Abstract
Objective
This study examined the relationship between the number of co-existing health problems (patient comorbidities and caregiver chronic conditions) and quality of life (QOL) among patients with advanced cancer and their caregivers, and assessed the mediating and moderating role of meaning-based coping on that relationship.
Methods
Data came from patients with advanced cancers (breast, colorectal, lung, and prostate) and their family caregivers (N=484 dyads). Study hypotheses were examined with structural equation modeling using the actor-partner interdependence mediation model (APIMeM). Bootstrapping and model constraints were used to test indirect effects suggested by the mediation models. An interaction term was added to the standard actor-partner interdependence model (APIM) to test for moderation effects.
Results
More patient comorbidities were associated with lower patient QOL. More caregiver chronic conditions were associated with lower patient and caregiver QOL. Patient comorbidities and caregiver chronic conditions had a negative influence on caregiver meaning-based coping, but no significant influence on patient meaning based coping. Caregiver meaning-based coping mediated relationships between patient comorbidities and caregiver health conditions and patient and caregiver QOL. No significant moderating effects were observed.
Conclusions
Despite the severity of advanced cancer for patients and caregivers, the co-existing health problems of one member of the dyad have the potential to directly or indirectly affect the wellbeing of the other. Future research should consider how the number of patient comorbidities and caregiver chronic conditions, as well as the ability of patients and caregivers to manage those conditions, influences their meaning-based coping and wellbeing.
Background
Advanced cancers, generally defined as cancers unlikely to be cured, significantly affect the quality of life (QOL) of patients and their family caregivers [1, 2]. Unfortunately, advanced cancer is often not the only health problem that patients and caregivers face. Compared to the general population, people with cancer report a similar or higher prevalence of chronic health conditions [3–5]. Evidence suggests that chronic diseases have a negative influence on patient QOL after a cancer diagnosis, but the extent of this influence among advanced cancers is not known [4, 6]. Furthermore, little is known about how cancer caregivers’ own chronic conditions – an indicator of caregiver health - influence caregiver well-being. As increased age is a significant risk factor for chronic conditions [7], and cancer caregivers tend to be older [8], it is likely that the prevalence of chronic conditions in this group is high. Though various factors such as caregiver mental health and perceived burden have been identified as key predictors of cancer caregiver QOL at advanced stages of disease [2, 9], considerations of caregivers’ own health concerns are limited.
Interdependence theory, which focuses on how social interactions influence behaviors, provides a framework for investigating how the health problems of one member of the patient/caregiver dyad influence the health outcomes of the other. This theory describes both actor effects – in this case, the effects one person’s health problems have on their own QOL - and partner effects – or the influence of a person’s health problems on their partner’s QOL [10]. For example, patient comorbidities may complicate patient symptom attribution and increase disease burden (actor effect) [11–13]. In turn, this could influence the responsibilities of family caregivers and their QOL (partner effect) [14]. Significant health challenges of family caregivers may influence both the quality and quantity of care they can provide to the patient, affecting the patient’s QOL, another example of a partner effect. The existence of these partner effects have been little-explored in the advanced cancer context; however, this is especially important to consider given that the work of these caregivers may be more intensive than found in earlier stages of disease or for non-cancer conditions [15, 16].
Yet, in spite of the challenges they face, patients with cancer and their caregivers often find ways to thrive. Meaning-based coping has been described as the positive reappraisal and reinterpretation of a stressor [17]. Patients who identify benefits or meaning from their cancer experience [18, 19] or believe cancer contributes to their personal growth [20] may experience better QOL. The ability of family caregivers to find positive meaning in their cancer caregiving experience is also associated with improved outcomes, such as fewer depressive symptoms, lower perceived burden and better self-rated health [21–23]. As a moderating variable, a negative relationship between co-existing chronic conditions and QOL could be attenuated in individuals who engage in more meaning-based coping. As a mediating variable, meaning-based coping would help explain why co-existing chronic conditions influence QOL. There is a noticeable lack of literature, however, exploring how non-cancer health problems affect patients’ and caregivers’ ability to engage in meaning-based coping after the cancer diagnosis.
Purpose & Hypotheses
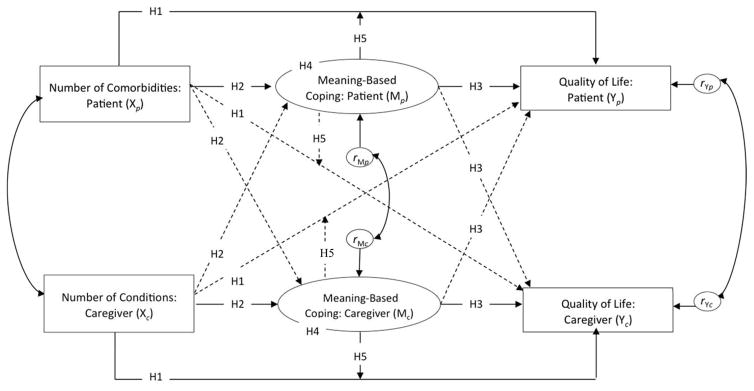
The purpose of this study was to examine the relationship between co-existing health problems (patient comorbidities and caregiver chronic conditions) and QOL among patients with advanced cancer and their caregivers, and to assess the mediating and moderating role of meaning-based coping on that relationship. Figure 1 depicts the model used for this study. The specific hypotheses are as follows:
Figure 1.
