Abstract
Objective To compare clinical outcomes between short term (up to 6 months) and long term (12 months) dual antiplatelet therapy (DAPT) after placement of a drug eluting stent in patients with and without diabetes.
Design Individual participant data meta-analysis. Cox proportional regression models stratified by trial were used to assess the impact of diabetes on outcomes.
Data source Medline, Embase, and Cochrane databases and proceedings of international meetings searched for randomised controlled trials comparing durations of DAPT after placement of a drug eluting stent. Individual patient data pooled from six DAPT trials.
Primary outcome Primary study outcome was one year risk of major adverse cardiac events (MACE), defined as cardiac death, myocardial infarction, or definite/probable stent thrombosis. All analyses were conducted by intention to treat.
Results Six trials including 11 473 randomised patients were pooled. Of these patients, 3681 (32.1%) had diabetes and 7708 (67.2%) did not (mean age 63.7 (SD 9.9) and 62.8 (SD 10.1), respectively), and in 84 (0.7%) the information was missing. Diabetes was an independent predictor of MACE (hazard ratio 2.30, 95% confidence interval 1.01 to 5.27; P=0.048 At one year follow-up, long term DAPT was not associated with a decreased risk of MACE compared with short term DAPT in patients with (1.05, 0.62 to 1.76; P=0.86) or without (0.97, 0.67 to 1.39; P=0.85) diabetes (P=0.33 for interaction). The risk of myocardial infarction did not differ between the two DAPT regimens (0.95, 0.58 to 1.54; P=0.82; for those with diabetes and 1.15, 0.68 to 1.94; P=0.60; for those without diabetes (P=0.84 for interaction). There was a lower risk of definite/probable stent thrombosis with long term DAPT among patients with (0.26, 0.09 to 0.80; P=0.02) than without (1.42, 0.68 to 2.98; P=0.35) diabetes, with positive interaction testing (P=0.04 for interaction), although the landmark analysis showed a trend towards benefit in both groups. Long term DAPT was associated with higher rates of major or minor bleeding, irrespective of diabetes (P=0.37 for interaction).
Conclusions Although the presence of diabetes emerged as an independent predictor of MACE after implantation of a drug eluting stent, compared with short term DAPT, long term DAPT did not reduce the risk of MACE but increased the risk of bleeding among patients with stents with and without diabetes.
Introduction
Dual antiplatelet therapy (DAPT) represents the evidence based standard of care among patients undergoing percutaneous coronary intervention. Treatment aims to reduce the risk of stent thrombosis after implantation of a coronary stent and prevent coronary atherothrombotic events at sites outside the stented segment. The optimal duration of DAPT after stent implantation in general, and particularly after implantation of a drug eluting stent, however, remains a matter of controversy.1 2 3 4 5 6 7 Currently, a minimum duration of six months has been advocated in professional guideline documents and adopted worldwide for management of patients receiving drug eluting stents, irrespective of type.8 9 10
Diabetes mellitus is a widely recognised risk factor for atherosclerosis, disease progression, and restenosis after percutaneous coronary intervention.11 12 13 14 Although new generation drug eluting stents have also been shown to provide improved safety and efficacy compared with balloon angioplasty, bare metal stents, and early generation drug eluting stents among patients with diabetes, such patients, particularly when they need treatment with insulin, have a high ischaemic risk.15 16 17 18 Increased platelet and thrombin reactivity and decreased response to therapeutic agents including aspirin and clopidogrel have been described in patients with diabetes.19 20
Whether diabetes should be taken into consideration in the selection of the most appropriate duration of DAPT remains unclear. Recently, it was proposed that the presence of diabetes can identify patients who benefit from prolonged DAPT because of the increased related ischaemic risk.4 6 21 Yet the evidence appraising the role of diabetes in the choice of the optimal duration is limited.22
We assessed the impact of diabetes status on outcomes after implantation of drug eluting stents in patients treated with short term (≤6 months) or long term (12 months) DAPT. We conducted a patient level pooled analysis of randomised trials comparing clinical outcomes between short term and long term treatment after implantation of a drug eluting stent and stratified outcomes according to diabetes status.
Methods
Study design
The present study was an individual participant data (IPD) meta-analysis of randomised controlled trials designed to investigate the efficacy and safety of long versus short term DAPT in patients with or without medically treated diabetes. The present meta-analysis was performed according to the PRISMA-IPD statements.23
In November 2015, we searched Medline, Embase, Cochrane controlled trials register databases, and main international websites and meetings for randomised controlled trials directly comparing short term (3-6 months) and long term (≥12 months) DAPT among patients undergoing percutaneous coronary intervention with drug eluting stents. We excluded trials that looked at DAPT for 12 months compared with more than 12 months. The following keywords were used: “randomized clinical trial”, “drug-eluting stent”, “dual antiplatelet therapy”, “clopidogrel”, “aspirin”, “thienopyridines” (see appendix for supplementary methods). No language or publication date restrictions were imposed. The most recent data for a given study were abstracted. The internal validity of randomised controlled trials was assessed by evaluating concealment of allocation, blind adjudication of events, and inclusion of all randomised patients in the analysis. The quality of trials included in the meta-analysis was appraised with Cochrane methods (selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias).
Three investigators (GG, MV, and TP) independently did the systematic search and critically identified studies to ensure satisfaction of the collected studies.
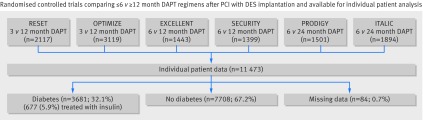
Among qualifying trials, those for which we obtained patient level data from the principal investigators were finally included in the present meta-analysis and combined in a single pooled database. In addition to the four previously included randomised controlled trials,24 25 26 27 28 we included the SECURITY29 and the ITALIC30 trials (fig 1; tables A-D in appendix). The intention to treat population was used for these analyses, including all patients according to randomised treatment arm regardless of actual treatment. Data beyond one year were censored to preserve analysis homogeneity. Furthermore, we excluded a quarter of patients randomised to bare metal stents from the PRODIGY population to restrict the analysis to patients receiving a drug eluting stent.25 31 Characteristics of the included studies are described in tables A-D in the appendix.
Fig 1 Studies and patients included in analysis of individual patient data. PCI=percutaneous coronary intervention; DES=drug eluting stent
Definitions end endpoints
Our primary endpoint was the one year rate of major adverse cardiac events (MACE), including the composite of cardiac death, myocardial infarction, or definite/probable stent thrombosis, as previously described.24 Secondary endpoints included the one year rate of major and minor bleeding, all cause death, cardiac death, stroke, myocardial infarction, stent thrombosis (definite, probable, and definite/probable), and target vessel revascularisation, and combinations of these endpoints.
We incorporated the endpoint definitions as applied in each trial. Stent thrombosis was defined according to criteria from the academic research consortium.32 Four of the included trials defined bleeding according to TIMI (thrombolysis in myocardial infarction) criteria.33 One trials used the modified REPLACE-2/GUSTO criteria,26 while another trial used the BARC (bleeding academic research consortium) criteria.34 In each trial a blinded clinical event committee adjudicated events (table B in appendix). Table C in the appendix reports endpoint definitions in each included trial.
Patient involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in the design and implementation of the study. There are no plans to involve patients in dissemination.
Statistical analysis
We report categorical variables as count and percentages and compared them with a conditional regression analysis stratified by trial. Continuous variables are reported as means and standard deviation and were compared with a two way analysis of variance stratified by trial. We carried out an individual patient data meta-analysis with a one stage approach.
Results are reported as hazard ratios with 95% confidence intervals. We used a mixed effects Cox regression model that took into account the variation between trials in baseline hazard and hazard ratios to derive an overall hazard ratio across trials (see supplementary methods in appendix).35 36 We used Cox regression for formal interaction testing to evaluate consistency of treatment effect between the groups with and without diabetes. Cumulative survival curves were constructed with the Kaplan-Meier model.
From the pooled patient level database, we also investigated all endpoints in the subgroup of patients with diabetes who were receiving treatment with insulin. We also examined the risk of MACE with long term versus short term DAPT in prespecified subgroups: by clinical presentation (acute coronary syndrome or stable), age (<65 or ≥65), sex, and presence of multivessel disease.
As a sensitivity analysis, we compared long term versus short term DAPT for MACE, myocardial infarction, definite/probable stent thrombosis, and major or minor bleeding after censoring clinical events occurring before the landmark time point (landmark analyses at time of DAPT discontinuation) and excluding patients who prematurely discontinued DAPT (defined by stopping at least one month before the period scheduled by randomisation, unless caused by an adverse event such as bleeding).
