Abstract
Background
Middle-aged women are at risk of weight gain and associated comorbidities. Deliberate restriction of food intake (dieting) produces short-term weight loss but is largely unsuccessful for long-term weight management. Two promising approaches for the prevention of weight gain are intuitive eating (ie, eating in accordance with hunger and satiety signals) and the development of greater psychological flexibility (ie, the aim of acceptance and commitment therapy [ACT]).
Objectives
This pilot study investigated the usage, acceptability, and feasibility of “Mind, Body, Food,” a Web-based weight gain prevention intervention prototype that teaches intuitive eating and psychological flexibility skills.
Methods
Participants were 40 overweight women (mean age 44.8 [standard deviation, SD, 3.06] years, mean body mass index [BMI] 32.9 [SD 6.01] kg/m2, mean Intuitive Eating Scale [IES-1] total score 53.4 [SD 7.46], classified as below average) who were recruited from the general population in Dunedin, New Zealand. Module completion and study site metrics were assessed using Google Analytics. Use of an online self-monitoring tool was determined by entries saved to a secure online database. Intervention acceptability was assessed postintervention. BMI, intuitive eating, binge eating, psychological flexibility, and general mental and physical health were assessed pre- and postintervention and 3-months postintervention.
Results
Of the 40 women enrolled in the study, 12 (30%) completed all 12 modules (median 7.5 [interquartile range, IQR, 2-12] modules) and 4 (10%) used the self-monitoring tool for all 14 weeks of the intervention period (median 3 [IQR 1-9] weeks). Among 26 women who completed postintervention assessments, most women rated “Mind, Body, Food” as useful (20/26, 77%), easy to use (17/25, 68%) and liked the intervention (22/25, 88%). From pre- to postintervention, there were statistically significant within-group increases in intuitive eating (IES-2 total score P<.001; all IES-2 subscale scores: P ≤.01), psychological flexibility (P=.01), and general mental health (P<.001) as well as significant decreases in binge eating (P=.01). At the 3-month follow-up, IES-2 improvements were maintained, and there were further improvements in binge eating (P<.001) and general mental health (P=.03), and a marginal yet nonsignificant tendency for further improvement in psychological flexibility (P=.06). There were no significant within-group changes in BMI from pre- to postintervention and postintervention to 3-month follow-up (P=.46 and P=.93, respectively).
Conclusions
The “Mind, Body, Food” prototype Web-based intervention is appealing to middle-aged women and may be a useful tool to help women learn intuitive eating and ACT skills, reduce binge eating, and maintain weight over 3 months. Further work to improve the user experience and engagement is required before testing the online intervention in a randomized controlled trial.
Keywords: Web-based intervention, overweight, obesity, prevention, middle-aged women, BMI, intuitive eating, acceptance and commitment therapy
Introduction
Despite the high prevalence of reported attempts at weight control, obesity rates worldwide continue to increase [1-3]. Since obesity is associated with many adverse health consequences [4], and weight loss interventions have shown modest long-term success [5-7], there is an increasing focus on the prevention of weight gain [8,9]. Among middle-aged women (40-50 years), weight gains of 0.5 to 0.7 kg per year have been observed [10-12], and there is evidence that the greatest risk for weight gain is among women who are already overweight or obese [10]. Around menopause, weight gain is associated with increases in cardiovascular risk factors such as blood pressure, total cholesterol, low-density lipoprotein cholesterol, triglycerides, and fasting insulin [12]. For these reasons, effective weight gain prevention has been identified as an important goal for premenopausal women [12], because even among middle-aged women who report following healthy weight control behaviors (eg, decreased food quantity, exercise, reducing fat intake), weight gain is observed [1].
Intuitive eating is a nondieting, adaptive approach to eating behavior characterized by eating for physical rather than emotional reasons, relying on internal hunger and satiety cues, unconditional permission to eat when hungry and what food is desired, and choosing nutritious foods to help one’s body function well [13-15]. Although intuitive eating shares similarities with mindful eating, there are differences. Mindful eating involves paying attention, without judgment, to the eating experience and to hunger/satiety cues and eating attentively without distraction [16]. However, intuitive eating also takes nutrition into consideration when choosing foods to enhance/support body function and involves giving oneself unconditional permission to eat not only when hungry but those foods one truly feels like eating [13-15]. Cross-sectional research has shown intuitive eating to be positively related to body appreciation, self-esteem, and satisfaction with life and inversely related to eating disorder symptomatology, poor interoceptive awareness, body surveillance, body shame, body mass index (BMI), and internalization of media appearance ideals [14]. Intuitive eating was inversely associated with BMI in a nationwide sample of middle-aged women [17] and intuitive eating interventions have lowered cholesterol levels, blood pressure, disordered eating, body dissatisfaction, and depression and improved diet quality, physical activity, stress management, and self-esteem [18,19]. Compared to diet group participants, participants who practice intuitive eating have been shown to maintain improvements in metabolic function (eg, blood pressure, blood lipids) even in the absence of weight loss, whereas little improvement was sustained in diet group participants [19]. A recent review of 20 studies evaluating intuitive eating interventions [18] reported reductions in weight in 6 studies, weight maintenance in 8 studies, and mixed results in 2 studies.
Long-term weight management is enhanced by effective emotion regulation skills [20,21]. A growing body of evidence supports the effectiveness of acceptance and commitment therapy (ACT) in the management of obesity [22-27]. ACT-based interventions focus on improving psychological flexibility, which is the ability to remain mindfully aware and accepting of one’s experience in the present moment (eg, thoughts, feelings, bodily sensations) while also clarifying one’s values and choosing to engage in behavior that is consistent with those values [28]. ACT-based skills do not teach control or avoidance of eating triggers but rather develop skills that create a different relationship with these triggers: allowing individuals to be present without acting on the triggers (ie, acceptance). Acceptance-based interventions (ie, teaching skills such as values clarity and behavioral commitment, awareness of decision-making processes, and distress tolerance) have been shown to increase psychological flexibility and improve weight control, particularly for those who tend to eat in response to emotional and environmental triggers [29]. In randomized controlled trials (RCTs) among adults attempting weight loss, brief (ie, 6-8 hours) ACT-based interventions have been reported to be more effective for weight loss compared to no-treatment [25,27]. Tapper’s [27] findings suggest that the effect of the intervention on BMI was largely brought about by reductions in binge eating, while Lillis [25] reported that weight-specific acceptance and psychological flexibility significantly mediated BMI outcomes. Recently, Sairanen et al [30] reported that among overweight adults, the ability to recognize and accept aversive internal experiences (without reacting to them) was positively associated with eating for physical rather than emotional reasons.
Intuitive eating and ACT appear to be particularly well suited for integration, and to our knowledge, this is the first study to test them when used together. Both approaches focus on fostering a mindful, accepting, and open stance to one’s experiences. Intuitive eating teaches individuals to be more mindfully aware of and follow the body’s hunger and satiety cues, while ACT teaches individuals how to cope more effectively with negative and unwanted cognitive and emotional cues through awareness and acceptance. ACT skills may complement intuitive eating by helping to decouple eating behavior from emotional cues and external triggers, allowing for hunger and satiety cues to play a stronger role in regulating eating behavior.
Web-based interventions have the ability to have a major public health impact. They can present complex health information in simple formats (eg, video, graphic, audio) [31], overcome time and travel barriers of face-to-face interventions [32], reach a large audience [33], reduce stigma related to being overweight or obese [34], and facilitate weight management [35]. ACT interventions have been adapted for Web-based delivery and have been shown to be effective in teaching ACT-based skills to manage conditions such as tinnitus [36], chronic pain [37], work-related stress [38], and multiple behavioral health risks [39]; however, there are no published studies testing Web-based ACT for eating behavior interventions. Although a small number of studies have investigated Web-based healthy eating interventions based on nondiet and size acceptance approaches among young adults [40,41], no published study to date has, to our knowledge, designed and evaluated an online intuitive eating intervention. Integrating ACT and intuitive eating is a novel approach to changing eating behavior that when delivered online would provide an accessible weight management intervention grounded in evidence-based theory.
We developed an online intuitive eating intervention called “Mind, Body, Food,” based on the intuitive eating principles set forth by Tribole and Resch [15] and incorporating ACT-based skills. The aim of “Mind, Body, Food” was to teach middle-aged women intuitive eating skills facilitated via acquiring ACT-based skills. It was theorized that increased psychological flexibility resulting from the acquired ACT-based skills will further enable women to eat more intuitively by helping them to handle feelings, thoughts, urges, or cravings that can trigger eating when not physically hungry. The aim of this pilot study was to design an evidence-based prototype online intuitive eating intervention and investigate its acceptability, feasibility, and usage among middle-aged women.
Methods
Research Design and Setting
For this prospective single-arm pilot intervention study, participants were recruited from the community in Dunedin, New Zealand, and assessed preintervention, postintervention, and at 3-month follow-up. They accessed the intuitive eating intervention directly via the Internet. The University of Otago Human Ethics Committee granted ethical approval (reference code: H13/057). The Ngāi Tahu Research Consultation Committee approved the research methods as being consistent with the needs of the Ngāi Tahu iwi (South Island Māori, the indigenous population of New Zealand).
Participants and Recruitment
Women aged 40 to 50 years (inclusive) were eligible to participate in the study if they were able to communicate in English, able to engage in gentle physical activity (ie, walk at a leisurely pace for 10 minutes or more), premenopausal (ie, having a menstrual period in the preceding three months or currently being on any form of hormonal contraceptives that stopped menstruation [42]), and regularly accessed the Internet and email at least three days per week. To target women with the greatest potential to benefit from training in intuitive eating, we further restricted inclusion to women with below average Intuitive Eating Scale scores (IES) [13] (summed total IES score less than 65, based on nationwide survey data for overweight NZ women [17]) and with a BMI of at least 26.5 kg/m2 (calculated using measured height and weight). Women were excluded if they were pregnant or lactating, taking hormone replacement therapy, or a current smoker or if they had a history of hysterectomy, oophorectomy, diabetes, cancer, cardiovascular disease, or eating disorder. Additionally, women were excluded if they currently were taking a medication that may affect their appetite or were enrolled in any weight loss program.