Hypothesized Model: Patient and Caregiver Number of Comorbidities/Conditions, Meaning-Based Coping, and Quality of Life
Note: Subscript p refers to patients and subscript c refers to caregivers. The hypotheses relevant to each path in the model have been noted (i.e., H1 refers to Hypotheses 1). H5 also considered the moderating role of one dyad member’s meaning-based coping on the relationship between comorbidities/conditions and QOL of the other (paths not shown). Independent effects (i.e., actor effects) are represented by solid lines. Interdependent effects (i.e., partner effects) are represented by dashed lines. Error covariances are represented by curved double-headed arrows.
-
H1
The number of patient comorbidities and caregiver conditions will be inversely associated with their own QOL and the QOL of their dyadic partner.
-
H2
The number of patient comorbidities and caregiver conditions will be inversely associated with their own meaning-based coping and the meaning-based coping of their dyadic partner.
-
H3
Meaning-based coping will be directly associated with (a) patients’ and caregivers’ own QOL and (b) the QOL of the dyadic partner.
-
H4
Meaning-based coping will mediate the relationship between comorbidities/conditions and QOL for each dyad member.
-
H5
Meaning-based coping will moderate the relationship between comorbidities/conditions and QOL for each dyad member.
Method
Participants
Data came from a randomized clinical trial (RCT) that tested the efficacy of brief and extensive versions an evidence-based program on outcomes for patients with advanced cancer and their caregivers compared to usual care [24]. Institutional Review Board approval was obtained from the patient’s cancer center and the University of Michigan (coordinating site). The current analysis used baseline data. The RCT included 484 patients with advanced cancer and their family caregivers (N=484 dyads). Eligible patients had a new diagnosis of advanced breast, colon, lung or prostate cancer during the previous six months or progression of advanced disease during that timeframe. Advanced cancers were defined as cancers at stage III or IV of disease and a limited five-year survival rate (below 50%). Patients also had to have a life expectancy of at least six months (physician assessed), be at least 21 years old, and live within 75 miles a participating cancer center. Family caregivers had to be at least 18 years old and identified by the patient as his/her primary source of emotional or physical support. Caregivers were excluded if they had been diagnosed with cancer during the previous year or were in active treatment for cancer. Data were collected in the home while a research staff member, who was blinded to the RCT group assignments of dyads, was present. Patients and caregivers completed their self-administered questionnaires separately, without consulting with each other.
Measures
Comorbidities/conditions
Patients and caregivers responded to the following question: “Do you have any other health problems (such as heart disease, arthritis, diabetes, etc.) at this time?” Respondents who answered “yes” then named their health problems. The number of comorbidities/conditions variable was based on a count of the number of problems reported. The maximum number reported at baseline was five (no limit was imposed). Comorbidities refer to the health problems reported by patients (cancer as the index condition); conditions refer to the health problems reported by caregivers.
Meaning-based coping
Meaning-based coping was assessed with four items from the benefit dimension of the Appraisal of Illness Scale (patients; α = .75) and the Appraisal of Caregiving Scale (caregivers; α = .70) [25–27]. An example item from this scale is “I’ve grown a lot since this situation began.” This measure uses a 5-point Likert scale that ranges from 1 (strongly disagree) to 5 (strongly agree). Latent variables measuring patient and caregiver meaning-based coping were included.
Quality of life
Patient QOL was measured with the Functional Assessment of Cancer Therapy: General Scale (FACT-G version 4; α = .89) [28]. Caregivers answered a modified version of this scale measuring their own QOL (adapted with permission of FACIT.org; α = .90) [24]. The scales assess physical, social, emotional, and functional QOL. This measure uses a 5-point Likert scale that ranges from 0 (not at all) to 4 (very much). Scoring followed established instructions with higher overall scores indicating better QOL.
Covariates
Age, sex, race, income, cancer type, patient treatment, patient-caregiver relationship type and length of time since patient diagnosis were obtained. Standard measures were used to capture these concepts. Caregiver burden was assessed to account for subjective between-dyad variations in caregiving demands. It was measured using a summary score from two subscales (disrupted schedule and lack of family support; 10 items) of the Caregiver Reaction Assessment (α = .86) [29], and six items added by study researchers assessing caregiver self-care (daily exhaustion; level of demand; time for self; finishing tasks; time for enjoyable activities; self-care guilt). This measure uses a 5-point Likert scale that ranges from 1 (strongly disagree) to 5 (strongly agree).
