Abstract
Background
Bladder disorders associated with interstitial cystitis are frequently characterized by increased contractility and pain. The purposes of this study were to examine (1) the effects of blocking mammalian target of rapamycin (mTOR) on the exaggerated bladder activity and pain evoked by cystitis and (2) the underlying mechanisms responsible for the role of mTOR in regulating cystic sensory activity.
Results
The expression of p-mTOR, mTOR-mediated phosphorylation of p70 ribosomal S6 protein kinase 1 (p-S6K1), 4 E–binding protein 4 (p-4 E-BP1), as well as phosphatidylinositide 3-kinase (p-PI3K) pathway were amplified in cyclophosphamide rats as compared with control rats. Blocking mTOR by intrathecal infusion of rapamycin attenuated bladder hyperactivity and pain. In addition, blocking PI3K signal pathway attenuated activities of mTOR, which was accompanied with decreasing bladder hyperactivity and pain. Inhibition of either mTOR or PI3K blunted the enhanced spinal substance P and calcitonin gene-related peptide in cyclophosphamide rats.
Conclusions
The data for the first time revealed specific signaling pathways leading to cyclophosphamide-induced bladder hyperactivity and pain, including the activation of mTOR and PI3K. Inhibition of these pathways alleviates cystic pain. Targeting one or more of these signaling molecules may present new opportunities for treatment and management of overactive bladder and pain often observed in cystitis.
Keywords: Cystic pain, mTOR, cystitis, bladder activity, rapamycin
Background
Interstitial cystitis, also known as bladder pain syndrome (IC/BPS) is a chronic pathological condition of the bladder characterized by symptoms such as pelvic pain and urgency or frequency in urination.1 IC/BPS impacts normal physical and mental health and presents a remarkable negative effect on the quality of life of patients.1 Patients with IC/BPS constantly feel painful at normal bladder pressure, suggesting amplified excitability of their micturition reflex pathway.2 This is likely due to impairments of the sensory inputs originated from the bladder to the spinal cord and central nervous system. Nonetheless, treatment options for cystic pain have been limited, partly due to our poor understanding of the underlying mechanisms responsible for pain.
Mammalian target of rapamycin (mTOR) is a serine threonine protein kinase. There are two distinct mTOR forms of protein complexes, mTOR complex 1 (mTORC1) and mTORC2. In general, mTORC1 is composed of raptor, mLST8, and mTOR and is known to gate translation of most proteins by phosphorylation of specific downstream effectors including p70 ribosomal S6 protein kinase (p70 S6Ks) and 4 E-BPs.3 mTOR, S6K1, and 4 E-BP1 are expressed in the mammalian nervous system, particularly in the spinal cord dorsal horn.4,5
Activation of mTOR, in particular, mTORC1 that is more sensitive to rapamycin, leads to promotion of the phosphorylation of downstream effectors, such as p70 S6K1, and this further governs mRNA translation.3 The mTORC1 is well known for its critical roles in the regulation of protein synthesis and growth, and further, the compelling evidence supports the notion that mTOR plays an important role in the modulation of long-term neuronal plasticity.5,6 Specifically, mTOR and its downstream effectors have been identified in the spinal cord dorsal horn and contribute to transmission and modulation of pain.7 For example, intrathecal administration of rapamycin, a specific inhibitor of mTOR, produces anti-nociception in models of inflammation.7–9 Local perfusion of rapamycin into the spinal cord significantly attenuates formalin-induced neuronal hyperexcitability in the dorsal horn.10 Note that rapamycin can attenuate pain response and this is accompanied with downregulated mTOR, S6K1, and 4 E-BP1 by rapamycin.11 These findings indicate that mTOR and its downstream signals are activated under persistent pain conditions and contribute to the development of spinal pain sensitization.
The superficial dorsal horn is the first synaptic site from peripheral afferent nerves to the central nervous system12,13 and plays an important role in modulating pain.14,15 Specifically, the dorsal horn at the lumbar levels (i.e., L5 to L6) is the first synaptic site receiving (sharing) pain inputs from both visceral organs (i.e., bladder) and the hind paw. Thus, in this study, we determined the role played by mTOR at this level of lumbar superficial dorsal horn in regulating bladder hypersensitivity and mechanical hyperalgesia in rats following cystitis with systemic administration of cyclophosphamide (CYP). In a cystitis model of CYP, rats’ bladder appears to be hyperactive with an elevated voiding pressure and thereby leads to mechanical pain.16,17 In general, mechanical paw withdrawal threshold (PWT) of rat hind paw in response to the stimulation of von Frey filaments was employed to assess mechanical pain under pathophysiological conditions.4,18
On the basis of these previous findings, we suspected that mTOR in the superficial dorsal horn of the lumbar spinal cord is likely changed in CYP-rats. We also suspected that mTOR is likely an important player for the induction and maintenance of cystic pain. We hypothesized that CYP upregulates the protein expression of mTOR signal pathways in the superficial dorsal horn, resulting in bladder hyperactivity and pain. Moreover, blocking spinal mTOR by intrathecal injection of rapamycin would attenuate the amplified bladder activity and pain response evoked by CYP. We also hypothesized that CYP upregulates expression of phosphatidylinositide 3-kinase (PI3K), an upstream signal of mTOR.3 We speculated that blocking spinal PI3K would attenuate activities of mTOR pathway thereby leading to a reduction in bladder hyperactivity and pain.
