Abstract
Background
The complexity of health information often exceeds patients’ skills to understand and use it.
Objective
To develop survey items assessing how well healthcare providers communicate health information.
Methods
Domains and items for the Consumer Assessment of Healthcare Providers and Systems (CAHPS)® Item Set for Addressing Health Literacy were identified through an environmental scan and input from stakeholders. The draft item set was translated into Spanish and pretested in both English and Spanish. The revised item set was field tested with a randomly selected sample of adult patients from 2 sites using mail and telephonic data collection. Item-scale correlations, confirmatory factor analysis, and internal consistency reliability estimates were estimated to assess how well the survey items performed and identify composite measures. Finally, we regressed the CAHPS global rating of the provider item on the CAHPS core communication composite and the new health literacy composites.
Results
A total of 601 completed surveys were obtained (52% response rate). Two composite measures were identified: (1) Communication to Improve Health Literacy (16 items); and (2) How Well Providers Communicate About Medicines (6 items). These 2 composites were significantly uniquely associated with the global rating of the provider (communication to improve health literacy: P<0.001, b = 0.28; and communication about medicines composite: P = 0.02, b = 0.04). The 2 composites and the CAHPS core communication composite accounted for 51% of the variance in the global rating of the provider. A 5-item subset of the Communication to Improve Health Literacy composite accounted for 90% of the variance of the original 16-item composite.
Conclusions
This study provides support for reliability and validity of the CAHPS Item Set for Addressing Health Literacy. These items can serve to assess whether healthcare providers have communicated effectively with their patients and as a tool for quality improvement.
Keywords: health literacy, CAHPS, patient survey, communication
Health literacy is the capacity to obtain, communicate, process, and understand basic health information and services to make health decisions.1 A nationally representative assessment of English literacy among American adults aged 16 and older estimated that only 12% of US adults have proficient health literacy.2 Over a third of US adults (77 million) have difficulty with common health tasks, such as following directions on a prescription drug label or adhering to a childhood immunization schedule using a standard chart.3
The complexity of health information and the communication skills of healthcare providers affect patient understanding.4,5 Reducing health literacy demands has recently emerged as a national health priority6,7 and provider-patient communication objectives are included in the national health promotion and disease prevention program Healthy People 2020.8 Although health literacy has long been recognized as an important healthcare issue,9-12 attention has now turned to health care providers’ role in improving patient understanding.
The Consumer Assessment of Healthcare Providers and Systems (CAHPS)® Clinician and Group 12-month survey includes a question that asks, “How often does your provider explain things in a way that was easy to understand?” Responses to this item, however, do not indicate which aspects of communication are problematic or how providers and their practices can improve the quality of their communications. The CAHPS Item Set for Addressing Health Literacy was developed as both a measure of whether healthcare providers have succeeded in reducing the health literacy demands they place on patients, and as a tool for quality improvement.
METHODS
Item Development
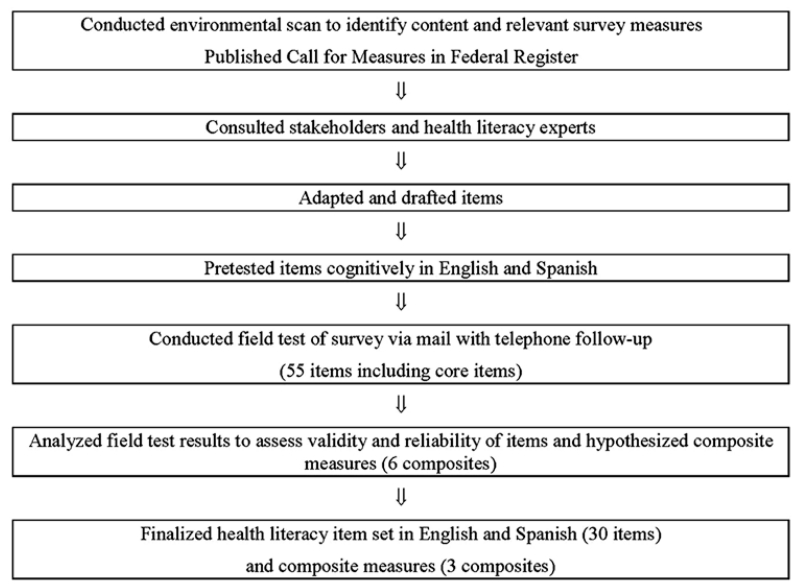
We followed the standard CAHPS approach for developing surveys (Fig. 1). We conducted an environmental scan to identify domains of interest and relevant survey items. A Call for Measures was issued in the Federal Register to obtain additional measures, but few responses were submitted and no additional measures were obtained. We interviewed health literacy experts and held stakeholder meetings—including representatives from government agencies, healthcare providers, health literacy experts and advocates, and consumers—to prioritize the domains the item set should cover and learn about other potential sources of survey items. We mapped the survey items that we collected to the domains, and modified or adapted measures in the public domain to make them “CAHPS-like.” We drafted new survey items for the domains for which we were unable to identify appropriate existing items.
FIGURE 1.
Overview of survey development and testing approach.
