SUMMARY
Antibody blockade of the inhibitory CTLA-4 pathway has led to clinical benefit in a subset of patients with metastatic melanoma. Anti-CTLA-4 enhances T cell responses, including production of IFN-γ, which is a critical cytokine for host immune responses. However, the role of IFN-γ signaling in tumor cells in the setting of anti-CTLA-4 therapy remains unknown. Here we demonstrate that patients identified as non-responders to anti-CTLA-4 (ipilimumab) have tumors with genomic defects in IFN-γ pathway genes. Furthermore, mice bearing melanoma tumors with knockdown of IFN-γ receptor 1 (IFNGR1) have impaired tumor rejection upon anti-CTLA-4 therapy. These data highlight that loss of the IFN-γ signaling pathway is associated with primary resistance to anti-CTLA-4 therapy. Our findings demonstrate the importance of tumor genomic data, especially IFN-γ related genes, as prognostic information for patients selected to receive treatment with immune checkpoint therapy.
Keywords: melanoma, anti-CTLA-4, ipilimumab, IFN-γ signaling, copy number alteration, primary resistance
eTOC
Genomic defects in the interferon pathway genes reduce the chance of response to immune checkpoint blockade therapy with anti-CTLA-4 for melanoma in humans and experimental models.
INTRODUCTION
Blockade of T cell inhibitory pathways has become a new paradigm in cancer therapy. Current immune inhibitory pathways that are being targeted include cytotoxic-lymphocyte antigen-4 (CTLA-4) and programmed-death-1 and its ligand (PD-1/PD-L1) (Sharma and Allison, 2015a, b). Anti-CTLA-4 and anti-PD-1 monotherapies have led to significant clinical benefits in patients with melanoma, lung cancer, renal cell carcinoma, and bladder cancer (Borghaei et al., 2015; Hodi et al., 2010; Motzer et al., 2015; Robert et al., 2011; Rosenberg et al., 2016). The first antibody approved by the FDA was anti-CTLA-4 (ipilimumab, Bristol-Myers Squibb), which improved median overall survival in patients with metastatic melanoma (Hodi et al., 2010; Robert et al., 2011). Although ipilimumab therapy resulted in significant survival benefit in about 20% of patients with metastatic melanoma, the majority of patients, however, did not benefit from this therapy. To date, mechanisms responsible for lack of clinical responses in some patients remain unknown.
Our previous studies demonstrated that ipilimumab treatment led to an increase in IFN-γ production by T cells (Liakou et al., 2008). Studies in mice also indicated that anti-CTLA-4 treatment of tumor-bearing mice enhanced IFN-γ production by T cells and IFN-γ signaling in T cells plays an essential role for anti-tumor immune response mediated by anti-CTLA-4 therapy (Fu et al., 2011; Shi et al., 2016). As an essential effector molecule for immune responses (Dunn et al., 2006), IFN-γ exerts its downstream effects by binding to the IFN-γ receptor (IFNGR) consisting of two subunits, IFNGR1 and IFNGR2. Binding of IFN-γ to its receptor results in recruitment and activation of the Janus kinases, JAK1 and JAK2, and subsequent phosphorylation, dimerization, and activation of a transcription factor known as signal transducer and activator of transcription (STAT)1. STAT1 homodimers then translocate to the nucleus where they bind to specific promoter elements and modulate transcription of IFN-γregulated genes (Ikeda et al., 2002). This series of events of IFN-γ signaling culminate in immune cell activation.
In addition to immune cell activation, in vitro treatment with IFN-γ can also directly inhibit tumor cell growth and promote tumor cell apoptosis by binding to IFN-γ receptor and subsequent activation of the JAK-STAT signaling pathway (Chin et al., 1997; Detjen et al., 2001; Ikeda et al., 2002). Therefore, tumor cells containing defective IFN-γ signaling pathway genes may be resistant to IFN-γ-mediated growth inhibition and apoptosis. Since our data indicate that anti-CTLA-4 treatment resulted in significant production of IFN-γ, we hypothesized that tumor cells containing defective IFN-γ signaling pathway genes may be resistant to anti-CTLA-4 therapy.
Here, we show that melanoma samples from patients who lacked clinical responses to ipilimumab harbor a much higher rate of genomic defects in the IFN-γ pathway genes as compared to melanoma samples obtained from patients who had clinical responses to ipilimumab. We used shRNA technology to abolish IFNGR1 expression in the B16/BL6 melanoma tumor cell line and found that these cells were resistant to IFN-γ treatment in vitro. In addition, mice treated with anti-CTLA-4 demonstrated impaired rejection of B16/BL6 tumors lacking expression of the IFNGR1 gene as compared to those bearing B16/BL6 tumors with intact expression of the IFNGR1 gene. Overall, our data demonstrate that IFN-γ signaling deficiency in melanoma tumor cells is associated with lack of response to anti-CTLA-4 treatment.
RESULTS
Melanoma tumors resistant to ipilimumab therapy contain genomic defects in IFN-γ pathway genes
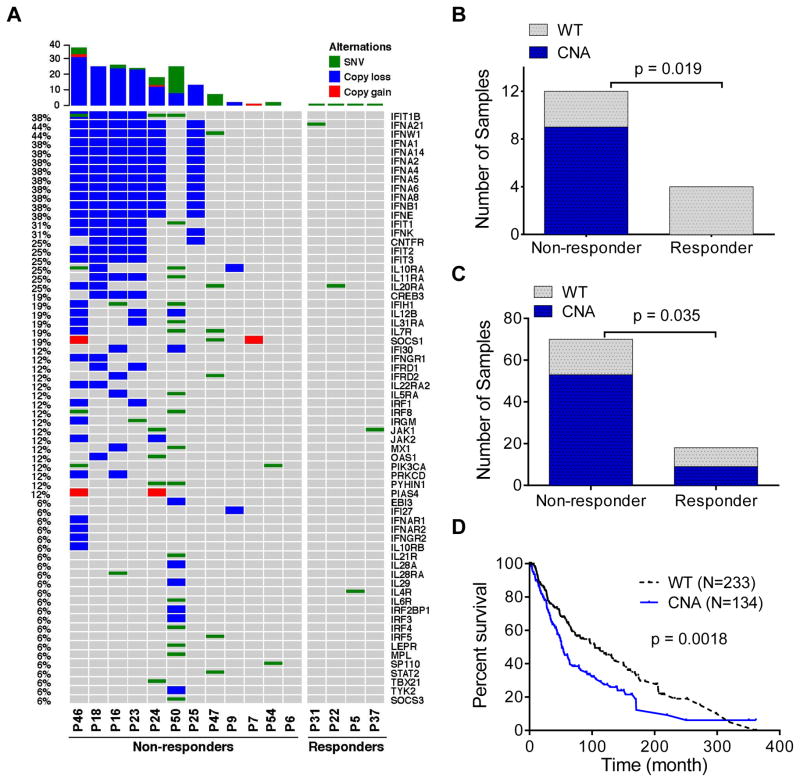
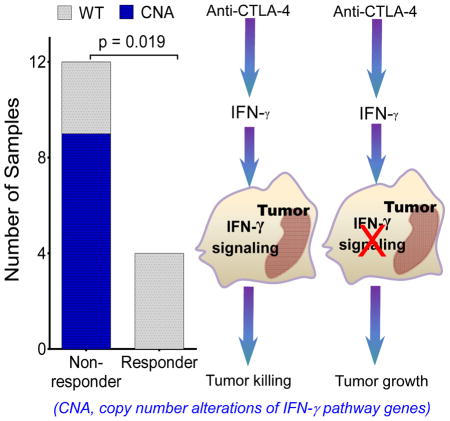
We evaluated available whole exome sequencing (WES) data for genomic changes of IFN-γ pathway genes in melanoma tumors from 16 patients (Table S1), which consisted of 12 patient who did not respond to ipilimumab therapy (non-responders) and 4 patients who did respond to ipilimumab therapy (responders). IFN-γ pathway genes were defined by the QIAGEN human interferon and receptor functional gene grouping and other databases (Table S2). Tumor samples from non-responders were found to have significantly more somatic mutations including copy number alterations (CNAs) and single nucleotide variants (SNVs) of the IFN-γ pathway genes (Figure 1A). A total of 184 mutations were detected in the 12 non-responders, including 142 CNAs and 42 SNVs; whereas only 4 mutations were detected in the responders, all of which are SNVs. We identified an average of 15.33 mutations in IFN-γ pathway genes in non-responders as compared to an average of only 1 mutation in responders. A permutation test demonstrated that the significant enrichment of mutations in non-responders was not observed by chance (p = 0.015, Figure S1A). However, we did not observe a significant difference in the enrichment of SNVs between the non-responders and responders (p = 0.261, Figure S1B). These data suggest that CNAs, as oppose to SNVs, are the dominant genomic events that are associated with resistance to ipilimumab therapy.
