Abstract
Atrial fibrillation (AF) is the most common cardiac arrhythmia and shares many of the same risk factors as another common clinical condition, sleep apnea. The estimated prevalence of sleep apnea has increased over the past decade, and reflects a parallel increase in the most prominent risk factors of obesity and overweight. Both obstructive and central sleep apnea have been associated with AF in multiple studies, with the risk of AF increasing 2-4-fold compared to those without sleep breathing disorder. Continuous positive airway pressure (CPAP) has been shown to reduce the rate of AF recurrence following catheter ablation in patients with sleep apnea. However, the mechanisms by which sleep apnea precipitates AF or vice versa, remain unclear. In this Review, we examine the current date linking AF and sleep apnea, discuss the existing data supporting a mechanistic link between the two conditions, present the existing evidence for the effectiveness of CPAP in this growing population, and suggest approaches to screen AF patients for sleep breathing disorders.
Keywords: Sleep Apnea, Atrial Fibrillation, CPAP, Outcomes, Arrhythmia Control
Introduction
Atrial fibrillation (AF) is the most commonly encountered arrhythmia in clinical practice. There are an estimated 33 million individuals with AF worldwide, with approximately 5 million new cases annually. The incidence and prevalence of AF increases with age, with a 2-3-fold increase between ages 60 and 80.[1,2] Sleep disordered breathing (SDB), characterized by respiratory pauses of at least 10 seconds during sleep that result in oxyhemoglobin desaturation, is estimated to affect 17% of men and 9% of women aged 50-70.[3] These estimates are significantly increased compared to two decades ago, and reflect a parallel increase in the most prominent risk factors for SBD, overweight and obesity.[3] SDB encompasses a broad clinical spectrum ranging from mild airway resistance to prolonged apnea.
Obstructive sleep apnea (OSA), characterized by recurrent partial or complete collapse of the upper airway during sleep and associated with excessive daytime sleepiness, is estimated to affect 14% of men and 5% of adult women.[3] In the developed world, the majority of OSA cases are secondary, occurring as a result of overweight and obesity.[3] In secondary OSA, local fat deposition in the neck has been implicated as the cause of upper airway collapse and impaired neuromuscular control of the airway. In a small proportion of patients with clinical evidence of OSA, no abnormality of the upper airway can be identified on routine clinical examination. These individuals are considered to have idiopathic OSA. Previous work utilizing acoustic ultrasound and x-ray demonstrated that these individuals often have relatively small mandibles and posterior displacement of the mandibular symphysis, both of which affect the support to the anterior pharyngeal wall.[4]
Central sleep apnea (CSA) is characterized by diminished or absent respiratory effort during sleep, also associated with oxygen desaturation and daytime somnolence. In some cases of CSA, very shallow breathing can alternate with very deep breathing, as is the case with Cheyne-Stokes respiration. The estimated prevalence of CSA varies, but has been thought to account for up to one-fifth of all cases of SDB.[5] Similar to OSA, CSA occurs most often secondary to an underlying condition such as heart failure, neuromuscular dysfunction or narcotic use. Primary or idiopathic CSA is quite rare, and results from decreased input to respiratory motor neurons. The causes of idiopathic CSA are not known.
Association Between AF And Sleep Apnea
Obstructive Sleep Apnea And AF
OSA has been shown to contribute to increased AF burden.[1,6] Epidemiologic studies have identified a strong association of OSA and AF, with an increased risk for AF that is 2 to 4 times that of those without SDB.[7,8] In a large, prospective, community-based cohort, Mehra and colleagues found that individuals with SDB had 4 times the odds of AF as those without SDB (OR 4.02, 95% CI 1.03- 15.74) after adjustment for age, sex, BMI and prevalent coronary heart disease. A secondary analysis of the same cohort found no dose-response relationship between risk for AF and severe to very severe SDB.[7] In contrast, Tanigawa et al observed that the risk of AF was linearly associated with severity of SDB in a communitybased study of Japanese men; the odds of AF increased more than 2-fold for those with 5-15 apneic or hypopneic events per hour (2.47, 95% CI 0.91-6.69) and more than 5-fold for those with >15 apneic or hypopneic events per hour (5.66, 95% CI 1.75-18.34).[9] Gami et al prospectively assessed the risk of OSA, as determined by the Berlin questionnaire among 524 patients with AF or atrial flutter referred to a tertiary care center for cardioversion. After adjustment for risk factors, AF was significantly associated with OSA, with AF conferring twice the odds of OSA (OR 2.19, 95% CI 1.40-3.42) compared to a general cardiology population without AF.[10] Not all studies, however, have shown an association between OSA and AF. In a case-control study of patients with lone AF that excluded diabetics, Porthan and colleagues observed that the prevalence of sleep apnea in AF patients did not differ from those without AF (32% versus 29%, p=0.67).[11] However, the number of subjects in this study was small and the power to detect an association was therefore limited.
