Abstract
Objective:
To characterize the frequency of and risk factors for out-of-hospital sudden neurologic deaths.
Methods:
During the initial 25 months (February 1, 2011–March 1, 2013) of the San Francisco Postmortem Systematic Investigation of Sudden Cardiac Death Study, we captured incident WHO criteria sudden cardiac deaths (SCDs) through active surveillance of consecutive out-of-hospital deaths, which must be reported to the medical examiner by law. All cases were referred for full autopsy with detailed examination of the heart and cranial vault, toxicology, and histology. A multidisciplinary committee adjudicated a final cause of death.
Results:
Of 352 incident SCDs, 335 (95%) underwent systematic evaluation including full autopsy. Of these 335 cases, 18 (5.4%) were sudden neurologic deaths (mean age 60.6 years [SD 17.6, range 27–87]; 67.7% female), which accounted for 14.9% of the 121 noncardiac sudden deaths. The risk of sudden neurologic death compared to non-neurologic SCD was lower in male and white participants (p < 0.01). Neurologic causes included intracranial hemorrhage (8), sudden unexpected death in epilepsy (6, including 2 with juvenile myoclonic epilepsy), aneurysmal subarachnoid hemorrhage (2), acute ischemic stroke (1), and aspiration from Huntington disease (1). Most deaths were unwitnessed (16; 89%) with asystole at presentation (17; 94%). Prior stroke/TIA was not associated with risk of stroke (odds ratio [OR] 1.4 [95% confidence interval (CI) 0.18–11.8], p = 0.73), but antithrombotic medication use was (OR 3.9 [95% 1.01–15.5], p = 0.05).
Conclusions:
Sudden neurologic death is an important cause of out-of-hospital apparent SCDs. Low prevailing autopsy rates may result in systematic misclassification of apparent SCDs and underestimation of the incidence of sudden neurologic death.
Sudden cardiac death (SCD) is defined as a sudden unexpected death occurring within 1 hour of symptom onset for witnessed events, or within 24 hours of being observed symptom-free for unwitnessed events.1 By this definition, there are 184,000 to 450,000 sudden cardiac deaths in the United States annually and more than 90% occur out of the hospital.2 Since complete autopsies are uncommon and investigations for these natural deaths are limited, a cardiac cause is often assumed and cerebrovascular deaths or sudden unexpected death in epilepsy (SUDEP) could be missed. Therefore, we conducted complete autopsies and systematically evaluated consecutive out-of-hospital SCDs as part of the Postmortem Systematic Investigation of Sudden Cardiac Death (POST SCD) Study.3
METHODS
From February 2011 to March 2013, through active, real-time surveillance of all medical examiner cases, we identified all incident SCDs within the city and county of San Francisco.3 State law mandates reporting all out-of-hospital deaths to the medical examiner.1 All cases were referred for systematic and comprehensive evaluations, including full autopsies, toxicology, and detailed heart and cranial vault examinations. A multidisciplinary committee of cardiologists and cardiac electrophysiologists, anatomic and forensic pathologists, and a neurologist adjudicated the causes of death by consensus. Stata (StataCorp LP, College Station, TX) was used for all statistical analyses.
Standard protocol approvals, registrations, and patient consents.
Local institutional review board approval with a waiver of informed consent was obtained for this study.
RESULTS
Of 352 consecutive SCDs identified during the 25-month study period, 335 (95.2%) underwent a systematic evaluation and full autopsy (table 1). Of these 335 cases, 18 (5.4%) had an acute neurologic cause of death (table 2). Sudden neurologic death accounted for 15% (18 of 121) of all noncardiac deaths, and was the most common noncardiac cause of sudden death after drug overdose. The risk of sudden neurologic death compared to non-neurologic sudden cardiac death was lower in male (p = 0.001) and white participants (p = 0.01). Sudden neurologic deaths were typically unwitnessed (16; 89% vs 74%; p = 0.26) and had asystole at initial presentation (15; 83% vs 79%; p = 0.14).
Table 1.