We performed a further sensitivity analysis including the two randomised controlled trials for which we did not have patient level data.37 38 In this case, we compared ≤6 month versus 12 month DAPT in patients with and without diabetes for net clinical adverse events (NACE; defined as the composite of all cause death, myocardial infarction, stroke, or major bleeding) because the published data ffom these two randomised controlled trials only reported hazard ratios for this endpoint in patients with or without diabetes. We used a two stage approach for this analysis. We calculated hazard ratios and 95% confidence intervals from the individual patient data available from the six randomised controlled trials and used the hazard ratios and risk ratios published in the subgroup analyses for the ISAR-SAFE and I-LOVE-IT 2 trials, respectively (see table E in appendix).37 38 We then combined all the estimates of effectiveness using standard meta-analysis methods.
We assessed heterogeneity with τ2 statistic, with values <0.04, 0.04-0.36, and >0.36 representing mild, moderate, and severe heterogeneity, respectively.39
Values of P<0.05 were considered significant for all analyses. We used Stata version 14 (StataCorp, College Station, TX), R (R Foundation for Statistical Computing, Vienna, Austria), and Reviewer Manager version 5.2 (RevMan; Nordic Cochrane Centre, Copenhagen).
Results
Figure 1 shows the study population (the study flow diagram is shown in fig A in the appendix). Six trials were included in the final analysis, comprising PRODIGY,25 OPTIMIZE,26 EXCELLENT,27 RESET,28 SECURITY,29 and ITALIC30 (tables A-C in appendix). Among these randomised controlled trials, two studies compared 3 month with 12 month DAPT (RESET and OPTIMIZE), two studies compared 6 month with 12 month DAPT (EXCELLENT and SECURITY), and two studies compared 6 month with 24 month DAPT (PRODIGY and ITALIC) (fig 1). The risk of bias was generally low, although the treatment was open label in all trials, and SECURITY and ITALIC were stopped early because of recruitment problems (table D in appendix). When we checked the individual patient data, we did not identify any relevant issues undermining the data integrity.
Patient population
Among the 11 473 randomised patients identified, 3681 (32.1%) had diabetes (mean age 63.7, SD 9.9), 7708 (67.2%) did not have diabetes (mean age 62.8, SD 11.0), and the information was missing in 84 (0.7%) (fig 1). Among patients with diabetes, 677 patients (mean age 62.8, SD 10.1) were treated with insulin (18.4% of those with diabetes; 5.9% of the overall population). The numbers randomised to long term versus short term DAPT were, respectively, 1853 and 1828 in the group with diabetes, 340 and 337 in the group with diabetes treated with insulin, and 3848 and 3860 in the group without diabetes.
Baseline characteristics
Baseline characteristics were well balanced between long term and short term DAPT arms within the groups with and without diabetes (table 1). There were, however, distinct differences in almost every variable between patients with and without diabetes (table F in appendix). Patients with diabetes were older, more likely to be women, and had higher rates of cardiovascular disease (hypertension, hypercholesterolaemia, previous myocardial infarction, previous percutaneous coronary intervention, previous coronary artery bypass grafting, previous stroke, and renal dysfunction) than those without diabetes (table F in appendix). Stable angina was more often the clinical presentation in both those with and without diabetes. Patients with diabetes had more extensive coronary artery disease, as evidenced by the higher number of diseased vessels, treated vessels and lesions, bifurcation treatment, stents implanted, and longer total stent length but smaller stent diameter implanted (table F in appendix).
Table 1.
Baseline characteristics according to randomisation for duration of dual antiplatelet therapy (DAPT) after implantation of drug eluting stent in randomised controlled trials according to diabetes status. Figures are percentages (numbers) of patients unless specified otherwise
| Characteristic | Diabetes (n=3681) | No diabetes (n=7708) | |||||
|---|---|---|---|---|---|---|---|
| Long DAPT (n=1853) | Short DAPT (n=1828) | P value | Long DAPT (n=3848) | Short DAPT (n=3860) | P value | ||
| Mean (SD) age (years) | 63.7 (10.0) | 63.6 (9.9) | 0.60 | 62.8 (11.1) | 62.8 (10.8) | 0.73 | |
| Men | 64.0 (1186/1853) | 65.8 (1202/1828) | 0.27 | 72.0 (2770/3848) | 72.2 (2787/3860) | 0.83 | |
| Hypertension | 87.4 (1618/1852) | 87.0 (1591/1828) | 0.76 | 75.1 (2889/3846) | 74.5 (2873/3856) | 0.54 | |
| Hypercholesterolaemia | 72.3 (1326/1834) | 71.9 (1302/1810) | 0.81 | 60.7 (2308/3803) | 60.1 (2296/3821) | 0.59 | |
| Smoking | 17.6 (274/1558) | 19.5 (301/1543) | 0.17 | 23.6 (799/3381) | 24.0 (816/3403) | 0.74 | |
| Previous myocardial infarction | 22.6 (371/1638) | 25.2 (416/1652) | 0.09 | 21.2 (742/3505) | 20.2 (706/3501) | 0.30 | |
