Abstract
Purpose of review
We sought to provide a review of the recent literature regarding the prevalence and epidemiological trends in pelvic floor disorders (PFDs) including pelvic organ prolapse (POP), urinary incontinence (UI) and fecal incontinence (FI). We also examined the current trends in surgical treatment for these disorders and discuss future care needs.
Recent findings
Approximately one quarter of all women suffer from at least one or more PFDs. UI represents the most common PFD with an estimated prevalence of 15–17% while FI affects approximately 9% of adult women. POP is more difficult to assess with prevalence estimates ranging from 3–8%. Surgery for PFDs is common as 20% of women undergo stress UI or POP surgery over their lifetime. As the aging population grows, the number of women with PFDs will increase substantially and the demand for care for these disorders will continue to grow through the year 2050.
Summary
PFDs are a significant public health issue and they negatively impact the lives of millions of adult women. The projected increase in the number of women affected by PFDs over the next 40 years will create increased demand for providers properly trained in Female Pelvic Medicine and Reconstructive Surgery.
Keywords: Pelvic floor disorders, pelvic organ prolapse, urinary incontinence, epidemiological trends, future care needs
Introduction
Pelvic floor disorders (PFDs) include pelvic organ prolapse (POP), urinary incontinence (UI) and fecal incontinence (FI). PFDs are prevalent medical conditions affecting the lives of many women throughout the world. In understanding the prevalence and various risk factors associated with PFDs, providers can better identify at-risk patients and provide improved care for those women who are already affected. In this article, we aim to provide a comprehensive review of the estimated prevalence and epidemiological trends in PFDs, examine the current trends in surgical treatment for these disorders, and discuss future projections of PFDs.
Epidemiological Trends in PFD
Overall Pelvic Floor Disorders
Nygaard and colleagues demonstrated the significant public health burden of PFDs in their landmark study in 2008. Using National Health and Nutrition Examination Survey (NHANES) data from 2005 to 2006 the authors found that 23.7% of U.S. women had at least one PFD.(1*) In a subsequent study, our group utilized NHANES data from 2005 and 2010 on 7,924 non-pregnant women aged 20 years and older to assess the prevalence of PFDs. PFDs were defined as moderate to severe UI, at least monthly FI, or symptomatic POP (seeing or feeling a bulge). The proportion of women suffering from at least one or more burdensome PFDs was 25.0% (95% CI 23.6–26.3), confirming Nygaard’s previous findings.(2) In addition, there was no significant trend in PFD prevalence over the 5-year period. Recently, these rates were further confirmed in a survey of 5,236 primiparous women 20 years after a vaginal or cesarean delivery when Gyhagen and colleagues found that 31.7% had at least one symptomatic PFD and that 14.8% had two or more.(3) In examining risk factors for PFDs, older age was the most significant risk factor with over 50% of women over the age of 80 having one or more PFD.(2**) In addition to age, risk factors also included increased parity, elevated body mass index (BMI), prior hysterectomy, and presence of co-morbid diseases.(2) Gyhagen’s study found prior vaginal delivery had the strongest association with having all three symptomatic PFDs.(3)
Urinary Incontinence
UI represents the most common PFD and is comprised of stress urinary incontinence (SUI) and overactive bladder (OAB), which includes urinary urgency with or without urgency urinary incontinence (UUI), urinary frequency, and nocturia. In our NHANES study, we defined UI to include moderate to severe symptoms using the incontinence severity index, translating to at least weekly leakage or monthly leakage of volumes more than drops. We estimated that the combined prevalence of UI was 17.1% (95% CI 15.8–18.4),(2) which is similar to Nygaard et al. who estimated the prevalence of UI to be 15.7%.(1) As with other PFDs, SUI and OAB prevalence increases with age and affects up to 43.1% of women over 40 years old.(2, 4, 5) In addition to age, previous studies have found SUI and OAB are associated with higher BMI, increasing waist circumference, higher parity, prior vaginal delivery, prior hysterectomy, smoking, depression, irritable bowel syndrome, sleep apnea, and presence of neurological disorders.(2, 4, 6)
Data are mixed regarding the prevalence of UI across racial/ethnic groups. In a large ethnically-diverse, cross-sectional Internet-based study of 10,000 survey participants, Coyne et al. estimated a 30.0% prevalence of lower urinary tract symptoms (including urinary leakage, OAB symptoms and voiding symptoms) in women aged 18–70 years.(4) The increased prevalence may be due to in part to their broader definition as well as a more diverse study population. Other studies looking at UI across ethnicities have found UI is more common in non-Hispanic white women,(2, 7) SUI is highest among white women,(4, 7) and OAB/UUI is more common in African-American women.(4, 6) However, recently Maserejian and colleagues failed to find a statistical difference in UI between ethnicities when adjusting for age.(8) Regardless, providers should proactively assess for bothersome OAB and SUI in all patients, with particular diligence in older populations.
