Abstract
We identified traditional risk factors and investigated poorly understood risk factors for suicide attempts according to gender in a large Korean population. We analyzed the data from 6,768 males and 12,475 females with suicidal ideation obtained from the nationwide 2013 Korean Community Health Survey. The dependent variable was suicide attempts within the past year. There was a significant trend towards an increase in suicide attempts with decreasing age in both genders. Compared with those who were married, suicide attempts were significantly higher among those who were widowed, divorced, or separated for males (odds ratio [OR], 2.07; 95% confidence interval [CI], 1.34–3.20), but lower for females (OR, 0.66; 95% CI, 0.45–0.98). Current smoking and depression were significant risk factor for suicide attempts in males and females. However, monthly household income, myocardial infarction, and osteoporosis were significantly associated with suicide attempts only in males, whereas education level, recipient of National Basic Livelihood Security, family contact, leisure activity, and drinking frequency were significantly associated only in females. These findings indicate that gender difference should be considered in the assessment, prevention, and management of future suicide attempts by community policy-makers and clinicians.
Keywords: Gender, Suicide Attempt, Risk Factors, Community Health Survey
Graphical Abstract
INTRODUCTION
Suicide is one of the most serious and urgent public health issues in Korea in part because the suicide rate is continuously and rapidly increasing. Suicide is the fourth leading cause of death in Korea behind malignant neoplasm, cerebrovascular disease, and heart disease (1). In 2014, the suicide rate was 27.3 per 100,000 people, which is 2.4 times higher than the Organization for Economic Cooperation and Development (OECD) average and the highest among OECD members (2).
It is important to identify the risk factors for suicidal ideation and suicide attempts in the general population because these suicidal behaviors are positively associated with completed suicide (2). Although many risk factors for suicide attempts have been identified (3-15), more effective intervention strategies for mental health and suicide prevention can be developed when the gender-specific underlying risk factors for suicide attempts are better understood (16). To our knowledge, however, few studies have examined gender-specific risk factors for suicide attempts in a large general population. Furthermore, although many studies have investigated the relationships between sociodemographic factors and suicide attempts, relatively few studies have evaluated the associations of socio-family relationships, health behaviors, and health status with suicide attempts.
Therefore, this study confirmed gender differences in the traditional risk factors associated with suicide attempts, providing evidence and a basis for improved suicide prevention policies. We also examined novel risk factors for suicide attempts according to gender using national survey data from a large sample of the general Korean population with suicidal ideation.
MATERIALS AND METHODS
Subjects
We analyzed data from the Korean Community Health Survey (CHS) that was conducted by the Korea Centers for Disease Control and Prevention between August and October 2013. The Korean CHS is a nationwide survey carried out by trained surveyors using computer-assisted personal interviewing methods. Multistage, stratified, and random samplings were used to select representative households from 253 local Korean communities based on the information obtained during resident registration; an average of 900 individuals from each local community were surveyed. The 2013 Korean CHS utilized a standardized questionnaire with 258 questions to assess a wide range of health topics including health status, morbidity, health service use, and health behaviors.
A total of 228,781 individuals who were 19 years of age or older participated in the 2013 survey. After excluding participants with missing data regarding sociodemographic variables, socio-family relationships, health behaviors, and health status, 19,243 participants (6,768 males and 12,475 females) who had experienced suicidal ideation were included in the final analyses of the associations between the study covariates and suicide attempts.
Measurements
The dependent variable was gender-specific suicide attempts among adults with suicidal ideation. Suicidal ideation was defined as having had thoughts of wanting to die in the past year. A suicide attempt was defined as having experienced suicidal ideation and actually making a suicide attempt in the past year. Data regarding four sets of potential risk factors for suicide attempts were collected using a standardized questionnaire: sociodemographic factors, socio-family relationships, health behaviors, and health status.
The sociodemographic factors included age group (19–44, 45–64, 64–74, and ≥ 75 years), residential region (urban and rural), marital status (never married, married, and widowed/divorced/separated), household composition (living alone, single generation, two generations, and three generations), education level (not educated, primary school, middle or high school, and college or higher), monthly household income (≤ 100, 101–200, 201–400, and ≥ 401 million won), employment status (employed, unemployed, and housewife/student), and National Basic Livelihood Security System status (recipient and non-recipient). The socio-family relationships included family contact, neighbor contact, friend contact, religious activity, friendship activity, leisure activity, and charity activity), grouping as < 1 time and ≥ 1 time per month.
Health behaviors included smoking status (never, former, and current smokers), drinking frequency (none, ≤ 1 time, 2–3 times, and ≥ 4 times per week), moderate physical activity (≤ 2 times and ≥ 3 times per week), walking activity (≤ 2 times and ≥ 3 times per week), and sleep duration (≤ 6 hour, 7–8 hours, and ≥ 9 hours per day). Health status included self-rated health (good, fair, and poor), self-rated oral health (good, fair, and poor), perceived usual stress (very low, low, high, and very high), experience of depressive mood (no and yes), and body mass index (BMI; ≤ 18.4, 18.5–24.9, and ≥ 25.0 kg/m2). Hypertension, diabetes, dyslipidemia, stroke, myocardial infarction, osteoarthritis, osteoporosis, asthma, hepatitis B, and depression were classified as diagnosed or never diagnosed.
Statistical analysis
The gender-specific characteristics of the participants were compared based on the presence or absence of suicide attempts using χ2 tests. Before and after adjusting for all of the evaluated covariates (sociodemographic factors, socio-family relationships, health behaviors, and health status), the odds ratio (OR) and 95% confidence interval (CI) values for suicide attempts for each factor were estimated using a multivariate logistic regression analysis. All statistical analyses were conducted with SPSS software version 22.0 (SPSS; Chicago, IL, USA) and a P value < 0.05 was considered to indicate statistical significance.
Ethics statement
This study was conducted in accordance with the Declaration of Helsinki guidelines. Written informed consent was obtained from all participants in the Korean CHS and the survey protocol was approved by the institutional review board of the Korean Centers for Disease Control and Prevention (2013-06EXP-01-3C).