| Previous PCI | 19.5 (321/1646) | 21.4 (354/1658) | 0.19 | 15.7 (550/3511) | 16.6 (585/3516) | 0.27 | |
| Previous CABG | 7.7 (126/1645) | 7.3 (121/1657) | 0.70 | 5.6 (196/3507) | 5.4 (190/3518) | 0.73 | |
| Previous stroke | 4.4 (54/1230) | 6.2 (78/1257) | 0.05 | 3.3 (81/2457) | 3.1 (78/2482) | 0.76 | |
| Creatinine >106.08 μmol/L | 10.9 (79/725) | 8.2 (59/720) | 0.08 | 7.4 (133/1804) | 6.9 (125/1812) | 0.58 | |
| Clinical presentation: | |||||||
| Stable angina pectoris | 62.5 (1159/1853) | 59.8 (1094/1828) | 0.09 | 56.6 (2178/3847) | 57.7 (2227/3860) | 0.34 | |
| Acute coronary syndrome | 37.5 (694/1853) | 40.2 (734/1828) | 43.4 (1669/3847) | 42.3 (1633/3860) | |||
| STEMI | 3.3 (61/1853) | 3.0 (55/1828) | — | 6.4 (247/3847) | 6.9 (265/3860) | — | |
| NSTEMI | 7.4 (137/1853) | 7.2 (131/1828) | — | 9.0 (348/3847) | 8.5 (328/3860) | — | |
| Unstable angina | 26.8 (496/1853) | 30.0 (548/1828) | — | 27.9 (1074/3847) | 26.9 (1040/3860) | — | |
| Discharge drugs: | |||||||
| Aspirin | 99.9 (1292/1293) | 99.9 (1277/1278) | 0.99 | 99.5 (2693/2706) | 99.8 (2694/2699) | 0.06 | |
| Clopidogrel | 99.8 (1290/1293) | 99.6 (1273/1278) | 0.47 | 99.7 (2699/2706) | 99.6 (2688/2699) | 0.49 | |
| β blockers | 71.5 (765/1070) | 70.8 (759/1072) | 0.72 | 70.0 (1555/2222) | 68.4 (1527/2232) | 0.26 | |
| ACEI/ARB | 60.3 (645/1070) | 62.6 (671/1072) | 0.27 | 56.9 (1265/2222) | 57.1 (1275/2232) | 0.90 | |
| Statins | 86.5 (926/1070) | 87.7 (940/1072) | 0.43 | 86.8 (1928/2222) | 88.1 (1966/2232) | 0.19 | |
| Mean (SD) diseased vessels/patient | 1.53 (0.9) | 1.54 (0.9) | 0.79 | 1.48 (0.8) | 1.49 (0.8) | 0.81 | |
| Mean (SD) No of treated vessels/patient | 1.22 (0.5) | 1.25 (0.5) | 0.15 | 1.21 (0.4) | 1.20 (0.4) | 0.41 | |
| Mean (SD) No of stents/patient | 1.58 (0.9) | 1.60 (0.9) | 0.64 | 1.51 (0.8) | 1.48 (0.8) | 0.31 | |
| Mean (SD) No of lesions stented/patient | 1.33 (0.6) | 1.34 (0.6) | 0.83 | 1.26 (0.5) | 1.26 (0.5) | 0.53 | |
| Mean (SD) total stent length/patient (mm) | 39.0 (26.1) | 39.3 (26.7) | 0.85 | 34.6 (22.9) | 33.9 (23.1) | 0.35 | |
| Mean (SD) smallest stent implanted (mm) | 3.0 (0.5) | 3.0 (0.4) | 0.35 | 3.1 (0.8) | 3.1 (0.5) | 0.78 | |
| Type of drug eluting stent: | |||||||
| PES | 4.1 (75/1844) | 4.2 (76/1820) | <0.001 | 4.8 (182/3831) | 4.8 (183/3840) | <0.001 | |
| SES | 4.3 (80/1844) | 3.7 (68/1820) | 11.1 (425/3831) | 2.5 (96/3840) | |||
| EES | 39.4 (727/1844) | 34.7 (631/1820) | 35.4 (1357/3831) | 30.9 (1185/3840) | |||
| ZES | 47.5 (875/1844) | 52.9 (962/1820) | 44.1 (1689/3831) | 57.0 (2190/3840) | |||
| BES | 4.0 (74/1844) | 3.8 (70/1820) | 4.0 (154/3831) | 4.2 (160/3840) | |||
| Mixed | 0.5 (9/1844) | 0.4 (8/1820) | 0.5 (19/3831) | 0.3 (13/3840) | |||
| Other | 0.2 (4/1844) | 0.3 (5/1820) | 0.1 (5/3831) | 0.3 (13/3840) | |||
| Stented coronary artery: | |||||||
| Left main | 2.3 (23/998) | 2.7 (27/1002) | 0.58 | 2.3 (54/2369) | 2.2 (52/2372) | 0.84 | |
| LAD | 62.5 (726/1161) | 65.5 (763/1165) | 0.14 | 62.8 (1657/2639) | 62.3 (1656/2659) | 0.70 | |
| LCx | 35.1 (381/1087) | 33.0 (358/1085) | 0.31 | 31.2 (778/2497) | 30.7 (758/2472) | 0.71 | |
| RCA | 39.7 (428/1078) | 39.8 (434/1091) | 0.97 | 34.5 (862/2497) | 30.6 (868/2508) | 0.95 | |
| Bifurcation | 18.4 (115/624) | 18.8 (115/612) | 0.87 | 16.0 (225/1410) | 14.3 (203/1424) | 0.21 | |
| Chronic total occlusion | 2.0 (22/1084) | 2.7 (29/1083) | 0.32 | 2.3 (51/2240) | 2.4 (55/2247) | 0.71 | |
BES=biolimus eluting stent; CABG=coronary artery bypass graft; EES=everolimus eluting stent; GFR=glomerular filtration rate; LAD=left anterior descending artery; NSTEMI=non-ST elevation myocardial infarction; PCI=percutaneous coronary intervention; PES=paclitaxel eluting stent; SES=sirolimus eluting stent; STEMI= ST elevation myocardial infarction; SVG=saphenous vein graft; ZES=zotarolimus eluting stent.
Impact of diabetes on the primary endpoint
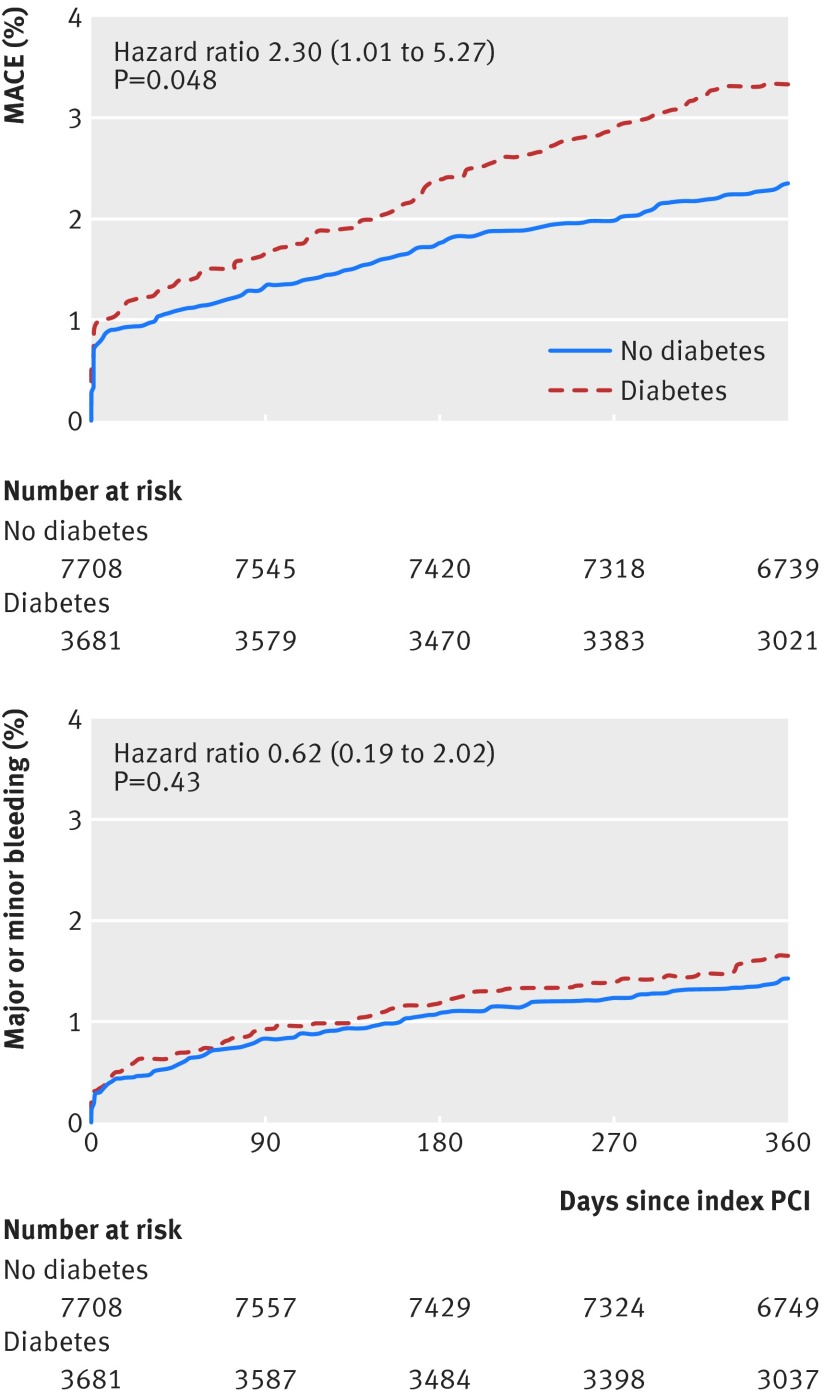
Diabetes (P=0.046), number of diseased vessels (P=0.004), and total stent length per patient (P=0.002) were independent predictors of MACE. Compared with patients without diabetes, those with diabetes had significantly higher rates of MACE (adjusted hazard ratio 2.30, 95% confidence interval 1.01 to 5.27; P=0.048) (fig 2).
Fig 2 Ischaemic and bleeding events in patients with and without diabetes. PCI=percutaneous coronary intervention
Long term v short term DAPT for primary endpoint according to diabetes status
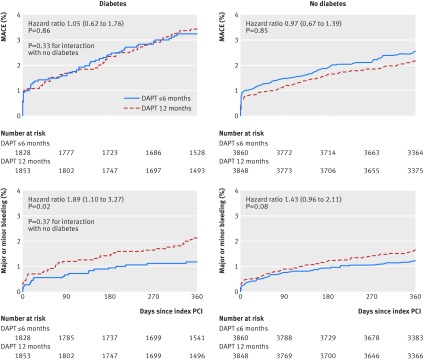
The rates of MACE at one year were similar among patients treated with long term versus short term DAPT in each subgroup (hazard ratio 1.05, 95% confidence interval 0.62 to 1.76, P=0.86, τ2=0.16, for those with diabetes; 0.97, 0.67 to 1.39, P=0.85, τ2=0.06, for those without diabetes; interaction P=0.33) (fig 3, table 2).
Fig 3 Ischaemic and bleeding events in patients with or without diabetes according to long term and short term DAPT. PCI=percutaneous coronary intervention
Table 2.