Translation
We translated the health literacy items into Spanish using the CAHPS guidelines for translation13 to produce a Spanish version that was conceptually equivalent to the English, easy to understand, and understood by Spanish speakers from different countries. The CAHPS approach involves 2 forward translations and then a bilingual committee review to resolve translation issues by consensus. The translators and bilingual reviewers that participated in producing the Spanish version were selected using the CAHPS guidelines for selecting translators and reviewers.14 In recent years, the translation by committee approach used has been shown to yield superior translations and has come to be seen as the recommended approach.15-17
Cognitive Interviews
Cognitive interviewing is a technique used to evaluate how survey respondents understand, mentally process, and respond to survey items and to use this information to modify and refine survey measures.18,19 This approach has been used routinely to evaluate CAHPS surveys in both English and Spanish.20-22 We conducted 2 rounds of cognitive interviews in both English and Spanish. We recruited interviewees that represented a mix of participants in terms of sex, race/ethnicity, insurance status, country of origin, and educational level, with the majority of respondents having <12 years of schooling.
Field Testing
We integrated the health literacy items, into the CAHPS Clinician and Group 12-month survey, interspersing the health literacy items among the core survey items. Table 1 shows the 30 health literacy items that were field-tested.
TABLE 1.
CAHPS Health Literacy Supplemental Item Set for Ambulatory Care (Field Test Version) Hypothesized Multi-Item Composites
| Survey Items | Response Format | |
|---|---|---|
| Patient/provider communication (in the last 12 mo) | ||
| #8 | How often did this provider interrupt you when you were talking? | N/AN/S/U/AA/A |
| #9 | How often did this provider talk too fast when talking with you? | N/AN/S/U/AA/A |
| #10 | How often did this provider use medical words you did not understand? | N/AN/S/U/AA/A |
| #11 | Were any of the explanations this provider gave you hard to understand because of an accent or the way the provider spoke English? |
Yes, definitely/Yes, somewhat/No |
| #12 | Did you feel this provider really cared about you as a person? | Yes, definitely/Yes, somewhat/No |
| #13 | Did this provider ignore what you told him or her? | Yes, definitely/Yes, somewhat/No |
| #14 | Did this provider use a condescending, sarcastic, or rude tone or manner with you? | Yes, definitely/Yes, somewhat/No |
| #15 | Did this provider show interest in your questions and concerns? | Yes, definitely/Yes, somewhat/No |
| #17 | How often did this provider answer all your questions to your satisfaction? | N/AN/S/U/AA/A |
| #18 | How often did this provider give you all the information you wanted about your health? |
N/AN/S/U/AA/A |
| Communication about health problems or concerns (in the last 12 mo) | ||
| #19 | Did this provider encourage you to talk about all your health problems or concerns? |
Yes, definitely/Yes, somewhat/No |
| #21 | How often did this provider give you easy to understand instructions about taking care of these health problems or concerns? |
N/AN/S/U/AA/A |
| Disease self-management (in the last 12 mo) | ||
| #23 | How often did this provider give you easy to understand instructions about what to do to take care of this illness or health condition? |
N/AN/S/U/AA/A |
| #24 | How often did this provider ask you to repeat back or describe how you were going to follow the doctor’s instructions? |
N/AN/S/U/AA/A |
| #25 | Sometimes doctors give instructions that are hard to follow. How often did this provider ask you whether you would have any problems doing what you need to do to take care of this illness or health condition? |
N/AN/S/U/AA/A |
| #26 | How often did this provider explain what to do if this illness or health condition got worse or came back? |
N/AN/S/U/AA/A |
| #27 | How often did this provider use pictures, drawings, or models to explain things to you? |
N/AN/S/U/AA/A |
| Communication about medicines (In the last 12 mo) | ||
| #29 | How often did this provider give you easy to understand instructions about how to take your medicines? |
N/AN/S/U/AA/A |
| #30 | Did this provider explain the possible side effects of your medicines? | Yes/No |
| #31 | How often did this provider explain the possible side effects of your medicines in a way that was easy for you to understand? |
N/AN/S/U/AA/A |
| #32 | Other than a prescription, did this provider give you written information or write down information about how to take your medicines? |
Yes/No |
| #33 | How often was the written information you were given easy to understand? | N/AN/S/U/AA/A |
| #34 | How often did this provider suggest ways to help you remember to take your medicines? |
N/AN/S/U/AA/A |
| Communication about test results (in the last 12 mo) | ||
| #36 | When this provider ordered a blood test, x-ray, or other test for you, how often did someone from this doctor’s office follow up to give you those results? |
N/AN/S/U/AA/A |
| #37 | How often were the results of your blood test, x-ray, or other test easy to understand? |
N/AN/S/U/AA/A |
| Communication about forms (in the last 12 mo) | ||
| #40 | How often did someone explain the purpose of a form before you signed it? | N/AN/S/U/AA/A |
| #41 | How often were you offered help in filling out a form at this doctor’s office? | N/AN/S/U/AA/A |
| #42 | How often were the forms that you got at this doctor’s office easy to fill out? | N/AN/S/U/AA/A |
| #43 | How often were the forms that you had to fill out available in Spanish? | N/AN/S/U/AA/A |
Item numbers refer to the numbering used in the field test version of the survey.