RESULTS
Suicide attempts according to gender and age
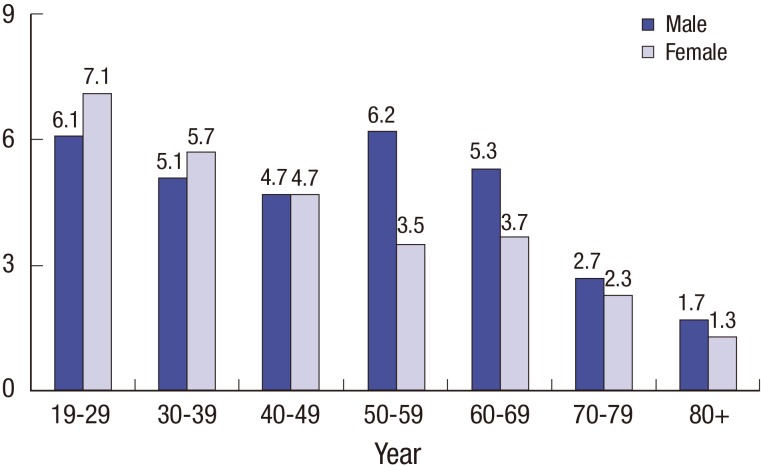
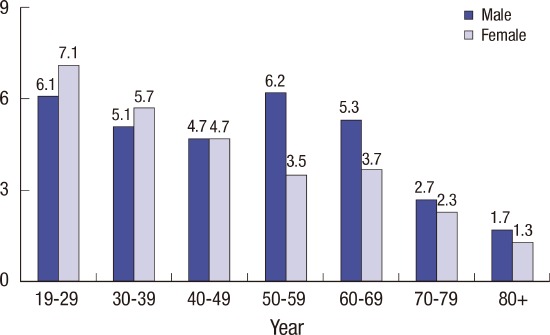
Of the 6,768 males and 12,475 females who had experienced suicidal ideation, 314 males (4.6%) and 481 females (3.9%) actually made a suicide attempt within the past year. The rates of suicide attempts decreased with age in both males and females (both P < 0.001). The rates of suicide attempt were 6.1%, 5.1%, 4.7%, 6.2%, 5.3%, 2.7%, and 1.7% for males and 7.1%, 5.7%, 4.7%, 3.5%, 3.7%, 2.3%, and 1.3% for females in the 19–29, 30–39, 40–49, 50–59, 60–69, 70–79, and ≥ 80 age groups, respectively (Fig. 1).
Fig. 1.
Proportion of suicide attempt decreased according to age in both males and females (Ps < 0.001).
Gender-specific association of covariates with suicide attempts
Tables 1 and 2 show the gender-specific associations of sociodemographic factors, socio-family relationships, health behaviors, and health status with suicide attempts. In both males and females, the proportion of suicide attempts significantly decreased with increasing age (all P < 0.001). Of the sociodemographic factors, marital status, household composition, monthly household income, employment status, and National Basic Livelihood Security System status were significantly associated with suicide attempts among males (all P < 0.05). By contrast, region of residence, marital status, household composition, education level, and National Basic Livelihood Security System status were significantly associated with suicide attempts among females (all P < 0.05) (Table 1). Of the socio-family relationships, family contact, friend contact, and friendship activity were significantly associated with suicide attempts among males, whereas family contact, neighbor contact, friendship activity, and leisure activity were significantly associated with suicide attempts among females (Table 1).
Table 1. Sociodemographic factors and socio-family relations according to self-reported suicide attempts.
| Parameters | Males (n = 6,768) | P value | Females (n = 12,475) | P value | ||
|---|---|---|---|---|---|---|
| Suicide attempts (−) (n = 6,454) |
Suicide attempts (+) (n = 314) |
Suicide attempts (−) (n = 11,994) |
Suicide attempts (+) (n = 481) |
|||
| Sociodemographic factors | ||||||
| Age group | < 0.001 | < 0.001 | ||||
| 19–44 yr | 1,626 (25.2) | 88 (28.0) | 3,102 (25.9) | 201 (41.8) | ||
| 45–64 yr | 2,394 (37.1) | 147 (46.8) | 4,603 (38.4) | 172 (35.8) | ||
| 65–74 yr | 1,433 (22.2) | 54 (17.2) | 2,432 (20.3) | 81 (16.8) | ||
| ≥ 75 yr | 1,001 (15.5) | 25 (8.0) | 1,857 (15.5) | 27 (5.6) | ||
| Residential region | 0.307 | 0.007 | ||||
| Urban | 3,410 (52.8) | 171 (54.5) | 6,760 (56.4) | 299 (62.2) | ||
| Rural | 3,044 (47.2) | 143 (45.5) | 5,234 (43.6) | 182 (37.8) | ||
| Marital status | < 0.001 | < 0.001 | ||||
| Married | 964 (14.9) | 56 (17.8) | 1,041 (8.7) | 77 (16.0) | ||
| Never married | 4,353 (67.4) | 157 (50.0) | 7,110 (59.3) | 270 (56.1) | ||
| Widowed, divorced, or separated | 1,137 (17.6) | 101 (32.2) | 3,843 (32.0) | 134 (27.9) | ||
| Household composition | < 0.001 | 0.042 | ||||
| Living alone | 974 (15.1) | 75 (23.9) | 2,174 (18.1) | 74 (15.4) | ||
| Single generation | 2,222 (34.4) | 79 (25.2) | 3,258 (27.2) | 119 (24.7) | ||
| Two generations | 2,757 (42.7) | 144 (45.9) | 5,351 (44.6) | 246 (51.1) | ||
| Three generations | 501 (7.8) | 16 (5.1) | 1,211 (10.1) | 42 (8.7) | ||
| Education level | 0.077 | < 0.001 | ||||
| Non-formal education | 320 (5.0) | 14 (4.5) | 1,847 (15.4) | 55 (11.4) | ||
| Primary school | 1,481 (22.9) | 63 (20.1) | 3,325 (27.7) | 106 (22.0) | ||
| Middle or high school | 3,030 (46.9) | 171 (54.5) | 4,607 (38.4) | 235 (48.9) | ||
| College or higher | 1,623 (25.1) | 66 (21.0) | 2,215 (18.5) | 85 (17.7) | ||
| Monthly household income | < 0.001 | 0.962 | ||||
| ≤ 100 million won | 2,490 (38.6) | 156 (49.7) | 4,585 (38.2) | 183 (38.0) | ||
