Abstract
Objectives To determine the effect of a consumer‐directed information campaign to increase knowledge of folate for the prevention of neural tube defects among women of child‐bearing age, and to measure women’s recall of sources of information and knowledge about folate.
Design A community randomized trial.
Setting Three matched pairs of geographically distinct Local Government Areas in the state of Victoria, Australia.
Intervention Printed information recommending folate intake to decrease the risk of neural tube defects was disseminated to women of child‐bearing age in three of the Local Government Areas selected randomly.
Main outcome measure The proportion of women aware of the association between folate and spina bifida.
Results Of 1197 women interviewed prior to the intervention, 12.4% (adjusted for the cluster and population sampling unit) were aware of folate and neural tube defects. After the intervention, there was not only a significant background increase of 3.4% (P=0.02) in folate awareness since the pre‐intervention survey (n=603), but also a significant additional increase of 4.0% (P=0.04) owing to the intervention itself (n=603). Only 70% of women who were aware of folate knew the correct timing.
Conclusions The provision of printed educational material can increase folate awareness among women of child‐bearing age. A comprehensive, long‐term and ongoing health promotion campaign including such material, together with initiatives by relevant health service providers and the food industry, could best address the current low levels of folate awareness among women of child‐bearing age.
Keywords: community intervention, folate, neural tube defects, randomized trial
Introduction
Neural tube defects (NTDs) are a group of major congenital structural abnormalities of the brain, skull and spinal cord affecting at least one pregnancy in 630 in Victoria, Australia. 1 The introduction of antenatal screening and termination of affected pregnancies has reduced the birth prevalence. However, the number of affected pregnancies has been constant in recent years, 1 in spite of the evidence since the early 1990s from randomized controlled trials that an adequate intake of folate periconceptionally can reduce risk of NTDs by about two‐thirds. 2 , 3 Health authorities have recommended a daily intake of folate of 0.4 mg for the prevention of NTDs, 4 which is far in excess of the habitual dietary intake of most Australian women. 5 It is for this reason that the fortification of staple foods with folate has been recommended. 6
While there is strong evidence for the role of folate as a beneficial form of care, levels of knowledge are low, with usually less than 20% of women aware of the reduction of NTDs associated with folate. 7 In the absence of relevant knowledge, women are unable to initiate appropriate behavioural change to increase folate intake. Until this is addressed, the individual losses and other societal burdens from NTDs will remain. Further, it is inappropriate to direct educational or informational campaigns solely towards women planning a pregnancy, as many pregnancies are unplanned. Therefore such campaigns directed at all women of child‐bearing age are necessary. There is debate as to how evidence‐based information should be communicated to consumers. This paper reports the evaluation of a randomized trial of a consumer‐directed informational campaign in which the objective was to increase knowledge of the role of folate in the prevention of NTDs. The effect of sociodemographic factors on the outcome was also assessed.
Methods
Study population
The study population was a random sample of women of child‐bearing age (15–44 years) living in six Local Government Areas (LGAs) in Victoria, Australia, having a total population of 442 000 of whom 25% were women of child‐bearing age. The six LGAs represented approximately 10% of the population of Victoria.
Assignment
There were three pairs of LGAs (or clusters) matched on numbers of births per annum, proportion of women who were of non‐English‐speaking background, size, rural or metropolitan status, sociodemographic profile and geographic isolation from other potentially selected LGAs. One of each of the pairs of LGAs was assigned to be the intervention site after a baseline survey had been done, using a random draw in public by two individuals independent of the project team.
Intervention implementation
The intervention was based on printed material which had been extensively reviewed by a range of health professionals and focus groups, and was provided to one randomly selected LGA in each cluster pair. This material (available on request) was directed towards all women, not just those contemplating pregnancy, and was presented at a level consistent with about 7 years of schooling, based on the Flesch–Kincaid grade level. 8 The material consisted of an A3 poster, a single‐sided A5 brief leaflet, and the more detailed information kit incorporating two double‐sided A4 folded brochures and a magnetized card (for fridge, etc.), enclosed in a band. The unit costs for these components were: posters $A2.96; information kits $A0.49 [including the magnet ($A0.17) and band]; and brief leaflets $A0.05. Although moderately expensive, the magnet was seen as more likely to be retained as a tangible reminder.