Item 43 was only included in the Spanish version of the survey.
CAHPS indicates Consumer Assessment of Healthcare Providers and Systems; N/AN/S/U/AA/A = Never/Almost never/Sometimes/Usually/Almost always/Always.
Two sites participated in the field test: a health plan located in New York City and an outpatient clinic based in an academic medical center in the southern United States. In recruiting field test partners, we targeted sites that would provide racial and ethnic diversity, sufficient numbers of Spanish speakers, and patients with limited health literacy skills. Both the health plan and the clinic provide free or low-cost health coverage to patients on Medicaid or who have no insurance at all and serve a largely low-income, minority population.
The sample frame for the field test included 1200 randomly selected adult patients who had at least 1 outpatient visit in the prior 12 months (600 per site). We used a combination of mail and phone survey administration, which involved a notification letter, 2 survey mailings, a reminder letter, and multiple follow-up phone calls to nonrespondents. To maximize response rates among Spanish speakers, Hispanic respondents were mailed materials in both English and Spanish. Respondents who completed a survey were mailed a thank you letter with a check for $10.
Composite Development
One of the goals of the field test was to assess whether reliable and valid composites could be constructed. A composite is composed of ≥ 2 survey items that are closely related conceptually and statistically. Composites are useful for both internal and public reporting of survey results because they summarize a large amount of data in a concise manner.23 Analyses were conducted to estimate the reliability and validity of the composites.24,25
As shown in Table 1, we placed health literacy items that were conceptually related into 6 groupings (multi-item composites): (1) patient/provider communication (10 items); (2) communication about health problems or concerns (2 items); (3) disease self-management (6 items); (4) communication about medicines (6 items); (5) communication about test results (2 items); and (6) communication about forms (3 items in English and 4 items in Spanish). We then ran tests of these 6 hypothesized composites to see whether the items in each “hung” together and could therefore be scored as a composite. The cutoff for inclusion of an item in a composite measure was an item-rest correlation of ≥ 0.30. We also examined the correlation of each item to the composite it was not hypothesized to represent to assess whether the composites represent statistically unique aspects of communication to improve health literacy. Through an iterative process, we revised the placement of items into composites, taking into account correlations between the items and item content, and reran the correlation analysis to assess the fit of each individual item into the composite it was hypothesized to represent. We also conducted categorical confirmatory factor analysis in Mplus26 to assess the fit of the composite structure. In addition, we identified a short subset of items from a final 16-item composite (Communication to Improve Health Literacy) by regressing the composite score on the items in it to identify the subset of items that accounted for most of the variance in this composite. We used a maximum R2 forward selection procedure (MaxR option in SAS PROC REG) that tests the effects of switching different combinations of items on the total amount of variance explained. Our goal was to identify a subset of items that accounted for 90% of the variance in the 16-item composite score.
We also wanted to check that the health literacy composites had an effect on global ratings of the provider distinct from the effect of an existing communication composite comprised of 5 items from the CAHPS Clinician and Group survey. We therefore regressed the global rating of provider item (0–10 rating where 0 = worse possible provider and 10= best possible provider) on the new composites and the CAHPS core communication composite.
RESULTS
Field Test Response
We obtained 601 completed surveys for a response rate of 52%. Overall, more surveys were completed in English (79%) than Spanish (21%) and more surveys were completed by mail (65%) than by phone (35%). Similar response rates were obtained from each field test site (51% and 53%).
Table 2 shows the demographic characteristics of survey respondents. Blacks were the largest racial group (45% as compared with 21% each for whites and other). Hispanics constituted 39% of respondents. Most respondents were female (80%) and 61% of the sample was 45 years or older. A significant proportion of respondents (36%) had less than a high school education, 24% graduated high school or obtained a general educational development, 26% had some college, and 12% had more than a college degree. Forty-two percent reported that their health was fair or poor. Demographic characteristics were not available for those that did not respond to the survey; therefore nonresponse bias could not be estimated.
TABLE 2.
Demographic Characteristics of Clinician and Group Health Literacy Sample (N = 601)
| Questions | Response | Percentage |
|---|---|---|
| Self-rated overall health | Excellent | 8.9 |
| Very good | 16.3 | |
| Good | 30.5 | |
| Fair | 32.3 | |
| Poor | 9.6 | |
| Missing | 2.4 | |
| Highest level of completed education |
Eighth grade or less | 16.1 |
| Some high school, but did not graduate |
20.1 | |
| High school graduate or GED | 23.8 | |
| Some college or 2-y degree | 25.6 | |
| 4-y college graduate | 7.5 | |
| >4-y college degree | 4.9 | |
| Missing | 2.0 | |
| Hispanic or Latino origin | Hispanic or Latino | 39.4 |
| Not Hispanic or Latino | 55.1 | |
| Missing | 5.5 | |
| Race | American Indian or Alaska Native |
0.8 |
| Asian | 1.0 | |
| Black | 44.5 | |
| Native Hawaiian or Other Pacific Islander |
0.2 | |
| White | 20.5 | |
| Other | 21.3 | |
| ≥ 2 races | 2.2 | |
| Missing | 9.3 | |
| Age category | 18-24 | 5.3 |
| 25–34 | 9.3 | |
| 35–44 | 16.7 | |
| 45–54 | 22.0 | |
| 55–64 | 24.6 | |
| 65–74 | 14.2 | |
| Missing | 7.9 | |
| Sex | Female | 79.7 |
| Male | 17.3 | |
| Missing | 3.0 |
GED indicates general educational development.
