic hypertension on the individual's peri‐operative and long‐term cardiovascular risk. The other is to consider whether the blood pressure measured in the primary care setting is associated with adverse peri‐operative events and to decide whether this should be reduced before surgery.
The association between hypertension and peri‐operative harm was first reported in the 1950s 9, 10. Systolic blood pressures in excess of 170 mmHg and diastolic blood pressures in excess of 110 mmHg were associated with complications such as myocardial ischaemia 11. Hypertension was the second‐most common factor associated with postoperative morbidity 12. In 2003, Weksler et al. published a ‘quasi’‐randomised controlled study of 989 treated hypertensive patients who had diastolic blood pressures between 110 and 130 mmHg measured in the anaesthetic room 13. In one group, surgery proceeded after intranasal nifedipine, and in the other group, surgery was delayed while further antihypertensive treatment was pursued in hospital. During the first three postoperative days, the rates of neurological and cardiovascular complications were similar. One might conclude that there was no difference in an infrequent outcome, or that the study had insufficient power to detect a small difference (see section below, treatment for hypertension: extension of evidence from the community to the peri‐operative period).
The association of hypertension with cardiovascular disease is established, but there is no clear evidence that patients with stage 1 or 2 hypertension (Table 1) without evidence of target organ damage have increased peri‐operative cardiovascular risk 14. Patients with stage 3 or 4 hypertension, who are more likely to have target organ damage, have not been subjected to rigorous randomised controlled trials of peri‐operative interventions. There is evidence that hypertension with target organ damage is associated with a small increased incidence of peri‐operative major adverse cardiovascular events 4. It is not known whether or not reducing blood pressure in these patients during a postponement of planned surgery would reduce this rate of events; there is sparse evidence to guide a decision. Any decision should take into account factors other than blood pressure, namely: age; comorbidity; functional capacity (i.e. functional status and reserve); and the urgency and indication for surgery (see section below, ‘The treatment of cardiovascular risk, not hypertension’). The latest guidelines published by the National Institute for Health and Care Excellence (NICE), in conjunction with the British Hypertension Society, recognise the importance of target organ damage in the management of hypertension by targeting a lower threshold for further medical intervention 1. Whether or not these thresholds and targets should be rigorously applied in the peri‐operative setting is not clear.
Table 1.
Categorisation of the stages of hypertension
| Category | Systolic blood pressure; mmHg | Diastolic blood pressure; mmHg |
|---|---|---|
| Stage 1 | 140–159 | 90–99 |
| Stage 2 | 160–179 | 100–109 |
| Stage 3 | 180–209 | 110–119 |
| Stage 4 | ≥ 210 | ≥ 120 |
Patients with hypertension (controlled or uncontrolled) demonstrate a more labile haemodynamic profile than their non‐hypertensive counterparts 5. The induction of anaesthesia and airway instrumentation can lead to a pronounced increase in sympathetic activation, which may lead to a significant increase in blood pressure and heart rate. A reduction in systemic vascular resistance soon after the induction of anaesthesia commonly leads to varying degrees of hypotension. Reduction in vascular resistance is multifactorial and may be secondary to loss of the baroreceptor reflex control, central neuraxial blockade, and direct effects of anaesthetic agents. The effect on vascular tone will be exaggerated by ‘deep’ or excessive anaesthesia and in patients who are fluid‐depleted. This, and the often exaggerated haemodynamic response to surgery, pain and emergence from anaesthesia, have also been described as being more common in the hypertensive population 6. Some researchers have demonstrated an association between pre‐operative hypertension and relatively minor physiological derangements such as intra‐operative hypotension, hypertension and arrhythmia, but studies have not conclusively demonstrated that fluctuations in haemodynamic variables cause clinically significant harm 15. Larger studies to investigate differences between untreated hypertensive patients and those treated (successfully and unsuccessfully) have not demonstrated increased rates of peri‐operative cardiovascular events. However, these findings may not be applicable to current practice, as many of these studies were conducted in the late 1970s 16.