| 101–200 million won | 1,402 (21.7) | 71 (22.6) | 2,492 (20.8) | 103 (21.4) | ||
| 201–400 million won | 1,589 (24.6) | 63 (20.1) | 2,978 (24.8) | 121 (25.2) | ||
| ≥ 401 million won | 973 (15.1) | 24 (7.6) | 1,939 (16.2) | 74 (15.4) | ||
| Employment status | < 0.001 | 0.467 | ||||
| Employed | 4,030 (62.4) | 151 (48.1) | 5,454 (45.5) | 205 (42.6) | ||
| Unemployed | 2,306 (35.7) | 156 (49.7) | 1,507 (12.6) | 64 (13.3) | ||
| Housewife or student | 118 (1.8) | 7 (2.2) | 5,033 (42.0) | 212 (44.1) | ||
| National Basic Livelihood Security status | < 0.001 | < 0.001 | ||||
| Non-recipient | 5,946 (92.1) | 245 (78.0) | 11,085 (92.4) | 408 (84.8) | ||
| Recipient | 508 (7.9) | 69 (22.0) | 909 (7.6) | 73 (15.2) | ||
| Socio-family relations | ||||||
| Family contact | < 0.001 | < 0.001 | ||||
| < 1 time per mon | 1,697 (26.3) | 124 (39.5) | 2,302 (19.2) | 139 (28.9) | ||
| ≥ 1 time per mon | 4,757 (73.7) | 190 (60.5) | 9,692 (80.8) | 342 (71.1) | ||
| Neighbor contact | 0.107 | < 0.001 | ||||
| < 1 time per mon | 2,182 (33.8) | 120 (38.2) | 3,269 (27.3) | 177 (36.8) | ||
| ≥ 1 time per mon | 4,272 (66.2) | 194 (61.8) | 8,725 (72.7) | 304 (63.2) | ||
| Friend contact | 0.021 | 0.204 | ||||
| < 1 time per mon | 1,966 (30.5) | 115 (36.6) | 3,907 (32.6) | 170 (35.3) | ||
| ≥ 1 time per mon | 4,488 (69.5) | 199 (63.4) | 8,087 (67.4) | 311 (64.7) | ||
| Religious activity | 0.574 | 0.055 | ||||
| < 1 time per mon | 5,241 (81.2) | 251 (79.9) | 7,999 (66.7) | 341 (70.9) | ||
| ≥ 1 time per mon | 1,213 (18.8) | 63 (20.1) | 3,995 (33.3) | 140 (29.1) | ||
| Friendship activity | < 0.001 | < 0.001 | ||||
| < 1 time per mon | 3,434 (53.2) | 207 (65.9) | 6,654 (55.5) | 308 (64.0) | ||
| ≥ 1 time per mon | 3,020 (46.8) | 107 (34.1) | 5,340 (44.5) | 173 (36.0) | ||
| Leisure activity | 0.095 | 0.042 | ||||
| < 1 time per mon | 5,113 (79.2) | 261 (83.1) | 10,249 (85.5) | 427 (88.8) | ||
| ≥ 1 time per mon | 1,341 (20.8) | 53 (16.9) | 1,745 (14.5) | 54 (11.2) | ||
| Charity activity | 0.703 | 0.747 | ||||
| < 1 time per mon | 6,114 (94.7) | 299 (95.2) | 11,361 (94.7) | 454 (94.4) | ||
| ≥ 1 time per mon | 340 (5.3) | 15 (4.8) | 633 (5.3) | 27 (5.6) | ||
Values are presented as number (%).
Table 2. Health behaviors and health statuses according to self-reported suicide attempts.
| Health behaviors and status | Males (n = 6,768) | P value | Females (n = 12,475) | P value | ||
|---|---|---|---|---|---|---|
| Suicide attempts (−) (n = 6,454) |
Suicide attempts (+) (n = 314) |
Suicide attempts (−) (n = 11,994) |
Suicide attempts (+) (n = 481) |
|||
| Health behaviors | ||||||
| Smoking status | < 0.001 | < 0.001 | ||||
| Never smokers | 1,108 (17.2) | 41 (13.1) | 10,754 (89.7) | 359 (74.6) | ||
| Former smokers | 2,404 (37.2) | 68 (21.7) | 495 (4.1) | 38 (7.9) | ||
| Current smokers | 2,942 (45.6) | 205 (65.3) | 745 (6.2) | 84 (17.5) | ||
| Drinking frequency | 0.115 | < 0.001 | ||||
| None | 1,789 (27.7) | 78 (24.8) | 5,443 (45.4) | 180 (37.4) | ||
| ≤ 1 time per wk | 2,160 (33.5) | 106 (33.8) | 5,350 (44.6) | 200 (41.6) | ||
| 2–3 times per wk | 1,215 (18.8) | 51 (16.2) | 877 (7.3) | 69 (14.3) | ||
| ≥ 4 times per wk | 1,290 (20.0) | 79 (25.2) | 324 (2.7) | 32 (6.7) | ||
| Moderate physical activity | 0.049 | 0.854 | ||||
| ≤ 2 times per wk | 5,019 (77.8) | 259 (82.5) | 9,609 (80.1) | 387 (80.5) | ||
| ≥ 3 times per wk | 1,435 (22.2) | 55 (17.5) | 2,385 (19.9) | 94 (19.5) | ||
| Walking activity | 0.069 | 0.065 | ||||
| ≤ 2 times per wk | 2,687 (41.6) | 147 (46.8) | 4,768 (39.8) | 171 (35.6) | ||
| ≥ 3 times per wk | 3,767 (58.4) | 167 (53.2) | 7,226 (60.2) | 310 (64.4) | ||
| Sleep duration | 0.002 | 0.260 | ||||
| ≤ 6 hr per day | 3,308 (51.3) | 185 (58.9) | 6,703 (55.9) | 287 (59.7) | ||
| 7–8 hr per day | 2,717 (42.1) | 101 (32.2) | 4,760 (39.7) | 174 (36.2) | ||
| ≥ 9 hr per day | 429 (6.6) | 28 (8.9) | 531 (4.4) | 20 (4.2) | ||