Item Distributions
We conducted analyses to evaluate the distribution of survey items. The percentage of ceiling effects for the items ranged from 13% (q27) to 98% (q14) with a median of 70%. The percentage of floor effects ranged from 0.43% (q31) to 49% (q27) with a median of 3%. Item 14 was an outlier in terms of its ceiling effect (almost 98% of respondents said that their provider did not use a condescending, sarcastic, or rude tone or manner). However, this item was retained in the item set because endorsement of the item, although rare, can send a strong message to clinicians about how patients perceive them.
Correlations Between Items and Composites
We analyzed the extent to which items correlated together into multi-item composites and the internal consistency reliability of the composites. Appendix A shows correlations between items and the 6 hypothesized composites. Items that were highly correlated with their composite, whether or not this correlation was significantly higher, were deemed acceptable. These correlations indicate that the data are not consistent with the hypothesized composites. Some items did not correlate with the composite they were hypothesized to represent, whereas others related to multiple composites. For example, item 13 correlated only 0.19 with the patient/provider communication composite. Examination of the correlations suggested 2 composites: one on communication to improve health literacy and a smaller composite focused on communication about medicines.
A 2-factor categorical confirmatory factor analysis model representing the revised item configuration fit the data well (Comparative Fit Index = 0.958; Tucker-Lewis Index = 0.953; Root Mean Square Error of Approximation = 0.068). Factor loadings were all statistically significant. Standardized loadings ranged from 0.436 to 0.913 for the communication to improve health literacy factor and from 0.655 to 0.965 for communication about medicines. The estimated correlation between the 2 factors was 0.784. Thus, the confirmatory factor analysis provided support for the 2 new CAHPS composites.
Table 3 provides the item-scale correlations for the 2 composites. We included item 21 in the Communication to Improve Health Literacy composite, because it gets at a key aspect of patient/provider communication. We ended up excluding it from the final version of the new item set because this item is part of the CAHPS core survey. Item-composite correlations for the 16 remaining items ranged from 0.30 (item 10) to 0.79 (item 18). The composite on communication about medicines—called How Well Providers Communicate About Medicines—included 5 items (plus item 29, a screener from the CAHPS Clinician and Group core items). Only 3 of the 5 items (item 31, 33, and 34), however, were scored because items 30 and 32 are screeners for the items that follow them. Although item 29 (How often did this provider give you easy to understand instructions about how to take your medicines?) was more highly correlated with the Communication to Improve Health Literacy composite, it remained in the Communication About Medicines composite based on its strong conceptual relationship to the other items in that composite. The item-composite correlations for the 3 items that are not screeners was 0.60 for item 34, 0.52 for item 31, and 0.49 for item 33.
TABLE 3.
Item-Scale Correlation Matrix for the Final Composite Measures (n = 492)
| Item # |
Item Description | Communication to Improve Health Literacy Composite |
Communication About Medicines |
|---|---|---|---|
| 8 | Provider interrupts you when you were talking? | 0.40 | 0.24 |
| 9 | Provider talks too fast when talking with you? | 0.35 | 0.04 |
| 10 | Provider uses medical words you did not understand? | 0.30 | 0.06 |
| 11 | Explanations this provider gave you hard to understand because of an accent or the way the provider spoke English? |
0.36 | 0.21 |
| 12 | Provider really cared about you as a person? | 0.58 | 0.22 |
| 15 | Provider shows interest in your questions and concerns? | 0.61 | 0.23 |
| 17 | Provider answers all your questions to your satisfaction? | 0.71 | 0.36 |
| 18 | Provider gives you all the information you wanted about your health? | 0.79 | 0.37 |
| 19 | Provider encourages you to talk about all your health problems or concerns? | 0.64 | 0.34 |
| 21 | Provider gives you easy to understand instructions about taking care of these health problems or concerns? |
0.75 | 0.42 |
| 23 | Provider gives you easy to understand instructions about what to do to take care of this illness or health condition? |
0.72 | 0.37 |
| 24 | Provider asks you to repeat back or describe how you were going to follow the provider’s instructions? |
0.61 | 0.41 |
| 25 | Provider asks you whether you would have any problems doing what you need to do to take care of this illness or health condition? |
0.51 | 0.34 |
| 26 | Provider explains what to do if this illness or health condition got worse or came back? |
0.68 | 0.36 |
| 37 | Were the results of your blood test, x-ray, or other test easy to understand? | 0.56 | 0.31 |
| 40 | Someone explain the purpose of a form before you signed it? | 0.42 | 0.28 |
| 29 | Provider gives you easy to understand instructions about how to take your medicines? | 0.64 | 0.36 |
| 31 | Provider explains the possible side effects of meds in a way that was easy to understand? |
0.52 | 0.52 |
| 33 | Provider gives you written information or write down information about how to take your medicines that was easy to understand? |
0.26 | 0.49 |
| 34 | Provider suggests ways to help you remember to take your medicines? | 0.37 | 0.60 |
| 13 | Provider ignores what you told him or her? | 0.21 | 0.08 |
| 14 | Provider uses a condescending, sarcastic, or rude tone or manner with you? | 0.22 | 0.01 |
| 27 | Provider use pictures, drawings, or models to explain things to you? | 0.31 | 0.49 |
| 36 | Someone from this provider’s office follow up to give you those results? | 0.43 | 0.41 |
| 41 | Offered help in filling out a form at this Provider’s office? | 0.34 | 0.52 |
| 42 | Were the forms that you got at this Provider’s office easy to fill out? | 0.37 | 0.11 |
| 43 | Were the forms that you had to fill out available in Spanish? | 0.03 | 0.02 |
Item numbers refer to the numbering used in the field test version of the survey.