Under the slogan ‘Folate for Women – Folate before Pregnancy’ were the recommendations for actions for risk reduction of NTDs, i.e. taking a low dose (0.5 mg, as recommended by the National Health and Medical Research Council 9 ), choosing foods fortified with folate, and eating more of the foods that are naturally rich in folate, with the information that the folic acid tablet was the most effective means by which women could increase their folate intake.
The intervention was implemented between late July and early October 1997. The intervention material, along with a letter outlining the nature of the project and its requirements, was disseminated substantially in person (all information kits and brief leaflets, and 66% of the posters) to locations where the target group, women of child‐bearing age, might be expected to see it and be interested enough to read it. This included pharmacies, Maternal and Child Health Centres (MCHCs) for the information kits, and supermarkets for the brief leaflets. The poster, again with a request for prominent display and including copies of the information kits and posters, was also delivered or mailed to kindergartens, child care centres, a variety of community centres such as neighbourhood houses, youth drop‐in centres and job centres, schools (primary, secondary and tertiary, private and State), hospitals, infant‐related shops (toys and clothes), sporting groups, health services (e.g. dental surgeries, physiotherapy clinics, dietitians, weight loss groups, chiropractic clinics and naturopaths), libraries, fitness centres and hairdressers.
Although medical practitioners had no direct involvement in the intervention, those practicing in the intervention areas were advised by mail on commencement of the study, and provided with single copies of the brief leaflet and information kit.
During the intervention, periodic visits were made to monitor it. Near the end of the intervention period, supermarkets were encouraged to enclose the brief leaflets with customers’ shopping. At the closure of the intervention, locations were visited to collect remaining stocks of material, in order both to estimate resources used and to avoid variable exposure times. There was a mail‐out to all locations where posters had been left or sent, with a request to remove posters from public view.
Outcome measures
The primary outcome measure was folate awareness. Folate awareness was assessed by asking women if they knew any way in which spina bifida could be prevented; for those who answered ‘Yes’ or ‘Not sure’, this was followed by the question: ‘Which one of the following prevents spina bifida if there is enough in the mother’s diet: vitamin A, vitamin C, vitamin D, thiamine or folate (or folic acid)?’. Secondary outcome measures (determined in folate‐aware women) were sources of information on folate and knowledge of when to increase folate intake and folate‐rich foods. Answers to a series of questions about where and when they had seen or heard the information were obtained from women who answered ‘Yes’ to the question: ‘Have you seen or heard any information about folate and prevention of birth defects of the spinal cord?’.
Sample size
Because of the expense, logistic issues and the possibility of contamination between LGAs with large populations, it was decided a priori that the maximum number of pairs of LGAs would be three, giving six communities in all. There were two sample size estimates. For the baseline survey, it was calculated that 200 interviews in each LGA would provide an estimate of the level of awareness within 4% over an awareness range between 10% and 35% (with 95% confidence, a power of 80% and an intercluster standard error of 3%). The sample size needed to detect a doubling of the proportion aware from the unadjusted baseline level of awareness of 14% to 28% (α=0.05, two‐sided, 1 − β=0.80), given individual randomization, was 146 in each LGA. Power calculations using matched pairs with randomization by group indicated that 200 in each LGA would be required to detect the same effect size and power. 10
Survey methodology
A scannable questionnaire (available on request) for use in a telephone survey was developed to measure awareness of the relationship between folate and NTDs, sources of information on folate, food sources of folate, dosage and timing. This questionnaire was administered to women of child‐bearing age, identified from a random current list of telephone numbers generated for each LGA using the marketing‐ pro software (Windows version: Desktop Marketing Systems Pty Ltd, Kew, Victoria, Australia). This was done both before and after the intervention (in November–December of both 1996 and 1997). Responses were not obtained from non‐English speakers. Respondents who were in the first survey were excluded from the second. A quota of 2% of responses was set in the 40–44 year group, corresponding to the proportion of births in this age group in the target population. In the post‐intervention survey the information kit was offered to respondents who expressed concern during the interview.
Telephone interviewers were unaware of the LGA allocation, and the interviewing schedule was structured so that all LGAs were surveyed at comparable rates both over time and by interviewer.