| Health status | ||||||
| Self-rated health | < 0.001 | 0.008 | ||||
| Good | 1,425 (22.1) | 53 (16.9) | 2,043 (17.0) | 67 (13.9) | ||
| Fair | 2,327 (36.1) | 79 (25.2) | 4,540 (37.9) | 163 (33.9) | ||
| Poor | 2,702 (41.9) | 182 (58.0) | 5,411 (45.1) | 251 (52.2) | ||
| Self-rated oral health | 0.012 | 0.762 | ||||
| Good | 973 (15.1) | 43 (13.7) | 1,795 (15.0) | 73 (15.2) | ||
| Fair | 1,595 (24.7) | 57 (18.2) | 3,645 (30.4) | 153 (31.80 | ||
| Poor | 3,886 (60.2) | 214 (68.2) | 6,554 (54.6) | 255 (53.0) | ||
| Perceived usual stress | < 0.001 | < 0.001 | ||||
| Little | 577 (8.9) | 17 (5.4) | 763 (6.4) | 14 (2.9) | ||
| Low | 2,362 (36.6) | 45 (14.3) | 4,100 (34.2) | 78 (16.2) | ||
| High | 2,696 (41.8) | 163 (51.9) | 5,615 (46.8) | 222 (46.2) | ||
| Very high | 819 (12.7) | 89 (28.3) | 1,516 (12.6) | 167 (34.7) | ||
| Experience of depressive mood | < 0.001 | < 0.001 | ||||
| No | 4,673 (72.4) | 126 (40.1) | 7,993 (66.6) | 153 (31.8) | ||
| Yes | 1,781 (27.6) | 188 (59.9) | 4,001 (33.4) | 328 (68.2) | ||
| Body mass index | 0.091 | 0.049 | ||||
| ≤ 18.4 kg/m2 | 438 (6.8) | 31 (9.9) | 1,038 (8.7) | 50 (10.4) | ||
| 18.5–24.9 kg/m2 | 4,310 (66.8) | 198 (63.1) | 8,094 (67.5) | 299 (62.2) | ||
| ≥ 25.0 kg/m2 | 1,706 (26.4) | 85 (27.1) | 2,862 (23.9) | 132 (27.4) | ||
| Diagnosed with hypertension | 0.395 | 0.047 | ||||
| Never | 4,342 (67.3) | 204 (65.0) | 8,188 (68.3) | 349 (72.6) | ||
| Ever | 2,112 (32.7) | 110 (35.0) | 3,806 (31.7) | 132 (27.4) | ||
| Diagnosed with diabetes | 0.202 | 0.180 | ||||
| Never | 5,455 (84.5) | 257 (81.8) | 10,394 (86.7) | 427 (88.8) | ||
| Ever | 999 (15.5) | 57 (18.2) | 1,600 (13.3) | 54 (11.2) | ||
| Diagnosed with dyslipidemia | 0.757 | 0.253 | ||||
| Never | 5,488 (85.0) | 269 (85.7) | 9,845 (82.1) | 385 (80.0) | ||
| Ever | 966 (15.0) | 45 (14.3) | 2,149 (17.9) | 96 (20.0) | ||
| Diagnosed with stroke | 0.019 | 0.099 | ||||
| Never | 6,101 (94.5) | 287 (91.4) | 11,588 (96.6) | 458 (95.2) | ||
| Ever | 353 (5.5) | 27 (8.6) | 406 (3.4) | 23 (4.8) | ||
| Diagnosed with myocardial infarction | 0.046 | 0.026 | ||||
| Never | 6,224 (96.4) | 296 (94.3) | 11,767 (98.1) | 465 (96.7) | ||
| Ever | 230 (3.6) | 18 (5.7) | 227 (1.9) | 16 (3.3) | ||
| Diagnosed with osteoarthritis | 0.241 | 0.370 | ||||
| Never | 5,634 (87.3) | 267 (85.0) | 8,196 (68.3) | 338 (70.3) | ||
| Ever | 820 (12.7) | 47 (15.0) | 3,798 (31.7) | 143 (29.7) | ||
| Diagnosed with osteoporosis | 0.001 | 0.177 | ||||
| Never | 6,244 (96.7) | 293 (93.3) | 9,286 (77.4) | 385 (80.0) | ||
| Ever | 210 (3.3) | 21 (6.7) | 2,708 (22.6) | 96 (20.0) | ||
| Diagnosed with asthma | 0.391 | 0.009 | ||||
| Never | 6,093 (94.4) | 300 (95.5) | 11,331 (94.5) | 441 (91.7) | ||
| Ever | 361 (5.6) | 14 (4.5) | 663 (5.5) | 40 (8.3) | ||
| Diagnosed with hepatitis B | 0.157 | 0.419 | ||||
| Never | 6,224 (96.4) | 298 (94.9) | 11,691 (97.5) | 466 (96.9) | ||
| Ever | 230 (3.6) | 16 (5.1) | 303 (2.5) | 15 (3.1) | ||
| Diagnosed with depression | < 0.001 | < 0.001 | ||||
| Never | 5,952 (92.2) | 219 (69.7) | 10,412 (86.8) | 245 (50.9) | ||
| Ever | 502 (7.8) | 95 (30.3) | 1,582 (13.2) | 236 (49.1) | ||
Values are presented as number (%).
Regarding health behaviors, smoking status was significantly associated with suicide attempts in both males and females. Moderate physical activity and sleep duration were significantly associated with suicide attempts among males, while drinking frequency was significantly associated with suicide attempts among females (Table 2). Of the health statuses, self-rated health, perceived usual stress, experience of depressive mood, myocardial infarction, and depression were significantly associated with suicide attempts in both genders. Self-rated oral health, stroke, and osteoporosis were significantly associated with suicide attempts among males, while BMI, hypertension, and asthma were significantly associated among females (Table 2).