Figure 1. Melanoma tumors resistant to ipilimumab therapy contain genomic defects in IFN-γ pathway genes.
(A) Landscape of CNAs of IFN-γ pathway genes in 16 melanoma tumors (See Table S1 for patient information). Each column represents a patient tumor sample as labeled at the bottom. The bar plot at the top of the figure represents the total number of genes with CNA or SNV in that specific sample. The numbers on the left side represent the percentage of melanoma samples carrying CNA or SNV of each specific gene. The gene names are labeled on the right side of the figure. See Figure S1 for permutation analyses of CNAs (A) and SNVs (B) between responders and non-responders. Figure S3 depicts the two common interferon gene clusters deleted in ipilimumab non-responders. (B) Numbers of melanoma tumor samples with wild-type (grey bars) and carrying CNAs (blue bars) of IFN-γ pathway genes in responders (N=4) vs. non-responders (N=12) to ipilimumab therapy in our cohort. See Table S2 for a complete list of defined IFN-γ pathway genes. (C) Numbers of melanoma tumor samples with wild-type (grey bars) and carrying CNAs (blue bars) of IFN-γ pathway genes in responders (N=18) vs. non-responders (N=70) in an independent cohort. See also Table S3 for responder and non-responder patients and Figure S2 for detailed distribution of CNAs in these patients. The associations of somatic CNAs with ipilimumab clinical responses in Figure 1B and C were based on one-tailed Fisher’s exact test. (D) Kaplan-Meier survival curve of patients with metastatic melanoma containing CNAs in IFN-γ pathway genes (N=134) vs. those with melanoma tumors containing wild-type IFN-γ pathway genes (N=233). The p-value was based on log rank test.
A significantly higher proportion of tumors from non-responder patients (9/12 = 75%) had CNAs involving IFN-γ pathway genes than tumors from responder patients (0/4 = 0%) (p=0.019, Figure 1B). The most significant CNAs included genomic loss of key IFN-γ pathway genes such as IFNGR1, IRF-1, JAK2, and IFNGR2, as well as amplification of important IFN-γ pathway inhibitors including SOCS1 and PIAS4 (Figure 1A). Collectively, these data strongly suggest that tumors from non-responder patients contain a significantly higher number of genomic defects leading to, at least in part, defective IFN-γ signaling that may result in primary resistance to ipilimumab therapy.
To confirm these initial findings, we evaluated an independent cohort of patients that was previously published (Van Allen et al., 2015). Patients were divided into responders and non-responders to ipilimumab therapy, with the exclusion of all patients who were listed as stable disease (Table S3). Our analyses confirmed a higher frequency of CNAs involving IFN-γ pathway genes in non-responder patients as compared to responder patients (Figure 1C and Figure S2).
Tumors with CNAs of the IFN-γ pathway genes correlate with shorter survival in patients with metastatic melanoma
Since our data suggested that CNAs of the IFN-γ pathway genes in melanoma tumors may predict primary resistance to ipilimumab therapy, we hypothesized that patients bearing melanoma tumors containing CNAs of IFN-γ pathway genes would be less responsive to endogenous IFN-γ associated with host immune response and therefore, should have poor clinical outcome. To test this, we analyzed the available data on a total of 367 patients with metastatic melanoma in the TCGA database. Of these patients, 134 had CNAs of the IFN-γ pathway genes, whereas the other 233 contained wild-type IFN-γ pathway genes. We found that the patients with tumors containing CNAs of IFN-γ pathway genes had significantly shorter overall survival (40 months) than those with wild-type tumors (48.2 months, p = 0.0018) (Figure 1D).
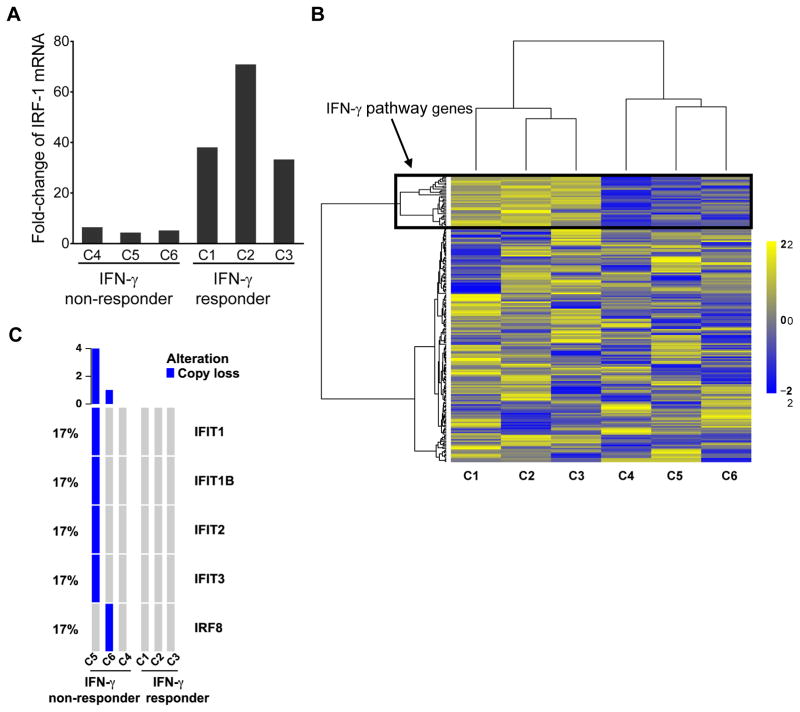
Melanoma cell lines that are refractory to in vitro treatment with IFN-γ contain genomic defects in IFN-γ pathway genes
Next, we evaluated 6 primary tumor cell lines derived from patients with melanoma to determine whether differences in response to in vitro treatment with IFN-γ correlated to the mutation status of IFN-γ pathway genes. We found that IFN-γ treatment of 3 primary melanoma tumor cell lines (C1–3) demonstrated significant induction of IRF-1, which is a downstream gene of the IFN-γ signaling pathway. However, 3 other cell lines (C4–6) had minimal induction of the IRF-1 gene in response to IFN-γ (Figure 2A). Unsupervised clustering of gene expression fold changes between post-treatment vs. pre-treatment samples for the 6 cell lines confirmed differences in expression of IFN-γ pathway genes for the IFN-γ responder vs. IFN-γ non-responder cell lines (Figure 2B). From the microarray data, we identified a subset of 36 probes (Table S4) that were significantly and consistently increased in the 3 IFN-γ responder cell lines as compared to the 3 IFN-γ non-responder cell lines (Figure 2B). This subset of probes was comprised of genes that are related to the IFN-γ pathway including IRF-1, CXCL10, IFIT1, IFIT2 and IFIT3 (Table S4). As indicated in Figure 2B, all of these IFN-γ pathway genes have higher fold changes in the responder than in the non-responder cell lines with IFN-γ treatment. In addition, we found copy number loss in key IFN-γ pathway genes in two of the three IFN-γ non-responder cell lines. Cell line C5 had copy number loss for IFIT1, IFIT2, IFIT3 and IFIT1B genes while cell line C6 had loss of the IRF8 gene. On the contrary, there was no copy number loss in the 3 IFN-γ responder cell lines (Figure 2C). These data demonstrate that tumor cells that are less responsive to in vitro IFN-γ treatment are likely to harbor loss of IFN-γ pathway genes.
Figure 2. Human melanoma cell lines that are refractory to in vitro treatment with IFN-γ contain genomic defects in IFN-γ pathway genes.
(A) IRF-1 gene expression fold change after IFN-γ treatment in the 6 cell lines derived from human melanoma tumors. The 3 cell lines (C1, C2 and C3) with higher fold changes were defined as IFN-γ responders and the other 3 (C4, C5 and C6) as IFN-γ non-responders. (B) Heatmap of unsupervised clustering analysis of the scaled log2 fold changes of gene expression in the 6 cell lines after IFN-γ treatment. The top panel in the black box illustrated the 36 probes (see Table S4 for details) showing consistent higher fold changes in C1, C2 and C3. (C) IFN-γ pathway gene copy number loss in 3 IFN-γ non-responder melanoma cells lines vs. 3 responder cell lines. See also Figure S3 and Table S4.