Item 43 was only included in the Spanish version of the survey.
Shading indicates the correlations for the items that belong to the composite under that column.
Although we received 601 surveys, only 492 contained sufficient data to qualify as an analytic complete.
Item-scale correlations are corrected for item overlap with the total score (ie, item-rest correlations).
Other Items
Composite measures need to be closely related, both statistically and conceptually. Items 13, 14, 27, 36, 41, 42, and 43 did not correlate distinctly with either of the final composites. Although some of these items (27, 36, and 41) have substantial correlations (r ≥ 0.40) with one or both of the composites and while the patterns of correlations for these items were similar to other items that were included in the composites, they did not fit into either of the composites conceptually and were therefore not included.
Five-item Composite on Communication to Improve Health Literacy
The large number of items (16) included in the Communication to Improve Health Literacy composite makes it unlikely that all users would choose to use it. Hence, we conducted additional analyses to identify a shorter version of this composite. We found that 5 items (18, 19, 24, 29, and 37) accounted for 90% of the variance in the 16-item Communication to Improve Health Literacy composite and could constitute a shorter version of this composite.
Means, SDs, and Internal Consistency Reliability Estimates
Composite scores were calculated in a 2-step process: linearly transforming the items to a 0–100 possible range and then averaging the items within each composite. The mean for the 16-item Communication to Improve Health Literacy composite (0–100 possible range) was 86 (SD = 16) The mean for the 5-item How Well Providers Communicate About Medicines composite was 60 (SD = 35). The mean for the 5-item (items 18, 19, 24, 29, 37) Communication to Improve Health Literacy composite was 84 (SD = 21).
Internal consistency reliability estimates for the 3 composites were 0.89 (16-item Communication to Improve Health Literacy), 0.71 (How Well Providers Communicate About Medicines), and 0.79 (5-item Communication to Improve Health Literacy). In comparison, the 5 CAHPS core communication items that were administered in the field test had an internal consistency reliability of 0.88. The correlation between the 16-item Communication to Improve Health Literacy composite and the How Well Providers Communicate About Medicines composite was 0.39.
Associations With Global Rating of Provider
The correlations between items and composites with the global rating of the provider indicate the extent to which a composite “drives” the rating. The higher the correlation between a composite and the global rating of the provider, the more an increased score for that composite is associated with a better rating for the provider.
The correlations of the items not included in any composite with the global rating of the provider ranged from −0.08 (P>0.05; item 43) to 0.44 (P <0.001; item 36). Correlations of the individual 5 items in the short Communication to Improve Health Literacy composite with the global rating of the provider ranged from 0.42 (item 37: test results easy to understand) to 0.61 (item 18: provider gave all information wanted about health).
We regressed the global rating of the provider item on the 5-item Communication to Improve Health Literacy composite and the How Well Providers Communicate About Medicines composite. Both composites, 5-item Communication to Improve Health Literacy (b = 0.45; P<0.0001) and 5-item How Well Providers Communicate About Medicines, (b = 0.04; P<0.01) were significantly associated with of the global rating of the provider and accounted for 42% of the variance of the rating.
A regression predicting the global rating of the provider revealed significant unique effects of all the 3 composites (the 16-item version of the Communication to Improve Health Literacy composite: P<0.001, b = 0.28; the 5-item Communication About Medicines composite: P = 0.0207, b = 0.036); and the CAHPS 5-core item communication composite: P<0.0001, b = 0.35). The adjusted R2 indicated that 51% of the variance in the global rating was accounted for by these 3 communication composites. Hence, the composites account for a majority of the variance in the overall perceptions of the provider and each composite contributes important unique information about patients’ health care experiences.
Final Version of the CAHPS Item Set for Addressing Health Literacy and Composites
The final version of the item set includes 30 supplemental items designed for use with the CAHPS Clinician and Group survey. The items address 6 main topic areas: (1) communication to improve health literacy; (2) communication about health problems and concerns; (3) communication about medicines; (4) communication about tests; (5) communication about forms; and (6) disease self-management. We identified 2 composites that can be calculated and reported, one that provides a composite score on communication to improve health literacy and one that provides a composite score on communication about medicines. We also identified a short version of the former composite that has similar explanatory power with a third the number of items. The final version of the health literacy item set was cognitively tested again as part of other CAHPS survey development efforts. Revisions to the item set were made based on the results of additional testing and as part of an effort to harmonize various CAHPS supplemental item sets. The final version of the item set can be found on the CAHPS Web site at https://www.cahps.ahrq.gov/Surveys-Guidance/CG.aspx.