Clinical outcomes in long term versus short term dual antiplatelet therapy (DAPT) after implantation of drug eluting stent stratified by diabetes
| Diabetes (n=3681) | No diabetes (n=7708) | P for interaction | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Long DAPT (n=1853) | Short DAPT (n=1828) | HR (95% CI) | P value | τ2 | Long DAPT (n=3848) | Short DAPT (n=3860) | HR (95% CI) | P value | τ2 | |||
| MACE | 62 (3.3) | 58 (3.2) | 1.05 (0.62 to 1.76) | 0.86 | 0.16 | 82 (2.1) | 97 (2.5) | 0.97 (0.67 to 1.39) | 0.85 | 0.06 | 0.33 | |
| All cause death, MI, or stroke | 74 (4.0) | 66 (3.6) | 1.10 (0.79 to 1.54) | 0.58 | 0.00 | 93 (2.4) | 99 (2.6) | 1.02 (0.72 to 1.46) | 0.91 | 0.07 | 0.48 | |
| Cardiac death, MI, or stroke | 69 (3.7) | 59 (3.2) | 1.12 (0.79 to 1.60) | 0.52 | 0.01 | 90 (2.3) | 106 (2.7) | 1.01 (0.68 to 1.49) | 0.97 | 0.11 | 0.16 | |
| All cause death, MI, stroke, or major bleeding | 81 (4.4) | 69 (3.8) | 1.16 (0.83 to 1.60) | 0.39 | 0.01 | 109 (2.8) | 107 (2.8) | 1.12 (0.76 to 1.66) | 0.56 | 0.12 | 0.58 | |
| Cardiac death, MI, stroke, or major bleeding | 81 (4.4) | 71 (3.9) | 1.10 (0.79 to 1.53) | 0.57 | 0.01 | 117 (3.0) | 120 (3.1) | 1.23 (0.77 to 1.96) | 0.38 | 0.22 | 0.46 | |
| All cause death or MI | 68 (3.7) | 59 (3.2) | 1.16 (0.78 to 1.72) | 0.46 | 0.04 | 83 (2.2) | 90 (2.3) | 1.02 (0.71 to 1.47) | 0.91 | 0.07 | 0.39 | |
| Cardiac death or MI | 60 (3.2) | 56 (3.1) | 1.05 (0.65 to 1.69) | 0.85 | 0.11 | 80 (2.1) | 93 (2.4) | 1.08 (0.69 to 1.70) | 0.73 | 0.16 | 0.37 | |
| All cause death | 49 (2.6) | 39 (2.1) | 1.34 (0.87 to 2.06) | 0.19 | 0.02 | 59 (1.5) | 57 (1.5) | 1.05 (0.73 to 1.51) | 0.81 | 0.00 | 0.53 | |
| Cardiac death | 30 (1.6) | 23 (1.3) | 1.29 (0.75 to 2.23) | 0.36 | 0.00 | 37 (1.0) | 35 (0.9) | 1.17 (0.72 to 1.91) | 0.53 | 0.03 | 0.58 | |
| Stroke | 13 (0.7) | 10 (0.5) | 1.29 (0.56 to 2.97) | 0.55 | 0.02 | 15 (0.4) | 16 (0.4) | 0.94 (0.47 to 1.90) | 0.87 | 0.00 | 0.57 | |
| MI | 37 (2.0) | 39 (2.1) | 0.95 (0.58 to 1.54) | 0.82 | 0.03 | 55 (1.4) | 62 (1.6) | 1.15 (0.68 to 1.94) | 0.60 | 0.19 | 0.84 | |
| Definite ST | 4 (0.2) | 11 (0.6) | 0.34 (0.11 to 1.08) | 0.07 | 0.04 | 13 (0.3) | 8 (0.2) | 1.63 (0.67 to 3.97) | 0.28 | 0.02 | 0.04 | |
| Probable ST | 3 (0.2) | 5 (0.3) | 0.59 (0.14 to 2.48) | 0.47 | 0.00 | 4 (0.1) | 4 (0.1) | 0.87 (0.21 to 3.62) | 0.85 | 0.10 | 0.61 | |
| Definite/probable ST | 7 (0.4) | 16 (0.9) | 0.26 (0.09 to 0.80) | 0.02 | 0.47 | 17 (0.4) | 12 (0.3) | 1.42 (0.68 to 2.98) | 0.35 | 0.00 | 0.04 | |
| MI or definite/probable ST | 42 (2.3) | 46 (2.5) | 0.90 (0.55 to 1.46) | 0.66 | 0.06 | 60 (1.6) | 71 (1.8) | 0.94 (0.64 to 1.38) | 0.75 | 0.04 | 0.79 | |
| TVR | 56 (3.0) | 71 (3.9) | 0.82 (0.57 to 1.90) | 0.30 | 0.02 | 107 (2.8) | 115 (3.0) | 0.86 (0.63 to 1.16) | 0.32 | 0.03 | 0.42 | |
| Major or minor bleeding | 38 (2.1) | 21 (1.1) | 1.89 (1.10 to 3.27) | 0.02 | 0.02 | 62 (1.6) | 46 (1.2) | 1.43 (0.96 to 2.11) | 0.08 | 0.01 | 0.37 | |
| Major bleeding | 14 (0.8) | 8 (0.4) | 1.72 (0.72 to 4.10) | 0.22 | 0.00 | 30 (0.8) | 14 (0.4) | 2.56 (1.08 to 6.07) | 0.03 | 0.43 | 0.69 | |
| Minor bleeding | 24 (1.3) | 13 (0.7) | 3.91 (1.24 to 12.40) | 0.02 | 0.87 | 33 (0.9) | 35 (0.9) | 0.82 (0.49 to 1.37) | 0.45 | 0.04 | 0.11 | |
MACE=major adverse cardiac events (cardiac death, myocardial infarction (MI), or definite/probable stent thrombosis (ST)); TVR=target vessel revascularisation.
Within the group of patients with diabetes, there were no significant differences in MACE between long term and short term DAPT at one year among prespecified subgroups (sex, age ≥65, acute coronary syndrome, multivessel disease) as well as in patients without diabetes (table 3). Even in subgroups there was no significant interaction between diabetes and DAPT regimen (table 3).
Table 3.
Major adverse cardiac events (MACE) for long term versus short term dual antiplatelet therapy (DAPT) after implantation of drug eluting stent in subgroups of patients with or without diabetes
| Diabetes (n=3681) | No diabetes (n=7708) | P for interaction for diabetes/DAPT | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | P value | τ2 | P for interaction | HR (95% CI) | P value | τ2 | P for interaction | |||
| Age (years): | ||||||||||
| <65 | 1.26 (0.33 to 4.77) | 0.74 | 1.87 | 0.84 | 0.84 (0.52 to 1.34) | 0.46 | 0.04 | 0.50 | 0.58 | |
| ≥65 | 1.09 (0.68 to 1.76) | 0.71 | 0.00 | 1.05 (0.68 to 1.63) | 0.82 | 0.05 | 0.91 | |||
| Sex: | ||||||||||
| Women | 1.32 (0.78 to 2.21) | 0.30 | 0.03 | 0.09 | 1.25 (0.65 to 2.37) | 0.50 | 0.14 | 0.20 | 0.90 | |
| Men | 0.67 (0.38 to 1.21) | 0.90 | 0.08 | 0.77 (0.55 to 1.10) | 0.15 | 0.00 | 0.69 | |||
| Clinical presentation: | ||||||||||
| Stable CAD | 1.10 (0.63 to 1.92) | 0.74 | 0.09 | 0.84 | 1.21 (0.79 to 1.85) | 0.38 | 0.03 | 0.20 | 0.79 | |
| ACS | 0.98 (0.37 to 2.58) | 0.97 | 0.83 | 0.76 (0.43 to 1.33) | 0.34 | 0.16 | 0.66 | |||
| Multivessel disease: | ||||||||||
| No | 1.74 (0.91 to 3.32) | 0.09 | 0.17 | 0.09 | 1.27 (0.82 to 1.96) | 0.28 | 0.06 | 0.12 | 0.43 | |
| Yes | 0.75 (0.36 to 1.57) | 0.44 | 0.38 | 0.69 (0.37 to 1.28) | 0.24 | 0.20 | 0.87 | |||
ACS=acute coronary syndrome; CAD=coronary artery disease.
Bleeding events
There were no significant differences in terms of bleeding in patients with or without diabetes (adjusted hazard ratio 0.62, 95% confidence interval 0.19 to 2.02; P=0.43) (fig 2; table G in appendix). Conversely, 12 month DAPT was associated with a significantly higher rate of major or minor bleeding compared with short term DAPT in patients with diabetes (1.89, 1.10 to 3.27; P=0.02; τ2=0.02) and a non-significant increase in those without diabetes (1.43, 0.96 to 2.11; P=0.08; τ2=0.01; interaction P=0.37) (fig 3, table 2). Major bleeding events were consistently increased with long term DAPT in both populations, though significantly only in patients without diabetes (1.72, 0.72 to 4.10, P=0.22, τ2=0.00, for those with diabetes; 2.56, 1.08 to 6.07, P=0.03, τ2=0.43, in those without diabetes; interaction P=0.69; table 2).