Central Sleep Apnea And AF
In clinical practice, OSA and CSA often coexist. Generally, patients are considered to have CSA when more than 50% of their apneic and hypopneic episodes are associated with reduced or absent respiratory drive.[5] As discussed above, this condition is prevalent among particular populations such as those with heart failure and primary neuromuscular disorders, and has also been associated with AF. Sin et al found AF to be associated with CSA in a retrospective analysis of 450 individuals with CHF referred to a tertiary care sleep center.[12] In this analysis, AF conferred a 4-fold increase in the risk of CSA (4.13, 95% CI 1.53-11.4), but no increased risk for OSA. An association between CSA and AF has also been observed in community-based cohorts without overt heart failure or underlying cardiac dysfunction. In an analysis of the Sleep Heart Health Study, we demonstrated that CSA conferred double the risk for incident AF (OR 2.06, 95% CI 1.23-3.44, p=0.0057) in an unselected population without clinical signs of SDB.[13] This association was also confirmed prospectively by Leung et al in a population with presumed idiopathic CSA, free of heart failure, coronary artery disease or stroke. The risk of AF was higher in those with CSA (3.3% versus 1.7%, p<0.001) than in those without SDB.[14]
Potential Mechanisms
Although the majority of evidence supports a strong association between sleep apnea and AF, it remains unclear whether SDB is causal in the development of AF, as the two conditions share many of the same risk factors. Furthermore, the mechanism by which this may occur remains unclear. For example, obesity is a common risk factor for SDB and AF. But whether the link underlying the association is obesity itself or resulting effects on left atrial pressure and size, inflammatory and pro-fibrotic molecules, insulin resistance, or increased mean arterial blood pressure and atrial fibrosis is unknown. It has been suggested that the physiologic changes of SDB including intermittent hypoxia, hypercarbia, and intrathoracic pressure fluctuations predispose to arrhythmia through electrical and structural remodeling.[15]
The proposed mechanism by which hypoxia promotes AF is via autonomic nervous system dysfunction and electrical remodeling. In a dog model of intermittent hypoxia, Lu and colleagues found that hypoxia initially resulted in parallel changes in heart rate variability (HRV) indices associated with sympathetic and parasympathetic activity such that the atrial effective refractory period (AERP) and AF vulnerability were not affected.[16] However, with repeated hypoxic episodes, the parasympathetic indices of HRV were increased to a greater extent relative to sympathetic indices, and the AERP and AF vulnerability were also increased. This suggests that autonomic system imbalance may precipitate electrical changes in the atria that predispose to AF. Autonomic nervous system dysfunction is further supported in the development of AF based on studies of CSA patients in whom increased concentrations of plasma and urinary norepinephrine and epinephrine have been documented, independent of left ventricular dysfunction.[17]
Hypercarbia has also been implicated in electrical remodeling. In a sheep model, Stevenson et al found an inverse linear association between the effective refractory periods of the right and left atria and end-tidal CO2 levels in hypercarbic sheep that was not present in the hypoxic or control sheep.[18] In addition, atrial conduction times during pacing at a constant cycle length and during extrastimulus testing were significantly prolonged during and after resolution of hypercapnia. In contrast, no corresponding changes in conduction times were observed in the hypoxic or control sheep during or after resolution of hypoxia. Interestingly, AF vulnerability was eliminated during hypercapnia but was significantly increased following resolution of hypercapnia and normalization of ERP. This suggests that hypercapnia may not promote AF acutely, but rather may promote electrical substrate remodeling over time after repeated exposure.
There is also data suggesting that hypercapnia can result in cardiac structural changes. In studies of ventricular myocytes isolated from rat hearts, White et al observed that exposure to medium with high levels of CO2 resulted in decreased cell to cell conduction.[19] Vorperian and colleagues exposed anesthesized dogs to an elevated mixture of inhaled CO2 with resultant decrease in serum pH. They found that hypercarbia resulted in slowed propagation of impulses in the transverse direction, perhaps due to connexin dysfunction.[20] However, it is unclear why these changes would occur selectively in the transverse rather than longitudinal direction and whether these structural changes occur in the atrium as well.
Fluctuations in intrathoracic pressure have also been implicated in electrical remodeling.[21] Sympathetic stimulation during acute episodes of tracheal obstruction can produce increased intracellular calcium load, leading to shortening of action potential duration and initiation of AF.[22-24] In a porcine model, Linz and colleagues simulated tracheal occlusion with and without the application of negative intrathoracic pressure (NTP).[25] They found a significant decrease (161 versus 96 ms, p<0.0001) in the atrial effective refractory period (AERP) after two minutes of tracheal occlusion with -100mbar. In contrast, tracheal occlusion without NTP had no effect on AERP. The change in AERP was associated with increased inducibility of AF (0% normal breathing or tracheal occlusion without NTP versus 91% with NTP). Linz also investigated the effect of autonomic changes; atropine prevented AERP shortening in NTP, did not affect the AERP during normal breathing and decreased AF inducibility with NTP from 91% to 17%. These data suggest that negative intrathoracic pressure can precipitate electrophysiologic changes that increase the inducibility of AF, and that these changes may be mediated by an autonomic effect.
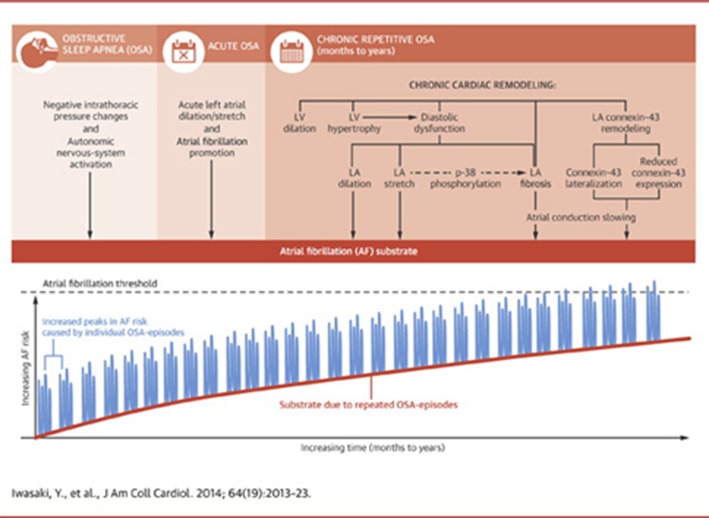
There is also evidence of structural remodeling resulting from repeated episodes of OSA with fluctuating intrathoracic pressure. Iwasaki and colleagues created a rat model of OSA, in which the airway of intubated rats was occluded at end expiration for 40s followed by an 80s recovery period 20 times per day, 5 days per week for 4 weeks. After OSA cycles, rats were ventilated with room air and then extubated.[26] This group was compared to rats subjected to the same ventilator-arrest cycles but without airway closure, and to rats ventilated with room air throughout the procedure. OSA produced a statistically significant increase in left atrial dilation that was not seen in the sham or control groups. No significant differences in atrial ERP or sinus node recovery time was found between the groups. However, conduction velocity was decreased, and AF inducibility and mean AF duration were increased significantly (p<0.05) in OSA rats compared with sham rats. The investigators also observed structural differences between the groups; there was increased fibrosis, decreased expression of connexin-43, and a lateralized distribution of this protein in OSA rats compared to sham and control rats. These structural changes may explain the changes in conduction velocity and inducibility of AF in the absence of changes in atrial refractoriness.
