Abstract
Background
While several studies suggest beneficial effects of lower sodium on cardiovascular disease, the relationship with total mortality remains controversial. Some have reported a J-shaped curve, but this may be due to poor quality measurement of sodium or confounding bias.
Objective
To examine the relationship of well-characterized measures of sodium intake, estimated from urinary sodium excretion, with long-term mortality.
Methods
Two trials [Phase I (1987-90) over 18 month and Phase II (1990-5) over 36 months in the Trials of Hypertension Prevention] implemented sodium reduction interventions. Multiple 24-hour urines were collected from pre-hypertensive adults aged 30-54 during these trial periods. Post-trial deaths were ascertained over a median 24 years through December 31, 2013 using the National Death Index. The association of mortality with both the randomized intervention and average sodium intake was examined.
Results
Among 744 Phase I and 2382 Phase II participants randomized to sodium reduction or control, 251 deaths occurred, with a nonsignificant 15% lower risk in the active intervention (hazard ratio (HR)=0.85, 95% CI=0.66-1.09, p=0.19). Among 2,974 participants not assigned to an active sodium intervention, 272 deaths occurred. There was a direct linear association of average sodium intake with mortality, with HR=0.75, 0.95, 1.00 (reference), and 1.07 (p-trend = 0.30) for <2300, 2300-<3600, 3600-<4800, and >=4800 mg/24hr, respectively, with HR=1.12 per 1000 mg/24hr (95% CI = 1.00-1.26, p=0.05) and no evidence of a J-shape or nonlinear relation. The HR per unit increase in sodium/potassium ratio was 1.13 (95% CI = 1.01-1.27, p=0.04).
Conclusions
This study, with carefully characterized measures of sodium intake, found an increased risk at high sodium intake and a direct relation with total mortality even at the lowest levels of sodium intake. Overall, these results are consistent with a benefit of reduced sodium and sodium/potassium on total mortality over a period of over 20 years.
Keywords: sodium, potassium, mortality, nutrition, diet
INTRODUCTION
Numerous randomized trials as well as observational studies have demonstrated a direct relationship between dietary sodium intake and blood pressure.1,2 While the effect is strongest among those with hypertension,3 there is also a smaller but consistent effect of lowering sodium on blood pressure among those with high normal or pre-hypertensive blood pressure levels. The DASH-Sodium trial, a dose-response trial with 3 levels of sodium intake, found a significant direct relationship of sodium intake with blood pressure levels that was evident among both those with and without hypertension.4 A recent Cochrane meta-analysis of data from 35 trials1 found that a 100 mmol reduction in 24-hour urinary sodium led to a reduction in systolic/diastolic blood pressure of 5.4/2. 8 among hypertensive individuals, and of 2.4/1.0 among normotensive individuals.
How well this blood pressure reduction translates into a beneficial effect on incidence of cardiovascular disease, and particularly on total mortality, remains controversial. A report from the Institute of Medicine in 20135 found that there was a link between excessive sodium intake and risk of cardiovascular disease (CVD), particularly for stroke. They also found, however, that the evidence on the effects of sodium intakes below 2,300 mg/24hr was inconsistent and inconclusive. Few studies had available data in this range of sodium and several that did report on outcomes associated with these levels suffered from limitations due to reverse causation, possible confounding and measurement error.6
Since that report, some additional observational studies7,8 and a meta-analysis9 have reported an increase in cardiovascular disease and mortality among those at the lowest levels of sodium intake, suggesting a U-shaped relationship of sodium and health outcomes. In contrast, data from 10 to 15-years of post-trial follow-up in Trials of Hypertension Prevention (TOHP) participants identified a direct linear relation of average sodium excretion with cardiovascular disease down to the lowest levels of intake.10 Unlike other reports, the latter study used a gold-standard assessment of sodium intake, based on the mean of several 24-hour sodium excretions accrued over 1.5-4 years of exposure ascertainment. In the current paper, we report on the relationship between sodium intake and total mortality during more extended follow-up through 2013, for a total of 23-26 years. We include results from analyses based on both exploration of the later effects of the randomized sodium reduction interventions in the TOHP trials as well as the observational relationship between average 24-hour sodium excretion in those who were not randomized to an active sodium intervention.
METHODS
TOHP Trials
The TOHP Follow-up Study is an observational follow-up of Phases I and II of TOHP, and has been described previously.11,12 Phase I of TOHP (TOHP I) took place from September 1987 to January 1990, and evaluated the effects on blood pressure over 18 months of four supplement and three lifestyle interventions, including weight loss and sodium reduction interventions.13 Participants included 2,182 men and women aged 30-54 years with high normal blood pressure. A total of 327 participants were randomized to the active sodium reduction, with 417 included in their usual care comparison group (Supplemental Figure 1).