OR and 95% CI values for the gender-specific relationships between suicide attempts and related factors
Table 3 shows the unadjusted and fully adjusted gender-specific relationships between suicide attempts and related factors. There was a significant trend towards an increase in suicide attempts with decreasing age in both genders. Compared with the ≥ 75 years age group, the OR for suicide attempts among those 65–74, and 45–64, and 19–44 years of age were increased by 1.49- (95% CI, 0.90–2.48), 2.65- (95% CI, 1.58–4.47), and 3.15-fold (95% CI, 1.66–5.96) among males and by 2.01- (95% CI, 1.26–3.23), 2.44- (95% CI, 1.48–4.05), and 4.67-fold (95% CI, 2.62–8.34) among females, respectively. Compared with those who were married, suicide attempts were significantly more frequent among those who were widowed, divorced, or separated in males (OR, 2.07; 95% CI, 1.34–3.20) but lower in females (OR, 0.66; 95% CI, 0.45–0.98). Although no significant associations between education level and suicide attempts were observed among males, there was a significant increasing trend in suicide attempts with decreasing education level (OR, 2.39; 95% CI, 1.44–3.97 for no formal education versus college or higher) among females. Suicide attempts were significantly more frequent in males earning 101–200 million won (OR, 1.84; 95% CI, 1.12–3.03) and ≤ 100 million won (OR, 1.94; 95% CI, 1.14–3.28) compared with ≥ 401 million won. Unlike males, there was no significant association between monthly household income and suicide attempts among females. Only females in the National Basic Livelihood Security System had a higher OR for suicide attempts (OR, 1.42; 95% CI, 1.03–1.96). No significant associations were observed between residential region, household composition, or employment status and suicide attempts.
Table 3. Odds ratios (OR) and 95% confidence intervals (CIs) for the associations of suicide attempts with the study covariates according to a multivariate logistic regression analysis.
| Variables | Males (n = 6,768) | Females (n = 12,475) | ||
|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | |
| Sociodemographic factors | ||||
| Age group (/≥ 75 yr) | ||||
| 65–74 yr | 1.51 (0.93–2.44) | 1.49 (0.90–2.48) | 2.29 (1.48–3.56) | 2.01 (1.26–3.23) |
| 45–64 yr | 2.46 (1.60–3.78) | 2.65 (1.58–4.47) | 2.57 (1.71–3.87) | 2.44 (1.48–4.05) |
| 19–44 yr | 2.17 (1.38–3.40) | 3.15 (1.66–5.96) | 4.46 (2.97–6.69) | 4.67 (2.62–8.34) |
| Rural (/urban) | 0.94 (0.75–1.18) | 1.08 (0.83–1.42) | 0.79 (0.65–0.95) | 1.06 (0.85–1.32) |
| Marital status (/married) | ||||
| Never married | 0.62 (0.45–0.85) | 1.32 (0.86–2.02) | 0.51 (0.40–0.67) | 0.75 (0.53–1.07) |
| Widowed, divorced, or separated | 1.53 (1.09–2.14) | 2.07 (1.34–3.20) | 0.47 (0.35–0.63) | 0.66 (0.45–0.98) |
| Household composition (/three generations) | ||||
| Two generations | 1.64 (0.97–2.77) | 1.61 (0.92–2.83) | 1.33 (0.95–1.85) | 1.08 (0.75–1.54) |
| Single generation | 1.11 (0.65–1.92) | 1.61 (0.87–2.96) | 1.05 (0.74–1.51) | 1.02 (0.68–1.54) |
| Living alone | 2.41 (1.39–4.18) | 1.55 (0.84–2.89) | 0.98 (0.67–1.44) | 0.90 (0.57–1.42) |
| Education level (/college or higher) | ||||
| Middle or high school | 1.39 (1.04–1.86) | 1.22 (0.88–1.71) | 1.33 (1.03–1.71) | 1.75 (1.29–2.37) |
| Primary school | 1.05 (0.74–1.49) | 1.05 (0.67–1.64) | 0.83 (0.62–1.11) | 1.81 (1.19–2.76) |
| Non-formal education | 1.08 (0.60–1.94) | 1.14 (0.57–2.28) | 0.78 (0.55–1.10) | 2.39 (1.44–3.97) |
| Monthly household income (/≥ 401 million won) | ||||
| 201–400 million won | 1.61 (0.99–2.59) | 1.59 (0.97–2.61) | 1.07 (0.79–1.43) | 0.95 (0.69–1.30) |
| 101–200 million won | 2.05 (1.28–3.29) | 1.84 (1.12–3.03) | 1.08 (0.80–1.47) | 0.86 (0.62–1.21) |
| ≤ 100 million won | 2.54 (1.64–3.93) | 1.94 (1.14–3.28) | 1.05 (0.79–1.38) | 0.96 (0.66–1.39) |
| Employment status (/employed) | ||||
| Unemployed | 1.81 (1.44–2.27) | 1.35 (0.98–1.85) | 1.13 (0.85–1.51) | 1.18 (0.84–1.67) |
| Housewife or student | 1.58 (0.73–3.45) | 2.15 (0.91–5.09) | 1.12 (0.92–1.36) | 1.05 (0.84–1.32) |
| Recipient of National Basic Livelihood Security (/non-) | 3.30 (2.49–4.37) | 1.34 (0.93–1.93) | 2.18 (1.69–2.82) | 1.42 (1.03–1.96) |
| Socio-family relations | ||||
| Family contact < 1 time per month (/≥1 time) | 1.83 (1.45–2.31) | 1.28 (0.98–1.66) | 1.71 (1.40–2.10) | 1.25 (1.00–1.58) |
| Neighbor contact < 1 time per month (/≥1 time) | 1.21 (0.96–1.53) | 0.87 (0.65–1.15) | 1.55 (1.29–1.88) | 1.03 (0.82–1.30) |
| Friend contact < 1 time per month (/≥1 time) | 1.32 (1.04–1.67) | 0.91 (0.68–1.20) | 1.13 (0.94–1.37) | 1.05 (0.84–1.31) |