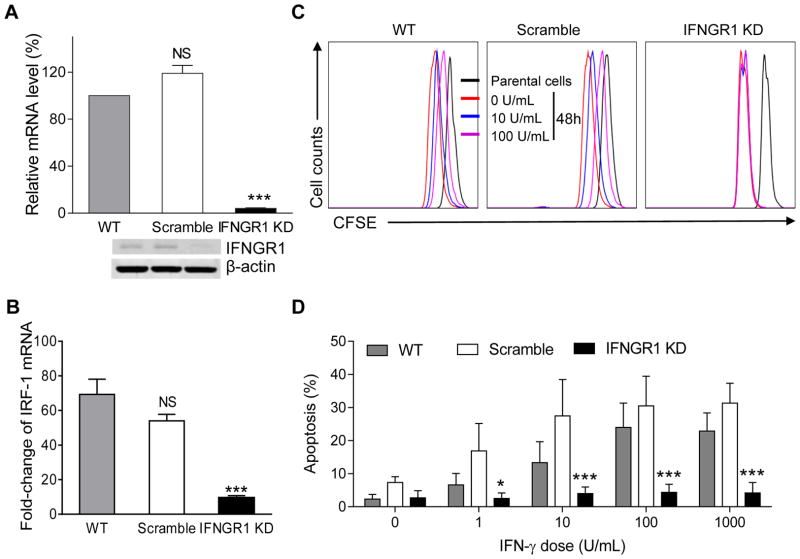
Knockdown of IFNGR1 attenuates IFN-γ-mediated suppression of B16/BL6 cell proliferation and apoptosis
To further study the impact of loss of IFN-γ signaling in tumor cells, we used shRNA technology to decrease expression of IFNGR1 in the murine B16/BL6 melanoma cell line, which is an IFN-γ responsive cell lines selected from a cohort of murine tumor cell lines (Figure S4). We confirmed effective knockdown of the IFNGR1 gene at both mRNA and protein levels (Figure 3A). Loss of upregulation of IRF-1 gene upon IFN-γ treatment further confirmed functional knockdown of the IFNGR1 gene (Figure 3B). IFN-γ resulted in dose-dependent inhibition of cell proliferation of the wild-type and scramble shRNA-transduced B16/BL6 cell lines. However, loss of the IFNGR1 gene restored proliferation of the B16/BL6 tumor cells even in the presence of IFN-γ (Figure 3C). Furthermore, loss of the IFNGR1 gene also attenuated IFN-γ– induced apoptosis of B16/BL6 tumor cells in vitro, irrespective of doses of IFN-γ (Figure 3D).
Figure 3. Knockdown of IFNGR1 gene in murine B16/BL6 melanoma attenuates IFN-γ mediated suppression of cell proliferation and apoptosis.
(A) Knockdown of IFNGR1 gene in B16/BL6 cell line (see also Figure S4). Top panel shows IFNGR1 mRNA levels as detected by RT-PCR in wild-type (WT), scramble shRNA (SC) transduced-, and IFNGR1 shRNA- transduced (IFNGR1 KD) B16/BL6 cells (bar graphs). The bottom panel shows IFNGR1 protein levels as detected by western blot in the same experimental groups with β-actin as an internal control. (B) RT-PCR analysis of IRF-1 mRNA expression of the above B16/BL6 cells treated with 1000 unit/ml of IFN-γ for 16 hours (NS, not significant; *** P < 0.0001). (C) B16/BL6 cells as described in (A) that were freshly labeled with CFSE (parental cells) or CFSE-prelabeled cells that were further cultured for 48 h in the absence or presence of varying doses of IFN-γ were analyzed for CFSE expression by flow cytometry. (D) Apoptosis rate as detected by flow cytometry in wild-type, scramble shRNA transduced, and IFNGR1 shRNA-transduced B16/BL6 cells in response to increasing concentrations of IFN-γ. Data in the bar graphs are means ± SEM. NS: no statistical significance, *: p<0.05, **: p<0.01, ***: p<0.001 by ANOVA analysis, as compared to the wild-type counterparts. All data are representative of three independent experiments.
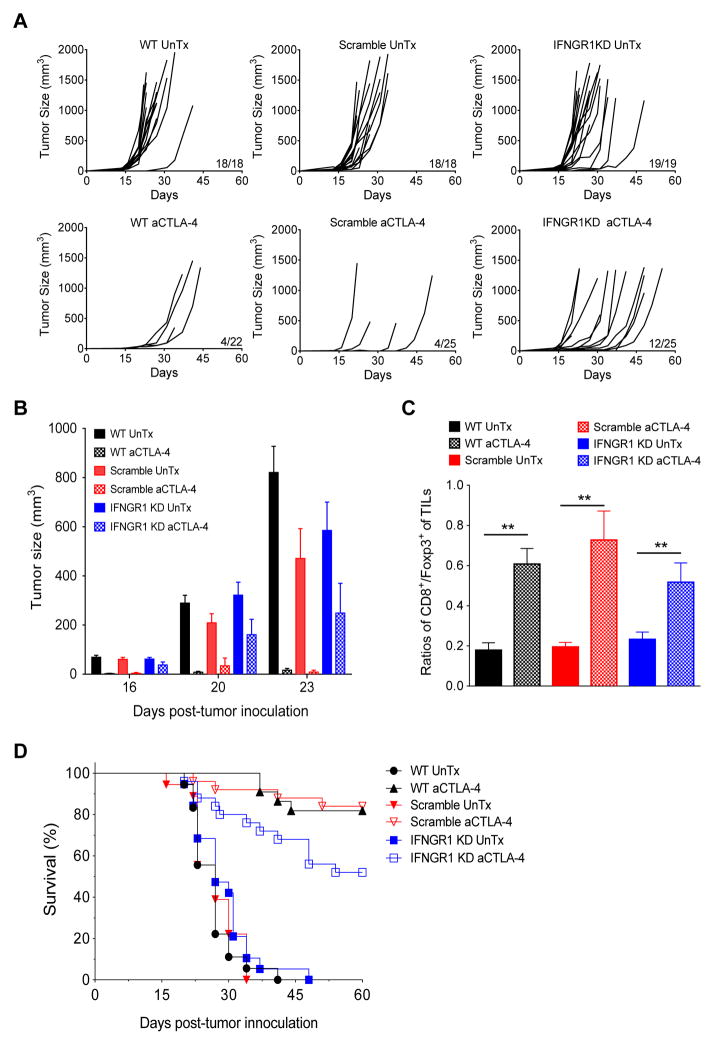
Knockdown of IFNGR1 gene in B16/BL6 tumors promotes in vivo tumor growth and reduces mouse survival in response to anti-CTLA-4 therapy
To assess effects of IFNGR1 knockdown on tumor growth in vivo, we inoculated C57BL/6 mice with B16/BL6 tumor cells and treated with anti-CTLA-4. Similar to our previously published studies (Fu et al., 2011), 100% of the wild-type, scramble shRNA-transduced, and IFNGR1 shRNA-transduced B16/BL16 cell lines proliferated and formed measurable tumors in untreated mice (Figure 4A). However, after anti-CTLA-4 treatment, 4/22 mice with wild-type B16/BL6 tumors and 4/25 mice with scramble shRNA-transduced B16/BL6 tumors had progressive tumor growth, while 12/25 mice with IFNGR1 shRNA-transduced B16/BL16 tumors had progressive tumor growth. We also evaluated the tumor burden in different cohorts of mice (Figure 4B). While we did not find significant difference in tumor size for all untreated cohorts, the growth of wild-type tumors and tumors transduced with the scramble shRNA was significantly inhibited by anti-CTLA-4 therapy. In contrast, tumors transduced with IFNGR1 shRNA had impaired response to anti-CTLA-4 therapy and were significantly larger as compared to control tumors (p<0.05). Of note, anti-CTLA-4 treated tumors from all cohorts of mice were found to have a significant increase in the ratio of CD8 effector T cells to FoxP3+ regulatory T cells (Figure 4C), an important index reflective of effective treatment of anti-CTLA-4 (Quezada et al., 2006), suggesting IFNGR1 knockdown in tumors does not significantly affect T cell infiltration into tumors. In addition, all untreated mice died as a result of tumor growth while anti-CTLA-4 treatment led to long-term survival of ~80% of mice bearing B16/BL6 tumors with intact IFNGR1 gene expression, which was significantly higher (p= 0.0174) than that of mice bearing B16/BL6 tumors lacking the IFNGR1 gene (Figure 4D). These data offer direct evidence that tumor cell loss of the IFNGR1 gene, which results in loss of IFN-γ signaling, leads to resistance to anti-CTLA-4 therapy.
Figure 4. Knockdown of IFNGR1 gene in B16/BL6 tumors promotes in vivo tumor growth and reduces survival in response to anti-CTLA-4 therapy.
