Abstract
Summary
An international consensus process resulted in exercise and physical activity recommendations for individuals with osteoporosis. Emphasis was placed on strength, balance, and postural alignment. Rather than providing generic restrictions, activity should be encouraged while considering impairments, fracture risk, activity history, and preference, and guidance on spine sparing techniques should be provided.
Introduction
The objectives of this study were to establish expert consensus on key questions posed by patients or health care providers regarding recommended assessment domains to inform exercise prescription, therapeutic goals of exercise, and physical activity and exercise recommendations for individuals with osteoporosis or osteoporotic vertebral fracture.
Methods
The Too Fit To Fracture expert panel identified researchers and clinicians with expertise in exercise and osteoporosis and stakeholder groups. We delivered a modified online Delphi survey (two rounds) to establish consensus on assessment, exercise, and physical activities for three cases with varying risk (osteoporosis based on bone mineral density; 1 spine fracture and osteoporosis; multiple spine fractures, osteoporosis, hyperkyphosis, and pain). Duplicate content analyses of free text responses were performed.
Results
Response rates were 52 % (39/75) and 69 % (48/70) for each round. Key consensus points are the following: (a) Current physical activity guidelines are appropriate for individuals with osteoporosis without spine fracture, but not for those with spine fracture; (b) after spine fracture, physical activity of moderate intensity is preferred to vigorous; (c) daily balance training and endurance training for spinal extensor muscles are recommended for all; (d) providing guidance on spine-sparing techniques (e.g., hip hinge) during activities of daily living or leisure, considering impairments, fracture risk, activity history, and preference, is recommended rather than providing generic restrictions (e.g., lifting <10 lbs, no twisting), but for those with vertebral fracture, especially in the presence of pain, multiple fractures, or hyperkyphosis, the risks of many activities may outweigh the benefits—physical therapist consultation is recommended. Examples of spine-sparing techniques and exercise prescription elements are provided.
Conclusions
Our recommendations guide health care providers on assessment, exercise prescription, and safe movement for individuals with osteoporosis.
Keywords: Bone mineral density, Exercise, Fracture risk, Osteoporosis, Physical activity, Physical therapy, Posture, Spine fracture
Introduction
Receiving a diagnosis of osteoporosis can create fear and uncertainty. The risk of death in those with a vertebral fracture is 2.7 times higher than those without fractures, and one woman in five who have a vertebral fracture will have another vertebral fracture within a year [1, 2]. Osteoporosis together with a fall can also result in hip fractures, which can cause pain, functional impairment, and lost independence, and over 25 % of individuals who suffer a hip fracture will die within the following year [3]. Osteoporosis management guidelines include nutrition, exercise, and pharmacotherapy but may also need to consider other behaviors, such as safe performance of activities of daily living.
High-quality research on the efficacy and safety of therapeutic exercise or physical activity among individuals with osteoporosis or vertebral fractures is scarce, posing barriers to health care providers and patients seeking exercise as a means to improve function or reduce fracture risk [4]. Recent exercise recommendations were developed for individuals with a diagnosis of osteoporosis or vertebral fracture, with careful consideration of the quality of available evidence, the benefits and harms, and the values and preferences of patients [5]; strong recommendations were made for multicomponent exercise. However, the recommendations do not address the safety or efficacy of many physical activities that patients wish to partake in, including activities of daily living. There is a distinction between the terms exercise and physical activity; exercise is defined as “…physical activity that is planned, structured, repetitive and purposive in the sense that improvement or maintenance of one or more components of physical fitness is an objective,” whereas physical activity refers to “…any bodily movement produced by skeletal muscles that results in energy expenditure” [6]. Therefore, physical activity includes activities of daily living or activities that are done for leisure or social engagement. As researchers who speak at community events or as health care providers, we have often encountered questions from patients about physical activity, and there is little research to support our answers. Example patient questions include the following: How much weight can I lift? Can I take part in yoga? Is it safe for me to golf, or play tennis? My doctor told me not to lift more than 5 pounds, how do I shop for my groceries? Further, it is unclear to patients how activities need to be modified in the presence of pain, the hyperkyphotic posture that can occur with vertebral fractures.
For many questions important to patients, there is little evidence to guide the answers. Therefore, we have performed an extensive consultation of stakeholders (e.g., researchers, physicians, physiotherapists, national osteoporosis societies) to come to consensus on recommendations related to physical activity and exercise. The Too Fit To Fracture initiative aimed to develop comprehensive exercise and physical activity recommendations for individuals with osteoporosis (based on a bone mineral density [BMD in g/cm2] T-score ≤−2.5) or osteoporotic vertebral fracture. Part of this initiative was to address questions frequently asked by patients or health care providers, where there is limited evidence to guide responses. Therefore, the objective of the current study was to establish expert consensus on key questions posed by patients or health care providers regarding recommended assessment domains to inform exercise prescription, therapeutic goals of exercise, and physical activity and exercise recommendations for individuals with osteoporosis or osteoporotic vertebral fracture.
Methods
We conducted a multistep process to determine important questions and establish expert consensus: (1) forming an expert panel, (2) gathering frequently asked questions and deciding on clinical scenarios, (3) conducting a modified RAND/UCLA Delphi process [7] to establish consensus, and (4) obtaining stakeholder input and finalizing the recommendations.
Forming the expert panel
The Too Fit To Fracture expert panel includes researchers and clinicians from Australia, Canada, Finland, and the USA, as well as partners from Osteoporosis Canada. Panel members had prior experience with guideline development or conducting clinical trials of exercise in individuals with osteoporosis, or relevant clinical or anatomy/biomechanics expertise.
Formalizing the questions and clinical scenarios
Webinars on physical activity held by Osteoporosis Canada for health care providers and for patient groups (such as the Canadian Osteoporosis Patient Network) resulted in “frequently asked questions” that were circulated to the expert panel. For round 1, the panel compiled a list of questions from the patient perspective using the frequently asked questions and questions posed to panel members in clinical practice (Table 1); the domains represented included assessment, therapeutic goals, appropriateness of current guidelines, safety of sports or activities (e.g., golf, yoga), and how to modify activities of daily living.
Table 1.
Questions posed in round 1 of the Too Fit To Fracture Consensus Process
| Question | Response possibilities |
|---|---|
| When setting goals or prescribing exercise, what key things should a health care provider ask, observe, screen for, or assess? | Free text answer |
| What information or test results would be needed to tailor the exercise prescription? | |
| What therapeutic goals should be set for this case1 when designing an exercise program? | Free text answer |
| Do you think that the guidelines detailed above are appropriate for this case1? |
|
| What, if anything, would you add or change about the guidelines above to make them more appropriate for the case1, or target the goals you set in the previous question? | Free text answer |
| “I would like to do strength training with weights. How much weight should I use?” |
|
| Please comment on the rationale for your answer (Free text) |
|
| “Do I need to avoid or modify any of the following activities because they are risky for me to do?” (select all that apply) |
|
| Yoga |
|
| Pilates | |
| Sports such as golf or tennis |
|
| Exercises targeting my abdominal or core muscles |
|
| All of these are safe for you to do | |
| I do not know | |
| “Are there any other exercises, sports, strength training machines, or movements I should avoid? Why?” | Free text answer |
| “Are there activities that I would normally do in a day that I cannot do, or that I need to do differently, like household chores or when caring for myself? Why?” | Free text answer |
| Would any of your exercise goals or recommendations for any of the cases change if the cases were male? Why or why not? | Free text answer |
| Would any of your treatment goals or exercise recommendations change if the cases were 10 years older? Why or why not? | Free text answer |
Questions were asked related to research priorities, and nutrition and exercise and are not included here as they do not address the objectives of the current project but can be found here [8]
All of the questions except for the first two and the last two were asked in the context of a particular case, where the description of the case was presented with each question for reference. The questions were repeated for three different cases. The first two and the last two questions in this list were asked only once at the start and end of the survey, respectively
All but the first and last two questions were posed from the perspective of the patient. The panel convened to decide on target clinical scenarios previously for a grading of recommendations, assessment, development, and evaluation process [9] that resulted in evidence-based exercise recommendations (5). The “patients” were based on two target groups: individuals with osteoporosis based on BMD (i.e., T-score ≤ −2.5) and individuals with a history of clinical or morphometric osteoporotic vertebral fracture. It was hypothesized by the panel that the presence of pain, multiple fractures, or altered posture may modify the recommendations. Therefore, the panel generated the following three patient scenarios to provide context for developing recommendations:
-
Case 1: Osteoporosis based on BMD, with no history of vertebral fracture:
“I am a 68 year-old woman. I am 168 cm tall and I weigh 66 kg. My femoral neck bone mineral density T-score is −2.2 and my lumbar spine bone mineral density T-score is −2.7. I have been told that I am at moderate risk for future fractures1, even though I have never broken a bone and don’t have any other risk factors.” -
Case 2: Osteoporosis based upon BMD with history of one vertebral fracture:
“I am a 68 year-old woman. I am 168 cm tall and I weigh 65 kg. My femoral neck bone mineral density T-score is −2.2 and my lumbar spine bone mineral density T-score is −3.2. I had an osteoporotic spine fracture last year. I have been told that I am at high risk for future fractures1.” -
Case 3: Osteoporosis based upon BMD with history of multiple vertebral fractures, pain, hyperkyphosis:
“I am a 68 year-old woman. I am 168 cm tall and I weigh 65 kg. My femoral neck bone mineral density T-score is −2.9 and lumbar spine bone mineral density T-score is −3.2. I have had several osteoporotic spine fractures over the years which have caused me to have a curved spine. I often experience pain with daily activities. I have been told that I am at high risk for future fractures1.”
The intent was to represent those at moderate or high risk of future fracture. Our target clinical scenarios did not represent those with a history of hip fracture, those with a BMD T-score between −1.0 and −2.5, with or without a history of a nonvertebral, nonhip fracture, or those with very low BMD (T-score <−3.0) but no history of fracture. There was interest in developing recommendations for those with a history of hip fracture or those with T-scores between −1.0 and −2.5, but including all of these additions was decided to be too broad a scope. The first case (i.e., osteoporosis without fracture) had characteristics that would place her in the moderate risk of fracture category according to the CAROC tool (http://www.osteoporosis.ca/health-care-professionals/clinical-tools-and-resources/fracture-risk-tool/) and would be associated with an 11 and 2.2 % probability of major osteoporotic fracture and hip fracture, respectively, in the next 10 years according to the FRAX tool (http://www.shef.ac.uk/FRAX/tool.aspx?country=19). Case 2 would be considered high risk of fracture according to the CAROC tool and would have a 17 and 3.5 % probability of major osteoporotic fracture and hip fracture, respectively, in the next 10 years according to the FRAX tool. Case 3 would be at high risk with a 23 and 7.1 % probability of major osteoporotic and hip fracture, respectively, in the next 10 years based on BMD and the presence of at least one vertebral fracture, although clinical judgment may also consider the presence of multiple fractures, pain and hyperkyphosis as additional risk modifiers. Therefore, one could generalize the recommendations to other scenarios in similar fracture risk categories, with consideration for the presence of impairments that may alter recommendations (e.g., hip fracture history might result in gait and balance impairments that require more conservative balance exercises or use of assistive aids). Indeed, individuals with hip fractures may present with a number of impairments that limit the generalizability of the recommendations, including cognitive impairment, frailty, or higher fall risk. It may be more appropriate to generate exercise or activity recommendations specific to individuals with a hip fracture history in the future.