Fecal Incontinence and Dual Fecal and Urinary Incontinence
FI, defined as leakage of mucus, liquid or solid stool occurring at least monthly, is estimated to affect 8.4% of adults(9*) and 9.4% of adult women.(2) As with other PFDs, the prevalence of FI increases with age with up to 15.3% of women aged 70 and older experiencing FI monthly.(10**) Other identified risk factors for FI are obesity, bowel disturbances such as diarrhea, having multiple chronic illnesses, smoking, and anal sphincter trauma including obstetrical injury.(2, 10, 11*) In the Nurses’ Health Study of more than 64,000 women, the prevalence of dual UI and FI was 7.2%.(12*) Recently, using NHANES data from 2005 to 2010, we found a similar dual incontinence prevalence rate of 6.0% (95% CI 5.0–7.1) in women over 50.(13*) Risk factors for dual incontinence include older age, depression, co-morbidities, diarrhea, multiparity, and hysterectomy.(12,13) Notably, dual incontinence has a greater negative impact on quality of life than either condition alone and should therefore be assessed in anyone reporting UI or FI alone.(12)
Pelvic Organ Prolapse
Based on our NHANES data, POP, commonly defined as seeing or feeling a bulge, is estimated to affect 2.9% of women aged 20 and older.(1, 2) In a review article published as part of the Fifth International Collaboration on Incontinence, Barber et al. found that symptomatic POP was present in 3–6% of the population, but when based on vaginal examination was present in up to 50%.(14*) Based on the validated International Consultation on Incontinence Questionnaire for vaginal symptoms (ICIQ-VS), 8.4% of respondents reported a vaginal bulge/lump and 4.9% reported a bulge or lump outside the vagina among 1,832 women in the United Kingdom.(15) As with other PFDs, the prevalence of POP increases with age until a peak of 5.1% in women aged 60–69.(2) The declining prevalence of POP after age 69 may in part be due to surgical correction being performed at younger ages. Although only about 10–20% of symptomatic women seek medical help, both conservative and surgical interventions have been shown to improve quality of life.(16*) This again speaks to the importance of proactive screening. In addition to parity and vaginal delivery, non-obstetric risk factors for POP surgery include age, constipation, increasing weight, and chronic obstructive pulmonary disease.(17)
Trends in Surgery for PFDs
Given the high prevalence of PFDs and the fact that surgery is an effective treatment option for these conditions, surgeries for SUI and POP are quite common. Our group conducted a population-based analysis and reported that the lifetime risk of surgery for either SUI or POP is 20.0% (95% CI 19.9–20.2) by the age of 80 years(18**), which is dramatically higher than previously estimated.(19, 20) This updated analysis assessed over 10 million women followed for almost 25 million person-years in a longitudinal fashion to provide relatively precise estimates. The risk of SUI surgery was 13.6% (95% CI 13.5–13.7) and the risk for POP surgery was 12.6% (95% CI 12.4–12.7) (Figure). This analysis also reported that the highest rates of surgery occurred in women aged 70–79 years. An analysis of Medicare beneficiaries supports the fact that POP surgery is common in women aged ≥ 65 years.(21*) In other countries, POP surgery rates may differ; for example, the lifetime risk of POP surgery in Western Australia was reported at 19%,(22) and the cumulative incidence for POP surgery in the Norwegian population was estimated to be 14.6% by the age of 85 years.(17)
Figure 1. Risks of SUI and POP surgery.