In Phase II of TOHP (TOHP II), which took place from December 1990 to March 1995, a factorial design was used to assess the effects of sodium reduction and weight loss on blood pressure in 2,382 pre-hypertensive men and women age 30-54 years who were followed carefully for 3-4 years.14 Eligible participants in TOHP II had a body mass index (BMI [calculated as weight in kilograms divided by height in meters squared]) representing 110% to 165% of desirable body weight. All 1,191 participants in an active sodium reduction intervention and 1,191 in a sodium control group were included in these analyses (Supplemental Figure 1).
Usual Intake of Sodium
During the trial periods, three to seven 24-hour urine collections were scheduled during 18 months of follow-up in TOHP I and three to four years in TOHP II. Usual intake of sodium or potassium or their ratio was calculated as the mean of available urinary excretion measures at 5 (lifestyle interventions) or 7 (nutritional supplement interventions) scheduled collections in TOHP I and at 3 to 5 scheduled collections during TOHP II. Mean sodium and potassium excretions, representing usual intake, were computed over all collections. All of the urinary sodium and potassium measures were expressed as mg/24hr.15 Additional description of these measures, including creatinine and coefficients of variation have previously been reported.10
Those who were randomized to an active sodium reduction were excluded from the observational analyses of usual intake because their 24-hour urine collections would provide a biased estimate of usual sodium intake due to short-term fluctuations during the active intervention. Of 2182 participants in TOHP I, 327 were excluded and of 2,382 participants in TOHP II, 1,191 were excluded for this reason. An additional 8 participants in TOHP I and 7 in TOHP II were excluded due to missing sodium excretion. Finally, 3 participants in TOHP I and 17 in TOHP II were excluded due to the occurrence of an incident CVD event or death during the period of exposure assessment (Supplemental Figure 2). Thus, 1,844 participants in TOHP I and 1,167 participants in TOHP II were included in this observational analysis. Of these, 37 participated in both TOHP I and II, leaving 2,974 unique individuals in the follow-up. For the 37 individuals participating in both phases, follow-up to the beginning of TOHP II contributed to TOHP I person-time, and that from TOHP II on contributed to TOHP II person-time.
Mortality Follow-up
Previously, we conducted a mail-based follow-up of all TOHP participants for cardiovascular disease endpoints through early 2005, with a search of the National Death Index (NDI) through December 2003.11,12 We conducted additional searches of the NDI in 2014 and 2015, accruing death information through December 2013. In the analysis of the randomized sodium intervention, all-cause mortality from the time of randomization through 2013 was included in an intention-to-treat analysis. Observational analyses of usual sodium intake included sodium assessed throughout the trial periods as the exposure and examined mortality following the trial periods through 2013.
Statistical Analysis
Analysis of the randomized sodium reduction intervention was based on the intention-to-treat principle. Comparisons of baseline trial characteristics by randomized intervention have previously been conducted.11,13,14 The hazard ratio (HR) for the effect of the randomized sodium intervention on all-cause mortality was estimated using a Cox regression analysis, stratified by trial phase with common predictor effects. Analyses were adjusted for clinic, age, race, and sex, and for the weight loss intervention in TOHP II. Cumulative incidence curves, adjusted for clinic, age, and sex, were estimated and plotted for each trial separately. We also estimated the cumulative HRs over time in five-year periods, and before and after 10 years of follow-up.
In observational analyses of usual intake, sodium excretion levels from three to seven 24-hour urine collections obtained during the course of the trial periods were averaged. Those not in an active sodium intervention who remained alive and CVD-free at the end of the trial periods were included in these analyses. Absolute levels of 24-hour urinary sodium excretion were grouped into categories of <2300, 2300 to <3600, 3600 to <4800, and 4800 mg or higher. Baseline characteristics by gender were expressed as percents or means, and were tested for trend over sodium categories using chi-square statistics or regression analysis.
Cox regression analysis was used to estimate the association of mortality with the absolute sodium level in a continuous fashion as well as after grouping into the previously mentioned categories. Models were adjusted for clinic, age, sex, race/ethnicity, and other treatment assignments (model 1), and additionally for education, baseline weight, alcohol use and amount, smoking, exercise, potassium excretion, and family history of cardiovascular disease (model 2). Interactions with time, gender, age, race, and the weight loss intervention in TOHP II were examined. Penalized splines with four degrees of freedom were used to examine linearity of effect. All analyses were conducted in SAS 9.2 except for the cumulative incidence plots and spline analyses which were conducted in R using the coxph function.
