Abstract
Background
For more than a century, appendicectomy has been the treatment of choice for appendicitis. Recent trials have challenged this view. This study assessed the benefits and harms of antibiotic therapy compared with appendicectomy in patients with non‐perforated appendicitis.
Methods
A comprehensive search was conducted for randomized trials comparing antibiotic therapy with appendicectomy in patients with non‐perforated appendicitis. Key outcomes were analysed using random‐effects meta‐analysis, and the quality of evidence was assessed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach.
Results
Five studies including 1116 patients reported major complications in 25 (4·9 per cent) of 510 patients in the antibiotic and 41 (8·4 per cent) of 489 in the appendicectomy group: risk difference −2·6 (95 per cent c.i. –6·3 to 1·1) per cent (low‐quality evidence). Minor complications occurred in 11 (2·2 per cent) of 510 and 61 (12·5 per cent) of 489 patients respectively: risk difference −7·2 (−18·1 to 3·8) per cent (very low‐quality evidence). Of 550 patients in the antibiotic group, 47 underwent appendicectomy within 1 month: pooled estimate 8·2 (95 per cent c.i. 5·2 to 11·8) per cent (high‐quality evidence). Within 1 year, appendicitis recurred in 114 of 510 patients in the antibiotic group: pooled estimate 22·6 (15·6 to 30·4) per cent (high‐quality evidence). For every 100 patients with non‐perforated appendicitis, initial antibiotic therapy compared with prompt appendicectomy may result in 92 fewer patients receiving surgery within the first month, and 23 more experiencing recurrent appendicitis within the first year.
Conclusion
The choice of medical versus surgical management in patients with clearly uncomplicated appendicitis is value‐ and preference‐dependent, suggesting a change in practice towards shared decision‐making is necessary.
Short abstract
Limitations of each evolving
Introduction
Acute appendicitis is the most common indication for emergency abdominal surgery worldwide: approximately one in every ten individuals will have acute appendicitis during their lifetime1. In the UK alone, approximately 40 000 appendicectomies are performed every year. Although appendicectomy is a routine surgical procedure with low mortality, 5–28 per cent of patients develop a complication2.
Since surgeons identified appendicitis as a source of pelvic sepsis and subsequent high mortality, appendicectomy has been considered mandatory3, 4. In 1956, Coldrey5 challenged this view in a report of 137 patients with acute appendicitis for more than 24 h treated with antibiotics rather than surgery. In 1977, researchers from China6 reported successful treatment of 92·9 per cent of 425 patients with acute appendicitis by traditional Chinese medicine alone. Nevertheless, appendicectomy remained the standard treatment for appendicitis7.
Another challenge to convention appeared in 1995 when a small randomized clinical trial (RCT)8 comparing antibiotics with appendicectomy suggested no difference in efficacy. In the past 10 years, improved CT, allowing more accurate diagnosis of acute appendicitis and preoperative differentiation of perforated versus non‐perforated appendicitis, has encouraged the conduct of additional RCTs9, 10, 11, 12, 13, 14.
A number of systematic reviews15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25 have attempted to synthesize the published evidence. However, earlier systematic reviews were limited by varying outcome definitions for antibiotic treatment versus surgery18, 22, 23, inclusion of retracted studies22, 23, 25, and inclusion of a study11 at very high risk of bias16, 22, 25. Furthermore, since the publication of the most recent meta‐analysis15, the results of two additional eligible RCTs have become available13, 14.
The present systematic review and meta‐analysis evaluated the relative merits of antibiotic therapy versus appendicectomy in patients with acute non‐perforated appendicitis. The approach was to consider the studies in a practical or pragmatic way, rather than using a mechanistic or explanatory perspective26. The interest was not in comparing appendicectomy with an antibiotic for all management, but rather in comparing a management strategy of immediate appendicectomy versus the clinically sensible alternative of antibiotics initially, with appendicectomy as necessary, depending on the response to antibiotics. This perspective guided presentation of the results.
Methods
Eligibility of studies
RCTs that compared antibiotic treatment with appendicectomy in patients with suspected acute non‐perforated appendicitis were included. Quasi‐RCTs were also included, but only in the sensitivity analysis. Studies with a very high risk of bias, in which both the description of methods and the baseline characteristics indicated that many patients randomized were not included, were excluded.
Data sources and searches
The comprehensive search conducted in the 2011 Cochrane systematic review of Wilms and colleagues22, which extended until June 2011, was updated. This consisted of three blocks of search terms for the concepts appendicitis, appendicectomy and antibiotic treatment, limited by the Cochrane filters for RCTs and the McMaster University Health Information Research Unit Clinical Queries hedges for therapeutic studies. The searches were adapted and run without language restrictions in MEDLINE, Embase and the Cochrane Central Register of Controlled Trials (CENTRAL) from 1 January 2011 to 4 December 2015. PubMed was also searched for in‐process citations, and the major clinical trial registries (ClinicalTrials.gov: http://clinicaltrials.gov/; International Clinical Trials Registry Platform Search Portal (ICTRP): http://apps.who.int/trialsearch/) were searched for ongoing trials. Appendix S1 (supporting information) shows details of the search strategy. In addition, reference lists of other previous systematic reviews15, 16, 17, 18, 19, 20, 21, 23, 24 comparing antibiotic treatment with appendicectomy in patients with non‐perforated appendicitis were searched.
Study selection
Using standard, pilot‐tested forms and working in teams of two, reviewers screened all titles and abstracts identified by the literature search independently, and obtained full‐text articles of any article identified as potentially eligible by either reviewer. The reviewers used standard, pilot‐tested forms to evaluate the full texts for eligibility and resolved disagreement by discussion or, if necessary, by consulting with a third reviewer.
Data extraction
Using standard pilot‐tested forms along with detailed instructions and working in teams of two, reviewers extracted data independently. A clinician–methodologist adjudicator resolved disagreements. Finally, authors were contacted to check the data for accuracy, and to provide additional information regarding the original studies, when needed.