| Religious activity < 1 time per month (/≥1 time) | 0.92 (0.70–1.22) | 0.97 (0.71–1.33) | 1.22 (0.99–1.49) | 1.06 (0.85–1.32) |
| Friendship activity < 1 time per month (/≥1 time) | 1.70 (1.34–2.16) | 1.24 (0.93–1.65) | 1.43 (1.18–1.73) | 1.09 (0.87–1.36) |
| Leisure activity < 1 time per month (/≥1 time) | 1.29 (0.96–1.75) | 0.94 (0.66–1.33) | 1.35 (1.01–1.80) | 1.45 (1.05–2.01) |
| Charity activity < 1 time per month (/≥1 time) | 0.90 (0.53–1.53) | 0.90 (0.50–1.61) | 1.07 (0.72–1.59) | 0.67 (0.43–1.05) |
| Health behaviors | ||||
| Smoking status (/never smokers) | ||||
| Former smokers | 0.76 (0.52–1.13) | 0.80 (0.53–1.23) | 2.30 (1.63–3.25) | 1.62 (1.11–2.36) |
| Current smokers | 1.88 (1.34–2.650 | 1.54 (1.06–2.25) | 3.38 (2.63–4.33) | 1.69 (1.26–2.27) |
| Drinking frequency (/none) | ||||
| ≤ 1 time per wk | 1.13 (0.84–1.52) | 1.18 (0.84–1.66) | 1.13 (0.92–1.39) | 1.06 (0.83–1.34) |
| 2–3 times per wk | 0.96 (0.67–1.38) | 1.10 (0.73–1.66) | 2.38 (1.79–3.17) | 1.79 (1.27–2.52) |
| ≥ 4 times per wk | 1.41 (1.02–1.94) | 1.37 (0.95–1.98) | 2.99 (2.02–4.42) | 1.91 (1.21–3.01) |
| Moderate physical activity ≤ 2 times per wk (/≥ 3 times) | 1.35 (1.00–1.81) | - | 1.02 (0.81–1.29) | - |
| Walking activity ≤ 2 times per wk (/≥ 3 times) | 1.23 (0.98–1.55) | - | 0.84 (0.69–1.01) | - |
| Sleep duration (/7–8 hr) | ||||
| ≤ 6 hr per day | 1.50 (1.17–1.93) | 1.28 (0.98–1.67) | 1.17 (0.97–1.42) | 1.01 (0.82–1.24) |
| ≥ 9 hr per day | 1.76 (1.14–2.70) | 1.58 (0.99–2.54) | 1.03 (0.64–1.65) | 0.63 (0.38–1.04) |
| Health status | ||||
| Self-rated health (/good) | ||||
| Fair | 0.91 (0.64–1.30) | 0.85 (0.58–1.23) | 1.10 (0.82–1.46) | 0.96 (0.71–1.31) |
| Poor | 1.81 (1.33–2.48) | 1.06 (0.73–1.56) | 1.41 (1.08–1.86) | 1.19 (0.85–1.65) |
| Self-rated oral health (/good) | ||||
| Fair | 0.81 (0.54–1.21) | 0.89 (0.58–1.37) | 1.03 (0.78–1.37) | 0.99 (0.73–1.34) |
| Poor | 1.25 (0.89–1.74) | 1.02 (0.71–1.49) | 0.96 (0.73–1.25) | 0.85 (0.63–1.14) |
| Perceived usual stress (/little) | ||||
| Low | 0.65 (0.37–1.14) | 0.64 (0.35–1.14) | 1.04 (0.58–1.84) | 0.87 (0.48–1.59) |
| High | 2.05 (1.24–3.41) | 1.40 (0.82–2.39) | 2.16 (1.25–3.72) | 1.16 (0.66–2.05) |
| Very high | 3.69 (2.17–6.26) | 1.82 (1.02–3.23) | 6.00 (3.46–10.43) | 2.27 (1.27–4.06) |
| Experience of depressive mood (/no experience) | 3.92 (3.10–4.94) | 2.34 (1.81–3.03) | 4.28 (3.52–5.21) | 2.43 (1.96–3.01) |
| Body mass index (/18.5–24.9 kg/m2) | ||||
| ≤ 18.4 kg/m2 | 1.54 (1.04–2.28) | 1.28 (0.82–1.98) | 1.30 (0.96–1.77) | 1.07 (0.77–1.50) |
| ≥ 25.0 kg/m2 | 1.09 (0.84–1.41) | 1.07 (0.80–1.42) | 1.25 (1.01–1.54) | 1.08 (0.86–1.35) |
| Ever diagnosed with hypertension (/never) | 1.11 (0.87–1.41) | 1.08 (0.81–1.45) | 0.81 (0.66–0.99) | 1.04 (0.80–1.34) |
| Ever diagnosed with diabetes (/never) | 1.21 (0.90–1.63) | 1.08 (0.77–1.52) | 0.82 (0.62–1.10) | 0.82 (0.59–1.13) |
| Ever diagnosed with dyslipidemia (/never) | 0.95 (0.69–1.31) | 0.64 (0.44–0.93) | 1.14 (0.91–1.44) | 1.04 (0.80–1.36) |
| Ever diagnosed with stroke (/never) | 1.63 (1.08–2.45) | 1.48 (0.92–2.37) | 1.43 (0.93–2.20) | 1.32 (0.81–2.14) |
| Ever diagnosed with myocardial infarction (/never) | 1.65 (1.00–2.70) | 1.98 (1.14–3.43) | 1.78 (1.07–2.99) | 1.75 (0.99–3.11) |
| Ever diagnosed with osteoarthritis (/never) | 1.21 (0.88–1.66) | 0.98 (0.67–1.41) | 0.91 (0.75–1.11) | 0.97 (0.75–1.25) |
| Ever diagnosed with osteoporosis (/never) | 2.13 (1.34–3.39) | 2.07 (1.19–3.59) | 0.86 (0.68–1.07) | 1.07 (0.81–1.42) |
| Ever diagnosed with asthma (/never) | 0.79 (0.46–1.36) | 0.72 (0.40–1.30) | 1.55 (1.11–2.16) | 1.17 (0.80–1.69) |
| Ever diagnosed with hepatitis B (/never) | 1.45 (0.86–2.44) | 0.91 (0.51–1.60) | 1.24 (0.73–2.10) | 0.91 (0.52–1.60) |
| Ever diagnosed with depression (/never) | 5.14 (3.98–6.65) | 2.89 (2.16–3.87) | 6.34 (5.26–7.64) | 4.22 (3.44–5.19) |
Values are presented as OR (95% CI).
Less family contact (OR, 1.25; 95% CI, 1.00–1.58) and less leisure activity (OR, 1.45; 95% CI, 1.05–2.01) were positively associated with suicide attempts among females, while none of the socio-family relationships were associated with suicide attempts among males.
Compared with never smokers, suicide attempts were significantly higher among current smokers in both males and females and among former smokers in females only. Only females showed a significant increase in suicide attempts with drinking frequency. Compared with females who never drank alcohol, females who drank alcohol 2–3 times per week (OR, 1.79; 95% CI, 1.27–2.52) and ≥ 4 times per week (OR, 1.91; 95% CI, 1.21–3.01) had a significantly higher likelihood of suicide attempts.