Ramos et al also created a rat model of OSA and similarly demonstrated increased atrial fibrosis (11.9 versus 8.32, p<0.01) in OSA rats compared to sham rats.[27] Amounts of angiotensinconverting enzyme were significantly increased, and matrix metalloproteinase-2 significantly decreased, in OSA rats compared to sham rats.[27] Thus, OSA may also predispose to AF through a mechanism of left atrial fibrosis. Taken together, there is a growing body of evidence that suggests that the physiologic effects of chronic SDB predispose to AF via electrical and structural remodeling that occurs over time ([Figure 1])
Figure 1. Mechanisms by Which OSA Leads to AF.
There is data from humans supporting electrical and structural remodeling secondary to OSA. Dimitri et al compared electrophysiologic parameters among 20 patients with OSA and 20 without OSA undergoing ablation for paroxysmal AF.[15] Electroanatomic maps of the right and left atria were obtained in all patients to compare the voltage, conduction velocity and distribution of complex atrial electrograms. There was no difference in the right or left atrial refractory periods between those with OSA and those without (p=0.9). However, patients with OSA had prolonged conduction times along the coronary sinus and RA (p=0.02), a longer corrected sinus node recovery time (p=0.02), and a greater number (p=0.003) and duration (p=0.03) of complex electrograms along the crista terminalis. OSA patients also had a longer p wave duration (p=0.01), lower atrial voltage (RA p<0.01, LA p=0.02), slower atrial conduction velocity (RA p=0.001, LA p=0.02) and more complex electrograms in both atria (RA p=0.02, LA p=0.01) compared to those without OSA.[15] In prior studies, p wave duration and dispersion, measures of prolonged and heterogeneous atrial conduction have been found to correlate with severity of OSA.[28,29] These data suggest a possible difference in underlying atrial substrate between AF patients with and without sleep apnea.
Clinical Outcomes And Effect Of CPAP Treatment
In humans, OSA confers increased risk of recurrent AF that is mitigated by CPAP therapy. In a population of patients with AF and atrial flutter referred for electrical cardioversion, Kanagala and colleagues found that untreated OSA was associated with increased AF recurrence.[30] Of the 39 patients with OSA, 27 were not receiving CPAP therapy (n=25) or were using it inappropriately (n=2). Among those with OSA, patients receiving CPAP had a lower rate of recurrence of AF at one year than those not receiving CPAP (42% versus 82%, p=0.013). Importantly, the recurrence rate among CPAP-treated patients was similar to control patients without OSA. Additionally, in the 25 patients with untreated OSA, the nocturnal oxygen desaturation was greater among those with recurrent AF (n=20) compared to those without AF recurrence (n=5, p=0.034).
The effect of OSA and CPAP has also been examined among patients undergoing catheter ablation of AF. Patel et al evaluated 3,000 consecutive patients undergoing pulmonary vein isolation between January 2004 and December 2007, of which 640 (21.3%) were identified as having OSA. Overall, patients with OSA had a statistically significant increase in procedural failures (p=0.024) compared to patients without OSA. Among those with paroxysmal AF, OSA patients had more non-pulmonary vein triggers and posterior wall firing than patients without OSA (20% versus 8%, p<0.001). This was also true in non-paroxysmal AF patients; patients with OSA had more non-pulmonary vein triggers than those without OSA (31% versus 19%, p = 0.001). Importantly, treatment with CPAP reduced the rate of AF recurrence (79% versus 68%, p=0.003). The presence of non-pulmonary vein triggers and absence of CPAP use strongly predicted ablation failure (HR 8.81, p<0.001).
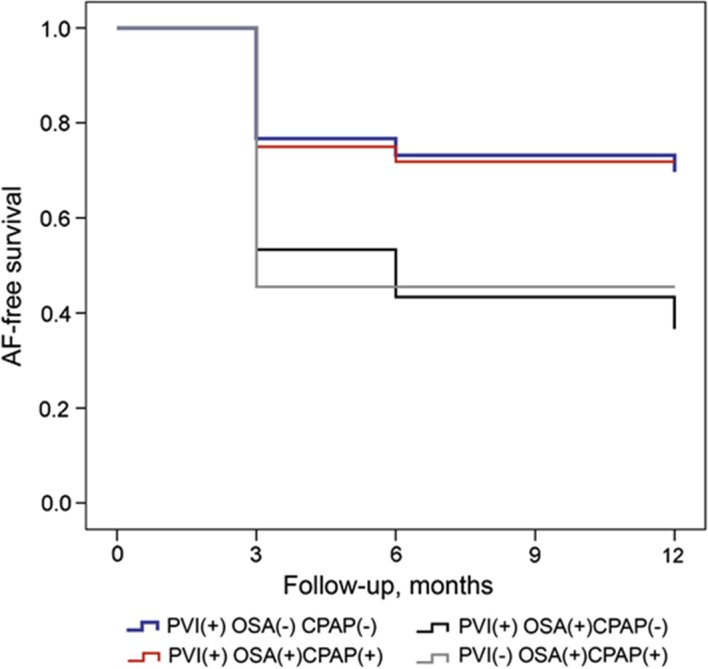
We found a similar pattern of outcomes when we examined 426 consecutive patients undergoing PVI between 2007 and 2010 at our institution. Sixty-two patients had a diagnosis of OSA confirmed by polysomnography, of which 32 were identified as receiving CPAP therapy. At one year following first PVI, 71.8% of OSA patients using CPAP were free of AF recurrence as compared to 36.7% of OSA patients not using CPAP (p=0.01). Survival analysis demonstrated that the rate of recurrence among CPAP-treated individuals was similar to that of patients without OSA at 1 year (67% versus 71.8%, p=0.94). In addition, AF-free survival off antiarrhythmic medications was higher among CPAP users compared to non-users (65.6% versus 33.3%, p=0.02; [Figure 2]).