Characteristics of sudden cardiac deaths (SCD), sudden neurologic deaths (SND), non-neurologic sudden deaths, and adult San Francisco population
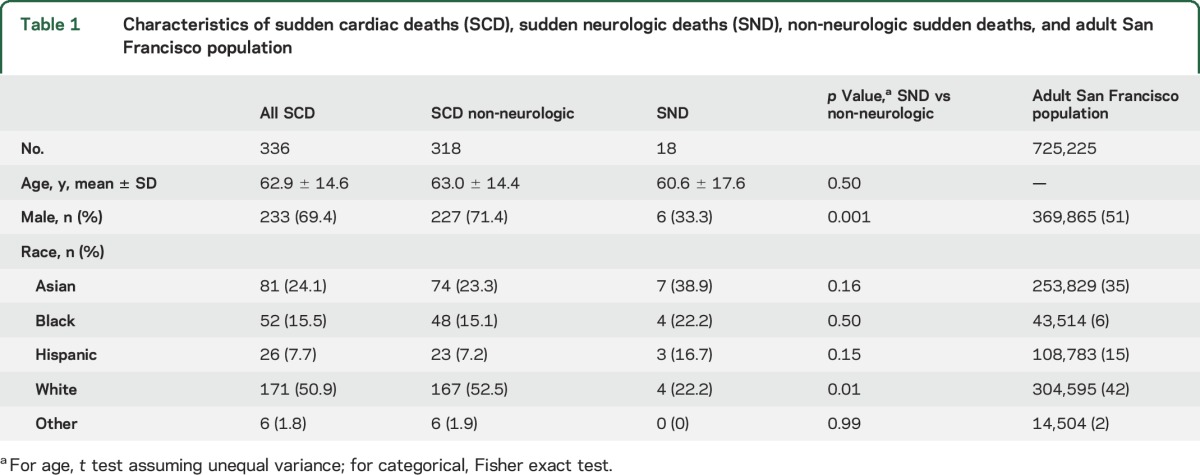
Table 2.
Consecutive cases of sudden neurologic death in San Francisco (February 1, 2011–March 1, 2013)
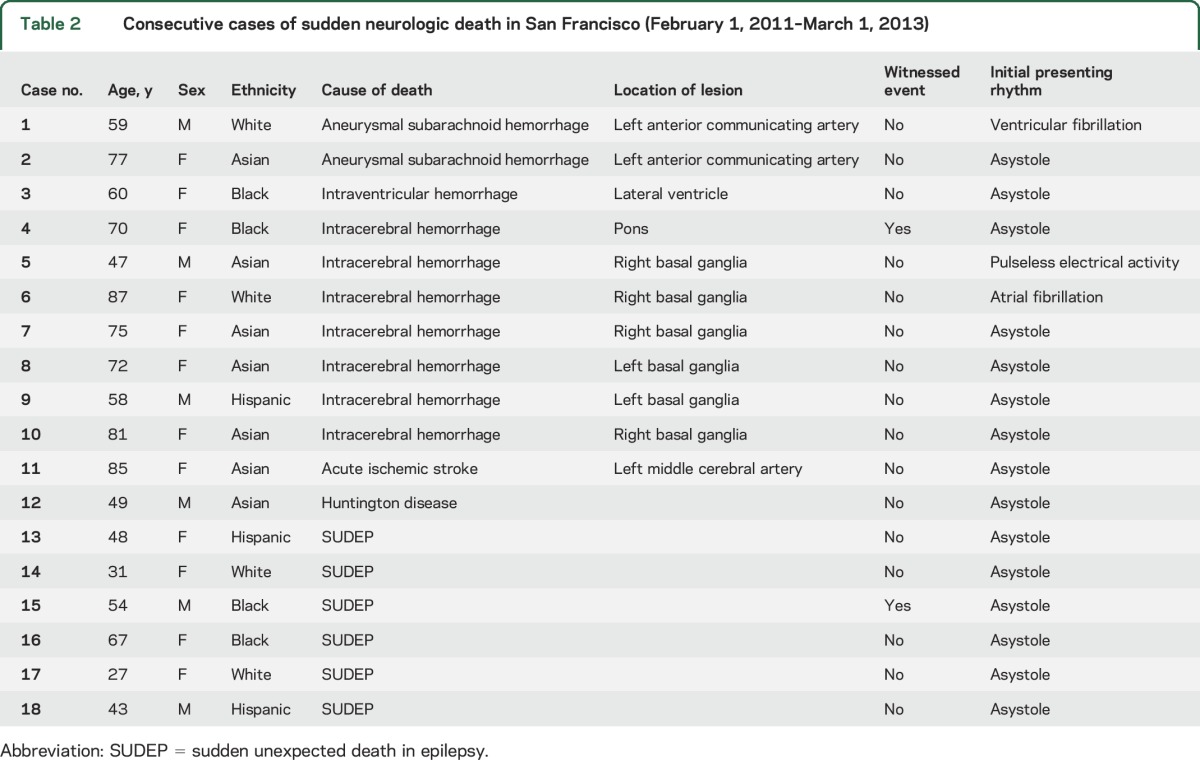
Most intracerebral (6/8) and subarachnoid (1/2) hemorrhage deaths occurred while on antiplatelet or anticoagulant therapy. One ischemic stroke death occurred in an 85-year-old woman with atrial fibrillation with an unwitnessed left middle cerebral artery stroke. Antiplatelet or anticoagulation use was associated with intracranial hemorrhage among noncardiac deaths (odds ratio [OR] 6.0 [95% confidence interval (CI) 1.5–24.8], p = 0.01) and overall (OR 3.9 [95% CI 1.01–15.5], p = 0.05). A history of stroke or TIA was not associated with hemorrhagic or ischemic stroke among noncardiac deaths (OR 1.1 [95% CI 0.13–9.8]; p = 0.92) or overall (OR 1.4 [95% CI 0.18–11.8], p = 0.73). In one case, postmortem interrogation of an implantable cardioverter defibrillator demonstrated that the patient had been repeatedly shocked for ventricular fibrillation, but the full autopsy revealed that aneurysmal subarachnoid hemorrhage was the cause of death that secondarily led to neurogenic ventricular fibrillation (figure).
