Abstract
Background
Both the proteasome inhibitor bortezomib and an oncolytic herpes simplex virus-1 (oHSV) expressing GMCSF are currently FDA-approved. While proteasome blockade can increase oHSV replication, immunological consequences and consequent immunotherapy potential are unknown. In this study, we investigated the impact of bortezomib combined with oHSV on tumor cell death and sensitivity to Natural Killier (NK) cell immunotherapy.
Experimental Design
Western blot, flow cytometry, and caspase 3/7 activity assays were used to evaluate the induction of apoptosis/autophagy and/or necroptotic cell death. Cellular and mitochondrial reactive oxygen species (ROS) production was measured utilizing CellROX™ and MitoSOX. Inhibitors/shRNA targeting ROS, JNK and RIP1 kinase (RIPK1) were utilized to investigate the mechanism of cell killing. The synergistic interaction between oHSV and bortezomib was calculated using a Chou-Talalay analysis. NK cells isolated from normal human blood were co-cultured with tumor cells to evaluate cellular interactions. Q-PCR, ELISA, and FACS analysis were used to evaluate NK cell activation. Intracranial tumor xenografts were utilized to evaluate anti-tumor efficacy.
Results
Combination treatment with bortezomib and oHSV induced necroptotic cell death and increased the production of mitochondrial ROS and JNK phosphorylation. Inhibitors/shRNA of RIPK1 and JNK rescued synergistic cell killing. Combination treatment also significantly enhanced NK cell activation and adjuvant NK cell therapy of mice treated with bortezomib and oHSV improved anti-tumor efficacy.
Conclusions
This study provides a significant rationale for triple combination therapy with bortezomib, oHSV, and NK cells to improve efficacy, in glioblastoma patients.
Introduction
Oncolytic Herpes Simplex Virus-1 (oHSV) specifically targets and kills tumors cells and is currently being evaluated for safety and efficacy in multiple clinical trials (1). The recent FDA approval of T-Vec, an oHSV for advanced non-resectable melanoma, underscores the potential of this biological treatment for therapy-resistant cancers (3, 4). A better understanding of the oHSV interactions with approved chemotherapy agents can help design more efficacious therapeutic strategies to combat cancer.
Increased protein synthesis and degradation are required for aggressive tumor growth, and are hallmarks of cancer (2). There are two major cellular pathways of protein degradation in eukaryotic cells: the ubiquitin-proteasome system (UPS) and the autophagy-lysosome system (autophagy). UPS-mediated proteolysis involves initial ubiquitination followed by proteasome-mediated degradation of targeted proteins. Thus, specific chemical inhibitors of the proteasome have emerged as effective anti-tumor drugs (3).
Bortezomib is a peptide-based, reversible inhibitor of the 26-S proteasome and is currently FDA approved for use in multiple myeloma and mantle cell lymphoma. We have previously demonstrated that induction of the unfolded protein response (UPR) in tumor cells (glioma, head and neck, and ovarian) after bortezomib treatment led to an increase of heat shock protein 90 (HSP90), which supported increased viral replication via enhanced nuclear location of the viral polymerase in vitro. This resulted in synergistic cancer cell killing in vitro, and treatment of mice with bortezomib and oHSV resulted in improved anti-tumor efficacy in vivo (4). Since proteasome blockade results in apoptotic cell death and oHSV has evolved several mechanisms to block apoptosis, here we evaluated the consequences of infecting bortezomib-treated cells with an oHSV and its effect on cellular death.
We observed that treatment of tumor cells with bortezomib prior to oHSV infection resulted in a RIPK1-dependent necroptotic cell death, leading to JNK-dependent ROS production. This increased necroptotic cell death was accompanied by enhanced pro-inflammatory cytokine induction and secretion, which could be harnessed to activate an anti-tumor immune response. Furthermore, combination therapy led to increased cell surface expression of NK cell activating markers on tumor cells. Co-culture of primary human NK cells with combination treated tumor cells increased NK cell TRAIL expression, which together enhanced NK cell activation and NK cell-mediated tumor cell killing. In vivo anti-tumor efficacy corroborated that proteasome blockade in conjunction with oncolysis set up the stage for efficient NK cell-mediated tumor cell killing, resulting in improved overall survival of tumor bearing mice. These findings support the translation of this triple treatment strategy in glioblastoma patients.
Materials and methods
Cell Lines and HSV
U251T3, LN229, T98G, X12V2, U87ΔEGFR, and Vero were maintained in Dulbecco's modified eagle's medium (DMEM; Gibco BRL, Grand Island, NY) supplemented with 10% fetal bovine serum (FBS). U251 cells were obtained from Dr. Erwin G. Van Meir (Emory University, Atlanta, GA) and U251T3 cells were created in our laboratory (May 2009) as a tumorigenic clone of U251 cells by serially passaging these cells three times in mice. LN229 and T98G cells were obtained in January 2005 from Erwin G. Van Meir (Emory University, Atlanta, GA). U87ΔEGFR cell line expresses a truncated, constitutively active, mutant form of epidermal growth factor receptor (EGFRvIII), and has been previously described (5). Monkey kidney epithelial derived Vero cells have not been authenticated since receipt. U87ΔEGFR (January 2015), LN229 (July 2013), U251T3 (January 2015), T98G (January 2015), X12V2 (August, 2015) cells were authenticated by the University of Arizona Genetics Core via STR profiling. All cell lines were maintained at 37°C in a humidified atmosphere with 5% carbon dioxide and maintained with 100 units of penicillin/mL, and 0.1 mg of streptomycin/mL (Pen/Strep). Cells are routinely monitored for changes in morphology and growth rate. All cells were negative for mycoplasma. The construction and generation of 34.5ENVE has been previously described and virus was prepared and titered as previously described (6, 7). Virus was propagated in Vero cells as described (8).
Cell Killing Assay
The cytotoxicity of bortezomib and 34.5ENVE was determined in each cell line by measuring the conversion of the tetrazolium salt MTT to formazan (MTT assay) as described (4). Based on the calculated ED50 of each agent, bortezomib and 34.5ENVE were diluted 0.0625, 0.125, 0.25, 0.5, 1, 2, and 4 times in a constant ratio. Cells were plated onto 96-well plates at approximately 50% confluence and pretreated with serially diluted concentrations of bortezomib for 16 hrs, then washed before the addition of serially diluted oHSV. 72 hrs post infection, cells were treated with 10 μl of the MTT labeling reagent and were gently shaken and incubated at 37°C in a 5% CO2 incubator. Four hours later, 100 μl of solubilization solution was added and incubated overnight to solubilize. Plates were read on the next day using a microplate reader at 590 nm. All assays were performed in triplicate. Combination indices were calculated using compusyn program. For rescue assays with necrostatin-1 (nec-1) or JNK inhibitor (SP0600125), cells were pretreated with nec-1 or SP0600125 before bortezomib treatment.
Flow Cytometric Analysis
Apoptosis and necrosis were quantified by double staining with annexin-V and 7AAD then analyzed by flow cytometry using a Becton Dickinson FACS LSRII flow cytometer (Becton-Dickinson, San Jose, CA) as previously described (9). U251T3 cells were pretreated with 12nM bortezomib for 16 hrs. 24 hours later, cells were washed and infected with PBS or 34.5ENVE at an MOI of 0.01. Twenty-four hours post virus infection, cells were processed according to manufacturer's instruction in the PE Annexin V Apoptosis Detection kit (BD Biosciences Pharmingen, San Diego, CA). Apoptosis was quantified on a fluorescence-activated cell sorter (FACS) LSRII (Becton Dickinson, Sunnyvale, CA), and data from 10,000 events were collected for further analysis.