The following data were extracted: sample size, participants' characteristics, antibiotic regimens and details of surgical management (laparoscopic or open, any antibiotic use), and the following outcomes (for both treatment groups): major complications at 1 year, including Clavien–Dindo complication classification grade III or above (conditions requiring endoscopic, radiological or surgical intervention, or causing organ dysfunction or death), such as appendiceal perforation, as well as deep infections, incisional hernias and adhesive bowel obstruction not requiring intervention; minor complications at 1 year, such as superficial wound infections, diarrhoea and abdominal discomfort; confirmed or suspected recurrence of appendicitis between 1 month and 1 year; rate of appendicectomy within 1 month of intervention; duration of hospital stay; and duration of sick leave.
Risk of bias
In the risk‐of‐bias assessment, each study was evaluated using a modified version of the Cochrane Collaboration's instrument27 according to four criteria: random sequence generation, allocation concealment, blinding and completeness of data. For each criterion, studies were judged to be at either high or low risk of bias.
Statistical analysis
Complete‐case analyses were carried out (including only patients who were followed and whose outcomes were available). Pooled estimates of risk differences were calculated by a random‐effects meta‐analysis using the DerSimonian and Laird approach (Freeman–Tukey double arcsine transformation). Heterogeneity was assessed for each outcome across studies using the I 2 statistic and Cochran's Q. For outcomes in which five or more studies were available, subgroup analyses were planned to examine the study level variables as potential sources of heterogeneity. These variables and the prespecified hypotheses that results would favour antibiotics were: those with CT confirmation of the diagnosis of non‐perforated appendicitis; and those with low risk of bias (separately for each risk‐of‐bias domain with at least 2 studies with high and at least 2 studies with low risk of bias).
For outcomes in which there was a significant difference between groups, sensitivity analyses were planned in which results were imputed for missing data in a manner that challenged the robustness of these differences28, 29, 30. If missing data were minimal (5 per cent or less), the plan was not to conduct these analyses.
Quality of evidence assessment
Guidance from the Grading of Recommendations Assessment, Development and Evaluation (GRADE) working group31, 32 provided the methodology for assessing quality of evidence.
Results
The search yielded 685 potentially relevant reports. After screening titles and abstracts and trial registries, and including six studies8, 9, 10, 11, 12, 33 in previous reviews15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25 (Fig. 1), 52 reports were retrieved for full‐text screening, of which a total of six RCTs were included: five in the final primary analysis8, 9, 12, 13, 14 and, in addition, one quasi‐RCT10 in a sensitivity analysis. Two RCTs were excluded: one because of subsequent retraction owing to plagiarism33 and the other because of postrandomization exclusions that led to serious prognostic imbalance11. Four of the six authors (including the author of the quasi‐RCT) confirmed the accuracy of the consensus data extraction, corrected some errors or provided additional information10, 12, 13, 14; two8, 9 were unable to assist with the requests or could not be contacted.
Figure 1.
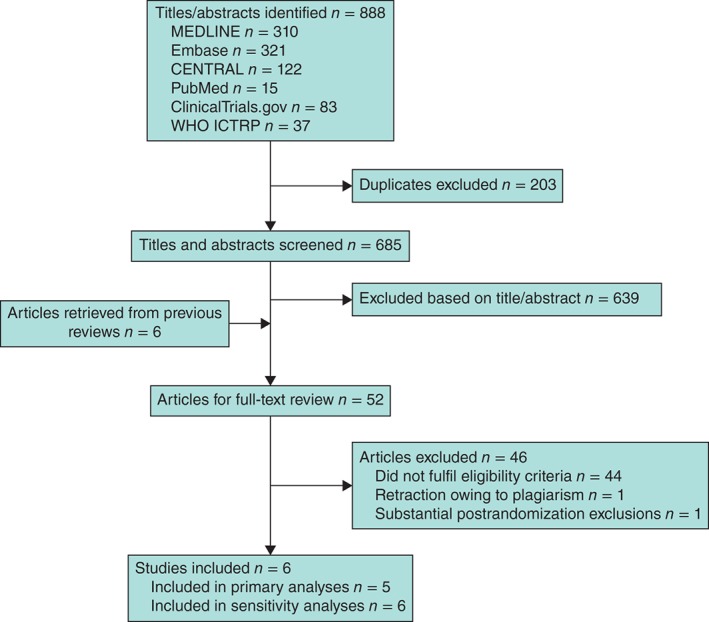
Flow chart showing selection of articles for review. WHO, World Health Organization; ICTRP, International Clinical Trials Registry Platform Search Portal
Table 1 summarizes the characteristics of studies included in primary analyses. The five included RCTs had a total 1116 adult patients; four studies8, 9, 12, 13 recruited adults and one14 children. The quasi‐RCT10 included 369 adults (Tables S1 and S2, supporting information). Definitions of complications varied across the included studies, and were also different between the treatment groups in some studies (Table S3, supporting information). Postoperative complications were reported consistently in all studies, but none used one of the common classification systems. For this review, complications were counted as minor or major based on their description in the original studies.
Table 1.