RESULTS
Analyses Based on Randomized Assignment
Detailed comparison of the randomized groups have been reported.11 Among the 744 participants in TOHP I who were randomized to the sodium reduction intervention or control, the average age was 43 years, 71% were male and 20% were black. Average weight was 191 pounds in men and 160 pounds in women, and average sodium excretion at baseline was 167 mmol/24hr (3839 mg/24hr) in men and 128 mmol/24hr (2948 mg/24hr) in women. Among the 2382 participants in TOHP II, the average age was 44 years, 66% were male and 18% were black. Because everyone was eligible for a weight loss intervention in TOHP II, weight was higher, with an average of 218 pounds in men and 184 pounds in women. Average sodium excretion at baseline was 199 mmol/24hr (4576 mg/24hr) in men and 154 mmol/24hr (3541 mg/24hr) in women. Baseline characteristics were evenly divided by randomized intervention, except that age was slightly higher in the sodium intervention group in both Phases I and II.11
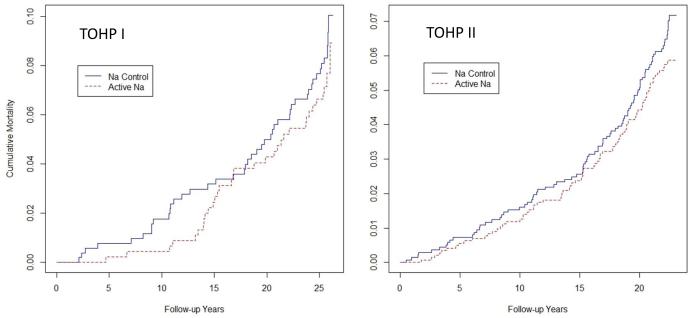
A total of 77 and 174 deaths occurred in the TOHP I and TOHP II participants, respectively, during the extended follow-up through 2013. Median follow-up time since randomization among survivors was 25.7 years for TOHP I and 22.4 years for TOHP II. Crude rates were slightly lower in the intervention groups (Table 1). In Cox models adjusting for clinic and basic demographic factors, the HR for mortality by randomized intervention group was 0.85 (95% confidence interval (CI) =0.66-1.09, p=0.19). Cumulative mortality curves showed a consistently lower incidence among those in the active group (Figure 1). Results were virtually identical in Phases I and II, as well as after further adjustment for baseline urinary sodium and body weight. When the cumulative HRs were examined over time (Supplemental Figure 3), the difference between randomized groups appeared largest at 10 years (HR=0.60, 95%CI = 0.34-1.06, p=0.08), followed by attenuation to the null by the end of follow-up after 23-26 years. Tests of interaction with time were not significant, however.
Table 1.
Total mortality from randomization in the Trials of Hypertension Prevention through 2013 by sodium intervention group.
|
Randomized Intervention
|
|||
|---|---|---|---|
| Sodium Reduction | Usual Care | ||
| A. Deaths/ Total (%) | |||
| TOHP I | 33/327 (10.1) | 44/417 (10.6) | |
| TOHP II | 82/1191 (6.9) | 92/1191 (7.7) | |
| B. Hazard Ratios* | HR | 95% CI | p |
| Model 1 | |||
| TOHP I | 0.84 | 0.54-1.32 | 0.46 |
| TOHP II | 0.85 | 0.63-1.14 | 0.28 |
| Combined | 0.85 | 0.66-1.09 | 0.19 |
| Model 2 | |||
| TOHP I | 0.86 | 0.54-1.37 | 0.52 |
| TOHP II | 0.85 | 0.63-1.15 | 0.30 |
| Combined | 0.85 | 0.66-1.10 | 0.21 |
From Cox regression analysis stratified by trial and adjusted for clinic, age, race, sex, and weight loss intervention (Model 1); plus baseline weight and sodium (Model 2).
HR = hazard ratio; CI = confidence interval.
Figure 1.
Cumulative total mortality by randomized sodium intervention group in TOHP I (left) and TOHP II (right). Each shows a lower but non-significant reduction in mortality in the active sodium reduction group (see Table 1).
Observational Analyses Based on Urinary Sodium Excretion
There were 1844 participants in TOHP I and 1167 in TOHP II who had not been randomized to a sodium reduction intervention, with 37 participating in both phases. Of these, 68% were men, 16% were black and the average age was 43 years. Average weight at baseline was 194 pounds in men and 164 pounds in women in phase I and 218 pounds in men and 184 pounds in women in TOHP II. During the trial periods, 3-7 24-hour urine excretions were scheduled, and 1-7 were collected from these individuals. The average number of excretions collected was 4.4 in TOHP I and 3.5 in TOHP II. The overall average sodium excretion during the trial period was 164 mmol/24hr (3766 mg/24hr). The average was 167 mmol/24hr (3847 mg/24hr) in men and 131 mmol/24hr (3003 mg/24hr) in women in TOHP I, and 190 mmol/24hr (4378 mg/24hr) in men and 147 mmol/24hr (3386 mg/24hr) in women in TOHP II.