Self-rated health and self-rated oral health were not associated with suicide attempts. However, psychological indices such as perceived usual stress, experience of depressive mood, and diagnosed, with depression were significantly associated with suicide attempts in both genders. Compared with participants with little stress, suicide attempts were significantly higher among those with very high stress in males (OR, 1.82; 95% CI, 1.02–3.23) and females (OR, 2.27; 95% CI, 1.27–4.06). Compared with participants without the experience of depressive mood, suicide attempts were significantly higher among those with depressive mood in males (OR, 2.34; 95% CI, 1.81–3.03) and females (OR, 2.43; 95% CI, 1.96–3.01). Having ever been diagnosed with depression was significantly associated with suicide attempts in both genders (OR, 2.89; 95% CI, 2.16–3.87 in males and OR, 4.22; 95% CI, 3.44–5.19 in females). Of the various chronic diseases evaluated in this study, participants who had ever been diagnosed with myocardial infarction (OR, 1.98; 95% CI, 1.14–3.43) and osteoporosis (OR, 2.07; 95% CI, 1.19–3.59) were significantly associated with suicide attempts only in males.
DISCUSSION
Suicide rates are higher among males than females in almost all countries (17) and the suicidal mortality for males is 2.4-fold higher than that for females in Korea (1). However, previous findings regarding the association between gender and suicide attempts have been inconsistent; some studies found that females have a greater risk for lifetime suicide attempts compared with males (5,6,8,10), while others found that gender was not associated with suicide attempts (7,11-13,15). Until now, the association between gender and suicide attempts had not been determined in Korea, although gender was not significantly associated with suicide attempts in this study (data not shown).
The suicide mortality per 100,000 persons in Korea increases with age from 4.5 deaths in those between the ages of 10 and 19 years to 78.6 deaths among those 80 years and over (1). Although a few studies have found no association between age and suicide attempts (8,11), many studies have reported that suicide attempts are predicted by a younger age (5,6,12,15). In this study, we found that suicide attempts were predicted by a younger age in both males and females, suggesting that younger age is a potent predictor of suicide attempts in both genders.
Studies have observed a significant association between marital status and suicide attempts, reporting that people who are unmarried, separated, or divorced are more likely to have suicide attempts than those who are married (3-5,10,12). However, other studies have found that marital status is not associated with suicide attempts (7,11,15). In the present study, males who were widowed, divorced, or separated participants had a higher risk for suicide attempts than that of male participants who were married, whereas the risk was lower risk for females. It is difficult to explain the opposing associations between marital status and suicide attempt according to gender in our study. One possible explanation is that males are more vulnerable after losing their spouse, while females are more likely to be supported by meaningful social and familial networks (18). In other words, compared with females, males have no safety social connections after marital breakdown. Another study also showed that divorce has a negative effect on suicidal mortality only among males (18). Further research is needed to confirm the gender-specific effect of marital status on suicide attempts.
A majority of studies have shown that education level is not independently associated with suicide attempts (7,8,10-13,15), while only one study reported a significant association (6). Lower levels of education are significantly associated with higher suicide rates in Korea (9), possibly because educational status has a more significant impact on social variables, such as occupation and income, in Korea than in other countries. In the present study, a lower level of education was an independent risk factor for suicide attempts in females, but not in males, suggesting that education level affects females more strongly.
Household economic status and financial problems are not associated with suicide attempts (8,13,15), although people with poor financial perceptions, compared with people with good financial perceptions, are more likely to have suicidal ideation (10). This study found that household income was significantly associated with suicide attempts in males but not in females. One possible explanation relies on traditional gender roles in Korea in which the family’s breadwinner is most often male. Only among males was unemployment a significant factor associated with suicide attempts in unadjusted models, although this association decreased after fully adjusting for other factors. Recipients of National Basic Livelihood Security System, which is the Korean social assistance system, were identified as being at risk for suicide attempts among females. Although there were gender differences in the factors associated with suicide attempts, the present results showed that socioeconomic status (SES) indicators such as education, income, employment, and social assistance, were significantly associated with suicide attempts. Previous research has shown that low SES characteristics are directly associated with the risks of suicide (19) and suicide attempts (14).
Strong connections with family and community support may be protective factors against suicide. This study found weak, but significant, associations for a low frequency of family contact and leisure activity with suicide attempts in females. Family discord is a significant risk factor of suicide in the elderly (20) and social integration (social interaction and religious involvement) is independently associated with suicide in adults (21). However, to date, few studies have examined the effects of socio-family environments on suicide attempts according to gender. Family conflict and a poor relationship with one’s family are more likely to be associated with suicidal ideation and suicide attempts (8,13). Significant associations of subjective (feeling) and objective (living alone or being without friends) loneliness have been found with suicidal ideation and suicide attempts (22) but social support is not significantly associated with either suicidal ideation or suicide attempts (15).
Smoking and risky alcohol consumption have been identified as risk factors for suicide mortality (23). We found that current smoking was associated with suicide attempts in both genders, while frequent drinking was associated in females, but not males. Smoking and alcohol were independently associated with suicide attempts in a meta-analysis (13) and alcohol-use disorders were found to be independently associated with suicide attempts (6). By contrast, it has been reported that neither suicidal ideation nor suicide attempts are predicted by alcohol disorders (12) or alcohol abuse (5). The correlation between unhealthy behaviors (smoking, alcohol abuse, and drug abuse) and psychiatric disorders might explain the relationships of smoking and alcohol consumption with suicide attempts (24).
A current review observed a significant link between life stressors and suicidal behaviors across different age groups and a wide range of countries (25). A stressful event may push a person over the edge and lead to and suicide attempts. The present results show that very high perceived usual stress was significantly associated with suicide attempts in both genders. Depression is a significant predictor of risk of death by suicide (2,26). In the present study, depression was a potent risk factor for suicide attempts in males and females. Moreover, in both genders, the experience of depressive mood was significantly associated with suicide attempts. These findings concur with previous studies reporting significant relationships between depression and suicide attempts (5,8,11,12,15). In a path analysis of elderly subjects, depressive symptoms had the strongest influence on suicidal ideation and suicide attempts (27). In addition, both major and minor depression disorders are significant predictors of suicide in the old elderly (28) and depressive mood is independently associated with suicidal ideation in the general population (29).