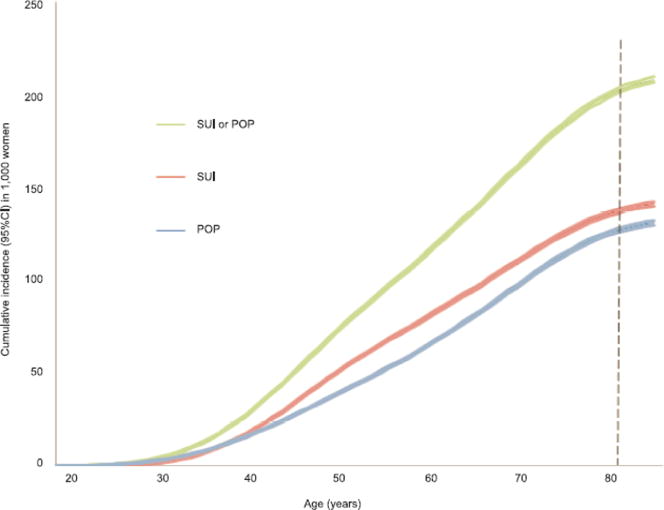
Cumulative incidence, or lifetime risk, of surgery for stress urinary incontinence (SUI), pelvic organ prolapse (POP), or SUI or POP surgery from age 18 years through age 84 years. The width of the line represents the 95% confidence interval (CI) of the cumulative incidence at each age. The cumulative incidence (95% CI) by age 80 years per 1,000 women was 200.1 (95% CI 198.7–201.5) for SUI or POP, 135.9 (95% CI 134.8–137.1) for SUI only, and 125.6 (95% CI 124.4–126.7) for POP only.
An important factor to consider when discussing trends in surgery for PFDs is the impact of the 2008 and 2011 safety notifications issued by the Food and Drug Administration (FDA) regarding vaginal mesh.(23, 24) After these FDA notices, several studies have evaluated trends in the use of mesh for POP. In an analysis of hospital discharge data of 275,000 women who underwent POP surgery from 2000 to 2010, there was an increase in the proportion of procedures which utilized mesh from 7.9% in 2000 to a peak of 32.2% in 2006, which then declined slightly to 27.5% in 2010.(25) Our group reported that the rate of mesh POP procedures increased from 2005–2010 and vaginal mesh procedure comprised 75% of mesh surgeries in a population-based study.(26) Local and/or regional trends may vary. For example, at a single academic medical center, vaginal mesh procedures decreased from 27% of all POP surgeries in early 2008 to 2% at the end of 2011,(27*) while mesh use increased in Portugal from 2000–2012.(28)
For SUI, midurethral slings have become the primary procedure performed and the gold standard SUI surgery.(29, 30) From 2000–2009, there was a dramatic decrease in SUI retropubic procedures with a corresponding increase in sling procedures in the U.S. Data from other countries, including England(31), Taiwan(32) and Korea,(33) show similar trends. Despite the fact that midurethral slings involve the use of vaginal mesh, no recent studies have assessed the impact of the FDA safety notification on the rates of SUI surgeries.
Limited recent data exist regarding trends in surgery for UUI or FI. Although sacral neuromodulation is a treatment option for UUI and FI, few longitudinal, population-based data regarding this procedure exist.(34) For FI, an analysis of inpatient hospital discharge data reported that the number of women who underwent a FI surgery, which did not include sacral neuromodulation, remained stable with 3,423 in 1998 and 3,509 in 2003.(35) Given that knowledge gaps exist regarding the trends in procedures for UUI and FI, future research should aim to address these important questions.
Future Care Needs
Over the next 40 years, the United States will experience significant growth in its aging population.(36) According to the 2012 U.S. Census Bureau projections the population aged 65 or older will nearly double by 2050 from its current 43.1 million to 83.7 million to make up 20.9% of the U.S. population. Even more dramatically, those 85 and older are projected to more than double from 5.9 million in 2012 (1.9% of the U.S. population) to 18 million in 2050 (almost 5% of the 2050 U.S. population). Of this older population, the majority will continue to be women making up 55% of those 65 and older in 2050.