To recruit women from a diverse range of socioeconomic and ethnic backgrounds, recruitment materials were circulated through local health promotion and social service networks, low socioeconomic neighborhoods, and organizations servicing Pacific and Māori populations. Recruitment materials were framed in the context of encouraging women interested in learning intuitive eating skills for long-term weight management. The study was also promoted in a local newspaper article.
Sample Size
We aimed for a sample size of 40 participants at the 3-month follow-up visit in order to investigate acceptability and usability as well as providing sufficiently precise estimates of outcome measure variability, correlations between repeated measures, and retention rates. The sample size was not determined according to statistical principles but was the number judged to be suitable for achieving the study objectives. The recruitment target was set at 58 women to account for an estimated 30% attrition rate, based on previous research [43].
“Mind, Body, Food” Intervention
The 12-module self-guided “Mind, Body, Food” intervention was developed through an iterative process involving extensive input from end-users. The content was guided by evidence-based research in the field [25,27] and the researchers’ own experience teaching intuitive eating (CCH, SB, TLT) and ACT skills (CCH, JL) face-to-face. A paper-based intervention prototype was pretested in focus groups and interviews with members of the target audience, followed by pretesting of a Microsoft PowerPoint-based prototype of the intervention. Following this, expert review of the intervention material, with a particular focus on intuitive eating (TT) and ACT (JL) content, was undertaken to ensure clarity and fidelity to the underpinning theoretical basis for the intervention. “Mind, Body, Food” content was then translated by a professional Web developer into a Web-based prototype (Figures 1 through 5), which was not compatible with mobile browsers. The Web-based prototype underwent usability and heuristic testing before the current study.
Figure 1.
"Mind, Body, Food" log-in page.
“Mind, Body, Food” consists of 12 modules, each covering skills related to intuitive eating and taking 15 to 20 minutes to complete. Table 1 presents “Mind, Body, Food” module titles and key skills and activities delivered. In each module, the key skills and their rationale were introduced in a 3- to 5-minute video featuring a discussion among three women (one dieter and two women who had learned intuitive eating). Each video commenced with discussion of a challenge related to eating (eg, recognizing physical hunger) before introducing the new skills and a discussion of the women’s experience of practicing the skills. Each module followed with a guided audio activity and typed activity. Guided experiential audio activities were used to deliver training in recognition of hunger and fullness signals and many of ACT’s core skills (eg, awareness and acceptance of thoughts and feelings; “surfing” urges to eat when not physically hungry [ie, acceptance]; visualizing placing thoughts on leaves floating in a stream [ie, ACT’s cognitive defusion skill]). Typed activities encouraged participants to reflect on how practicing the skills would make a difference to their life (ie, clarification of values). At the end of each module, users were encouraged to practice intuitive eating skills every day. Starting in Module 2, use of the Eating Awareness Tracker (EAT), a self-monitoring tool for recording nonjudgmental observations of eating-related experiences, was encouraged, and a library of additional resources was provided. The EAT enabled participants to monitor hunger, fullness, and mindfulness ratings during eating, each using 0 to 10 scales. Beginning in Module 1, the EAT was presented as an essential part of the intervention. Participants were encouraged to log into “Mind, Body, Food” to use the EAT as often as possible after meals or snacks and were provided an opportunity to practice using the EAT during Modules 2-11 by recording the most recent eating experience. At the end of each module, participants could choose to receive, via email or short message service (SMS), up to three daily prompts to use the EAT.
Table 1.
“Mind, Body, Food” modules (including the te reo Māori titles) and key skills taught in each module.
| Module | Title | Key skills | Activities |
| 1 | Ditch the Diets / Whakarerea te whakapuango | Giving self permission to eat wide range of foods. Guiding food choices based on what feels enjoyable and satisfying. | Practice before each snack/meal asking self, “It’s okay to have this, but will I truly enjoy this and feel satisfied?” Typed and audio activities: reflection on past experience of dieting, or labeling foods “forbidden.” |
| 2 | Tuning into Hunger / E rongo ana i te hikai | Recognizing what physical hunger feels like. Before eating, rating physical hunger on a scale 0 (absolutely empty) to 10 (sick from overeating). Initiating eating when hunger is rated 3 or 4. | Guided audio activity: scan of mouth, throat, and stomach to recognize physical signals of hunger. Typed activities: reflect on sensations of hunger (or lack of) before typical eating experiences, and reflect on how life would be different if body signals were listened to more often before eating. |
| 3 | Am I Full? Kua puta a pito? | Recognizing what fullness feels like and knowing when to take the last bite. While eating, rating fullness on a scale of 0 (absolutely empty) to 10 (sick from overeating). Finishing eating when fullness is rated 6 or 7. | Guided audio activity: awareness of stomach sensations to recognize physical signals of fullness. Typed activities: reflect on sensations of fullness after eating, and reflect on how life would be different if body signals were trusted to guide how much to eat. |
| 4 | One Bite at a Time / Kei ia ngau; ka ngau, a, ka ngau | Eating with nonjudgmental awareness (ie, mindfulness). Rating mindful eating on a scale from 0 (mindless eating) to 10 (mindful eating). Mindfully eating in 7 to 10 rating range. | Guided audio activity: practice mindfully eating a piece of dried fruit. Typed activity: reflect on usual level of mindfulness when eating and how the experience of eating would differ if more attention was paid to the food and how food affects the body. |
| 5 | Coping with Cravings / Whakataha atu te wararwara | Coping with urges to eat when not physically hungry (ie, acceptance). | Guided ACT audio activity: “urge surfing” to cope with a craving to eat when not physically hungry. Typed activities: reflect on common triggers to eat when not physically hungry and how life would be different if response to cravings was asking, “Am I physically hungry?” and “Is this food really what I feel like in this moment?” |
| 6 | Emotional Eating / Ka kai ki te whakarata i te mānuka | Identifying emotional triggers to eat (ie, acceptance). Coping with emotions without using food. | Guided ACT audio activity: practice making space for emotions (ie, not struggling to change them or get rid of them). Typed activities: reflect on common triggers to eat emotionally and how life would be different if allowing uncomfortable feelings to be present and not eating to change feelings. Ask, “Is emotional eating in line with what matters most in life?” |
| 7 | Every Body Deserves Respect / He mana tō ia tinana | Shifting focus from body appearance to appreciating body functions. | Guided audio activity: body scan with appreciation of body functions. Typed activities: describe self with nonjudgmental (ie, neutral or positive) words, and reflect on how life would be different if focus shifted from changing body’s appearance to appreciating body’s functions. |
| 8 | Dealing with Pressures to Diet / Whaihangatia ngā pēhanga o te whakapuako | Handling pressures to diet or engage in “fat talk.” | Audio activity: review of diet cycle, encourage body appreciation and reflection on positive experiences with intuitive eating to reinforce motivation to eat intuitively. Typed activities: reflect on positive changes made since beginning “Mind, Body, Food,” and identify responses to pressures to diet and “fat talk.” |
| 9 | Taming the Inner Critic / Whakarata te kaiwhakatāwai o roto | Distancing self from negative thoughts (ie, cognitive defusion). | Guided ACT audio activity: visualize placing unhelpful thoughts on leaves in a stream. Typed activities: identify techniques to “unhook” from unhelpful thoughts, and reflect on how life would differ if not attached to unhelpful thoughts. |
| 10 | Get Active Your Way / Kei a koe te tikanga korikori | Engaging in enjoyable physical activities every day. | Guided audio activity: Walking mindfully (ie, tuning into bodily sensations and surroundings while walking). Typed activities: reflect on benefits of physical activity and how to include physical activity in daily routine. |
| 11 | Fine Tuning Food Choices / Āta whiria te kai | Selecting healthier food options without feeling deprived. | Guided audio activity: mindful food shopping. Typed activity: identify enjoyable ways to eat more fruits and vegetables and choose lower fat foods without feeling deprived. |
| 12 | Staying on Track / Kia mau, kia ū | Staying motivated to maintain changes and recovering from “slips.” | Guided audio and typed activities: reflect on positive changes made since starting “Mind, Body, Food,” and identify barriers to eating intuitively and coping strategies. |
Participants completed the 12 modules over a 14-week period and were reminded by email during the first 12 weeks when each new module became available. A new module became available only once the previous module was completed (as defined by clicking Done on the last page of the module). Participants could also receive a weekly notification via SMS that each new module was available. No recommendations were given regarding how frequently the intervention should be accessed. The “Mind, Body, Food” intervention was available until the final 3-month follow-up assessment, allowing participants to revisit and revise previous material.
Figure 2.
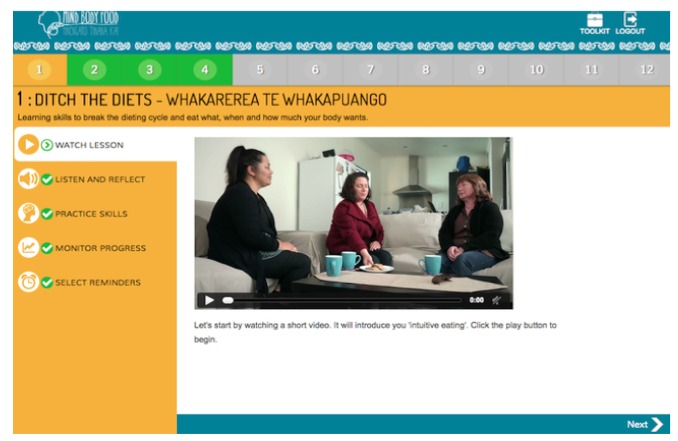
Video activity.
Figure 3.
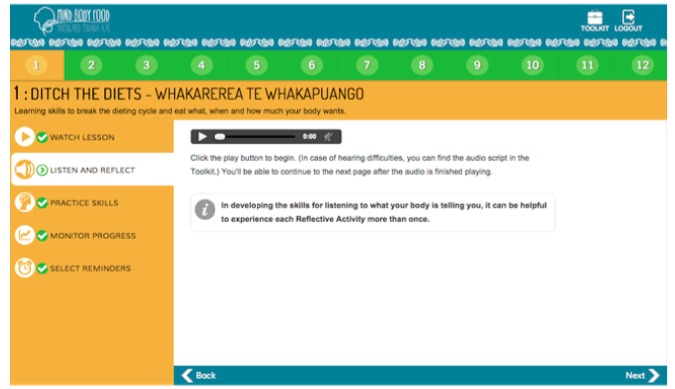
Audio activity.
Figure 4.