Caspase 3/7 Assay
Caspase-3 and -7 activities were measured at 24 hrs using Caspase 3/7 kit (Caspase-Glo 3/7 Assay, Cat. No. G8091, Promega, Madison, WI). This assay kit provides a proilluminescent Caspase 3/7 substrate, which contains the tetrapeptide sequence DEVD that is cleaved to release aminoluciferin. U251T3 cells were plated at 1 × 104 cells per well in 96 well plates and treated with 12nM of bortezomib. Twenty-four hours later, 0.01 MOI of oHSV was added to the cells. 24 hrs after oHSV infection, 100 ul of Caspase 3/7 substrate was added to the cells for one hour and luminescence was measured by a Fluostar Optima plate reader (BMG Labtech) in triplicate as directed by the manufacturer (7).
Western Blot Analysis and Antibodies
Cell lysates were fractionated by SDS-PAGE and transferred to polyvinylidene difluoride (PVDF) membranes. Blocked membranes were then incubated with antibodies against Anti-Cleaved Caspase 3, Caspase 8, LC3B, Rip1, phospho-JNK, and total JNK (Cell Signaling Technology, Waltham, MA), phosphorylated c-Jun (pS63) and total c-Jun (BD Biosciences Pharmingen, San Diego, CA), GAPDH (Abcam, Cambridge, MA) (each diluted 1:1000), HRP-conjugated secondary anti-mouse antibody (each diluted 1:1000) (GE Healthcare, Piscataway, NJ), HRP-conjugated secondary goat anti-rabbit antibody (each diluted 1:1000) (Dako, Hamburg, Germany), and the immunoreactive bands were visualized using enhanced chemiluminescence (ECL) (GE Healthcare, Piscataway, NJ).
Intracellular and Mitochondria Specific Reactive Oxygen Species (ROS) Measurement
Intracellular and mitochondria-specific ROS were measured using the cell-permeable CellROX™ Deep Red (Invitrogen, Carlsbad, CA) and MitoSOX Red Reagent (Invitrogen, Carlsbad, CA) which are fluorogenic probes designed to measure ROS in living cells. Cells were pretreated with 12nM bortezomib for 16 hrs. The next day, cells were washed and infected with PBS or 34.5ENVE at an MOI of 0.01. 24 hours after viral infection, 5 μl of CellROX™ Deep Red or MitoSOX Red Reagent was added to each sample and incubated at 37°C for 30min. ROS was quantified on a Becton Dickinson FACS Calibur flow cytometer (Becton Dickinson, San Jose, CA) as previously described (10).
In Vitro Viral Replication Assay
One day before viral infection, cancer cells were seeded onto six-well plates at a density that allowed them to become subconfluent and then treated with bortezomib (1 ~ 5 nM) 16 hrs prior to oHSV (MOI = 0.001 or 0.002) infection. Two hours after infection, cells were washed with PBS and media was replaced. 72 hours after virus infection, cells and media were collected and frozen/thawed three times to release the viruses. The number of infectious particles present in the resulting supernatant was determined by performing a standard plaque forming unit assay on Vero cells (6, 7). All assays were performed in triplicate.
Quantification of human IL-1α, IFNγ, and TNFα by ELISA
Human IL-1α, IFNγ, and TNFα (DuoSet ELISA kit, R&D Systems, Minneapolis, MN) were quantified in cell supernatants with/without co-cultured with primary NK cells or treated mice serum according to the manufacturer's recommendations.
Isolation of NK Cells from Human Donors
NK cells were isolated from fresh peripheral blood leukopacks (American Red Cross, Columbus, OH) by 30 minute incubation with RossetteSep cocktail (Stem Cell Technologies, Vancouver, BC) prior to Ficoll Hypaque (Sigma) density gradient centrifugation. NK cells were then cultured in 10% FBS RPMI media and used in downstream applications.
Live/Dead Cell Staining Cytotoxicity Assay with NK Cells
U251T3-mCherry cells, which stably express mCherry, were plated overnight at 3 × 105 cells/well. Where noted, cells were treated with/without ED50 bortezomib for 16 hours prior to infection, washed, and then infected with 34.5ENVE. Cells were infected for 2 hours with 34.5ENVE (MOI = 0.01) or mock infected. Uninfected viruses were washed out and human NK cells added at an effector/target ratio of 4:1. Twenty-four hours after NK cell addition, cells were imaged under fluorescent microscopy and harvested. Harvested cells were stained with Live/Dead Fixable Dead cell stain kit (Invitrogen, Carlsbad, CA) per the manufacturer's instruction and quantified using Becton Dickinson FACS LSR II (Becton Dickinson, San Jose, CA).
Animal Surgery
All mouse experiments were housed and handled in accordance with the Subcommittee on Research Animal Care of the Ohio State University guidelines and have been approved by the Institutional Review Board. Female athymic nu/nu mice (Charles River Laboratoties, Frederick, MD), 4-5-week-old for subcutaneous tumor model and 6-8 week-old for intracranial tumor model, were used for all studies.
For subcutaneous tumor studies, 1 × 106 CAL27 were implanted subcutaneously into the rear flank of nude mice. When tumors reached an average size of 100 mm3, tumor-implanted mice were randomized and intraperitoneally treated with PBS or bortezomib (0.8 mg/kg) twice a week. Seven days post bortezomib treatment, PBS or 34.5ENVE were administered intratumorally (1 × 105 PFU).
For intracranial tumor studies, anesthetized nude mice were fixed in a stereotactic apparatus, and a burr hole was drilled at 2 mm lateral to the bregma, to a depth of 3 mm. 1 × 105 GBM30 cells were implanted in 4 μl Hank's buffered salt solution. Seventy-two hours following cell implantation, mice were randomized and treated with PBS or 0.8 mg/kg of bortezomib twice a week. Ten days after tumor cell implantation, mice anesthetized and stereotactically inoculated with 1 × 105 pfu of 34.5ENVE or PBS at the same location. For experiments involving autologous NK cell adjuvant therapy, NK cells isolated from human donors and 1 × 105 NK cells were stereotactically inoculated at the same location 13 days post tumor implant. Animals were observed daily and were euthanized at the indicated time points or when they showed signs of tumor burden (hunched posture and weight loss).
Histology and Immunohistochemistry
Tumors were fixed in 4% buffered paraformaldehyde, followed by 30% sucrose at 4°C, embedded in OCT compound (Tissue Tek, Sakura Finetec, Torrance, CA) and cut into 10-μm sections. Representative sections were stained with Hematoxylin & Eosin (H&E) and then examined by light microscopy.
Statistical Analysis
To compare two independent treatments for continuous endpoints such as viral titers, apoptosis, ROS, and necroptosis, a student's t-test was used. A one-way ANOVA was utilized for multiple pairwise comparisons. To evaluate the synergistic interaction between bortezomib and oHSV, an interaction contrast or two-way ANOVA model was applied, using the Tukey method to correct for multiple comparisons. Synergistic effect represents that the combined treatment produced an effect (versus control) greater than the additive effect of two single treatments (versus control, respectively). A Log-rank test was used to compare survival curves for survival data and cox regression model was used to evaluate the interaction between bortezomib and oHSV on survival data. P values were adjusted for multiple comparisons by Holms’ procedure. All data analyses were performed using GraphPad Prism statistical software. A P value of 0.05 or less was considered significant.