This appreciation of labile haemodynamics in hypertensive patients has led to a number of anaesthetic techniques designed to achieve a more stable haemodynamic profile during surgery. These techniques include co‐induction, invasive arterial monitoring with titrated or prophylactic vasopressor therapy, depth‐of‐anaesthesia monitoring, beta‐blockers and the optimisation of stroke volume with intravascular fluid therapy. The omission of antihypertensive drugs, such as angiotensin‐converting enzyme inhibitors and receptor blockers, combined with the careful re‐introduction of these drugs after surgery, is common‐place and appears to be associated with fewer significant peri‐operative haemodynamic fluctuations 17. The introduction of peri‐operative beta‐blockade for high cardiac‐risk patients increases postoperative mortality, secondary to hypotension and stroke, albeit with less cardiac injury, as demonstrated in the POISE‐1 study 18. The anaesthetist should be aware that sudden withdrawal of certain antihypertensive agents such as clonidine, alpha‐methyldopa and beta‐blockers can be associated with adverse events. Withdrawal of beta‐blockers may also be associated with myocardial ischaemia that is often silent in the peri‐operative period and easily missed without continuous ECG monitoring and serial serum troponin measurements.
Best practice: the measurement of blood pressure
Blood pressure should be measured in primary care before non‐urgent surgical referral (Fig. 1). Surgical outpatients should arrange for primary care to supply blood pressure readings if these have not been documented in the referral letter. Blood pressure should be measured by pre‐operative assessment clinics in patients who attend the clinic without documented blood pressure readings from the last 12 months. The measurement should follow the principles mandated for primary care (see below) 1. Blood pressures less than 180 mmHg systolic and 110 mmHg diastolic in secondary care should not preclude elective surgery, although the patient should be asked to attend their general practice for the concurrent determination of whether primary care hypertension is present.
Figure 1.
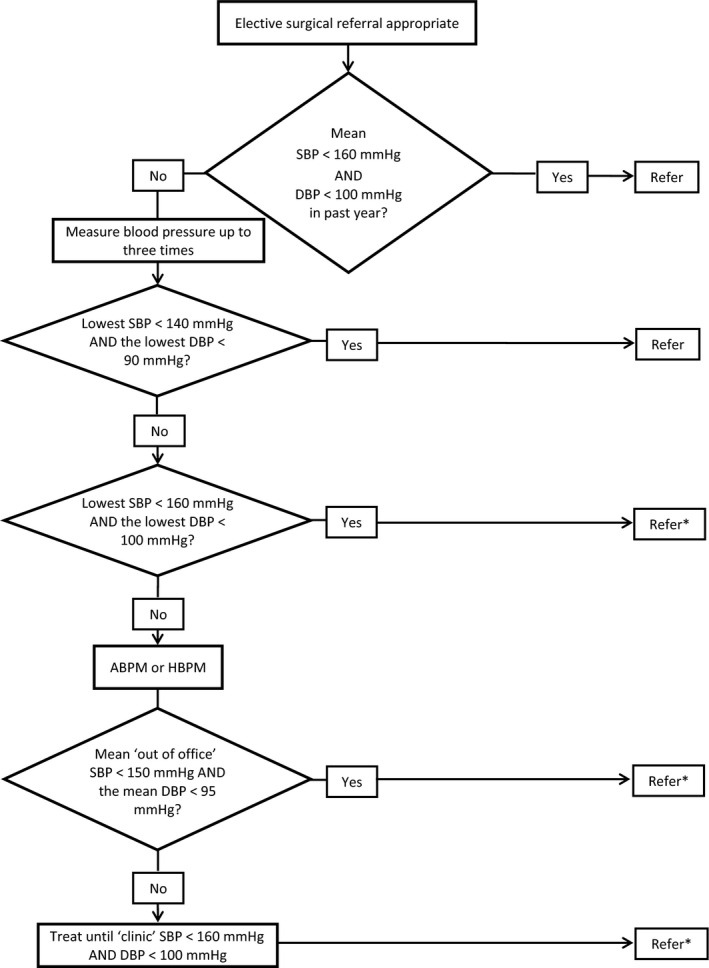
Primary care blood pressure assessment of patients before referral for elective surgery. *Investigations and treatment should continue to achieve blood pressures < 140/90 mmHg. ABPM and HBPM, ambulatory and home blood pressure measurement; DBP and SBP, diastolic and systolic blood pressure.