Figure 2. Kaplan-Meier Survival Curves According to Treatment Group.
In another recent study, the results of polysomnography were compared between patients with and without SDB who have undergone catheter ablation for AF. Naruse et al obtained overnight polysomnograms in 153 patients who had undergone pulmonary vein isolation one week earlier.[31] One hundred sixteen of the 153 patients (76%) were diagnosed with OSA. Over a mean follow-up period of 18 months, AF recurrence in OSA patients not receiving CPAP was higher than in those without OSA as well as those with OSA on CPAP therapy (53% versus 22% versus 33%, respectively; p<0.01). After controlling for LA volume, plasma NT-pro-BNP and LVEF on multivariate analysis, CPAP use was found to decrease the risk of AF recurrence. In Cox model analysis, there were higher rates of AF recurrence following ablation in those with OSA, (HR 2.61, p=<0.05) and improved rates of arrhythmia control among those treated with CPAP (HR 0.41, p<0.01).[31]
A meta-analysis of the effect of OSA on outcomes following catheter ablation of AF by Ng and colleagues found a 25% increased risk of AF recurrence after ablation in OSA patients compared to those without OSA (RR 1.25, 95% CI 1.08 to 1.45, p = 0.003). In secondary analyses, this increase in risk appeared to be present among those diagnosed with OSA according to overnight PSG (RR 1.40, 95% CI 1.16 to 1.68, p = 0.0004), but not among those diagnosed with OSA by the Berlin Questionnaire (RR 1.07, 95% CI 0.91 to 1.27, p = 0.39).[32] A more recent metaanalysis examined 7 studies with a total population of 1,087 individuals.[33] They found that the relative risk reduction of CPAP on AF recurrence ranged from 30% to 56%, with an overall risk reduction of 42% for CPAP (RR 0.58, 95% CI 0.51-0.67, p<0.001). Interestingly, the same magnitude of risk reduction of CPAP on AF recurrence was observed in those who underwent PVI as well as those who did not undergo ablation. [Table 1] summarizes the studies that have evaluated the effect of OSA on AF recurrence following catheter ablation.
Table 1. Summary of Studies Examining the Effect of OSA on AF Recurrence.
| Study | Number Patients | Mean Age | OSA Diagnosis | Mean Follow-Up | % PAF | Ablation Strategy | Method of AF Detection |
|---|---|---|---|---|---|---|---|
| Patel et al[31] | 3,000 | 55.7 | PSG | 32 mo | 53.4 | PVI + LA linear ablation | Event monitor + 48h Holter |
| Matiello et al | 174 | 52.5 | PSG | 12 mo | 56.3 | PVI + LA linear ablation | Holter |
| Chilukuri et al | 109 | 605 | Berlin | 11 mo | 68 | PVI | ECG + telephone, Event monitor for symptoms |
| Tang et al | 178 | 57.2 | Berlin | 344 days | 100 | PVI | ECG + 24h Holter |
| Chilukuri et al | 210 | 58 | Berlin | 25 mo | 57 | PVI | ECG + telephone, Event monitor for symptoms |
| Jongnarangsin et al | 324 | 57 | PSG | 7 mo | 72 | PVI + CFAE | ECG + 30d autotrigger monitor |
| Naruse et al[33] | 249 | 60 | PSG | 18.8 mo | 54 | PVI + LA linear ablation | ECG |
| Fein et al[32] | 426 | 56.8 | PSG | 12 mo | 57 | PVI + LA linear ablation | ECG and Event monitorr |
Finally, the effect of CPAP on AF progression was recently examined in the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF).[34] In this analysis of 10,132 patients with AF enrolled in a nationwide registry, Holmqvist and colleagues documented an 18% prevalence of OSA. Those with OSA were more symptomatic, had greater rates of interventions for AF and higher rate of hospitalization, but a comparable risk of death, stroke, and myocardial infarction. The rate of AF progression was similar between the OSA and no OSA group (HR 1.06, 95% CI 0.89-1.28, p=0.51). Similarly, no difference in the risk of death, stroke, and myocardial infarction was observed between those on CPAP compared to those not receiving CPAP therapy. However, the rate of AF progression for those receiving CPAP therapy was lower than those with OSA not on CPAP, as well as those without OSA (HR 0.66, 95% CI 0.46-0.94, p=0.02).
CPAP therapy may reduce AF recurrence by preventing or reversing the structural changes of SDB. In a prospective, single center study of patients undergoing cardiac MRI prior to PVI, patients with sleep apnea on shorter duration of CPAP therapy were more likely to have persistent than paroxysmal AF, as well as increased LV mass, larger LA dimensions and lower right ventricular ejection fraction.[35] Bayir and colleagues obtained echocardiograms of 30 patients with moderate to severe OSA and free of cardiovascular disease, at baseline and after 6 months of CPAP therapy. They found significant reductions in inter-atrial (39.2 versus 28.7ms, P<0.0001, left atrial (20.5 versus 15.6ms, p=0.002) and right atrial (20.7 versus 13.1ms, p<0.0001) conduction times. Measures of diastolic dysfunction (E/A ratio 0.9 versus 1.1, p<0.0001) were also improved after CPAP.(36) Effects of CPAP have been shown to decrease LA volume as well as LV systolic and diastolic dysfunction.[37-39] One study of 37 patients with chronic heart failure found that CPAP did not affect blood pressure, heart rate or cardiac output significantly.[40] Thus, CPAP may produce physiologic changes that result in decreased LA size and filling, and which reduce the rate of AF recurrence by decreasing filling pressures and preventing substrate changes. However, this study was designed to demonstrate that CPAP in patients with severe heart failure does not lead to hemodynamic compromise, and thus was limited in its ability to shed light on underlying mechanism of CPAP effect.