Data Analysis Strategy
The hypotheses were examined using the actor-partner interdependence mediation model or APIMeM [30]. This model consists of three pairs of variables corresponding to each dyad member: predictor variables (comorbidities/conditions); mediator variables (meaning-based coping); and, outcome variables (QOL). The APIMeM captures actor and partner effects between members of a dyad. Bootstrapping and model constraints were used to test indirect effects suggested by the mediation models. An interaction term was added to the standard actor-partner interdependence model (APIM) [31] to test for moderation effects. All models included correlations between predictor variables, and covariances of error terms of the mediator and outcome variables.
Structural equation modeling (SEM) was used to estimate the model parameters using MPlus version 6.1. There was a low percentage of missing data (less than 5%) and use of Little’s MCAR test determined that the data were missing completely at random; thus, maximum likelihood estimation was used. A standardized dataset was created and used to conduct SEM in MPlus because of the inefficiency of standardized solutions for dyadic data provided by path analysis software [32].The chi-square statistic, comparative fit index (CFI), and the root mean squared error of approximation (RMSEA) were used to determine the adequacy of model fit. The indicators of adequate model fit for these indices are a non-significant chi-square statistic or a chi-square to degrees of freedom ratio of less than 2; a CFI above .90; and a RMSEA value of .05 or less [33].
Results
Sample Characteristics
Demographic information obtained from patients and caregivers at baseline is presented in Table 1. The average age of patients was 60.5 years (SD: 11.5; range: 26–95) and of caregivers 56.5 years (SD: 13.4; range: 18–88). A majority of patients (62%) and caregivers (56.8%) were female. Approximately 80% of patients and caregivers were White. A majority of patients (75.6%) and caregivers (82.9) were married or living as married, and 70% of patients and caregivers were in a marital relationship with each other.
Table 1.
Patient and Caregiver Demographic Information
| Patients (N=484) | Caregivers (N=484) | Difference Testsa | |
|---|---|---|---|
| Age in years | |||
| Mean (SD) | 60.5 (11.5) | 56.5 (13.4) | * |
| Range | 26–95 | 18–88 | |
| Sex (%) | |||
| Female | 62.0 | 56.8 | NS |
| Male | 38.0 | 43.1 | |
| Race (%) | |||
| American Indian/Alaskan Native | 0.2 | 0 | NS |
| Asian | 1.0 | 1.2 | |
| Black | 15.3 | 15.9 | |
| Pacific Islander | 0.2 | 0 | |
| White | 79.3 | 79.6 | |
| Multiracial | 3.9 | 2.5 | |
| Highest level of education in years | |||
| Mean (SD) | 14.5 (2.7) | 14.6 (2.8) | NS |
| Marital Status (%) | |||
| Married/Living as married | 75.6 | 82.9 | * |
| Divorced/Separated | 13.2 | 8.1 | |
| Widowed | 6.0 | 2.3 | |
| Never married | 5.2 | 6.8 | |
| Relationship to patient (%; caregiver only) | -- | ||
| Spouse | -- | 70.0 | |
| Daughter | -- | 12.0 | |
| Son | -- | 3.3 | |
| Sister/Brother | -- | 0.2 | |
| Other relative | -- | 5.6 | |
| Friend | -- | 4.3 | |
| Unknown/Coding error | -- | 4.5 | |
| Currently living with patient (caregiver only) | -- | ||
| % Yes | -- | 82.6 | |
Paired sample t-tests, McNemar’s Test, or Wilcoxon Signed-Rank Test.
p<.05;
NS: not significant.
Medical information obtained from patients and caregivers at baseline is presented in Table 2. The types of cancers reported by patients were breast (32.4%), lung (29.1%), colorectal (25.4%), and prostate (13.0%). Most patients were receiving some sort of treatment (89%), a majority of whom were receiving chemotherapy (76.4%). Among patients and caregivers, hypertension and heart disease were the most commonly reported comorbidities/conditions.
Table 2.
Patient and Caregiver Medical Information at Baseline
| % or M (SD) | Difference Testsa | ||
|---|---|---|---|
| Patient cancer type | |||
| Breast | 32.4 | ||
| Lung | 29.1 | ||
| Colorectal | 25.4 | ||
| Prostate | 13.0 | ||
| Patient treatment typeb | |||
| Chemotherapy | 76.4 | ||
| Hormone therapy | 18.3 | ||
| Radiation | 9.2 | ||
| Experimental therapy | 8.5 | ||
| Surgery | 3.2 | ||
| Other treatment/not specified | 6.0 | ||
| Type of comorbidity/condition (yes/no) | |||
| Hypertension | PT | 39.9 | ** |
| CG | 30.0 | ||
| Heart Problems | PT | 30.4 | NS |
| CG | 26.4 | ||
| Depression | PT | 26.2 | NS |
| CG | 21.9 | ||
| Arthritis | PT | 18.0 | NS |
| CG | 16.5 | ||
| Diabetes | PT | 14.0 | * |
| CG | 9.3 | ||
Paired sample t-tests or McNemar’s Test.