Analysis
The analysis of the main outcome measure, the proportion of women aware of the association between folate and spina bifida, was estimated using survey analysis in the stata statistical software package (Release 5.0, 1997: Stata Corporation, College Station, USA). This analysis incorporated in it the effects of all of the pairs (strata), the LGA sampling unit (population sampling unit) and the age/location population sampling fraction. Multivariate logistic regression modelling was conducted to adjust for and assess sociodemographic variables, giving P‐values appropriate to the LGA as the unit of analysis. The strength of associations between folate awareness and sources of information was determined using a similar analysis in stata, adjusting for the LGA sampling unit.
Ethics approval
Approval for this study was granted by the Victorian Government, Department of Human Services Ethics Committee.
Results
Characteristics of populations surveyed
Pre‐intervention, a total of 1197 women were interviewed by telephone; and post‐intervention 1206 were interviewed. To obtain these, a total of approximately 8000 telephone numbers were contacted. Up to five calls per number were made, and an 85% contact rate was achieved, of which 42% provided an eligible subject; of these 75% agreed to participate. Thus, of the overall number of calls made, 27% yielded a study subject. However, this percentage varied according to age group. with only 15% in the 15–24 year group and 29% in the 25–44 year group.
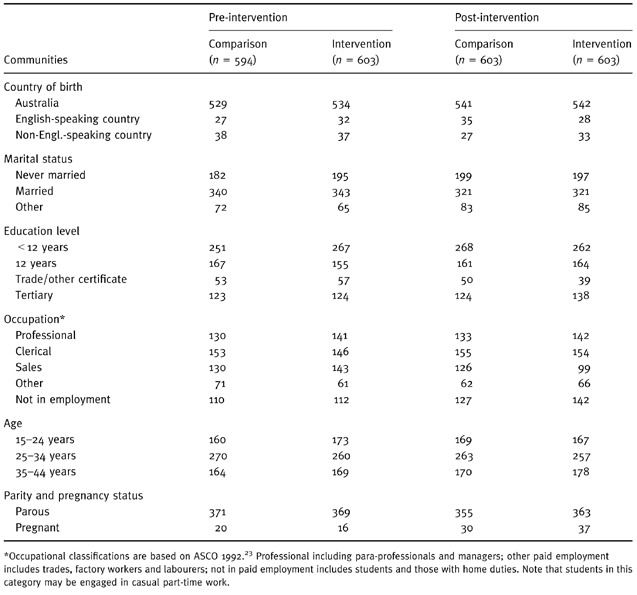
Demographic characteristics of the groups before and after intervention are shown in Table 1. Numbers only are presented, and these are comparable between LGAs because of the comparability of the numbers sampled in each LGA. There was close agreement between all demographic characteristics measured at the two survey times, but between the pre‐ and post‐intervention surveys there was a significant difference in occupational status (P=0.01). The metropolitan sites had a higher proportion of non‐Australian‐born women and women aged 25–34 years than the rural locations (both P < 0.001). Pregnancy status was volunteered pre‐intervention and asked for post‐intervention (at the request of the Ethics Committee); therefore, the numbers are not strictly comparable between survey times, but are comparable within survey times.
Table 1.
Demographic attributes of survey populations in pre‐intervention and post‐intervention surveys, combined means
Folate awareness
Correct responses to the folate awareness question are shown as percentages in Table 2 for pre‐ and post‐intervention. At baseline (pre‐intervention), control and intervention communities have been combined since no differences were found at that time (P=0.44); the overall estimate of awareness was 12%. This varied significantly by age, with women less than 25 years of age being significantly less likely to be aware (5% compared with 19% in the 25–34 year age group and 12% in the group aged 35 years and over; P < 0.001), and by occupational status, with those in professional occupations being significantly more likely to be aware (20%, P=0.03) than those in other occupational groups.
Table 2.