(A) In vivo tumor growth rate in B16/BL6 wild-type tumors as compared to scramble shRNA- and IFNGR1 shRNA-transduced tumors in mice treated with anti-CTLA-4 (lower panel). Upper panels are untreated controls (UnTx). (B) Tumor load of wild-type, scramble shRNA- and IFNGR1 shRNA-transduced tumors in mice treated with anti-CTLA-4. Data in the bar graphs are means ± SEM. (C) Ratio of CD8 T cells to Foxp3+ regulatory T cells in wild-type, scramble shRNA- and IFNGR1 shRNA-transduced tumors from mice on day 14 post anti-CTLA-4 treatment. Data in the bar graphs are means ± SEM; **p<0.01 by student’s t-test, as compared to the untreated controls. (D) Survival rate of mice bearing B16/BL6 wild-type tumors as compared to scramble shRNA- and IFNGR1 shRNA-transduced tumors with and without treatment of anti-CTLA-4. All data are pooled results from 2–3 independent experiments.
DISCUSSION
Ipilimumab (anti-CTLA-4) therapy has provided significant clinical benefit to patients with metastatic melanoma. However, only a subset of patients, approximately 20%, derive long-term survival benefit (Hodi et al., 2010). To date, extensive efforts are ongoing to understand response and resistance mechanisms to anti-CTLA-4 therapy. Multiple publications have reported that anti-CTLA-4, and other immune checkpoint therapies, lead to an increase in IFN-γ production (Alegre et al., 1998; Chen et al., 2009; Dulos et al., 2012; Liakou et al., 2008; Paradis et al., 2001; Peng et al., 2012), which plays an important role in immune responses (Dunn et al., 2006; Szabo et al., 2003). For example, we previously reported that treatment of patients with ipilimumab led to enhanced immune responses including increased IFN-γ production by T cells expressing inducible costimulator (ICOS) (Liakou et al., 2008).
IFN-γ plays a critical role in regulating T cell responses, including driving Th1 immune responses, which are required for tumor rejection (Dunn et al., 2006; Szabo et al., 2003). IFN-γ elicits multiple signals in T cells to enable effective T cell function, while loss of IFN-γ pathways in T cells impairs T cell responses and permits tumor growth and persistence (Ikeda et al., 2002; Kaplan et al., 1998). These data established a clear role for IFN-γ in shaping immune responses, especially anti-tumor T cell responses.
IFN-γ has also been shown to affect tumor cell growth. For example, in vitro data demonstrated that IFN-γ can directly inhibit tumor cell growth and promote tumor cell apoptosis (Chin et al., 1997; Detjen et al., 2001; Ikeda et al., 2002). Previous pre-clinical studies have also shown that defects in IFNGR1, JAK1, and JAK2 genes render tumor cells unresponsive to IFN-γ, which enables tumor cell growth in the presence of IFN-γ (Dunn et al., 2005; Ikeda et al., 2002; Kaplan et al., 1998). These data suggest effective antitumor immune responses depend upon functional IFN-γ signaling pathway in tumor cells.
Although there are likely to be multiple mechanisms that lead to resistance to ipilimumab therapy, we hypothesized that tumor cells with defective IFN-γ signaling would be resistant to anti-CTLA-4 therapy. Consistent with this hypothesis, our clinical data indicate that tumors from patients with metastatic melanoma who did not respond to ipilimumab had higher frequency of genomic alterations of IFN-γ pathway genes as compared to tumor samples from patients with clinical responses to ipilimumab (Figure 1). These genomic alterations include copy number loss of key IFN-γ pathway genes such as IFNGR1, IRF-1, JAK2, and IFNGR2, as well as amplification of important IFN-γ pathway inhibitors including SOCS1 and PIAS4 (Figure 1). In addition, a concurrent report suggests that the loss of IFN-γ pathway genes, such as JAK1 and JAK2, is associated with resistance to anti-PD-1 therapy (Zaretsky et al., 2016). Therefore, it is possible that IFN-γ pathway gene defects represent an important resistance mechanism for multiple immune checkpoint therapies.
Our data revealed that a surprisingly high proportion (9/12 =75%) of ipilimumab non-responders harbor certain genomic defects of the IFN-γ pathway genes (Figure 1). Loss of IFNGR1, IFNGR2, JAK2, and IRF-1 genes (Figure 1) would impair the IFN-γ signaling pathway (Dunn et al., 2006; Ikeda et al., 2002). Other genomic losses in these non-responder tumors include downstream IFN-γ pathway genes such as the family of IFIT1, IFIT2, and IFIT3 genes (Figure 1 and Figure S3B). Although their functions are not completely understood, it was reported that these genes promote tumor apoptosis and loss of them would favor tumor growth (Reich, 2013).
In addition, we identified amplification of two well-known suppressors of the IFN-γ signaling pathway, SOCS1 and PIAS4 (Liu et al., 2001; Song and Shuai, 1998). Interestingly, we also observed co-deletions of IFNA, IFNB, MTAP, and miR-31 genes on chromosome 9p21 (6/12=50%, Figure 1 and Figure S3A). Although IFNA and IFNB genes are not essential genes for the IFN-γ signaling pathway, loss of the MTAP gene, which encodes methylthioadenosine phosphorylase, has been reported to result in intracellular accumulation of its enzymatic substrate methylthioadenosine that can inactivate transcription factor STAT1, the central component of the IFN-γ signaling pathway (Mowen et al., 2001). Moreover, loss of miR-31 has been reported to promote Th2-biased immune response that is known to favor tumor growth (van der Heide et al., 2016). Taken together, these data allow us to compile a possible gene signature consisting of loss of IFN-γ signaling-related genes (IFNGR1, IFNGR2, JAK2, IRF-1, IFIT1, IFIT2, IFIT3, MTAP, and miR31) and amplification of IFN-γ signaling pathway suppressor genes (SOCS1 and PIAS4) that may serve as a genomic biomarker to stratify patients for probability of response to immune checkpoint therapy.
Our data are based on a small number of patients and will need to be validated prospectively in larger cohorts of patients, including patients who receive combination immunotherapy strategies. It is possible that certain combination therapies may overcome the effects generated by defects in IFN-γ pathway genes. Additional studies in pre-clinical models would be needed to test the impact of combination immunotherapy strategies on tumor cells lacking key IFN-γ pathway genes. Further studies to elucidate other potential intra-tumoral mechanisms of resistance to immune checkpoint therapies, including epigenetic, transcriptional and translational mechanisms, are warranted.
Overall, our data highlight an IFN-γ pathway gene signature that warrants confirmation in prospective clinical trials. Based upon the study with anti-PD1 (Zaretsky et al., 2016) and our study with anti-CTLA-4, the cumulative data indicate that loss of IFN-γ signaling in tumor cells may represent a common mechanism for tumor resistance to immune checkpoint therapy. Additional studies will be needed to determine whether these genomic data can be used prospectively to stratify patients for treatment or propose novel combination treatments that may overcome resistance.
METHODS AND RESOURCES
CONTACT FOR REAGENT AND RESOURCE SHARING
Inquiries and requests should be directed and will be fulfilled by lead author Padmanee Sharma, Departments of Genitourinary Medical Oncology at the University of Texas MD Anderson Cancer Center. Email: PadSharma@mdanderson.org.
EXPERIMENTAL MODEL AND SUBJECT DETAILS
Melanoma patients and assessment of clinical benefit on ipilimumab
A cohort of 16 patients with metastatic melanoma was included in this study. These patients were treated at the UT MD Anderson Cancer Center between October 2011 and March 2015 and had tumor samples collected and analyzed under IRB-approved protocols (IRB LAB00-063; LAB03-0320; 2012-0846; PA13-0291; PA12-0305). Of note, these studies were conducted in accordance with the Declaration of Helsinki and approved by the UT MD Anderson Cancer Center institutional review board. Electronic medical charts were reviewed independently by two investigators to assign clinical response group. These 16 patients (Table S1) were treated with CTLA-4 blockade, with 4 responding, while 12 progressed, as defined by RECIST criteria (Therasse et al., 2000) at 3–6 months after initiation of therapy.
Clinical samples
Tumor samples were obtained from the UT MD Anderson Cancer Center Department of Pathology archive and Institutional Tumor Bank with appropriate written informed consent and institutional IRB (LAB00-063; LAB03-0320; 2012-0846; PA13-0291; PA12-0305). Tumor biopsy samples were collected at multiple time points during treatment when feasible, including pre-treatment, on-treatment and progression anti-CTLA-4 biopsies. All samples utilized for analysis were reviewed in central pathology to ensure viable tumor was present.