Results
Impact of bortezomib and oHSV on cell death
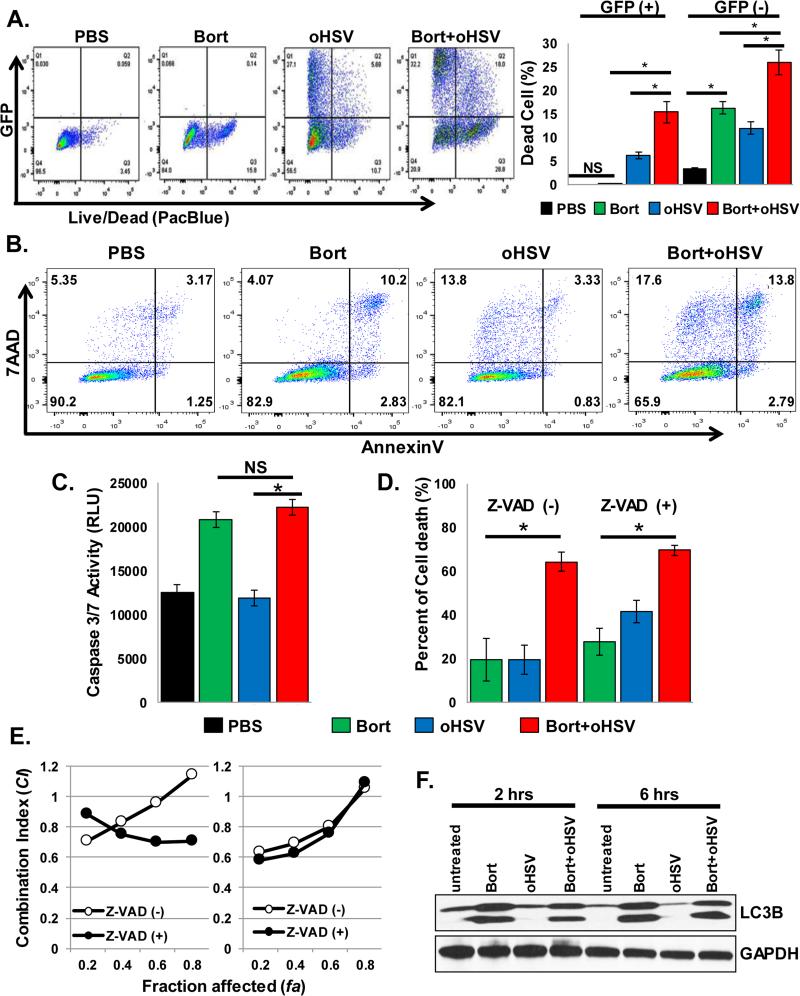
To understand the impact of bortezomib and oHSV treatment on the mechanisim of cell death, we first evaluated their impact on cellular death and apoptosis by measring changes in cell killing upon treatment with bortezomib and/or oHSV. While bortezomib treatment increased oHSV-infected GFP positive cells and also synergistically increased total dead cells (Fig. 1A), a synergistic increase in the percentage of annexin-positive apoptotic cells was not observed in combination treated cells (Fig. 1B). Consistent with these results, no further increase in Caspase 3 activity was observed (Fig. 1C) in combination-treated cells versus bortezomib alone. Pretreatment of cells with Z-VAD-FMK, a pan Caspase inhibitor, did not affect the synergistic cell killing observed between bortezomib and oHSV (Fig. 1D-E). Taken together, these data suggest that treatment of oHSV-infected cells with bortezomib resulted in increased tumor cell killing by a mechanism that was independent of apoptosis.
Figure 1. Combination treatment-induced synergistic cell killing is independent of apoptotic and autophagic cell death.
A) Live/Dead cell staining of infected (GFP +ve), uninfected (GFP −ve), bortezomib, and/or oHSV treated cells. U251T3 glioma cells were pretreated with 12nM bortezomib for 16 hours prior to 34.5ENVE infection at an MOI of 0.01. After twenty-four hours cells were harvested and stained with a Live/Dead Fixable Aqua Dead Cell staining solution. Representative scatter plots and the mean % of dead cells in GFP+ve and GFP-ve population are indicated. B) Annexin V vs. 7AAD scatter dot plots of bortezomib and/or oHSV treated cells. C) Quantification of Caspase 3/7 activity measured using a caspase 3/7 activity assay kit. D-E) The effect of caspase inhibitor, Z-VAD-FMK, treatment was assessed on combination treatment-induced synergistic killing. U251T3 cells were pretreated with/without 20uM of Z-VAD-FMK for 1 hour and then treated with serially diluted bortezomib. Sixteen hours later, drug was washed out and cells were treated with serially diluted 34.5ENVE. Bortezomib and 34.5ENVE were serially diluted at concentrations of 0.0625, 0.125, 0.25, 0.5, 1, 2, and 4 times their ED50 in a constant ratio. Seventy-two hours after34.5ENVE infection, cell viability was measured via MTT assay. D) Data points represent the mean % cell viability relative to uninfected cells. E) Effect of Z-VAD-FMK treatment on synergistic cell killing of tumor cells treated with bortezomib and oHSV. Data shown as fraction affected (fa) versus combination index (CI) plots. CI < 1 indicate synergy, CI = 1 indicate additive, and CI > 1 indicate antagonistic interaction. F) U251T3 cells were treated as in (A), and cells were harvested after 2 and 6 hours. Cell lysates were probed with antibodies against LC3B and GAPDH was used as a loading control. All flow cytometric analyses data are representative of three independent experiments. Errors bars represent ± SD for each group.
Cellular autophagy is usually considered as a cellular stress response to counter cellular apoptosis (11) and dysregulated autophagy results in cell death with oncolytic adenoviruses (12). Since wild-type HSV infection can also initiate autophagy (13, 14), the cellular autophagic response was assessed by comparing the accumulation of LC3IIb in cells following treatment. Western blot analysis revealed no obvious change in LC3IIb accumulation in cells treated with the combination of oHSV and bortezomib, suggesting that changes in cellular autophagy likely did not contribute to the increased cell death observed in combination treated cells (Fig. 1F).
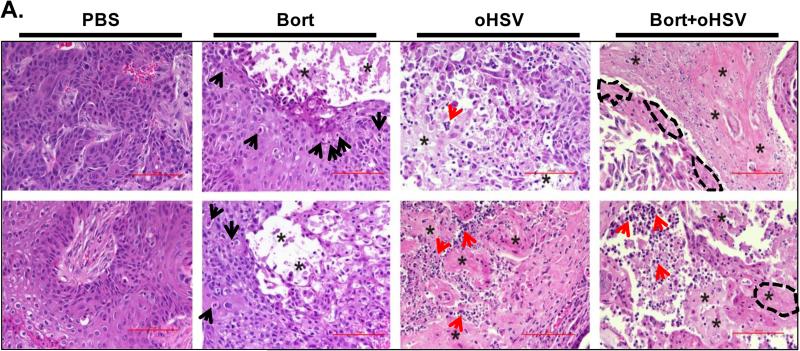
Analysis of Hematoxylin & Eosin (H&E)-stained sections of xenograft tumors from nude mice treated with bortezomib and/or oHSV revealed large geographic areas of necrosis in tumors from mice treated with both bortezomib and oHSV (Fig. 2). Tumors from mice treated with bortezomib showed condensed nuclei, a morphological feature associated with apoptosis (black arrow heads). While tumors from mice treated with oHSV alone showed evidence of necrosis, tumor tissues from mice treated with both bortezomib and/or oHSV displayed extensive areas of tumor necrosis throughout the tumor (asterisks) with extensive immune cell infiltration (red arrow heads). Tumor sections from combination treated mice revealed cells that appeared to have undergone karyohexis (fragmented DNA) or karyolysis (anuclear cells with absent chromatin) surrounding necrotic areas suggestive of necrotic tissue death (encircled with dotted lines). Collectively, these observations implied that combination treatment with bortezomib and oHSV possibly induced necroptic cell death, a mechanism of cell death that is distinct from the effects of either treatment alone on tumor cells.
Figure 2. Bortezomib and oHSV combination treatment induces necroptotic cell death in vivo.
A) Subcutaneously implanted CAL27 head&neck tumors from mice treated with bortezomib (0.8 mg/kg) and/or HBSS or 1 × 105 pfu of oHSV were harvested and sectioned 3 days after virus injection. Data shown are representative H&E stained images of tumor sections from mice treated with PBS, bortezomib (Bort), oHSV, or the combination of Bortezomib and oHSV (Bort + oHSV). Black arrows indicate tumor cells with condensed nuclei, morphological features associated with apoptosis. Red arrows indicate areas with extensive immune cell infiltration. Asterisks (*) indicate areas of necrotic tissue. Cells displaying characteristic features of karyohexis or karyolysis are encircled by a dotted line.