Other clinical outcomes
The risk of myocardial infarction was significantly increased among patients with diabetes compared with those without diabetes (adjusted hazard ratio 3.66, 95% confidence interval 1.25 to 10.69; P=0.018), and it was the major determinant of the overall increase of MACE (table G in appendix). There were, however, no significant differences in the risk of myocardial infarction between long term versus short term DAPT (0.95, 0.58 to 1.54, P=0.82, τ2=0.03, for those diabetes; 1.15, 0.68 to 1.94, P=0.60, τ2=0.19, for those without diabetes; interaction P=0.84; table 2).
The risk of definite or probable stent thrombosis was numerically but not significantly increased among patients with diabetes compared with those without (adjusted hazard ratio 1.89, 95% confidence interval 0.31 to 11.38; P=0.49; table G in appendix). There was a reduction in the risk of definite/probable stent thrombosis with long term compared with short term DAPT among patients with diabetes but with severe heterogeneity (0.26, 0.09 to 0.80; P=0.02; τ2=0.47), whereas no such effect was observed in patients without diabetes (1.42, 0.68 to 2.98; P=0.35; τ2=0.00), with positive interaction testing (interaction P=0.04; table 2).
Table 2 (and table G in appendix) reports all other endpoints. No significant differences emerged between patients treated with long term versus short term DAPT in patients with and without diabetes.
Sensitivity analyses
Consistent with the main analysis, rates of MACE were similar with long term or short term DAPT in both patients with and without diabetes in a landmark analysis in which we censored events encountered before DAPT discontinuation and excluding patients who stopped DAPT early (table H in appendix). This analysis confirmed the absence of differences observed in terms of myocardial infarction and the trend towards an increased risk of bleeding with DAPT for 12 months. In contrast with the main analysis, the rates of definite/probable stent thrombosis showed a trend towards reduced event rates in both patients with and without diabetes treated with DAPT for 12 months compared with short term treatment.
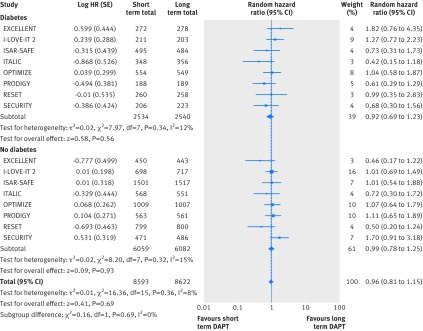
The overall results suggesting similar outcomes with short term and long term DAPT, irrespective of diabetes status, were further confirmed when we carried out the meta-analysis including published results from the ISAR-SAFE38 and I-LOVE-IT 237 trials. The composite of all cause death, myocardial infarction, stroke, or major bleeding was similar between short term and long term DAPT in both patients with diabetes (5074 patients; hazard ratio 0.92, 95% confidence interval 0.69 to 1.23; P=0.56; I2=12%; fig 4) and without diabetes (12 141 patients; 0.99, 0.78 to 1.25; P=0.69; I2=15%; fig 4), without significant heterogeneity between these subgroups (P=0.69; I2=0%; fig 4).
Fig 4 Net adverse clinical events in patients with and without diabetes according to long term and short term DAPT in eight randomised trials
Discussion
This patient level analysis of six randomised trials assessed clinical outcomes of long term versus short term DAPT in patients with or without diabetes. It showed that patients with diabetes, including those treated with insulin, had a higher baseline risk profile and showed an increased risk of MACE but not of bleeding, even after adjustment. Compared with short term DAPT, long term DAPT was associated with similar rates of MACE in patients with and without diabetes, although stent thrombosis was reduced. The risk of MACE did not differ across the prespecified subgroups of patients (by acute coronary syndrome, sex, multivessel disease, and age ≥65). Short term DAPT was associated with reduced risks of bleeding, irrespective of diabetes status.
To date, nine randomised controlled trials have looked at 3 or 6 months compared with 12 or more months of DAPT after implantation of a drug eluting stent.25 26 27 28 29 30 37 38 40 To our knowledge, this is the first comprehensive study to explore the comparison of clinical outcomes of short term (≤6 months) with long term (12 months) DAPT after drug eluting stent implantation according to diabetes status. The strength of our analysis is represented by the inclusion of individual patient level data from a large patient population from six multicentre multinational randomised trials. Individual patient level meta-analysis overcomes important limitations of study level meta-analysis and improves internal validity and allows for time to event, subgroup, and covariable adjusted analyses.
Drug eluting stents and DAPT
Compared with bare metal stents, drug eluting stents have consistently reduced the risk of restenosis and repeat revascularisation at the expense of safety concerns because of an increase in late and very late stent thrombosis.41 42 In particular, first generation drug eluting stents were associated with a four to fivefold higher risk of late and very late stent thrombosis compared with bare metal stents, leading to the concept of “the longer the better” regarding duration of DAPT in patients with drug eluting stents. Of note, new generation stents have been shown to be safer in terms of stent thrombosis than both early generation stents and bare metal stents.43 44 45 Prolonged DAPT, however, is associated with increased risks of bleeding and death, as well as healthcare costs.3 46 Therefore, the optimal duration is of paramount clinical relevance, although still a matter of debate.
Diabetes mellitus and DAPT
Diabetes mellitus is a key risk factor for atherosclerosis, disease progression, and restenosis during follow-up, particularly if patients are insulin dependent, even after coronary revascularisation.11 12 15 16 17 18 Notably, the detrimental metabolic state that accompanies diabetes is responsible for abnormalities in endothelial and platelet function that can contribute to accelerated atherosclerosis and increase the risk of adverse cardiovascular events.19 20 A large body of evidence has described the role of increased platelet activity and adhesion in the progression of vascular complications observed in patients with diabetes, characterised by a high incidence of cardiovascular events and lower antithrombotic efficacy of treatment with aspirin and clopidogrel.19 20 Indeed, patients with diabetes mellitus might have a smaller than expected response to aspirin (because of accelerated renewal of platelets and alteration of thromboxane pathway) and clopidogrel (the lower response to the drug in those with diabetes is mainly caused by abnormalities in the active metabolite pharmacokinetic profile, with only a minor contribution of platelet dysfunction related to the P2Y12 signalling pathway). Therefore, the clinical translation of these findings could lead to the concept that prolonged DAPT in patients with diabetes might be the rational approach, although it has not been clearly demonstrated.
A recent large observational study has suggested that extending the duration of clopidogrel treatment beyond 12 months could decrease rates of very late death or myocardial infarction only in patients with diabetes who had been treated with a first generation drug eluting stent compared with either patients without diabetes or those who had other stent types, although the latter group had an overall event rate higher than patients with a drug eluting stent.21 This study, however, like other retrospective studies, has relevant limitations, and appropriate adjustment is unlikely to eliminate selection bias.22 Randomised studies comparing different DAPT regimens have provided results of subgroup analyses. Interestingly, some contrasting evidence emerged from these analyses on the role of diabetes, although dedicated studies on the impact of diabetes, including in patients treated with insulin, have not been published to date.