The setting in which blood pressure is measured should be relaxed and temperate in a standardised environment with current calibrated equipment. The seated patient should have their supported arm outstretched for at least one minute before the initial reading. The pulse rate and rhythm should be recorded before the blood pressure is measured by a validated device. Automated sphygmomanometers (www.bhsoc.org/bp-monitors) are inaccurate when the pulse is irregular, when the blood pressure should be measured by auscultation over the brachial artery during manual deflation of an arm cuff.
Blood pressure should be measured in both arms in patients scheduled for vascular or renal surgery. If the difference between arms in systolic pressure is greater than 20 mmHg, repeat the measurements; subsequently, measure from the arm with the higher blood pressure.
The patient is normotensive if the blood pressure measurement is less than 140/90 mmHg. If the first measurement is equal to or higher than 140/90 mmHg, the blood pressure should be measured twice more, with each reading at least one minute apart. The lower of the last two readings is recorded as the blood pressure; if it is less than 140/90 mmHg the patient is normotensive.
If the reading is between 140/90 mmHg and 179/109 mmHg, the patient may have stage 1 or 2 hypertension. In primary care, the patient would be offered ambulatory (ABPM) or home blood pressure monitoring (HBPM) to establish their true blood pressure (GRADE 1B). If the reading is equal to or higher than 180/110 mmHg in primary care, the patient may have severe hypertension and would be considered for immediate treatment.
Best practice: the diagnosis of hypertension
General practitioners should establish whether blood pressure has been measured and managed in all adults before non‐urgent surgical referrals. A blood pressure measurement taken within the preceding 12 months should be detailed in the referral letter.
The diagnosis of hypertension in patients referred for investigation of surgical disease that are not treated for hypertension and who have not had a blood pressure measurement in the preceding 12 months follows the same process as any other primary care patient. We recommend that the practice instigates ambulatory or home blood pressure measurements before non‐urgent referrals if the standard blood pressure is equal to or greater than 160/100 mmHg. If the patient's ABPM/HBPM blood pressure is equal to or greater than 150/95 mmHg (or equal to or greater than 135/85 mmHg with target organ damage), the patient is diagnosed as having hypertension; treatment should be discussed and commenced using the NICE/BHS CG127 algorithm 19. This process can take place at the same time as urgent surgical referral, but a reduction in blood pressure to less than 160/100 mmHg should precede non‐urgent surgical referral. The referral letter should document that an informed discussion has taken place with patients who decline treatment, or detail that all appropriate attempts have been made to reduce blood pressure for patients with persistent hypertension, which might have included specialist investigations.
Surgical outpatients should request that general practitioners forward primary care blood pressure measurements if these have not been documented in the referral letter. Pre‐operative assessment clinics should measure the blood pressures of patients who present without documentation of primary care blood pressures. If the blood pressure is raised above 180 mmHg systolic or 110 mmHg diastolic, the patient should return to their general practice for primary care assessment and management of their blood pressure, as detailed above (Fig. 2). If the blood pressure is above 140 mmHg systolic or 90 mmHg diastolic, but below 180 mmHg systolic and below 110 mmHg diastolic, the GP should be informed, but elective surgery should not be postponed.
Figure 2.