Alternatively, CPAP may reduce AF recurrence by mitigating AF triggers. A temporal association between SDB and arrhythmic events has been shown,[41] in which the risk for AF is significantly increased in the immediate post-apneic period, suggesting that SDB may also constitute a trigger for AF. This again suggests that CPAP may modulate the triggers, rather than the substrate for AF. These findings have direct clinical relevance as AF ablation in patients with OSA may require an ablation strategy that emphasizes nonpulmonary vein triggers.
Screening For SDB
The American Academy of Sleep Medicine considers those with AF to be high risk for SDB and recommends evaluation for sleep apnea in these individuals.[42] However, this has not yet become standard practice primarily because sleep apnea remains under-suspected and under-diagnosed by electrophysiology physicians treating patients with AF. In addition, overnight sleep studies are cumbersome and a mechanism for coordinating sleep apnea screening and treatment referral has not been established in electrophysiology clinics. Given the clear evidence for improved arrhythmia control with CPAP therapy following cardioversion and catheter ablation of AF, it remains to be seen whether ablation and antiarrhythmic therapy offer benefit to patients with SDB in the absence of CPAP treatment. In the future, a multidisciplinary approach that involves screening all patients with AF for OSA, and referral to a sleep specialist may become the standard of care.
The gold standard for the diagnosis of sleep apnea is overnight polysomnography, typically conducted in a sleep laboratory, which can be costly and cumbersome for patients. However, these are cumbersome and are less and less covered by insurance companies. Home sleep studies have recently obtained FDA approval for diagnosis of sleep apnea and offer patients and treated physicians the opportunity to assess the presence of SDB in a natural sleeping environment, and often time in timely fashion. All currently available home sleep study devices are able to diagnose OSA, though not all have been validated for use in patients with AF. Some home sleep testing devices also have thoracic impedance bands to allow diagnosis of CSA. Comparisons of portable sleep devices and polysomnopgraphy for the diagnosis of OSA demonstrated good sensitivity and specificity (95.3% and 75%, respectively)[43] and correlation and accuracy (AUC difference=0.04)[44] between major clinical indices such as apnea hypopnea index and respiratory disturbance index.
Conclusions
Atrial fibrillation is the most common cardiac arrhythmia and shares many of the same risk factors as another common clinical condition, sleep apnea. There is a clear association between both obstructive and central sleep apnea and risk for AF. Several studies have shown a link between some of the physiologic changes of SDB and AF, and CPAP has in some cases been shown to reduce the rate of AF incidence and recurrence following catheter ablation in patients with SDB. However, further study is needed to establish a clear mechanistic link between the two conditions.
Future Directions
There are an estimated 5 million new cases of AF per year, which represents a significant proportion of health care costs and morbidity.[1] Gaining insight into the mechanistic role of SDB in the development of AF is key to successful AF prevention and treatment strategies. Additional studies are needed to better understand the mechanism underlying the associations between SDB and AF. In particular, prospective studies examining the feasibility and impact of universal screening for diagnosis and treatment of SDB in patients with AF on arrhythmia outcomes and patient well being are needed.
Clinical Perspective
Atrial fibrillation (AF) and sleep apnea have been associated in multiple studies, with a risk for AF that are 2 to 4 times that of those without sleep disordered breathing. There is emerging evidence from animal and human studies that the physiologic changes of sleep apnea including hypoxia, hypercapnia and intrathoracic pressure fluctuations precipitate electrical and structural changes. Some of these changes occur acutely after an apneic episode, while others occur with repeated exposure over time. There is also evidence that continuous positive airway pressure (CPAP) may reverse some of these changes, thereby reducing the risk for AF recurrence after cardioversion and ablation. However, a detailed understanding of the mechanisms by which sleep apnea precipitates electrical and structural remodeling remains unknown. Further studies are needed to evaluate the feasibility of universal screening for SDB, and the effect of therapy on both the development and progression of AF.
Disclosures
None.
References