Baseline characteristics by average level of urinary sodium and gender during the trials are presented in Table 2. Many of those at a higher level of urinary sodium excretion were participants in Phase II of TOHP. Those with lower sodium levels were more likely to have a college education, drink alcohol, exercise, and be of lower weight, especially among men. They also tended to have a lower level of systolic and diastolic blood pressure. No association was found with smoking or race. Measures of urinary sodium and potassium were highly correlated, with an overall r=0.49 and significant trends across levels of sodium in both men and women. During the post-trial follow-up 272 deaths occurred, with 189 among TOHP I participants and 83 among TOHP II participants (Table 3). Median follow-up time following the trial periods among survivors was 23.9 years for TOHP I and 18.8 years for TOHP II. In Cox regression models stratified by phase and adjusted for demographic variables, the HR increased over categories of urinary sodium excretion, but the trend did not reach statistical significance. Compared to the reference category of 3600-<4800 mg/24hr, the HRs were 0.74 for those with <2300 mg/24hr, 0.90 for those with 2300-<3600 mg/24hr, and 1.13 for those with ≥ 4800 mg/24hr (p for trend = 0.092). After further adjustment for baseline variables, these were 0.75, 0.95, and 1.07 (p-trend = 0.30) over <2300, 2300-<3600 and >=4800 mg/24hr, respectively. In a corresponding comparison of the lowest (<2300 mg/24hr) to the highest (>=4800 mg/24hr) sodium groups, the HR was 0.70 (95%CI = 0.39-1.27).
Table 2.
Baseline characteristics among participants with follow-up information in the Trials of Hypertension Prevention cohorts by categories of sodium, stratified by sex.
| Sodium Excretion (mg/24hr) |
P for Trend | ||||
|---|---|---|---|---|---|
| <2300 | 2300-<3600 | 3600-<4800 | >=4800 | ||
| MEN | |||||
| N | 131 | 679 | 771 | 478 | |
| Phase II (%) | 16.8 | 28.3 | 39.6 | 52.3 | <0.0001 |
| Age (yrs) | 42.5 | 42.7 | 42.9 | 42.3 | 0.49 |
| Black (%) | 16.0 | 9.7 | 10.4 | 8.8 | 0.11 |
| College (%) | 82.4 | 69.7 | 66.8 | 63.8 | 0.0002 |
| Current smoker (%) | 14.5 | 9.9 | 9.9 | 9.6 | 0.31 |
| Past smoker (%) | 30.5 | 35.6 | 39.0 | 40.0 | 0.026 |
| Alcohol (% drinker) | 62.6 | 51.8 | 48.0 | 41.6 | <0.0001 |
| Alcohol (drinks/wk among drinkers) |
7.7 | 7.8 | 7.2 | 6.7 | 0.018 |
| Exercise (% ≥once/wk) | 77.8 | 74.5 | 69.8 | 67.5 | 0.0018 |
| Weight (lbs) | 181.3 | 192.1 | 204.9 | 221.6 | <0.0001 |
| SBP | 124.9 | 125.2 | 125.7 | 126.4 | 0.0039 |
| DBP | 84.3 | 84.4 | 84.8 | 85.0 | <0.0001 |
| # Excretions | 4.1 | 4.3 | 4.2 | 3.9 | 0.0014 |
| Sodium (mmol/24hr) | 83.9 | 133.2 | 180.7 | 253.9 | - |
| Potassium (mmol/24hr) | 50.3 | 59.7 | 67.6 | 76.0 | <0.0001 |
| Sodium/Potassium Excretion Ratio |
1.95 | 2.52 | 2.94 | 3.65 | <0.0001 |
| WOMEN | |||||
| N | 181 | 503 | 208 | 60 | |
| Phase II (%) | 24.3 | 42.7 | 51.9 | 51.7 | <0.0001 |
| Age (yrs) | 44.3 | 43.9 | 43.0 | 43.2 | 0.031 |
| Black (%) | 25.4 | 28.2 | 26.9 | 26.7 | 0.87 |
| College (%) | 47.5 | 44.9 | 41.8 | 40.0 | 0.18 |
| Current smoker (%) | 16.6 | 10.5 | 12.5 | 13.3 | 0.45 |
| Past smoker (%) | 27.6 | 26.6 | 22.1 | 25.0 | 0.27 |
| Alcohol (% drinker) | 35.4 | 24.9 | 22.1 | 33.3 | 0.11 |
| Alcohol (drinks/wk among drinkers) |
5.6 | 5.5 | 4.5 | 3.5 | 0.025 |
| Exercise (% ≥once/wk) | 62.6 | 59.3 | 60.6 | 56.7 | 0.54 |
| Weight (lbs) | 156.3 | 172.2 | 182.2 | 191.7 | <0.0001 |
| SBP | 126.2 | 126.5 | 126.8 | 126.4 | 0.63 |
| DBP | 84.2 | 84.6 | 85.0 | 85.0 | 0.0037 |
| # Excretions | 3.9 | 4.1 | 3.7 | 3.4 | 0.0034 |
| Sodium (mmol/24hr) | 80.2 | 128.5 | 176.7 | 249.8 | - |
| Potassium (mmol/24hr) | 40.7 | 48.7 | 56.7 | 66.8 | <0.0001 |
| Sodium/Potassium Excretion Ratio |
2.34 | 2.96 | 3.42 | 4.01 | <0.0001 |
Data represent means or percentages.