Modified RAND/UCLA Delphi consensus process
The expert panel identified and agreed upon 75 researchers and clinicians to invite to the consensus process based on a history of high-quality research on osteoporosis and physical activity in older adults, or recognized clinical expertise in physical activity and osteoporosis. Stakeholder groups identified included Osteoporosis Canada, Osteoporosis Australia, the Canadian Physiotherapy Association, the National Osteoporosis Foundation, the Finnish Osteoporosis Association, and the International Osteoporosis Foundation. A patient representative from the Canadian Osteoporosis Patient Network was invited. For round 1, we used FluidSurveys (http://fluidsurveys.com/) to distribute an online survey including the questions in Table 1 to all invitees, as part of a RAND/UCLA Delphi method to identify appropriate physical activity recommendations for defined clinical indications, as was done for the 2010 Osteoporosis Clinical Practice Guidelines [10]. Three reminders were sent, 1 to 2 weeks apart.
The expert panel subsequently reads the responses to all questions, and each member was assigned up to two questions where they were to perform a content analysis on responses/comments provided by participants; each question was reviewed by at least two panel members. Conventional content analyses consisted of identifying common themes and grouping responses accordingly, as well as identifying areas of agreement or consensus, and areas of disagreement or lack of consensus, and was standardized by providing panel members with a guide [11]. Panel members assigned to a question met via telephone to confirm the areas of agreement and to develop a recommendation. For round 2, each recommendation or set of recommendations was presented with the question “Do you agree with the recommendations?” with the following possible answers: (1) yes, (2) no, (3) I do not know, (4) I agree with some of it/them but not all of it/them, and (5) other. The latter two had open text boxes for clarification and comments. Seventy individuals were invited to round 2 (all who responded to round 1 and new invitees) and sent three reminders. The responses were reviewed by at least two panel members for areas of consensus and areas of disagreement using the same protocol as round 1. All panel members agreed that no further rounds were necessary after round 2 because the majority of respondents were in agreement with what was proposed. The recommendations were revised based on input from round 2.
Stakeholder input and finalizing recommendations
The rationale, methods, results, and recommendations were drafted and circulated to the panel, respondents, and stakeholder groups for review and comment on its utility and clarity. Several of the recommendations were presented at the American Society for Bone and Mineral Research annual meeting in 2013 [12]. These activities offered a “round 3” or final opportunity to provide input on the recommendations. Revisions were made to address stakeholder feedback.
Results
All of the recommendations evolved from an amalgamation of expert responses—they were not based on a review of evidence. The expert panel provided additional input and indirect evidence (e.g., observational studies or biomechanical modeling studies) to support the recommendations, which are cited where appropriate. It was noted that there is no adequately powered evidence regarding the benefits and harms of exercise to enable the development of specific recommendations for all potential case presentations of individuals with osteoporosis that all clinicians will be able to interpret and apply. A previous Too Fit To Fracture report outlines the available evidence regarding the benefits and harms of exercise for individuals with osteoporosis, with or without a history of vertebral fracture [13]—the evidence presented in that report is not included here. However, many stakeholders who participated in that review process also contributed here, and so were aware of the evidence reviewed and resultant recommendations.
The response rate for round 1 was 52 % (39/75), and the response rate for round 2 was 69 % (48/70); those who responded in one or more rounds are listed in Table 2. Agreement with the recommendations (a “yes” answer in round 2) ranged from 65 to 95 %. Many respondents who reported that they did not agree with some or all of the recommendation suggested a revision. Several respondents identified the need to clarify the audience for the recommendations, the need to consider individual patient characteristics, and comprehensive osteoporosis management; so, we have added the “Target audience and considerations when implementing the Too Fit To Fracture recommendations in individuals with osteoporosis or osteoporotic vertebral fracture” section, below, prior to the recommendations resulting from the consensus process (“Recommendations on assessment to guide activity prescription for individuals with osteoporosis, with or without a history of vertebral fracture,” “Goals of therapeutic exercise for individuals with osteoporosis,” “Physical activity and exercise guidelines for individuals with osteoporosis,” and “How to address frequently asked questions posed by individuals with osteoporosis” sections).
Table 2.
Researchers and clinicians who contributed to one or more rounds of the Too Fit To Fracture Delphi Consensus, or were on the expert panel (bold), in alphabetical order by first name; the patient advocates are not listed
| Alexandra Papaioannou, MD, MSc, FRCPC, FACP, Professor, Department of Medicine, McMaster University, Canada |
| Amanda Lorbergs, Postdoctoral Research Fellow at Harvard Medical School, Hebrew Senior Life, Institute for Aging Research, USA |
| Angela M. Cheung, MD, PhD, FRCPC, CCD, Director, Osteoporosis Program, Department of Medicine, University of Toronto, Canada |
| Angela Juby, MBChB, Associate Professor, University of Alberta, Canada |
| Ari Heinonen, PhD, Professor, Department of Health Sciences, University of Jyväskylä, Finland |
| Belinda Beck, PhD, Associate Professor, Griffith Health Institute, Australia |
| Bonny O’Hare, BScPT, Clinical Physiotherapist, Director: Pro Motion Physiotherapy, Osteo-Circuit, Canada |
| Caitlin McArthur, PT, PhD student, Aging, Health and Wellbeing Program, University of Waterloo |
| Carleen Lindsay, PT, MScAH, GCS, Bristol Physical Therapy, Connecticut, USA |
| Catherine M. Jankowski, PhD, Associate Professor, University of Colorado Anschutz Medical Campus, College of Nursing and Division of Geriatric Medicine, USA |
| Cathie Sherrington, Associate Professor, The George Institute for Global Health, University of Sydney, Australia |
| Debra Butt, MD, Assistant Professor, Department of Family and Community Medicine, The Scarborough Hospital, University of Toronto, Canada |
| Debra J. Rose, PhD Director, Institute of Gerontology and Center for Successful Aging, California State University, Fullerton. USA |
| Douglas P. Kiel, MD, MPH, Professor of Medicine, Harvard Medical School, Director Musculoskeletal Research Center, Institute for Aging Research, Hebrew Senior Life |
| George Ioannidis, PhD, Assistant Professor, Department of Medicine, McMaster University, Canada |
| Gustavo Duque, MD, PhD, FRACP. Ageing Bone Research Program, Sydney Medical School Nepean, University of Sydney, Australia |
| Harri Sievanen, ScD, Research Director, The UKK Institute for Health Promotion Research, and President, Finnish Osteoporosis Association, Finland |
| Heather Frame, MD, Scientific Advisory Council, Osteoporosis Canada |
| Heather Keller, PhD, Professor, Department of Kinesiology, University of Waterloo, Canada |
| Heather McKay, PhD, Professor, University of British Columbia; Director, Centre for Hip Health and Mobility, Canada |
| Heikki Kroger, MD, PhD, Department of Orthopaedics, Traumatology and Hand Surgery, Kuopio University Hospital, Finland |
| Irene Poulidoulis, MD, Assistant Professor, Department of Family & Community Medicine, University of Toronto, Canada |
| Jacqueline Close, MBBS, MD, Associate Professor, Neuroscience Research Australia & Prince of Wales Clinical School, University of New South Wales, Australia |
| John D. Wark, PhD, Professor, Department of Medicine, University of Melbourne, Australia |
| Jonathan D. Adachi, MD FRCPC, Professor of Medicine, St Joseph’s Healthcare – McMaster University, Canada |
| Judi Laprade, BScPT, PhD, Division of Anatomy, University of Toronto, Canada |
| Juhani Multanen, PT, PhD Student, Department of Health Sciences, University of Jyväskylä, Finland |
| Karen Kemmis, PT, DPT, MS, GCS, SUNY Upstate Medical University, United States of America |
| Kathy Shipp, PT, PhD, Department of Community and Family Medicine, Duke University, United States of America |
| Kerrie M. Sanders, PhD, Associate Professor, Australian Institute of Musculoskeletal Sciences, University of Melbourne, Western Health, St Albans, Victoria, Australia |
| Kirsti Uusi-Rasi, PhD, Adjunct Professor Senior Researcher UKK Institute, Finland |
| Klaus Engelke, PhD, Institute of Medical Physics, University of Erlangen-Nuremberg, Germany |
| Laetitia Michou, MD, CHUL Research Centre, Université Laval |
| Leon Flicker, MB BS, PhD, FRACP, Professor and Director of Geriatric Medicine, Western Australian Centre for Health & Ageing, Western Australian Institute for Medical Research, University of Western Australia |
| Lora Giangregorio, PhD, Associate Professor, Department of Kinesiology, University of Waterloo, Canada |
| Maarit Piirtola, PT, PhD (Family Medicine); Department of Public Health, Hjelt Institute, University of Helsinki and the UKK Institute for Health Promotion Research, Finland, and Board Member, Finnish Osteoporosis Association |
| Mary Bouxsein, PhD, Assistant Professor, Department of Orthopedic Surgery, Harvard Medical School, USA |
| Maureen C. Ashe, PT, PhD, Associate Professor, Department of Family Practice, University of British Columbia, Canada |
| Norma J. MacIntyre, PT, PhD, Associate Professor, School of Rehabiliation Science, McMaster University, Canada |
| Phil Chilibeck, PhD, Professor, College of Kinesiology, University of Saskatchewan, Canada |
| Ravi Jain, Ontario Osteoporosis Strategy & Osteoporosis Canada |
| Robin Daly, PhD, Chair of Exercise and Ageing, Associate Head of School (Research), Deakin University, Australia |
| Rowena Ridout, MD FRCPC, Toronto Western Hospital, Canada and University of Toronto, Canada |
| Saija Kontulainen, PhD, Associate Professor, University of Saskatchewan, Canada |
| Sandy Iuliano-Burns, PhD, University of Melbourne, Australia |
| Sanna Kääriä, PhD, South Karelia Social and Health Care District, Finland |
| Sara Mecomber-Meeks, PT, MS, GCS |
| Sharron Steeves, Dip PT&OT Physiotherapist, Physio Fitness, New Brunswick, Canada |
| Sherri Betz, PT, GCS, CEEAA, PMA®-CPT United States |
| Stephanie Grant, M.S., OTR/L; United Osteoporsis Centers, Gainesville, GA, USA |
| Stephen Lord, PhD, Professor, University of New South Wales, Neuroscience Research Australia, Australia |
| Stuart McGill, PhD, Professor, Department of Kinesiology, University of Waterloo, Canada |
| Stuart Warden, BPhysio PhD, FACSM, Associate Professor, Department of Physical Therapy, Indiana University-Purdue University Indianapolis, USA |
| Susan W. Muir-Hunter, PT, PhD, Assistant Professor, School of Physical Therapy, University of Western Ontario, Canada |
| Susan Randall, MSN, FNP-BC, Senior Director, Science and Education, National Osteoporosis Foundation, USA |
| Susan Whiting, PhD, College of Pharmacy and Nutrition, University of Saskatchewan, Canada |
| Suzanne Morin, MD, MSc, Associate Professor, Department of Medicine, McGill University |
| Timo Jämsä, PhD, Professor in Medical Technology, Institute of Biomedicine, University of Oulu, Finland |
| Timo Rantalainen, PT, MSc, PhD Student Researcher, Department of Health Sciences, University of Jyväskylä, Finland |
| Wendy Katzman, PT, DPTSc, Associate Professor, Dept. of Physical Therapy and Rehabilitation Science, University of California San Francisco, USA |
| Wolfgang Kemmler, PhD, Professor, Institute of Medical Physics, University of Erlangen-Nuremberg, Germany |
Target audience and considerations when implementing the Too Fit To Fracture recommendations in individuals with osteoporosis or osteoporotic vertebral fracture
Too Fit To Fracture recommendations outlined here should be used by licensed health care providers who provide guidance on exercise or physical activity to individuals with osteoporosis, while adhering to their scope of practice and referring to the most appropriate provider when necessary (e.g., physical therapist, occupational therapist, kinesiologist). Clinical reasoning is required to tailor exercise/activity recommendations or goals to patient characteristics, such as comorbid conditions (e.g., physical, psychological, social), fall risk, and individual ability. Individuals with osteoporosis should be assessed and managed by a physician in accordance with clinical practice guidelines adopted by their respective countries. National osteoporosis societies should consider providing guidance on how to access appropriate health care providers trained in performing assessment and providing guidance on exercise or physical activity for individuals with osteoporosis.