Multiple responses for treatment options were possible so percentages are not equal to 100.
p<.05;
p<.001;
NS: not significant.
Table 3 provides the means and standard deviations for comorbidities/conditions, meaning based coping items, and quality of life at baseline. The average number of comorbidities/ conditions reported was 1.82 among patients (SD: 1.44; range 0–5) and 1.48 among caregivers (SD: 1.35; range 0–5). There were significant differences between the number of patient and caregiver comorbidities/conditions (p<.001). Most patients (77.5%) and caregivers (68.1%) reported at least one comorbidity/condition and almost one-third of patients (32.3%) and one-quarter of caregivers (23%) reported three or more comorbidities/conditions. There were also significant differences in their responses on two of the four items that comprised the meaning based coping latent variable (changes in relationships with others; inner strengths/resources). There were no significant differences in quality of life at baseline.
Table 3.
Study Variables and Values at Baseline
| Items | Patient Mean (SD) | Caregiver Mean (SD) | Difference Testsa |
|---|---|---|---|
| Number of comorbidities/conditions | 1.82 (1.44) | 1.48 (1.35) | ** |
| Meaning-based coping (latent variable with 4 items)b | |||
| I’ve grown a lot since this …situation began (PT) / most recent situation began (CG) | 3.58 (1.08) | 3.61 (.887) | NS |
| Each day has become more meaningful since this…situation started (PT) / most recent situation started (CG) | 3.79 (1.04) | 3.77 (.928) | NS |
| My relationships with others have become […] since this situation began…closer and more meaningful (PT) / more meaningful (CG) | 3.89 (.897) | 3.57 (.954) | ** |
| I’ve discovered […] I never knew I had…inner strengths (PT)/resources (CG) | 3.63 (.897) | 3.21 (.980) | ** |
| Quality of life ( FACT-G summary score)c | 75.73 (16.71) | 76.49 (15.81) | NS |
Paired sample t-tests;
p<.001;
NS: not significant.
Patients (PT) completed the Appraisal of Illness Scale (range: 1–5); Caregivers (CG) completed the Appraisal of Caregiving Scale (range: 1–5)
Patient range: 16.5 – 108; Caregiver range: 20.5 – 108
Hypotheses 1–4: Mediation Model
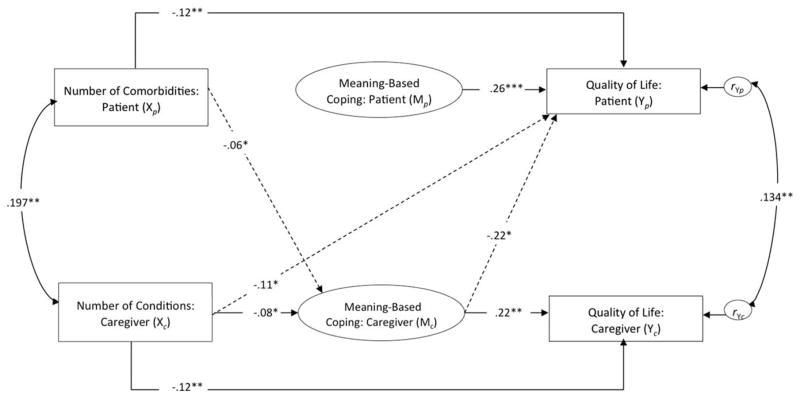
Figure 2 provides the standardized estimates for the mediation model tested. The model included the number of comorbidities/conditions (X); meaning-based coping as a mediator (M); and, QOL as an outcome (Y).
Figure 2.
Mediation Model Results – Hypotheses 1 – 3
Note: Estimates are standardized; only significant parameter estimates are reported. Independent effects (actor effects) are represented by solid lines. Interdependent effects (partner effects) are represented by dashed lines. Error covariances are represented by curved double-headed arrows. X= predictor variable; M=mediator variable; Y=outcome variable. Subscript p refers to patients and subscript c refers to caregivers. Model covariates included age, sex, race, income, cancer type, patient treatment, relationship type, length of time since patient diagnosis and caregiver burden. Model fit: X2/df=1.625; CFI=.93, RMSEA=.04. +p < .10; *p < .05; **p<.01
H1: Influence of Comorbidities/Conditions on QOL (X→Y)
Supporting the study hypothesis, more comorbidities in patients (β=−0.12; p=0.005) were associated with lower patient QOL. Similarly, more caregiver conditions were associated with lower caregiver QOL (β=−0.12; p=.003). In addition, more conditions among caregivers was associated with lower QOL among patients (β=−0.11; p=0.02).