Moreover, the releases of neurotransmitters such as substance P and calcitonin gene-related peptide (CGRP)19–21 within the dorsal horn play an important role in regulating pain responses.15 The levels of numerous neurotransmitters and related receptors in the dorsal horn have been targets to understanding of the underlying mechanisms responsible for pain.14,15 Accordingly, we further hypothesized that blocking mTOR and PI3K pathways attenuates the amplified levels of substance P and CGRP in the superficial dorsal horn of CYP rats.
Methods
Animal
Adult female Wistar rats (250–300 g) were housed in standard care facilities with water and food ad libitum on a 12 h light–dark cycle. All experimental procedures and protocols were reviewed and approved by the Animal Care and Use Committee of Chongqing Medical University and were carried out in accordance with the guidelines of the International Association for the Study of Pain.
Induction of cystitis
Rats were intraperitoneally (i.p.) injected with CYP (75 mg/kg, in the concentration of 75 mM, Sigma-Aldrich) every three days to induce chronic cystitis.16,17 On the eighth day, experiments were performed. Control rats received saline injections.
Bladder catheterization
Rats were treated perioperatively for 96 h with trimethoprim-sulfmethoxazole (150 mg/250 mL) in their drinking water. On day of catheter implantation, rats were anesthetized by sodium pentobarbital (60 mg/kg, i.p.) and 15 µg of buprenorphine in 1 mL of normal saline was given subcutaneously for postoperative analgesia. The dorsal neck and lower abdomen were clipped, prepped with 1% povidone iodine, and sterilely draped. A 4-cm incision was made in the lower abdomen to expose the bladder and a small incision was made in the dome. A 25-cm polyethylene-50 catheter with a cuff was inserted into the bladder and secured with a 6-0 silk purse-string suture. The catheter was tunneled subcutaneously to the dorsal neck, anchored, and the free end was stoppered with a blunted 22 gauge needle. The abdominal wound was closed with 4-0 silk suture and the skin was closed with three 4-0 silk interrupted sutures. The catheter was covered with a dressing and secured to the rat’s back.
Intrathecal catheter for administration of drugs
After completion of bladder catheter implantation, one end of polyethylene-10 tubing was inserted intrathecally through an incision in the cisternal membrane and advanced 7–9 cm caudal until the tip of the catheter was positioned at the lumbar spinal level (L5 to L6). The other end of the intrathecal tubing was sutured to the musculature and skin at the incision site and externalized to the back of the rat. Animals were allowed to recover and then returned to the animal care facility where they were housed individually. Five days were allowed before the experiments were performed.
Mechanical sensitivity and cystometry
In this study, all experiments were performed in a double-blinded manner. On the day of experimentation, individual rats were placed in a Plexiglas chamber (25 × 8 × 9 cm) with a wire mesh floor. The bladder catheter was connected to a three-way stopcock connected to an infusion pump and pressure transducer. Rats were allowed to acclimate to the chamber for 30–40 min. First, saline was infused into the bladder at 10 mL/h for 1 h and mechanical sensitivity was examined and urodynamic measurement was performed to collect baseline data.
To quantify the mechanical sensitivity of the hindpaw, rats were placed in individual plastic boxes and allowed to acclimate for > 30 min. Mechanical PWT of rat hind paw in response to the stimulation of von Frey filaments was determined. A series of calibrated von Frey filaments (ranging from 0.5 to 18.0 g) were applied perpendicularly to the plantar surface of the hind paw with a sufficient force to bend the filaments for 60 s or until paw withdrew. In the presence of a response, the filament of next lower force was applied. In the absence of a response, the filament of next greater force was applied. To avoid injury during tests, the cutoff strength of the von Frey filament was 18 g. The tactile stimulus producing a 50% likelihood of withdrawal was determined using the “up-down” method.18 Each trial was repeated two times at approximately 2 min intervals. The mean value was used as the force producing a withdrawal response.4
Following collection of baseline data, a Hamilton microsyringe (250 µL) was connected to the intrathecal tubing to deliver 100 μl of dimethyl sulfoxide as vehicle control, antagonists to mTOR (rapamycin, 109 µM (10 µg), obtained from Selleck Chem) and inhibitor of PI3K (LY294002, 10 µM, obtained from Sigma-Aldrich). The volume of infused rapamycin and LY294002 was 100 μl. An infusion pump was used to deliver those vehicle and drugs and the pump was set to constantly over a period of 30 min. Note that a prior study11 used the same approach to intrathecally infuse rapamycin (1, 5, and 10 µg) and LY294002 (1, 5, and 10 µM). It was shown that 10 µg of rapamycin and 10 µM of LY294002 were effective to attenuate mechanical and thermal hyperalgesia. We selected accordingly those doses in our current study.