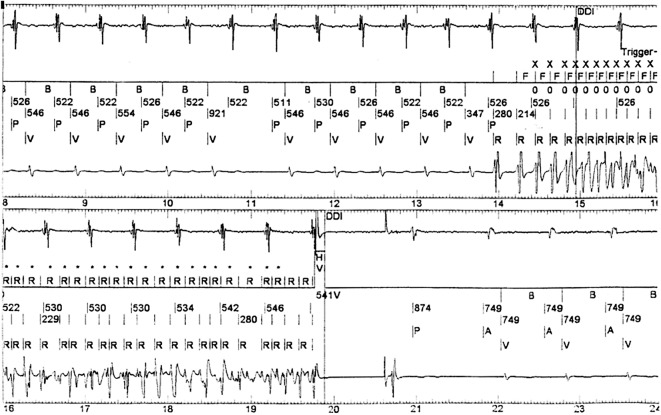
Figure. Postmortem interrogation of an implantable cardioverter-defibrillator (ICD) from a 59-year-old man with history of heart failure and unwitnessed sudden death found to have aneurysmal subarachnoid hemorrhage on autopsy.
This representative intracardiac ECG demonstrates intrinsic sinus (P) with paced ventricular (V) rhythm degenerating to ventricular fibrillation (R), which was recognized by the ICD and treated with a 35 J shock, restoring atrial-ventricular (AV) paced rhythm. Ventricular fibrillation recurred shortly thereafter and was treated with >30 ICD shocks until the battery of the device was depleted.
Of the 6 SUDEP cases, 3 had nonspecific cardiac findings (minor thickening of septal and posterior left ventricle and interstitial fibrosis) and 1 case had a witnessed seizure followed by asystole and apnea. Two cases were in young women with juvenile myoclonic epilepsy, including 1 who had recently stopped taking seizure medications. SUDEP cases were significantly younger than other sudden neurologic deaths and the cohort overall (mean age 45 years; SD 14.8; range 27–67; p = 0.001 and p = 0.002, respectively).