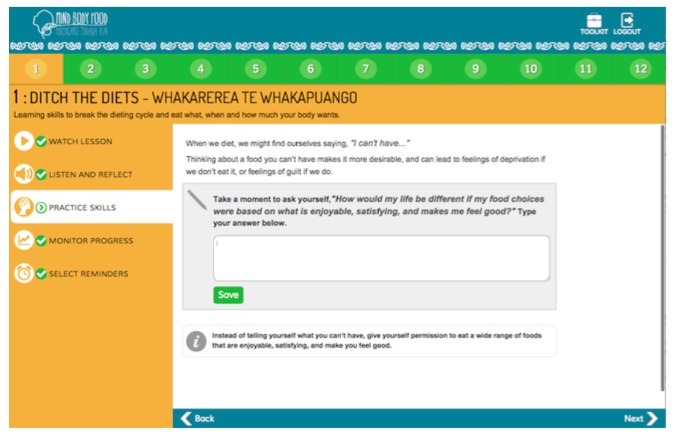
Typed activity.
Figure 5.
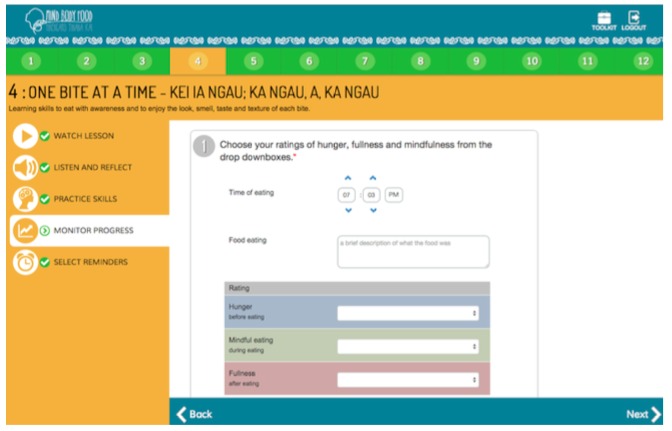
Eating Awareness Tracker (EAT) self-monitoring tool.
Procedures
During the initial contact, a preliminary check of eligibility criteria was conducted. Preliminary screening criteria included premenopausal status, 40 to 50 years of age, and BMI greater than 26.5 kg/m2 based on self-reported height and weight. Women satisfying initial eligibility criteria were then emailed a Web-based screening questionnaire to evaluate exclusion criteria and Participant Information and Consent Form. Women who satisfied all inclusion and exclusion criteria were invited to participate in the study and were asked to complete the preintervention assessment by visiting the clinic located on campus. Women who did not meet eligibility criteria were offered a list of nondieting resources (eg, books, websites).
At the preintervention assessment, participants provided informed consent and upon enrollment in the study were assigned a username and passcode. At this time, they were given a brief tour of a module to familiarize them with the Web application. An intervention evaluation was completed online after the 12th module or during the postintervention clinic visit. At the final clinic visit, participants received a $20 grocery voucher as reimbursement for their costs in traveling to measurement sessions.
Measures
Usage
Google Analytics [44] was used to record usage data for measuring the mean number of modules completed and mean session duration (one session was defined as a group of interactions with “Mind, Body, Food” until a log-out action or a period of 30 minutes of inactivity). User identification tracking (using email addresses at log-in) was enabled in Google Analytics to show data from individual users. The total number of modules completed was determined by the exit page (the last page a user viewed before exiting “Mind, Body, Food”) for each participant over the course of the study to identify the highest module number viewed. EAT usage was determined by the mean number of weeks participants saved at least one EAT entry to a secure online database over the 14-week trial. To determine if illness or technical difficulties affected EAT usage, all participants were asked in the postintervention questionnaire to report if for more than five days over the past 14 weeks their appetite had been affected or if their access to “Mind, Body, Food” had been limited.
Acceptability
A 32-item Web-delivered postintervention evaluation was developed to assess the acceptability of “Mind, Body, Food.” Acceptability questions were informed by the technology acceptance model [45] and focused on perceived usefulness (ie, the extent that using “Mind, Body, Food” enhances one’s ability to learn intuitive eating skills), ease of use, and user satisfaction. Questions such as “Overall, to what extent was ‘Mind, Body, Food’ useful to you?” were answered using 5-point Likert-type items (1—not useful to 5—extremely useful).
Participant Pre-, Post-, and 3-Month Follow-Up Characteristics
Paper-based questionnaires were administered during the preintervention assessment (62 items) and during both postintervention and 3-month follow-up assessments (56 items). All questionnaires were checked for completeness during the clinic visit, and participants were asked to answer any missed questions at that time.
The 23-item IES-2 [14] was used to measure women’s tendency to eat intuitively. The subscales measure eating for physical rather than emotional reasons, unconditional permission to eat, reliance on hunger and satiety cues to guide eating, and body-food choice congruence (eg, choosing to eat foods that provide energy and stamina). Statements (eg, “I trust my body to tell me when to eat”) were rated using subscales comprising 5-point Likert-type items (1—strongly disagree to 5—strongly agree). Providing evidence of its construct validity, the IES-2 total score and subscale scores have been positively related to body appreciation, self-esteem, and satisfaction with life and inversely related to eating disorder symptomology, poor interoceptive awareness, body surveillance, body shame, BMI, and internalization of media appearance ideals among women [14]. The IES-2 has also been found to yield internally consistent and stable scores with samples of women, providing evidence of reliability [14]. Preintervention, postintervention and 3-month follow-up IES-2 total score Cronbach alphas were .86, .90, and .91, respectively. Of the IES-2 subscales, all Cronbach alphas were .74 or higher (considered to be acceptable [46]) with three exceptions: preintervention Body-Food Choice Congruence subscale, postintervention and 3-month follow-up Unconditional Permission to Eat subscale Cronbach alphas were .61, .60, and .64, respectively.
Two questions were adapted from the Eating Disorder Examination-Screening Version (EDE-S) [47] to measure recent binge eating behavior. The first question asked, “Over the past 4 weeks (28 days), have there been any times when you have eaten what other people would regard as an unusually large amount of food?” to which participants were asked to respond Yes or No. Responses to this question were used to create a dichotomous variable (ie, binge eating vs no binge eating). The second question asked, “On how many days out of the last 28 have you had episodes like this when you may have also felt either unable to prevent them or unable to stop them once they had started?” Participants were asked to respond with the number of days. The EDE-S has high sensitivity (.90-.94) and specificity (.80-.96) in detecting eating disorders in community samples [47].
Height and weight were measured to calculate BMI for investigating preliminary effectiveness for weight gain prevention. A trained research assistant measured height to the nearest 0.1 centimeters using a stadiometer. Shoes were removed prior to the measurement. Weight was measured to the nearest 0.1 kilogram using a standard electronic scale while participants wore light clothing. Both height and weight were measured twice at each assessment and the mean values were used.
ACT-based processes (ie, psychological flexibility) were measured using the 7-item Acceptance and Action Questionnaire-II (AAQ-II) [48]. Items such as “My painful experiences and memories make it difficult for me to live a life that I would value” were answered using 7-point Likert-type items (1—never true to 7—always true). Higher scores reflected higher psychological inflexibility. The AAQ-II has good validity and reliability with various samples including college students and community-based adults [48]. Preintervention, postintervention, and 3-month follow-up AAQ-II scores had excellent Cronbach alphas (.91, .92, and .94, respectively).
Quality of life was measured by the Short Form 12-item Health Survey (SF-12v2) [49]. The SF-12v2 assesses eight domains of health, which are collapsed into two component summary measures of health: physical (incorporating Physical Functioning, Role-Physical, Bodily Pain, and General Health subscales) and mental (incorporating Vitality, Social Functioning, Role-Emotional, and Mental Health subscales) [50]. The component summaries have good reliability and validity among large community samples [51]. Preintervention, postintervention and 3-month follow-up SF-12v2 scores had acceptable Cronbach alphas (for physical summary measure: .79, .87, and .78, respectively; for mental summary measure: .84, .85, and .83, respectively).
Items assessing ethnicity, highest educational level, occupation status, and employment status were obtained from Statistics NZ’s Census 2006 [52]. Ethnicity data were used to assign responders to one of five categories in the following order: Māori, Pacific Islander, Asian, Other and NZ European. Occupational status was used to assess socioeconomic status using the NZ Socioeconomic Index (NZSEI-06) [53]. Classification codes were retrieved from an online searchable database provided by Statistics New Zealand to identify the appropriate NZSEI-06 score [53]. When participants recorded a partner’s occupation, the higher index score among the two was used to estimate household socioeconomic status. NZSEI-06 scores range from 10 to 90 with higher scores indicating higher socioeconomic status.
Statistical Analysis
Mainly descriptive analyses were conducted due to the exploratory nature of the pilot study. Analyses were conducted using all available data. Means and standard deviations (SDs) for continuous variables and frequencies and percentages for categorical variables were calculated to describe the study sample. Analyses of differences between those completing and not completing the study and the within-group changes during the intervention were performed according to modified intention-to-treat principles, including all eligible women with available data but irrespective of their degree of participation with the intervention. Chi-squared tests and two sample t tests examined whether baseline characteristics predicted retention. Paired t and Wilcoxon matched-pairs signed-rank tests were performed to assess the overall significance of within-group changes over time among continuous variables, and McNemar tests were used in the same way for categorical variable comparisons. Spearman correlations were used to assess associations between changes from preintervention to postintervention in each of total IES-2 scores, the four IES subscale scores, BMI, and AAQ-II scores. Statistical analyses were performed using Stata 11.2 software (StataCorp LP) using 2-sided tests with the level of statistical significance set at P<.05.
Results
Recruitment and Retention
During recruitment, of the 97 women who expressed interest in the study, 75 women met preliminary screening criteria and subsequently were invited to complete the online eligibility assessment. Five women did not complete the online eligibility assessment, and only 45 women met the study inclusion criteria (see Figure 6 for reasons women were excluded). A total of 40 women were enrolled in the study from August to September 2014. The postintervention retention rate was 65% (26/40) and 63% (25/40) at the 3-month follow-up. Although the attrition rate was similar to that predicted (30%), the sample size at follow-up was lower than had been aimed for due to the number of women not meeting eligibility criteria. Figure 6 presents the flow of participants through the study.
Figure 6.