SBP = systolic blood pressure; DBP = diastolic blood pressure.
Table 3.
Total mortality following the Trials of Hypertension Prevention through 2013 by categories of urinary sodium excretion and urinary sodium/potassium excretion ratio among those not in a sodium reduction intervention.
|
Sodium Excretion (mg/24hr)
|
HR per 1000 mg/24hr |
||||||
|---|---|---|---|---|---|---|---|
| <2300 | 2300-<3600 | 3600-<4800 | ≥ 4800 | P-trend | P | ||
| A. Deaths/ Total (%) | |||||||
| TOHP I | 22/246 (8.9) | 73/775 (9.4) | 63/566 (11.1) | 31/257 (12.1) | |||
| TOHP II | 1/66 (1.5) | 32/407 (7.9) | 30/413 (7.3) | 20/281 (7.1) | |||
| B. Hazard Ratios | |||||||
| Model 1 | |||||||
| HR 95%CI |
0.74 0.46-1.19 |
0.90 0.67-1.20 |
1.00 (Reference) |
1.13 0.80-1.59 |
0.092 | 1.13 1.03-1.24 |
0.013 |
| Model 2 | |||||||
| HR 95%CI |
0.75 0.45-1.26 |
0.95 0.70-1.29 |
1.00 (Reference) |
1.07 0.75-1.54 |
0.30 | 1.12 1.00-1.26 |
0.052 |
| Sodium/Potassium Excretion Ratio | HR per unit |
||||||
| <2 | 2-<3 | 3-<4 | ≥ 4 | P-trend | p | ||
|
| |||||||
| C. Deaths/ Total (%) | |||||||
| TOHP I | 37/364 (10.2) | 81/812 (10.0) | 45/458 (9.8) | 26/210 (12.4) | |||
| TOHP II | 7/127 (5.5) | 32/475 (6.7) | 27/368 (7.3) | 17/197 (8.6) | |||
| D. Hazard Ratios | |||||||
| Model 1 | |||||||
| HR 95%CI |
0.81 0.55-1.20 |
0.86 0.63-1.16 |
1.00 (Reference) |
1.28 0.86-1.88 |
0.033 | 1.19 1.06-1.33 |
0.0024 |
| Model 2 | |||||||
| HR 95%CI |
0.90 0.60-1.34 |
0.86 0.64-1.17 |
1.00 (Reference) |
1.20 0.81-1.78 |
0.14 | 1.13 1.01-1.27 |
0.035 |
From Cox proportional hazards regression models stratified by trial phase and adjusted for age, sex, race/ethnicity, clinic, and treatment assignment (Model 1), plus education status, baseline weight, alcohol use, smoking, exercise, potassium excretion (in sodium model), and family history of cardiovascular disease (Model 2).
HR = hazard ratio; CI = confidence interval.
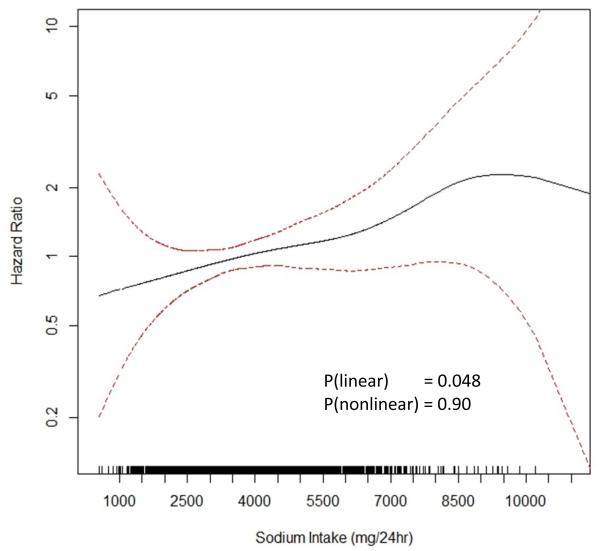
When average urinary sodium excretion was treated as a continuous term, the HR was 1.12 per 1000 mg/24hr (p=0.052). In spline analysis, there was a direct linear relation of intake with later mortality, with no deviation from linearity detected (Central Illustration). No significant interactions were identified by time, gender, age, race, or by weight loss intervention in TOHP II.
Central Illustration.