DISCUSSION
Recent years have seen an increased awareness of the mismatch between patients’ health literacy skills and the demands that are placed on them. There is a growing recognition that healthcare providers have a responsibility to improve patients’ understanding of health information. The CAHPS Item Set for Addressing Health Literacy is a tool to help healthcare providers identify areas for quality improvement in how they communicate health information to patients. It also serves as a measure of whether healthcare providers’ have succeeded in reducing the health literacy demands they place on patients.
The results from the analysis of the field test data provide support for the reliability and validity of the CAHPS Item Set for Addressing Health Literacy. They also show that higher ratings on many of the health literacy items and on the composites go hand in hand with more favorable global ratings of providers.
Depending on their focus, survey users have the flexibility to pick and choose items and are not required to field the entire item set or to field all the items within 1 topic area. In addition to the individual items in the item set, we identified 2 composite measures that can be used for both internal and public reporting: How Well Providers Communicate About Medicines consisting of 5 items, and Communication to Improve Health Literacy consisting of a long 16-item version and a short 5-item version. The short version of this composite allows users to score how well healthcare providers are addressing their patients’ health literacy needs without having to use all 16 items in the long version of the composite. Additional information on calculating composite scores can be found in the CAHPS Clinician & Group Surveys and Instructions (https://www.cahps.ahrq.gov/Surveys-Guidance/CG/Get-CG-Surveys-and-Instructions.aspx).
This study has several limitations. First, the health literacy item set was tested exclusively with a population insured by Medicaid managed care plans or Medicare. Further research is needed to test the health literacy item set with other insured populations (eg, those with commercial insurance). Second, the study was limited to English-speaking and Spanish-speaking populations. Further, we were unable to obtain sufficient Spanish language surveys to adequately compare the psychometric measurement properties of the health literacy items and composite measures by language. Additional research is needed to fully assess the Spanish version of the item, and to test the item set with other non–English-speaking populations.
Despite these limitations, the CAHPS Item Set for Addressing Health Literacy can serve as a tool to measure, from the patient’s perspective, how well healthcare providers’ are meeting their patients’ health literacy needs and to use this information for quality improvement purposes. To further aid quality-improvement efforts, each of the items in the item set has been mapped to recommendations made in the American Medical Association’s Health Literacy Educational Toolkit, Second edition.27 This Health Literacy Quality Crosswalk can be found in the document About the CAHPS Item Set for Addressing Health Literacy (https://www.cahps.ahrq.gov/Surveys-Guidance/Item-Sets/Health-Literacy.aspx).
Acknowledgments
Supported by a contract from the Agency for Healthcare Research and Quality (HHSP233200600332P). R.D.H. was also supported in part by grants from AHRQ (U18 HS016980), NIA (P30AG021684), and the NIMHD (2P20MD000182).
APPENDIX A.
Item-scale Correlations for Hypothesized Composites Measures (n = 492)
| Item # |
Item Description | Patient/ Provider Communica- tion |
Communication/ Health Problems or Concerns |
Communication/ Disease Self- Management |
Communicat- ion About Medicines |
Communica- tion About Tests |
Communica- tion About Forms |
0–10 Rating of the Provider |
|---|---|---|---|---|---|---|---|---|
| 8 | Provider interrupts you when you were talking? |
0.48 | 0.29 | 0.25 | 0.27 | 0.19 | 0.14 | 0.33 |
| 9 | Provider talks too fast when talking with you? |
0.43 | 0.25 | 0.19 | 0.08 | 0.16 | 0.06 | 0.24 |