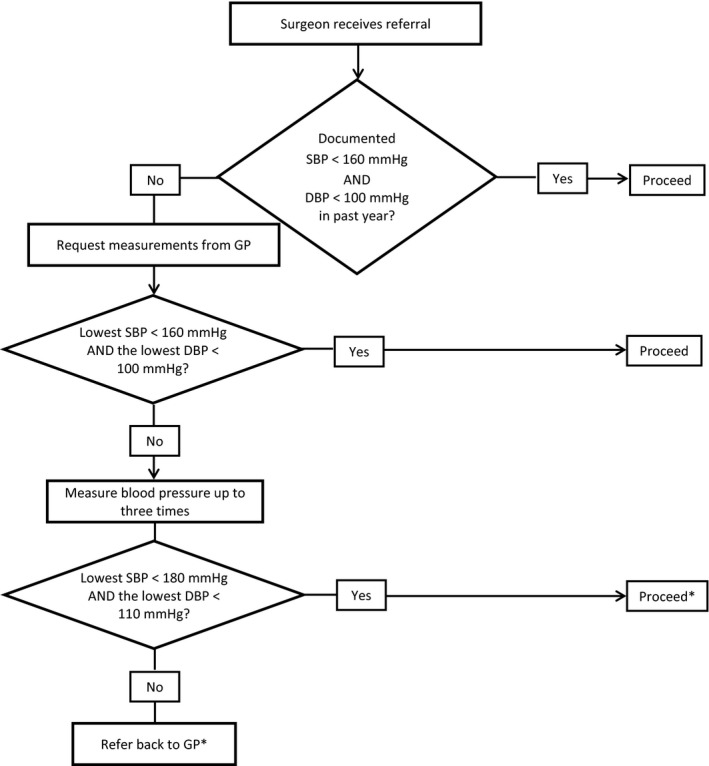
Secondary care blood pressure assessment of patients after referral for elective surgery. *The GP should be informed of blood pressure readings in excess of 140 mmHg systolic or 90 mmHg diastolic, so that the diagnosis of hypertension can be refuted or confirmed and investigated and treated as necessary. DBP and SBP, diastolic and systolic blood pressure.
Best practice: the treatment of hypertension
This section summarises the recommendations for primary care following the diagnosis of hypertension. There is good evidence (GRADE 1A) for the treatment of hypertension with one or more of the following: diuretics (thiazide, chlorthalidone and indapamide); beta‐blockers; calcium channel‐blockers (CCB); angiotensin converting enzyme (ACE) inhibitors, or an angiotensin‐2 receptor blocker (ARB) 1. In the future, the threshold for treating high blood pressure might change to cardiovascular risk (see below, the treatment of cardiovascular risk, not hypertension).
Step 1 treatment
Patients aged less than 55 years should be offered an ACE inhibitor, or a low‐cost ARB. If an ACE inhibitor is prescribed but is not tolerated (for example, because of cough), offer a low‐cost ARB. Angiotensin‐converting enzyme inhibitors and ARBs are not recommended in women of childbearing potential. An ACE inhibitor should not be combined with an ARB.
Patients aged over 55 years and Black patients of African or Caribbean family origin of any age should be offered a CCB. If a CCB is not suitable, for example because of oedema or intolerance, or if there is evidence of heart failure or a high risk of heart failure, a thiazide‐like diuretic should be offered.
If diuretic treatment is to be initiated or changed, offer a thiazide‐like diuretic, such as chlorthalidone (12.5–25.0 mg once daily), or indapamide (1.5 mg modified‐release once daily or 2.5 mg once daily), in preference to a conventional thiazide diuretic such as bendroflumethiazide or hydrochlorothiazide.
For patients who are already having treatment with bendroflumethiazide or hydrochlorothiazide and whose blood pressure is stable and well controlled, treatment with the bendroflumethiazide or hydrochlorothiazide should be continued.
Beta‐blockers are not a preferred initial therapy for hypertension. However, beta‐blockers may be considered in younger patients, particularly those with an intolerance or contraindication to ACE inhibitors and ARBs, or women of childbearing potential or patients with evidence of increased sympathetic drive. If beta‐blockers are started and a second drug is required, add a CCB rather than a thiazide‐like diuretic to reduce the person's risk of developing diabetes.
Step 2 treatment
If blood pressure is not controlled by Step 1 treatment, use a CCB in combination with either an ACE inhibitor or an ARB.