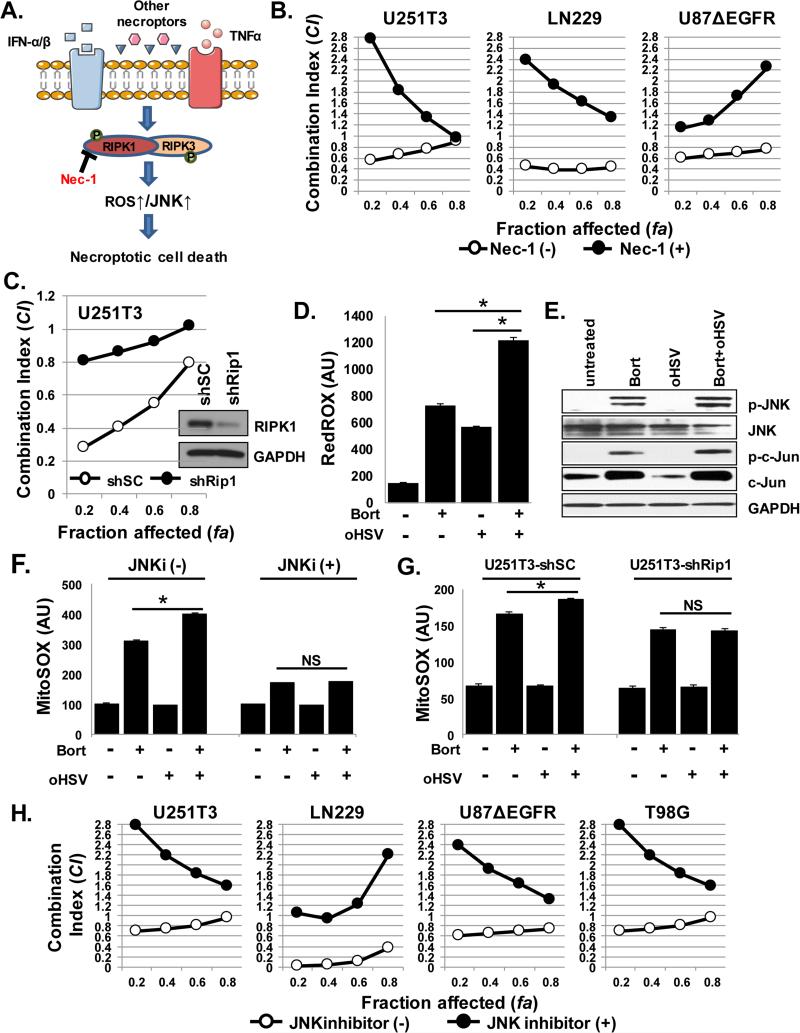
Combination treatment with Bortezomib and oHSV induces Receptor Interacting Protein Kinase 1 (RIPK1) dependent necroptotic cell death
Necroptotic cell death is a mechanism of cell death that involves the formation of a receptor interacting protein kinase 1 (RIPK1) dependent complex that results in increased ROS and JNK activity which leads to a regulated necrosis-like cell death (11) (Fig. 3A). Thus, we tested the involvement of necroptotic cell death in synergistic cell death of oHSV-infected cells after bortezomib treatment. Pretreatment with necrostatin-1 (Nec-1), an inhibitor of RIPK1, or molecular knock down of RIPK1 significantly reduced the synergistic cell killing observed upon infection of bortezomib treated cells (Fig. 3B-C and Supplementary Fig. S1) (15). Interestingly, both Nec-1 treatment and RIPK1 knock down did not reduce the bortezomib-induced increase in virus replication (Supplementary Fig. S2), indicating a role for necroptosis in cell death but not virus replication following combinatorial treatment. Measurement of cellular ROS levels revealed significantly more ROS production in cells treated with bortezomib and oHSV compared to either agent alone (Fig. 3D).
Figure 3. Combination treatment with bortezomib and oHSV induces necroptotic cell death.
A) Schematic illustration of the necroptotic cell death pathway. B-C) The interaction between bortezomib and 34.5ENVE on cell killing was analyzed by the median-effect method of the Chou-Talalay analysis. Data are presented as fraction affected (fa) versus combination index (CI) plots with/without Necrostatin-1 (Nec-1) (B) or with RIPK1 knock down (C). D) Cellular ROS production was measured using a CellROX kit. U251T3 cells were treated with 12nM bortezomib for 16 hours prior to 34.5ENVE infection (MOI = 0.01). ROS was assessed twenty-four hours later. Data points represent the mean and error bars indicate ± SD confidence intervals for each group performed in triplicate. E) U251T3 glioma cells were pretreated with/without 12nM bortezomib for 16 hours and then infected with oHSV (MOI = 0.01). Cells were then harvested 2 and 6 hours later and probed with antibodies against phospho-JNK (p-JNK), total JNK, phospho-c-Jun (pc-Jun), and total c-Jun by western blot analysis. GAPDH was used as a loading control. F) Specific mitochondrial ROS production was measured using MitoSOX kit. U251T3 cells were pretreated with/without 10 uM JNK inhibitor (SP0600125) and then treated with 12nM bortezomib for 16 hours prior to 34.5ENVE infection (MOI = 0.01). Mitochondrial ROS production was assessed twenty-four hours later. Data points represent the mean and error bars indicate ± SD confidence intervals for each group performed in triplicate. G) U251T3 cells were transduced with a RIPK1 shRNA- or non-targeting shRNA-expressing lentivirus. Stably transduced cells were then treated with 12 nM bortezomib for 16 hours prior to 34.5ENVE infection (MOI = 0.01). Mitochondrial specific ROS production was then assessed twenty-four hours later. Data are shown as mean and ± SD confidence interval of three replicates for each group. H) JNK inhibitor treatment rescued the synergistic cell death caused by combinatorial therapy. Cells were treated with SP0600125 (10uM) prior to bortezomib treatment (16 hours) and the interaction between bortezomib and oHSV on cell killing was analyzed by the median-effect method of the Chou-Talalay analysis. Data are presented as fraction affected (fa) versus combination index (CI) plots.
The primary downstream effectors of RIPK1-induced necroptotic cell death are JNK activation and increased mitochondrial ROS (Fig. 3A) (16, 17). Changes in JNK activation (Fig. 3E) and mitochondrial ROS production (Fig. 3F-G) were tested in U251T3 tumor cells treated with ED50 doses of bortezomib (12nM) followed by ED50 doses of oHSV (MOI=0.01) infection. Western blot analysis revealed an increased phosphorylation of JNK and c-Jun upon treatment with both bortezomib and oHSV (Fig. 3E). Using a MitoSOX assay, a significant increase in mitochondrial-released ROS levels was observed in combination treated cells. However, pretreatment with either JNK inhibitor or RIPK1 knockdown reversed this increased mitochondrial ROS production in combination treated cells (Fig. 3F-G). Since JNK signaling contributes to necroptotic cell death, we assessed the role of JNK signaling on the combination treatment interaction. In all cell lines tested, JNK inhibition reduced the synergistic cell killing observed with combination treatment (Fig. 3H and Supplementary Fig. S1). Taken together, these data suggest that combination treatment with bortezomib and oHSV induced necroptotic cell death through the RIPK1/JNK pathway, and that this induction is essential to achieve synergistic cell killing after bortezomib and oHSV treatment.
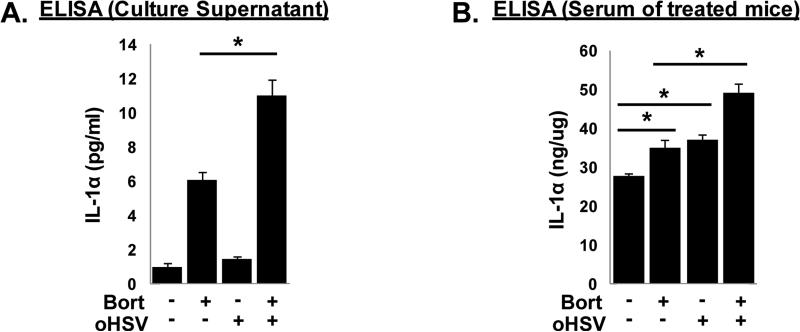
Combination treatment activates pro-inflammatory pathways
Necroptotic cell death results in rapid plasma membrane permeabilization that activates and releases cytokines, such as IL-1α, that can trigger vigorous inflammatory responses (18, 19). To investigate whether combination treatment-induced necroptotic cell death also increases pro-inflammatory cytokine secretion, we measured changes in secreted protein (Fig. 4A) of pro-inflammatory cytokine such as IL-1α from tumor cells treated with bortezomib and oHSV in vitro and in vivo (Fig. 4). Increased IL-1α secretion was observed in vitro and in the serum of GBM30 intracranial tumor-bearing mice treated with bortezomib and oHSV (Fig. 4B).