In order to estimate the future prevalence of PFDs in the U.S. population, our group used U.S. Census and NHANES data. We estimated that the number of women with PFDs will increase substantially by 2050 with an expected 43.8 million women having at least one PFD by 2050.(37**) We then estimated the annual procedure rates for SUI or POP surgery using the 2008 U.S. Census projections, inpatient data obtained from the 2007 Nationwide Inpatient Sample (the largest publicly available database of hospital discharges in the U.S.) and outpatient data from the 2006 National Survey of Ambulatory Surgery (a database of surgical outpatient procedures in hospital-based or freestanding clinics but not physician office-based procedures).(38) According to our estimates, surgical rates for SUI or POP will increase 42.7% by 2050. Annual procedure rates will increase from 210,700 to 310,050 for SUI and from 166,000 to 245,970 for POP. These data indicate surgical rates will increase starting from the age of 20 onward until 80 when rates will then decrease.(38) Recently, Kirby and colleagues examined Kaiser Permanent San Diego data and found their Urogynecology clinic had experienced a 116% increase in new patients annually compared to 2000.(39) Using past clinic data, the authors estimated the demand for care for PFDs would increase by 35% from 2010 to 2030.(39**) Taken together both studies indicate that a significant increase in both the number of women with PFDs and those seeking care for PFDs will occur over the next 20 to 40 years.
Recognizing this increasing burden of PFDs, research has begun to assess the capability of the provider workforce trained to treat these conditions. Yune and colleagues surveyed general gynecologists regarding comfort in managing various urogynecologic conditions and found that although most respondents felt comfortable managing SUI and POP, younger gynecologists offered less treatment options.(40) Similarly, Casiano and colleagues found that younger gynecologists performed mostly midurethral slings, anterior and/or posterior repairs and cystoscopies with few performing more complex urogynecologic procedures.(41) Thus, the burden for providing comprehensive treatment for PFDs will increasingly fall on sub-specialty trained providers. In order to deliver comprehensive pelvic care, Kirby and colleagues estimate that 1 PFD physician specialist, 0.5 nurse practitioner, 0.5 registered nurse continence specialist and 0.75 pelvic floor physical therapist were needed for every 100,000 women, with higher specialist provider demand if fewer midlevel providers are available.(39)
Conclusions
Pelvic floor disorders are a significant public health issue affecting the lives of millions of adult women. Providers should assess for PFDs regularly, especially in patients with one existing PFD and in older populations. Surgery can offer effective treatment for PFDs, and many patients with symptomatic PFDs elect to undergo surgery. As the U.S. population ages over the next 40 years, the burden of PFDs will become greater and the number of surgeries performed for PFDs per year will increase. This increased demand for PFD treatment and care in the future will lead to a greater need for providers properly trained in Female Pelvic Medicine and Reconstructive Surgery, the newest board-certified subspecialty within the field of Obstetrics and Gynecology.
Key Points.
PFDs are common and affect an estimated 25% of all women in the United States
Approximately 20% of women will undergo surgery for stress urinary incontinence and pelvic organ prolapse at some point in their lives.
Over the next 40 years as the aging population grows the number of women affected by PFDs will significantly increase resulting in increased demand for properly trained providers to give proper treatments and care for these burdensome disorders.
Acknowledgments
None
Financial support or sponsorship
Dieter AA has received funding from the NIH NIDDK Loan Repayment Program for clinical researchers. Wu JM is supported by K23HD068404, Eunice Kennedy Shriver National Institute of Child Health & Human Development. For the remaining author, none were declared.