H2: Influence of Comorbidities/Conditions on Meaning-Based Coping (X→M)
Patient number of comorbidities were not associated with patient meaning-based coping; however, among caregivers, having more conditions was associated with lower meaning-based coping (β=−0.08; p=0.02). In addition, more patient comorbidities were associated with lower meaning-based coping among caregivers (β=−0.06; p=0.04).
H3: Influence of Meaning-Based Coping on QOL (M→Y)
As expected, significant effects were found when examing the direct relationship between meaning-based coping and QOL. More meaning-based coping in patients was associated with higher patient QOL (β=0.26; p<.001). Similarly, more caregiver meaning-based coping was associated with higher caregiver QOL (β=0.22; p=.006). In addition, more caregiver meaning-based coping was associated with lower patient QOL (β=−0.22; p=.019).
H4: Meaning-Based Coping as a Mediator (X→M→Y)
The results from testing H1–H3 indicated that caregiver meaning-based coping might mediate the relationship between: (a) caregiver number of chronic conditions and caregiver QOL; (b) caregiver number of comorbidities and patient QOL; (c) patient number of chronic conditions and patient QOL; and, (d) patient number of chronic conditions and caregiver QOL.
Bootstrapping confirmed three significant mediation effects (a, b and d). First, there was a significant indirect effect (β=−0.02; 95% CI: −0.054, −0.002) of caregiver number of comorbidities on caregiver QOL, mediated by caregiver meaning-based coping (a). Given the evidence of a direct effect between caregiver conditions and caregiver QOL, these results confirm partial mediation. Second, there was a significant indirect effect (β=0.02; 95% CI: .001, .048) of caregiver number of comorbidities on patient QOL, mediated by caregiver meaning-based coping (b). Given the evidence of a direct effect between caregiver conditions and patient QOL, these results also confirm partial mediation. Lastly, there was a significant indirect effect (β=−0.01; 95% CI: −0.046, −0.001) of patient number of comorbidities on caregiver QOL, mediated by caregiver meaning-based coping (d). As there was no observed direct effect between patient number of condtions and caregiver QOL, these results (d) suggest a full mediation effect.
Hypothesis 5: Meaning-Based Coping as a Moderator
Meaning-based coping was also tested as a possible moderator of the relationship between comorbidities and QOL. The interaction terms were a added to a model that included main actor and partner effects between comorbidities/conditions and QOL and between meaning-based coping and QOL. None of the interaction terms were significant.
Conclusions
This study examined the relationship between co-existing health problems and quality of life among patients with advanced cancer and their caregivers, while investigating the mediating and moderating role of meaning-based coping on that relationship. Of particular interest was the influence of one individual’s health problems on their own health outcomes (i.e., actor effects) and the other person’s health outcomes (i.e., partner effects). Findings suggest that as the number of patient comorbidities and caregiver conditions increased, their own QOL decreased. In addition, as caregivers’ number of conditions increased, QOL reported by patients worsened. Although cancer and non-cancer related studies have found a relationship between patient number of chronic conditions and QOL [4, 6, 12], this research has focused on the effect of an individuals’ comorbidities on their own outcomes and has not focused primarily on the advanced cancer context. Findings from this study extend that research and indicate within the patient/caregiver dyad, the comorbidities/conditions of one member of the dyad have the potential to directly or indirectly affect the wellbeing of the other.
Associations were also found between the number of comorbidities/conditions among both dyad members and caregiver meaning-based coping. More comorbidities/conditions among patients and caregivers were associated with lower meaning-based coping among caregivers but not patients. Our findings lend support to previous studies showing that caregivers exhibit significant levels of psychological distress, especially as the patient’s disease progresses [34]. Because caregivers likely bear the responsibility for managing their own health problems, as well as the responsibility and burden of managing the patient’s health problems, the negative impact of comorbidities/conditions on caregivers’ ability to find meaning might be stronger. On the other hand, it is interesting to note that neither patient comorbidities nor caregiver conditions influenced patient meaning-based coping. The significance of advanced disease, a higher likelihood that the primary cause of patient mortality would be cancer and not co-existing conditions [5], could help explain why other patient/caregiver health problems posed no additional influence on patient meaning-based coping.
Meaning-based coping was found to mediate, but not moderate, the relationship between comorbidities/conditions and QOL. Specifically, only caregiver meaning-based coping helped to explain the negative relationship between patient comorbidities and caregiver conditions, as well as, patient and caregiver QOL. Previous research has identified caregivers as a primary source of emotional support for patients [35, 36]. As such, caregivers may play a significant role in setting the emotional tenor in the care-giving and care-receiving experience, helping to patients to reframe or find positive meaning in the illness. Hence, caregiver meaning-based coping emerged as an important pathway in the relationship between comorbidities/conditions and QOL.