A history of epilepsy was identified in 15 of 335 (4.5%) sudden deaths; 6 (40%) were SUDEP. Of the remaining 9 sudden deaths in epilepsy patients, 7 died of cardiac causes (2 hypertrophy, 2 cardiomyopathy, 1 chronic coronary artery disease, 1 acute coronary artery disease, 1 heart failure) and 2 had noncardiac deaths (1 intracranial hemorrhage, 1 incarcerated hernia). A history of epilepsy was associated with a substantially higher relative risk of sudden neurologic death compared to sudden cardiac death (relative risk 10.6, 95% CI 4.6–25.5; p < 0.0001). Similarly, 7.5% (25 of 335) sudden deaths had a history of at least 1 seizure, often in the setting of alcohol withdrawal; 24% (6 of 25) were SUDEP. For the 10 cases with history of seizure but not epilepsy, 5 died of cardiac causes, 1 had a pulmonary embolism, 1 had hemorrhage, and 3 had an overdose.
DISCUSSION
In this comprehensive, population-based study of consecutive out-of-hospital apparent SCDs, 5.4% were due to an acute neurologic cause. These sudden neurologic deaths represented the largest group of noncardiac sudden deaths after drug overdose. The lower risk of sudden neurologic death compared to sudden cardiac death among male and white participants and a corresponding trend toward increased risks in women and the fast-growing population of Asians and Hispanics may justify follow-up studies to evaluate whether greater vigilance is warranted for specific demographics. Prior estimates of out-of-hospital sudden death were derived from ethnically homogeneous populations with low autopsy rates (typically <15%) or were based on retrospective review of records from incomplete or selectively applied investigations.4 Moreover, in the rare cases when they are performed, autopsies for natural out-of-hospital deaths often exclude cranial vault or neuropathologic examination, thereby increasing the risk for misclassification.5,6
Given that the case fatality rate for stroke is high, cerebrovascular deaths were not unexpected. Although stroke can cause death through direct mass effect, hydrocephalus, and herniation, especially when unwitnessed and untreated, neurocardiogenic pathways can also be involved. For instance, subarachnoid hemorrhage can cause characteristic electrocardiographic changes and a Takotsubo pattern of apical hypokinesis and cardiac injury (voodoo death) and increased intracranial pressure can cause autonomic changes and arrhythmias.7 For SUDEP, the mechanism of death may also include neurocardiogenic and neurorespiratory mechanisms.
Assuming that 5.4% of apparent SCDs are sudden neurologic deaths, as we found, then there are 10,000 to 25,000 sudden neurologic deaths in the United States annually.2 Similarly, if half of the 2.3% of intracerebral hemorrhage deaths we observed were missed without a full autopsy, this would translate into 2,000 to 5,000 fatal intracerebral hemorrhages annually (a 30% increase in incidence).8 For aneurysmal subarachnoid hemorrhage, similar assumptions would result in an additional 500 to 1,300 fatal subarachnoid hemorrhages annually (a nearly 25% increase in incidence).9 For SUDEP, assuming a 1% prevalence of epilepsy among San Francisco adult population of 725,225, the 3.4 out-of-hospital cases per year we observed represents about half of the expected SUDEP cases, though our methods only capture out-of-hospital deaths.10
A failure to identify sudden neurologic deaths, particularly among those at high risk for SCD, has potential implications for interpreting the results in large cardiovascular trials. Those at high risk for SCD are often on antithrombotic therapy, which increases the risk of hemorrhage. Yet identifying intracerebral hemorrhage adverse outcomes among these clinical trial participants typically relies on the overburdened medical examiner and coroner's infrastructure, low prevailing autopsy rates, and unreliable death certificates. Although the limited number of outcomes in our study precludes a precise characterization of associated risk factors, overall misclassification of these outcomes in cardiovascular clinical trials could shift balance of the relative risks and benefits of antithrombotic therapy.
Sudden neurologic death accounts for a substantial proportion of sudden deaths that would otherwise meet the widely applied epidemiologic definition of out-of-hospital SCD. Systematic autopsies of nearly every SCD in San Francisco over a 2-year period allowed for the accurate recognition of these neurologic causes and provide a framework for revising estimates of the incidence of acutely fatal neurologic events. These data may change public health estimates of disease burden and mortality attributed to SCD and to neurologic disorders in the general population, for women and certain race-ethnic subgroups in particular, and among high-risk participants in cardiovascular clinical trials.