Footnotes
Conflicts of interest
None
References
- 1*.Nygaard I, Barber MD, Burgio KL, et al. Prevalence of symptomatic pelvic floor disorders in US women. Jama. 2008;300(11):1311–6. doi: 10.1001/jama.300.11.1311. Epub 2008/09/19. • This is a landmark study reporting national prevalence of PFDs in the United States. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2**.Wu JM, Vaughan CP, Goode PS, et al. Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstetrics and gynecology. 2014;123(1):141–8. doi: 10.1097/AOG.0000000000000057. Epub 2014/01/28. • This study used NHANES data to estimate prevalence and trends of PFDs from 2005 to 2010. Although there was no statistical trend, the significance of PFDs as a public health issue was further demonstrated, with one in four women reporting at least one disorder. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gyhagen M, Akervall S, Milsom I. Clustering of pelvic floor disorders 20 years after one vaginal or one cesarean birth. International urogynecology journal. 2015 doi: 10.1007/s00192-015-2663-3. Epub 2015/02/25. [DOI] [PubMed] [Google Scholar]
- 4.Coyne KS, Sexton CC, Bell JA, et al. The prevalence of lower urinary tract symptoms (LUTS) and overactive bladder (OAB) by racial/ethnic group and age: results from OAB-POLL. Neurourology and urodynamics. 2013;32(3):230–7. doi: 10.1002/nau.22295. Epub 2012/08/01. [DOI] [PubMed] [Google Scholar]
- 5.Coyne KS, Sexton CC, Vats V, et al. National community prevalence of overactive bladder in the United States stratified by sex and age. Urology. 2011;77(5):1081–7. doi: 10.1016/j.urology.2010.08.039. Epub 2011/01/25. [DOI] [PubMed] [Google Scholar]
- 6.Coyne KS, Margolis MK, Kopp ZS, Kaplan SA. Racial differences in the prevalence of overactive bladder in the United States from the epidemiology of LUTS (EpiLUTS) study. Urology. 2012;79(1):95–101. doi: 10.1016/j.urology.2011.09.010. Epub 2011/11/08. [DOI] [PubMed] [Google Scholar]
- 7.Mitchell ES, Woods NF. Correlates of urinary incontinence during the menopausal transition and early postmenopause: observations from the Seattle Midlife Women’s Health Study. Climacteric: the journal of the International Menopause Society. 2013;16(6):653–62. doi: 10.3109/13697137.2013.777038. Epub 2013/04/09. [DOI] [PubMed] [Google Scholar]
- 8.Maserejian NN, Minassian VA, Chen S, et al. Treatment status and risk factors for incidence and persistence of urinary incontinence in women. International urogynecology journal. 2014;25(6):775–82. doi: 10.1007/s00192-013-2288-3. Epub 2014/01/31. [DOI] [PubMed] [Google Scholar]
- 9*.Ditah I, Devaki P, Luma HN, et al. Prevalence, trends, and risk factors for fecal incontinence in United States adults, 2005–2010. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association. 2014;12(4):636–43. e1–2. doi: 10.1016/j.cgh.2013.07.020. Epub 2013/08/03. • Using NHANES data from 2005 to 2010, this study estimated the prevalence, trends, and risk factors for fecal incontinence in 14,579 non-institutionalized men and women. [DOI] [PubMed] [Google Scholar]
- 10**.Whitehead WE, Borrud L, Goode PS, et al. Fecal incontinence in US adults: epidemiology and risk factors. Gastroenterology. 2009;137(2):512–7. 7, e1–2. doi: 10.1053/j.gastro.2009.04.054. Epub 2009/05/05. • This is the first study to report national prevalence of FI in the United States. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11*.Bharucha AE, Dunivan G, Goode PS, et al. Epidemiology, pathophysiology, and classification of fecal incontinence: state of the science summary for the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) workshop. The American journal of gastroenterology. 2015;110(1):127–36. doi: 10.1038/ajg.2014.396. Epub 2014/12/24. • In addition to prevalence and epidemiology, this publication from the NIDDK workshop also addressed the pathophysiology of FI, management and associated financial burden, and impact on quality of life for patients and caregivers. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12*.Matthews CA, Whitehead WE, Townsend MK, Grodstein F. Risk factors for urinary, fecal, or dual incontinence in the Nurses’ Health Study. Obstetrics and gynecology. 2013;122(3):539–45. doi: 10.1097/AOG.0b013e31829efbff. Epub 2013/08/08. • This was the first study to estimate the prevalence of and risk factors for dual incontinence in a large sample size, using survey data from 64,396 women in the Nurses’ Health Study. This allowed investigators to examine unique risk factors for dual incontinence compared with fecal and urinary incontinence alone. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13*.Wu JM, Matthews CA, Vaughan CP, Markland AD. Urinary, fecal, and dual incontinence in older u.s. Adults. J Am Geriatr Soc. 2015;63(5):947–53. doi: 10.1111/jgs.13385. • This study used NHANES data from 2005 to 2010 to investigate the prevalence of dual incontinence and risk factors for dual incontinence in a large population-based analysis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14*.Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. International urogynecology journal. 2013;24(11):1783–90. doi: 10.1007/s00192-013-2169-9. • As a part of the Fifth International Collaboration on Incontinence, using a review of literature from the prior 4 years, this publication compiled data on the incidence and prevalence of symptomatic POP and surgery, as well as suggested standardized guidelines for reporting surgical outcomes. [DOI] [PubMed] [Google Scholar]
- 15.Cooper J, Annappa M, Dracocardos D, et al. Prevalence of genital prolapse symptoms in primary care: a cross-sectional survey. International urogynecology journal. 2015;26(4):505–10. doi: 10.1007/s00192-014-2556-x. [DOI] [PubMed] [Google Scholar]
- 16*.Doaee M, Moradi-Lakeh M, Nourmohammadi A, et al. Management of pelvic organ prolapse and quality of life: a systematic review and meta-analysis. International urogynecology journal. 2014;25(2):153–63. doi: 10.1007/s00192-013-2141-8. • In a systematic review and meta-analysis, thirty-two RCTs were evaluated to determine the effects of treatment of POP on patients’ quality of life. [DOI] [PubMed] [Google Scholar]
- 17.Lonnee-Hoffmann RA, Salvesen O, Morkved S, Schei B. Self-reported pelvic organ prolapse surgery, prevalence, and nonobstetric risk factors: findings from the Nord Trondelag Health Study. International urogynecology journal. 2015;26(3):407–14. doi: 10.1007/s00192-014-2509-4. [DOI] [PubMed] [Google Scholar]
- 18**.Wu JM, Matthews CA, Conover MM, et al. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201–6. doi: 10.1097/AOG.0000000000000286. • This analysis assessed over 10 million women followed for almost 25 million person-years in a longitudinal fashion to provide relatively current estimates of the lifetime risk of undergoing surgery for either stress incontinence and/or pelvic organ prolapse by the age of 80 years. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Olsen AL, Smith VJ, Bergstrom JO, et al. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89(4):501–6. doi: 10.1016/S0029-7844(97)00058-6. [DOI] [PubMed] [Google Scholar]
- 20.Fialkow MF, Newton KM, Lentz GM, Weiss NS. Lifetime risk of surgical management for pelvic organ prolapse or urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(3):437–40. doi: 10.1007/s00192-007-0459-9. [DOI] [PubMed] [Google Scholar]
- 21*.Khan AA, Eilber KS, Clemens JQ, et al. Trends in management of pelvic organ prolapse among female Medicare beneficiaries. Am J Obstet Gynecol. 2014 doi: 10.1016/j.ajog.2014.10.025. • This study evaluated Medicare beneficiaries from 1999 to 2009 and noted that 14–15% of women with a POP diagnosis underwent surgical repair. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith FJ, Holman CD, Moorin RE, Tsokos N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010;116(5):1096–100. doi: 10.1097/AOG.0b013e3181f73729. [DOI] [PubMed] [Google Scholar]
- 23.FDA Public Health Notification: Serious Complications Associated with Transvaginal Placement of Surgical Mesh in Repair of Pelvic Organ Prolapse. 2008 Oct 20; doi: 10.1016/j.eururo.2009.01.055. Issued. (Accessed on March 19, 2015 at http://www.fda.gov/medicaldevices/safety/alertsandnotices/publichealthnotifications/ucm061976.htm) [DOI] [PubMed]
- 24.FDA Safety Communication: Update on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse. 2011 Jul 13; doi: 10.1007/s00192-011-1581-2. Issued on. Available at: http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm262435.htm Retrieved on March 19, 2015. [DOI] [PubMed]
- 25.Rogo-Gupta L, Rodriguez LV, Litwin MS, et al. Trends in surgical mesh use for pelvic organ prolapse from 2000 to 2010. Obstet Gynecol. 2012;120(5):1105–15. doi: 10.1097/aog.0b013e31826ebcc2. [DOI] [PubMed] [Google Scholar]