Unexpectedly, increased meaning-based coping among caregivers was associated with decreased QOL among patients. A possible contributor to this finding could be the use of baseline data. While the diagnosis of advanced disease requires psychological adjustment on the part of both patients and caregivers, the time it takes to make that adjustment could differ. A previous study of posttraumatic growth in patients with advanced liver cancer found that, for all but one of the dimensions assessed, patient’s posttraumatic growth was unchanged for the first six months following diagnosis [37]. The caregivers’ ability to find growth and benefit, prior to the other partner being able to do so, could be a source of concern for the patient. In their discussion of meaning-making among individuals with advanced cancer, Lethborg and colleagues [19] describes this process for patients as “dynamic”, “bittersweet”, and “taxing.” Challenges to the psychosocial health of individuals with a terminal illness cannot be understated. Patients may need more time than caregivers to make sense of their advanced disease and end-of life issues, adapt to the challenges they will face in the present and future, and identify areas of benefit and growth. It could also be the case that caregivers can more readily find tangible, meaningful ways that their lives have changed because of the cancer diagnosis because of their role in patient care and support. It will be important to examine this unexpected finding in future research.
Limitations
The study collected data about the number and type of comorbidities/conditions of patients and caregivers using a self-report measure. While evidence supports the use of a self-report measure to “count” chronic diseases [38], data was not available on condition severity, time since diagnosis of the comorbidity/condition, or disease management. Those with greater symptom severity , more recently diagnosed conditions, and those less able to manage their chronic diseases may have more challenges that could negatively influence their meaning-based coping and QOL. In addition, the use of an open-ended question to collect data on comorbidities/conditions instead of a checklist could have resulted in underreporting of these health problems; however, previous research supports the use of self-report when examining psychosocial outcomes [39]. Another limitation was that due the sample size and racial distribution in this study, testing differences between racial groups was not feasible. Research indicates that chronic diseases are a major contributor to poorer health outcomes among minority populations, such as African Americans [40]. Testing differences between racial groups could help identify areas of risk and need. The study was also limited by the cross-sectional nature of the analysis, which precludes a determination of causality. Lastly, while significant, the indirect effects are small; however, it is important to note these estimates control for the influence of a number of patient and caregiver factors.
Implications
A unique contribution of this study is the consideration of how patient comorbidities and caregiver chronic conditions influenced their QOL in the advanced cancer context. At advanced stages of disease, where curative treatment is no longer the goal, supporting and maintaining patient QOL becomes the most important goal. Thus, while advanced cancer may contribute more to patient mortality than their comorbidities, study results suggest that efforts to improve patient QOL should not ignore patient comorbid conditions – or the chronic conditions of their caregivers.
This study takes an important first step in identifying that in this sample of patient/caregiver dyads facing advanced cancer, a significant relationship was observed between comorbidities/conditions, caregiver meaning-based coping, and patient/caregiver quality of life. An important next step is to confirm this finding in other, similar samples as well as to understand how this occurs. Future qualitative research should explore the mechanisms by which the number of comorbidities/conditions, as well as the ability of patients and caregivers to manage those conditions, influences their health outcomes. Elucidating these mechanisms would identify important intervention targets. For example, in the practice setting, it may be useful to help patients and caregivers in skill-building and resource-finding that will help them manage their conditions individually, as a unit, and as often the case with multimorbidity, with multiple medical providers. Additional resources for caregiver assessment at the patient’s care settings may be necessary for this to occur. Tailoring existing cancer-related interventions and chronic disease management programs could be beneficial for patient/caregiver dyads managing advanced cancer and other illnesses.
Acknowledgments
The preparation of this manuscript by the first author was supported by Rackham Graduate School at the University of Michigan, and the Cancer Health Disparities Training Program (2T32CA128582-06) and Center for Health Equity Research at the University of North Carolina. Data come from a study funded by a grant from the National Cancer Institute (RO1CA107383, L. Northouse).