Establishment of tumor cell lines from tumor samples
Tumor cell lines were established from metastatic melanoma samples from patients enrolled on the IRB-approved adoptive T cell therapy study for the use of Tumor Infiltrating Lymphocytes (#2004-0069). Briefly, a single cell suspension was obtained through manual dissection of the tumor specimen followed by incubation with an enzymatic digestion cocktail (0.375% Collagenase Type I, 75 μg/ml hyaluronidase and 250 units/ml DNase I in RPMI 1640) in a humidified incubator at 37°C with 5% CO2 and with gentle rotation for 2–3h. The digested material was then filtered through a 70 um filter, washed, resuspended in fresh media (RPMI 1640 with Glutamax, 10% FBS, 10mM HEPES, 1X Pen/Strep, 20 μg/ml, 50 μM 2-mercaptoethanol, Insulin-Selenium-Transferrin supplement (5 μg/ml, Invitrogen) and plated in one well of a 6-well culture plate. On the next day, the non-adherent cells were washed out and fresh media was added. Cultures were deemed established when the expanded cells stained positive for a melanoma tumor marker and negative for a fibroblast marker (CD90). MCSP-1 was used as a melanoma tumor surface marker to assess the purity of the tumor cell line by flow cytometry once enough cells were grown. All cell lines were tested for mycoplasma and fingerprinted before use.
Cell lines were validated by STR DNA fingerprinting using the Promega 16 High Sensitivity STR Kit (Catalog # DC2100). The STR profiles were compared to online search databases (DSMZ/ATCC/JCRB/RIKEN) of 2455 known profiles; along with the MD Anderson Characterized Cell Line Core (CCLC) database of 2556 know profiles. The STR profiles matched known DNA fingerprints or were unique.
Mice, cell lines, and reagents
C57BL/6 mice were purchased from the Jackson Laboratory. All in vivo experiments used female mice. Experiments were carried out under pathogen-free conditions according to approved protocols from the UT MD Anderson Cancer Center IACUC. The B16/BL6 murine melanoma cell line and B16/BL6 expressing GM-CSF (GVAX) were maintained, used, and grown as previously published (Fu et al., 2011). Puromycin of 2 μg/ml was added to the culture medium for maintenance of B16/BL6-IFNGR1 knockdown and B16/BL6-scramble cell lines. All cell lines used in this study were tested to make sure they were free of mycoplasma. Anti-CTLA-4 monoclonal antibody (clone 9H10) was purchased from BioXcell.
METHOD DETAILS
Microarray gene expression analysis
Pre- and post-treatment samples were collected for total RNA isolation using the Qiagen RNeasy Mini Kit. Total RNA was used for Affymetrix GeneChip Human Genome U133 2.0 Array analysis. Microarray data were preprocessed using the affy bioconductor package. Background correction and quantile normalization were performed using the Robust Multi-chip Average (RMA) function in affy. The fold changes of interferon pathway genes were calculated by comparing the expression values of selected genes from Table S2 in the IFN-γ-treated vs. untreated cell lines. Unsupervised clustering of the fold changes after IFN-γ treatment were used to partition the 6 samples into 2 clusters.
Whole exome sequencing (WES) analysis
WES experiments were performed on tumor tissues from 16 patients (4 responders and 12 non-responders) as well as 6 melanoma tumor-derived cell lines. Normal peripheral blood was used as controls. The initial 250ng genomic DNA was sheared using low Tris-EDTA buffer. KAPA Hyper Prep Kit (#KK8504) was used for end repair, A-base addition, adapter ligation, and library enrichment PCR. Library construction was performed following manufacturer's instructions. Sample concentrations were measured following library construction using the Agilent Bioanalyzer. Hybridization reaction was then performed. In terms of target capture, the Agilent SureSelect-XT Target Enrichment (#5190-8646) protocol was followed, according to manufacturer guidelines. The libraries were then normalized to equal concentrations using an Eppendorf Mastercycler EP Gradient instrument and pooled to equimolar amounts on the Agilent Bravo B platform. Libraries were quantified using the KAPA Library Quantification Kit (#KK4824). For the cell line samples, genomic DNA was sheared, end repaired, ligated with barcoded Illumina sequencing adapters, amplified, size selected and subjected to in solution hybrid capture using the Agilent SureSelect Human All Exon v2.0 bait set (Fisher et al., 2011; Gnirke et al., 2009). The resulted libraries were then qPCR quantified, pooled, and sequenced with 76 base paired-end reads using Illumina HiSeq 2000 sequencer. The median on-target read coverage ranges from 101X to 232X. The tumor purity ranges from 80% to 95%, except 50% for only one sample.
The raw reads were aligned to the human hg19 reference genome using the BWA aligner (bwa-0.7.5a) (Gnirke et al., 2009). Duplicate reads were marked using the Picard (v1.112, http://broadinstitute.github.io/picard/) “MarkDuplicates” module. The “IndelRealigner” and “BaseRecalibrator” modules of the Genome Analysis Toolkit were applied to the obtained BAM files for indel realignment and base quality recalibration. Mutect (v1.1.4) was used to each tumor and its matching normal sample to detect somatic single nucleotide variants (SNVs) (Cibulskis et al., 2013). The detected SNVs were annotated with ANNOVA (Wang et al., 2010) and compared with public databases such as dbSNP (Sherry et al., 2001), 1000 genome (http://www.1000genomes.org/) and ESP6500 (http://evs.gs.washington.edu/EVS/). To ensure accuracy, the following criteria was required to each detected somatic SNV: allele frequency (AF) > 0.05; the coverage is at least 30 reads for the tumor and 10 for the normal; the AF from the normal sample <=0.01. The filtered somatic SNVs were annotated with dbSNP and compared with public databases. To avoid including germline mutations, we further required the AF < 0.01 from both the ESP6500 and 1000 genome databases. Detected SNVs in dbSNPs were discarded. An in-house R package ExomeCN was applied to infer somatic copy number alterations (CNAs) by first calculating the tumor/normal read counts log2 ratio of the capture regions (minimum reads counts >= 5, map quality >= 10) followed by segmentation (alpha='0.01' nperm='10000' undoSplit='sdundo' undoSD='2' minWidth='3') (Olshen et al., 2004).
The associations of somatic CNAs with ipilimumab clinical responses were based on one-tailed Fisher’s exact test. A sample is called to carry a gene gain (or loss) if the log2 copy ratio of tumor over normal of this gene > 0.5 (or < -0.5) in the patient data. The log2 copy ratio cutoff was 1 in the cell line WES data and 0.7 in Van Allen’s WES data. We define a sample as mutant if it carries the loss of any of the regular interferon genes or gain of any of the 4 interferon pathway inhibitors (SOCS1, SOCS3, PIAS1 and PIAS4). There were 73 non-responders including 3 stable disease patients and 27 responders including 9 stable disease patients. We analyzed the obtained 70 responders and 18 responders after excluding the stable disease patients in each group. WES data are currently being deposited to dbGap with the accession numbers pending. These data will be available to interested parties upon request.
Knockdown of IFNGR1 gene in murine B16 tumor cells
Lentiviral particles of mouse shRNA specific to IFNGR1 gene and control scramble shRNA were purchased from Santa Cruz Biotechnology. Transduction of B16/BL16 cells were carried out according to manufacturer’s instruction. Briefly, mouse melanoma B16/BL16 cells were cultured in 12-well plate to reach 50% confluence, transduced with lentiviral particles, split into 100mm plates, and then selected with puromycin-containing culture medium. Single cell colonies were selected and expanded in puromycin-containing culture medium. RT-PCR and western blot were then used to confirm the extent of individual IFNGR1 gene knockdown.
RT-PCR analysis
At indicated time points after IFN-γ treatment, total RNA was isolated with RNeasy Plus Micro Kit (QIAGEN, Valencia, CA) and cDNA was synthesized with miScript II RT Kit (QIAGEN, Valencia, CA). Expression of target genes was determined by 7500 Fast Real-Time PCR System (Applied Biosystems, Foster City, CA) with SYBR® Green PCR Master Mix (Applied Biosystems, Foster City, CA) according to manufacturer’s instructions. β-actin was used as an internal control. Each sample was examined at least in triplicates. PCR product specificity was confirmed by a melting-curve analysis. The relative mRNA expression was calculated by using 2-Δ ΔCt method. qSTAR qPCR Primer Pairs for RT-PCR were purchased from OriGene Technologies (Rockville, MD).
Western blot analysis
For Western blotting, cells were homogenized in RIPA buffer (Santa Cruz Biotechnology, Dallas, TX) plus phosphatase and protease inhibitor cocktail, 10 mM NaF, 1 mM PMSF and 1 mM Na3VO4. Protein extracts were clarified and concentrations were measured with Pierce Protein Assay kit (Thermo Fisher Scientific). Anti-IFNGR1 antibody was purchased from Novus Biologicals, Littleton, CO; β-actin (Cell Signaling Technology, Dnavers, MA) was used as a loading control. Goat anti-rabbit secondary antibodies were obtained from LI-COR Biosciences. The fluorescent signals were developed with Odyssey® CLx Imaging System (LI-COR Biosciences, Licoln, NE).