| 10 | Provider uses medi- cal words you did not understand? |
0.39 | 0.2 | 0.15 | 0.08 | 0.23 | 0.12 | 0.17 |
| 11 | Explanations this provider gave you hard to understand because of an accent or the way the provider spoke English? |
0.42 | 0.3 | 0.21 | 0.24 | 0.17 | 0.23 | 0.22 |
| 12 | Provider really cares about you as a person? |
0.57 | 0.51 | 0.4 | 0.29 | 0.33 | 0.12 | 0.54 |
| 13 | Provider ignores what you told him or her? |
0.19 | 0.12 | 0.19 | 0.1 | 0.1 | −0.02 | 0.2 |
| 14 | Provider uses a condescending, sarcastic, or rude tone or manner with you? |
0.22 | 0.14 | 0.16 | 0.03 | 0.12 | 0.06 | 0.16 |
| 15 | Provider shows interest in your questions and concerns? |
0.51 | 0.56 | 0.48 | 0.3 | 0.36 | 0.21 | 0.46 |
| 17 | Provider answers all your questions to your satisfaction? |
0.62 | 0.61 | 0.58 | 0.43 | 0.42 | 0.26 | 0.58 |
| 18 | Provider gives you all the information you wanted about your health? |
0.67 | 0.68 | 0.66 | 0.45 | 0.4 | 0.3 | 0.61 |
| 19 | Provider encourages you to talk about all your health problems or concerns? |
0.51 | 0.58 | 0.56 | 0.39 | 0.33 | 0.38 | 0.49 |
| 21 | Provider gives you easy to understand instructions about taking care of these health problems or concerns? |
0.67 | 0.58 | 0.61 | 0.49 | 0.37 | 0.27 | 0.53 |
| 23 | Provider gives you easy to understand instructions about what to do to take care of this illness or health condition? |
0.59 | 0.68 | 0.54 | 0.45 | 0.45 | 0.34 | 0.53 |
| 24 | Provider asks you to repeat back or describe how you were going to follow the provider’s instructions? |
0.44 | 0.51 | 0.66 | 0.45 | 0.45 | 0.36 | 0.47 |
| 25 | Provider asks you whether you would have any problems doing what you need to do to take care of this illness or health condition? |
0.38 | 0.46 | 0.55 | 0.36 | 0.31 | 0.26 | 0.37 |
| 26 | Provider explains what to do if this illness or health condition got worse or came back? |
0.57 | 0.57 | 0.59 | 0.43 | 0.46 | 0.3 | 0.51 |
| 27 | Provider uses pictures, drawings, or models to explain things to you? |
0.19 | 0.25 | 0.37 | 0.48 | 0.25 | 0.24 | 0.27 |
| 29 | Provider gives you easy to understand instructions about how to take your medicines? |
0.52 | 0.54 | 0.54 | 0.36 | 0.42 | 0.3 | 0.43 |
| 30 | Provider explains the possible side effects of your medicines? |
0.36 | 0.33 | 0.45 | 0.50 | 0.35 | 0.25 | 0.37 |
| 31 | Provider explains the possible side effects of your medicines in a way that was easy for you to understand? |
0.4 | 0.38 | 0.33 | 0.29 | 0.28 | 0.2 | 0.34 |
| 32 | Provider gives you written information or write down information about how to take your medicines? |
0.05 | 0.17 | 0.24 | 0.40 | 0.18 | 0.22 | 0.13 |
| 33 | Was the written information you were given easy to understand? |
0.37 | 0.31 | 0.24 | 0.33 | 0.29 | 0.29 | 0.26 |
| 34 | Provider suggests ways to help you remember to take your medicines? |
0.18 | 0.33 | 0.52 | 0.61 | 0.37 | 0.35 | 0.32 |
| 36 | Someone from this provider’s office follow up to give you those results? |
0.3 | 0.29 | 0.41 | 0.44 | 0.48 | 0.28 | 0.44 |
| 37 | Were the results of your blood test, x- ray, or other test easy to understand? |
0.47 | 0.38 | 0.49 | 0.36 | 0.48 | 0.37 | 0.42 |
| 40 | Someone explain the purpose of a form before you signed it? |
0.3 | 0.37 | 0.35 | 0.34 | 0.41 | 0.35 | 0.31 |
| 41 | Offered help in filling out a form at this provider’s office? |
0.19 | 0.31 | 0.4 | 0.51 | 0.29 | 0.36 | 0.21 |
| 42 | Were the forms that you got at this provider’s office easy to fill out? |
0.26 | 0.29 | 0.26 | 0.13 | 0.34 | 0.27 | 0.31 |
| 43 | Were the forms that you had to fill out available in Spanish? |
−0.04 | 0.04 | 0.06 | 0.02 | 0 | 0.18 | −0.08 |
| 38 | What number would you use to rate this provider? |
0.62 | 0.57 | 0.57 | 0.44 | 0.5 | 0.26 | 0.00 |
Item numbers refer to the numbering used in the field test version of the survey.
Although we received 601 surveys, only 492 contained sufficient data to qualify as an analytic complete.
Shading indicates the correlation for items that were hypothesized to belong to the composite under that column. Item-scale correlations were corrected for item overlap with th total score (ie, item-rest correlations).