In the EXCELLENT trial, there was a significant interaction between diabetes status and duration of DAPT (interaction P<0.001) for the primary endpoint (composite of cardiac death, myocardial infarction, or ischaemia driven target vessel revascularisation at 12 months), with patients with diabetes having a significant benefit with DAPT for 12 months compared with 6 months, whereas patients without diabetes had a significantly lower event rate with short term DAPT.27 Also the DAPT trial showed a significant interaction between diabetes and treatment arm (interaction P=0.01), although patients with diabetes did not benefit from prolonged DAPT (30 months) compared with patients without diabetes who experienced a lower risk of MACCE (major adverse cardiovascular and cerebrovascular events) (mainly because of a decreased risk of myocardial infarction and stent thrombosis).46 The recent dedicated subanalysis of the DAPT trial showed that prolonged DAPT reduced the risk of myocardial infarction, but this benefit was attenuated in patients with diabetes compared with those without diabetes.47 Similarly, in the DES-LATE, patients with diabetes showed a trend towards benefit from interrupting DAPT at 12 months, although the P value for interaction was borderline (P=0.07).48 Conversely, other trials, including OPTIMIZE,26 RESET,28 I-LOVE-IT 2,37 ISAR-SAFE,38 ARCTIC Interruption,49 and the recently published IVUS-XPL40 did not show significant heterogeneity between subgroups with and without diabetes. Even if characterised by a different design not matching with eligibility criteria of our meta-analysis (inclusion of patients with a history of myocardial infarction one to three years before, irrespective of percutaneous coronary intervention performed or drug eluting stent implanted), the recent substudy by the PEGASUS-TIMI 54 trial also confirmed the absence of potential significant heterogeneity related to diabetes status.50 Indeed, consistent with the findings in patients without diabetes, those with diabetes had long term benefits in terms of ischaemia and cardiovascular death but increased risk of bleeding with ticagrelor compared with placebo in addition to a background treatment with aspirin.50
Perspectives for clinical practice
Our study shows that compared with short term DAPT, long term DAPT does not provide benefits in terms of ischaemic protection but rather increases the risk of bleeding, irrespective of diabetes status. Although patients with diabetes are at increased risk for ischaemic events, and prolonged DAPT is often advised in these patients, our analysis indicates that prolonged treatment is not associated with improved outcomes among patients with stents with and without diabetes, even when we restricted the analysis to the subgroup of patients with diabetes treated with insulin (see supplementary results in appendix). Although we observed a lower risk of definite/probable stent thrombosis with DAPT for 12 months in patients with diabetes, this finding should be interpreted in the context of high heterogeneity between trials, hampering definitive conclusions; moreover the absence of consistent benefit in terms of composite endpoints of ischaemic events (adding stent thrombosis to myocardial infarction or death (cardiac or all cause)) as well as at the landmark analyses (in which we excluded events occurring in the first three to six months when both randomised treatments were, by study design, identical) was reassuring on the clinical implications of this small excess of stent thrombosis in such patients. On the contrary, the relevance of our overall findings should be interpreted in light of the baseline characteristics of the included patients, particularly concerning the risk of bleeding. Indeed, compared with studies dedicated to patients with high risk (such as LEADERS-FREE with 18.6% of all bleeding and 7.3% of major bleeding (BARC type 3 or 5) at one year51), our study population can be considered at low risk given that the overall rate of major or minor bleeding events was about 1.5% at one year, of which major bleeding was 0.6% compared with 0.4%, 0.4%, 2.6%, 0.7%, 0.9%, and 0.3% in RESET, EXCELLENT, PRODIGY, OPTIMIZE, SECURITY, and ITALIC trials, respectively. Furthermore, a recent meta-regression analysis of DAPT trials underlined the concept that in the contemporary era of drug eluting stents, bleeding has a stronger impact on mortality than stent thrombosis.5 In line with this, the absence of benefit at the expense of an increased risk of bleeding in patients with diabetes treated with long term compared with short term DAPT is relevant and underlines the opportunity to shorten DAPT in this subset of patients.
Limitations
Our study shares limitations of other meta-analyses, although the analysis of patient level data mitigates some of them. As the six randomised controlled trials we included were not specifically designed to investigate outcomes in the subgroup of patients with diabetes, our study has intrinsic limitations of subgroup analyses and should be considered as hypothesis generating. The pooling of data, however, allowed us to obtain a large number of patients with diabetes (n=3681) as well as insulin treated diabetes (n=677) to be compared with patients without diabetes. Even though we collected individual data from randomised controlled trials, the post hoc nature of this analysis introduces biases. Furthermore, it remains unclear if our findings could be applicable to all patients with diabetes irrespective of its type (type 1 or 2) as this information was not available.
The results described cannot be extended to all types of drug eluting stent because zotarolimus and everolimus eluting stents were more commonly implanted. Similarly, as all patients received clopidogrel, our findings could have differed if novel anti-platelet agents such as prasugrel or ticagrelor had been used. Definitions of some clinical endpoints differed slightly across trials, potentially introducing effect modifiers. Although the meta-analysis of eight randomised controlled trials confirmed the findings of short versus long term DAPT, this was conducted without patient level data from two randomised controlled trials, and net clinical adverse events was the only endpoint that we were able to analyse from the published data in the subgroups for diabetes status. Finally, most of the trials randomised patients at the time of the percutaneous coronary intervention or a month later, before the three to six months planned discontinuation of DAPT. Differences in events occurring within three to six months of DAPT are chance effects, but the sensitivity analysis that excluded those events confirmed the findings of the main analysis.
Conclusions
Although the presence of diabetes emerged as an independent predictor of MACE, long term compared with short term DAPT did not reduce the risk of MACE but increased the risk of bleeding among patients with and without diabetes. This study might have relevant implications for clinicians and patients and could modify current daily clinical practice. A shorter DAPT regimen was found to be effective and safe in patients with and without diabetes. Diabetes per se should not be a driver for prolonging DAPT over the mandatory period after implantation of a drug eluting stent because of increased risks compared with potential benefits of this strategy. Future studies should be specifically designed and powered to deal with patients with diabetes and should explore the optimal duration of DAPT according to the type of diabetes and its medical management.
What is already known on this topic
Dual antiplatelet therapy (DAPT) is the standard of care among patients undergoing percutaneous coronary intervention, but its optimal duration is debated, particularly after implantation of a drug eluting stent
Some trials have shown that short term (up to 6 months) DAPT is not inferior to 12 months of treatment
As diabetes is a well known risk factor for cardiovascular disease as well as for disease progression and ischaemic complications after percutaneous coronary intervention, patients might benefit from prolonged DAPT
What this study adds
After percutaneous coronary intervention with implantation of a drug eluting stent, patients with diabetes, including those receiving treatment with insulin, were confirmed to be at higher risk of ischaemic events compared with patients without diabetes, though long term compared with short term DAPT did not reduce ischaemic or composite endpoints and slightly increased the risk of bleeding in patients with and without diabetes
Short term DAPT after implantation of a drug eluting stent is as effective as long term DAPT in patients with or without diabetes and might reduce risks and costs of prolonged treatment
Web Extra.
Extra material supplied by the author
Appendix: Supplementary material
Contributors: GG and MV conceived and designed the study; GG, MV, and TP collected the data; GG, BRdaC, and MV undertook the statistical analysis; GG, MV, and SW drafted the manuscript; all authors had full access to all the data, including statistical reports and tables; all authors analysed and interpreted the data; all authors critically revised the manuscript for important intellectual content; MV is guarantor.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: MV has received research grants from The Medicines Company and Terumo; GG reports research grants from the European Association of Percutaneous Cardiovascular Interventions (EAPCI) and from the Cardiopath PhD Program (Federico II University of Naples); DLB is on the advisory boards for Cardax, Elsevier Practice Update Cardiology, Medscape Cardiology, Regado Biosciences; board of directors for Boston VA Research Institute, Society of Cardiovascular Patient Care; chair of American Heart Association Quality Oversight Committee; data monitoring committees at Duke Clinical Research Institute, Harvard Clinical Research Institute, Mayo Clinic, Population Health Research Institute; honorariums from American College of Cardiology (senior associate editor, Clinical Trials and News, ACC.org), Belvoir Publications (editor in chief, Harvard Heart Letter), Duke Clinical Research Institute (clinical trial steering committees), Harvard Clinical Research Institute (clinical trial steering committee), HMP Communications (editor in chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (guest editor; associate editor), Population Health Research Institute (clinical trial steering committee), Slack Publications (chief medical editor, Cardiology Today’s Intervention), Society of Cardiovascular Patient Care (secretary/treasurer), WebMD (CME steering committees); Clinical Cardiology (deputy editor), NCDR-ACTION registry steering committee (vice-chair), VA CART research and publications committee (chair); and has received research funding from Amarin, AstraZeneca, Bristol-Myers Squibb, Eisai, Ethicon, Forest Laboratories, Ischemix, Medtronic, Pfizer, Roche, Sanofi Aventis, The Medicines Company; royalties from Elsevier (editor, Cardiovascular Intervention: A Companion to Braunwald’s Heart Disease); site co-investigator: Biotronik, Boston Scientific, St. Jude Medical; trustee: American College of Cardiology; unfunded research: FlowCo, PLx Pharma, Takeda; other authors report no conflicts of interest.
Ethical approval: Not required.
Data sharing: No additional data available.
Transparency: The manuscript’s guarantor affirms that the manuscript is an honest, accurate, and transparent account of the study being reported, that no important aspects of the study have been omitted and that any discrepancies from the study as planned have been explained.