Characteristics of the included studies
| Reference | Study design | Participants | Intervention (antibiotic therapy) | Control (appendicectomy) | Outcomes assessed | Funding and conflict of interest statement |
|---|---|---|---|---|---|---|
| Eriksson and Granström8 | Single‐centre randomized trial | Patients (n = 41) aged 18–75 years with history and clinical signs of acute appendicitis, positive findings at ultrasonography, and raised levels of inflammatory markers (CRP or WBC) |
Intravenous cefotaxime 2 g twice daily and tinidazole 800 mg once daily for 2 days, followed by oral ofloxacin 200 mg and tinidazole 500 mg twice daily for 8 days Proceeded to appendicectomy based on clinician's judgement – no prespecified criteria |
Open appendicectomy (100%) Antibiotics given only to patients with perforation or abdominal spillage |
Appendicectomy rate within index admission Success of treatment Complications (at 1 year) Recurrence (at 1 year) Length of stay Pain (VAS) Pain (use of medication) |
Funding: Karolinska Institute, Swedish Hoechst, Pfizer, Mutual Group Life Insurance Company Förenade Liv No conflict of interest reported |
| Salminen et al. 13 | Multicentre randomized trial | Patients (n = 530) aged 18–60 years admitted to the emergency department with clinical suspicion of uncomplicated acute appendicitis diagnosed by CT. Excluded if any of the following: appendicolith, perforation, abscess or suspicion of tumour |
Intravenous ertapenem sodium 1 g once daily for 3 days, followed by oral levofloxacin 500 mg once daily and metronidazole 500 mg three times per day for 7 days Appendicectomy performed if progressive infection, perforated appendicitis or peritonitis suspected on examination within 12–24 h after admission |
Open (94%) or laparoscopic (6%) appendicectomy with prophylactic antibiotics Postoperative antibiotics given only in patients with suspected wound infection |
Primary outcome Antibiotic group: resolution of appendicitis resulting in discharge from hospital without need for surgical intervention and no recurrent appendicitis during a minimum follow‐up of 1 year Appendicectomy group: successful appendicectomy Secondary outcomes Overall postinterventional complications Late recurrence after 1 year (unreported*) Length of stay Length of sick leave Postoperative pain (VAS) Use of pain medication (unreported*) |
Funding: Government research grant (EVO Foundation) awarded to Turku University Hospital Dr Salminen reported receiving personal fees for lectures from Merck and Roche; no other disclosures |
| Styrud et al. 9 | Multicentre randomized trial | Men (n = 252) aged 18–50 years with clinically suspected acute non‐perforated appendicitis and CRP > 10 mg/l |
Intravenous cefotaxime 2 g twice daily and tinidazole 800 mg once daily for 2 days, followed by oral ofloxacin 200 mg and tinidazole 500 mg twice daily for 10 days Proceeded to appendicectomy based on clinician's judgement – no prespecified criteria |
Open (94%) or laparoscopic (6%) appendicectomy Unclear whether prophylactic or postoperative antibiotics given |
Appendicectomy rate within index admission Success of treatment Complications (at 1 year) Recurrence (at 1 year) Length of stay Length of sick leave Pain (unreported*) |
Funding: Swedish Society of Medicine, Karolinska Institute, Wallenius Corporation, Aventis Pharma No conflict of interest reported |
| Svensson et al. 14 | Single‐centre randomized (pilot) trial |
Children (n = 50) aged 5–15 years with clinical diagnosis of acute appendicitis Exclusion criteria: Suspicion of perforated appendicitis on the basis of generalized peritonitis An appendiceal mass diagnosed by clinical examination and/or imaging Previous non‐operative treatment of acute appendicitis All patients had at least one ultrasound examination, 4 had CT |
Intravenous meropenem 10 mg/kg three times daily and metronidazole 20 mg/kg once daily for at least 48 h. Once the child was well clinically and tolerating oral intake, antibiotics continued with oral ciprofloxacin 20 mg/kg twice daily and metronidazole 20 mg/kg once daily for 8 days Proceeded to appendicectomy based on clinician's judgement – no prespecified criteria |
Laparoscopic appendectomy (100 per cent) Prophylactic antibiotics given to all. Intravenous antibiotic continued for 24 h to patients with gangrenous appendicitis and for 3 days in those with perforated appendicitis |
Primary outcome: resolution of symptoms without significant complications (defined as length of stay over 7 days, abscess, need for surgery within 48 h (antibiotic group only), recurrence of appendicitis within 3 months, or negative appendicectomy). Secondary outcomes Length of stay Other complications (wound infection, wound dehiscence, diarrhoea, etc.) Recurrent appendicitis at 1 year Total costs |
Funding: Crown Princess Lovisa's Foundation, the Hirsch Foundation No conflict of interest reported |
| Vons et al.12 | Multicentre randomized trial | Patients (n = 243) aged 18–68 years with uncomplicated acute appendicitis, diagnosed by CT |
Amoxicillin plus clavulanic acid 3–4 g per day for 8–15 days, intravenously to those with nausea or vomiting, and orally to all others Appendicectomy undertaken if: Symptoms and abdominal tenderness failed to resolve after 48 h Persistence of pain or fever at 8 days prompted CT and possible appendicectomy or Sustained high WBC or high CRP concentration on day 15 prompted appendicectomy without additional CT |
Open (34%) or laparoscopic (66%) appendicectomy with single‐dose prophylactic antibiotics Postoperative antibiotics given if complicated appendicitis found |
Primary outcome: occurrence of peritonitis within 30 days of initial treatment (defined as perforated appendicitis in antibiotic group, postoperative peritonitis in appendicectomy group) Secondary outcomes Complications (other than peritonitis) at 1 year Recurrence (defined as appendicectomy performed between 30 days and 1 year, with confirmed diagnosis of appendicitis) Pain (number of days with VAS 4 or more) Length of stay Length of sick leave |
Funding: French Ministry of Health, Programme Hospitalier de Recherche Clinique 2002 No conflict of interest reported |
CRP, C‐reactive protein; WBC, white blood cell count; VAS, visual analogue scale.
Outcome prespecified as a secondary outcome but no data presented in publication.
Histopathological diagnosis of acute appendicitis was made using standard criteria (mucosal inflammation) in one study12, using stringent criteria in another (intramural inflammation required)13, but remained unclear in most8, 9, 10, 14. In the included trials, rates of negative appendicectomy varied from 0 to 15 per cent, with median of 3 per cent in the appendicectomy arms.
Risk‐of‐bias assessment
All studies probably generated random sequence adequately; one study likely failed to conceal randomization. None of the studies blinded patients, healthcare providers, outcome assessors or data analysts (Table 2; Table S2, supporting information). Loss to follow‐up at 1 year was substantial, varying from 7 to 22 per cent, and was similar in the two groups within each study8, 12, 13, 14, although unclear in one study report9.
Table 2.