Ten minutes after intrathecal infusion, mechanical sensitivity of the hindpaws was again determined. Post-treatment cystometry was also performed after completion of mechanical sensitivity examination. Thus, six groups were included in this study: saline rats + vehicle infusion (n = 8); CYP-rats + vehicle infusion (n = 12); saline rats + rapamycin (n = 6); CYP-rats + rapamycin (n = 12); saline rats + LY294002 (n = 6); and CYP-rats + LY294002 (n = 10).
In a subset of experiments, in order to examine the effects of blocking mTOR and PI3K on the levels of substance P and CGRP vehicle (n = 12), rapamycin (10 µg, n = 10) and LY294002 (10 µM, n = 10) were intrathecally given using an infusion pump in CYP-rats, respectively. The pump was set to constantly deliver vehicle or the drugs over a period of 30 min. At the end of infusion, rats were euthanized by sodium pentobarbital (120 mg/kg, i.p.) and the superficial dorsal horn tissues (L4–L6) were obtained under an anatomical microscope for Western blot and ELISA experiments.
Western blot analysis
Total protein of the superficial dorsal horn tissues was extracted by homogenizing dorsal horn sample in ice-cold immunoprecipitation assay buffer. The lysates were centrifuged and the supernatants were collected for measurements of protein concentrations. After being denatured by heating at 95℃ for 5 min in buffer, the supernatant samples containing 20 µg of protein were loaded onto 4–20% Mini-PROTEAN TGX gels and electrically transferred to a polyvinylidene fluoride membrane. The membrane was blocked in 5% nonfat milk in 0.1% Tween-tris-buffered saline buffer and was incubated overnight with respective primary antibody. The primary antibodies include: rabbit anti-p-mTOR/p-S6K1/p-4 E-BP1 antibodies (1:200); rabbit anti-mTOR/S6K1/4 E-BP1 antibodies (1:200–1:500); rabbit anti-p-PI3K p85; and anti-PI3K p85 antibodies (1:250). Next, the membranes were washed and incubated with an alkaline phosphatase conjugated anti-rabbit secondary antibody (1:1000). All these primary antibodies were purchased from the Abcam Co. and/or Cayman Chemical Co; and goat anti-rabbit secondary antibody was purchased from Santa Cruz Biotechnology. The immunoreactive proteins were detected by enhanced chemiluminescence. The bands recognized by the primary antibody were visualized by exposure of the membrane onto an X-ray film. The membrane was stripped and incubated with mouse anti-β-actin to show equal loading of the protein. Then, the film was scanned and the optical density of all protein bands was first analyzed using the Scion Image software, and values for densities of immunoreactive bands/β-actin band densities from the same lane were determined. Each of the values was then normalized to a control sample.
ELISA measurements
To examine the levels of substance P and CGRP in the superficial dorsal horn of the spinal cord, ELISA methods were employed. Substance P was measured using substance P ELISA kit following the manufacturer’s instructions (Abcam Co., Cambridge, MA). Briefly, the diluted tissue supernatant (100 μl) was placed in a 96-well goat anti-mouse IgG-coated plate and incubated for 2 h. After incubation, the plate was washed using the provided washing buffer, and the color was developed by adding para-nitrophenylphosphate (200 μl) substrate after 45 min and determined by an ELISA plate reader. Wavelength of the ELISA plate reader was set at 450 nm. The amount of substance P was calculated by using a substance P standard curve. In the similar way, the CGRP content of the samples (100 μl supernatant) was determined using a commercial CGRP ELISA kit (Cayman Chemical Co.). Briefly, the diluted samples were placed in a 96-well plate incubated with precoated anti-rat IgG antibody overnight, washed and developed, and quantified.22
Statistical analysis
Data for mechanical threshold, voiding pressure, and intercontraction interval were analyzed using a two-way repeated-measure ANOVA since multiple interventions were compared among groups. Data for Western blot analysis were analyzed using two sample t-test. Data for ELISA measurement of substance P and CGRP were analyzed using one-way ANOVA. Values were presented as means ± SEM. For all analyses, differences were considered significant at P < 0.05. All statistical analyses were performed by using SPSS 13.0 (SPSS, Chicago, USA).