- 1.Van Wagoner David R, Piccini Jonathan P, Albert Christine M, Anderson Mark E, Benjamin Emelia J, Brundel Bianca, Califf Robert M, Calkins Hugh, Chen Peng-Sheng, Chiamvimonvat Nipavan, Darbar Dawood, Eckhardt Lee L, Ellinor Patrick T, Exner Derek V, Fogel Richard I, Gillis Anne M, Healey Jeff, Hohnloser Stefan H, Kamel Hooman, Lathrop David A, Lip Gregory Y H, Mehra Reena, Narayan Sanjiv M, Olgin Jeffrey, Packer Douglas, Peters Nicholas S, Roden Dan M, Ross Heather M, Sheldon Robert, Wehrens Xander H T. Progress toward the prevention and treatment of atrial fibrillation: A summary of the Heart Rhythm Society Research Forum on the Treatment and Prevention of Atrial Fibrillation, Washington, DC, December 9-10, 2013. Heart Rhythm. 2015 Jan;12 (1):e5–e29. doi: 10.1016/j.hrthm.2014.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chugh Sumeet S, Havmoeller Rasmus, Narayanan Kumar, Singh David, Rienstra Michiel, Benjamin Emelia J, Gillum Richard F, Kim Young-Hoon, McAnulty John H, Zheng Zhi-Jie, Forouzanfar Mohammad H, Naghavi Mohsen, Mensah George A, Ezzati Majid, Murray Christopher J L. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014 Feb 25;129 (8):837–47. doi: 10.1161/CIRCULATIONAHA.113.005119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peppard Paul E, Young Terry, Barnet Jodi H, Palta Mari, Hagen Erika W, Hla Khin Mae. Increased prevalence of sleep-disordered breathing in adults. Am. J. Epidemiol. 2013 May 1;177 (9):1006–14. doi: 10.1093/aje/kws342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rivlin J, Hoffstein V, Kalbfleisch J, McNicholas W, Zamel N, Bryan A C. Upper airway morphology in patients with idiopathic obstructive sleep apnea. Am. Rev. Respir. Dis. 1984 Mar;129 (3):355–60. doi: 10.1164/arrd.1984.129.3.355. [DOI] [PubMed] [Google Scholar]
- 5.Eckert Danny J, Jordan Amy S, Merchia Pankaj, Malhotra Atul. Central sleep apnea: Pathophysiology and treatment. Chest. 2007 Feb;131 (2):595–607. doi: 10.1378/chest.06.2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benjamin Emelia J, Chen Peng-Sheng, Bild Diane E, Mascette Alice M, Albert Christine M, Alonso Alvaro, Calkins Hugh, Connolly Stuart J, Curtis Anne B, Darbar Dawood, Ellinor Patrick T, Go Alan S, Goldschlager Nora F, Heckbert Susan R, Jalife José, Kerr Charles R, Levy Daniel, Lloyd-Jones Donald M, Massie Barry M, Nattel Stanley, Olgin Jeffrey E, Packer Douglas L, Po Sunny S, Tsang Teresa S M, Van Wagoner David R, Waldo Albert L, Wyse D George. Prevention of atrial fibrillation: report from a national heart, lung, and blood institute workshop. Circulation. 2009 Feb 3;119 (4):606–18. doi: 10.1161/CIRCULATIONAHA.108.825380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehra Reena, Benjamin Emelia J, Shahar Eyal, Gottlieb Daniel J, Nawabit Rawan, Kirchner H Lester, Sahadevan Jayakumar, Redline Susan. Association of nocturnal arrhythmias with sleep-disordered breathing: The Sleep Heart Health Study. Am. J. Respir. Crit. Care Med. 2006 Apr 15;173 (8):910–6. doi: 10.1164/rccm.200509-1442OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mehra Reena, Stone Katie L, Varosy Paul D, Hoffman Andrew R, Marcus Gregory M, Blackwell Terri, Ibrahim Osama A, Salem Rawan, Redline Susan. Nocturnal Arrhythmias across a spectrum of obstructive and central sleep-disordered breathing in older men: outcomes of sleep disorders in older men (MrOS sleep) study. Arch. Intern. Med. 2009 Jun 22;169 (12):1147–55. doi: 10.1001/archinternmed.2009.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tanigawa T, Yamagishi K, Sakurai S, Muraki I, Noda H, Shimamoto T, Iso H. Arterial oxygen desaturation during sleep and atrial fibrillation. Heart. 2006 Dec;92 (12):1854–5. doi: 10.1136/hrt.2005.081257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gami Apoor S, Pressman Gregg, Caples Sean M, Kanagala Ravi, Gard Joseph J, Davison Diane E, Malouf Joseph F, Ammash Naser M, Friedman Paul A, Somers Virend K. Association of atrial fibrillation and obstructive sleep apnea. Circulation. 2004 Jul 27;110 (4):364–7. doi: 10.1161/01.CIR.0000136587.68725.8E. [DOI] [PubMed] [Google Scholar]
- 11.Porthan Kimmo Markus, Melin John Henry, Kupila Jukka Tapani, Venho Kari Kauko Kalervo, Partinen Markku Mikael. Prevalence of sleep apnea syndrome in lone atrial fibrillation: a case-control study. Chest. 2004 Mar;125 (3):879–85. doi: 10.1378/chest.125.3.879. [DOI] [PubMed] [Google Scholar]
- 12.Sin D D, Fitzgerald F, Parker J D, Newton G, Floras J S, Bradley T D. Risk factors for central and obstructive sleep apnea in 450 men and women with congestive heart failure. Am. J. Respir. Crit. Care Med. 1999 Oct;160 (4):1101–6. doi: 10.1164/ajrccm.160.4.9903020. [DOI] [PubMed] [Google Scholar]
- 13.Tung P, Levitzky Y, Wang R, Weng J, Quan S, Gottlieb D, Rueschman M, Punjabi N, Mehra R, Bertisch S, Benjamin E, Redline S. Obstructive and Central Sleep Apnea and Risk of Atrial Fibrillation. Abstract. American Heart Association Scientific Sessions. 2014;17143:130–0. doi: 10.1161/JAHA.116.004500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leung Richard S T, Huber Matthias A, Rogge Thomas, Maimon Nimrod, Chiu Kuo-Liang, Bradley T Douglas. Association between atrial fibrillation and central sleep apnea. Sleep. 2005 Dec;28 (12):1543–6. doi: 10.1093/sleep/28.12.1543. [DOI] [PubMed] [Google Scholar]
- 15.Dimitri Hany, Ng Michelle, Brooks Anthony G, Kuklik Pawel, Stiles Martin K, Lau Dennis H, Antic Nicholas, Thornton Andrew, Saint David A, McEvoy Doug, Antic Ral, Kalman Jonathan M, Sanders Prashanthan. Atrial remodeling in obstructive sleep apnea: implications for atrial fibrillation. Heart Rhythm. 2012 Mar;9 (3):321–7. doi: 10.1016/j.hrthm.2011.10.017. [DOI] [PubMed] [Google Scholar]