Figure 4. Combination treatment-induced necroptotic cell death enhances pro-inflammatory cytokine secretion.
A) ELISA quantification of secreted pro-inflammatory cytokine. U251T3 glioma cells were pretreated with 12nM bortezomib for 16 hours prior to 34.5ENVE infection at an MOI of 0.01. Six hours post 34.5ENVE infection, media were harvested and assessed for secreted IL-1α via ELISA. B) Athymic nude mice were stereotactically implanted with patient derived primary GBM30 cells. Five days post tumor implantation mice were treated with PBS/bortezomib (0.8 mg/kg) via intraperitoneal route twice a week for the duration of the study. On day 10, 1×105 pfu of 34.5ENVE were intratumorally injected. Three days post 34.5ENVE treatment; murine serum was collected and assessed for secreted IL-1α via ELISA. Data points represent the mean and error bars indicate ± SD for each group (N=5/each group) performed in triplicate.
Combination treated-tumor cells activate NK cells
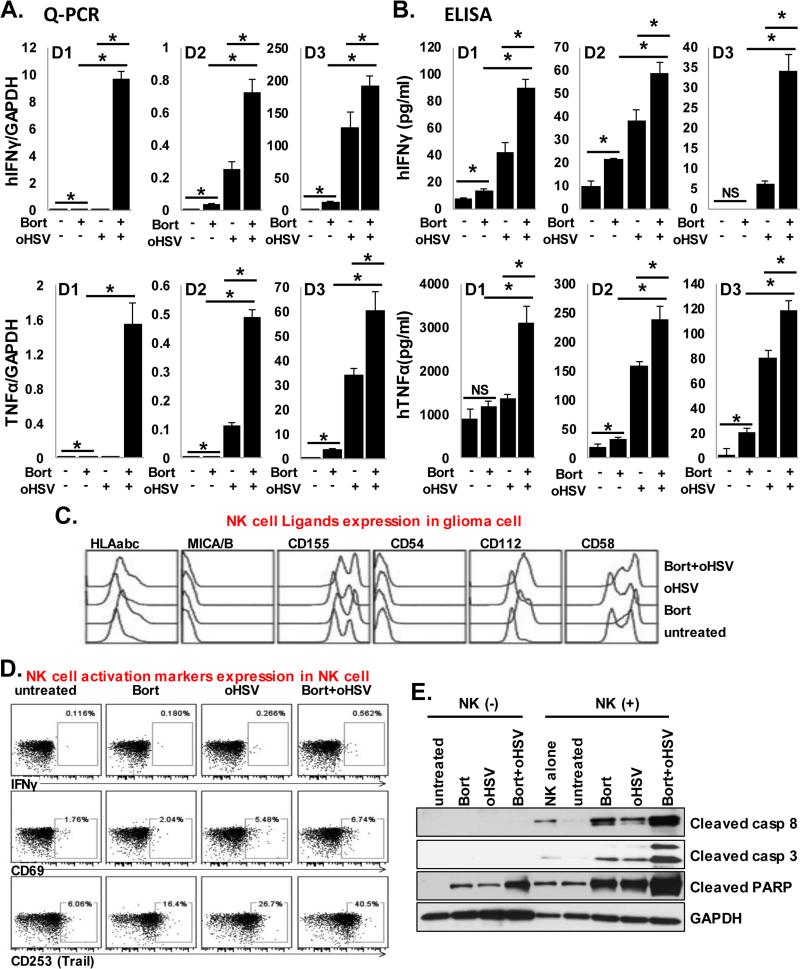
IL-1α (observed after combination treatment above) has been previously shown to result in enhanced NK cell activity against tumor cells (20, 21). Thus, we investigated the impact of combination treatment of tumor cell sensitization to NK cell activity. Primary donor-derived human NK cells from three different donors were co-cultured with combination treated tumor cells for 24hrs. Enzyme linked immunosorbent assays (ELISA) were then used to assess IFNγ and TNFα secretion following co-culture. Consistent with previous reports (22), NK cells co-cultured with bortezomib-treated cells expressed and secreted significantly higher levels of TNFα and IFNγ versus controls (Fig. 5A-B). More importantly, combination treatment with bortezomib and oHSV resulted in a significant enhancement of both TNFα and IFNγ gene expression and cytokine secretion over either single agent alone (Fig. 5A-B).
Figure 5. Bortezomib and oHSV therapy enhances NK cell activation.
A-B) U251T3-mCherry+ glioma cells were pretreated with 12nM bortezomib 16 hours prior to 34.5ENVE infection at an MOI of 0.01. Two hours post 34.5ENVE infection, unbound virus was washed out and cells were overlaid with/without primary human NK cells from three independent donors (D1, D2, and D3). Twenty-four hours later, culture supernatants were analyzed for TNFα and IFN-γ gene expression and secretion by Q-PCR (A) and ELISA (B). C) Flow cytometric analysis of NK cell activating ligands (HLA abc, MICA/B, CD155, CD54, CD112, and CD58) on tumor cells after treatment with bortezomib and/or oHSV as indicated. D) Flow cytometric analysis of NK cell activating receptors TRAIL and CD69 as well as intracellular IFNγ after co-culture with treated tumor cells as indicated. E) Western blot analysis of the cleavage of caspases 8, 3, and PARP in treated tumor cells co-cultured with primary NK cells. GAPDH was used as a loading control.
Tumor cell surface ligands can also initiate cross talk with NK cells to mediate their activity (23). Thus, we evaluated changes in both NK activating ligands on tumor cells and NK cell activation markers on NK cells co-cultured with glioma cells treated with or without bortezomib in the presence or absence of oHSV. Flow cytometric analysis of NK cell-activating ligands on treated tumor cells revealed that bortezomib and combination treatment induced a significant increase in tumor cell surface expression of NK cell activating receptors: CD58, CD112, and CD155 (Fig. 5C). Furthermore, an assessment of NK cell activating receptors was conducted 24 hours post exposure to treated tumor cells. A significant increase in NK cell surface expression of CD69 and TRAIL was observed when cultured with combination treated tumor cells versus each treatment alone (Fig. 5B and 5D).
NK cells are known to induce apoptosis of target cells. Thus, we investigated the effect of NK cells on tumor cell apoptosis. Immunoblot analysis for cleaved Caspase 8, cleaved Caspase 3, and cleaved PARP of glioma cells in the presence or absence of NK cells revealed increased activation of Caspase 8, Caspase 3, and PARP in combination treated tumor cells co-cultured with human donor NK cells, revealing enhanced tumor cell sensitivity to NK cell-mediated apoptotic death (Fig. 5E).