Results
Effects of blocking mTOR and PI3K on mechanical hypersensitivity and bladder activity
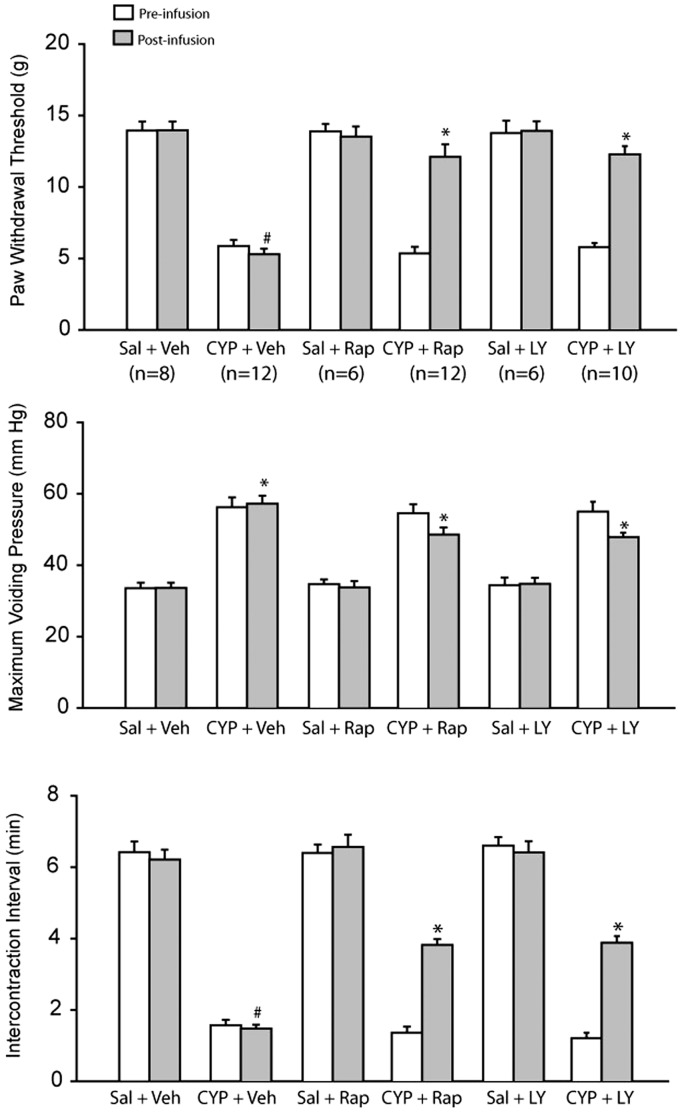
After we obtained all the data of mechanical sensitivity and cystometry, control vehicle, rapamycin (mTOR inhibitor), and LY294002 (PI3K inhibitor) were intrathecally infused. Figure 1 (top panel) showed that CYP decreased PWT in rats with vehicle infusion (5.41 ± 0.35 g, P < 0.05 vs. saline control; n = 12) compared with saline control rats (13.66 ± 0.72 g, n = 8). As rapamycin (n = 12) and LY294002 (n = 10) were infused, a decrease in PWT evoked by CYP was blunted. PWT was 11.98 ± 0.93 g after rapamycin (P < 0.05 vs. CYP-rats with vehicle infusion) and 12.27 ± 0.68 g after LY294002 (P < 0.05 vs. CYP-rats with vehicle infusion), respectively. Note that there was no changes of PWT observed in saline control rats after infusion either rapamycin or LY294002 (n = 6 in each group), suggesting that blocking mTOR and PI3K had no significant effects on mechanical sensitivity in rats under normal bladder conditions.
Figure 1.
Effects of blocking mTOR and PI3K pathways on CYP-evoked bladder mechanical hypersensitivity and intercontraction interval. Top panel: CYP decreased PWT and intrathecal administration of rapamycin and LY294002 blunted the effects of CYP. *P < 0.05 versus pre-infusion and #P < 0.05 versus post-infusion of all other groups. Number of animals is shown in the figure and they were the same in other panels. Middle and bottom panels: CYP amplified maximum voiding pressure and decreased intercontraction interval. Rapamycin and LY294002 largely recovered the shortened intercontraction interval induced by CYP without significantly altering maximum voiding pressure. In middle panel, *P < 0.05 versus respective saline control rats with post-infusion. In bottom panel, *P < 0.05 versus pre-infusion; and #P < 0.05 versus post-infusion of all other groups. Sal: saline; Veh: vehicle; CYP: cyclophosphamide; Rap: rapamycin; and LY: LY294002. Data were analyzed using a two-way repeated-measure ANOVA.
Figure 1 (middle and bottom panels) further showed that CYP increased maximum voiding pressure and decreased intercontraction interval. As rapamycin and LY294002 were intrathecally infused, the shortened intercontraction interval evoked by CYP was largely recovered without significantly altering maximum voiding pressure.