References
- 1.Valgimigli M, Ariotti S, Costa F. Duration of dual antiplatelet therapy after drug-eluting stent implantation: will we ever reach a consensus?Eur Heart J 2015;36:1219-22. 10.1093/eurheartj/ehv053 pmid:25761893. [DOI] [PubMed] [Google Scholar]
- 2.Valgimigli M, Costa F, Byrne R, Haude M, Baumbach A, Windecker S. Dual antiplatelet therapy duration after coronary stenting in clinical practice: results of an EAPCI survey. EuroIntervention 2015;11:68-74. 10.4244/EIJV11I1A11 pmid:25982650. [DOI] [PubMed] [Google Scholar]
- 3.Navarese EP, Andreotti F, Schulze V, et al. Optimal duration of dual antiplatelet therapy after percutaneous coronary intervention with drug eluting stents: meta-analysis of randomised controlled trials. BMJ 2015;350:h1618 10.1136/bmj.h1618 pmid:25883067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Montalescot G, Brieger D, Dalby AJ, Park SJ, Mehran R. Duration of Dual Antiplatelet Therapy After Coronary Stenting: A Review of the Evidence. J Am Coll Cardiol 2015;66:832-47. 10.1016/j.jacc.2015.05.053 pmid:26271067. [DOI] [PubMed] [Google Scholar]
- 5.Capodanno D, Gargiulo G, Buccheri S, Giacoppo D, Capranzano P, Tamburino C. Meta-Analyses of Dual Antiplatelet Therapy Following Drug-Eluting Stent Implantation: Do Bleeding and Stent Thrombosis Weigh Similar on Mortality?J Am Coll Cardiol 2015;66:1639-40. 10.1016/j.jacc.2015.05.085 pmid:26429096. [DOI] [PubMed] [Google Scholar]
- 6.Palmerini T, Stone GW. Optimal duration of dual antiplatelet therapy after drug-eluting stent implantation: conceptual evolution based on emerging evidence. Eur Heart J 2016;37:353-64. 10.1093/eurheartj/ehv712 pmid:26795933. [DOI] [PubMed] [Google Scholar]
- 7.Palmerini T, Benedetto U, Bacchi-Reggiani L, et al. Mortality in patients treated with extended duration dual antiplatelet therapy after drug-eluting stent implantation: a pairwise and Bayesian network meta-analysis of randomised trials. Lancet 2015;385:2371-82. 10.1016/S0140-6736(15)60263-X pmid:25777667. [DOI] [PubMed] [Google Scholar]
- 8.Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS guidelines on myocardial revascularization. EuroIntervention 2015;10:1024-94. 10.4244/EIJY14M09_01 pmid:25187201. [DOI] [PubMed] [Google Scholar]
- 9.Levine GN, Bates ER, Blankenship JC, et al. American College of Cardiology Foundation American Heart Association Task Force on Practice Guidelines Society for Cardiovascular Angiography and Interventions. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol 2011;58:e44-122. 10.1016/j.jacc.2011.08.007 pmid:22070834. [DOI] [PubMed] [Google Scholar]
- 10.Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2016;68:1082-115. 10.1016/j.jacc.2016.03.513 pmid:27036918. [DOI] [PubMed] [Google Scholar]
- 11.Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA 2002;287:2570-81. 10.1001/jama.287.19.2570 pmid:12020339. [DOI] [PubMed] [Google Scholar]
- 12.Van Belle E, Périé M, Braune D, et al. Effects of coronary stenting on vessel patency and long-term clinical outcome after percutaneous coronary revascularization in diabetic patients. J Am Coll Cardiol 2002;40:410-7. 10.1016/S0735-1097(02)01971-X pmid:12142104. [DOI] [PubMed] [Google Scholar]
- 13.Rydén L, Grant PJ, Anker SD, et al. Authors/Task Force Members ESC Committee for Practice Guidelines (CPG) Document Reviewers. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). Eur Heart J 2013;34:3035-87. 10.1093/eurheartj/eht108 pmid:23996285. [DOI] [PubMed] [Google Scholar]
- 14.Alabas OA, Hall M, Dondo TB, et al. Long-term excess mortality associated with diabetes following acute myocardial infarction: a population-based cohort study. J Epidemiol Community Health 2016;jech-2016-207402 10.1136/jech-2016-207402. pmid:27307468. [DOI] [PubMed] [Google Scholar]
- 15.Koskinas KC, Siontis GC, Piccolo R, et al. Impact of Diabetic Status on Outcomes After Revascularization With Drug-Eluting Stents in Relation to Coronary Artery Disease Complexity: Patient-Level Pooled Analysis of 6081 Patients. Circ Cardiovasc Interv 2016;9:e003255 10.1161/CIRCINTERVENTIONS.115.003255 pmid:26823484. [DOI] [PubMed] [Google Scholar]
- 16.Windecker S, Stortecky S, Stefanini GG, et al. Revascularisation versus medical treatment in patients with stable coronary artery disease: network meta-analysis. BMJ 2014;348:g3859 10.1136/bmj.g3859 pmid:24958153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bangalore S, Kumar S, Fusaro M, et al. Outcomes with various drug eluting or bare metal stents in patients with diabetes mellitus: mixed treatment comparison analysis of 22,844 patient years of follow-up from randomised trials. BMJ 2012;345:e5170 10.1136/bmj.e5170 pmid:22885395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Armstrong EJ, Waltenberger J, Rogers JH. Percutaneous coronary intervention in patients with diabetes: current concepts and future directions. J Diabetes Sci Technol 2014;8:581-9. 10.1177/1932296813517058 pmid:24876623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Santilli F, Simeone P, Liani R, Davì G. Platelets and diabetes mellitus. Prostaglandins Other Lipid Mediat 2015;120:28-39. 10.1016/j.prostaglandins.2015.05.002 pmid:25986598. [DOI] [PubMed] [Google Scholar]
- 20.Jung JH, Tantry US, Gurbel PA, Jeong YH. Current antiplatelet treatment strategy in patients with diabetes mellitus. Diabetes Metab J 2015;39:95-113. 10.4093/dmj.2015.39.2.95 pmid:25922803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thukkani AK, Agrawal K, Prince L, et al. Long-Term Outcomes in Patients With Diabetes Mellitus Related to Prolonging Clopidogrel More Than 12 Months After Coronary Stenting. J Am Coll Cardiol 2015;66:1091-101. 10.1016/j.jacc.2015.06.1339 pmid:26337986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bittl JA. Dual-Antiplatelet Therapy for Diabetic Patients After Stent Implantation: Lessons From an Observational Study. J Am Coll Cardiol 2015;66:1102-4. 10.1016/j.jacc.2015.06.1338 pmid:26337987. [DOI] [PubMed] [Google Scholar]
- 23.Stewart LA, Clarke M, Rovers M, et al. PRISMA-IPD Development Group. Preferred Reporting Items for Systematic Review and Meta-Analyses of individual participant data: the PRISMA-IPD Statement. JAMA 2015;313:1657-65. 10.1001/jama.2015.3656 pmid:25919529. [DOI] [PubMed] [Google Scholar]
- 24.Palmerini T, Sangiorgi D, Valgimigli M, et al. Short- versus long-term dual antiplatelet therapy after drug-eluting stent implantation: an individual patient data pairwise and network meta-analysis. J Am Coll Cardiol 2015;65:1092-102. 10.1016/j.jacc.2014.12.046 pmid:25790880. [DOI] [PubMed] [Google Scholar]
- 25.Valgimigli M, Campo G, Monti M, et al. Prolonging Dual Antiplatelet Treatment After Grading Stent-Induced Intimal Hyperplasia Study (PRODIGY) Investigators. Short- versus long-term duration of dual-antiplatelet therapy after coronary stenting: a randomized multicenter trial. Circulation 2012;125:2015-26. 10.1161/CIRCULATIONAHA.111.071589 pmid:22438530. [DOI] [PubMed] [Google Scholar]
- 26.Feres F, Costa RA, Abizaid A, et al. OPTIMIZE Trial Investigators. Three vs twelve months of dual antiplatelet therapy after zotarolimus-eluting stents: the OPTIMIZE randomized trial. JAMA 2013;310:2510-22.pmid:24177257. [DOI] [PubMed] [Google Scholar]
- 27.Gwon HC, Hahn JY, Park KW, et al. Six-month versus 12-month dual antiplatelet therapy after implantation of drug-eluting stents: the Efficacy of Xience/Promus Versus Cypher to Reduce Late Loss After Stenting (EXCELLENT) randomized, multicenter study. Circulation 2012;125:505-13. 10.1161/CIRCULATIONAHA.111.059022 pmid:22179532. [DOI] [PubMed] [Google Scholar]