Bortezomib and oHSV treatment enhances NK cell anti-tumor effects in vitro and vivo
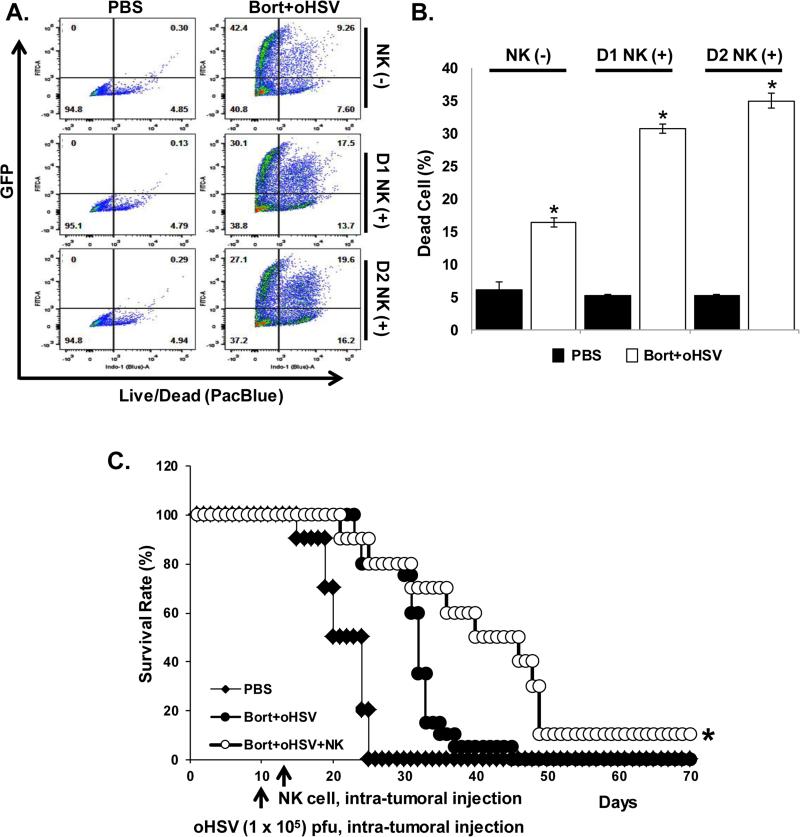
Collectively, these results demonstrate that combination treatment induced necroptotic cell death accompanied by increased pro-inflammatory cytokine expression and NK cell activation. Thus, we tested if we could harness the NK cell sensitivity of combination treated tumors with NK cell adjuvant therapy. U251T3-mCherry cells were pretreated with or without bortezomib for 16 hrs followed by oHSV treatment at an MOI of 0.01 (ED50). Two hours later, cells were washed to remove unbound virus and then overlaid with primary donor-derived human NK cells from two independent donors. Twenty-four hours later, cell killing was assessed via live/dead cell staining and FACS analysis. Glioma cell killing was significantly higher of glioma cells treated with bortezomib and oHSV after co-culture with NK cells from two different donors (a 1.9- and 2.1-fold increase compared to no NK cell co-culture samples) as indicated by FACS analysis (both mCherry and Pacblue positive) (Figure 6A-B). Consistent with previous reports, both bortezomib and oHSV as single agent treatments also sensitized glioma cells to NK cell mediated killing (Supplementary Fig. S3) (24).
Figure 6. Combination therapy significantly enhances NK cell adjuvant therapy.
A-B) U251T3-mCherry+ cells were pretreated with or without bortezomib for 16 hours followed by oHSV treatment at an MOI of 0.01. Two hours post oHSV infection, unbound virus was washed out and cells were then overlaid with primary human NK cells from two independent donors. Twenty-four hours later, cells were harvested and stained with a Live/Dead Fixable Aqua Dead Cell staining solution. A) Representative quadrant plots of Live/Dead cells and viral GFP after gating on mCherry positive cells. B) The mean % positive number of dead cells following co-culture with primary NK cells (after mCherry+ gating). Errors bars represent ± SD for each group. C) Athymic nude mice bearing intracranial GBM30 tumors were treated with bortezomib (0.8 mg/kg) intraperitoneally twice a week for the duration of the study and oHSV on day 10 post tumor implantation. NK cell adjuvant therapy was conducted using fresh primary human NK cells via intratumoral injection of 1 × 105 primary NK cells 3 days post oHSV treatment. Mice were then monitored for survival. Kaplan Meier survival curves of animals in each group (N=10 for PBS, Bort+oHSV, and Bort+oHSV+NK cell) are indicated.
To test the therapeutic efficacy of this in vivo, intracranial tumor bearing mice treated with bortezomib and oHSV were further treated with normal human NK cell adjuvant therapy and evaluated for survival. NK cell therapy significantly improved survival of mice treated with both bortezomib and oHSV (Fig. 6C). Taken together, these data indicate that 1) combination treatment-induced necroptotic cell death resulted in the activation of NK cells and 2) NK cell adjuvant therapy enhanced therapeutic efficacy of mice.
Discussion
The recent approval of T-Vec for melanoma reflects the promising effects of biological therapy to treat some of the most aggressive cancers. We have previously demonstrated that the proteasome inhibitor bortezomib induced expression of HSP90 that supported nuclear localization of the viral polymerase, leading to increased virus replication and anti-tumor efficacy of oHSV. Therapeutic combination treatment strategies such as this result in a decrease in the doses of each treatment necessary and thus hold promise for the treatment of solid tumors while minimizing toxicity (4). In our study, we found that combination treatment with bortezomib and oHSV sensitized tumor cells to exogenous cellular immunotherapy with primary NK cells. Since autologous NK cell immunotherapy for GBM patients (NCT00331526, and NCT01588769), Neukoplast or NK-92 therapy, and proteasome inhibitors are all being evaluated in patients (NCT00900809, NCT02465957 and NCT00990717). This study lays down the rationale for testing oHSV therapies in conjunction with NK cell therapy. Since oHSV is given by intra-tumoral injection, it would be feasible to infuse NK cells along with the virus by a direct injection into tumor site in patients given bortezomib systemically.
While bortezomib induces ER stress and apoptosis, HSV-1 can hijack cellular pathways to override this response (25). Here, we found that oHSV infection of bortezomib treated cells synergistically increased cell death independent of both apoptosis and/or autophagic cell death. Many standard cancer chemotherapeutic drugs including bortezomib, doxorubicin, and cisplatin exert their anticancer activity by inducing cellular apoptosis. Resistance to apoptosis often occurs in patients and presents a challenge to the development of cancer therapeutics that rely on cellular suicide death mechanisms. Interestingly, since HSV-1 infected cells are resistant to apoptotic cell death, infected cells are primed to enter necroptotic cell death (26). In this study, we found that combination treatment of bortezomib and oHSV induces caspase-independent necroptotic cell death in glioma and highlights the therapeutic potential of this treatment for tumors that do not respond to traditional chemotherapies due to defects in pro-apoptotic signaling. It is important to note that bortezomib is thought to have very low BBB penetration (27). Consistent with this finding, we did not observe any improvement in the survival of mice bearing intracranial tumors treated with this single agent (Supplementary Figure S4). However, we have previously demonstrated increased vascular leakiness in tumors after oHSV therapy (28). It is thus interesting to speculate if oHSV therapy can also be exploited to improve penetration of drugs, such as bortezomib, into tumors where with limited penetration.
Apoptotic cell death is accompanied by membrane blebbing, resulting in apoptotic bodies that are engulfed by phagocytes and thus culminating in an immunologically silent death (29, 30). Necrotic cells, however, undergo a rapid loss of membrane integrity that allows the release of cytokines, resulting in a robust inflammatory response (31-34), which can ultimately result in an anti-tumoral immune response. Our results indicate necroptotic cell death is a cell death mechanism downstream of virus replication and its blockade does not affect oHSV replication in vitro (Supplementary Figure S2). Interestingly, necroptotic cell death-associated inflammation can also serve as a mechanism for pathogen clearance (18). Here, we observed a significant induction of the secretion of several cytokines, such as IL-1α in combination treated tumors in vitro and in vivo. These findings suggest that this enhanced inflammatory response may herald a significant and long term anti-tumor immune response. Bortezomib treatment has also been proven to sensitize human and mouse tumor cells to TRAIL and/or NK cell-mediated killing through the expression of apoptosis-inducing death receptors, such as DR5 (22, 24). NK cells are innate lymphocytes capable of mediating cytotoxicity against tumor and virally infected cells and do not require the presence of a specific tumor antigen for recognition (35). Alternatively, others have also reported that bortezomib can have NK cell immunosuppressive effects by inhibiting cellular proliferation (36, 37). In this study, we report increased expression of NK cell activating receptors CD155, CD112, and CD58 after exposure to proteasome inhibitor. More significantly, the increased expression of these NK activating cell surface markers was retained after oHSV infection of bortezomib treated cells. Co-culture of NK cells with combination treated tumor cells also resulted in increased NK cell TNFα and IFNγ secretion, as well as NK cell-mediated apoptosis.