ACKNOWLEDGMENT
The authors thank Benjamin Colburn, Nina Clark, and Rana Khan for data acquisition and Amy Hart for key facilitation of activities in the Office of the Chief Medical Examiner, County of San Francisco.
GLOSSARY
- CI
confidence interval
- OR
odds ratio
- SCD
sudden cardiac death
- SUDEP
sudden unexpected death in epilepsy
AUTHOR CONTRIBUTIONS
Anthony Kim contributed to study conception and design, acquisition of data, drafting the manuscript, analysis and interpretation of data, and critical revision of the manuscript. Ellen Moffatt contributed to acquisition of data and critical revision of the manuscript. Philip Ursell contributed to acquisition of data and critical revision of the manuscript. Orrin Devinsky contributed to critical revision of the manuscript. Jeffrey Olgin contributed to acquisition of data and critical revision of the manuscript. Zian Tseng contributed to acquisition of study funding, study conception and design, acquisition of data, analysis and interpretation of data, and critical revision of the manuscript.
STUDY FUNDING
This study was funded by NIH R01 HL102090 (NHLBI) to Z.H.T. and UCSF-CTSI UL1 TR000004 (NCATS) to A.S.K. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
DISCLOSURE
A. Kim reports grants from NIH/NCATS during the conduct of the study and research grants from SanBio and BioGen outside of the submitted work. E. Moffatt and P. Ursell report no disclosures relevant to the manuscript. O. Devinsky was Principal Investigator of the North American SUDEP Registry during the conduct of the study. J. Olgin reports no disclosures relevant to the manuscript. Z. Tseng reports grants from NIH/NHLBI during the conduct of the study and personal fees from Biotronik, outside the submitted work. Go to Neurology.org for full disclosures.
REFERENCES
- 1.World Health Organization. Sudden Cardiac Death. World Health Organization Technical Report Series, Report 726. Geneva: World Health Organization; 1985. [Google Scholar]
- 2.Zheng ZJ, Croft JB, Giles WH, Mensah GA. Sudden cardiac death in the United States, 1989 to 1998. Circulation 2001;104:2158–2163. [DOI] [PubMed] [Google Scholar]
- 3.Tseng ZH, Hayward RM, Clark NM, et al. Sudden death in patients with cardiac implantable electronic devices. JAMA Intern Med 2015;175:1342–1350. [DOI] [PubMed] [Google Scholar]
- 4.Chugh SS, Jui J, Gunson K, et al. Current burden of sudden cardiac death: multiple source surveillance versus retrospective death certificate-based review in a large U.S. community. J Am Coll Cardiol 2004;44:1268–1275. [DOI] [PubMed] [Google Scholar]
- 5.Nemetz PN, Tanglos E, Sands LP, Fisher WP Jr, Newman WP III, Burton EC. Attitudes toward the autopsy: an 8-state survey. MedGenMed 2006;8:80. [PMC free article] [PubMed] [Google Scholar]
- 6.Hoyert DL. The changing profile of autopsied deaths in the United States, 1972–2007. NCHS Data Brief 2011:1–8. [PubMed] [Google Scholar]
- 7.Samuels M. Cardiopulmonary aspects of acute neurologic diseases. In: Neurological and Neurosurgical Intensive Care, 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2004. [Google Scholar]
- 8.Centers for Disease Control and Prevention NCHS. Underlying cause of death 1999–2013 on CDC WONDER online database, released 2015: data are from the Multiple Cause of Death Files, 1999–2013, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Available at: wonder.cdc.gov/ucd-icd10.html. Accessed October 23, 2015.
- 9.Inamasu J, Miyatake S, Tomioka H, et al. Subarachnoid haemorrhage as a cause of out-of-hospital cardiac arrest: a prospective computed tomography study. Resuscitation 2009;80:977–980. [DOI] [PubMed] [Google Scholar]
- 10.Tomson T, Nashef L, Ryvlin P. Sudden unexpected death in epilepsy: current knowledge and future directions. Lancet Neurol 2008;7:1021–1031. [DOI] [PubMed] [Google Scholar]