Cell proliferation assays
Cell proliferation in response to IFN-γ treatment was assessed by either the CellTiter 96 cell proliferation assay from Promega or flow cytometry. For the Promega’s cell proliferation assay, 2000 cells were cultured in 96-well pates, treated with various concentrations of IFN-γ for 72 hours, and then incubated with CellTiter 96 AQueous One Solution Reagent for 1-4 hours per manufacturer’s protocol before recording the absorbance at 490 nm on SpectraMax M2 (Molecular Devices). For flow cytometry analysis, cell proliferation was detected using CellTrace CFSE Cell Proliferation Kit from ThermoFisher Scientific (Grand Island, NY), as described previously (Shi et al., 2013). Briefly, tumor cells were labeled with 5 μM CFSE for 20 min at 37°C and then treated with various doses of IFN- γ for different periods of time as specified in relevant figures. Cells were then washed twice and harvested to detect CSFE dilution using BD LSR II flow cytometer (BD Biosciences, San Jose, CA). All experiments were performed in triplicates and repeated at least three times.
Cell apoptosis assay
Cell apoptosis was analyzed by flow cytometry, as described previously (Shi et al., 2013). In brief, wild-type (WT), scrambled shRNA-, or IFNGR1 shRNA-transduced B16/BL6 melanoma cells were treated with different doses of IFN-γ (0–1000 U/mL) for 48 h (dose-response studies). Cells were then stained with Annexin-V and 7-AAD using Annexin V Apoptosis Detection Kit I from BD Pharmingen and detected with BD LSR II flow cytometer (BD Biosciences, San Jose, CA). All experiments were performed in triplicates and repeated at least three times.
Tumor models, analysis and treatment
Tumor inoculation and treatment protocol has been previously described (Fu et al., 2011). Briefly, anesthetized mice were injected in the right flank intradermally with 1 x 104 B16/BL6, B16/BL6-IFNGR1 knockdown, B16/BL6-scramble control, or wild-type B16/BL6 cells at day 0, and then treated by injecting 1 x 106 irradiated GVAX (150 Gy) in the left flank. Gvax was given on day 3, 6, 9 after tumor inoculation, together with intraperitoneal injections of 200 (day 3) or 100 μg (day 6 and 9) of anti-CTLA-4 monoclonal antibody. Tumor growth was monitored by measuring tumor size with a caliper 2 to 3 times per week. Mice were euthanized when tumor size reached 1.5 cm in diameter, or ulceration reached 0.2 cm or moribund occurred, and recorded as death.
Isolation of tumor infiltrating lymphocytes (TILs) was previously described (Fu et al., 2011). In brief, tumors were minced and digested with 1 mg/mL collagenase D and 200 μg/mL DNAse mix (Roche; Indianapolis, IN) by incubating at 37°C for 45 min with mixing every 5 min. The digestants were then passed through 40 micron filter, loaded on Histopaque®-1077 (Sigma) and spun at 2000 rpm for 20 min without brake. Cells at the interphase were collected and washed in 5% RPMI 1640 containing 1 mM EDTA. The cells were stained for surface expression of CD4 and CD8, as well as intracellular staining of Foxp3. Flow cytometry data were acquired on LSRII (BD Biosciences) and analyzed using Flowjo software (Tree Star).
TCGA patient survival analysis
We downloaded the level 3 CNA and clinical data for 367 metastatic melanoma patients from the Broad Institute’s GDAC firehose website (https://gdac.broadinstitute.org/). Similar to the WES analysis, we used log2 tumor vs normal ratio > 0.7 (< −0.7) to define copy gain or loss. A patient is defined as a mutant if it carries the loss of any of the regular interferon genes or gain of any of the 4 interferon pathway inhibitors. As a result, 134 patients carry CNAs whereas the other 233 do not. We found that the patients with containing CNAs have significantly shorter overall survival (median: 40 months) than the wild-type patients (median: 48.2 months, p = 0.0018, log rank test).
QUALIFICATION AND STATISTICAL ANALYSIS
All group results are expressed as mean ± SEM, if not stated otherwise. Comparisons between groups were made using the two-tailed Student’s T-Test, unless stated otherwise. Statistical significance as compared to untreated controls was denoted with * (p < 0.05), ** (p < 0.01), *** (p < 0.001) in the Figures and Figure legends. Statistical analysis was performed in Graph Pad PRISM 6.
DATA AND SOFTWARE AVAILABILITY
The microarray data have been submitted in MIME-compliant format to GEO, with an accession number of GSE85898. The WES data are currently being submitted to the dbGap database. While the accession number is pending, the data will be made available to interested parties upon direct request to the lead author.
Supplementary Material
Figure S1. Difference in CNA and SNV enrichment between non-responders and responders to ipilimumab therapy, related to Figure 1A. (A) The frequency of average total mutation (CNA + SNV) ratios between 12 non-responders and 4 responders in a total of 1,000 simulations. (B) The frequency of only SNV ratios between 12 non-responders and 4 responders.
Figure S2. Landscape representation of CNAs of IFN-γ pathway genes in melanoma tumors from non-responders and responders to ipilimumab of an independent dataset, related to Figure 1C. Each column represents one sample. The bar graph at the top of the figure represents the total number of genes with CNAs in that specific sample. The numbers on the left side represent the percentage of melanoma samples carrying CNAs of each specific gene. Gene names are listed on the right.
Figure S3. Two common interferon gene clusters deleted in ipilimumab non-responders, related to Figure 1&2. (A) The most frequent CNAs in ipilimumab non-responders located at chromosome 9p21.3, including IFN-α/β genes, MTAP, and miR31, etc. (B) The second frequent CNAs in ipilimumab non-responders located at chromosome 10q23.31, including IFIT1, 2, and 3, etc.
Figure S4. Responsiveness of mouse cancer cell lines B16/BL6, MB49, and Renca to IFN-γ treatment, related to Figure 3. Tumor cells treated with varying concentrations of IFN-γ for 48 h were assessed for their survivals.
Table S1. Patient clinical characteristics and clinical responses. Related to Figure 1.
Table S2. IFN-γ pathway related genes. Related to Figure 1.
Table S3. Responders and non-responders to ipilimumab with exception of all SD patients. Related to Figure 1.
Table S4. The log2 fold change of selected probes after IFN-γ stimulation of each cell line. Related to Figure 2.
Table.
KEY RESOURCES TABLE
| REAGENT or RESOURCE | SOURCE | IDENTIFIER |
|---|---|---|
| Antibodies | ||
| InVivoMAb Anti-Mouse CTLA-4 | Bio X cell | Cat# BE0131; RRID: AB_10950184 |
| Anti-Human CD90 PE | eBiosciences | Cat# 12-0909-42; RRID:AB_10670624 |
| Anti-Human MCSP-1 PE | Miltenyi Biotec | Cat# 130-091-225; RRID:AB_244198 |
| Mouse Monoclonal Anti-Human IFNGR1 | Novus Biologicals | Cat# NB100-64793; RRID:AB_959548 |
| Anti-Mouse CD4 Pacific Blue | Biolegend | Cat# 100534; RRID:AB_493375 |
| Anti-Mouse CD8 BV785 | Biolegend | Cat# 100750; RRID:AB_2562610 |
| Anti-Mouse Foxp3-AF532 | eBiosciences | Cat# 58-5773-82 RRID:AB_11218870 |
| Chemicals, Peptides, and Recombinant Proteins | ||
| Collagenase Type I | Thermo Fisher Scientific | Cat# 17100017 |
| Collagenase D | Roche | Cat#11088866001 |
| DNase I | Thermo Fisher Scientific | Cat# EN0525 |
| Puromycin | Thermo Fisher Scientific | Cat# A1113803 |
| Insulin-Selenium-Transferrin Supplement | Thermo Fisher Scientific | Cat# 41400045 |
| Recombinant Human IFN-γ | Peprotech | Cat# 300-02 |
| Recominant Murine IFN-γ | Peprotech | Cat# 315-05 |
| SyBR Green PCR Master Mix | Thermo Fisher Scientific | Cat# 4309155 |
| Critical Commercial Assays | ||
| PowerPlex 16 HS System | Promega | Cat# DC21 |
| RNeasy Mini Kit | Qiagen | Cat# 74104 |
| RNeasy Plus Micro Kit | Qiagen | Cat# 74034 |
| miScript II RT Kit | Qiagen | Cat# 21816 |
| Pierce BCA Protein Assay Kit | Thermo Fisher Scientific | Cat# 23227 |
| CellTiter 96 Aqueous One Solution Cell Proliferation Assay Kit | Promega | Cat# G3582 |
| CellTrace™ CFSE Cell Proliferation Kit | ThermoFisher Scientific | Cat# C34554 |
| Annexin V Apoptosis Detection Kit I | BD Biosciences | Cat# 556547 |
| GeneChip Human Genome U133 2.0 | Affymetrix | Part# 902483 |
| Deposited Data | ||
| Raw data files for microarray analysis | NCBI Gene Expression Omnibus | Accession# GSE85898 |
| Raw data files for WES | dbGap | Accession# pending |
| Experimental Models: Cell Lines | ||
| Human melanoma-derived cell lines (C1–6) | This paper | |
| GM-CSF-expressing B16/BL6 melanoma (GVAX) | James Allison | Quezada, S.A., et al. 2006 {Quezada, 2006 #14} |
| IFNGR1 shRNA-transduced B16/BL6 melanoma | This paper | |
| Scrambled shRNA-transduced B16/BL6 melanoma | This paper | |
| Experimental Models: Organisms/Strains | ||
| C57BL/6J mice | Jackson Laboratories | Stock# 000664 |
| Recombinant DNA | ||
| Lentiviral particles encoding IFNGR1 shRNA | Santa Cruz | Cat# sc-35636-V |
| Lentivirial particles encoding scrambled shRNA | Santa Cruz | Cat# sc-108080 |
| Sequence-Based Reagents | ||
| SureSelect Human All Exon 44 Mb V2.0 Bait Set | Agilent | Part# 5190-2885 |
| SureSelect-XT Target Enrichment | Agilent | Part# 5190-2902 |
| Software and Algorithms | ||
| BWA Aligner (bwa-0.7.5a) | Li and Durbin, 2009 | http://bio-bwa.sourceforge.net |
| Picard (V1 112) “MarkDuplicates” module | Broad Institute | http://broadinstitute.github.io/picard |
| Mutect (v1.1.4) | Broad Institute | https://www.broadinstitute.org/cancer/cga/mutect |
| ExomeCN | Jianhua Zhang | MD Anderson Cancer Center |
| Affy | Gautier L, et al, 2004 | https://bioconductor.org/packages/release/bioc/html/affy.html |
Highlights.