mTOR signal pathways engaged in CYP-induced mechanical hypersensitivity
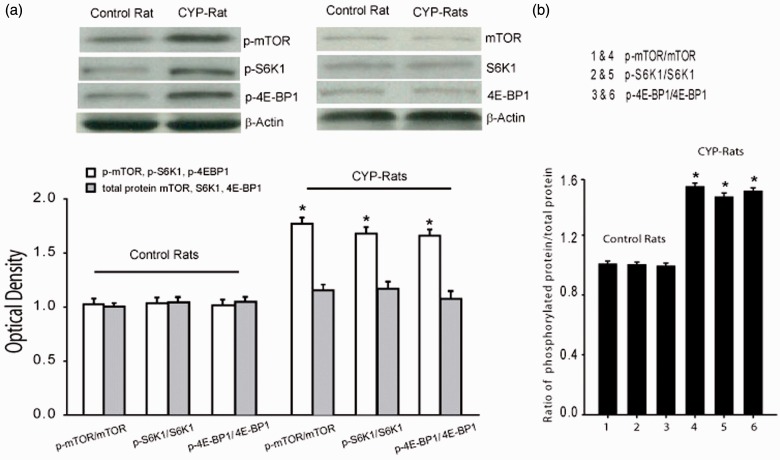
Figure 2(a) showed the protein expression of p-mTOR, p-S6K1, and p-4E-BP1 as well as mTOR, S6K1, and 4E-BP1 in saline control rats and CYP-rats. CYP significantly increased the protein levels of p-mTOR- and mTOR-mediated p-S6K1 and p-4E-BP1 in the superficial dorsal horn as compared with control rats. Optical density for p-mTOR, p-S6K1, and p-4E-BP1was 0.99 ± 0.12, 1.03 ± 0.22, and 1.04 ± 0.21 in control rats and 1.76 ± 0.33, 1.66 ± 0.31, and 1.64 ± 0.30 in CYP-rats (P < 0.05 vs. control rats, n = 6–10 in each group). Note that total protein of mTOR, S6K1, and 4E-BP1 levels was not significantly increased in CYP-rats. Furthermore, Figure 2(b) demonstrated that the ratio of p-mTOR, p-S6K1, and p-4E-BP1 levels versus total protein of mTOR, S6K1, and 4E-BP1 levels was significantly increased in CYP-rats.
Figure 2.
Expression of mTOR pathways in control rats and CYP-rats. (a) Top panel: typical bands and bottom panel: averaged data, showing that p-mTOR, p-S6K1, and p-4E-BP1 in the dorsal horn of the spinal cord were upregulated in CYP-rats. *P < 0.05 versus control rats (n = 6–10 in each group). There were insignificant differences in total protein expression of mTOR, S6K1, and 4E-BP1 in control rats and CYP-rats (P > 0.05. n = 6–10 in each group). (b) The ratio of p-mTOR, p-S6K1, and p-4E-BP1 levels versus total protein of mTOR, S6K1, and 4E-BP1 levels was significantly increased in CYP-rats. *P < 0.05 versus control rats (n = 6–10 in each group). In this study, data were analyzed using two sample t-test.
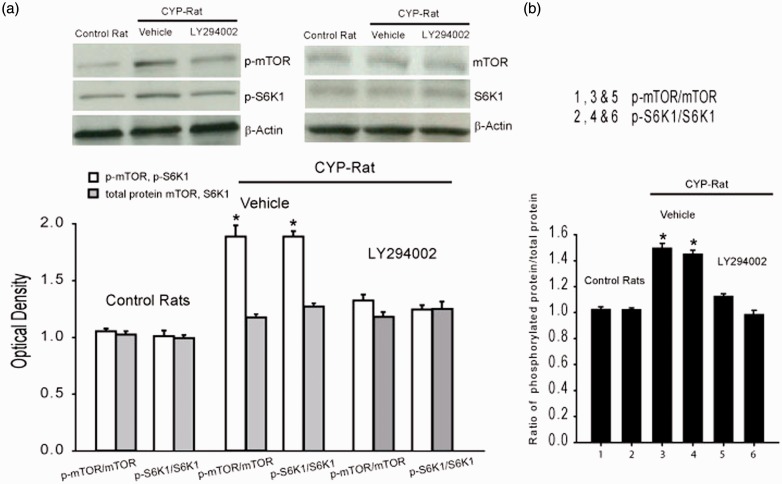
We also examined the effects of blocking PI3K on expression of p-mTOR and p-S6K1. Figure 3(a) demonstrated that the protein expression of p-mTOR and p-S6K1 was significantly increased in CYP-rats (n = 6–10) as compared with saline control rats (n = 6–8). When LY294002 was infused into the spinal cord of CYP-rat, the amplified activities of p-mTOR and p-S6K1 evoked by CYP were significantly attenuated (n = 6–10 in each group). Nonetheless, total protein of mTOR and S6K1 levels was not significantly altered by LY294002 in CYP-rats. Figure 3(b) demonstrated that the ratio of p-mTOR and p-S6K1 levels versus total protein of mTOR and S6K1 levels was significantly increased in CYP-rats and this was inhibited after infusion of LY294002.
Figure 3.