Folate awareness in women stratified by demographic characteristics
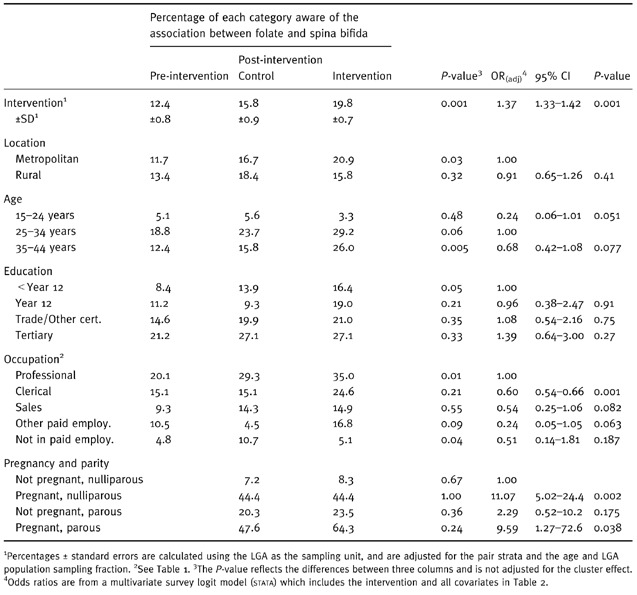
After the intervention, there was a background temporal change in folate awareness as measured by the increase in the comparison communities of 3.4% (P=0.02), and an increase above this owing to the intervention of 4.0% [odds ratio (OR)=1.37, 95% confidence interval (CI)=1.33–1.42, P=0.001], using the LGA as the sampling unit and adjusting for pairs and population sampling fraction. Owing to the under‐representation of women aged less than 20 years and the 2% quota on those aged 40 years or more, the folate awareness was estimated for ages of 20–39 years only, and comparable differences owing to the passage of time and to the intervention were found: 14.7%, 19.1% and 23.2% for the pre‐intervention, comparison and post‐intervention communities, respectively.
In general, the differences seen at baseline within the covariates remained in the post‐intervention survey, in the comparison and intervention communities. Of particular interest was the change shown over time and between the comparison and intervention communities within each stratum of the socio‐economic variables. This is indicated by the P‐value in the fifth column of Table 2. Multivariate analysis including the intervention and all the socio‐economic variables showed that age and occupational status remained significant. ORs, 95% CIs and associated P‐values are shown in the last three columns of Table 2.
In the post‐intervention survey, 5.6% women stated that they were pregnant. The data on parity and pregnancy have been stratified into four mutually exclusive levels. When compared with the group of women who neither had had a baby nor were pregnant, all other groups were more likely to be folate‐aware; however, only those women who were pregnant were significantly so.
Women who were folate‐aware were asked questions relating to food sources of folate and the correct timing to minimize risk of NTDs. Post‐intervention, for these women, 83% (or only 15% of the whole sample) were aware of the correct food sources and 70% (or 13% overall) were aware of the correct timing.
Post‐intervention information sources, and knowledge about folate and NTDs
Four hundred and seventy‐five posters, 3940 information kits and 67 200 brief leaflets were distributed, targeting a population of approximately 45 000 women of child‐bearing age. In total, 14 supermarkets, 28 pharmacies, 26 MCHCs and 385 additional venues for posters received the intervention material.
Overall, 193 (32%) of those in the intervention locations reported seeing information on folate and spina bifida, compared with 129 (21%) in the comparison communities (see Table 3: any source versus no sources; OR=1.80, CI=1.41–2.31, P=0.005).
Table 3.
Sources of information about folate and impact on folate awareness
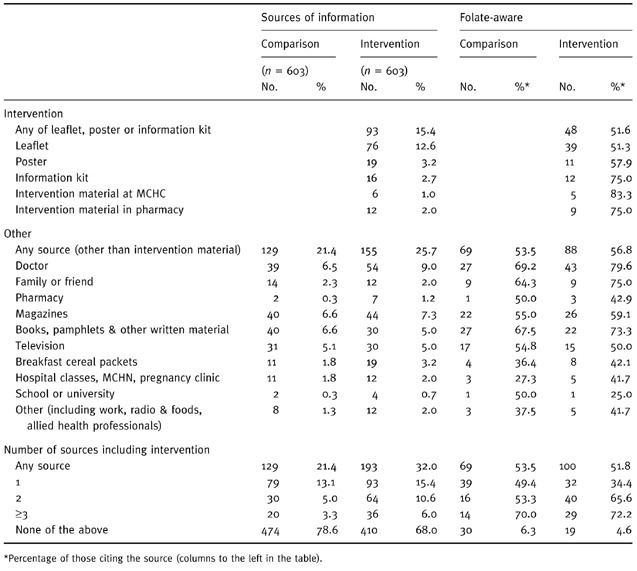
Of the intervention material, the leaflet, distributed mainly in supermarkets, was remembered as being seen by four times as many women as either the poster or the information kit. Awareness of the association between folate and spina bifida was highest in those who reported seeing the information kit (75%), compared with either the poster (58%) or the leaflet (51%). Neither pharmacies nor MCHCs (although both were specifically targeted for the intervention) made an impact on women: 2% and 1%, respectively, were reported as sources of information, although the awareness of those who did cite these sources was high (>75%).