Recommendations on assessment to guide activity prescription for individuals with osteoporosis, with or without a history of vertebral fracture
There was consensus that when setting goals, prescribing exercise, or advising on safe physical activity as part of a person-centered management plan, a health care provider should assess the following domains:
Medical history and medications, comorbid conditions, and contraindications to exercise.
Fracture risk-results of assessment using a validated risk calculator2 or assessment of risk factors (e.g., fracture history at osteoporotic sites after age of 40, age, sex, and glucocorticoid use, and BMD T-score at femoral neck if available). A patient should be referred for X-rays, and a fracture risk assessment should be done in the presence of 6 cm of historic height loss or 2-cm measured height loss, if a fracture risk assessment has not been performed by a family physician or specialist [10].
Fall3 risk—a person is considered at risk if they present with an acute fall, have had two or more falls in the past 12 months, or present with gait and balance difficulties (in accordance with the American Geriatrics Society/British Geriatrics Society [AGS/BGS] guidelines [14]). In a clinical setting, performance-based tests of balance and mobility may inform the nature of the balance impairment or safety during movement; if an individual has had two or more falls or an acute fall, multifactorial assessment and intervention may be required4.
Physical performance—note the presence of impairment or pain during movements, e.g., lower extremity muscle strength during sit-to-stand, body mechanics during movement, slow gait speed4. An exercise professional may also consider evaluation of domains such as muscular strength or endurance, neuromuscular or functional performance (e.g., coordination, balance, mobility), flexibility, and aerobic capacity.
Standing posture—look for hyperkyphosis, hyperlordosis or hypolordosis [17, 18].
Barriers and facilitators to physical activity—e.g., current physical activity levels, self-efficacy, time, pain, comorbid conditions, access (e.g., socioeconomic status, rural versus urban, available transportation), and patient preferences.
It may not be possible to assess or ascertain all of these areas in all settings. The list provides a comprehensive set of factors that might influence goal-setting, physical activity recommendations, or modifications to activity that may be required. Even brief assessments of each domain may reveal when referral to specialists or other care or service providers is warranted.
There was general consensus that the recommendations would be similar for men and women. When asked if the recommendations would change if the cases were 10 years older, respondents indicated that the health, function, and fall or fracture risk should inform tailoring of any recommendations, rather than chronological age. However, many noted that increasing age may coincide with an increased prevalence of comorbid conditions or impairments that should be considered, particularly if they contribute to an increased risk of falls, fractures, or adverse events during activity. Increasing age by 10 years would increase the FRAX-derived probability of future fracture (e.g., from 11 and 2.2 % risk of major osteoporotic and hip fracture, respectively, to 14 and 4.4 % in case 1).
Goals of therapeutic exercise for individuals with osteoporosis
There was consensus that the main therapeutic goal that should be targeted in individuals with osteoporosis is fracture prevention, via the following subgoals:
Fall prevention: To prevent falls, improved mobility and balance, maintaining or increasing strength in major muscle groups and power in the lower limbs, and optimizing postural alignment are therapeutic targets.
Safe movement: Safe movement includes an emphasis on postural alignment and proper body mechanics to protect the spine from harmful loads (“spine sparing”), and goals to increase muscular endurance in spinal extensors, and stretch muscles that restrict mobility or optimal alignment, e.g., pectorals, hip flexors.
Slow the rate of bone loss: Whether exercise can maintain or increase BMD in individuals with osteoporosis or vertebral fractures has yet to be conclusively established. Inferences about the effect of exercise on BMD are often based on studies in heterogeneous groups of postmenopausal women and men, where osteoporosis was sometimes an exclusion criterion. Given the lack of evidence that exercise can increase BMD in older adults with established osteoporosis, we suggest that the goal should be to slow the rate of bone loss. Concurrent therapeutic goals include maintaining/increasing strength in major muscle groups and participating in weight-bearing physical activity. Based on available evidence at this time, there should not be an expectation among patients with osteoporosis that exercise will have a certain effect on their BMD. We recommend goal-setting that encourages the concept that exercise may help maintain bone mass and discourages the assumption that exercise will increase BMD in osteoporotic individuals.
Notably, preventing the loss of or increasing muscle strength or endurance is a cross-cutting therapeutic target across all of the goals above. Pain control may also be a realistic and relevant goal specific to individuals with prevalent vertebral fractures that may be amenable to exercise. We do not want to de-emphasize the importance of addressing other impairments that may present on an individual level (e.g., neuropathy), particularly as it pertains to safe movement. Clinical reasoning is required to further tailor goal-setting beyond the goals of therapeutic exercise for osteoporosis. Additional goals that were noted during the consensus process, but are not specific to individuals with osteoporosis, include the following:
Maintain or improve cardiovascular fitness;
Aim to achieve or exceed national physical activity guidelines for many health-related benefits including improved quality of life and physical function.
Physical activity and exercise guidelines for individuals with osteoporosis
Physical activity guidelines for older adults have been defined by organizations such as the Canadian Society for Exercise Physiology (CSEP) (http://www.csep.ca/english/view.asp?x=949), the Centers for Disease Control (CDC) (http://www.cdc.gov/physicalactivity/everyone/guidelines/olderadults.html) [19], the Australian Government Department of Health (http://www.health.gov.au/internet/main/publishing.nsf/content/health-pubhlth-strateg-phys-act-guidelines#chba), and the American College of Sports Medicine (ACSM) (http://journals.lww.com/acsm-msse/Fulltext/2009/07000/Exercise_and_Physical_Activity_for_Older_Adults.20.aspx) [20] (Box 1). There was a general consensus that current physical activity guidelines could not be applied to all individuals with osteoporosis or history of vertebral fracture, and that as risk increased, there was less confidence that the guidelines were appropriate (Table 3).
Box 1. Consistent recommendations across physical activity guidelines for older adults (≥65 years) put forward by the American College of Sports Medicine (ACSM), the Center for Disease Control (CDC), and the Canadian Society for Exercise Physiology (CSEP).
Moderate intensity aerobic physical activity of ≥30 min of ≥5 days per week (or 150 min total) OR at least 20 to 60 min of vigorous intensity aerobic physical activity ≥3 days per week (or 75 min total), where bouts should be at least 10 min long;
Exercises to improve balance or prevent falls ≥2 days per week for those who have balance problems or who are frequent fallers;
Resistance/strength training exercises for major muscle groups ≥2 days per week;
Note that ACSM specifies the following:
Very light or light intensity best for older adults or previously sedentary individuals
Aerobic physical activity and resistance training should be between a moderate- (5–6) and vigorous- (7–8) intensity on a scale of 0 to 10. The type of resistance training program should be a progressive weight-training program or weight-bearing calisthenics (8–10 exercises involving the major muscle groups of 8–12 repetitions each), stair climbing, and other strengthening activities that use the major muscle groups
Table 3.
Responses to the question “Do you think that the guidelines detailed above are appropriate for this case?”, presented as a % of total respondents (n=39)
| Moderate risk | High risk (1 vertebral fracture) | High risk (≥1 vertebral fracture, pain, kyphosis) | |
|---|---|---|---|
| Yes | 54 % | 31 % | 23 % |
| No | 36 % | 49 % | 62 % |
| I don’t know | 4 % | 10 % | 22 % |
| Missing | 0 | 10 % | 13 % |
For individuals with osteoporosis based on BMD but no history of vertebral fracture, the guidelines were generally considered appropriate. There was general consensus that current physical activity guidelines are not appropriate for individuals with a history of vertebral fracture, especially in the presence of pain or hyperkyphosis, and alternative recommendations were proposed. Below are detailed exercise recommendations for individuals with osteoporosis; how the recommendations vary in the presence of vertebral fracture is noted. There was a strong emphasis on resistance and balance training, or multicomponent exercise for all individuals with osteoporosis, with or without vertebral fracture (Table 4).
Table 4.