Effects of blocking PI3K on mTOR expression. (a) Top panel: typical bands and bottom panel: averaged data, showing expression of p-mTOR and p-S6K1 was amplified in the dorsal horn of CYP-rats with vehicle treatment (n = 6–10) as compared with saline control rats (n = 6–8). Blocking PI3K signal pathway by intrathecal infusion of LY294002 attenuated increases in p-mTOR and p-S6K1 in CYP-rats. *P < 0.05 versus control animals and CYP-animals infused with LY294002 (n = 6–10 in each group). (b) The ratio of p-mTOR and p-S6K1 levels versus total protein of mTOR and S6K1 levels was significantly increased in CYP-rats. This was attenuated by infusion of LY294002. *P < 0.05 versus control rats and CYP-animals infused with LY294002 (n = 6–10 in each group). In this study, data were analyzed using two sample t-test.
The levels of substance P and CGRP
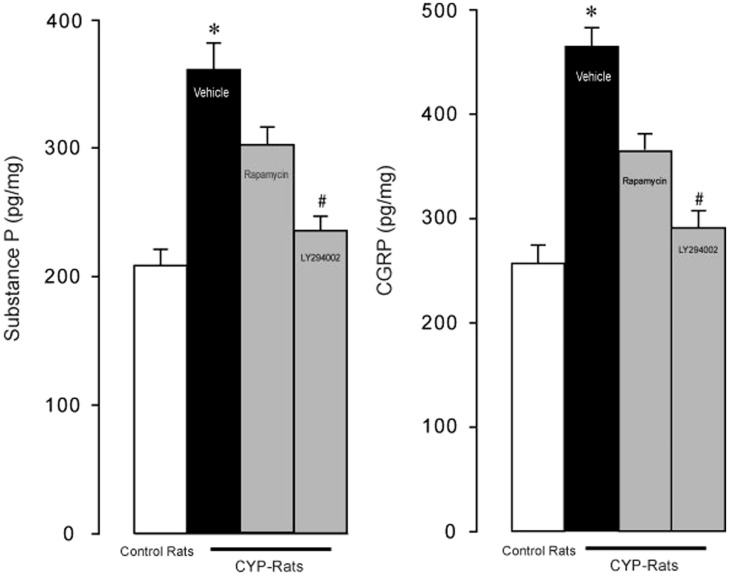
In additional experiments, we examined the effects of CYP on the levels of substance P and CGRP in the superficial dorsal horn of the spinal cord. Figure 4 showed that substance P and CGRP were significantly increased in CYP-rats with vehicle infusion (n = 12) as compared with control rats (n = 8). Substance P was 206 ± 14 pg/mg in control rats and 356 ± 19 pg/mg in CYP-rats with vehicle infusion (P < 0.05 vs. control rats). CGRP was 253 ± 19 pg/mg in control rats and 468 ± 20 pg/mg in CYP-rats with vehicle infusion (P < 0.05 vs. control rats). Furthermore, blocking individual mTOR and PI3K signaling pathways by intrathecal infusion of rapamycin and LY294002 (n = 10 in each group) significantly attenuated amplifications in substance P and CGRP evoked by CYP. Note that LY294002 had a greater inhibitory effect on substance P and CGRP than rapamycin did.
Figure 4.
Effects of blocking mTOR and PI3K pathways on the levels of substance P and CGRP. CYP significantly increased substance P and CGRP as compared with controls, and blocking mTOR and PI3K by rapamycin and LY294002 significantly attenuated the enhancement in substance P and CGRP evoked by CYP. Note that LY294002 had a greater inhibitory effect on substance P and CGRP than rapamycin did. *P < 0.05, indicated CYP-rats with vehicle infusion (n = 12) versus control rats (n = 8) and CYP-rats with rapamycin (n = 10) and LY294002 (n = 10) infusion. #P < 0.05, indicated CYP-rats with rapamycin versus CYP-rats with LY294002. Note that data were analyzed using one-way ANOVA.
Discussion
Results of the current study demonstrate that the expression of p-mTOR, mTOR-p-S6K1, p-4E-BP1, and p-PI3K pathway were upregulated in CYP-rats as compared with control rats. Blocking mTOR by intrathecal infusion of rapamycin attenuated bladder hyperactivity and pain. Blocking PI3K signal attenuated activities of mTOR and also decreased bladder hyperactivity and pain. Moreover, enhanced spinal substance P and CGRP evoked by CYP were blunted after inhibition of either mTOR or PI3K.
We consistently observed development of mechanical hyperalgesia and hypersensitivity in CYP-rats. We further demonstrated that expression of p-mTOR, p-S6K1, and p-4E-BP1 in the superficial dorsal horn of CYP-rats was upregulated, and mTOR antagonist rapamycin infused into the dorsal horn attenuated mechanical hyperalgesia and restored shortened intercontraction interval evoked by CYP.