Risk of bias
| Reference | Random sequence generation | Allocation concealment | Blinding | Completeness of data |
|---|---|---|---|---|
| Eriksson and Granström8 | + | – | – | + |
| Salminen et al. 13 | + | + | – | + |
| Styrud et al. 9 | + | + | – | – |
| Svensson et al. 14 | + | + | – | + |
| Vons et al. 12 | + | + | – | – |
+, Low risk of bias; −, high risk of bias.
Outcome assessment
Rate of appendicectomy within 1 month
Some 561 of the 562 patients allocated to surgery underwent appendicectomy (range across studies 99·6–100 per cent). The pooled estimate was 99·6 (95 per cent c.i. 98·9 to 100) per cent (high‐quality evidence). Of the appendicectomies, 434 (77·4 per cent) were open and 127 (22·6 per cent) laparoscopic. Of the 550 patients allocated to antibiotic therapy, 47 underwent an appendicectomy within 1 month (range across studies 4·8–11·7 per cent). The pooled estimate was 8·2 (5·2 to 11·8) per cent (high‐quality evidence) (Table 3).
Table 3.
GRADE evidence profile: antibiotic therapy versus appendicectomy for acute non‐perforated appendicitis
| No. of patients with data* Time frame | Quality assessment | Summary of findings | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study event rates | Absolute risk difference† | Certainty in estimates | ||||||||
| Risk of bias | Inconsistency | Indirectness | Imprecision | Publication bias | Antibiotic therapy | Appendicectomy | ||||
| Major complications | ||||||||||
|
999 (5) 1 year |
Serious limitations: major and minor complications likely under‐reported in antibiotics group | No serious limitations | No serious limitations | Serious limitations: 95% confidence interval crosses 0, indicating no difference | Undetected | 25 of 510 (4·9) | 41 of 489 (8·4) |
−2·6 (−6·3, 1·1)% Favours antibiotic therapy |
Low | |
| Minor complications | ||||||||||
|
999 (5) 1 year |
Serious limitations: major and minor complications likely under‐reported in antibiotics group | Serious limitations: inconsistent forest plot estimates | No serious limitations | Serious limitations: 95% confidence interval crosses 0, indicating no difference | Undetected | 11 of 510 (2·2) | 61 of 489 (12·5) |
−7·2 (−18·1, 3·8)% Favours antibiotic therapy |
Very low | |
| Recurrence of appendicitis | ||||||||||
|
999 (5) 1 year |
No serious limitations | No serious limitations | No serious limitations | No serious limitations | Undetected | 114 of 510 (22·4) |
0 of 489 (0) |
22·6 (15·6 to 30·4)% Favours appendicectomy |
High | |
| Rate of appendicectomy within 1 month | ||||||||||
|
1112 (5) 1 month |
No serious limitations | No serious limitations | No serious limitations | No serious limitations | Undetected | 47 of 550 (8·5) |
561 of 562 (99·8) |
91·8 (88·2, 94·8)% Favours antibiotic therapy |
High | |
| Length of hospital stay | ||||||||||
|
1100 (5) In hospital |
No serious limitations | No serious limitations | Serious limitations: most patients operated on using open approach; laparoscopic approach would shorten length of hospital stay | No serious limitations | Undetected |
0·41 (0·26 to 0·57) days Favours appendicectomy |
Moderate | |||
| Length of sick leave | ||||||||||
|
1017 (3) 1 month |
No serious limitations | Serious limitations: inconsistent forest plot estimates | Serious limitations: most patients operated on using open approach; laparoscopic approach would shorten length of sick leave | Serious limitations: 95% confidence interval crosses 0, indicating no difference | Undetected |
−3·58 (−8·27, 1·11) days Favours antibiotic therapy |
Very low | |||
Values in parentheses are percentages unless indicated otherwise; values are
number of studies and
95 per cent confidence interval.
Major complications
Of the 510 patients allocated to antibiotic therapy, 25 had major complications versus 41 of 489 patients in the appendicectomy group: risk difference −2·6 (95 per cent c.i. –6·3 to 1·1) per cent (low‐quality evidence) (Fig. 2, Table 3). Major complications in the appendicectomy group included 32 appendiceal perforations, five deep infections, two incisional hernias, one laparoscopic adhesiolysis and one death. Major complications in the antibiotic therapy group included 23 appendiceal perforations, one adhesive bowel obstruction and one death. The quality of evidence was rated as low because of imprecision and high risk of bias (Table 3).
Figure 2.
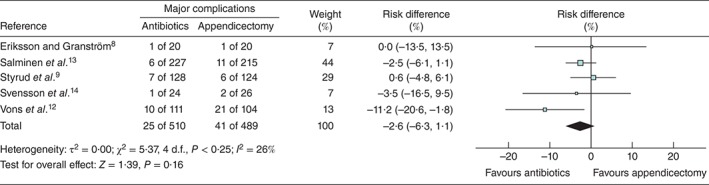
Forest plot showing absolute risk difference in major complications in antibiotic therapy versus appendicectomy group. Risk differences are shown with 95 per cent c.i.
Minor complications
Of the 510 patients allocated to antibiotic therapy, 11 had minor complications versus 61 of 489 patients in the appendicectomy group: risk difference −7·2 (95 per cent c.i. –18·1 to 3·8) per cent (very low‐quality evidence) (Fig. 3). Minor complications included 38 superficial wound infections, 22 instances of abdominal or incisional discomfort at 1 year (reported only by Salminen and colleagues13), and one case of diarrhoea in the appendicectomy group. Minor complications in the antibiotic group included three superficial wound infections, 4 instances of abdominal or incisional discomfort at 1 year (reported only by Salminen and colleagues13), and four complications that were not stated in more detail. None of the included trials reported any adverse effects of antibiotic treatment (such as diarrhoea or allergic reaction). The quality of evidence was rated as very low because of imprecision, inconsistency and high risk of bias in reporting complications (Table 3).
Figure 3.