Summary of exercise of physical activity recommendations for individuals with osteoporosis1
| Type | How often per week? | Osteoporosis | Osteoporosis and history of vertebral fracture | Examples and comments |
|---|---|---|---|---|
| Balance training | Daily for ≥15–20 min | Progress from “standing still” exercises” to dynamic Fig. 1. | Can do during daily walks or activities: Standing still: ↓ base of support e.g., Semi-tandem stance, one-leg stand; shift weight between heels & toes while standing Dynamic movements: Tai Chi; tandem walk, dancing |
|
| Strength Training | ≥2 days a week | 8–12 repetitions per exercise. Intensity at 8–12 repetitions maximum2 |
8–12 repetitions per exercise. Aim for 8–12 repetitions maximum2, but form and alignment more important than intensity |
Min. 1 exercise each for: legs; arms; chest; shoulders; back. Use: exercise bands; weights, or body weight against gravity. 1–3 sets/exercise. Train at ↓ intensity initially if: sedentary; conditions affecting activity; high fracture risk; strength training novice |
| Aerobic Exercise | ≥5 days per week, ≥30 min/day | Moderate- to vigorous-intensity | Moderate intensity | Do bouts of 10 min or more – accumulate 30 min/day. On a 0–10 scale where 0=rest, and 10=maximum effort, aim for intensity of 5–8. Moderate: You are breathing heavier than usual. You can have a conversation, but you couldn’t sing. Vigorous: You are breathing much heavier than usual. You would not be able to converse or sing. |
| Spine Sparing | During daily activities | Spine loads supine < standing < seated. Alignment more important than intensity. |
Modify activities that flex (bending forward) or twist the spine; most risky when rapid, repetitive, weighted, bending all the way forward, or twisting to the side. Avoid lifting to or lowering from the floor. | |
| Spinal Extensor Training | Daily for 5–10 min | Emphasis on endurance for back extensors. Perform “holds” 3–5 seconds. | Lie face up on firm surface, knees bent, feet flat. Use pillow only if head doesn’t reach floor. Gently press shoulders into floor, as if they are becoming “heavy” into the ground - hold. Repeat 3–5 times | |
| Activity Recommendations | Apply to ADLs, activities of leisure and exercise | May be able to continue most activities with attention to activity considerations. Avoid high fall risk or contact sports. | The risks of exercise machines, many classes and some ADLs may outweigh benefits. Consult with physical/occupational therapist on safe ADL and activity performance. | Activity considerations: Modify or avoid activities that require repeated, rapid, repetitive, weighted or end-range twisting or flexion of the spine, avoid high fall risk or contact sports. Use hip hinge instead of spinal flexion to bend, and step-to-turn instead of twisting. |
ADL activities of daily living, RM repetitions maximum2
The table summarizes some of the broader recommendations that came out of the consensus process, but was not a product of the consensus process. The table does not thoroughly summarize all recommendations. How the exercise recommendations or physical activity recommendations should be tailored based on case presentation requires clinical judgment. Please refer to the text for a better appreciation of the differences in recommendations between case presentations.
Repetitions maximum (RM) refers to the maximum level of resistance or difficulty for a given exercise that can be performed for the stated number of repetitions, e.g., 1RM squat is the maximum amount of weight you can lift with good form in a squat one time, 8RM bicep curl is the maximum amount of weight you can lift in a bicep curl eight times
Resistance exercise for individuals with osteoporosis
Progressive resistance training for major muscle groups (with the exception of spinal extensors, rotators, and flexors, see next paragraph) should be designed to increase muscle strength, i.e., 8–12 repetitions at an intensity rating of 5–8 on a 0–10 scale (e.g., Borg Rating of Perceived Exertion, see also ““How much weight can I lift during exercise?” (Key points in Box 3)” section), consistent with the ACSM Position Stand on Exercise and Physical Activity for Older Adults [20]. Emphasis should be placed on achieving proper form and spinal alignment. For individuals with a history of vertebral fracture, form, and alignment should be the focus rather than intensity, followed by careful attention to safe progression of intensity (see ““How much weight can I lift during exercise?” (Key points in Box 3)” section). Exercises that are functional, e.g., squat or sit-to-stand and stair climbing, are encouraged.
Box 3. Key points—How Much Weight Can I Lift During Exercise?
General:
Resistance or difficulty should be selected to create an intensity of ~8–12 repetitions maximum, or 5–8 on 0–10 scale (e.g., Borg Rating of Perceived Exertion). Persons previously sedentary, unfamiliar with resistance training, at high fracture risk or with conditions that affect activity participation may need to train at lower intensity, at least initially.
Progressive overload over time is necessary to see improvement.
Avoid making absolute restrictions about amount of weight allowed, instead place emphasis on safe movement recommendations, e.g., use hip hinge (Fig. 1) instead of spine flexion; avoid rapid, repetitive, weighted, or end-range flexion or rotation of the spine; avoid lifting from or lowering to the floor, provide examples using Table 5.
In individuals with a history of vertebral fracture:
A consultation with a therapist with training in exercise prescription for osteoporosis is highly recommended. In the absence of such consultation, it may be advisable to limit resistance exercises to those that use body weight, the floor, or the wall to provide resistance.
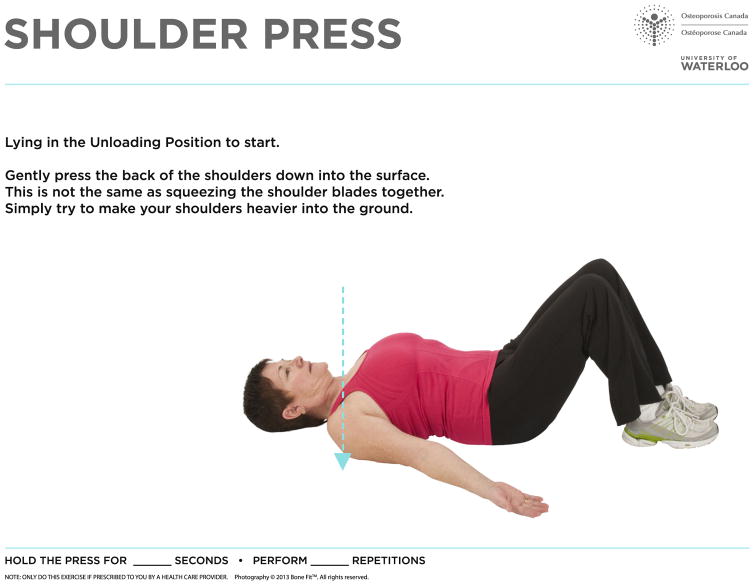
Resistance exercises aimed at increasing muscular endurance in spinal extensors should be performed daily to maintain or improve posture. Endurance is emphasized because the spinal extensors are postural muscles that require endurance. An example protocol for performing isometric holds and suggested progressions are described in Box 2. Individuals with hyperkyphosis may require a pillow to support their head during supine exercise to maintain the spine in neutral alignment. Resistance exercises for the back extensors, or for major muscle groups, should be performed in positions where the spine is least loaded whenever feasible. Loads on the spine are least in supine, followed by prone, standing and then seated, and highest when seated with trunk flexion [21].
Box 2. Example Protocol for Isometric Holds to Train Spinal Extensors and Flexors. Note: the protocol below was not a result of the consensus, it is one example of how to operationalize the recommendations.
Protocol: The target duration for the isometric holds is 5–10 s; to increase the difficulty, increase the number of times the isometric holds are repeated (up to 5), with 3–5 s of rest in between each 5–10 s hold (e.g., perform hold for 5 s, rest 3 s, repeat 3–5 times). To progress the difficulty further, three sets of repeated isometric holds can be performed (e.g., 3–5 holds for 10 s each with 5 s of rest in between, rest 1 min, repeat three times). Spinal extensors should be trained daily. An example that could be performed by a novice is the “Shoulder Press” (Fig. 2). Further progression can be achieved by choosing a more challenging exercise (e.g., add leg press into floor, or arm or leg lengthener, or progress to prone extensions while maintaining a neutral lumbar spine position). If other muscles that support the spine (e.g., trunk flexors, obliques) are being trained, they can also be trained daily, or as advised by an exercise professional with training in osteoporosis. Examples of exercises that can be used include abdominal bracing, progressing to front or side plank on the wall or floor.
Traditional examples of exercises to improve strength/endurance in “core” or “abdominal” muscles involve repeated flexion or rotation of the spine, and individuals with osteoporosis are traditionally told to avoid them. If there is a need to train trunk flexors or rotators to improve core strength, isometric exercises, or holds (e.g., abdominal bracing, front and side planks on wall or floor) are preferable to exercises that involve active trunk flexion or twisting (e.g., curl ups, sit-ups). The protocol in Box 2 could also be used. Exercises to improve endurance of trunk flexors or extensors can be progressed from supine through to standing, to ensure incorporation of correct core activation through functional movements.
Ensuring optimal alignment and avoiding undesirable spinal loading (i.e., application of rapid, repetitive, weighted or end-range flexion, or twisting torque to the spine, or combined loading) during any type of exercise is important. Maintaining the head over the base of the support and increasing lumbar lordosis during standing reduces spinal loading even in the presence of hyperkyphosis in the thoracic spine [22]. To minimize spinal loading during activities requiring bending, it is recommended that the “hip hinge” (Fig. 1) be used: flexing at the hips and knees while bringing the hips posterior to the base of support and maintaining the head over the base of support.
Fig. 1.
Hip hinge for sitting or bending
Balance training to prevent falls
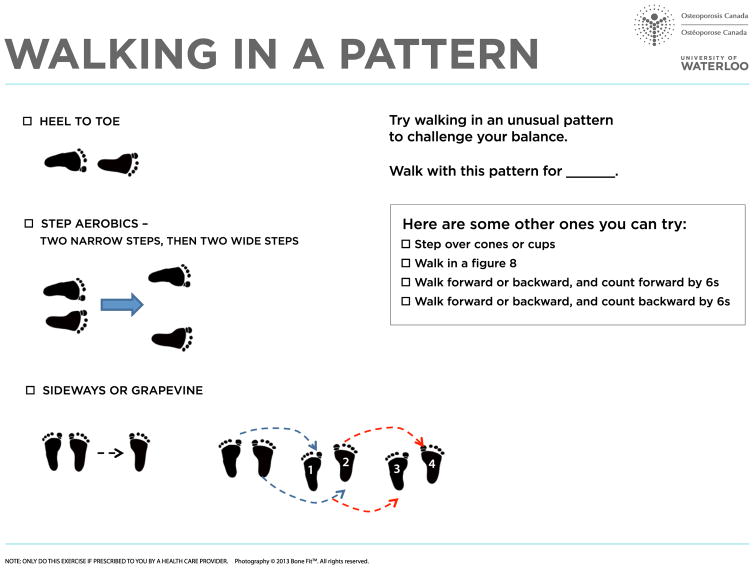
All individuals with osteoporosis, and not just those with balance impairments, should perform challenging balance exercises daily for a minimum of 15–20 min, or for a cumulative time of 2 h per week. Example exercises include those that reduce the base of support in static stance (e.g., semitandem, tandem, or one-legged stand), include a dynamic or three-dimensional balance challenge (e.g., Tai Chi, tandem walk, walking on heels or toes (Fig. 3)), or include other strategies to challenge balance systems (e.g., weight shifting, reduced contact with support objects, dual-tasking, close eyes during static balance challenges). Progression of the balance challenge (e.g., moving to a more difficult exercise, removing vision or contact with support object, or dual-tasking) should occur over time.
Fig. 3.