Spline plot of average sodium intake based on multiple 24hr excretions and total mortality in observational analysis of usual intake.
Shown is the hazard ratio for total mortality over more than 20 years as a function of usual sodium intake averaged over 3-7 urine collections over 1-3 years at baseline. Mortality is lowest among those with usual sodium intake less than 2300 mg/24hr and highest among those with levels above 6000 mg/24hr. There is a significant direct linear effect of sodium with mortality (p=0.048) with no evidence of non-linearity (p=0.90) in spline analysis.
In analyses of the sodium/potassium ratio, there was a significant trend across categories of <2, 2-<3, 3-<4 and 4+ with HRs of 0.81, 0.86, 1.00 (reference), and 1.28, respectively (p for trend = 0.033). The trend was slightly attenuated after further adjustment for baseline characteristics to 0.90, 0.86, 1.00, and 1.20, respectively (p for trend = 0.14). In a comparison of the lowest (<2) to the highest (≥4) category, the HR was 0.75 (95%CI = 0.47-1.20). There was also a linear relation to mortality with a HR of 1.13 per unit increase in the ratio (p=0.035), with no significant deviation from linearity found in spline analysis (Supplemental Figure 4). There were no significant interactions with time, gender, age, or race, or with the weight loss intervention in TOHP II.
DISCUSSION
The health effects of sodium intake remain controversial despite clear effects on blood pressure. Many studies have found conflicting results when examining effects of sodium consumption on incidence of cardiovascular disease or on CVD or total mortality. Much of the controversy results from unique methodologic challenges arising from the study of sodium.6 Unlike macronutrients which can be assessed with food frequency questionnaires, sodium is typically hidden in processed foods and can vary from brand to brand. Studies using questionnaires to assess sodium intake8 are thus using an instrument that may be biased due to both random and systematic errors. In addition, while 24hr diet recalls or food records can assess intake at the population or group levels, these are inadequate to assess individual consumption because of large day-to-day variation in diet.16
Many studies that have examined the health effects of dietary sodium are based on urinary sodium excretion data. In these studies, quality of the exposure assessment has varied substantially. Overnight or spot urine samples may not adequately reflect intake compared to “gold standard” 24hr urine specimens.17,18 Several studies that have found a U- or J-shaped relationship of sodium intake with CVD or mortality have employed overnight or urinary spot samples to estimate dietary sodium intake,7,19,20 but these estimates could be affected by error in estimation of dietary sodium. Even a single 24hr urine specimen may not be sufficient to accurately estimate usual sodium consumption. In a simulated space flight, urinary sodium excretion demonstrated considerable variability despite a constant sodium intake.21,22 Researchers estimated that three 24-hour collections would improve accuracy to 75% compared to sodium ingestion, and that seven would be needed to improve accuracy to 92%.23 The TOHP study reported here included up to seven excretion measures, and includes the most accurate sodium exposure assessment in relation to outcomes to date.
Another issue that may lead to bias in effect estimates is the possibility of reverse causation. Some studies include participants with prior cardiovascular7,19 or other diseases, including diabetes.24,25 These individuals may have been advised to limit their sodium intake, or have reduced caloric intake and consequently reduced sodium intake related to their underlying illness, leading to apparent increased risk among those with low levels. The same is true for those with hypertension,26 due to the well-known relationship of sodium to blood pressure. Participants in the TOHP trials did not have prior hypertension, diabetes or CVD, and these results should not suffer from this problem of reverse causation.
Some limitations of our analysis should be noted. First, in the randomized comparison while TOHP participants were randomized to an active sodium intervention or usual care, it is not clear how well they maintained the intervention over time, particularly over more than 20 years. In fact, there was some indication of a difference between randomized groups through 10 years that was not maintained with longer follow-up. On our previous follow-up for incident CVD conducted in 2004-5,11 those in the sodium intervention reported a stronger preference for low sodium foods at 14-17 years post-randomization. Whether this difference was maintained over an additional 9 years, though, is unknown.
Second, in our observational analysis while we have accurate measures of sodium intake during the trial periods, we have no later measures of sodium intake during the course of follow-up. It is likely that there were changes in usual diet over the long course of follow-up, a limitation that is shared with most observational analyses of excretion data and long-term outcomes. We did not, however, find any significant interaction with time.
Finally, it is possible that some of the effect of our estimate of usual sodium intake may be related to other dietary factors, such as more fruit and vegetable intake and less consumption of saturated fat. While some dietary information was available in TOHP I, this was collected in only a small subset in TOHP II. We were thus unable to control for such factors in our analyses with sufficient power. All of our analyses, however, controlled for the weight loss intervention in TOHP II as well as for baseline weight, which should be correlated with energy intake. Potassium excretion may be another marker for a more healthy dietary pattern and was included in our adjusted models.