If a CCB is not suitable for Step 2 treatment, for example because of oedema or intolerance, or if there is evidence of heart failure or a high risk of heart failure, offer a thiazide‐like diuretic.
For Black patients of African or Caribbean family origin, consider an ARB in preference to an ACE inhibitor, in combination with a CCB.
Step 3 treatment
Before considering Step 3 treatment, check that drugs from Step 2 have been prescribed at optimal doses, or at the maximum tolerated doses. If treatment with three drugs is required, the combination of ACE inhibitor or ARB, CCB and thiazide‐like diuretic should be used.
Step 4 treatment
If resistant blood pressure exceeds 140/90 mmHg in clinic after treatment with the optimal or highest‐tolerated doses of an ACE inhibitor, or an ARB plus a CCB, with a diuretic; adding a fourth antihypertensive drug and expert advice should be considered.
Further diuretic therapy with low‐dose spironolactone (25 mg once daily) should be considered if the serum potassium concentration < 4.6 mmol.l−1. Caution is required in patients with reduced estimated glomerular filtration rates because of an increased risk of hyperkalaemia. Increasing the dose of thiazide‐like diuretics should be considered if the serum potassium concentration > 4.5 mmol.l−1.
Serum sodium and potassium concentrations and renal function should be checked within 1 month of increasing diuretic dose, and repeated as required thereafter. If further diuretic therapy for resistant hypertension at Step 4 is not tolerated, or is contraindicated or ineffective, consider an alpha‐blocker or beta‐blocker. If blood pressure remains uncontrolled with the optimal or maximum tolerated doses of four drugs, expert advice should be sought if it has not yet been obtained.
As recently as 2008, the HYVET study demonstrated the clinical benefits of treating hypertension in people aged ≥ 80 years, while health economic analysis has confirmed the cost effectiveness of this strategy 1, 20. As a result, NICE now recommends that patients aged ≥ 80 years should be offered treatment only if they have stage 2 hypertension. The 2011 Hypertension Guideline also recommends that the decision to treat should be based on standing blood pressure, and should take into account the presence of co‐morbidities such as dementia. The guideline also makes a distinction between initiating treatment in the over‐80s and continuing long‐term and well‐tolerated treatment when patients reach this age. In other words, patients who were started on treatment when younger should not have their current therapy back‐titrated when they celebrate their 80th birthday.
The treatment of cardiovascular risk, not hypertension
It is likely that treatment for hypertension will no longer be based upon blood pressure 21. This is a surprising statement; the diagnosis of hypertension that merits treatment has – until recently – been based on patients’ blood pressure, irrespective of other cardiovascular risk factors, despite the NICE guidance recognising their importance 1. This practice conflicts with the treatment of hypercholesterolaemia, which is not based on the cholesterol concentration alone, but instead on the composite 5‐ or 10‐year risk of: stroke; myocardial infarction; heart failure; cardiovascular morbidity; or death, ascribed to these diagnoses. The magnitude by which cardiovascular disease is reduced by treatment for both hypercholesterolaemia and hypertension is dependent on the composite cardiovascular risk, not the concentration of cholesterol or the blood pressure. Anaesthetists should gauge their concern for a hypertensive patient by the calculated five‐year rate of cardiovascular events, not by the blood pressure measurement per se.
Hypertension is common; this is responsible for the well‐publicised reduction in population rates of stroke by antihypertensive treatment. The absolute effect of treatment for the individual, even over a five‐year period, is smaller than many anaesthetists might realise. Table 2 presents the effect of five‐year antihypertensive treatment for cardiovascular risk in a population quartered by the five‐year rate of any cardiovascular event. Planned major surgery temporarily increases mortality. For instance, planned open repair of abdominal aortic aneurysm increases mortality in the first postoperative month ten times, whereas endovascular repair increases mortality four times. If cardiovascular events are similarly increased by major planned surgery, one would anticipate that the pre‐operative antihypertensive treatment of cardiovascular risk would have a proportionately greater absolute effect on the rates of events while their risk remains elevated. Table 3 illustrates the absolute effect of established antihypertensive treatment in the month following a planned operation in patients from Table 2, assuming two scenarios: that the operation does not affect the rates of cardiovascular events; and that the operation increases the rates of cardiovascular events six times.