The impact of NK cells on combination therapy was also assessed in vivo. NK cell adjuvant therapy resulted in significant enhancement of murine survival following bortezomib and oncolytic virus treatment in tumor bearing mice. We and others have previously shown that modulation of host immune responses can limit intra-tumoral infiltration of innate immune response mediators, such macrophages and NK cells, and thereby result in increased viral propagation and enhanced anti-tumor efficacy (10, 38, 39). We have also recently shown that elevated TNFα production in the tumor microenvironment leads to oHSV infected cell apoptosis and can limit viral replication and efficacy (40). We hypothesize that a major limitation to exploiting endogenous NK cells to augment immunotherapy of infected tumors is likely due to low effector to target cell ratios. Here, we show NK cell adjuvant therapy can be exploited to enhance the NK:infected tumor cell ratio and result in increased tumor cell sensitivity to NK cell-mediated killing that can augment combination therapy. In bortezomib and oHSV treated mice, NK cell adjuvant therapy resulted in a significant enhancement of the survival of glioma bearing mice. It would be important to note that as virus treatments in combination with agents that enhance oncolysis and/or immunotherapeutic effects are translated into patients, we might uncover previously unidentified toxicities that might be due to virus dose amplifications or increases in an inflammatory response. While both viral dose amplifications as well as severe inflammatory responses can be checked by anti-herpetic treatments and steroids or other anti-inflammatories there would be a need to monitor these patients carefully for potential signs of toxicity. Recent studies have highlighted the contextually-dependent effects of the host innate anti-viral response: which can be detrimental when mediating virus clearance, but beneficial in activating anti-tumor responses (41). To our knowledge, this is the first study to exploit NK cell adjuvant therapy in combination with virotherapy and proteasome blockade. Since proteasome inhibitors, oHSV, and autologous NK cell immunotherapy are currently being investigated individually in GBM patients, our study may help guide the future clinical development of novel combination therapies for GBM.
Supplementary Material
Translational Relevance.
Oncolytic virus (OV) therapy has emerged as a promising biological therapy with many potential applications. FDA approval of first oncolytic HSV (oHSV) (T-Vec), for use in advanced melanoma, highlights its relevance in cancer. Using a combination treatment modality with bortezomib, an FDA approved peptide-based reversible proteasome inhibitor, we found that oHSV induced inflammatory necroptotic cell death accompanied by the secretion of inflammatory cytokines into the tumor microenvironment. This resulted in natural killer (NK) cell activation and increased sensitization of infected tumor cells to NK cell-mediated killing. Furthermore, using primary human NK cells and in vivo models, bortezomib and oHSV combination treatment sensitized tumor cells to primary NK cell immunotherapy, resulting in increased tumor killing and murine survival. Since proteasome inhibitors, oHSVs, and autologous NK cell immunotherapy are currently being investigated individually in GBM patients, our study provides the rationale for combining these therapies in future clinical trials.
Acknowledgments
Grant Support
This work was supported by: R01 NS064607, P30 CA016058, R01 CA150153, P30 NS045758, (to Balveen Kaur); IRG-67-003-50 (to Ji Young Yoo); CA 186542-01A1 (to Alena Cristina Jaime-Ramirez), T32 CA009338 (to Chelsea Bolyard), P01CA163205 (to Balveen Kaur and Michael Caligiuri) and Pelotonia Fellowship Program (to Alena Cristina Jaime-Ramirez, Hongsheng Dai, and Tejaswini Nallanagulagari).
Footnotes
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- 1.Kanai R, Wakimoto H, Cheema T, Rabkin SD. Oncolytic herpes simplex virus vectors and chemotherapy: are combinatorial strategies more effective for cancer? Future Oncol. 2010;6(4):619–34. doi: 10.2217/fon.10.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hui B, Shi YH, Ding ZB, Zhou J, Gu CY, Peng YF, et al. Proteasome inhibitor interacts synergistically with autophagy inhibitor to suppress proliferation and induce apoptosis in hepatocellular carcinoma. Cancer. 2012;118(22):5560–71. doi: 10.1002/cncr.27586. [DOI] [PubMed] [Google Scholar]
- 3.Cvek B, Dvorak Z. The Ubiquitin-Proteasome System (UPS) and the Mechanism of Action of Bortezomib. Current Pharmaceutical Design. 2011;17(15):1483–99. doi: 10.2174/138161211796197124. [DOI] [PubMed] [Google Scholar]
- 4.Yoo JY, Hurwitz BS, Bolyard C, Yu JG, Zhang JY, Selvendiran K, et al. Bortezomib-Induced Unfolded Protein Response Increases Oncolytic HSV-1 Replication Resulting in Synergistic Antitumor Effects. Clinical Cancer Research. 2014;20(14):3787–98. doi: 10.1158/1078-0432.CCR-14-0553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Narita Y, Nagane M, Mishima K, Huang HJ, Furnari FB, Cavenee WK. Mutant epidermal growth factor receptor signaling down-regulates p27 through activation of the phosphatidylinositol 3-kinase/Akt pathway in glioblastomas. Cancer Res. 2002;62(22):6764–9. [PubMed] [Google Scholar]
- 6.Yoo JY, Haseley A, Bratasz A, Chiocca EA, Zhang JY, Powell K, et al. Antitumor Efficacy of 34.5ENVE: A Transcriptionally Retargeted and “Vstat120”-expressing Oncolytic Virus. Molecular Therapy. 2012;20(2):287–97. doi: 10.1038/mt.2011.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bolyard C, Yoo JY, Wang PY, Saini U, Rath KS, Cripe TP, et al. Doxorubicin synergizes with 34.5ENVE to enhance antitumor efficacy against metastatic ovarian cancer. Clin Cancer Res. 2014;20(24):6479–94. doi: 10.1158/1078-0432.CCR-14-0463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoo JY, Pradarelli J, Haseley A, Wojton J, Kaka A, Bratasz A, et al. Copper chelation enhances antitumor efficacy and systemic delivery of oncolytic HSV. Clin Cancer Res. 2012;18(18):4931–41. doi: 10.1158/1078-0432.CCR-12-0697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Racoma IO, Meisen WH, Wang QE, Kaur B, Wani AA. Thymoquinone inhibits autophagy and induces cathepsin-mediated, caspase-independent cell death in glioblastoma cells. PLoS One. 2013;8(9):e72882. doi: 10.1371/journal.pone.0072882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alvarez-Breckenridge CA, Yu JH, Price R, Wojton J, Pradarelli J, Mao HY, et al. NK cells impede glioblastoma virotherapy through NKp30 and NKp46 natural cytotoxicity receptors. Nature Medicine. 2012;18(12):1827. doi: 10.1038/nm.3013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wojton J, Meisen WH, Kaur B. How to train glioma cells to die: molecular challenges in cell death. J Neurooncol. 2016;126(3):377–84. doi: 10.1007/s11060-015-1980-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klein SR, Piya S, Lu Z, Xia Y, Alonso MM, White EJ, et al. C-Jun N-terminal kinases are required for oncolytic adenovirus-mediated autophagy. Oncogene. 2015;34(41):5295–301. doi: 10.1038/onc.2014.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lussignol M, Queval C, Bernet-Camard MF, Cotte-Laffitte J, Beau I, Codogno P, et al. The Herpes Simplex Virus 1 Us11 Protein Inhibits Autophagy through Its Interaction with the Protein Kinase PKR. J Virol. 2013;87(2):859–71. doi: 10.1128/JVI.01158-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Orvedahl A, Alexander D, Talloczy Z, Sun QH, Wei YJ, Zhang W, et al. HSV-1ICP34.5 confers neurovirulence by targeting the Beclin 1 autophagy protein. Cell Host & Microbe. 2007;1(1):23–35. doi: 10.1016/j.chom.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 15.Christofferson DE, Yuan JY. Necroptosis as an alternative form of programmed cell death. Current Opinion in Cell Biology. 2010;22(2):263–8. doi: 10.1016/j.ceb.2009.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Papa S, Bubici C, Zazzeroni F, Pham CG, Kuntzen C, Knabb JR, et al. The NF-kappa B-mediated control of the JNK cascade in the antagonism of programmed cell death in health and disease. Cell Death Differ. 2006;13(5):712–29. doi: 10.1038/sj.cdd.4401865. [DOI] [PubMed] [Google Scholar]