In contrast to some other studies, we found a direct linear relation of an accurate measure of usual sodium intake to total mortality over a period of 23-26 years, with higher risk at high sodium intake and no evidence of a U- or J-shape, though as in other studies power is limited to estimate effects at the tails of the sodium distribution. The relationship was slightly stronger for the sodium/potassium ratio, two electrolytes that are suspected of playing joint roles in the pathogenesis of hypertension.27 Our analysis of the randomized sodium interventions was also consistent with an effect on mortality, with an estimated 15% reduced risk, albeit non-significant, among those randomly assigned to the active sodium reduction intervention vs. usual care.
Average levels of sodium intake in the U.S. remain too high,28 and even appear to be increasing.29 In 2010 the Institute of Medicine recommended a gradual reduction in sodium levels,30 which would be more palatable to consumers. Such reductions appear feasible,31 and would serve to reduce the population level of blood pressure, incidence of hypertension, and help prevent subsequent morbidity and mortality.
Supplementary Material
ACKNOWLEDGEMENTS
FUNDING SOURCES
TOHP I and II were supported by cooperative agreements HL37849, HL37852, HL37853, HL37854, HL37872, HL37884, HL37899, HL37904, HL37906, HL37907, and HL37924, all from the National Heart, Lung, and Blood Institute (NHLBI), National Institutes of Health. The TOHP Follow- up Study was supported by grant HL57915 from the NHLBI and award 14GRNT18440013 from the American Heart Association (AHA). The NHLBI and AHA had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Abbreviations
- TOHP
Trials of Hypertension Prevention
- CVD
cardiovascular disease
- HR
hazard ratio
- CI
confidence interval
- SBP
systolic blood pressure
- DBP
diastolic blood pressure
Footnotes
This paper was presented at the AHA Scientific Sessions 2015.
Conflict of Interest Disclosures: None
REFERENCES
- 1.He FJ, Li J, MacGregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013 Apr 5;346:f1325. doi: 10.1136/bmj.f1325. 2013. [DOI] [PubMed] [Google Scholar]
- 2.Aburto N, Ziolkovska N, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ. 2013 Apr 5;346:f1326. doi: 10.1136/bmj.f1326. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whelton PK, Appel LJ, Espeland MA, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group. JAMA. 1998 Mar 18;279(11):839–846. doi: 10.1001/jama.279.11.839. [DOI] [PubMed] [Google Scholar]
- 4.Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 5.IOM (Institute of Medicine) Sodium intake in populations: Assessment of evidence. The National Academies Press; Washington, DC: 2013. [PubMed] [Google Scholar]
- 6.Cobb LK, Anderson CA, Elliott P, et al. Methodological issues in cohort studies that relate sodium intake to cardiovascular disease outcomes: a science advisory from the american heart association. Circulation. 2014 Mar 11;129(10):1173–1186. doi: 10.1161/CIR.0000000000000015. [DOI] [PubMed] [Google Scholar]
- 7.O'Donnell M, Mente A, Rangarajan S, et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 2014 Aug 14;371(7):612–623. doi: 10.1056/NEJMoa1311889. [DOI] [PubMed] [Google Scholar]
- 8.Kalogeropoulos AP, Georgiopoulou VV, Murphy RA, et al. Dietary sodium content, mortality, and risk for cardiovascular events in older adults: the Health, Aging, and Body Composition (Health ABC) Study. JAMA internal medicine. 2015 Mar;175(3):410–419. doi: 10.1001/jamainternmed.2014.6278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Graudal N, Jurgens G, Baslund B, Alderman MH. Compared with usual sodium intake, low- and excessive-sodium diets are associated with increased mortality: a meta-analysis. Am J Hypertens. 2014 Sep;27(9):1129–1137. doi: 10.1093/ajh/hpu028. [DOI] [PubMed] [Google Scholar]
- 10.Cook NR, Appel LJ, Whelton PK. Lower levels of sodium intake and reduced cardiovascular risk. Circulation. 2014 Mar 4;129(9):981–989. doi: 10.1161/CIRCULATIONAHA.113.006032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cook NR, Cutler JA, Obarzanek E, et al. The long-term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the Trials of Hypertension Prevention. BMJ. 2007;334:885–888. doi: 10.1136/bmj.39147.604896.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cook NR, Obarzanek E, Cutler JA, et al. Joint effects of sodium and potassium intake on subsequent cardiovascular disease: The Trials of Hypertension Prevention (TOHP) Follow-up Study. Arch Intern Med. 2009;169(1):32–40. doi: 10.1001/archinternmed.2008.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Trials of Hypertension Prevention Collaborative Research Group The effects of nonpharmacologic interventions on blood pressure of persons with high normal levels. Results of the Trials of Hypertension Prevention, Phase I. J Amer Med Assoc. 1992;267(9):1213–1220. doi: 10.1001/jama.1992.03480090061028. [DOI] [PubMed] [Google Scholar]