- 26.Jonsson Funk M, Edenfield AL, Pate V, et al. Trends in use of surgical mesh for pelvic organ prolapse. American journal of obstetrics and gynecology. 2013;208(1):79, e1–7. doi: 10.1016/j.ajog.2012.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27*.Skoczylas LC, Turner LC, Wang L, et al. Changes in prolapse surgery trends relative to FDA notifications regarding vaginal mesh. Int Urogynecol J. 2014;25(4):471–7. doi: 10.1007/s00192-013-2231-7. • When evaluting trends in POP surgery at a single academic medical center, the authors found that among 1,211 women who underwent 1,385 POP procedures, there was a decrease in vaginal mesh procedures from 27% in early 2008 to 2% at the end of 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mascarenhas T, Mascarenhas-Saraiva M, Jr, Ricon-Ferraz A, et al. Pelvic organ prolapse surgical management in Portugal and FDA safety communication have an impact on vaginal mesh. Int Urogynecol J. 2015;26(1):113–22. doi: 10.1007/s00192-014-2480-0. [DOI] [PubMed] [Google Scholar]
- 29.Jonsson Funk M, Levin PJ, Wu JM. Trends in the surgical management of stress urinary incontinence. Obstetrics and gynecology. 2012;119(4):845–51. doi: 10.1097/AOG.0b013e31824b2e3e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Geller EJ, Wu JM. Changing trends in surgery for stress urinary incontinence. Curr Opin Obstet Gynecol. 2013;25(5):404–9. doi: 10.1097/GCO.0b013e3283648cdd. [DOI] [PubMed] [Google Scholar]
- 31.Withington J, Hirji S, Sahai A. The changing face of urinary continence surgery in England: a perspective from the Hospital Episode Statistics database. BJU Int. 2014;114(2):268–77. doi: 10.1111/bju.12650. [DOI] [PubMed] [Google Scholar]
- 32.Wu CJ, Tong YC, Hsiao SM, et al. The surgical trends and time-frame comparison of primary surgery for stress urinary incontinence, 2006–2010 vs 1997–2005: a population-based nation-wide follow-up descriptive study. Int Urogynecol J. 2014;25(12):1683–91. doi: 10.1007/s00192-014-2443-5. [DOI] [PubMed] [Google Scholar]
- 33.Cho SY, Jeong SJ, Yeo JK, et al. Nationwide database of surgical treatment pattern for patients with stress urinary incontinence in Korea. International neurourology journal. 2014;18(2):91–4. doi: 10.5213/inj.2014.18.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cameron AP, Anger JT, Madison R, et al. National trends in the usage and success of sacral nerve test stimulation. J Urol. 2011;185(3):970–5. doi: 10.1016/j.juro.2010.10.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sung VW, Rogers ML, Myers DL, et al. National trends and costs of surgical treatment for female fecal incontinence. Am J Obstet Gynecol. 2007;197(6):652, e1–5. doi: 10.1016/j.ajog.2007.08.058. [DOI] [PubMed] [Google Scholar]
- 36.Ortman JM, Velkoff VA, Hogan H. An Aging Nation: The Older Population in the United States. U.S Department of Commerce Economics and Statistics Administration; 2014. Apr 1, www.census.gov/prod/2014pubs/p25-1140.pdf. 2015 Report No. [Google Scholar]
- 37**.Wu JM, Hundley AF, Fulton RG, Myers ER. Forecasting the prevalence of pelvic floor disorders in U.S. Women: 2010 to 2050. Obstetrics and gynecology. 2009;114(6):1278–83. doi: 10.1097/AOG.0b013e3181c2ce96. • This study predicts the prevalence of PFDs through the year 2050 in the United States using U.S. Census projections and NHANES data. [DOI] [PubMed] [Google Scholar]
- 38.Wu JM, Kawasaki A, Hundley AF, et al. Predicting the number of women who will undergo incontinence and prolapse surgery, 2010 to 2050. American journal of obstetrics and gynecology. 2011;205(3):230, e1–5. doi: 10.1016/j.ajog.2011.03.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39**.Kirby AC, Luber KM, Menefee SA. An update on the current and future demand for care of pelvic floor disorders in the United States. American journal of obstetrics and gynecology. 2013;209(6):584, e1–5. doi: 10.1016/j.ajog.2013.09.011. • This study uses Kaiser Permanente data to estimate the future care needs of patients seeking care for PFDs. [DOI] [PubMed] [Google Scholar]
- 40.Yune JJ, Siddighi S. Perceptions and practice patterns of general gynecologists regarding urogynecology and pelvic reconstructive surgery. Female pelvic medicine & reconstructive surgery. 2013;19(4):225–9. doi: 10.1097/SPV.0b013e3182995107. [DOI] [PubMed] [Google Scholar]
- 41.Casiano ER, Wendel GD, Jr, Congleton MJ, Wai CY. Urogynecology training and practice patterns after residency. Journal of surgical education. 2012;69(1):77–83. doi: 10.1016/j.jsurg.2011.06.007. [DOI] [PubMed] [Google Scholar]