References
- 1.Rodriguez AM, Mayo NE, Gagnon B. Independent contributors to overall quality of life in people with advanced cancer. British Journal of Cancer. 2013;108:1790–1800. doi: 10.1038/bjc.2013.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim Y, Given BA. Quality of life of family caregivers of cancer survivors: Across the trajectory of the illness. Cancer. 2008;112:2556–2568. doi: 10.1002/cncr.23449. [DOI] [PubMed] [Google Scholar]
- 3.Ogle KS, Swanson GM, Woods N, Azzouz F. Cancer and comorbidity: Redefining chronic diseases. Cancer. 2000;88:653–663. doi: 10.1002/(SICI)1097-0142(20000201)88:3<653::AID-CNCR24>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 4.Smith AW, Reeve BB, Bellizzi KM, Harlan LC, Klabunde CN, Amsellem M, Bierman AS, Hays RD. Cancer, comorbidities, and health-related quality of life of older adults. Health Care Financing Review. 2008;29:41–56. [PMC free article] [PubMed] [Google Scholar]
- 5.Edwards BK, Noone AM, Mariotto AB, Simard EP, Boscoe FP, Henley SJ, Jemal A, Cho H, Anderson RN, Kohler BA, Eheman CR, Ward EM. Annual Report to the Nation on the status of cancer, 1975–2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer. 2014;120:1290–1314. doi: 10.1002/cncr.28509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caravati-Jouvenceaux A, Launoy G, Klein D, Henry-Amar M, Abeilard E, Danzon A, Pozet A, Velten M, Mercier M. Health-related quality of life among long-term survivors of colorectal cancer: a population-based study. The Oncologist. 2011;16:1626–1636. doi: 10.1634/theoncologist.2011-0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rowland JH, Yancik R. Cancer survivorship: The interface of aging, comorbidity, and quality care. Journal of the National Cancer Institute. 2006;98:504–505. doi: 10.1093/jnci/djj154. [DOI] [PubMed] [Google Scholar]
- 8.Romito F, Goldzweig G, Cormio C, Hagedoorn M, Andersen BL. Informal caregiving for cancer patients. Cancer. 2013;119:2160–2169. doi: 10.1002/cncr.28057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wadhwa D, Burman D, Swami N, Rodin G, Lo C, Zimmermann C. Quality of life and mental health in caregivers of outpatients with advanced cancer. Psycho-Oncology. 2013;22:403–410. doi: 10.1002/pon.2104. [DOI] [PubMed] [Google Scholar]
- 10.Van Lange PAM, Rusbult CE. Interdependence Theory. In: Van Lange PAM, Kruglanski AW, Higgins ET, editors. Handbook of Theories in Social Psychology. SAGE; Los Angeles: 2012. pp. 251–272. [Google Scholar]
- 11.Mao JJ, Armstrong K, Bowman MA, Xie SX, Kadakia R, Farrar JT. Symptom burden among cancer survivors: Impact of age and comorbidity. Journal of the American Board of Family Medicine. 2007;20:434–443. doi: 10.3122/jabfm.2007.05.060225. [DOI] [PubMed] [Google Scholar]
- 12.Fortin M, Lapointe L, Hudon C, Vanasse A, Ntetu AL, Maltais D. Multimorbidity and quality of life in primary care: A systematic review. Health and Quality of Life Outcomes. 2004;2 doi: 10.1186/1477-7525-2-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vogeli C, Shields AE, Lee TA, Gibson TB, Marder WD, Weiss KB, Blumenthal D. Multiple chronic conditions: prevalence, health consequences, and implications for quality, care management, and costs. Journal of General Internal Medicine. 2007;22:391–395. doi: 10.1007/s11606-007-0322-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burton LC, Newsom JT, Schulz R, Hirsch CH, German PS. Preventive Health Behaviors among Spousal Caregivers. Preventive Medicine. 1997;26:162–169. doi: 10.1006/pmed.1996.0129. [DOI] [PubMed] [Google Scholar]
- 15.Thomas C, Morris SM, Harman JC. Companions through cancer: the care given by informal carers in cancer contexts. Social Science & Medicine. 2002;54:529–544. doi: 10.1016/S0277-9536(01)00048-X. [DOI] [PubMed] [Google Scholar]
- 16.Kim Y, Schulz R. Family caregivers' strains: Comparative analysis of cancer caregiving with dementia, diabetes, and frail elderly caregiving. Journal of Aging and Health. 2008;20:483–503. doi: 10.1177/0898264308317533. [DOI] [PubMed] [Google Scholar]
- 17.Wenzel L, Glanz K, Lerman C. Stress, coping and health behavior. In: Glanz K, Rimer BK, Lewis FM, editors. Health Behavior and Health Education. Jossey-Bass; San Francisco: 2002. pp. 210–239. [Google Scholar]
- 18.Mellon SL, Northouse LL, Weiss LK. A population-based study of the quality of life of cancer survivors and their family caregivers. Cancer Nursing. 2006;29:120–133. doi: 10.1097/00002820-200603000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Lethborg C, Aranda S, Bloch S, Kissane D. The role of meaning in advanced cancer - integrating the constructs of assumptive world, sense of coherence and meaning-based coping. Journal of Psychosocial Oncology. 2006;24:27–42. doi: 10.1300/J077v24n01_03. [DOI] [PubMed] [Google Scholar]