- 28.Kim BK, Hong MK, Shin DH, et al. RESET Investigators. A new strategy for discontinuation of dual antiplatelet therapy: the RESET Trial (REal Safety and Efficacy of 3-month dual antiplatelet Therapy following Endeavor zotarolimus-eluting stent implantation). J Am Coll Cardiol 2012;60:1340-8. 10.1016/j.jacc.2012.06.043 pmid:22999717. [DOI] [PubMed] [Google Scholar]
- 29.Colombo A, Chieffo A, Frasheri A, et al. Second-generation drug-eluting stent implantation followed by 6- versus 12-month dual antiplatelet therapy: the SECURITY randomized clinical trial. J Am Coll Cardiol 2014;64:2086-97. 10.1016/j.jacc.2014.09.008 pmid:25236346. [DOI] [PubMed] [Google Scholar]
- 30.Gilard M, Barragan P, Noryani AA, et al. 6- versus 24-month dual antiplatelet therapy after implantation of drug-eluting stents in patients nonresistant to aspirin: the randomized, multicenter ITALIC trial. J Am Coll Cardiol 2015;65:777-86. 10.1016/j.jacc.2014.11.008 pmid:25461690. [DOI] [PubMed] [Google Scholar]
- 31.Valgimigli M, Borghesi M, Tebaldi M, Vranckx P, Parrinello G, Ferrari R. PROlonging Dual antiplatelet treatment after Grading stent-induced Intimal hyperplasia studY Investigators. Should duration of dual antiplatelet therapy depend on the type and/or potency of implanted stent? A pre-specified analysis from the PROlonging Dual antiplatelet treatment after Grading stent-induced Intimal hyperplasia studY (PRODIGY). Eur Heart J 2013;34:909-19. 10.1093/eurheartj/ehs460 pmid:23315904. [DOI] [PubMed] [Google Scholar]
- 32.Cutlip DE, Windecker S, Mehran R, et al. Academic Research Consortium. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation 2007;115:2344-51. 10.1161/CIRCULATIONAHA.106.685313 pmid:17470709. [DOI] [PubMed] [Google Scholar]
- 33.Bovill EG, Terrin ML, Stump DC, et al. Hemorrhagic events during therapy with recombinant tissue-type plasminogen activator, heparin, and aspirin for acute myocardial infarction. Results of the Thrombolysis in Myocardial Infarction (TIMI), Phase II Trial. Ann Intern Med 1991;115:256-65. 10.7326/0003-4819-115-4-256 pmid:1906692. [DOI] [PubMed] [Google Scholar]
- 34.Mehran R, Rao SV, Bhatt DL, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation 2011;123:2736-47. 10.1161/CIRCULATIONAHA.110.009449 pmid:21670242. [DOI] [PubMed] [Google Scholar]
- 35.Crowther MJ, Look MP, Riley RD. Multilevel mixed effects parametric survival models using adaptive Gauss-Hermite quadrature with application to recurrent events and individual participant data meta-analysis. Stat Med 2014;33:3844-58. 10.1002/sim.6191 pmid:24789760. [DOI] [PubMed] [Google Scholar]
- 36.Rondeau V, Michiels S, Liquet B, Pignon JP. Investigating trial and treatment heterogeneity in an individual patient data meta-analysis of survival data by means of the penalized maximum likelihood approach. Stat Med 2008;27:1894-910. 10.1002/sim.3161 pmid:18069745. [DOI] [PubMed] [Google Scholar]
- 37.Han Y, Xu B, Xu K, et al. Six Versus 12 Months of Dual Antiplatelet Therapy After Implantation of Biodegradable Polymer Sirolimus-Eluting Stent: Randomized Substudy of the I-LOVE-IT 2 Trial. Circ Cardiovasc Interv 2016;9:e003145 10.1161/CIRCINTERVENTIONS.115.003145 pmid:26858080. [DOI] [PubMed] [Google Scholar]
- 38.Schulz-Schüpke S, Byrne RA, Ten Berg JM, et al. Intracoronary Stenting and Antithrombotic Regimen: Safety And EFficacy of 6 Months Dual Antiplatelet Therapy After Drug-Eluting Stenting (ISAR-SAFE) Trial Investigators. ISAR-SAFE: a randomized, double-blind, placebo-controlled trial of 6 vs. 12 months of clopidogrel therapy after drug-eluting stenting. Eur Heart J 2015;36:1252-63. 10.1093/eurheartj/ehu523 pmid:25616646. [DOI] [PubMed] [Google Scholar]
- 39.da Costa BR, Juni P. Systematic reviews and meta-analyses of randomized trials: principles and pitfalls. Eur Heart J 2014;35:3336-45. 10.1093/eurheartj/ehu424 pmid:25416325. [DOI] [PubMed] [Google Scholar]
- 40.Hong SJ, Shin DH, Kim JS, et al. IVUS-XPL Investigators. 6-Month Versus 12-Month Dual-Antiplatelet Therapy Following Long Everolimus-Eluting Stent Implantation: The IVUS-XPL Randomized Clinical Trial. JACC Cardiovasc Interv 2016;9:1438-46. 10.1016/j.jcin.2016.04.036 pmid:27212028. [DOI] [PubMed] [Google Scholar]
- 41.Stone GW, Moses JW, Ellis SG, et al. Safety and efficacy of sirolimus- and paclitaxel-eluting coronary stents. N Engl J Med 2007;356:998-1008. 10.1056/NEJMoa067193 pmid:17296824. [DOI] [PubMed] [Google Scholar]
- 42.Bavry AA, Kumbhani DJ, Helton TJ, Borek PP, Mood GR, Bhatt DL. Late thrombosis of drug-eluting stents: a meta-analysis of randomized clinical trials. Am J Med 2006;119:1056-61. 10.1016/j.amjmed.2006.01.023 pmid:17145250. [DOI] [PubMed] [Google Scholar]
- 43.Bangalore S, Kumar S, Fusaro M, et al. Short- and long-term outcomes with drug-eluting and bare-metal coronary stents: a mixed-treatment comparison analysis of 117 762 patient-years of follow-up from randomized trials. Circulation 2012;125:2873-91. 10.1161/CIRCULATIONAHA.112.097014 pmid:22586281. [DOI] [PubMed] [Google Scholar]
- 44.Valgimigli M, Tebaldi M, Borghesi M, et al. PRODIGY Investigators. Two-year outcomes after first- or second-generation drug-eluting or bare-metal stent implantation in all-comer patients undergoing percutaneous coronary intervention: a pre-specified analysis from the PRODIGY study (PROlonging Dual Antiplatelet Treatment After Grading stent-induced Intimal hyperplasia studY). JACC Cardiovasc Interv 2014;7:20-8. 10.1016/j.jcin.2013.09.008 pmid:24332420. [DOI] [PubMed] [Google Scholar]
- 45.Bhatt DL. EXAMINATION of new drug-eluting stents--top of the class!Lancet 2012;380:1453-5. 10.1016/S0140-6736(12)61021-6 pmid:22951304. [DOI] [PubMed] [Google Scholar]
- 46.Mauri L, Kereiakes DJ, Yeh RW, et al. DAPT Study Investigators. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med 2014;371:2155-66. 10.1056/NEJMoa1409312 pmid:25399658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Meredith IT, Tanguay JF, Kereiakes DJ, et al. DAPT Study Investigators. Diabetes Mellitus and Prevention of Late Myocardial Infarction After Coronary Stenting in the Randomized Dual Antiplatelet Therapy Study. Circulation 2016;133:1772-82. 10.1161/CIRCULATIONAHA.115.016783 pmid:26994121. [DOI] [PubMed] [Google Scholar]
- 48.Lee CW, Ahn JM, Park DW, et al. Optimal duration of dual antiplatelet therapy after drug-eluting stent implantation: a randomized, controlled trial. Circulation 2014;129:304-12. 10.1161/CIRCULATIONAHA.113.003303 pmid:24097439. [DOI] [PubMed] [Google Scholar]
- 49.Collet JP, Silvain J, Barthélémy O, et al. ARCTIC investigators. Dual-antiplatelet treatment beyond 1 year after drug-eluting stent implantation (ARCTIC-Interruption): a randomised trial. Lancet 2014;384:1577-85. 10.1016/S0140-6736(14)60612-7 pmid:25037988. [DOI] [PubMed] [Google Scholar]
- 50.Bhatt DL, Bonaca MP, Bansilal S, et al. Reduction in Ischemic Events With Ticagrelor in Diabetic Patients With Prior Myocardial Infarction in PEGASUS-TIMI 54. J Am Coll Cardiol 2016;67:2732-40. 10.1016/j.jacc.2016.03.529 pmid:27046160. [DOI] [PubMed] [Google Scholar]
- 51.Urban P, Meredith IT, Abizaid A, et al. LEADERS FREE Investigators. Polymer-free Drug-Coated Coronary Stents in Patients at High Bleeding Risk. N Engl J Med 2015;373:2038-47. 10.1056/NEJMoa1503943 pmid:26466021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix: Supplementary material