Other sources of information were cited by 26% and 21% of the intervention and comparison communities, respectively. Doctors (8% overall), magazines (7%), books and other written material (6%) and television (5%) were the most commonly cited sources. Breakfast cereal boxes were cited by less than 3%. Nearly all sources were reported more commonly by those in intervention communities, although the differences did not reach significance. Women who had seen any source of information were more likely to be aware of the folate association (52%) than those women who reported never having seen information (7% or less; OR=17.31, CI=9.69–30.9, P < 0.001). Amongst these sources of information, folate awareness was highest in those who cited doctors, family or friends.
More women in the intervention communities (17.1%) than in the comparison communities (8.1%) reported seeing more than one source of information, and there was a significant increasing trend in folate awareness with increasing number of sources [OR(trend)=4.56, CI=3.80–5.47, P < 0.001], with over 70% of women who had seen three or more sources of information being aware of the association between folate and spina bifida.
Discussion
Response rates and internal and external validity
Response rates overall were satisfactory, although there may have been an under‐representation of young women, perhaps owing to a reluctance to be interviewed, a greater mobility, and/or restricted access to telephones. Differences in access to telephones seems unlikely, as a high proportion of households have telephones (96.6% in Victoria in 1991) and there are only small differences in telephones access between age groups. 11
The agreement between the survey population groups over the time period of the study, and between the comparison and intervention communities in the demographic characteristics, is good. There was also agreement with census statistics for the corresponding LGAs, although non‐Australian‐born people are under‐represented compared with the total Victorian population owing to oversampling of the rural LGAs.
Effect of intervention on folate awareness
This study has shown significant changes both in time and as a result of the intervention in folate awareness. Even this brief intervention had a positive impact on folate awareness, the 4% difference between the comparison and intervention groups being significant. If the levels of awareness of the post‐intervention comparison communities are considered to represent an intermediate measure of exposure to folate information, then there was a significant increasing trend in the overall awareness from baseline (12%) to intervention (20%). Thus the study provided evidence that the 2‐month intervention had the effect of significantly accelerating the acquisition of awareness of the association between folate and spina bifida over the underlying temporal rate of increase. This effect remained even when the under‐represented age groups, namely those less than 20 years and greater than 39 years, were excluded from the analysis. Unless the non‐responders in the younger age groups had a much lower level of awareness (which is unlikely since only 5% of the sample were aware), the significance of the overall outcome is unlikely to change.
Pre‐intervention sample size calculations indicated that with 80% power it would be possible to detect a 14% increase in folate awareness, yet the 4% increase found in the study proved to be significant. This unexpected significance we believe to be the result of the adjustment by age and LGA population fraction used in the analysis, giving increased efficiency and not taken into account in the sample size estimates. A paper dealing with the technical aspects of analysis associated with the unexpected significance is in preparation.
There were, however, large differences in folate awareness across the age strata and in the efficacy of the intervention for particular age groups. Younger women (15–24 years) were less aware than older women and did not benefit from this intervention, nor was there was any indication of a temporal trend in this age group. Lower folate awareness in younger women has also been observed by others. 12 , 13 This study confirms that innovative and ongoing health promotion activity will be required to impact on the folate awareness of this group. Women with less education and in less skilled employment, or those not in paid employment, also had lower folate awareness, as has also been found in the Netherlands. 14 Although the folate awareness of pregnant and parous women was considerably higher than that of non‐pregnant and nulliparous women, it is uncertain as to whether or not these women obtained this information at a time when they might have initiated behavioural change to reduce their risk of an NTD pregnancy. Following the extensive Health Education Authority folic acid awareness campaign in the United Kingdom, the majority of pregnant women (77%) stated that they knew the benefits of folic acid pre‐pregnancy; however, overall compliance was not good, with 43% taking folic acid pre‐pregnancy. 15 None the less, awareness of the role of folate in reducing the risk of NTDs is a predictor of the periconceptional use of folic acid. 16
It is apparent that, in the absence of a comparison community, the benefit of the intervention would have been overestimated. This assumes that the increase in awareness in the comparison arm was indicative of a background change over time, rather than of contamination from the intervention, which, on balance, seems improbable. Had there been contamination from the intervention, the ‘true’ effect of the intervention would have been even larger, so the claim that the intervention was effective is not speculative. There is debate as to how the effectiveness of information provision to consumers should be evaluated, 17 but this study confirms the advantage of randomized control trial design. 18 We believe that our study is the first such study relating to periconceptional folate, and the recently published Cochrane Review on this subject noted the absence of controlled studies examining the impact of disseminating this information. 19