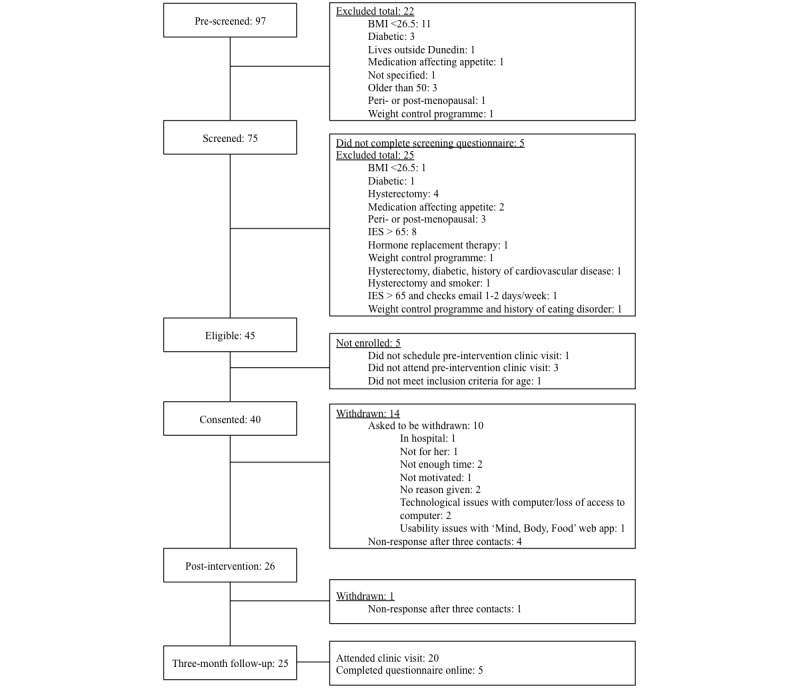
"Mind, Body, Food" study participant flow diagram.
Baseline Characteristics
Table 2 presents the sample’s demographic characteristics at baseline in comparison with corresponding NZ Census data. The sample was overrepresentative of NZ European women (30/37, 81.1% vs 69.8%) but similarly representative of Māori (4/37, 10.8% vs 11.7%) and Pacific (1/37, 2.7% vs 4.4%) women. University-educated women were overrepresented (21/37, 56.8% vs 17.7%). Women with NZSEI-06 (estimating socioeconomic status) scores in the lower two quartiles were underrepresented (10-33: 2/37, 5.4% vs 23.1%, 34-44: 3/37, 8.1% vs 29.4%). Half (18/36, 50.0%) of women reported dieting for 20 years or longer. There were no statistically significant differences in demographic characteristics or other measures such as intuitive eating, binge eating, general mental health, psychological inflexibility, and BMI between women who were retained and not retained at 3-month follow-up.
Table 2.
Baseline characteristics of “Mind, Body, Food” participants (n=40).
| Characteristic | All participants | National data | |
| Age, years, mean | 44.8 | — | |
| IES-1a summed total score [17], mean | 53.4 | 69.4 | |
| Ethnicity [54], %b | |||
|
|
New Zealand European | 81.1 | 69.8 |
|
|
Māori | 10.8 | 11.7 |
|
|
Pacific | 2.7 | 4.4 |
|
|
Other | 5.4 | 4.6 |
| Highest level of education attained [54], %b | |||
|
|
Secondary school or less | 16.2 | 59.1 |
|
|
Technical/trade school or polytechnic | 27.0 | 23.2 |
|
|
University | 56.8 | 17.7 |
| Employment [55], %b | |||
|
|
Employed | 89.2 | 81.2-81.8 |
|
|
Employed full time | 59.5 | — |
|
|
Employed part time | 29.7 | — |
|
|
Homemaker | 5.4 | — |
|
|
Other | 5.4 | — |
| Socioeconomic status (NZSEI-06)c [56], %b | |||
|
|
62-90 (higher socioeconomic status) | 48.6 | 26.0 |
|
|
45-61 | 37.8 | 21.5 |
|
|
34-44 | 8.1 | 29.4 |
|
|
10-33 (lower socioeconomic status) | 5.4 | 23.1 |
| BMId (kg/m2) [57], mean | 32.92 | 27.8 | |
| IES-2e total, mean | 2.53 | — | |
|
|
UPEf, mean | 3.06 | — |
|
|
EPRg, mean | 2.17 | — |
|
|
RHSh, mean | 2.33 | — |
|
|
B-FCCi, mean | 2.85 | — |
| AAQ-IIj, mean | 22.01 | — | |
| PCSk, mean | 50.01 | — | |
| MCSl, mean | 46.32 | — | |
| Binge eating, %m | |||
|
|
Yes | 46.2 | — |
|
|
No | 53.8 | — |
| Dieting history, %n | |||
|
|
0-4 years | 27.8 | — |
|
|
5-19 years | 22.2 | — |
|
|
20+ years | 50.0 | — |
aIES-1: Intuitive Eating Scale-1 (summed scores have potential range 21-105).
bMissing data, n=3.
cNew Zealand Socioeconomic Index.
dBMI: body mass index.
eIES-2: Intuitive Eating Scale-2 (mean scores have potential range 1-5).
fUPE: Unconditional Permission to Eat subscale.
gEPR: Eating for Physical Rather than Emotional Reasons subscale.
hRHS: Reliance on Internal Hunger and Satiety cues.
iB-FCC: Body-Food Choice Congruence.
jAAQ-II: Acceptance and Action Questionnaire-II.
kPCS: Short Form 12-item (version 2) Health Survey Physical Component Summary.
lMCS: Short Form 12-item (version 2) Health Survey Mental Component Summary.
mMissing data, n=1.
nMissing data, n=4.
Usage During the 14-week Intervention
Google Analytics recorded “Mind, Body, Food” online traffic for 37 participants for 92 days at the end of the 14-week trial. A programming delay prevented monitoring from the start of the study, which explains missing usage data for three women. Of the 37 participants for whom usage data were available, 12 (32%) completed all 12 modules, 11 (30%) completed 7 to 11 modules, 12 (32%) completed 1 to 6 modules, and two women (5%) completed no modules. The median number of modules completed was 7.5 (interquartile range [IQR] 2-12) modules. The median number of sessions during the monitored period was 7 (a minimum of 1 session to a maximum of 66 sessions). The median session duration during the monitored period was 12 minutes, 54 seconds (a minimum of 3 minutes, 58 seconds, to a maximum of 100 minutes, 8 seconds). The median number of EAT entries over the 14-week intervention was 7 (a minimum of 1 entry to a maximum of 314 entries). The median number of weeks that participants recorded eating experiences in the EAT was 3 (IQR 1-9) weeks. Of the 40 participants enrolled in the study, 4 women (10%) used the EAT for at least 12 weeks of their intervention period, 7 (18%) used the EAT for 7 to 11 weeks, 20 (50%) used the EAT for 1 to 6 weeks, and 9 (23%) did not use the EAT during their intervention period.
Eleven women had limited access to “Mind, Body, Food” for more than 5 days, predominantly due to being away from home (n=8) or technical issues (n=3). Technical issues that prevented module completion included attempting to access “Mind, Body, Food” from an incompatible browser (n=3), using incorrect login details (n=1), and other issues not described (n=1). Seven women reported appetite being affected for more than 5 days (eg, due to illness) during the 14-week intervention.
Acceptability
A total of 26 women completed acceptability measures, and of these 12 had completed all modules, 10 completed 7 to 11 modules, and 4 completed 2 to 6 modules. Table 3 shows that participants’ overall impression of “Mind, Body, Food” was positive. Most participants liked “Mind, Body, Food” and found the intervention useful (20/26, 77%), easy to use (17/25, 68%), easy to understand (23/25, 92%), and would recommend the program to others (21/25, 84%). Nearly half (12/25, 48%) of participants reported that “Mind, Body, Food” made it easy to learn intuitive eating skills.
Table 3.
User experiences of “Mind, Body, Food” (n=26).