Table 2.
The effect of antihypertensive treatment on the five‐year rates of events (per 1000) in a population quartered on the basis of the untreated cardiovascular five‐year risk: lowest quartile (< 11% risk); next quartile (11–15% risk); next quartile (15–21% risk); highest quartile (> 21% risk)
| Quartile of risk | Any event | Stroke | CHD | Heart failure | ||||
|---|---|---|---|---|---|---|---|---|
| No treatment | Treatment | No treatment | Treatment | No treatment | Treatment | No treatment | Treatment | |
| Highest quartile | ||||||||
| Event rates | 270/1000 | 232/1000 | 70/1000 | 58/1000 | 63/1000 | 53/1000 | 47/1000 | 34/1000 |
| Event reduction | 38/1000 | 12/1000 | 10/1000 | 13/1000 | ||||
| Second quartile | ||||||||
| Event rates | 180/1000 | 156/1000 | 49/1000 | 40/1000 | 42/1000 | 36/1000 | 27/1000 | 23/1000 |
| Event reduction | 24/1000 | 9/1000 | 6/1000 | 4/1000 | ||||
| Third quartile | ||||||||
| Event rates | 120/1000 | 100/1000 | 36/1000 | 29/1000 | 33/1000 | 28/1000 | 15/1000 | 13/1000 |
| Event reduction | 20/1000 | 7/1000 | 5/1000 | 2/1000 | ||||
| Lowest quartile | ||||||||
| Event rates | 60/1000 | 46/1000 | 17/1000 | 11/1000 | 17/1000 | 14/1000 | 6/1000 | 5/1000 |
| Event reduction | 14/1000 | 6/1000 | 3/1000 | 1/1000 | ||||
CHD, coronary heart disease.
Table 3.
The absolute reduction in event rates per 1000 patients per month by antihypertensive treatment, assuming that the control rate is unaffected by surgery (‘same’) or increased, in this example sixfold (‘× 6’)
| Quartile of risk | Any event | Stroke | CHD | Heart failure | ||||
|---|---|---|---|---|---|---|---|---|
| Same | × 6 | Same | × 6 | Same | × 6 | Same | × 6 | |
| Highest quartile | 0.6 | 3.8 | 0.2 | 1.2 | 0.2 | 1 | 0.2 | 1.3 |
| Next quartile | 0.4 | 2.4 | 0.2 | 0.9a | 0.1 | 0.6 | 0.1 | 0.4 |
| Next quartile | 0.3 | 1.8 | 0.1 | 0.7 | 0.1 | 0.6 | 0.0 | 0.2 |
| Lowest quartile | 0.2 | 1.2 | 0.1 | 0.6 | 0.1 | 0.3 | 0.0 | 0.1 |
The ‘0.2’ was rounded up from a value near 0.15, which is why this value × 6 is 0.9, not 1.2.
CHD, coronary heart disease.
This guideline has outlined that blood pressure before planned non‐urgent surgery is measured in primary care, where the diagnosis of hypertension is made, and treatment is managed. The lifelong risk of mortality and morbidity may be unaffected by postponing surgery for the assessment of cardiovascular risk by primary care and possible antihypertensive treatment 22. For instance, clinicians might like to consider the uncertainty in how long it takes for cardiovascular risk to fall with antihypertensive medication (as opposed to how long it takes for blood pressure to fall), and the 1% relative increase in cardiovascular risk that accompanies each postponed month, due to the patient ageing. Clinicians might also consider that patients who smoke or who have hypercholesterolaemia are not subjected to the summary cancellations justified by blood pressure readings. A further consideration is the absence of a scale of enthusiasm for postponing surgery that matches the continuum of cardiovascular risk, which would result in older smoking hypercholesterolaemic normotensive men having surgery postponed more frequently than younger hypertensive women who do not have any other cardiovascular risk factors.