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.H.R. 3590—111th Congress: Patient Protection and Affordable Care Act. 2009. [Google Scholar]
- 2.Kutner M, Greenberg E, Jin Y, et al. The Health Literacy of America’s Adults: Results From the 2003 National Assessment of Adult Literacy. National Center for Educational Statistics; Washington, DC: 2006. [Google Scholar]
- 3.U. S. Department of Health and Human Services . America’s Health Literacy: Why We Need Accessible Health Information. U. S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion; Rockville, MD: 2009. [Google Scholar]
- 4.U.S. Department of Health and Human Services . Communicating Health: Priorities and Strategies for Progress. US Department of Health and Human Services, Office of Disease Prevention and Health Promotion; Washington, DC: 2003. [Google Scholar]
- 5.Baker DW. The meaning and the measure of health literacy. J Gen Intern Med. 2006;21:878–883. doi: 10.1111/j.1525-1497.2006.00540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parker R, Ratzan SC. Health literacy: a second decade of distinction for Americans. J Health Commun. 2010;15(Suppl 2):20–33. doi: 10.1080/10810730.2010.501094. [DOI] [PubMed] [Google Scholar]
- 7.Koh H, Berwick D, Clancy C, et al. New federal policy initiatives to boost health literacy can help the nation move beyond the cycle ofcostly “crisis care.”. Health Aff. 2012;31:434–443. doi: 10.1377/hlthaff.2011.1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.U.S. Department of Health and Human Services . Healthy Pople 2010: Understanding and Improving Health. 2nd ed. U.S. Government Printing Office; Washington, DC: 2000. [Google Scholar]
- 9.Adams K, Corrigan JM. Priority areas for national action: transforming healthcare quality. The National Academies Press; Washington, DC: 2003. [PubMed] [Google Scholar]
- 10.Institute of Medicine . Health Literacy: A Prescription to End Confusion. The National Academies Press; Washington, DC: 2004. [PubMed] [Google Scholar]
- 11.DeWalt DA, Callahan LF, Hawk Victoria H, et al. Health literacy universal precautions toolkit. Agency for Healthcare Research and Quality; Rockville, MD: 2010. [Google Scholar]
- 12.Berkman ND, DeWalt DA, Pignone MP, et al. Literacy and Health Outcomes. Agency for Healthcare Research and Quality; Rockville, MD: 2004. [Google Scholar]
- 13.Weidmer, et al. [Accessed May 14, 2012];Guidelines for Translating CAHPS Surveys. 2006 Available at: https://www.cahps.ahrq.gov/Surveys-Guidance/Helpful-Resources/Translating-Surveys.aspx.
- 14.Solano-Flores, et al. [Accessed May 14, 2012];The Assessment and Selection of Translators and Translation Reviewers. 2006 Available at: https://www.cahps.ahrq.gov/Surveys-Guidance/Helpful-Resources/Translating-Surveys.aspx.
- 15.Harkness JA, Van de Vijver FJR, Molher PPh. Cross-Cultural Survey Methods. John Wiley & Sons Inc.; Hoboken, NJ: 2003. [Google Scholar]
- 16.Behling O, Law KS. Translating Questionnaires and Other Research Instruments: Problems and Solutions. Sage; Thousand Oaks, CA: 2000. pp. 07–131. (Sage University Papers Series on Quantitative Applications in the Social Sciences). [Google Scholar]
- 17.U.S. Census Bureau Methodology and Standards Council . The Translation of Surveys: An Overview of Methods and Practices and the Current State of Knowledge. Census Bureau Guideline: Language Translation of Data Collection Instruments and Supporting Materials. US Census Bureau; Washington, DC: 2000. Working Paper. [Google Scholar]
- 18.Hughes KA. Comparing Pretesting Methods: Cognitive Interviews, Respondent Debriefing, and Behavior Coding; Annual Meeting of the Federal Committee on Statistical Methodology; Arlington, VA: US Census Bureau. 2003. [Google Scholar]
- 19.Willis G. Cognitive Interviewing: A Tool for Improving Questionnaire Design. Sage Publications; Thousand Oaks, CA: 2004. [Google Scholar]
- 20.Harris-Kojetin LD, Fowler FJ, Brown JA, et al. The use of cognitive testing to develop and evaluate CAHPS 1.0 core survey items. Med Care. 1999;37:MS10–MS21. doi: 10.1097/00005650-199903001-00002. [DOI] [PubMed] [Google Scholar]
- 21.Levine RE, Fowler FJ, Jr., Brown JA. Role of cognitive testing in the development of the CAHPS Hospital Survey. Health SerRes. 2005;40(6 pt 2):2037–2056. doi: 10.1111/j.1475-6773.2005.00472.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weech-Maldonado R, Weidmer B, Morales L, et al. Cross-cultural adaptation of survey instruments: the CAHPS experience. In: Cynamon ML, Kulka RA, editors. Seventh Conference on Health Survey Research Methods. US Dept of Health and Human Services; Hyattsville, MD: 2001. pp. 75–82. DHSS Publications No. [PHS] 01-1013. Publication PHS 01-1013. [Google Scholar]
- 23.McGee J, Kanouse DE, Sofaer S, et al. Making survey results easy to report to consumers: How reporting needs guided survey design in CAHPS. Med Care. 1999;37(suppl 3):MS32–MS40. doi: 10.1097/00005650-199903001-00004. [DOI] [PubMed] [Google Scholar]
- 24.Solomon LS, Hays RD, Zaslavsky AM, et al. Psychometric properties of a group-level Consumer Assessment of Health Plans Study (CAHPS) instrument. Med Care. 2005;43:53–60. [PubMed] [Google Scholar]
- 25.Hays RD, Chong K, Brown J, et al. Patient reports and ratings of individual physicians: an evaluation of the DoctorGuide and Consumer Assessment of Health Plans Study provider-level surveys. Am J Med Qual. 2003;18:190–196. doi: 10.1177/106286060301800503. [DOI] [PubMed] [Google Scholar]
- 26.Muthen LK, Muthen BO. Mplus User’s Guide. Muthen & Muthen; Los Angeles, CA: 2009. [Google Scholar]
- 27.Agency for Healthcare Research and Quality . About the CAHPS Item Set for Addressing Health Literacy Document No. 1311. 2011. [Google Scholar]