| Acceptability measures | n (%) | Median | ||
| Overall impression | ||||
|
|
Overall, to what extent did you like “Mind, Body, Food?” | 4 | ||
|
|
|
Disliked very much | 0 (0) |
|
|
|
|
Disliked somewhat | 0 (0) |
|
|
|
|
Neither liked nor disliked | 3 (12) |
|
|
|
|
Liked somewhat | 10 (40) |
|
|
|
|
Liked very much | 12 (48) |
|
|
|
|
Missing | 1 |
|
|
|
Overall, to what extent was “Mind, Body, Food” useful to you? | 4 | ||
|
|
|
Not useful | 0 (0) |
|
|
|
|
A little useful | 2 (8) |
|
|
|
|
Somewhat useful | 4 (15) |
|
|
|
|
Quite useful | 9 (35) |
|
|
|
|
Extremely useful | 11 (42) |
|
|
|
Overall, to what extent did you find “Mind, Body, Food” easy to use? | 4 | ||
|
|
|
Not at all easy | 0 (0) |
|
|
|
|
Not very easy | 3 (12) |
|
|
|
|
Somewhat easy | 5 (20) |
|
|
|
|
Very easy | 12 (48) |
|
|
|
|
Extremely easy | 5 (20) |
|
|
|
|
Missing | 1 |
|
|
|
Overall, to what extent did you find “Mind, Body, Food” content easy to understand? | 4 | ||
|
|
|
Not at all easy | 0 (0) |
|
|
|
|
Not very easy | 0 (0) |
|
|
|
|
Somewhat easy | 2 (8) |
|
|
|
|
Very easy | 15 (60) |
|
|
|
|
Extremely easy | 8 (32) |
|
|
|
|
Missing | 1 |
|
|
|
Overall, to what extent did “Mind, Body, Food” make it easy for you to learn intuitive eating skills? | 3 | ||
|
|
|
Not at all easy | 0 (0) |
|
|
|
|
Not very easy | 2 (8) |
|
|
|
|
Somewhat easy | 11 (44) |
|
|
|
|
Very easy | 9 (36) |
|
|
|
|
Extremely easy | 3 (12) |
|
|
|
|
Missing | 1 |
|
|
|
Would you recommend “Mind, Body, Food” to others? | 5 | ||
|
|
|
No, definitely wouldn’t | 0 (0) |
|
|
|
|
No, probably wouldn’t | 0 (0) |
|
|
|
|
Unsure | 4 (16) |
|
|
|
|
Yes, probably would | 8 (32) |
|
|
|
|
Yes, definitely would | 13 (52) |
|
|
|
|
Missing | 1 |
|
| Usefulness of program features | ||||
|
|
How useful did you find the videos? | 4 | ||
|
|
|
Not useful | 0 (0) |
|
|
|
|
A little useful | 4 (16) |
|
|
|
|
Somewhat useful | 4 (16) |
|
|
|
|
Quite useful | 7 (28) |
|
|
|
|
Extremely useful | 10 (40) |
|
|
|
|
Missing | 1 |
|
|
|
How useful did you find the audio activities? | 3 | ||
|
|
|
Not useful | 4 (16) |
|
|
|
|
A little useful | 5 (20) |
|
|
|
|
Somewhat useful | 7 (28) |
|
|
|
|
Quite useful | 7 (28) |
|
|
|
|
Extremely useful | 2 (8) |
|
|
|
|
Missing | 1 |
|
|
|
How useful did you find the typed activities? | 3 | ||
|
|
|
Not useful | 4 (16) |
|
|
|
|
A little useful | 3 (12) |
|
|
|
|
Somewhat useful | 11 (44) |
|
|
|
|
Quite useful | 4 (16) |
|
|
|
|
Extremely useful | 3 (12) |
|
|
|
|
Missing | 1 |
|
|
|
How useful did you find the E.A.T.? | 2 | ||
|
|
|
Not useful | 5 (21) |
|
|
|
|
A little useful | 9 (38) |
|
|
|
|
Somewhat useful | 5 (21) |
|
|
|
|
Quite useful | 3 (13) |
|
|
|
|
Extremely useful | 2 (8) |
|
|
|
|
Missing | 2 |
|
|
|
How useful did you find the email reminders to begin the next module? | 3 | ||
|
|
|
Not useful | 2 (8) |
|
|
|
|
A little useful | 1 (4) |
|
|
|
|
Somewhat useful | 5 (20) |
|
|
|
|
Quite useful | 9 (36) |
|
|
|
|
Extremely useful | 8 (32) |
|
|
|
|
Missing | 1 |
|
Of all module components, the videos were more frequently rated as being quite or extremely useful by participants compared to the audio and typed activities (Table 3). Five out of 24 women (21%) women rated the EAT self-monitoring tool as quite or extremely useful, 3 out of 19 women (16%) found email reminders to use the EAT useful, and 4 out of 12 women (33%) found SMS reminders to use the EAT useful (not shown). In regards to reminders sent to begin the next module, 17 out of 26 women (68%) rated the email reminders as quite or extremely useful. Of the women (9/24, 38%) who chose to receive SMS reminders to begin the next module, 6 (67%) rated the reminders as useful (not shown).
Of the 20 women who currently owned a smartphone, 16 (80%) reported that if it were available a mobile version of “Mind, Body, Food” would be quite or extremely useful to them.
Changes in Eating Behavior
The study was not designed to detect the effects of the intervention on the outcome measures (no control group was included), but within-group comparisons were performed as part of the feasibility component of the pilot study. From pre- to postintervention, there were statistically significant increases in IES-2 total scores and all four IES-2 subscale scores (Table 4). There was no evidence that these improvements diminished at the 3-month follow-up. Based on use of the dichotomous variable (ie, binge eating vs no binge eating), 7 out of 14 women who reported eating a significantly large amount of food (ie, binge eating) at the preintervention assessment reported no binge eating at the postintervention assessment. There were no women who transitioned from no binge eating at the preintervention assessment to binge eating at the postintervention assessment or at the 3-month follow-up; 4 women who reported binge eating at postintervention no longer reported binge eating at the 3-month follow-up. McNemar’s test revealed a significant decrease in the proportion of women binge eating from the pre- to postintervention visits (P=.01) and a significant decrease from postintervention to follow-up (P<.001). The median days women who were categorized as binge eaters reported binge eating at preintervention was 4.25 (IQR 2.5-10) days, at postintervention was 4 (IQR 2-8) days, and at the 3-month follow-up it was 2 (IQR 2-4) days. A Wilcoxon matched-pairs signed-rank test was used to examine changes in the reported number of days women were unable to prevent or stop episodes of eating an unusually large amount of food and revealed a significant decrease from pre- to postintervention (P=.03) and no evidence of a change from postintervention to follow-up (P=.57).
Table 4.
Changes from pre- (n=26) to postintervention (n=26) and from postintervention to 3-month follow-up (n=25).
| Characteristic | Mean (SD) | Change (SD)a | 95% CI | P valueb | |
| IES-2c total | |||||
|
|
Preintervention | 2.54 (0.58) | — | — | — |
|
|
Postintervention | 3.45 (.55) | 0.94 (0.67) | 0.67, 1.21 | <.001 |
|
|
3-month follow-up | 3.53 (.61) | 0.08 (0.55) | −0.15, 0.31 | .47 |
| UPEd | |||||
|
|
Preintervention | 3.07 (0.73) | — | — | — |
|
|
Postintervention | 3.56 (.54) | 0.52 (0.87) | 0.17, 0.87 | .01 |
|
|
3-month follow-up | 3.47 (.58) | −0.09 (0.64) | −0.36, 0.17 | .76 |
| EPRe | |||||
|
|
Preintervention | 2.19 (0.96) | — | — | — |
|
|
Postintervention | 3.21 (.89) | 1.08 (0.96) | 0.69, 1.46 | <.001 |
|
|
3-month follow-up | 3.49 (.88) | 0.28 (0.89) | −0.09, 0.65 | .13 |
| RHSf | |||||
|
|
Preintervention | 2.33 (0.77) | — | — | — |
|
|
Postintervention | 3.58 (.76) | 1.28 (0.98) | 0.89, 1.68 | <.001 |
|
|
3-month follow-up | 3.55 (.81) | −0.03 (0.68) | −0.31, 0.25 | .81 |
| B-FCCg | |||||
|
|
Preintervention | 2.87 (0.61) | — | — | — |
|
|
Postintervention | 3.59 (.81) | 0.74 (0.61) | 0.50, 1.00 | <.001 |
|
|
3-month follow-up | 3.72 (.72) | 0.13 (0.87) | −0.23, 0.49 | .45 |
| BMIh (kg/m2) | |||||
|
|
Preintervention | 32.93 (4.85) | — | — | — |
|
|
Postintervention | 32.81 (5.31) | −0.13 (0.88) | −0.48, 0.23 | .46 |
|
|
3-month follow-upi | 32.80 (5.29) | −0.01 (0.57) | −0.28, 0.26 | .93 |
| AAQ-IIj | |||||
|
|
Preintervention | 22.46 (8.67) | — | — | — |
|
|
Postintervention | 18.23 (8.14) | −4.23 (7.13) | −7.11, -1.35 | .006 |
|
|
3-month follow-up | 16.08 (7.73) | −2.60 (6.58) | −5.32, 0.16 | .06 |
| SF-12v2 PCSk | |||||
|
|
Preintervention | 50.46 (7.83) | — | — | — |
|
|
Postintervention | 50.87 (11.02) | 0.29 (9.35) | −3.49, 4.06 | .88 |
|
|
3-month follow-up | 52.13 (6.78) | 1.26 (10.46) | −3.06, 5.58 | .55 |
| SF-12v2 MCSl | |||||
|
|
Preintervention | 45.63 (6.31) | — | — | — |
|
|
Postintervention | 50.24 (7.41) | 5.07 (6.31) | 2.52, 7.61 | <.001 |
|
|
3-month follow-up | 53.70 (4.99) | 3.45 (7.71) | 0.27, 6.63 | .03 |
aChanges from pre- to postintervention and postintervention to 3-month follow-up.
bPaired t tests were used to compare IES-2 scores, BMI, AAQ-II scores, and SF-12v2 scores.
cIES-2: Intuitive Eating Scale-2.
dUPE: Unconditional Permission to Eat subscale.
eEPR: Eating for Physical Rather than Emotional Reasons subscale.
fRHS: Reliance on Internal Hunger and Satiety cues.
gB-FCC: Body-Food Choice Congruence.
hBMI: body mass index.
iBMI change from postintervention to 3-month follow-up (n=20).
jAAQ-II: Acceptance and Action Questionnaire-II.
kPCS: Short Form 12-item (version 2) Health Survey Physical Component Summary.
lMCS: Short Form 12-item (version 2) Health Survey Mental Component Summary.
Psychological Inflexibility, Quality of Life, and BMI
Psychological inflexibility decreased significantly from pre- to postintervention (mean change −4.23 [SD 7.13], P=.006), and there was a tendency for a further decrease in psychological inflexibility from postintervention to 3-month-follow-up (mean change −2.60 [SD 6.58], P=.06) (Table 4). There were no significant changes in general physical health from pre- to postintervention (pre- to postintervention PCS scores: mean change 0.29 [SD 9.35], P=.88; postintervention to 3-month follow-up PCS scores: mean change 1.26 [SD 10.46], P=.55). However, general mental health improved significantly from pre- to postintervention with a further improvement postintervention to 3-month follow-up (mean change 5.07 [SD 6.31], P<.001; mean change 3.45 [SD 7.71], P=.03, respectively). There were no statistically significant changes in BMI from pre- to postintervention or postintervention to 3-month follow-up (mean change −0.13 [SD 0.88], P=.46 and mean change −0.01 [SD 0.57], P=.93, respectively).
Associations Between Changes in Intuitive Eating With BMI and Psychological Inflexibility
Spearman correlations showed a statistically significant inverse relationship between pre- to postintervention change in total intuitive eating scores and pre- to postintervention change in BMI (rs=−.43, P=.03). Thus, greater decreases in BMI were associated with greater increases in intuitive eating. However, when relationships with individual subscales were examined, a significant association was found for only one subscale: greater decreases in BMI were associated with greater increases in eating for physical rather than emotional reasons (rs=−.56, P=.003). There was also a statistically significant inverse relationship between change in psychological inflexibility scores and change in intuitive eating scores (rs=−.52, P=.006); that is, greater improvements in psychological flexibility were associated with greater increases in total intuitive eating scores. Furthermore, larger improvements in psychological flexibility were associated with greater increases in two subscale scores: eating for physical rather than emotional reasons (rs=−.41, P=.04) and reliance on hunger and satiety cues (rs=−.62, P<.001). A greater reduction in psychological inflexibility scores was also associated with a greater decrease in BMI (r=.41, P=.04).