Communication
Pre‐operative assessment clinics should inform general practitioners when they measure raised blood pressures in patients who have not had readings taken in primary care in the preceding 12 months. The letter should request that the general practitioner determine whether the patient has hypertension in primary care. The letter should also state whether or not surgery will proceed without a diagnosis of hypertension being made or treatment commenced.
Appendix 1 is an example of a letter explaining that surgery will not proceed until the diagnosis of hypertension has been excluded or confirmed, and in the latter case treated with the patient's consent. It is important that the patient has a copy and is instructed to make an appointment at their surgery with a nurse or a doctor and to take the letter with them. The language used should seek cooperative management rather than demand action. In the first instance, the GP will need to establish that the blood pressure is high and this is not a white coat effect. It must be clearly stated how to re‐establish the procedural pathway when the blood pressure has been shown to be satisfactory, treated or not.
Appendix 1.
Example of letter to general practitioner from pre‐assessment clinic following measurement of raised blood pressure in patients who have not had readings taken in primary care in the preceding 12 months.
Dear Doctor
Unfortunately, the procedure for Mr/Ms …………………. has been postponed because their blood pressure was found to be 182/114 in their pre‐operative assessment. It was measured several times following the AAGBI/BHS guidelines. The guidelines suggest a blood pressure level higher than 180/110 is unsuitable for elective anaesthesia.
We have asked the patient to make an appointment at their surgery for further assessment of their blood pressure. We would be grateful if you could verify that this is the true blood pressure level and not a white coat effect and treat appropriately if the patient has hypertension.
We will be pleased to accept the patient back for surgery if their clinical blood pressure is below 160/100. Please ask the patient to contact ……………………… and inform us of their current blood pressure and what medication, if any, was required to achieve this.
Many thanks in anticipation of your help with this matter
The following GPs were consulted about this letter:
Dr Chris Arden, Dr Ivan Benett, Dr Mark Davis, Dr Richard Falk, Prof David Fitzmaurice, Prof Ahmet Fuat, Dr Napa Gopi, Dr Kathryn Griffith, Dr Rosie Heath, Prof Richard Hobbs, Dr Paul Johnson Prof Richard McManus, Dr Jonathan Morrell, Dr Washik Parkar, Dr Neil Paul, Dr Jon Pittard, Dr Peter Savill, Dr Jonathan Shribman, Dr Harjit Singh, Dr Heather Wetherell.
This is a consensus document produced by members of a Working Party established by the Association of Anaesthetists of Great Britain and Ireland (AAGBI) and the British Hypertension Society (BHS). It has been seen and approved by the AAGBI Board of Directors and the BHS Executive. It is licensed under a Creative Commons Attribution‐NonCommercial‐NoDerivatives 4.0 International License. Date of review: 2020.
Re‐use of this article is permitted in accordance with the Creative Commons Deed, Attribution 2.5, which does not permit commercial exploitation.
References
- 1. National Institute for Health and Care Excellence . Hypertension: Clinical management of primary hypertension in adults. 2011 NICE Clinical Guideline CG127. http://www.nice.org.uk/guidance/cg127 (accessed 15/01/2015).