Walking patterns that could be used to provide a dynamic balance challenge. Individuals with osteoporosis should start with static balance challenges (e.g., semi-tandem stance, one-leg stance) using a support object, and progress to harder challenges, or less reliance on support object, before progressing to dynamic balance challenges
Aerobic physical activity
Individuals with osteoporosis but no history of vertebral fracture should aim to achieve 150 min of moderate- to vigorous-intensity aerobic physical activity per week in bouts of 10 min or more, consistent with current guidelines [19, 23]. The mode of aerobic physical activity should most often include weight-bearing activity (e.g., walking, dancing, or other activities where full body weight is supported by limbs). Individuals with a history of vertebral fracture can also aim to achieve 150 min of moderate-intensity aerobic physical activity per week in bouts of 10 min or more, but vigorous-aerobic physical activity may not be appropriate—several respondents opined that high-intensity aerobic physical activity might increase the risk of falls or fractures.
Shorter, more frequent bouts of moderate-intensity aerobic physical activity (e.g., 10 min at a time, 3 times per day) are acceptable in lieu of 30 min of continuous activity if the patient prefers, or if endurance is low. Choice of aerobic activity needs to be informed by the person’s balance capacity, presence of pain, and ability to maintain proper spinal alignment. Aerobic exercise should not supplant resistance and balance training in individuals with osteoporosis, with or without vertebral fracture.
Other considerations
Individuals with osteoporosis but no history of vertebral fracture should consider pursuing initial instruction on proper form, as well as how to progress the intensity, frequency or duration over time from an exercise professional that has training in exercise prescription for osteoporosis. All exercise programs should incorporate the basic principles of exercise program design (e.g., specificity, overload, progression).
For individuals with osteoporosis and a history of vertebral fracture, a physical therapist consultation is recommended for safe and appropriate exercise prescription and for cues to improve spinal alignment during exercise. Intermittent monitoring and progression should be performed by an exercise professional that has training specific to exercise prescription for individuals with osteoporosis. Guidance on how to minimize future fall and fracture risk may be needed, for example:
how to achieve and maintain good alignment;
how to transition in/out of exercises or use exercise equipment without excessive bending/twisting;
problem-solve strategies to improve safety and adherence to exercise (e.g., recommending indoor walking in inclement weather);
provide instruction on the use of assistive aids to reduce fall risk if balance is impaired.
Exercise or education on positioning for pain control could be considered in the presence of pain at rest or during activity. Examples are the following: sitting in erect alignment with appropriate lumbar spine support, spending time in supine (to encourage spinal extension, and stretching of the pectoral and front shoulder muscles) or prone (to encourage spinal extension and flexibility of the hip flexors).
How to address frequently asked questions posed by individuals with osteoporosis
“How much weight can I lift during exercise?” (Key points in Box 3)
To maintain or improve muscular strength in major muscle groups (with the exception of trunk flexors or extensors), 8–12 repetitions should be performed, and the weight chosen should be a weight where the desired number of repetitions can be performed safely, but the last few repetitions are challenging to do (or 8–12 repetitions maximum). The ASCM recommendations of an intensity of 5–8 on a 0 to 10 scale (e.g., Borg Rating of Perceived Exertion) are appropriate [23], but individuals at high risk of fracture (e.g., with history of vertebral fracture) should prioritize form and alignment over intensity. Individuals who are previously sedentary, with comorbid conditions that affect activity participation, at high fracture risk or unfamiliar with resistance training may need to train at a lower intensity, at least initially. Novices should start with one set of each exercise. Progressive overload over time is necessary to improve muscle strength or endurance; progression can occur in the form of increased repetitions, sets, resistance, or exercise difficulty. Lifting weighted objects from or lowering them to the floor should be avoided—lifting or lowering objects should be performed from/to knee height or higher.
For cases where previous vertebral fractures or pain were present, there was more concern, and less agreement among experts about safety of lifting during exercise or activities of daily living (“Are there daily activities that I normally do that I should not, or that I should do differently?” section). Although some respondents suggested recommending that patients lift no more than 5–10 lbs (2.3–4.6 kg), there was no reason or evidence provided to support that recommendation, and other respondents recommended emphasizing safe movement (or spine-sparing techniques) rather than a particular weight limit. Therefore, we discourage generalizing the recommended weight lifted to a limit of 5–10 lbs (2.3–4.6 kg) across all individuals with osteoporosis, as it suggests that if you avoid lifting more than a set weight, risk is eliminated. Instead, we recommend providing guidance on “spine sparing,” or safe movement—see summary below, Box 3, and Table 4.
A rationale for the recommendations around lifting was developed by members of the expert panel with input from stakeholders in the latter stages of the consensus process. It is not just the amount of weight lifted, but how the weight is lifted that influences future fracture risk. The torque generated is not dependent only on the mass, but on the moment arm, or the distance from the pivot point to the point where the force is applied. For example, carrying a load out in front with elbows bent 90°, or in one hand at the side of the body imposes a greater compressive load on the spine than dividing the weight between two hands and carrying it at one’s sides, close to the body (Box 4) [24, 25]. In the thoracic spine, holding 11 lbs (5 kg) in each hand with elbows flexed to 90° has been reported to increase the compressive loads at T8 and T12, ~ 3.0 and 3.5 times that of standing, respectively [22]. Carrying a load on only one side of the body requires added muscle activation (and therefore greater forces on the spine) to counterbalance the applied load. Bending forward will also increase the compressive and shear loads on the spine (24). Therefore, in theory, a person with a history of spine fractures might be able to hold a given weight safely if the weight is divided between hands held at sides, but not if it is held in front of the body, or while bending forward with it. “Do not lift more than 5 lbs” only works if a patient knows how to move safely with that 5 lbs (2.3 kg).
Box 4. Example recommendation to reduce spinal loading while carrying groceries.
When carrying groceries, there should be approximately equal loads in each hand, with the weight light enough so the spine can be maintained in maximal lengthened erect posture. Lift and lower the bags to a surface at knee or hip height; avoid lifting from or lowering to the floor. If there is a need to turn while carrying them, step to turn rather than twisting the spine.
Factors such as bone strength and posture also influence the safety of lifting. A prospective study reported that the average strength (estimated using finite element analysis) in lumbar vertebrae of men ≥65 years old with and without incident vertebral fractures was 4,320 Newtons (N) (SD1620) and 6,880 N (SD2300), respectively [26]. Similar estimates of vertebral body strength in a case-control study of postmenopausal women reported that estimated vertebral body strength was 4089 N (SD1344) in women with a moderate/severe vertebral deformities and 4,952 N (SD1565) in women with mild deformities, compared to 5,528 N (SD1898) in women with no fractures [27]. Estimating a “factor of risk,” or the ratio of estimated applied forces to the load at which a vertebra fractures (based on BMD, or other estimate of bone strength) might inform the safety of lifting or other activities [21]. However, there are many factors that influence the ability of vertebrae to withstand loads, such as the integrity of the vertebral disks, the presence of microdamage, muscle strength, or spinal curvature [21, 28]. Body position affects spinal loading, with or without weight; spinal loading during standing increases with increasing kyphosis, but can be reduced with an anterior pelvic tilt or increased lumbar lordosis to compensate [22]. Further, the presence of one vertebral fracture results in changes of the angulation of the spinal segments, even in the absence of noticeable changes in thoracic kyphosis [29]. The result is an increase in the moment arm between the vertebrae and the center of mass, which requires greater activation of spinal extensors and therefore an increase in the compressive and shear forces on the spine, even in standing [29]. Shear force profiles are greater in individuals with a history of vertebral fractures in standing, particularly at the upper midthoracic spine and thoracolumbar junction where fractures are particularly common. Shear force profiles would be substantially increased with forward flexion, and further increased if a load was held in the hands in front of the body [29]. Therefore, we recommend less emphasis on recommending maximum weights that can be lifted, and more emphasis on safe movement avoiding weighted flexion (e.g., bending using a hip hinge—Fig. 1, see also “Are there daily activities that I normally do that I should not, or that I should do differently?” section).
Summary of recommendations regarding weight lifted during exercise
Ideally, for individuals with osteoporosis, a consultation with a physical or occupational therapist or exercise professional with specific expertise in exercise therapy for osteoporosis is recommended. In particular, for individuals with a history of vertebral fracture, respondents expressed concern about the initiation of resistance training exercises without consultation of an exercise professional with training in osteoporosis. A consult with a physical or occupational therapist regarding the safety of movements against resistance during work or activities of daily living was also advised (e.g., opening a stuck window, refer to “Are there daily activities that I normally do that I should not, or that I should do differently?” section).
Individuals with osteoporosis can perform resistance training using the guidelines around intensity, or weight, described in Box 3—How much weight can I lift during exercise? When consultation with a therapist is not possible, for patients with a history of spine fracture, it may be advisable to limit resistance exercises to those that use body weight, the floor, or a wall to provide resistance—a conservative approach to maximize safety, but it may reduce the stimulus and resultant effect of the training on muscle strength. All individuals with osteoporosis should be advised to avoid rapid, repetitive, weighted, or end-range (i.e., movement to the end of the range of motion) rotation or flexion of the spine during exercise. Health care providers could consider providing examples of how to move more safely during exercise or activities of daily living (Table 5).
Table 5.
Movements or scenarios that can predispose a person with osteoporosis to fracture, and suggested alternatives to reduce the risk
| Movement | Example activity using the movement | Alternative ways to do it safely if indicated |
|---|---|---|
| End-range trunk flexion* |
|
|
| End-range trunk rotation* |
|
|
| Precarious balancing | Standing on unstable footstool, chair or ladder | Use a step stool with a wide base of support and non-slip materials on the stepping surface and interface with floor. |
| Lifting objects into or lowering from high storage areas |
|
|
| Lifting objects into low storage areas | Placing objects in low cupboards, putting laundry on floor | Avoid lowering or lifting from the floor – store at waist height. Bend with knees and hips not spine, stand close to load when bending, hold load close to body |
| Lifting using maximal strength | Moving furniture | Avoid – get someone else to lift it always |
| Rotation with feet planted | During vacuuming or raking | Step to turn, so that leading foot and torso face same direction |
| Walking or stepping onto slippery surfaces | Wet bathroom or kitchen floor, entryway, pool decks | Wear shoes or slippers with good traction, even in pool areas. Walk slowly, look and take test step before you walk. |
| Twisting or bending in combination with lifting |
|
|
| Transitions – Lying Standing | Getting out of bed | Slide arm out alongside ear, log roll onto side, bend knees 90°. Use other arm to push against bed to upright, place feet on floor, support weight on both hands, scoot bottom to edge of bed, use hip hinge to initiate forward movement and push through lower limbs to stand, using arms only if needed |
| Transitions – Standing Lying | Getting onto floor in supine or prone, or rolling over | Get down one knee at a time with neutral spine. Hip hinge forward to place hand on floor, gentle twist to place bottom on floor. Slide arm closest to floor out onto floor to lie on side, log roll into position |
| Prolonged sitting |
|
|
The table is to be used as an example for individuals for whom the activity and associated alternatives have been deemed acceptable by a health care provider. It is not assumed that all individuals with osteoporosis can use the recommendations in this table and not be at risk of fracture. For example, someone with multiple vertebral fractures and pain may need guidance from a trained health care professional to safely perform many activities here, or may need to avoid them. Refer to “Are there daily activities that I normally do that I shouldn’t, or that I should do differently?” section for recommendations on safe performance of activities of daily living
Of particular concern when loaded (e.g., holding weights, in seated) or resisted
Can I play sports, such as golf or tennis, or do exercise classes such as Pilates or yoga?