Discussion
Principal Findings
This pilot study is the first evaluation of an online intuitive eating intervention and demonstrated that middle-aged overweight women perceived the intervention to be an acceptable and useful way to learn intuitive eating skills. Among those women who completed all assessments, both psychological flexibility and all aspects of intuitive eating improved at the end of the intervention and were sustained at the 3-month follow-up. Binge eating and general mental health improved from preintervention to postintervention and there were further improvements in these outcomes at the 3-month follow-up. Results are consistent with the hypothesis that improvements in psychological flexibility may be linked with eating more intuitively.
To our knowledge, only one other published intuitive eating intervention (a face-to-face intervention) [58] has shown improvements in all aspects of intuitive eating (ie, unconditional permission to eat when hungry and what food is desired, eating for physical reasons, trusting bodily cues to determine when and how much to eat), as has been demonstrated in this pilot study. An innovative feature and major strength of the present study is the integration of intuitive eating with ACT skills. Many ACT skills are designed to build awareness and acceptance of internal experiences, which may in turn foster the ability to tune into and trust the body’s hunger and satiety cues and not react to emotions and cravings by eating. ACT’s focus on values- guided behavior may strengthen women’s commitment to eating intuitively by helping them to clarify the value of shifting to eating behavior that is enjoyable, sustainable, empowering, and health-focused rather than weight-focused. The ACT elements of the intervention may have also improved nonjudgment towards thoughts about food or feelings about one’s body and reduced reactivity towards experiences (ie, responding to internal and external experiences in deliberate and meaningful ways). Furthermore, the significant increase in psychological flexibility suggests the ACT strategies were active in the intervention. This study demonstrates support for and justifies further exploration of our innovative approach of integrating intuitive eating with ACT.
The significant reduction in binge eating behavior in this study is consistent with previous intuitive eating interventions [19] and ACT-based interventions [25,27]. Those who learn intuitive eating appear to be able to reduce the loss of control that often follows self-imposed restriction [18], and this ability may be enhanced by improved coping with emotional distress through development of ACT skills.
Improvements in women’s general mental health may be explained by the ACT-based skills taught in “Mind, Body, Food;” however, intuitive eating interventions which do not specifically incorporate ACT skills have also been reported to improve psychological well-being [18]. Enhanced awareness and being less judgmental may have benefited women in areas of life beyond their eating experiences, allowing them to respond to situations in more personally meaningful ways. Physical activity was not addressed until the tenth module, which was viewed by a minority of participants, and this may contribute to the absence of changes in general physical health.
It is encouraging that numerous improvements occurred in spite of only 30% of the sample completing all 12 modules. Low completion rates are typical of Web-based interventions [43,59,60]. A systematic review of trials of Web-based health promotion interventions reported that on average 50% (minimum 1%; maximum 93%) of study participants completed all intervention modules (with interventions typically 10 modules long and meant to be used once a week) [60]. However, in this review, 76% of the interventions included interaction of the participant with a counselor, a factor which predicted significantly better adherence [60] but was lacking in our “Mind, Body, Food” intervention. A recent Web-based weight gain prevention intervention more similar to ours has reported the percentage of women completing all modules to be lower than in our study [61]. Low completion rates in such interventions, including our own, may reflect waning interest, perceiving the early modules of the intervention as sufficiently useful for learning new skills and thereby feeling it unnecessary to complete the rest, or a lack of social support [62]. Further investigation could assist in determining how many and which combination of modules are associated with optimal improvement in intuitive eating prior to a future RCT. Another contributor to noncompletion may be the desire for weight loss rather than a shift in focus towards long-term healthier lifestyle behaviors [62], particularly among women starting at a higher BMI [63] or among those with high body dissatisfaction.
Low use of the EAT and the importance of self-monitoring to successful behavior change [64-66] suggest that simplification and improvement of the self-monitoring tool is needed. In response to feedback from target users during intervention development, women had to choose to receive reminders to use the EAT rather than receiving automatic reminders, and this may also have contributed to low usage. However, the reported improvements in intuitive eating and binge eating may suggest that for some women, a self-monitoring tool may not have been essential for learning intuitive eating.
Strengths and Limitations
The study strengths include an intervention that integrates two empirically tested approaches to eating behavior change (intuitive eating and ACT), use of an intervention design that was informed by input from end-users and underwent rigorous pretesting with women in the target audience prior to the pilot study; objective measures of BMI and intervention usage; validated measures of intuitive eating, binge eating, psychological flexibility, and quality of life; and a 3-month follow-up. The most significant limitations of the study were the lack of a comparison group, small sample size, analyses conducted on the subset of participants who were exposed to the intervention and had not dropped out for any reason, and delayed monitoring via Google Analytics; however, the pilot study was undertaken to inform improvements to the intervention prior to proceeding to an RCT incorporating a control group. The pilot study shared the high attrition common to many Web-based interventions and results were based on a small group completing the study. The high rate of attrition observed during the study (35% were lost by postintervention and 37% by 3-month follow-up) and the expectation that missing data from health-focused studies involving overweight participants will generally be informative means that we cannot be certain that those dropping out did not experience negative outcomes that could attenuate or even negate the positive findings reported here. Prior to a future randomized trial, further research is needed to determine ways to increase engagement and improve program completion. This may be achieved by making the tool smartphone compatible since accessing the program on the go is likely to be helpful to women in applying the skills in real-world settings. A reduction in the number of modules may also be useful. The sample was overrepresentative of highly educated women, which has been noted in several studies of Web-based weight management interventions [67-69], and results may not generalize to less educated women. The positive self-reported outcomes may reflect regression to the mean, repeated administration of the questionnaires, or social desirability bias.
Conclusion
To our knowledge, “Mind, Body, Food” is the first intervention to combine teaching intuitive eating skills and ACT-based strategies for behavior change. It is also the first Web-based intuitive eating intervention. The “Mind, Body, Food” intervention was generally acceptable to the target audience, and the pilot study showed improvements in intuitive eating, binge eating behavior, psychological flexibility and general mental health, in addition to weight maintenance. Given the 3-month follow-up period and lack of a control group, it is important that an improved version of the intervention is evaluated in an RCT to investigate its longer-term effectiveness. The RCT will also examine the hypothesized mechanism that greater psychological flexibility leads to more intuitive eating, which leads to prevention of weight gain.
Acknowledgments
The work was funded by a Performance-Based Research Fund grant from the Department of Human Nutrition, University of Otago, and a University of Otago Postgraduate Publishing Bursary (Doctoral) from the Graduate Research Committee. Thank you to James Case for Web design and programming, the authors who kindly shared their work with us during intervention development (Susan Albers, Meghan Butryn, Evan Forman, Ellen Frankel, Russ Harris, Steven Hayes, Judith Matz, Elyse Resch, Evelyn Tribole), and to the study participants.
Abbreviations
- AAQ-II
Acceptance and Action Questionnaire
- ACT
acceptance and commitment therapy
- B-FCC
body-food choice congruence
- BMI
body mass index
- EAT
Eating Awareness Tracker
- EDE-S
Eating Disorder Examination-Screening Version
- EPR
eating for physical rather than emotional reasons
- IES
Intuitive Eating Scale
- IES-2
Intuitive Eating Scale-2
- IQR
interquartile range
- MCS
Mental Component Summary
- NZSEI-06
New Zealand Socioeconomic Index
- PCS
Physical Component Summary
- RCT
randomized controlled trial
- RHS
reliance on internal hunger and satiety cues
- SD
standard deviation
- SES
socioeconomic status
- SF-12v2
Short Form 12-item (version 2) Health Survey
- SMS
short message service
- UPE
unconditional permission to eat
Footnotes
Conflicts of Interest: None declared.