Post‐intervention information sources, and knowledge of folate and NTDs
The majority of women had no recollection of folate‐related information, even in the intervention communities where printed information was widely distributed. There was, however, a higher recall of exposure to information in the intervention communities, with the intervention material being the most commonly cited source of information. Of this, the leaflet was the most frequently cited source, although women accessing this were not as folate‐aware as women receiving their knowledge from the information kit, general practitioners or some other written information. The impact of access to information on folate awareness was profound: overall 42% of women who recalled only a single source were aware, compared with 5% without recall. Furthermore, there was a gradient with increasing exposure: overall 72% of women who had seen three or more sources of information were folate‐aware. This confirms the reinforcing impact that information from multiple sources has on heightened awareness. Our experience suggests that there is a role for a variety of information, as the brief leaflet reached more women and in many instances would have met their information needs, while the information kit was more appealing to women contemplating pregnancy, who are generally seeking more detail and receptive to a larger amount of information.
Rationale for and limitations of the intervention
The demands of the study design, requiring assessment of the impact of an intervention, imposed constraints on the nature of the intervention itself. In particular, preferred modalities would be those with the least likelihood of contamination of comparison locations. There was also a limited time during which the intervention could be conducted, a restriction imposed by the need to evaluate an intervention within the lifetime of the project and potentially provide information for a foreshadowed statewide folate awareness campaign. The short‐term intervention had an advantage in that contamination between sites would be reduced. Another important consideration was the potential sustainability of the intervention, i.e. any intervention to be evaluated should be able to be used on a wider scale. This restricted the use of widespread media activity, and major community development and education. Also, the fact that no population‐based health promotion campaign had been conducted in Victoria, the low level of knowledge of the role of folate in the population and the relatively high level of literacy combined to make an intervention based largely on printed matter justifiable. Within the various evaluative models for information transfer of research findings, this approach would be classed as a passive dissemination model. This study has demonstrated that such an intervention is effective in increasing awareness and knowledge of the role of periconceptional folate.
Systematic reviews of other interventions with provision of printed educational materials to health care providers have also been shown to have only small effects and to be unlikely to cause rapid change in patient outcomes. 20 Over time, however, at least with respect to information dissemination about folate, the indications are strong that levels of knowledge are improved. It also seems that, where such ongoing programmes have been in place, there are concomitant changes in behaviour, as seen both in Western Australia and in the United Kingdom where there have been large increases in sales of folic acid post‐intervention. 21 , 22
Importantly, this study has also established that a trial randomized at a community level can be successfully implemented to evaluate the dissemination of printed matter as a health promotion action. In addition, the study has had other tangible benefits in underpinning the wider campaign in Victoria to increase awareness of periconceptional folate, and in informing other related policy initiatives.
In Australia, an increasing number of foods are being fortified with folate, and in November 1998 a pilot health claim for folate and NTDs on approved foods was introduced. However, there remains a role for other actions to increase folate awareness and encourage behavioural change to reduce the risk of NTDs. This study has confirmed that, in addition to direct provision of information to consumers, medical practitioners have a key role in informing women. A comprehensive, long‐term and ongoing health promotion programme involving relevant health service providers and the food industry could best address the current low levels of folate awareness.
Acknowledgements
Major funding for this project was provided by the Department of Human Services, Victoria, Australia.
References
- 1. Riley M & Halliday J. Congenital malformations in Victoria, 1983–1994. Melbourne: Perinatal Data Collection Unit, 1996.
- 2. MRC Vitamin Study Research Group . Prevention of neural tube defects: Results of the Medical Research Council Vitamin Study Research Group. Lancet, 1991; 338 : 149 152. [PubMed] [Google Scholar]
- 3. Czeizel A & Dudas I. Prevention of first occurrence neural tube defects by periconceptional vitamin supplementation. New England Journal of Medicine, 1992; 327 : 1832 1835. [DOI] [PubMed] [Google Scholar]
- 4. Expert Advisory Group . Folic Acid and the Prevention of Neural Tube Defects. London: Department of Health, Health Publication Unit, 1992.