There was consensus on recommendations related to sports or exercise classes that could be given to all individuals with osteoporosis or a history of vertebral fractures, with additional recommendations specific to individuals with osteoporotic vertebral fractures.
General recommendations related to sports or other recreational activities
Placing restrictions on activity may be a disincentive to physical activity participation. Many respondents noted that osteoporotic individuals with a history of participating in a sport or activity may have the skill and body awareness to continue it safely, particularly if they are taught spine-sparing techniques, or if modifications can be made. If the patient has a history of certain activities or a strong preference to do an activity, the activity should be encouraged if it can be performed safely, or modified; however, the decision to participate should be made in consultation with a health care provider. Factors that may affect decision-making include the patient’s physical health, functional status, and history of the activity, as well as time since fracture and time on therapy. For those individuals at high risk of fracture who are previously sedentary or unfamiliar with a risky sport or activity, it is advisable not to start them. If guidance on safe movement, spine-sparing techniques or modifications to activities are necessary, a referral to a physical or occupational therapist with training in osteoporosis management is recommended. Any symptoms consistent with fracture (e.g., acute back pain) that become apparent after physical activity warrant follow-up with a health care provider.
Individuals with osteoporosis but no vertebral fractures who have a history of participating in a sport or activity that is considered risky, or a strong desire to do so may be able to participate and should be made aware of the following Activity Considerations:
Activities that involve rapid, repetitive, weighted, or end-range twisting or flexion of the spine (e.g., golf or tennis swing, bending to retrieve balls) may need to be modified (e.g., partial swing, modified golfer’s reach, assistive device). Emphasis should be placed on slower, controlled movements.
Very high-impact sports (e.g., high-impact aerobics or plyometrics) may need to be modified or avoided. An example modification: a lower step height for aerobics.
Activities that have a high fall risk or involve contact (e.g., racquet sports, mountain biking, martial arts, skating, or skiing) may need to be modified so that they reduce injurious contact or are done at a slower pace, or avoided. Individuals with osteoporosis should be informed that fall or fracture risk is higher with fast movements or changes in direction, especially on hard or slippery surfaces, and that they should wear shoes with good traction.
Yoga or Pilates postures that require trunk forward flexion (rotating about the hips or spine) or twisting to end-range, particularly in sitting or standing, should be avoided, or modified. To maintain mobility in the spine, slow, controlled twisting in supine or side-lying is acceptable, as is midrange (but not end-range) spine flexion/extension with some weight supported by upper extremities (e.g., on all fours). There are case reports of spine fractures that may have resulted from yoga flexion postures in individuals with low bone mass [30].
In the presence of one vertebral fracture and osteoporosis, the risks associated with engaging in sports, exercise classes, or exercise machines may outweigh the benefits in some cases. Higher-impact activities (e.g., jumping, jogging, running), or activities with a high risk of falls or contact (e.g., martial arts), or rapid twisting (e.g., golf) may need to be avoided. The health care provider and patient should carefully consider the risks and benefits of a desired activity together, and the available resources to ensure patient safety (e.g., consultation with physical/occupational therapist for ways to modify activity or assistive devices, or attending a class taught by an instructor with training in osteoporosis). If a decision is made that the benefits of a desired activity outweigh the risks, consultation with an exercise professional with training in osteoporosis is recommended. Attention to the principles outlined in the above Activity Considerations is warranted for all activities.
In the presence of multiple vertebral fractures or painful fractures and osteoporosis, the risks of sports, higher-impact activities (e.g., jumping, jogging), and many exercise machines or classes outweigh the benefits. Exercise that is individually tailored by a physical therapist with training in osteoporosis or designed for individuals at high risk of fracture is ideal. To minimize the potential for harm and maximize the benefit, individuals with multiple fractures or painful fractures who wish to participate in physical activity or exercise should choose activities/exercise classes designed for older adults at high risk of fracture, or taught by an exercise instructor who has training on how to modify exercise for individuals with osteoporosis. Emphasis should be placed on slow and controlled movements, and modification or avoidance of activities that involve rapid, repetitive, weighted, or end-range twisting or flexion of the spine, or that have high fall risk.
Are there daily activities that I normally do that I should not, or that I should do differently?
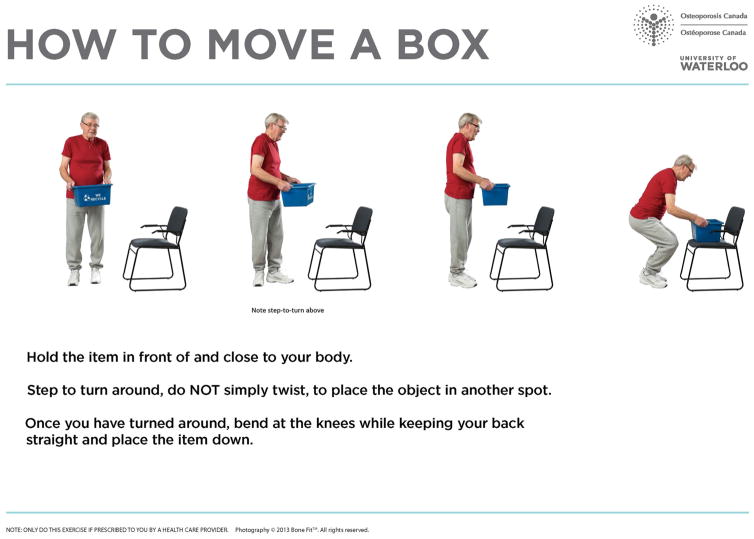
Attention to proper body mechanics is universal in injury prevention, and not specific to osteoporosis. It is more useful to demonstrate how to do a movement/task, or to provide alternatives, than to tell someone not to do a type of movement. Telling a person “do not twist” exemplifies a misunderstanding; twisting is the kinematic variable of creating a twisting motion, but twisting torque can be generated with no motion (e.g., when opening a heavy door). Of greatest concern are activities that involve rapid, weighted, repetitive, or end-range twisting or flexion of the spine, that result in spine postures that deviate from optimal alignment, or that increase fall risk (Table 5). Lifting from or lowering to the floor should be avoided. If lifting from or lowering to knee height or higher is necessary, bending with a “hip hinge” (Fig. 1) can reduce spinal loads when compared to bending with a flexed thoracic and lumbar spine. A “step-to-turn” can be used to modify activities that would have been performed by twisting the spine (Fig. 4). A step-to-turn is when one lifts one foot and steps to the direction one wishes to face, such that the toes and front of the torso move to face the same direction in one movement, rather than twisting the spine. There was consensus that individuals with osteoporosis would benefit from instruction on how to engage in activities of daily living using proper body mechanics. In addition, the presence of vertebral fractures, pain or hyperkyphosis may create the need for specialized assessment and recommendations.
Fig. 4.
An illustration of a step to turn followed by a hip hinge
For individuals with osteoporosis but no history of vertebral fracture
Limited to no restrictions need to be placed on activities of daily living for individuals with low bone mass but no history of vertebral fractures, provided they practice proper body mechanics. Specifically, it may be necessary to modify or avoid high-risk activities, which arguably should be modified or avoided by all people, e.g., lifting/lowering heavy objects to/from overhead or to/from the floor, lifting combined with twisting, performing rapid movements on slippery surfaces or precarious balancing (Table 5). The exception is when impairments in balance or posture, pain, or unsafe movement are evident—in these scenarios, a referral to a physical or occupational therapist for assessment and instruction on safe movement is recommended. Those who perform work-related lifting may need assessment, education, and task modification from a physical or occupational therapist.
For individuals with osteoporosis and a history of vertebral fracture(s)
Consider referring individuals at high risk of fracture to a physical or occupational therapist for evaluation of and instruction on proper body mechanics, and determining whether modifications are needed for activities of daily living, particularly in the presence of impairments in balance or posture, pain, or unsafe movement. It may be necessary to restrict housekeeping to light activities and to get help with activities that may apply flexion or twisting torque to the spine, (e.g., heavy lifting, cleaning gutters, shoveling, or changing light bulbs in ceiling lights). The characteristics of activities that should be avoided include rapid, repetitive, weighted or end-range twisting or flexion of the spine, heavy lifting, lifting overhead, or lifting combined with twisting or forward bending, rapid movements on slippery surfaces or precarious balancing (Table 5).
In the presence of multiple fractures or pain, a consultation with a physical or occupational therapist for instruction on proper body mechanics for activities of daily living is highly recommended, including light activities (e.g., sweeping, getting out of bed, or bathtub/shower). It is important that the patient avoid sitting or standing for long periods of time (e.g., sitting in a car), as it will be uncomfortable. Interspersing prolonged sitting or standing with 5–10-min periods lying in supine will reduce the loads on the spine (Table 5) and promote extension of the spine and stretching of the anterior trunk and shoulder muscles. If a task requires bending such that the head needs to move outside of the base of support, spinal loading forces are increased. For individuals with multiple vertebral fractures, these types of movements should be avoided, but if they cannot be, supporting some of the loading through the arms can reduce spine loading (e.g., if bending to reach an item, placing hands on the thighs to support some body weight).
Areas where lack of consensus may persist
There were three main areas of disagreement that remained after round 2. First, respondents were divided on the amount of emphasis that should be placed on the need for instruction by a trained exercise professional for individuals with osteoporosis. After round 2, some respondents maintained that all individuals with osteoporosis receive assessment and instruction or tailoring of exercise or physical activity, while conversely other respondents indicated that the costs of or access to an exercise professional with the appropriate expertise may make referral of all individuals with osteoporosis unrealistic. To address the lack of consensus, it is proposed that, in general, individuals with osteoporosis would benefit from assessment, tailoring of therapeutic exercise to individual needs and instruction on proper body mechanics during exercise and activities of daily living, and should pursue it if resources are available. However, if health professional resources are scarce, priority should be placed on referring those with pain due to vertebral fracture, impairments in posture or gait, unsafe movement, or comorbid conditions that result in an increased risk of adverse events with exercise or activity. Further, it was noted that not all health care providers have expertise specific to safe movement for people with osteoporosis. The Too Fit To Fracture initiative, and the work of groups such as Osteoporosis Canada or the National Osteoporosis Foundation, are aiming to better educate health care providers. Future knowledge translation efforts could be targeted at the providers of community exercise programs or nonclinician exercise professionals. For example, a “Bone Fit Basic” course was designed by a physical therapist and an expert scientific panel and is delivered by Osteoporosis Canada to fitness instructors; it will be informed by the current work (www.bonefit.ca). A similar course is available in Finland (http://www.ukkinstituutti.fi/tietoa_terveysliikunnasta/liikkumaan/luuliikuntaohjelmat).