References
- 1.Williams L, Germov J, Young A. Preventing weight gain: a population cohort study of the nature and effectiveness of mid-age women's weight control practices. Int J Obes (Lond) 2007 Jun;31(6):978–986. doi: 10.1038/sj.ijo.0803550.0803550 [DOI] [PubMed] [Google Scholar]
- 2.Yaemsiri S, Slining MM, Agarwal SK. Perceived weight status, overweight diagnosis, and weight control among US adults: the NHANES 2003-2008 Study. Int J Obes (Lond) 2011 Aug;35(8):1063–1070. doi: 10.1038/ijo.2010.229.ijo2010229 [DOI] [PubMed] [Google Scholar]
- 3.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF, Abraham JP, Abu-Rmeileh NM, Achoki T, AlBuhairan FS, Alemu ZA, Alfonso R, Ali MK, Ali R, Guzman NA, Ammar W, Anwari P, Banerjee A, Barquera S, Basu S, Bennett DA, Bhutta Z, Blore J, Cabral N, Nonato IC, Chang J, Chowdhury R, Courville KJ, Criqui MH, Cundiff DK, Dabhadkar KC, Dandona L, Davis A, Dayama A, Dharmaratne SD, Ding EL, Durrani AM, Esteghamati A, Farzadfar F, Fay DF, Feigin VL, Flaxman A, Forouzanfar MH, Goto A, Green MA, Gupta R, Hafezi-Nejad N, Hankey GJ, Harewood HC, Havmoeller R, Hay S, Hernandez L, Husseini A, Idrisov BT, Ikeda N, Islami F, Jahangir E, Jassal SK, Jee SH, Jeffreys M, Jonas JB, Kabagambe EK, Khalifa SE, Kengne AP, Khader YS, Khang Y, Kim D, Kimokoti RW, Kinge JM, Kokubo Y, Kosen S, Kwan G, Lai T, Leinsalu M, Li Y, Liang X, Liu S, Logroscino G, Lotufo PA, Lu Y, Ma J, Mainoo NK, Mensah GA, Merriman TR, Mokdad AH, Moschandreas J, Naghavi M, Naheed A, Nand D, Narayan KM, Nelson EL, Neuhouser ML, Nisar MI, Ohkubo T, Oti SO, Pedroza A, Prabhakaran D, Roy N, Sampson U, Seo H, Sepanlou SG, Shibuya K, Shiri R, Shiue I, Singh GM, Singh JA, Skirbekk V, Stapelberg NJ, Sturua L, Sykes BL, Tobias M, Tran BX, Trasande L, Toyoshima H, van de Vijver S, Vasankari TJ, Veerman JL, Velasquez-Melendez G, Vlassov VV, Vollset SE, Vos T, Wang C, Wang X, Weiderpass E, Werdecker A, Wright JL, Yang YC, Yatsuya H, Yoon J, Yoon S, Zhao Y, Zhou M, Zhu S, Lopez AD, Murray CJ, Gakidou E. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014 Aug 30;384(9945):766–781. doi: 10.1016/S0140-6736(14)60460-8.S0140-6736(14)60460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88. doi: 10.1186/1471-2458-9-88. http://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-9-88 .1471-2458-9-88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Douketis JD, Macie C, Thabane L, Williamson DF. Systematic review of long-term weight loss studies in obese adults: clinical significance and applicability to clinical practice. Int J Obes (Lond) 2005 Oct;29(10):1153–1167. doi: 10.1038/sj.ijo.0802982.0802982 [DOI] [PubMed] [Google Scholar]
- 6.Franz MJ, VanWormer JJ, Crain AL, Boucher JL, Histon T, Caplan W, Bowman JD, Pronk NP. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007 Oct;107(10):1755–1767. doi: 10.1016/j.jada.2007.07.017.S0002-8223(07)01483-6 [DOI] [PubMed] [Google Scholar]
- 7.Dombrowski SU, Knittle K, Avenell A, Araújo-Soares V, Sniehotta FF. Long term maintenance of weight loss with non-surgical interventions in obese adults: systematic review and meta-analyses of randomised controlled trials. BMJ. 2014;348:g2646. doi: 10.1136/bmj.g2646. http://www.bmj.com/cgi/pmidlookup?view=long&pmid=25134100 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: where do we go from here? Science. 2003 Feb 7;299(5608):853–855. doi: 10.1126/science.1079857.299/5608/853 [DOI] [PubMed] [Google Scholar]
- 9.Global action plan for the prevention and control of noncommunicable diseases 2013-2020. Geneva: World Health Organization; 2013. [2015-09-17]. http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf . [Google Scholar]
- 10.Brown WJ, Williams L, Ford JH, Ball K, Dobson AJ. Identifying the energy gap: magnitude and determinants of 5-year weight gain in midage women. Obes Res. 2005 Aug;13(8):1431–1441. doi: 10.1038/oby.2005.173. doi: 10.1038/oby.2005.173.13/8/1431 [DOI] [PubMed] [Google Scholar]
- 11.Macdonald HM, New SA, Campbell MK, Reid DM. Longitudinal changes in weight in perimenopausal and early postmenopausal women: effects of dietary energy intake, energy expenditure, dietary calcium intake and hormone replacement therapy. Int J Obes Relat Metab Disord. 2003 Jun;27(6):669–676. doi: 10.1038/sj.ijo.0802283.0802283 [DOI] [PubMed] [Google Scholar]
- 12.Wing RR, Matthews KA, Kuller LH, Meilahn EN, Plantinga PL. Weight gain at the time of menopause. Arch Intern Med. 1991 Jan;151(1):97–102. [PubMed] [Google Scholar]
- 13.Tylka TL. Development and psychometric evaluation of a measure of intuitive eating. J Couns Psychol. 2006;53(2):226–240. doi: 10.1037/0022-0167.53.2.226. [DOI] [Google Scholar]
- 14.Tylka TL, Kroon Van Diest AM. The Intuitive Eating Scale-2: item refinement and psychometric evaluation with college women and men. J Couns Psychol. 2013 Jan;60(1):137–153. doi: 10.1037/a0030893.2013-02249-006 [DOI] [PubMed] [Google Scholar]
- 15.Tribole E, Resch E. Intuitive eating: a revolutionary program that works. New York: St. Martin's Griffin; 2003. [Google Scholar]
- 16.Framson C, Kristal AR, Schenk JM, Littman AJ, Zeliadt S, Benitez D. Development and validation of the mindful eating questionnaire. J Am Diet Assoc. 2009 Aug;109(8):1439–1444. doi: 10.1016/j.jada.2009.05.006. http://europepmc.org/abstract/MED/19631053 .S0002-8223(09)00628-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Madden CE, Leong SL, Gray A, Horwath CC. Eating in response to hunger and satiety signals is related to BMI in a nationwide sample of 1601 mid-age New Zealand women. Public Health Nutr. 2012 Dec;15(12):2272–2279. doi: 10.1017/S1368980012000882.S1368980012000882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schaefer JT, Magnuson AB. A review of interventions that promote eating by internal cues. J Acad Nutr Diet. 2014 May;114(5):734–760. doi: 10.1016/j.jand.2013.12.024.S2212-2672(13)01896-0 [DOI] [PubMed] [Google Scholar]
- 19.Bacon L, Stern JS, Van Loan MD, Keim NL. Size acceptance and intuitive eating improve health for obese, female chronic dieters. J Am Diet Assoc. 2005 Jun;105(6):929–936. doi: 10.1016/j.jada.2005.03.011.S0002822305003226 [DOI] [PubMed] [Google Scholar]
- 20.Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005 Feb;6(1):67–85. doi: 10.1111/j.1467-789X.2005.00170.x.OBR170 [DOI] [PubMed] [Google Scholar]
- 21.Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005 Jul;82(1 Suppl):222S–225S. doi: 10.1093/ajcn/82.1.222S. http://www.ajcn.org/cgi/pmidlookup?view=long&pmid=16002825 .82/1/222S [DOI] [PubMed] [Google Scholar]
- 22.Forman EM, Butryn ML, Hoffman KL, Herbert JD. An Open Trial of an Acceptance-Based Behavioral Intervention for Weight Loss. Cognitive and Behavioral Practice. 2009 May;16(2):223–235. doi: 10.1016/j.cbpra.2008.09.005. [DOI] [Google Scholar]
- 23.Forman EM, Butryn ML, Juarascio AS, Bradley LE, Lowe MR, Herbert JD, Shaw JA. The mind your health project: a randomized controlled trial of an innovative behavioral treatment for obesity. Obesity (Silver Spring) 2013 Jun;21(6):1119–1126. doi: 10.1002/oby.20169. doi: 10.1002/oby.20169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Katterman SN, Goldstein SP, Butryn ML, Forman EM, Lowe MR. Efficacy of an acceptance-based behavioral intervention for weight gain prevention in young adult women. Journal of Contextual Behavioral Science. 2014 Jan;3(1):45–50. doi: 10.1016/j.jcbs.2013.10.003. [DOI] [Google Scholar]
- 25.Lillis J, Hayes SC, Bunting K, Masuda A. Teaching acceptance and mindfulness to improve the lives of the obese: a preliminary test of a theoretical model. Ann Behav Med. 2009 Feb;37(1):58–69. doi: 10.1007/s12160-009-9083-x. [DOI] [PubMed] [Google Scholar]
- 26.Niemeier HM, Leahey T, Palm Reed K, Brown RA, Wing RR. An acceptance-based behavioral intervention for weight loss: a pilot study. Behav Ther. 2012 Jun;43(2):427–435. doi: 10.1016/j.beth.2011.10.005. http://europepmc.org/abstract/MED/22440077 .S0005-7894(11)00142-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tapper K, Shaw C, Ilsley J, Hill AJ, Bond FW, Moore L. Exploratory randomised controlled trial of a mindfulness-based weight loss intervention for women. Appetite. 2009 Apr;52(2):396–404. doi: 10.1016/j.appet.2008.11.012.S0195-6663(08)00618-1 [DOI] [PubMed] [Google Scholar]
- 28.Hayes SC, Strosahl K, Wilson KG. Acceptance and Commitment Therapy. An experiential approach to behavior change. New York: Guilford Press; 1999. p. 1572304812. [Google Scholar]
- 29.Forman EM, Butryn ML. A new look at the science of weight control: how acceptance and commitment strategies can address the challenge of self-regulation. Appetite. 2015 Jan;84:171–180. doi: 10.1016/j.appet.2014.10.004. http://europepmc.org/abstract/MED/25445199 .S0195-6663(14)00474-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sairanen E, Tolvanen A, Karhunen L, Kolehmainen M, Järvelä E, Rantala S, Peuhkuri K, Korpela R, Lappalainen R. Psychological flexibility and mindfulness explain intuitive eating in overweight adults. Behav Modif. 2015 Jul;39(4):557–579. doi: 10.1177/0145445515576402.0145445515576402 [DOI] [PubMed] [Google Scholar]
- 31.Murray E. Med 2.0. 2012. [2016-08-29]. Web-based interventions for behavior change and self-management: potential, pitfalls, and progress http://www.medicine20.com/2012/2/e3/
- 32.Wieland LS, Falzon L, Sciamanna CN, Trudeau KJ, Brodney S, Schwartz JE, Davidson KW. Interactive computer-based interventions for weight loss or weight maintenance in overweight or obese people. Cochrane Database Syst Rev. 2012;8:CD007675. doi: 10.1002/14651858.CD007675.pub2. http://europepmc.org/abstract/MED/22895964 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.ITU World Telecommunication/ICT Indicators Database. International Telegraph Union; 2015. [2015-11-12]. Core Household Indicators: Access to and use of ICT by households and individuals http://www.itu.int/en/ITU-D/Statistics/Documents/statistics/2016/CoreHouseholdIndicator.xls . [Google Scholar]
- 34.Hague AL, White AA. Web-based intervention for changing attitudes of obesity among current and future teachers. J Nutr Educ Behav. 2005;37(2):58–66. doi: 10.1016/s1499-4046(06)60017-1. [DOI] [PubMed] [Google Scholar]
- 35.Neve M, Morgan PJ, Jones PR, Collins CE. Effectiveness of web-based interventions in achieving weight loss and weight loss maintenance in overweight and obese adults: a systematic review with meta-analysis. Obes Rev. 2010 Apr;11(4):306–321. doi: 10.1111/j.1467-789X.2009.00646.x.OBR646 [DOI] [PubMed] [Google Scholar]
- 36.Hesser H, Gustafsson T, Lundén C, Henrikson O, Fattahi K, Johnsson E, Zetterqvist WV, Carlbring P, Mäki-Torkko E, Kaldo V, Andersson G. A randomized controlled trial of Internet-delivered cognitive behavior therapy and acceptance and commitment therapy in the treatment of tinnitus. J Consult Clin Psychol. 2012 Aug;80(4):649–661. doi: 10.1037/a0027021.2012-00872-001 [DOI] [PubMed] [Google Scholar]
- 37.Buhrman M, Skoglund A, Husell J, Bergström K, Gordh T, Hursti T, Bendelin N, Furmark T, Andersson G. Guided internet-delivered acceptance and commitment therapy for chronic pain patients: a randomized controlled trial. Behav Res Ther. 2013 Jun;51(6):307–315. doi: 10.1016/j.brat.2013.02.010.S0005-7967(13)00048-X [DOI] [PubMed] [Google Scholar]
- 38.Mattila E, Orsama A, Ahtinen A, Hopsu L, Leino T, Korhonen I. Personal health technologies in employee health promotion: usage activity, usefulness, and health-related outcomes in a 1-year randomized controlled trial. JMIR Mhealth Uhealth. 2013;1(2):e16. doi: 10.2196/mhealth.2557. http://mhealth.jmir.org/2013/2/e16/ v1i2e16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lappalainen P, Kaipainen K, Lappalainen R, Hoffrén H, Myllymäki T, Kinnunen M, Mattila E, Happonen AP, Rusko H, Korhonen I. Feasibility of a personal health technology-based psychological intervention for men with stress and mood problems: randomized controlled pilot trial. JMIR Res Protoc. 2013;2(1):e1. doi: 10.2196/resprot.2389. http://www.researchprotocols.org/2013/1/e1/ v2i1e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Greene GW, White AA, Hoerr SL, Lohse B, Schembre SM, Riebe D, Patterson J, Kattelmann KK, Shoff S, Horacek T, Blissmer B, Phillips BW. Impact of an online healthful eating and physical activity program for college students. Am J Health Promot. 2012;27(2):e47–e58. doi: 10.4278/ajhp.110606-QUAN-239. [DOI] [PubMed] [Google Scholar]
- 41.Kattelmann KK, Bredbenner CB, White AA, Greene GW, Hoerr SL, Kidd T, Colby S, Horacek TM, Phillips BW, Koenings MM, Brown ON, Olfert MD, Shelnutt KP, Morrell JS. The effects of Young Adults Eating and Active for Health (YEAH): a theory-based Web-delivered intervention. J Nutr Educ Behav. 2014;46(6):S27–S41. doi: 10.1016/j.jneb.2014.08.007.S1499-4046(14)00637-X [DOI] [PubMed] [Google Scholar]
- 42.Research on the menopause in the 1990s. Geneva: World Health Organization; 1996. http://apps.who.int/iris/bitstream/10665/41841/1/WHO_TRS_866.pdf . [Google Scholar]
- 43.Arem H, Irwin M. A review of web-based weight loss interventions in adults. Obes Rev. 2011 May;12(5):e236–e243. doi: 10.1111/j.1467-789X.2010.00787.x. http://europepmc.org/abstract/MED/20804523 .OBR787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Google Analytics. 2015. [2015-09-15]. https://www.google.com/analytics .