- 16.Lu Zhibing, Nie Li, He Bo, Yu Lilei, Salim Mohamed, Huang Bing, Cui Bo, He Wenbo, Wu Wei, Jiang Hong. Increase in vulnerability of atrial fibrillation in an acute intermittent hypoxia model: importance of autonomic imbalance. Auton Neurosci. 2013 Oct;177 (2):148–53. doi: 10.1016/j.autneu.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 17.Naughton M T, Benard D C, Liu P P, Rutherford R, Rankin F, Bradley T D. Effects of nasal CPAP on sympathetic activity in patients with heart failure and central sleep apnea. Am. J. Respir. Crit. Care Med. 1995 Aug;152 (2):473–9. doi: 10.1164/ajrccm.152.2.7633695. [DOI] [PubMed] [Google Scholar]
- 18.Stevenson Irene H, Roberts-Thomson Kurt C, Kistler Peter M, Edwards Glenn A, Spence Steven, Sanders Prashanthan, Kalman Jonathan M. Atrial electrophysiology is altered by acute hypercapnia but not hypoxemia: implications for promotion of atrial fibrillation in pulmonary disease and sleep apnea. Heart Rhythm. 2010 Sep;7 (9):1263–70. doi: 10.1016/j.hrthm.2010.03.020. [DOI] [PubMed] [Google Scholar]
- 19.White R L, Spray D C, Campos de Carvalho A C, Wittenberg B A, Bennett M V. Some electrical and pharmacological properties of gap junctions between adult ventricular myocytes. Am. J. Physiol. 1985 Nov;249 (5 Pt 1):C447–55. doi: 10.1152/ajpcell.1985.249.5.C447. [DOI] [PubMed] [Google Scholar]
- 20.Vorperian V R, Wisialowski T A, Deegan R, Roden D M. Effect of hypercapnic acidemia on anisotropic propagation in the canine ventricle. Circulation. 1994 Jul;90 (1):456–61. doi: 10.1161/01.cir.90.1.456. [DOI] [PubMed] [Google Scholar]
- 21.Chen Peng-Sheng, Chen Lan S, Fishbein Michael C, Lin Shien-Fong, Nattel Stanley. Role of the autonomic nervous system in atrial fibrillation: pathophysiology and therapy. Circ. Res. 2014 Apr 25;114 (9):1500–15. doi: 10.1161/CIRCRESAHA.114.303772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jayachandran J V, Sih H J, Winkle W, Zipes D P, Hutchins G D, Olgin J E. Atrial fibrillation produced by prolonged rapid atrial pacing is associated with heterogeneous changes in atrial sympathetic innervation. Circulation. 2000 Mar 14;101 (10):1185–91. doi: 10.1161/01.cir.101.10.1185. [DOI] [PubMed] [Google Scholar]
- 23.Ogawa Masahiro, Zhou Shengmei, Tan Alex Y, Song Juan, Gholmieh Ghassan, Fishbein Michael C, Luo Huai, Siegel Robert J, Karagueuzian Hrayr S, Chen Lan S, Lin Shien-Fong, Chen Peng-Sheng. Left stellate ganglion and vagal nerve activity and cardiac arrhythmias in ambulatory dogs with pacing-induced congestive heart failure. J. Am. Coll. Cardiol. 2007 Jul 24;50 (4):335–43. doi: 10.1016/j.jacc.2007.03.045. [DOI] [PubMed] [Google Scholar]
- 24.Sharifov Oleg F, Fedorov Vadim V, Beloshapko Galina G, Glukhov Alexey V, Yushmanova Anna V, Rosenshtraukh Leonid V. Roles of adrenergic and cholinergic stimulation in spontaneous atrial fibrillation in dogs. J. Am. Coll. Cardiol. 2004 Feb 4;43 (3):483–90. doi: 10.1016/j.jacc.2003.09.030. [DOI] [PubMed] [Google Scholar]
- 25.Linz Dominik, Schotten Ulrich, Neuberger Hans-Ruprecht, Böhm Michael, Wirth Klaus. Negative tracheal pressure during obstructive respiratory events promotes atrial fibrillation by vagal activation. Heart Rhythm. 2011 Sep;8 (9):1436–43. doi: 10.1016/j.hrthm.2011.03.053. [DOI] [PubMed] [Google Scholar]
- 26.Iwasaki Yu-Ki, Kato Takeshi, Xiong Feng, Shi Yan-Fen, Naud Patrice, Maguy Ange, Mizuno Kyoichi, Tardif Jean-Claude, Comtois Philippe, Nattel Stanley. Atrial fibrillation promotion with long-term repetitive obstructive sleep apnea in a rat model. J. Am. Coll. Cardiol. 2014 Nov 11;64 (19):2013–23. doi: 10.1016/j.jacc.2014.05.077. [DOI] [PubMed] [Google Scholar]
- 27.Ramos Pablo, Rubies Cira, Torres Marta, Batlle Montserrat, Farre Ramon, Brugada Josep, Montserrat Josep M, Almendros Isaac, Mont Lluís. Atrial fibrosis in a chronic murine model of obstructive sleep apnea: mechanisms and prevention by mesenchymal stem cells. Respir. Res. 2014;15 () doi: 10.1186/1465-9921-15-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Can Ilknur, Aytemir Kudret, Demir Ahmet Uğur, Deniz Ali, Ciftci Orcun, Tokgozoglu Lale, Oto Ali, Sahin Altay. P-wave duration and dispersion in patients with obstructive sleep apnea. Int. J. Cardiol. 2009 Apr 17;133 (3):e85–9. doi: 10.1016/j.ijcard.2007.11.037. [DOI] [PubMed] [Google Scholar]
- 29.Baranchuk Adrian, Parfrey Brendan, Lim Leonard, Morriello Florence, Simpson Christopher S, Hopman Wilma M, Redfearn Damian P, Fitzpatrick Michael. Interatrial block in patients with obstructive sleep apnea. Cardiol J. 2011;18 (2):171–5. [PubMed] [Google Scholar]
- 30.Kanagala Ravi, Murali Narayana S, Friedman Paul A, Ammash Naser M, Gersh Bernard J, Ballman Karla V, Shamsuzzaman Abu S M, Somers Virend K. Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation. 2003 May 27;107 (20):2589–94. doi: 10.1161/01.CIR.0000068337.25994.21. [DOI] [PubMed] [Google Scholar]