- 2. Cook TM, Woodall N, Frerk C. Fourth National Audit Project. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. British Journal of Anaesthesia 2011; 106: 617–31. [DOI] [PubMed] [Google Scholar]
- 3. Cook TM, Andrade J, Bogod DG, et al. The 5th National Audit Project (NAP5) on accidental awareness during general anaesthesia: patient experiences, human factors, sedation, consent and medicolegal issues. Anaesthesia 2014; 69: 1102–16. [DOI] [PubMed] [Google Scholar]
- 4. Howell SJ, Sear JW, Foex P. Hypertension, hypertensive heart disease and perioperative cardiac risk. British Journal of Anaesthesia 2004; 92: 57–83. [DOI] [PubMed] [Google Scholar]
- 5. Longnecker DE. Alpine anesthesia: can pretreatment with clonidine decrease the peaks and valleys? Anesthesiology 1987; 67: 1–2. [PubMed] [Google Scholar]
- 6. Prys‐Roberts C, Greene LT, Meloche R, Foex P. Studies of anaesthesia in relation to hypertension II. Haemodynamic consequences of induction and endotracheal intubation. British Journal of Anaesthesia 1971; 43: 531–47. [DOI] [PubMed] [Google Scholar]
- 7. Guyatt GH, Oxman AD, Kunz R, et al. Going from evidence to recommendations. British Medical Journal 2008; 336: 1049–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Guyatt GH, Oxman AD, Vist G, et al. for the GRADE Working Group . Rating quality of evidence and strength of recommendations GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. British Medical Journal 2008; 336: 924–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Smithwick RH, Thompson JE. Splanchnicectomy for essential hypertension; results in 1,266 cases. Journal of the American Medical Association 1953; 152: 1501–4. [DOI] [PubMed] [Google Scholar]
- 10. Thompson JE, Smithwick RH. Surgical measures in hypertension. Geriatrics 1953; 8: 611–9. [PubMed] [Google Scholar]
- 11. Goldman L, Caldera DL, Nussbaum SR, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. New England Journal of Medicine 1977; 297: 845–50. [DOI] [PubMed] [Google Scholar]
- 12. Khuri SF, Daley J, Henderson W, et al. The National Veterans Administration surgical risk study: risk adjustment for the comparative assessment of the quality of surgical care. Journal of the American College of Surgeons 1995; 180: 519–31. [PubMed] [Google Scholar]
- 13. Weksler N, Klein M, Szendro G, et al. The dilemma of immediate preoperative hypertension: to treat and operate, or to postpone surgery? Journal of Clinical Anesthesia 2003; 15: 179–83. [DOI] [PubMed] [Google Scholar]
- 14. Hanada S, Kawakami H, Goto T, et al. Hypertension and anesthesia. Current Opinion in Anaesthesiology 2006; 19: 315–9. [DOI] [PubMed] [Google Scholar]
- 15. Chung F, Mezei G, Tong D. Pre‐existing medical conditions as predictors of adverse events in day case surgery. British Journal of Anaesthesia 1999; 83: 262–70. [DOI] [PubMed] [Google Scholar]
- 16. Goldman L, Caldera DL. Risks of general anesthesia and elective operation in the hypertensive patient. Anesthesiology 1979; 50: 285–92. [DOI] [PubMed] [Google Scholar]
- 17. Comfere T, Sprung J, Kumar MM, et al. Angiotensin system inhibitors in a general surgical population. Anesthesia and Analgesia 2005; 100: 636–44. [DOI] [PubMed] [Google Scholar]
- 18. Devereaux PJ, Yang H, Yusuf S, et al. Effects of extended release metoprolol succinate in patients undergoing non‐cardiac surgery (POISE trial): a randomised controlled trial. Lancet 2008; 371: 1839–47. [DOI] [PubMed] [Google Scholar]
- 19. Hypertension Pathyways. http://pathways.nice.org.uk/pathways/hypertension#path=view%3A/pathways/hypertension/diagnosis-and-assessment-of-hypertension.xml&content=view-index (accessed 16/01/2015).
- 20. Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. New England Journal of Medicine 2008; 358: 1958–60. [DOI] [PubMed] [Google Scholar]
- 21. Sundström J, Arima H, Woodward M, et al. on behalf of the Blood Pressure Lowering Treatment Trialists' Collaboration . Blood pressure‐lowering treatment based on cardiovascular risk: a meta‐analysis of individual patient data. Lancet 2014; 384: 591–8. [DOI] [PubMed] [Google Scholar]
- 22. Carlisle JB. Too much blood pressure? Anaesthesia 2015; 70: 773–8. [DOI] [PubMed] [Google Scholar]