- 17.Vande Walle L, Wirawan E, Lamkanfi M, Festjens N, Verspurten J, Saelens X, et al. The mitochondrial serine protease HtrA2/Omi cleaves RIP1 during apoptosis of Ba/F3 cells induced by growth factor withdrawal. Cell Research. 2010;20(4):421–33. doi: 10.1038/cr.2010.18. [DOI] [PubMed] [Google Scholar]
- 18.Kaczmarek A, Vandenabeele P, Krysko DV. Necroptosis: the release of damage-associated molecular patterns and its physiological relevance. Immunity. 2013;38(2):209–23. doi: 10.1016/j.immuni.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 19.Meng L, Jin W, Wang X. RIP3-mediated necrotic cell death accelerates systematic inflammation and mortality. Proc Natl Acad Sci U S A. 2015;112(35):11007–12. doi: 10.1073/pnas.1514730112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marhaba R, Nazarenko I, Knofler D, Reich E, Voronov E, Vitacolonna M, et al. Opposing effects of fibrosarcoma cell-derived IL-1 alpha and IL-1 beta on immune response induction. Int J Cancer. 2008;123(1):134–45. doi: 10.1002/ijc.23503. [DOI] [PubMed] [Google Scholar]
- 21.Mishra R, Polic B, Welsh RM, Szomolanyi-Tsuda E. Inflammatory cytokine-mediated evasion of virus-induced tumors from NK cell control. J Immunol. 2013;191(2):961–70. doi: 10.4049/jimmunol.1203328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lundqvist A, Abrams SI, Schrump DS, Alvarez G, Suffredini D, Berg M, et al. Bortezomib and depsipeptide sensitize tumors to tumor necrosis factor-related apoptosis-inducing ligand: a novel method to potentiate natural killer cell tumor cytotoxicity. Cancer Res. 2006;66(14):7317–25. doi: 10.1158/0008-5472.CAN-06-0680. [DOI] [PubMed] [Google Scholar]
- 23.Lundqvist A, Yokoyama H, Smith A, Berg M, Childs R. Bortezomib treatment and regulatory T-cell depletion enhance the antitumor effects of adoptively infused NK cells. Blood. 2009;113(24):6120–7. doi: 10.1182/blood-2008-11-190421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hallett WH, Ames E, Motarjemi M, Barao I, Shanker A, Tamang DL, et al. Sensitization of tumor cells to NK cell-mediated killing by proteasome inhibition. J Immunol. 2008;180(1):163–70. doi: 10.4049/jimmunol.180.1.163. [DOI] [PubMed] [Google Scholar]
- 25.Mulvey M, Arias C, Mohr I. Maintenance of endoplasmic reticulum (ER) homeostasis in herpes simplex virus type 1-infected cells through the association of a viral glycoprotein with PERK, a cellular ER stress sensor. J Virol. 2007;81(7):3377–90. doi: 10.1128/JVI.02191-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jerome KR, Fox R, Chen Z, Sears AE, Lee HY, Corey L. Herpes simplex virus inhibits apoptosis through the action of two genes, Us5 and Us3. J Virol. 1999;73(11):8950–7. doi: 10.1128/jvi.73.11.8950-8957.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Di K, Lloyd GK, Abraham V, MacLaren A, Burrows FJ, Desjardins A, et al. Marizomib activity as a single agent in malignant gliomas: ability to cross the blood-brain barrier. Neuro Oncol. 2016;18(6):840–8. doi: 10.1093/neuonc/nov299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kurozumi K, Hardcastle J, Thakur R, Yang M, Christoforidis G, Fulci G, et al. Effect of tumor microenvironment modulation on the efficacy of oncolytic virus therapy. J Natl Cancer Inst. 2007;99(23):1768–81. doi: 10.1093/jnci/djm229. [DOI] [PubMed] [Google Scholar]
- 29.Nagata S, Hanayama R, Kawane K. Autoimmunity and the clearance of dead cells. Cell. 2010;140(5):619–30. doi: 10.1016/j.cell.2010.02.014. [DOI] [PubMed] [Google Scholar]
- 30.Lauber K, Blumenthal SG, Waibel M, Wesselborg S. Clearance of apoptotic cells: getting rid of the corpses. Mol Cell. 2004;14(3):277–87. doi: 10.1016/s1097-2765(04)00237-0. [DOI] [PubMed] [Google Scholar]
- 31.Fadok VA, Bratton DL, Rose DM, Pearson A, Ezekewitz RA, Henson PM. A receptor for phosphatidylserine-specific clearance of apoptotic cells. Nature. 2000;405(6782):85–90. doi: 10.1038/35011084. [DOI] [PubMed] [Google Scholar]
- 32.Golstein P, Kroemer G. Cell death by necrosis: towards a molecular definition. Trends Biochem Sci. 2007;32(1):37–43. doi: 10.1016/j.tibs.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 33.Zong WX, Thompson CB. Necrotic death as a cell fate. Genes Dev. 2006;20(1):1–15. doi: 10.1101/gad.1376506. [DOI] [PubMed] [Google Scholar]
- 34.Pasparakis M, Vandenabeele P. Necroptosis and its role in inflammation. Nature. 2015;517(7534):311–20. doi: 10.1038/nature14191. [DOI] [PubMed] [Google Scholar]
- 35.Herberman RB, Ortaldo JR. Natural killer cells: their roles in defenses against disease. Science. 1981;214(4516):24–30. doi: 10.1126/science.7025208. [DOI] [PubMed] [Google Scholar]
- 36.Chang CL, Hsu YT, Wu CC, Yang YC, Wang C, Wu TC, et al. Immune mechanism of the antitumor effects generated by bortezomib. J Immunol. 2012;189(6):3209–20. doi: 10.4049/jimmunol.1103826. [DOI] [PubMed] [Google Scholar]
- 37.Berges C, Haberstock H, Fuchs D, Miltz M, Sadeghi M, Opelz G, et al. Proteasome inhibition suppresses essential immune functions of human CD4+ T cells. Immunology. 2008;124(2):234–46. doi: 10.1111/j.1365-2567.2007.02761.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haseley A, Boone S, Wojton J, Yu L, Yoo JY, Yu J, et al. Extracellular matrix protein CCN1 limits oncolytic efficacy in glioma. Cancer Res. 2012;72(6):1353–62. doi: 10.1158/0008-5472.CAN-11-2526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thorne AH, Meisen WH, Russell L, Yoo JY, Bolyard CM, Lathia JD, et al. Role of cysteine-rich 61 protein (CCN1) in macrophage-mediated oncolytic herpes simplex virus clearance. Mol Ther. 2014;22(9):1678–87. doi: 10.1038/mt.2014.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meisen WH, Wohleb ES, Jaime-Ramirez AC, Bolyard C, Yoo JY, Russell L, et al. The Impact of Macrophage- and Microglia-Secreted TNFalpha on Oncolytic HSV-1 Therapy in the Glioblastoma Tumor Microenvironment. Clin Cancer Res. 2015;21(14):3274–85. doi: 10.1158/1078-0432.CCR-14-3118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Meisen WH, Kaur B. How can we trick the immune system into overcoming the detrimental effects of oncolytic viral therapy to treat glioblastoma? Expert Rev Neurother. 2013;13(4):341–3. doi: 10.1586/ern.13.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.