- 5. Australian Bureau of Statistics . National Nutrition Survey: Selected Highlights Australia 1995, Catalogue No. 4802.0. Canberra: ABS, 1997.
- 6. National Health and Medical Research Council . Folate Fortification Canberra: AGPS, 1995.
- 7. Bower C. Folate and the prevention of neural tube defects. Australian Journal of Nutrition and Dietetics, 1996; 53 (Suppl.): S5 S8. [Google Scholar]
- 8. Kitching J. Patient information leaflets – the state of the art. Journal of the Royal Society of Medicine, 1990; 83 : 298 300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. National Health and Medical Research Council . Revised statement on the relationship between dietary folic acid and neural tube defects such as spina bifida. 115th session. Canberra, 1993. [PubMed]
- 10. Shipley MJ, Smith PG, Dramaix M. Calculation of power for matched pair studies when randomization is by group. International Journal of Epidemiology, 1989; 18 : 457 461. [DOI] [PubMed] [Google Scholar]
- 11. Steel D, Vella J, Harrington P. Quality issues in telephone surveys: coverage, non‐response and quota sampling. Australian Journal of Statistics, 1996; 38 : 15 34. [Google Scholar]
- 12. McGovern E, Moss H, Grewal G, Taylor A, Bjornsson S, Pell J. Factors affecting the use of folic acid supplements in pregnant women in Glasgow. British Journal of General Practice, 1997; 47 : 635 637. [PMC free article] [PubMed] [Google Scholar]
- 13. Bower C, Blum L, O’Daly K, Higgins C, Loutsky F, Kosky C. Promotion of folate for the prevention of neural tube defects: knowledge and use of periconceptional folic acid supplements in Western Australia, 1992 to 1995. Australian and New Zealand Journal of Public Health, 1997; 21 : 16 21. [DOI] [PubMed] [Google Scholar]
- 14. De Walle H, Van Der Pal K, De Jong‐van den Berg L et al. Periconceptional folic acid in the Netherlands in 1995. Socioeconomic differences. Journal of Epidemiology and Community Health, 1998; 52 : 826 827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Neil A, Laing R, Perez P, Spencer P. The ‘Folic Acid Campaign’: has the message got through? A questionnaire study. Journal of Obstetrics and Gynaecology, 1999; 19 : 22 25. [DOI] [PubMed] [Google Scholar]
- 16. McDonnell R, Johnson Z, Doyle A, Sayers G. Determinants of folic acid knowledge and use among antenatal women. Journal of Public Health Medicine, 1999; 21 : 145 149. [DOI] [PubMed] [Google Scholar]
- 17. Sorenson G, Emmons K, Hunt M, Johnston J. Implications of the results of community intervention trials. Annual Review of Public Health, 1998; 19 : 379 416. [DOI] [PubMed] [Google Scholar]
- 18. Oakely A. Experimentation and social interventions: a forgotten but important history. BMJ, 1998; 317 : 1239 1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lumley J, Watson L, Watson M, Bower C. Periconceptional supplementation with folate and/or multivitamins for preventing neural tube defects (Cochrane Review). In: The Cochrane Library, Issue 4. Oxford: Update Software, 1998. [DOI] [PMC free article] [PubMed]
- 20. Freemantle N, Harvey E, Wolf F, Grimshaw J, Grilli R, Bero L. Printed educational materials to improve the behaviour of health care professionals and patient outcomes (Cochrane Review). In: The Cochrane Library, Issue 1. Oxford: Update Software, 1999.
- 21. Bower C, Blum L, O’Daly K, Higgins C, Loutsky F, Kosky C. Promotion of Folate for the Prevention of Neural Tube Defects: Knowledge and Use of Periconceptional Folic Acid Supplements in Western Australia 1992 to 1995. Australian and New Zealand Journal of Public Health, 1997; 21 : 716 721. [DOI] [PubMed] [Google Scholar]
- 22. Kadir R, Sabin C, Whitlow B, Brockbank E, Econmides D. Neural tube defects and periconceptional folic acid in England and Wales: retrospective study. BMJ, 1999; 319 : 92 93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Australian Bureau of Statistics . ASCO (Australian Standard Classification of Occupations), ABS Catalogue No. 1229.0 (1st edn). Canberra: ABS, 1992.