Second, some respondents argued that training major muscle groups to improve muscular endurance (i.e., 12–20 repetitions maximum), rather than muscular strength, was sufficient to induce hypertrophy and less risky than the 8–12 repetitions maximum suggested. It was also suggested that resistance training to improve muscular endurance might reduce fall risk and improve balance, with limited benefits for improving BMD in people with osteoporosis. We retained the recommendation supporting a goal of muscular strength, or hypertrophy, for all muscle groups other than spinal extensors (and flexors/rotators) because it is consistent with the language or goals used in the Canadian Physical Activity Guidelines and the ACSM Position Stand on Exercise and Physical Activity for Older Adults [20]. Also, because age-related changes in muscle include a loss of strength and size, and in particular a reduction in fibre area in fast-fatiguing type II fibers [31, 32], our aim is to encourage preservation of muscle size and strength. Training for strength traditionally requires an even higher intensity (i.e., lower repetitions maximum, often 5–8RM) than we or the ACSM prescribe and may not be safe for many older individuals with chronic conditions. Further, although the resistance may be less intense with endurance training, there is more time under tension and repetitive movement. Prolonged repetitions working against resistance may be harmful for individuals who are susceptible to fracture. Training at a 8–12 repetitions maximum intensity can be safely used in older adults with proper attention to body mechanics and alternatives to “weights” for resistance, which is what we encourage. Individuals who are previously sedentary, with comorbid conditions that affect activity participation, at high fracture risk or unfamiliar with resistance training may need to train at a lower intensity, at least initially.
In contrast to the area of disagreement above, some respondents argued that spinal extensors should be trained to increase strength rather than endurance. Indeed, studies evaluating strength training for spinal extensors in women with osteoporosis, with target ranges of 8–12 repetitions maximum, have demonstrated improvements in muscle strength in spinal extensors, while improvements in trunk and arm endurance have been observed after training using isometric holds [33]. The absence of conclusive evidence supporting strength over endurance training for spinal extensors (or vice versa) to improve posture or reduce fracture risk in individuals with osteoporosis precludes any definitive statement about which is better. Our emphasis on training spinal extensors for muscular endurance was based on the function of the muscles, in that they are required to have endurance to maintain posture for prolonged periods, rather than work against resistance at high intensity. Erector spinae are composed of a greater proportion of type I than type II fibers [34]. However, it is possible that strength training will result in improved endurance and vice versa. Regardless of the therapeutic goal, we emphasized isometric holds in a neutral spine position, or trunk extension to neutral (avoiding hyperextension), rather than repeated movements throughout the range of motion against resistance.
Although the majority of respondents agreed that trunk extension exercises are recommended for individuals with osteoporosis or vertebral compression fractures, there was no detailed discussion or consensus on exactly which type of trunk extension exercise is the safest and most effective. Indeed, although we have emphasized a supine exercise as a starting point in Box 2, progressive resisted trunk extension exercises done in prone lying or in standing have been used for muscle strengthening or endurance training in individuals with osteoporosis and vertebral fractures [35–37], and some respondents suggested that they be recommended. There were respondents that expressed concern that prone trunk extension exercises beyond a neutral spine position (i.e., hyperextension) placed unnecessary compression on the posterior elements of the spinal vertebrae. However, prone trunk extensions can be performed over pillows or a bolster, while maintaining a neutral lumbar spine position and aiming for extension through a small range of motion in the thoracic region. Two fractures related to prone exercise in women with spine fractures have been reported; one a costal cartilage avulsion during a prone unilateral arm lift and another a rib fracture when rolling supine to prone [35], reinforcing the need to ensure optimal alignment and prevent undesirable spinal loading during both exercise and during transitions into and out of positions. Trunk extension exercises can also be performed with a neutral spine against a wall in standing, or in a quadruped position, using arm raises to target thoracic extensors (with weight of arm or addition of resistance bands to progress the trunk extensor muscle work). Training core muscles in standing allows for the correction of habitual movement patterns used in daily activities involving reaching overhead. Additional considerations include the presence of impairments (e.g., hyperkyphosis, spinal stenosis, knee pain, wrist/hand pain, impaired balance) that might limit the capacity to assume a supine, prone or quadruped position, the props or equipment to be used (e.g., pillows, resistance bands) or the need to perform prone/supine lying for pain relief in addition to exercise. For example, some older adults may find it easier to get into supine or prone on a bed than getting onto the floor, or into a quadruped position. Quadruped arm and leg lifts allow training of the thoracic and lumbar extensors in a neutral spine position, but require sufficient trunk and balance control to prevent twisting or teetering that might increase the risk of unfavorable spinal loading. Few trials evaluating the efficacy of exercise in individuals with vertebral fractures exist; so, we conclude that we advocate for progressive resistance training of the trunk extensors for individuals with osteoporosis or vertebral compression fractures, and it may be premature to establish consensus on the exact type of trunk extension exercise that is safest or most effective.
Summary and conclusions
Current physical activity guidelines may not be appropriate or address the needs of individuals with osteoporosis. Our consensus process provides recommendations for health care providers on assessment and goal setting to inform exercise or physical activity prescription for individuals with osteoporosis, as well as how to adapt current physical activity guidelines for those at moderate or high risk of fracture, and how to address a few commonly asked questions by patients. Key messages include the following: emphasis on multicomponent exercise that includes resistance and balance training, emphasis on training balance and spinal extensors daily, and guidance on safe movement and how to empower patients to find ways to do activities that they have a strong desire to do, rather than provide broad restrictions. We are partnering with Osteoporosis Canada to disseminate the recommendations in the Bone Fit workshop for physiotherapists and kinesiologists (http://www.bonefit.ca/), and to develop tools for patients and health care providers. Future research should examine the efficacy of the recommendations for improving patient-important outcomes, or the utility of knowledge translation activities for changing practice related to exercise and physical activity in individuals with osteoporosis.
Limitations and future directions
Our patient frequently asked questions were derived from Canadian patients, with input from clinicians from four countries on our expert panel, so they may not present a global perspective. We did not address the optimal methods for helping people integrate the recommended exercises or activities into their lifestyle, although examples exist [38].
In future, we wish to develop the recommendations into user-friendly summaries and tools that could be used for knowledge translation. The Too Fit To Fracture initiative has also developed priorities for future research to advance the field [8].
Fig. 2.
Shoulder press: an example of an exercise for training spinal extensor endurance
Acknowledgments
This work was completed in partnership with Osteoporosis Canada: Contributions include participation from members of the Scientific Advisory Council and the Bone Fit Development Committee, input from the Canadian Osteoporosis Patient Network, and financial support. We would like to acknowledge financial support from the University of Waterloo. The International Osteoporosis Foundation was a participating stakeholder and provided feedback on the report. The recommendations were reviewed and endorsed by the National Osteoporosis Foundation. Dr. Harri Sievanen and Dr. Maarit Piirtola reviewed the report on behalf of the Finnish Osteoporosis Association, and also contributed at all stages of the consensus process. Osteoporosis Australia’s Medical and Scientific Advisory Committee reviewed the report at several stages and contributed to the final recommendations. We thank Dr. Andrew Briggs from Arthritis and Osteoporosis Victoria, Dr. Cathie Sherrington and Dr. Raymond Lee for their review of and feedback on the manuscript. We would like to thank Cheryl Kieswetter, Eric Bowman, and Michael McLeod for their assistance with the consensus process. Dr. Giangregorio is a recipient of a Canadian Institutes of Health Research (CIHR) New Investigator Award and an Early Researcher Award from the Ontario Ministry of Research and Innovation. Dr. Ashe has received career awards from CIHR and the Michael Smith Foundation for Health Research. Dr. Papaioannou is the Scientific Director for the Geriatric Education and Research in Aging Sciences (GERAS) Centre at St. Peter’s Hospital. She is the CIHR and Eli Lilly Research Chair in Osteoporosis. Dr. Cheung is supported by a CIHR Senior Investigator Award. Dr. Papaioannou is a CIHR- Eli Lilly Canada Research Chair. We would like to acknowledge funding from the Hallman Undergraduate Research Fellowship.
Footnotes
According to FRAX and Canadian Association of Radiologists and Osteoporosis Canada criteria.
Reader should consult clinical practice guidelines adopted by their country for recommended risk calculator. Example risk calculators available online include the FRAX risk calculator (http://www.shef.ac.uk/FRAX/), CAROC risk calculator (http://www.osteoporosis.ca/health-care-professionals/clinical-tools-and-resources/fracture-risk-tool/), Garvan Risk Calculator (http://garvan.org.au/promotions/bone-fracture-risk/calculator/)
A fall is defined as an event which results in a person coming to rest inadvertently on the ground or floor or other lower level (http://www.who.int/mediacentre/factsheets/fs344/en/).
The consensus process did not extend to a consensus on the type of assessments to be used for falls or physical function, only the domains to be assessed. The AGS/BGS Guidelines include more detailed suggestions regarding assessment of fall risk and physical function for fall prevention. However, some domains that may inform exercise prescription (e.g., aerobic capacity, strength) may not be adequately represented in the AGS/BGS guidelines—http://www.americangeriatrics.org/health_care_professionals/clinical_practice/clinical_guidelines_recommendations/prevention_of_falls_summary_of_recommendations. The cut points that have been used to define slow gait speed as it pertains to predicting adverse health outcomes or mortality vary from <0.8 to <1.0 m/s [15, 16].
Conflicts of interest: A. Papaioannou is or has been a consultant, or on a speaker's bureau for, or received unrestricted grants from the following: Amgen, Eli Lilly, Merck Canada Inc., Novartis, Pfizer, Warner Chilcott. L. Giangregorio has received one grant from Merck Canada Inc. that is unrelated to the current work and has consulted for Eli Lilly. McGill S, Wark JD, Laprade J, Heinonen A, Ashe MC,MacIntyre NJ, Cheung AM, Shipp K, Keller H, and Jain R state that they have no conflicts of interest.