Melanoma tumors with loss of IFN-γ signaling lack response to ipilimumab
Cell lines that are resistant to IFN-γ in vitro have defective IFN-γ pathway
Mice bearing IFNGR1 knockdown tumors have high mortality despite anti-CTLA-4 therapy
Acknowledgments
The research work was supported by a Stand Up To Cancer-Cancer Research Institute Cancer Immunology Dream Team Translational Research Grant (SU2C-AACR-DT1012; J.P.A., P.S., S.K.S., J.G.; Stand Up To Cancer is a program of the Entertainment Industry Foundation administered by the American Association for Cancer Research [AACR]); Conquer Cancer Foundation-American Society of Clinical Oncology (ASCO) 2012 Young Investigator Award (J.G.); Cancer Prevention Research in Texas (CPRIT) RP120108 (P.S.); NIH/NCI R01 CA1633793 (P.S.); NIH/NCI K12 CA088084 (J.G.), NIH/NCI P30CA016672 (M.D. Anderson Cancer Center institutional grant), the Melanoma Research Alliance Team Science Award (JAW), the Kenedy Memorial Foundation grant # 0727030 (JAW), and philanthropic contributions to The University of Texas MD Anderson Cancer Center Melanoma Moon Shot Program. STR DNA fingerprinting was done by the Cancer Center Support Grant-funded Characterized Cell Line Core, NCI # CA016672. Drs. Sharma and Allison are founders and advisors for Jounce Therapeutics. Dr. Sharma also serves as a consultant for BMS, AstraZeneca, Amgen and Glaxo SmithKline. Dr. Allison is an inventor of intellectual property owned by the University of California, Berkeley, and licensed to BMS and has received royalties from BMS. Dr. Allison is also inventor of intellectual property owned by Memorial-Sloan Kettering Cancer Center and licensed to Merck. Drs. Sharma and Allison are members of the Parker Institute for Cancer Immunotherapy. Dr. Roszik is a paid consultant for Merck KGaA, Darmstadt, Germany. Dr. Wargo has honoraria from speakers’ bureau of Dava Oncology and Illumina and is an advisory board member for GlaxoSmithKline, Bristol-Myers Squibb, Novartis and Roche/Genentech. She has received research support from Roche-Genentech, GlaxoSmithKline, Novartis, and Bristol-Myers Squbb.
Footnotes
AUTHOR CONTRIBUTIONS
PS was responsible for overall experimental design and supervision for laboratory studies, data analyses and manuscript editing; JG was responsible for in vitro and in vivo experimental design, clinical data collection, analysis, and manuscript writing; LZS designed and did the experiments with cells and mice, analyzed data and contributed to manuscript writing; JC, LX, and QH performed in vitro and animal studies; HZ, TC, JR and SEW performed WES and microarray data analysis and contributed to manuscript writing; CB provided melanoma derived cell lines and WES analysis of these cell lines; JW and PLC contributed to melanoma clinical data and WES data collection and analysis; PH, JPA and AF contributed to overall data analyses and manuscript construction.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alegre ML, Shiels H, Thompson CB, Gajewski TF. Expression and function of CTLA-4 in Th1 and Th2 cells. J Immunol. 1998;161:3347–3356. [PubMed] [Google Scholar]
- Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, Chow LQ, Vokes EE, Felip E, Holgado E, et al. Nivolumab versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. New Engl J Med. 2015;373:1627–1639. doi: 10.1056/NEJMoa1507643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H, Liakou CI, Kamat A, Pettaway C, Ward JF, Tang DN, Sun J, Jungbluth AA, Troncoso P, Logothetis C, et al. Anti-CTLA-4 therapy results in higher CD4+ICOShi T cell frequency and IFN-gamma levels in both nonmalignant and malignant prostate tissues. Proc Natl Acad Sci U S A. 2009;106:2729–2734. doi: 10.1073/pnas.0813175106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin YE, Kitagawa M, Kuida K, Flavell RA, Fu XY. Activation of the STAT signaling pathway can cause expression of caspase 1 and apoptosis. Molecular and cellular biology. 1997;17:5328–5337. doi: 10.1128/mcb.17.9.5328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cibulskis K, Lawrence MS, Carter SL, Sivachenko A, Jaffe D, Sougnez C, Gabriel S, Meyerson M, Lander ES, Getz G. Sensitive detection of somatic point mutations in impure and heterogeneous cancer samples. Nature biotechnology. 2013;31:213–219. doi: 10.1038/nbt.2514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Detjen KM, Farwig K, Welzel M, Wiedenmann B, Rosewicz S. Interferon gamma inhibits growth of human pancreatic carcinoma cells via caspase-1 dependent induction of apoptosis. Gut. 2001;49:251–262. doi: 10.1136/gut.49.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dulos J, Carven GJ, van Boxtel SJ, Evers S, Driessen-Engels LJ, Hobo W, Gorecka MA, de Haan AF, Mulders P, Punt CJ, et al. PD-1 blockade augments Th1 and Th17 and suppresses Th2 responses in peripheral blood from patients with prostate and advanced melanoma cancer. Journal of immunotherapy. 2012;35:169–178. doi: 10.1097/CJI.0b013e318247a4e7. [DOI] [PubMed] [Google Scholar]
- Dunn GP, Koebel CM, Schreiber RD. Interferons, immunity and cancer immunoediting. Nat Rev Immunol. 2006;6:836–848. doi: 10.1038/nri1961. [DOI] [PubMed] [Google Scholar]
- Dunn GP, Sheehan KC, Old LJ, Schreiber RD. IFN unresponsiveness in LNCaP cells due to the lack of JAK1 gene expression. Cancer Res. 2005;65:3447–3453. doi: 10.1158/0008-5472.CAN-04-4316. [DOI] [PubMed] [Google Scholar]
- Fisher S, Barry A, Abreu J, Minie B, Nolan J, Delorey TM, Young G, Fennell TJ, Allen A, Ambrogio L, et al. A scalable, fully automated process for construction of sequence-ready human exome targeted capture libraries. Genome biology. 2011;12:R1. doi: 10.1186/gb-2011-12-1-r1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu T, He Q, Sharma P. The ICOS/ICOSL pathway is required for optimal antitumor responses mediated by anti-CTLA-4 therapy. Cancer Res. 2011;71:5445–5454. doi: 10.1158/0008-5472.CAN-11-1138. [DOI] [PubMed] [Google Scholar]
- Gnirke A, Melnikov A, Maguire J, Rogov P, LeProust EM, Brockman W, Fennell T, Giannoukos G, Fisher S, Russ C, et al. Solution hybrid selection with ultra-long oligonucleotides for massively parallel targeted sequencing. Nature biotechnology. 2009;27:182–189. doi: 10.1038/nbt.1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodi FS, O'Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel JC, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–723. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikeda H, Old LJ, Schreiber RD. The roles of IFN gamma in protection against tumor development and cancer immunoediting. Cytokine Growth Factor Rev. 2002;13:95–109. doi: 10.1016/s1359-6101(01)00038-7. [DOI] [PubMed] [Google Scholar]
- Kaplan DH, Shankaran V, Dighe AS, Stockert E, Aguet M, Old LJ, Schreiber RD. Demonstration of an interferon gamma-dependent tumor surveillance system in immunocompetent mice. Proc Natl Acad Sci U S A. 1998;95:7556–7561. doi: 10.1073/pnas.95.13.7556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liakou CI, Kamat A, Tang DN, Chen H, Sun J, Troncoso P, Logothetis C, Sharma P. CTLA-4 blockade increases IFNgamma-producing CD4+ICOShi cells to shift the ratio of effector to regulatory T cells in cancer patients. Proc Natl Acad Sci U S A. 2008;105:14987–14992. doi: 10.1073/pnas.0806075105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu B, Gross M, ten Hoeve J, Shuai K. A transcriptional corepressor of Stat1 with an essential LXXLL signature motif. Proc Natl Acad Sci U S A. 2001;98:3203–3207. doi: 10.1073/pnas.051489598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motzer RJ, Escudier B, McDermott DF, George S, Hammers HJ, Srinivas S, Tykodi SS, Sosman JA, Procopio G, Plimack ER, et al. Nivolumab versus Everolimus in Advanced Renal-Cell Carcinoma. N Engl J Med. 2015;373:1803–1813. doi: 10.1056/NEJMoa1510665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mowen KA, Tang J, Zhu W, Schurter BT, Shuai K, Herschman HR, David M. Arginine methylation of STAT1 modulates IFNalpha/beta-induced transcription. Cell. 2001;104:731–741. doi: 10.1016/s0092-8674(01)00269-0. [DOI] [PubMed] [Google Scholar]