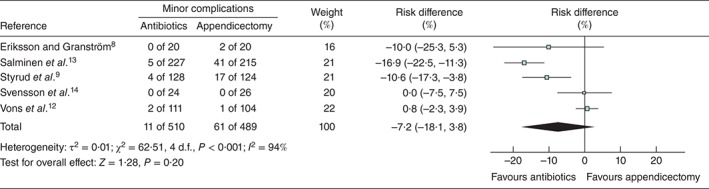
Forest plot showing absolute risk difference in minor complications in antibiotic therapy versus appendicectomy group. Risk differences are shown with 95 per cent c.i.
Recurrence of appendicitis within 1 year
None of the patients who underwent appendicectomy were reported to have recurrent appendicitis. The pooled estimate of recurrence in the antibiotic group, of whom 114 of 510 patients had a suspected or proven recurrence of appendicitis within 1 year, was 22·6 (15·6 to 30·4 per cent) (high‐quality evidence) (Table 3). Of these 114 appendices, 14 (12·3 per cent) were not inflamed on subsequent histopathology. Average (mean or median) time from initial conservative treatment with antibiotics to recurrence varied between 3·4 and 7·0 months in the included trials.
Duration of hospital stay
Three studies8, 9, 12 reported, and two authors13, 14 later provided data on hospital stay. Patients in the appendicectomy arms had a modestly shorter duration of hospital stay: mean difference 0·41 (95 per cent c.i. 0·26 to 0·57) days (moderate‐quality evidence) (Fig. 4, Table 3).
Figure 4.
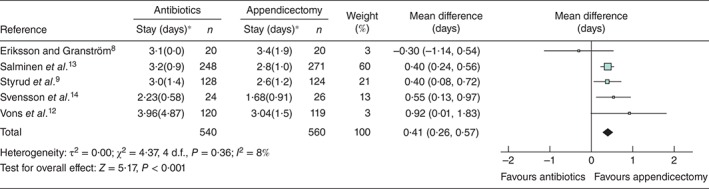
Forest plot showing mean difference in length of hospital stay in antibiotic therapy versus appendicectomy group. Mean differences are shown with 95 per cent c.i. *Values are mean(s.d.)
Duration of sick leave
Two studies9, 12 reported, and one author13 later provided data on sick leave. One study14 enrolled only children, and so sick leave was not applicable. The duration of sick leave did not differ materially between the groups; the mean difference was −3·58 (95 per cent c.i. –8·27 to 1·11) days, favouring antibiotic therapy (very low‐quality evidence) (Fig. 5, Table 3).
Figure 5.
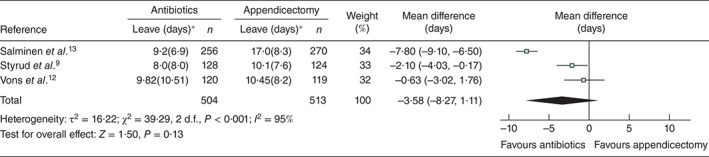
Forest plot showing mean difference in length of sick leave in antibiotic therapy versus appendicectomy group. Mean differences are shown with 95 per cent c.i. *Values are mean(s.d.)
Subgroup and sensitivity analyses
Neither the prespecified subgroup analyses nor the sensitivity analyses explained differences in minor or major complication rates (Figs S1–S6, supporting information).
Discussion
Five RCTs that followed more than 1100 patients with non‐perforated appendicitis for 1 year demonstrated both advantages and disadvantages to an initial management strategy of antibiotics with appendicectomy only as necessary versus immediate appendicectomy. Advantages of the antibiotic regimen include a potentially lower rate of major complications (primarily appendiceal perforations) (2·6 per cent less, low‐quality evidence), a potentially lower rate of minor complications (7·2 per cent less, very low‐quality evidence), potentially shorter sick leave (4 days shorter, very low‐quality evidence), and a lower rate of appendicectomies in the first month after presentation (91·8 per cent less, high‐quality evidence). These advantages need to be traded off against a 22·6 per cent incidence of recurrence of appendicitis at 1 year (high‐quality evidence) and potentially longer hospital stay (by 0·4 days, moderate‐quality evidence) (Table 3).
Relative to previous systematic reviews, this analysis has many strengths. Use of explicit eligibility criteria led to the exclusion of two trials11, 33 inappropriately included in other reviews16, 22, 23, 25: one that has been retracted owing to plagiarism33 and another trial that suffered from serious prognostic imbalance11. A comprehensive search led to the inclusion of two recently published trials13, 14. Two reviewers determined eligibility, assessed risk of bias, and abstracted data independently and in duplicate, with adjudication by a third reviewer as necessary. Rigorous meta‐analyses were conducted and prespecified subgroup effects were explored. Sensitivity analysis including a quasi‐randomized study did not change the results appreciably. The GRADE approach31, 32 was applied to assess quality of evidence for each outcome (Table 3).
Limitations of this review are largely those of the primary studies. As the diagnosis of appendicitis was made without CT in three of the RCTs8, 9, 14, they included patients with complicated appendicitis, and those without appendicitis at all. For studies that used CT, the rate of perforated appendix was variable: 18 per cent in the appendicectomy group in the French study12, but only 1 per cent in the Finnish trial13. This could be due to inaccuracy of the CT scans or progression of initially non‐perforated appendicitis. CT is far from perfect in differentiating complicated from uncomplicated appendicitis34, whereas scoring systems might be more helpful in selecting patients in future trials35.
The rate of operation in patients who did not have appendicitis on histopathology was very low in the included trials (0–3 per cent in most, and 15 per cent in 1 using clinical diagnosis only8). Although CT is limited in differentiating uncomplicated from complicated appendicitis, it has a high level of accuracy in differentiating patients with, and without appendicitis, leading to low rates of negative appendicectomy where CT was used routinely36. Another factor is that the threshold for the diagnosis of appendicitis based on histopathological findings (undefined in most of the studies) may have been low or very low. Only the Finnish study13 reported use of stringent criteria, which require inflammation in the muscularis of the appendix. Such strict criteria have been reported to yield higher negative appendicectomy rates37.