- 31.Naruse Yoshihisa, Tada Hiroshi, Satoh Makoto, Yanagihara Mariko, Tsuneoka Hidekazu, Hirata Yumi, Ito Yoko, Kuroki Kenji, Machino Takeshi, Yamasaki Hiro, Igarashi Miyako, Sekiguchi Yukio, Sato Akira, Aonuma Kazutaka. Concomitant obstructive sleep apnea increases the recurrence of atrial fibrillation following radiofrequency catheter ablation of atrial fibrillation: clinical impact of continuous positive airway pressure therapy. Heart Rhythm. 2013 Mar;10 (3):331–7. doi: 10.1016/j.hrthm.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 32.Ng Chee Yuan, Liu Tong, Shehata Michael, Stevens Steven, Chugh Sumeet S, Wang Xunzhang. Meta-analysis of obstructive sleep apnea as predictor of atrial fibrillation recurrence after catheter ablation. Am. J. Cardiol. 2011 Jul 1;108 (1):47–51. doi: 10.1016/j.amjcard.2011.02.343. [DOI] [PubMed] [Google Scholar]
- 33.Shukla A. Effect of Obstructive Sleep Apnea Treatment on Atrial Fibrillation Recurrence. JACC: Clinical Electrophysiology. 2015;1:41–51. doi: 10.1016/j.jacep.2015.02.014. [DOI] [PubMed] [Google Scholar]
- 34.Holmqvist Fredrik, Guan Ni, Zhu Zhaoyin, Kowey Peter R, Allen Larry A, Fonarow Gregg C, Hylek Elaine M, Mahaffey Kenneth W, Freeman James V, Chang Paul, Holmes DaJuanicia N, Peterson Eric D, Piccini Jonathan P, Gersh Bernard J. Impact of obstructive sleep apnea and continuous positive airway pressure therapy on outcomes in patients with atrial fibrillation-Results from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF). Am. Heart J. 2015 May;169 (5):647–654.e2. doi: 10.1016/j.ahj.2014.12.024. [DOI] [PubMed] [Google Scholar]
- 35.Neilan Tomas G, Farhad Hoshang, Dodson John A, Shah Ravi V, Abbasi Siddique A, Bakker Jessie P, Michaud Gregory F, van der Geest Rob, Blankstein Ron, Steigner Michael, John Roy M, Jerosch-Herold Michael, Malhotra Atul, Kwong Raymond Y. Effect of sleep apnea and continuous positive airway pressure on cardiac structure and recurrence of atrial fibrillation. J Am Heart Assoc. 2013;2 (6) doi: 10.1161/JAHA.113.000421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bayir Pinar Türker, Demirkan Burcu, Bayir Omer, Duyuler Serkan, Firat Hikmet, Güray Umit, Güray Yeşim, Tatar Emel Çadalli. Impact of continuous positive airway pressure therapy on atrial electromechanical delay and P-wave dispersion in patients with obstructive sleep apnea. Ann Noninvasive Electrocardiol. 2014 May;19 (3):226–33. doi: 10.1111/anec.12106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Khan Akram, Latif Faisal, Hawkins Beau, Tawk Maroun, Sivaram Chittur A, Kinasewitz Gary. Effects of obstructive sleep apnea treatment on left atrial volume and left atrial volume index. Sleep Breath. 2008 May;12 (2):141–7. doi: 10.1007/s11325-007-0142-x. [DOI] [PubMed] [Google Scholar]
- 38.Bradley T Douglas, Logan Alexander G, Kimoff R John, Sériès Frédéric, Morrison Debra, Ferguson Kathleen, Belenkie Israel, Pfeifer Michael, Fleetham John, Hanly Patrick, Smilovitch Mark, Tomlinson George, Floras John S. Continuous positive airway pressure for central sleep apnea and heart failure. N. Engl. J. Med. 2005 Nov 10;353 (19):2025–33. doi: 10.1056/NEJMoa051001. [DOI] [PubMed] [Google Scholar]
- 39.Arias Miguel A, García-Río Francisco, Alonso-Fernández Alberto, Mediano Olga, Martínez Isabel, Villamor José. Obstructive sleep apnea syndrome affects left ventricular diastolic function: effects of nasal continuous positive airway pressure in men. Circulation. 2005 Jul 19;112 (3):375–83. doi: 10.1161/CIRCULATIONAHA.104.501841. [DOI] [PubMed] [Google Scholar]
- 40.Schroll Stephan, Sériès Frédéric, Lewis Keir, Benjamin Amit, Escourrou Pierre, Luigart Ruth, Pfeifer Michael, Arzt Michael. Acute haemodynamic effects of continuous positive airway pressure in awake patients with heart failure. Respirology. 2014 Jan;19 (1):47–52. doi: 10.1111/resp.12193. [DOI] [PubMed] [Google Scholar]
- 41.Monahan Ken, Storfer-Isser Amy, Mehra Reena, Shahar Eyal, Mittleman Murray, Rottman Jeff, Punjabi Naresh, Sanders Mark, Quan Stuart F, Resnick Helaine, Redline Susan. Triggering of nocturnal arrhythmias by sleep-disordered breathing events. J. Am. Coll. Cardiol. 2009 Nov 3;54 (19):1797–804. doi: 10.1016/j.jacc.2009.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Epstein Lawrence J, Kristo David, Strollo Patrick J, Friedman Norman, Malhotra Atul, Patil Susheel P, Ramar Kannan, Rogers Robert, Schwab Richard J, Weaver Edward M, Weinstein Michael D. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009 Jun 15;5 (3):263–76. [PMC free article] [PubMed] [Google Scholar]
- 43.Tonelli de Oliveira Ana Claudia, Martinez Denis, Vasconcelos Luiz Felipe T, Gonçalves Sandro Cadaval, Lenz Maria Carmo, Fuchs Sandra Costa, Gus Miguel, Abreu-Silva Erlon Oliveira, Moreira Leila Beltrami, Fuchs Flávio Danni. Diagnosis of obstructive sleep apnea syndrome and its outcomes with home portable monitoring. Chest. 2009 Feb;135 (2):330–6. doi: 10.1378/chest.08-1859. [DOI] [PubMed] [Google Scholar]
- 44.Rofail Lydia Makarie, Wong Keith K H, Unger Gunnar, Marks Guy B, Grunstein Ronald R. Comparison between a single-channel nasal airflow device and oximetry for the diagnosis of obstructive sleep apnea. Sleep. 2010 Aug;33 (8):1106–14. doi: 10.1093/sleep/33.8.1106. [DOI] [PMC free article] [PubMed] [Google Scholar]