- 20.Franks HM, Roesch SC. Appraisals and coping in people living with cancer: a meta-analysis. Psycho-Oncology. 2006;15:1027–1037. doi: 10.1002/pon.1043. [DOI] [PubMed] [Google Scholar]
- 21.Cohen CA, Colantonio A, Vernich L. Positive aspects of caregiving: Rounding out the caregiver experience. International Journal of Geriatric Psychiatry. 2002;17:184–188. doi: 10.1002/gps.561. [DOI] [PubMed] [Google Scholar]
- 22.Kim Y, Baker F, Spillers RL. Cancer caregivers' quality of life: Effects of gender, relationship, and appraisal. Journal of Pain and Symptom Management. 2007;34:294–304. doi: 10.1016/j.jpainsymman.2006.11.012. http://dx.doi.org/10.1016/j.jpainsymman.2006.11.012. [DOI] [PubMed] [Google Scholar]
- 23.Kramer BJ. Gain in the caregiving experience: Where are we? What next? The Gerontologist. 1997;37:218–232. doi: 10.1093/geront/37.2.218. [DOI] [PubMed] [Google Scholar]
- 24.Northouse LL, Mood DW, Schafenacker A, Kalemkerian G, Zalupski M, LoRusso P, Hayes DF, Hussain M, Ruckdeschel J, Mark Frendrick A, Trask PC, Ronis DL, Kershaw T. Randomized clinical trial of a brief and extensive dyadic intervention for advanced cancer patients and their family caregivers. Psycho-Oncology. 2013;22:555–563. doi: 10.1002/pon.3036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oberst M. Appraisal of Illness Scale (AIS-Revised): Manual for Use. Wayne State University; Detroit, MI: 1991. [Google Scholar]
- 26.Oberst M. Appraisal of Caregiving Scale (ACS-Revised): Manual for Use. Wayne State University; Detroit, MI: 1991. [Google Scholar]
- 27.Lambert SD, Yoon H, Ellis KR, Northouse LL. Measuring appraisal during advanced cancer: Psychometric testing of the appraisal of caregiving scale. Patient Education and Counseling. 2015;98:633–639. doi: 10.1016/j.pec.2015.01.0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, Silberman M, Yellen SB, Winicour P, Brannon J. The Functional Assessment of Cancer Therapy scale: Development and validation of the general measure. Journal of Clinical Oncology. 1993;11:570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 29.Given CW, Given B, Stommel M, Collins C, King S, Franklin S. The caregiver reaction assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Research in Nursing & Health. 1992;15:271–283. doi: 10.1002/nur.4770150406. [DOI] [PubMed] [Google Scholar]
- 30.Ledermann TS, Macho S, Kenny DA. Assessing mediation in dyadic data using the actor-partner interdependence model. Structural Equation Modeling: A Multidisciplinary Journal. 2011;18:595–612. doi: 10.1080/10705511.2011.607099. [DOI] [Google Scholar]
- 31.Garcia RL, Kenny DA, Ledermann T. Moderation in the actor–partner interdependence model. Personal Relationships. 2015;22:8–29. doi: 10.1111/pere.12060. [DOI] [Google Scholar]
- 32.Kenny DA, Kashy DA, Cook WL. Dyadic Data Analysis. Guilford Press; New York: 2006. [Google Scholar]
- 33.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- 34.Pitceathly C, Maguire P. The psychological impact of cancer on patients’ partners and other key relatives: a review. European Journal of Cancer. 2003;39:1517–1524. doi: 10.1016/s0959-8049(03)00309-5. [DOI] [PubMed] [Google Scholar]
- 35.Given BA, Given CW, Kozachik S. Family support in advanced cancer. CA: A Cancer Journal for Clinicians. 2001;51:213–231. doi: 10.3322/canjclin.51.4.213. [DOI] [PubMed] [Google Scholar]
- 36.Stenberg U, Ruland CM, Miaskowski C. Review of the literature on the effects of caring for a patient with cancer. Psycho-Oncology. 2010;19:1013–1025. doi: 10.1002/pon.1670. [DOI] [PubMed] [Google Scholar]
- 37.Moore AM, Gamblin TC, Geller DA, Youssef MN, Hoffman KE, Gemmell L, Likumahuwa SM, Bovbjerb DH, Marsland A, Steel JL. A prospective study of posttraumatic growth as assessed by self-report and family caregiver in the context of advanced cancer. Psycho-Oncology. 2011;20:479–487. doi: 10.1002/pon.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bayliss EA, Ellis JL, Steiner JF. Subjective assessments of comorbidity correlate with quality of life health outcomes: Initial validation of a comorbidity assessment instrument. Health and Quality of Life Outcomes. 2005;3:1–8. doi: 10.1186/1477-7525-3-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gijsen R, Hoeymans N, Schellevis FG, Ruwaard D, Satariano WA, van den Bos GAM. Causes and consequences of comorbidity: A review. Journal of Clinical Epidemiology. 2001;54:661–674. doi: 10.1016/S0895-4356(00)00363-2. [DOI] [PubMed] [Google Scholar]
- 40.Adler NE, Rehkopf DH. U.S disparities in health: Descriptions, causes, and mechanisms. Annual Review of Public Health. 2008;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]