Risk of bias is a problem in all studies, with major limitations in some regarding allocation concealment, in all for blinding, and in many with respect to loss to follow‐up. There were also reporting problems that required some inferences in data abstraction (for example no study classified complications according to their severity, thus requiring reviewers' inferences regarding whether complications were major or minor). All authors failed to report complications of antibiotic therapy (such as diarrhoea or allergic reactions) and most failed to report appendicectomy complications in detail in patients who initially received antibiotics, but who went on to have appendicectomy for recurrent appendicitis8, 9, 12, 13.
Enrolment was slow in two of the biggest trials12, 13, which recruited approximately one to three patients per month per hospital. The largest trial13 was able to recruit less than 20 per cent of the patients treated for uncomplicated appendicitis in the trial hospitals during the enrolment period, and the study was actually terminated prematurely owing to slow enrolment. Thus, it is possible that only the least sick patients were enrolled in these trials. If that is so, the results of antibiotic treatment may not be as good if administered to sicker patients.
It is possible that some patients would prefer to avoid an appendicectomy because of rare but serious potential complications of general or spinal anaesthesia, but also because of possible short‐ and long‐term pain associated with surgery, with decreased quality of life. Unfortunately, investigators did not measure pain consistently or rigorously, and did not report quality of life at all.
Generalizability to current clinical practice is also a concern. Only 22·6 per cent of procedures in the appendicectomy group were performed laparoscopically. Systematic reviews38, 39 of RCTs comparing open with laparoscopic appendicectomy have shown that the laparoscopic approach is associated with reduced wound infections, as well as a lower rate of bowel obstruction. As the majority of minor complications were wound infections and incisional discomfort, it is likely that a laparoscopic approach will reduce the rate of minor complications. Furthermore, more frequent use of a laparoscopic approach should shorten hospital stay and sick leave38, 39. On the other hand, all RCTs reported in‐hospital intravenous antibiotic treatment for 2–3 days, and it might be possible to reduce length of stay by using a different antibiotic regimen.
Other limitations included insufficient follow‐up in all of the included studies. The rate of recurrent appendicitis was approximately 23 per cent during the first year; it is unknown how much this rate might rise with longer follow‐up. Similarly, introducing broad‐spectrum antibiotics to a large patient population carries the risk of worsening antibiotic resistance. It could be argued that antibiotics should be reserved for patients with a definitive diagnosis of uncomplicated appendicitis.
Despite the limitations of the available studies, they provide valuable evidence regarding the outcomes of antibiotic first versus immediate surgery for acute non‐perforated appendicitis. The trade‐off between the antibiotic‐first approach – potentially 3 per cent fewer major complications, 7 per cent fewer minor complications, 4 days' shorter sick leave and 92 per cent fewer appendicectomies in the first month – must be balanced against the disadvantages: a 23 per cent recurrence rate within 1 year and slightly longer hospital stay (half a day). Patients averse to surgery are likely to choose an initial trial of antibiotics; those averse to the possibility of recurrence may prefer immediate appendicectomy. Ensuring that the decision is consistent with patients' values and preferences requires shared decision‐making40.
Supporting information.
Additional supporting information may be found in the online version of this article:
Appendix S1 Search strategies (Word document)
Table S1 Characteristics of the study by Hansson and colleagues10 (Word document)
Table S2 Risk of bias in the study by Hansson and colleagues10 (Word document)
Table S3 Complications considered (Word document)
Fig. S1 Sensitivity analysis examining effect of inclusion of data from Hansson et al.10: forest plot showing absolute risk difference in major complications in antibiotic therapy versus appendicectomy groups (Word document)
Fig. S2 Sensitivity analysis examining effect of inclusion of data from Hansson et al.10: forest plot showing absolute risk difference in minor complications in antibiotic therapy versus appendicectomy groups (Word document)
Fig. S3 Subgroup analysis of studies with or without CT confirmation of diagnosis: forest plot showing absolute risk difference in major complications in antibiotic therapy versus appendicectomy groups (Word document)
Fig. S4 Subgroup analysis of studies with or without CT confirmation of diagnosis: forest plot showing absolute risk difference in minor complications in antibiotic therapy versus appendicectomy groups (Word document)
Fig. S5 Subgroup analysis according to completeness of data (high or low risk of bias): forest plot showing absolute risk difference in major complications in antibiotic therapy versus appendicectomy groups (Word document)
Fig. S6 Subgroup analysis according to completeness of data (high or low risk of bias): forest plot showing absolute risk difference in minor complications in antibiotic therapy versus appendicectomy groups (Word document)
Supporting information
Appendix S1 Search strategies
Table S1 Characteristics of the study by Hansson and colleagues10
Table S2 Risk of bias in the study by Hansson and colleagues10
Table S3 Complications considered
Fig. S1 Sensitivity analysis examining effect of inclusion of data from Hansson et al. 10: forest plot showing absolute risk difference in major complications in antibiotic therapy versus appendicectomy groups. Risk differences are shown with 95 per cent c.i.
Fig. S2 Sensitivity analysis examining effect of inclusion of data from Hansson et al. 10: forest plot showing absolute risk difference in minor complications in antibiotic therapy versus appendicectomy groups. Risk differences are shown with 95 per cent c.i.
Fig. S3 Subgroup analysis of studies with or without CT confirmation of diagnosis: forest plot showing absolute risk difference in major complications in antibiotic therapy versus appendicectomy groups. Risk differences are shown with 95 per cent c.i.
Fig. S4 Subgroup analysis of studies with or without CT confirmation of diagnosis: forest plot showing absolute risk difference in minor complications in antibiotic therapy versus appendicectomy groups. Risk differences are shown with 95 per cent c.i.