- 14.The Trials of Hypertension Prevention Collaborative Research Group Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high- normal blood pressure. The Trials of Hypertension Prevention, Phase II. The Trials of Hypertension Prevention Collaborative Research Group. Arch Intern Med. 1997;157(6):657–667. [PubMed] [Google Scholar]
- 15.Brown IJ, Tzoulaki I, Candeias V, Elliott P. Salt intakes around the world: implications for public health. International journal of epidemiology. 2009 Jun;38(3):791–813. doi: 10.1093/ije/dyp139. [DOI] [PubMed] [Google Scholar]
- 16.Caggiula AW, Wing RR, Nowalk MP, Milas NC, Lee S, Langford H. The measurement of sodium and potassium intake. Am J Clin Nutr. 1985 Sep;42(3):391–398. doi: 10.1093/ajcn/42.3.391. [DOI] [PubMed] [Google Scholar]
- 17.Ji C, Sykes L, Paul C, et al. Systematic review of studies comparing 24-hour and spot urine collections for estimating population salt intake. Revista panamericana de salud publica = Pan American journal of public health. 2012 Oct;32(4):307–315. doi: 10.1590/s1020-49892012001000010. [DOI] [PubMed] [Google Scholar]
- 18.Ji C, Miller MA, Venezia A, Strazzullo P, Cappuccio FP. Comparisons of spot vs 24-h urine samples for estimating population salt intake: validation study in two independent samples of adults in Britain and Italy. Nutrition, metabolism, and cardiovascular diseases : NMCD. 2014 Feb;24(2):140–147. doi: 10.1016/j.numecd.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 19.O'Donnell MJ, Yusuf S, Mente A, et al. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA. 2011 Nov 23;306(20):2229–2238. doi: 10.1001/jama.2011.1729. [DOI] [PubMed] [Google Scholar]
- 20.Pfister R, Michels G, Sharp SJ, Luben R, Wareham NJ, Khaw KT. Estimated urinary sodium excretion and risk of heart failure in men and women in the EPIC-Norfolk study. European journal of heart failure. 2014 Apr;16(4):394–402. doi: 10.1002/ejhf.56. [DOI] [PubMed] [Google Scholar]
- 21.Rakova N, Juttner K, Dahlmann A, et al. Long-term space flight simulation reveals infradian rhythmicity in human Na(+) balance. Cell metabolism. 2013 Jan 8;17(1):125–131. doi: 10.1016/j.cmet.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 22.Titze J, Dahlmann A, Lerchl K, et al. Spooky sodium balance. Kidney Int. 2014 Apr;85(4):759–767. doi: 10.1038/ki.2013.367. [DOI] [PubMed] [Google Scholar]
- 23.Lerchl K, Rakova N, Dahlmann A, et al. Agreement between 24-hour salt ingestion and sodium excretion in a controlled environment. Hypertension. 2015 Oct;66(4):850–857. doi: 10.1161/HYPERTENSIONAHA.115.05851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ekinci EI, Clarke S, Thomas MC, et al. Dietary salt intake and mortality in patients with type 2 diabetes. Diab Care. 2011;34(3):703–709. doi: 10.2337/dc10-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thomas MC, Moran J, Forsblom C, et al. The association between dietary sodium intake, ESRD, and all-cause mortality in patients with type 1 diabetes. Diab Care. 2011;34(4):861–866. doi: 10.2337/dc10-1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stolarz-Skrzypek K, Kuznetsova T, Thijs L, et al. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA. 2011;305(17):1777–1785. doi: 10.1001/jama.2011.574. [DOI] [PubMed] [Google Scholar]
- 27.Adrogue HJ, Madias NE. Sodium and potassium in the pathogenesis of hypertension. N Engl J Med. 2007;356:1966–1978. doi: 10.1056/NEJMra064486. [DOI] [PubMed] [Google Scholar]
- 28.Cogswell ME, Zhang Z, Carriquiry AL, et al. Sodium and potassium intakes among US adults: NHANES 2003–2008. Am J Clin Nutr. 2012;96:647–657. doi: 10.3945/ajcn.112.034413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pfeiffer CM, Hughes JP, Cogswell ME, et al. Urine sodium excretion increased slightly among U.S. adults between 1988 and 2010. The Journal of nutrition. 2014 May;144(5):698–705. doi: 10.3945/jn.113.187914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.IOM (Institute of Medicine) Strategies to reduce sodium intake in the United States. The National Academies Press; Washington, DC: 2010. [Google Scholar]
- 31.Levings JL, Cogswell ME, Gunn JP. Are reductions in population sodium intake achievable? Nutrients. 2014 Oct;6(10):4354–4361. doi: 10.3390/nu6104354. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.