The PI3K/Akt pathway is an intracellular signaling pathway in regulating the cell cycle. This important mechanism is directly related to cellular quiescence, proliferation, and longevity. PI3K can phosphorylate and activate Akt in the plasma membrane.23 The Akt leads to several downstream effects which alters transcription of p70 ribosomal S6K1 or 4E-BP1 and activating cAMP response element-binding protein and inhibition of p27, etc.3,6,23,24 Our study demonstrated that blocking PI3K attenuated p-mTOR and p-S6K1 expression, but also that intrathecal infusion of PI3K inhibitor attenuated hyperalgesia and restored shortened intercontraction interval observed in CYP-rats. This suggests that PI3K is necessary to play a regulatory role in mediating the effects of mTOR on CYP-evoked bladder mechanical pain and hyperactivity responses.
It is well known that stimulation of nociceptive receptors in the sensory nerves leads to the releases of substance P and CGRP from the nerve terminal of dorsal root ganglions into the superficial dorsal horn.20,25 Numerous receptors present on the presynaptic site of the nerve terminals and contribute to the releases of substance P and CGRP in regulating inflammatory pain.15 It is assumed that PI3K-mTOR pathway can indirectly affect these receptors such as transient receptor potential vanilloid 1 and thereby decrease the levels of substance P and CGRP.9 Another source of substance P and CGRP is likely originated from the dorsal horn interneurons.26,27 PI3K-mTOR signal pathway is likely to present in these interneurons containing two neuropeptides. Thus, blocking PI3K-mTOR can decrease the levels of those two neuropeptides. Nevertheless, in our current study, the levels of substance P and CGRP, as two important neurotransmitters engaged in inflammatory pain, were significantly increased in the superficial dorsal horn of CYP-rats. Moreover, the increased substance P and CGRP were significantly attenuated after respective injection of rapamycin and LY294002. Thus, our data suggest that amplified expression of spinal mTOR and its downstream pathways S6K1 or 4E-BP1 are likely engaged in CYP-induced bladder mechanical hyperalgesia and hyperactivity via the releases of substance P and CGRP.
Notably, we observed that LY294002 had a greater effect on substance P and CGRP than rapamycin did, indicating the role played by PI3K as a upstream pathway in regulating hypersensitive responses observed in CYP-rats via mTOR signals. This also suggests that mTOR is not the only downstream pathway of PI3K. With respect to the greater effect of LY294002, it could also be due to that the dose of rapamycin used in the present study was low. Nevertheless, to the best of our knowledge, there is lacking of evidence specifically showing the role played by mTOR and PI3K in regulating the releases of spinal substance P and CGRP in a pain model induced by CYP. Results of the present report suggest that substance P and CGRP regulated by mTOR and PI3K at the spinal level contribute to mechanical pain in CYP-induced cystitis.
Conclusion
In CYP-rats, spinal p-mTOR and mTOR-mediated p-S6K1 and p-4E-BP1 are upregulated, which results in mechanical pain and bladder hyperactivity. Intrathecal administration of rapamycin has a significant analgesic effect in a rat model of bladder pain with cystitis. Moreover, blocking PI3K blunts the amplified expression of p-mTOR pathways and thereby alleviates CYP-evoked bladder pain and exaggerated activity. Nonetheless, our data for the first time reveal specific signaling pathways leading to bladder pain and hyperactivity with cystitis, including the activation of mTOR and PI3K and downstream pathways. Results of our study provide a base for the mechanisms responsible for CYP-induced cystic pain. Targeting one or more of these signaling molecules involved in activation of mTOR at the spinal levels may present new opportunities for treatment and management of pain often observed in patients with cystitis.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Hanno PM, Erickson D, Moldwin R, et al. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J Urol 2015; 193: 1545–1553. [DOI] [PubMed] [Google Scholar]
- 2.Arms L, Girard BM, Malley SE, et al. Expression and function of CCL2/CCR2 in rat micturition reflexes and somatic sensitivity with urinary bladder inflammation. Am J Physiol Renal Physiol 2013; 305: F111–F122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hay N, Sonenberg N. Upstream and downstream of mTOR. Genes Dev 2004; 18: 1926–1945. [DOI] [PubMed] [Google Scholar]
- 4.Bao Y, Gao Y, Hou W, et al. Engagement of signaling pathways of protease-activated receptor 2 and mu-opioid receptor in bone cancer pain and morphine tolerance. Int J Cancer 2015; 137: 1475–1483. [DOI] [PubMed] [Google Scholar]