Fig. S5 Subgroup analysis according to completeness of data (high or low risk of bias): forest plot showing absolute risk difference in major complications in antibiotic therapy versus appendicectomy groups. Risk differences are shown with 95 per cent c.i
Fig. S6 Subgroup analysis according to completeness of data (high or low risk of bias): forest plot showing absolute risk difference in minor complications in antibiotic therapy versus appendicectomy groups. Risk differences are shown with 95 per cent c.i
Acknowledgements
The authors thank information specialist R. Cobain for advice regarding literature search strategies. They also thank the following researchers for checking extracted data for accuracy and/or providing additional information regarding the original studies: J. Assarsson, P. Salminen, J. Svensson and C. Vons.
This Antibiotic Therapy Versus Appendicectomy for Treatment of Nonperforated Acute Appendicitis (AVATAR) project was conducted by the Clinical Urology and Epidemiology (CLUE) Working Group supported by the Academy of Finland (number 276046), Competitive Research Funding of the Helsinki and Uusimaa Hospital District, Jane and Aatos Erkko Foundation, and Sigrid Jusélius Foundation. V.S. also received funding from Vatsatautien tutkimussäätiö Foundation and Mary and Georg Erhnrooth's Foundation. The sponsors had no role in the analysis and interpretation of the data, or preparation, review or approval of the manuscript.
Disclosure: The authors declare no conflict of interest.
References
- 1. Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 1990; 132: 910–925. [DOI] [PubMed] [Google Scholar]
- 2. Masoomi H, Nguyen NT, Dolich MO, Mills S, Carmichael JC, Stamos MJ. Laparoscopic appendectomy trends and outcomes in the United States: data from the Nationwide Inpatient Sample (NIS), 2004–2011. Am Surg 2014; 80: 1074–1077. [PubMed] [Google Scholar]
- 3. Fitz RH. Perforating inflammation of the vermiform appendix: with special reference to its early diagnosis and treatment. Am J Med Sci 1886; 92: 321–346. [Google Scholar]
- 4. McBurney C. Experience with early operative interference in cases of disease of the vermiform appendix. NY Med J 1889; 50: 676–684. [Google Scholar]
- 5. Coldrey E. Treatment of acute appendicitis. Br Med J 1956; 2: 1458–1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Combined traditional Chinese and western medicine in acute appendicitis. Chin Med J (Engl) 1977; 3: 266–269. [PubMed] [Google Scholar]
- 7. Adams ML. The medical management of acute appendicitis in a nonsurgical environment: a retrospective case review. Mil Med 1990; 155: 345–347. [PubMed] [Google Scholar]
- 8. Eriksson S, Granström L. Randomized controlled trial of appendicectomy versus antibiotic therapy for acute appendicitis. Br J Surg 1995; 82: 166–169. [DOI] [PubMed] [Google Scholar]
- 9. Styrud J, Eriksson S, Nilsson I, Ahlberg G, Haapaniemi S, Neovius G et al Appendectomy versus antibiotic treatment in acute appendicitis. A prospective multicenter randomized controlled trial. World J Surg 2006; 30: 1033–1037. [DOI] [PubMed] [Google Scholar]
- 10. Hansson J, Körner U, Khorram‐Manesh A, Solberg A, Lundholm K. Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg 2009; 96: 473–481. [DOI] [PubMed] [Google Scholar]
- 11. Turhan AN, Kapan S, Kütükçü E, Yiğitbaş H, Hatipoğlu S, Aygün E. Comparison of operative and non operative management of acute appendicitis. Ulus Travma Acil Cerrahi Derg 2009; 15: 459–462. [PubMed] [Google Scholar]
- 12. Vons C, Barry C, Maitre S, Pautrat K, Leconte M, Costaglioli B et al Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open‐label, non‐inferiority, randomised controlled trial. Lancet 2011; 377: 1573–1579. [DOI] [PubMed] [Google Scholar]
- 13. Salminen P, Paajanen H, Rautio T, Nordström P, Aarnio M, Rantanen T et al Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis. JAMA 2015; 313: 2340–2349. [DOI] [PubMed] [Google Scholar]
- 14. Svensson JF, Patkova B, Almström M, Naji H, Hall NJ, Eaton S et al Nonoperative treatment with antibiotics versus surgery for acute nonperforated appendicitis in children. Ann Surg 2015; 261: 67–71. [DOI] [PubMed] [Google Scholar]
- 15. Kirby A, Hobson RP, Burke D, Cleveland V, Ford G, West RM. Appendicectomy for suspected uncomplicated appendicitis is associated with fewer complications than conservative antibiotic management: a meta‐analysis of post‐intervention complications. J Infect 2015; 70: 105–110. [DOI] [PubMed] [Google Scholar]
- 16. Liu ZH, Li C, Zhang XW, Kang L, Wang JP. Meta‐analysis of the therapeutic effects of antibiotic versus appendicectomy for the treatment of acute appendicitis. Exp Ther Med 2014; 7: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Svensson J, Hall N, Eaton S, Pierro A, Wester T. A review of conservative treatment of acute appendicitis. Eur J Pediatr Surg 2012; 22: 185–194. [DOI] [PubMed] [Google Scholar]
- 18. Mason RJ, Moazzez A, Sohn H, Kathouda N. Meta‐analysis of randomized trials comparing antibiotic therapy with appendectomy for acute uncomplicated (no abscess or phlegmon) appendicitis. Surg Infect (Larchmt) 2012; 13: 74–84. [DOI] [PubMed] [Google Scholar]
- 19. Varadhan KK, Neal KR, Lobo DN. Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: meta‐analysis of randomised controlled trials. BMJ 2012; 344: e2156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fitzmaurice G. Antibiotics versus appendectomy in the management of acute appendicitis: a review of the current evidence. Can J Surg 2011; 54: 307–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Liu K, Fogg L. Use of antibiotics alone for treatment of uncomplicated acute appendicitis: a systematic review and meta‐analysis. Surgery 2011; 150: 673–683. [DOI] [PubMed] [Google Scholar]
- 22. Wilms IM, de Hoog DE, de Visser DC, Janzing HM. Appendectomy versus antibiotic treatment for acute appendicitis. Cochrane Database Syst Rev 2011; (11)CD008359. [DOI] [PubMed] [Google Scholar]
- 23. Ansaloni L, Catena F, Coccolini F, Ercolani, Gazzotti F , Pasqualini E et al Surgery versus conservative antibiotic treatment in acute appendicitis: a systematic review and meta‐analysis of randomized controlled trials. Dig Surg 2011; 28: 210–221. [DOI] [PubMed] [Google Scholar]
- 24. Varadhan KK, Humes DJ, Neal KR, Lobo DN. Antibiotic therapy versus appendectomy for acute appendicitis: a meta‐analysis. World J Surg 2010; 34: 199–209. [DOI] [PubMed] [Google Scholar]
- 25. Liu KL, Fogg L. Use of antibiotics alone for treatment of uncomplicated acute appendicitis: a systematic review and meta‐analysis. Surgery 2011; 150: 673–683. [DOI] [PubMed] [Google Scholar]
- 26. Karanicolas PJ, Montori VM, Devereaux PJ, Schünemann H, Guyatt GH. A new ‘mechanistic–practical’ framework for designing and interpreting randomized trials. J Clin Epidemiol 2009; 62: 479–484. [DOI] [PubMed] [Google Scholar]
- 27. Guyatt GH, Busse JW. Modification of Cochrane Tool to Assess Risk of Bias in Randomized Trials http://distillercer.com/resources/ [accessed 6 September 2015].