Contributor Information
L. M. Giangregorio, Department of Kinesiology, University of Waterloo, 200 University Ave W, Waterloo, ON N2L 3G1, Canada. Toronto Rehabilitation Institute–University Health Network, Toronto, Canada. Schlegel-University of Waterloo Research Institute for Aging, Waterloo, Canada
S. McGill, Department of Kinesiology, University of Waterloo, 200 University Ave W, Waterloo, ON N2L 3G1, Canada
J. D. Wark, Royal Melbourne Hospital Department of Medicine, University of Melbourne, Parkville, Australia
J. Laprade, Division of Anatomy, University of Toronto, Toronto, Canada. Ontario Osteoporosis Strategy and Osteoporosis Canada, Ontario, Canada
A. Heinonen, Department of Physiotherapy, Health Sciences, University of Jyvaskyla, Jyvaskyla, Finland
M. C. Ashe, Department of Family Practice and Centre for Hip Health and Mobility, University of British Columbia, Vancouver, Canada
N. J. MacIntyre, School of Rehabilitation Science, McMaster University, Hamilton, Canada
A. M. Cheung, Department of Medicine, University of Toronto, Toronto, Canada
K. Shipp, Department of Community and Family Medicine, Duke University, Durham, USA
H. Keller, Department of Kinesiology, University of Waterloo, 200 University Ave W, Waterloo, ON N2L 3G1, Canada. Schlegel-University of Waterloo Research Institute for Aging, Waterloo, Canada
R. Jain, Ontario Osteoporosis Strategy and Osteoporosis Canada, Ontario, Canada
A. Papaioannou, Department of Medicine, McMaster University and The Geriatric Education and Research in Aging Sciences (GERAS), Centre at St. Peter’s Hospital, Hamilton, Canada
References
- 1.Ioannidis G, Papaioannou A, Hopman WM, Akhtar-Danesh N, Anastassiades T, Pickard L, et al. Relation between fractures and mortality: results from the Canadian Multicentre Osteoporosis Study. CMAJ. 2009;181(5):265–271. doi: 10.1503/cmaj.081720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lindsay R, Silverman SL, Cooper C, Hanley DA, Barton I, Broy SB, et al. Risk of new vertebral fracture in the year following a fracture. JAMA. 2001;285(3):320–323. doi: 10.1001/jama.285.3.320. [DOI] [PubMed] [Google Scholar]
- 3.Cauley JA, Thompson DE, Ensrud KC, Scott JC, Black D. Risk of mortality following clinical fractures. Osteoporos Int. 2000;11(7):556–561. doi: 10.1007/s001980070075. [DOI] [PubMed] [Google Scholar]
- 4.Giangregorio Lora M, MacIntyre N, Thabane L, Cranney A, Cook R, Papaioannou A. Exercise for improving outcomes after osteoporotic vertebral fracture. 2010;(7) doi: 10.1002/14651858.CD008618.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giangregorio LM, Papaioannou A, MacIntyre NJ, Ashe MC, Heinonen A, Shipp K, et al. Too Fit To Fracture: exercise recommendations for individuals with osteoporosis or osteoporotic vertebral fracture. Osteoporos Int. 2014;25(3):821–835. doi: 10.1007/s00198-013-2523-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–131. [PMC free article] [PubMed] [Google Scholar]
- 7.Fitch K, Bernstein S, Aguilar MD, Burnand B, LaCalle JR, Lazaro P, et al. The RAND/UCLA appropriateness method user’s manual. RAND Corporation; Santa Monica: 2001. [Google Scholar]
- 8.Giangregorio LM, MacIntyre NJ, Heinonen A, Cheung AM, Wark JD, Shipp K, McGill S, Ashe MC, Laprade J, Jain R, Keller H, Papaioannou A. Too Fit To Fracture: a consensus on future research priorities in osteoporosis and exercise. Osteoporos Int. 2014 doi: 10.1007/s00198-014-2652-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Papaioannou A, Morin S, Cheung AM, Atkinson S, Brown JP, Feldman S, et al. 2010 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ. 2010;182(17):1864–1873. doi: 10.1503/cmaj.100771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 12.Giangregorio LM, Ashe MC, Shipp K, Cheung AM, Heinonen A, Papaioannou A, et al. “Is this exercise safe?”: building consensus around responses to common questions about physical activity posed by people with osteoporosis. J Bone Miner Res 2014 [Google Scholar]
- 13.Giangregorio LM, Papaioannou A, MacIntyre NJ, Ashe MC, Heinonen A, Shipp K, et al. Too Fit To Fracture: exercise recommendations for individuals with osteoporosis or osteoporotic vertebral fracture. Osteoporos Int. 2014;25(3):821–835. doi: 10.1007/s00198-013-2523-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kenny RA, Rubenstein LZ, Tinetti ME, Brewer K, Cameron KA, Capezuti EA, et al. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148–157. doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- 15.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4):412–423. doi: 10.1093/ageing/afq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE, Newman AB, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011;12(4):249–256. doi: 10.1016/j.jamda.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Greendale GA, Nili NS, Huang MH, Seeger L, Karlamangla AS. The reliability and validity of three non-radiological measures of thoracic kyphosis and their relations to the standing radiological Cobb angle. Osteoporos Int. 2010 doi: 10.1007/s00198-010-1422-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Macintyre NJ, Stavness CL, Adachi JD. The safe functional motion test is reliable for assessment of functional movements in individuals at risk for osteoporotic fracture. Clin Rheumatol. 2011;29(2):143–150. doi: 10.1007/s10067-009-1297-6. [DOI] [PubMed] [Google Scholar]
- 19.Centres for Disease Control. How much physical activity do older adults need? Centres Dis Control; Sep 1, 2014. [Google Scholar]
- 20.Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, Minson CT, Nigg CR, Salem GJ, et al. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41(7):1510–1530. doi: 10.1249/MSS.0b013e3181a0c95c. [DOI] [PubMed] [Google Scholar]
- 21.Myers ER, Wilson SE. Biomechanics of osteoporosis and vertebral fracture. Spine (Phila Pa 1976) 1997;22(24 Suppl):25S–31S. doi: 10.1097/00007632-199712151-00005. [DOI] [PubMed] [Google Scholar]
- 22.Bruno AG, Anderson DE, D’Agostino J, Bouxsein ML. The effect of thoracic kyphosis and sagittal plane alignment on vertebral compressive loading. J Bone Miner Res. 2012;27(10):2144–2151. doi: 10.1002/jbmr.1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chodzko-Zajko W, Proctor D, Fiatarone Singh M, Minson C, Nigg C, Salem G, et al. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41(7):1510–1530. doi: 10.1249/MSS.0b013e3181a0c95c. [DOI] [PubMed] [Google Scholar]
- 24.McGill SM, Marshall L, Andersen J. Low back loads while walking and carrying: comparing the load carried in one hand or in both hands. Ergonomics. 2013;56(2):293–302. doi: 10.1080/00140139.2012.752528. [DOI] [PubMed] [Google Scholar]
- 25.Iyer S, Christiansen BA, Roberts BJ, Valentine MJ, Manoharan RK, Bouxsein ML. A biomechanical model for estimating loads on thoracic and lumbar vertebrae. Clin Biomech (Bristol, Avon) 2010;25(9):853–858. doi: 10.1016/j.clinbiomech.2010.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang X, Sanyal A, Cawthon PM, Palermo L, Jekir M, Christensen J, et al. Prediction of new clinical vertebral fractures in elderly men using finite element analysis of CT scans. J Bone Miner Res. 2012;27(4):808–816. doi: 10.1002/jbmr.1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Melton LJ, III, Riggs BL, Keaveny TM, Achenbach SJ, Kopperdahl D, Camp JJ, et al. Relation of vertebral deformities to bone density, structure, and strength. J Bone Miner Res. 2010;25(9):1922–1930. doi: 10.1002/jbmr.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brinckmann P, Biggemann M, Hilweg D. Prediction of the compressive strength of human lumbar vertebrae. Clin Biomech (Bristol, Avon) 1989;4(Suppl 2):iii–27. doi: 10.1016/0268-0033(89)90071-5. [DOI] [PubMed] [Google Scholar]
- 29.Briggs AM, Wrigley TV, van Dieen JH, Phillips B, Lo SK, Greig AM, et al. The effect of osteoporotic vertebral fracture on predicted spinal loads in vivo. Eur Spine J. 2006;15(12):1785–1795. doi: 10.1007/s00586-006-0158-0. [DOI] [PubMed] [Google Scholar]
- 30.Sinaki M. Yoga spinal flexion positions and vertebral compression fracture in osteopenia or osteoporosis of spine: case series. Pain Pract. 2013;13(1):68–75. doi: 10.1111/j.1533-2500.2012.00545.x. [DOI] [PubMed] [Google Scholar]
- 31.Lexell J, Taylor CC, Sjostrom M. What is the cause of the ageing atrophy? Total number, size and proportion of different fiber types studied in whole vastus lateralis muscle from 15- to 83-year-old men. J Neurol Sci. 1988;84(2–3):275–294. doi: 10.1016/0022-510x(88)90132-3. [DOI] [PubMed] [Google Scholar]
- 32.Porter MM, Vandervoort AA, Lexell J. Aging of human muscle: structure, function and adaptability. Scand J Med Sci Sports. 1995;5(3):129–142. doi: 10.1111/j.1600-0838.1995.tb00026.x. [DOI] [PubMed] [Google Scholar]
- 33.Giangregorio LM, Macintyre NJ, Thabane L, Skidmore CJ, Papaioannou A. Exercise for improving outcomes after osteoporotic vertebral fracture. Cochrane Database Syst Rev. 2013;1:CD008618. doi: 10.1002/14651858.CD008618.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mannion AF, Dumas GA, Cooper RG, Espinosa FJ, Faris MW, Stevenson JM. Muscle fibre size and type distribution in thoracic and lumbar regions of erector spinae in healthy subjects without low back pain: normal values and sex differences. J Anat. 1997;190(Pt 4):505–513. doi: 10.1046/j.1469-7580.1997.19040505.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gold DT, Shipp KM, Pieper CF, Duncan PW, Martinez S, Lyles KW. Group treatment improves trunk strength and psychological status in older women with vertebral fractures: results of a randomized, clinical trial. J Am Geriatr Soc. 2004;52(9):1471–1478. doi: 10.1111/j.1532-5415.2004.52409.x. [DOI] [PubMed] [Google Scholar]
- 36.Sinaki M, Itoi E, Wahner HW, Wollan P, Gelzcer R, Mullan BP, et al. Stronger back muscles reduce the incidence of vertebral fractures: a prospective 10 year follow-up of postmenopausal women. Bone. 2002;30(6):836–841. doi: 10.1016/s8756-3282(02)00739-1. [DOI] [PubMed] [Google Scholar]
- 37.Hongo M, Itoi E, Sinaki M, Miyakoshi N, Shimada Y, Maekawa S, et al. Effect of low-intensity back exercise on quality of life and back extensor strength in patients with osteoporosis: a randomized controlled trial. Osteoporos Int. 2007;18(10):1389–1395. doi: 10.1007/s00198-007-0398-9. [DOI] [PubMed] [Google Scholar]
- 38.Clemson L, Fiatarone Singh MA, Bundy A, Cumming RG, Manollaras K, O’Loughlin P, et al. Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): randomised parallel trial. BMJ. 2012;345:e4547. doi: 10.1136/bmj.e4547. [DOI] [PMC free article] [PubMed] [Google Scholar]