- 45.Venkatesh V, Davis FD. A theoretical extension of the technology acceptance model: four longitudinal field studies. Management Science. 2000 Feb;46(2):186–204. doi: 10.1287/mnsc.46.2.186.11926. [DOI] [Google Scholar]
- 46.George D, Mallery P. SPSS for Windows step by step: A simple guide and reference. 11.0 update. 4th ed. Boston, MA: Allyn & Bacon; 2003. [Google Scholar]
- 47.Beglin SJ, Fairburn CG. Evaluation of a new instrument for the detection of eating disorders in community samples. Psychiatry Res. 1992 Dec;44(3):191–201. doi: 10.1016/0165-1781(92)90023-v. [DOI] [PubMed] [Google Scholar]
- 48.Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, Waltz T, Zettle RD. Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: a revised measure of psychological inflexibility and experiential avoidance. Behav Ther. 2011 Dec;42(4):676–688. doi: 10.1016/j.beth.2011.03.007.S0005-7894(11)00088-8 [DOI] [PubMed] [Google Scholar]
- 49.Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996 Mar;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 50.Ware J, Kosinski M, Turner-Bowker DM, Gandek B. User's manual for the SF-12v2 Health Survey with a supplement documenting SF-12 Health Survey. Lincoln, RI: QualityMetric Incorporated; 2007. [Google Scholar]
- 51.Cheak-Zamora NC, Wyrwich KW, McBride TD. Reliability and validity of the SF-12v2 in the medical expenditure panel survey. Qual Life Res. 2009 Aug;18(6):727–735. doi: 10.1007/s11136-009-9483-1. [DOI] [PubMed] [Google Scholar]
- 52.2006 Census questionnaires. Statistics New Zealand; 2006. [2015-09-15]. http://www.stats.govt.nz/Census/about-2006-census/2006-census-questionnaires.aspx . [Google Scholar]
- 53.Milne B, Byun U, Lee A. New Zealand socio-economic index 2006. Wellington: Statistics New Zealand; 2013. [2016-07-24]. http://www.stats.govt.nz/~/media/Statistics/surveys-and-methods/methods/research-papers/nz-socio-economic-index-2006/nz-socio-economic-index-2006.pdf . [Google Scholar]
- 54.2006 Census Data. Wellington: Statistics New Zealand; 2006. [2015-09-15]. http://www.stats.govt.nz/Census/2006CensusHomePage.aspx . [Google Scholar]
- 55.Household labour force survey: June quarter 2012. Wellington: Statistics New Zealand; 2012. [2015-09-15]. http://www.stats.govt.nz/browse_for_stats/income-and-work/employment_and_unemployment/HouseholdLabourForceSurvey_HOTPJun12qtr.aspx . [Google Scholar]
- 56.Davis P, Jenkin G, Coope P. New Zealand socio-economic index 1996: an update and revision of the New Zealand socio-economic index of occupational status. Wellington: Statistics New Zealand; 2003. http://www2.stats.govt.nz/domino/external/web/prod_serv.nsf/4aa2fc565310869fcc256bb4007a16d9/dc0ac1758236cb28cc256cef00748da5/$FILE/NZSEI96.pdf . [DOI] [PubMed] [Google Scholar]
- 57.Ministry of Health . Annual update of key results 2013/14: New Zealand Health Survey. Wellington: Ministry of Health; 2014. [2016-07-24]. http://www.health.govt.nz/system/files/documents/publications/annual-update-key-results-nzhs-2013-14-dec14-v2.pdf . [Google Scholar]
- 58.Bush HE, Rossy L, Mintz LB, Schopp L. Eat for life: a work site feasibility study of a novel mindfulness-based intuitive eating intervention. Am J Health Promot. 2014;28(6):380–388. doi: 10.4278/ajhp.120404-QUAN-186. [DOI] [PubMed] [Google Scholar]
- 59.Donkin L, Christensen H, Naismith SL, Neal B, Hickie IB, Glozier N. A systematic review of the impact of adherence on the effectiveness of e-therapies. J Med Internet Res. 2011;13(3):e52. doi: 10.2196/jmir.1772. http://www.jmir.org/2011/3/e52/ v13i3e52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kelders SM, Kok RN, Ossebaard HC, Julia E W C. Van Gemert-Pijnen JEWC. Persuasive system design does matter: a systematic review of adherence to web-based interventions. J Med Internet Res. 2012;14(6):e152. doi: 10.2196/jmir.2104. http://www.jmir.org/2012/6/e152/ v14i6e152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.van Genugten L, van Empelen P, Boon B, Borsboom G, Visscher T, Oenema A. Results from an online computer-tailored weight management intervention for overweight adults: randomized controlled trial. J Med Internet Res. 2012;14(2):e44. doi: 10.2196/jmir.1901. http://www.jmir.org/2012/2/e44/ v14i2e44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Khaylis A, Yiaslas T, Bergstrom J, Gore-Felton C. A review of efficacious technology-based weight-loss interventions: five key components. Telemed J E Health. 2010 Nov;16(9):931–8. doi: 10.1089/tmj.2010.0065. http://europepmc.org/abstract/MED/21091286 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dour CA, Horacek TM, Schembre SM, Lohse B, Hoerr S, Kattelmann K, White AA, Shoff S, Phillips B, Greene G. Process evaluation of Project WebHealth: a nondieting Web-based intervention for obesity prevention in college students. J Nutr Educ Behav. 2013;45(4):288–295. doi: 10.1016/j.jneb.2012.10.001.S1499-4046(12)00652-5 [DOI] [PubMed] [Google Scholar]
- 64.Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc. 2011 Jan;111(1):92–102. doi: 10.1016/j.jada.2010.10.008. http://europepmc.org/abstract/MED/21185970 .S0002-8223(10)01644-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Latner J, Wilson G. Self-monitoring and the assessment of binge eating. Behav Ther. 2002;33:465–477. [Google Scholar]
- 66.Linde JA, Jeffery RW, French SA, Pronk NP, Boyle RG. Self-weighing in weight gain prevention and weight loss trials. Ann Behav Med. 2005 Dec;30(3):210–216. doi: 10.1207/s15324796abm3003_5. [DOI] [PubMed] [Google Scholar]
- 67.Binks M, van Mierlo T. Utilization patterns and user characteristics of an ad libitum Internet weight loss program. J Med Internet Res. 2010;12(1):e9. doi: 10.2196/jmir.1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rothert K, Strecher VJ, Doyle LA, Caplan WM, Joyce JS, Jimison HB, Karm LM, Mims AD, Roth MA. Web-based weight management programs in an integrated health care setting: a randomized, controlled trial. Obesity (Silver Spring) 2006 Feb;14(2):266–272. doi: 10.1038/oby.2006.34. doi: 10.1038/oby.2006.34.14/2/266 [DOI] [PubMed] [Google Scholar]
- 69.Yardley L, Ware LJ, Smith ER, Williams S, Bradbury KJ, Arden-Close EJ, Mullee MA, Moore MV, Peacock JL, Lean ME, Margetts BM, Byrne CD, Hobbs RFD, Little P. Randomised controlled feasibility trial of a web-based weight management intervention with nurse support for obese patients in primary care. Int J Behav Nutr Phys Act. 2014;11:67. doi: 10.1186/1479-5868-11-67. http://www.ijbnpa.org/content/11//67 .1479-5868-11-67 [DOI] [PMC free article] [PubMed] [Google Scholar]