- Olshen AB, Venkatraman ES, Lucito R, Wigler M. Circular binary segmentation for the analysis of array-based DNA copy number data. Biostatistics. 2004;5:557–572. doi: 10.1093/biostatistics/kxh008. [DOI] [PubMed] [Google Scholar]
- Paradis TJ, Floyd E, Burkwit J, Cole SH, Brunson B, Elliott E, Gilman S, Gladue RP. The anti-tumor activity of anti-CTLA-4 is mediated through its induction of IFN gamma. Cancer immunology, immunotherapy : CII. 2001;50:125–133. doi: 10.1007/s002620100181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng W, Liu C, Xu C, Lou Y, Chen J, Yang Y, Yagita H, Overwijk WW, Lizee G, Radvanyi L, et al. PD-1 blockade enhances T-cell migration to tumors by elevating IFN-gamma inducible chemokines. Cancer Res. 2012;72:5209–5218. doi: 10.1158/0008-5472.CAN-12-1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quezada SA, Peggs KS, Curran MA, Allison JP. CTLA4 blockade and GM-CSF combination immunotherapy alters the intratumor balance of effector and regulatory T cells. J Clin Invest. 2006;116:1935–1945. doi: 10.1172/JCI27745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reich NC. A death-promoting role for ISG54/IFIT2. Journal of interferon & cytokine research : the official journal of the International Society for Interferon and Cytokine Research. 2013;33:199–205. doi: 10.1089/jir.2012.0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert C, Thomas L, Bondarenko I, O'Day S, MDJ, Garbe C, Lebbe C, Baurain JF, Testori A, Grob JJ, et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 2011;364:2517–2526. doi: 10.1056/NEJMoa1104621. [DOI] [PubMed] [Google Scholar]
- Rosenberg JE, Hoffman-Censits J, Powles T, van der Heijden MS, Balar AV, Necchi A, Dawson N, O'Donnell PH, Balmanoukian A, Loriot Y, et al. Atezolizumab in patients with locally 18 advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: a single-arm, multicentre, phase 2 trial. Lancet. 2016;387:1909–1920. doi: 10.1016/S0140-6736(16)00561-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma P, Allison JP. The future of immune checkpoint therapy. Science. 2015a;348:56–61. doi: 10.1126/science.aaa8172. [DOI] [PubMed] [Google Scholar]
- Sharma P, Allison JP. Immune checkpoint targeting in cancer therapy: toward combination strategies with curative potential. Cell. 2015b;161:205–214. doi: 10.1016/j.cell.2015.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherry ST, Ward MH, Kholodov M, Baker J, Phan L, Smigielski EM, Sirotkin K. dbSNP: the NCBI database of genetic variation. Nucleic acids research. 2001;29:308–311. doi: 10.1093/nar/29.1.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi LZ, Fu T, Guan B, Chen J, Blando JM, Allison JP, Xiong L, Subudhi SK, Gao J, Sharma P. Interdependent IL-7 and IFN-gamma signalling in T-cell controls tumour eradication by combined alpha-CTLA-4+alpha-PD-1 therapy. Nature communications. 2016;7:12335. doi: 10.1038/ncomms12335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi LZ, Kalupahana NS, Turnis ME, Neale G, Hock H, Vignali DA, Chi H. Inhibitory role of the transcription repressor Gfi1 in the generation of thymus-derived regulatory T cells. Proc Natl Acad Sci U S A. 2013;110:E3198–3205. doi: 10.1073/pnas.1300950110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song MM, Shuai K. The suppressor of cytokine signaling (SOCS) 1 and SOCS3 but not SOCS2 proteins inhibit interferon-mediated antiviral and antiproliferative activities. J Biol Chem. 1998;273:35056–35062. doi: 10.1074/jbc.273.52.35056. [DOI] [PubMed] [Google Scholar]
- Szabo SJ, Sullivan BM, Peng SL, Glimcher LH. Molecular mechanisms regulating Th1 immune responses. Annu Rev Immunol. 2003;21:713–758. doi: 10.1146/annurev.immunol.21.120601.140942. [DOI] [PubMed] [Google Scholar]
- Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. Journal of the National Cancer Institute. 2000;92:205–216. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- Van Allen EM, Miao D, Schilling B, Shukla SA, Blank C, Zimmer L, Sucker A, Hillen U, Geukes Foppen MH, Goldinger SM, et al. Genomic correlates of response to CTLA-4 blockade in metastatic melanoma. Science. 2015;350:207–211. doi: 10.1126/science.aad0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Heide V, Mohnle P, Rink J, Briegel J, Kreth S. Down-regulation of MicroRNA-31 in CD4+ T Cells Contributes to Immunosuppression in Human Sepsis by Promoting TH2 Skewing. Anesthesiology. 2016;124:908–922. doi: 10.1097/ALN.0000000000001031. [DOI] [PubMed] [Google Scholar]
- Wang K, Li M, Hakonarson H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic acids research. 2010;38:e164. doi: 10.1093/nar/gkq603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaretsky JM, Garcia-Diaz A, Shin DS, Escuin-Ordinas H, Hugo W, Hu-Lieskovan S, Torrejon DY, Abril-Rodriguez G, Sandoval S, Barthly L, et al. Mutations Associated with Acquired Resistance to PD-1 Blockade in Melanoma. N Engl J Med. 2016 doi: 10.1056/NEJMoa1604958. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Difference in CNA and SNV enrichment between non-responders and responders to ipilimumab therapy, related to Figure 1A. (A) The frequency of average total mutation (CNA + SNV) ratios between 12 non-responders and 4 responders in a total of 1,000 simulations. (B) The frequency of only SNV ratios between 12 non-responders and 4 responders.
Figure S2. Landscape representation of CNAs of IFN-γ pathway genes in melanoma tumors from non-responders and responders to ipilimumab of an independent dataset, related to Figure 1C. Each column represents one sample. The bar graph at the top of the figure represents the total number of genes with CNAs in that specific sample. The numbers on the left side represent the percentage of melanoma samples carrying CNAs of each specific gene. Gene names are listed on the right.
Figure S3. Two common interferon gene clusters deleted in ipilimumab non-responders, related to Figure 1&2. (A) The most frequent CNAs in ipilimumab non-responders located at chromosome 9p21.3, including IFN-α/β genes, MTAP, and miR31, etc. (B) The second frequent CNAs in ipilimumab non-responders located at chromosome 10q23.31, including IFIT1, 2, and 3, etc.
Figure S4. Responsiveness of mouse cancer cell lines B16/BL6, MB49, and Renca to IFN-γ treatment, related to Figure 3. Tumor cells treated with varying concentrations of IFN-γ for 48 h were assessed for their survivals.
Table S1. Patient clinical characteristics and clinical responses. Related to Figure 1.
Table S2. IFN-γ pathway related genes. Related to Figure 1.
Table S3. Responders and non-responders to ipilimumab with exception of all SD patients. Related to Figure 1.
Table S4. The log2 fold change of selected probes after IFN-γ stimulation of each cell line. Related to Figure 2.