- 28. Akl EA, Johnston BC, Alonso‐Coello P, Neumann I, Ebrahim S, Briel M et al Addressing dichotomous data for participants excluded from trial analysis: a guide for systematic reviewers. PLoS ONE 2013; 8: e57132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ebrahim S, Akl EA, Mustafa RA, Sun X, Walter SD, Heels‐Ansdell et al Addressing continuous data for participants excluded from trial analysis: a guide for systematic reviewers. J Clin Epidemiol 2013; 66: 1014–1021.e1. [DOI] [PubMed] [Google Scholar]
- 30. Ebrahim S, Johnston BC, Akl EA, Mustafa RA, Sun X, Walter SD et al Addressing continuous data measured with different instruments for participants excluded from trial analysis: a guide for systematic reviewers. J Clin Epidemiol 2014; 67: 560–570. [DOI] [PubMed] [Google Scholar]
- 31. Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck‐Ytter Y, Schünemann HJ et al What is ‘quality of evidence’ and why is it important to clinicians? BMJ 2008; 336: 995–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck‐Ytter Y, Alonso‐Coello P et al GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008; 336: 924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Malik AA, Bari SU. Conservative management of acute appendicitis. J Gastrointest Surg 2009; 13: 966–970. [DOI] [PubMed] [Google Scholar]
- 34. Leeuwenburgh MM, Wiezer MJ, Wiarda BM, Bouma WH, Phoa SS, Stockmann HB et al Accuracy of MRI compared with ultrasound imaging and selective use of CT to discriminate simple from perforated appendicitis. Br J Surg 2014; 101: e147–e155. [DOI] [PubMed] [Google Scholar]
- 35. Atema JJ, van Rossem CC, Leeuwenburgh MM, Stoker J, Boermeester MA. Scoring system to distinguish uncomplicated from complicated acute appendicitis. Br J Surg 2015; 102: 979–990. [DOI] [PubMed] [Google Scholar]
- 36. Rao PM, Rhea JT, Rattner DW, Venus LG, Novelline RA. Introduction of appendiceal CT: impact on negative appendectomy and appendiceal perforation rates. Ann Surg 1999; 229: 344–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mariadason JG, Wang WN, Wallack MK, Belmonte A, Matari H. Negative appendicectomy rate as a quality metric in the management of appendicitis: impact of computed tomography, Alvarado score and the definition of negative appendicectomy. Ann R Coll Surg Engl 2012; 94: 395–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sauerland S, Jaschinski T, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev 2010; (10)CD001546. [DOI] [PubMed] [Google Scholar]
- 39. Ohtani H, Tamamori Y, Arimoto Y, Nishiguchi Y, Maeda K, Hirakawa K. Meta‐analysis of the results of randomized controlled trials that compared laparoscopic and open surgery for acute appendicitis. J Gastrointest Surg 2012; 16: 1929–1939. [DOI] [PubMed] [Google Scholar]
- 40. Flynn D, Knoedler MA, Hess EP, Murad MH, Erwin PJ, Montori VM et al Engaging patients in health care decisions in the emergency department through shared decision‐making: a systematic review. Acad Emerg Med 2012; 19: 959–967. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Search strategies
Table S1 Characteristics of the study by Hansson and colleagues10
Table S2 Risk of bias in the study by Hansson and colleagues10
Table S3 Complications considered
Fig. S1 Sensitivity analysis examining effect of inclusion of data from Hansson et al. 10: forest plot showing absolute risk difference in major complications in antibiotic therapy versus appendicectomy groups. Risk differences are shown with 95 per cent c.i.
Fig. S2 Sensitivity analysis examining effect of inclusion of data from Hansson et al. 10: forest plot showing absolute risk difference in minor complications in antibiotic therapy versus appendicectomy groups. Risk differences are shown with 95 per cent c.i.
Fig. S3 Subgroup analysis of studies with or without CT confirmation of diagnosis: forest plot showing absolute risk difference in major complications in antibiotic therapy versus appendicectomy groups. Risk differences are shown with 95 per cent c.i.
Fig. S4 Subgroup analysis of studies with or without CT confirmation of diagnosis: forest plot showing absolute risk difference in minor complications in antibiotic therapy versus appendicectomy groups. Risk differences are shown with 95 per cent c.i.
Fig. S5 Subgroup analysis according to completeness of data (high or low risk of bias): forest plot showing absolute risk difference in major complications in antibiotic therapy versus appendicectomy groups. Risk differences are shown with 95 per cent c.i
Fig. S6 Subgroup analysis according to completeness of data (high or low risk of bias): forest plot showing absolute risk difference in minor complications in antibiotic therapy versus appendicectomy groups. Risk differences are shown with 95 per cent c.i