- 5.Costa-Mattioli M, Sossin WS, Klann E, et al. Translational control of long-lasting synaptic plasticity and memory. Neuron 2009; 61: 10–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Banko JL, Poulin F, Hou L, et al. The translation repressor 4E-BP2 is critical for eIF4F complex formation, synaptic plasticity, and memory in the hippocampus. J Neurosci 2005; 25: 9581–9590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Geranton SM, Jimenez-Diaz L, Torsney C, et al. A rapamycin-sensitive signaling pathway is essential for the full expression of persistent pain states. J Neurosci 2009; 29: 15017–15027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Price TJ, Rashid MH, Millecamps M, et al. Decreased nociceptive sensitization in mice lacking the fragile X mental retardation protein: role of mGluR1/5 and mTOR. J Neurosci 2007; 27: 13958–13967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu Q, Fitzsimmons B, Steinauer J, et al. Spinal phosphinositide 3-kinase-Akt-mammalian target of rapamycin signaling cascades in inflammation-induced hyperalgesia. J Neurosci 2011; 31: 2113–2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Asante CO, Wallace VC, Dickenson AH. Formalin-induced behavioural hypersensitivity and neuronal hyperexcitability are mediated by rapid protein synthesis at the spinal level. Mol Pain 2009; 5: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jiang Z, Wu S, Wu X, et al. Blocking mammalian target of rapamycin alleviates bone cancer pain and morphine tolerance via micro-opioid receptor. Int J Cancer 2016; 138: 2013–2020. [DOI] [PubMed] [Google Scholar]
- 12.Morgado C, Terra PP, Tavares I. Neuronal hyperactivity at the spinal cord and periaqueductal grey during painful diabetic neuropathy: effects of gabapentin. Eur J Pain 2010; 14: 693–699. [DOI] [PubMed] [Google Scholar]
- 13.Silva M, Amorim D, Almeida A, et al. Pronociceptive changes in the activity of rostroventromedial medulla (RVM) pain modulatory cells in the streptozotocin-diabetic rat. Brain Res Bull 2013; 96: 39–44. [DOI] [PubMed] [Google Scholar]
- 14.Bouhassira D, Lantéri-Minet M, Attal N, et al. Prevalence of chronic pain with neuropathic characteristics in the general population. Pain 2008; 136: 380–387. [DOI] [PubMed] [Google Scholar]
- 15.Hua X-Y, Yaksh TL. Dorsal horn substance P and NK1 receptors: study of a model system in spinal nociceptive processing. In: Malcangio M. (ed). Synaptic plasticity in pain, New York: Springer Science Business Media, 2009, pp. 109–138. [Google Scholar]
- 16.Chen B, Zhang H, Liu L, et al. PK2/PKR1 signaling regulates bladder function and sensation in rats with cyclophosphamide-induced cystitis. Mediators Inflamm 2015. 2015: 289519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sugino Y, O'Malley KJ, Wang Z, et al. Laser-capture microdissection for analysis of cell type-specific gene expression of muscarinic receptor subtypes in the rat bladder with cyclophosphamide-induced cystitis. Int Urol Nephrol 2015; 47: 637–642. [DOI] [PubMed] [Google Scholar]
- 18.Chaplan SR, Bach FW, Pogrel JW, et al. Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods 1994; 53: 55–63. [DOI] [PubMed] [Google Scholar]
- 19.Engel MA, Khalil M, Mueller-Tribbensee SM, et al. The proximodistal aggravation of colitis depends on substance P released from TRPV1-expressing sensory neurons. J Gastroenterol 2012; 47: 256–265. [DOI] [PubMed] [Google Scholar]
- 20.Lin Q, Li D, Xu X, et al. Roles of TRPV1 and neuropeptidergic receptors in dorsal root reflex-mediated neurogenic inflammation induced by intradermal injection of capsaicin. Mol Pain 2007; 3: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Puttfarcken PS, Han P, Joshi SK, et al. A-995662 [(R)-8-(4-methyl-5-(4-(trifluoromethyl)phenyl)oxazol-2-ylamino)-1,2,3,4-tetrahydr onaphthalen-2-ol], a novel, selective TRPV1 receptor antagonist, reduces spinal release of glutamate and CGRP in a rat knee joint pain model. Pain 2010; 150: 319–326. [DOI] [PubMed] [Google Scholar]
- 22.Al-Batran SE, Ducreux M, Ohtsu A. mTOR as a therapeutic target in patients with gastric cancer. Int J Cancer 2012; 130: 491–496. [DOI] [PubMed] [Google Scholar]
- 23.Shor B, Gibbons JJ, Abraham RT, et al. Targeting mTOR globally in cancer: thinking beyond rapamycin. Cell Cycle 2009; 8: 3831–3837. [DOI] [PubMed] [Google Scholar]
- 24.Bevan S, Quallo T, Andersson DA. TRPV1. Handb Exp Pharmacol 2014; 222: 207–245. [DOI] [PubMed] [Google Scholar]
- 25.Chaouch A, Besson JM. Peripheral and spinal mechanisms of nociception. Rev Neurol 1986; 142: 173–200. [PubMed] [Google Scholar]
- 26.Kozsurek M, Lukacsi E, Fekete C, et al. Cocaine- and amphetamine-regulated transcript peptide (CART) is present in peptidergic C primary afferents and axons of excitatory interneurons with a possible role in nociception in the superficial laminae of the rat spinal cord. Eur J Neurosci 2007; 26: 1624–1631. [DOI] [PubMed] [Google Scholar]
- 27.Wang D, Zhao J, Wang J, et al. Deficiency of female sex hormones augments PGE and CGRP levels within midbrain periaqueductal gray. J Neurol Sci 2014; 346: 107–111. [DOI] [PubMed] [Google Scholar]