Serious physical illness is also a significant predictor of suicide in the old elderly (28). Major physical diseases such as cancer and coronary heart disease significantly elevate the risk of suicide, particularly among women (30). In the present study, however, myocardial infarction and osteoporosis were significantly associated with suicide attempts. More severe chronic diseases are associated with a higher risk of suicide attempts (8), while some studies have shown that physical illnesses or multimorbidity is not associated with suicide attempts (13,15).
Several limitations should be considered when interpreting the present findings. First, the cross-sectional design used in this study prohibited the assessment of causal relationships, and thus it is uncertain whether the identified risk factors were present prior to the occurrences of suicidal ideation and suicide attempts. Second, because the information regarding suicide attempts was retrospectively assessed by self-report, it is possible that there was a recall bias. Third, information about suicide attempts was collected from only those who survived a suicide attempt because suicidal behaviors could not be evaluated from those who completed a suicide. Fourth, it was assumed that only subjects with suicidal ideation would attempt suicide, and as a result, impulsive suicidal attempts without suicidal ideation were not evaluated. However, when the associations between the studied risk factors and suicidal attempts were further analyzed including small numbers of impulsive suicidal attempts without suicidal ideation, similar findings were observed. Despite these limitations, the present study has several strengths. Data from a national survey were used, and thus a large nationally representative sample of the general population was evaluated. In addition, multiple covariates such as sociodemographic information, socio-family relationships, health behaviors, and various health statuses were simultaneously investigated according to gender.
In conclusion, this study identified gender-specific poorly understood risk factors for suicide attempts that may be useful for policy-making and suicide prevention. Gender differences should be considered in the assessment, prevention, and management of future suicide attempts by community policy-makers and clinicians. Further longitudinal studies are needed to characterize the gender-specific causal relationships between risk factors and suicidal behaviors fully.
Footnotes
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Study conception and design: Lee YH. Data acquisition: Kim M, Oh GJ. Data analysis and interpretation: Kim M, Oh GJ, Lee YH. Writing the draft: Kim M. Manuscript review and revision: Oh GJ, Lee YH. Approval of final manuscript: all authors.
References
- 1.Statistics Korea. Annual report on the cause of death statistics: 2014 [Internet] [accessed on 30 July 2016]. Available at http://kosis.kr.
- 2.Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventive interventions: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42:386–405. doi: 10.1097/01.CHI.0000046821.95464.CF. [DOI] [PubMed] [Google Scholar]
- 3.Weissman MM, Bland RC, Canino GJ, Greenwald S, Hwu HG, Joyce PR, Karam EG, Lee CK, Lellouch J, Lepine JP, et al. Prevalence of suicide ideation and suicide attempts in nine countries. Psychol Med. 1999;29:9–17. doi: 10.1017/s0033291798007867. [DOI] [PubMed] [Google Scholar]
- 4.Kjøller M, Helweg-Larsen M. Suicidal ideation and suicide attempts among adult Danes. Scand J Public Health. 2000;28:54–61. doi: 10.1177/140349480002800110. [DOI] [PubMed] [Google Scholar]
- 5.Bernal M, Haro JM, Bernert S, Brugha T, de Graaf R, Bruffaerts R, Lépine JP, de Girolamo G, Vilagut G, Gasquet I, et al. Risk factors for suicidality in Europe: results from the ESEMED study. J Affect Disord. 2007;101:27–34. doi: 10.1016/j.jad.2006.09.018. [DOI] [PubMed] [Google Scholar]
- 6.Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, Bruffaerts R, Chiu WT, de Girolamo G, Gluzman S, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192:98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scocco P, de Girolamo G, Vilagut G, Alonso J. Prevalence of suicide ideation, plans, and attempts and related risk factors in Italy: results from the European study on the epidemiology of mental disorders--world mental health study. Compr Psychiatry. 2008;49:13–21. doi: 10.1016/j.comppsych.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 8.Cheng JK, Fancher TL, Ratanasen M, Conner KR, Duberstein PR, Sue S, Takeuchi D. Lifetime suicidal ideation and suicide attempts in Asian Americans. Asian Am J Psychol. 2010;1:18–30. doi: 10.1037/a0018799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim MH, Jung-Choi K, Jun HJ, Kawachi I. Socioeconomic inequalities in suicidal ideation, parasuicides, and completed suicides in South Korea. Soc Sci Med. 2010;70:1254–1261. doi: 10.1016/j.socscimed.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 10.Dai J, Chiu HF, Conner KR, Chan SS, Hou ZJ, Yu X, Caine ED. Suicidal ideation and attempts among rural Chinese aged 16-34 years--socio-demographic correlates in the context of a transforming China. J Affect Disord. 2011;130:438–446. doi: 10.1016/j.jad.2010.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vera M, Reyes-Rabanillo ML, Huertas S, Juarbe D, Pérez-Pedrogo C, Huertas A, Peña M. Suicide ideation, plans, and attempts among general practice patients with chronic health conditions in Puerto Rico. Int J Gen Med. 2011;4:197–205. doi: 10.2147/IJGM.S17156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Handley TE, Inder KJ, Kay-Lambkin FJ, Stain HJ, Fitzgerald M, Lewin TJ, Attia JR, Kelly BJ. Contributors to suicidality in rural communities: beyond the effects of depression. BMC Psychiatry. 2012;12:105. doi: 10.1186/1471-244X-12-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li Y, Li Y, Cao J. Factors associated with suicidal behaviors in mainland China: a meta-analysis. BMC Public Health. 2012;12:524. doi: 10.1186/1471-2458-12-524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aschan L, Goodwin L, Cross S, Moran P, Hotopf M, Hatch SL. Suicidal behaviours in South East London: prevalence, risk factors and the role of socio-economic status. J Affect Disord. 2013;150:441–449. doi: 10.1016/j.jad.2013.04.037. [DOI] [PubMed] [Google Scholar]
- 15.Miret M, Caballero FF, Huerta-Ramírez R, Moneta MV, Olaya B, Chatterji S, Haro JM, Ayuso-Mateos JL. Factors associated with suicidal ideation and attempts in Spain for different age groups. Prevalence before and after the onset of the economic crisis. J Affect Disord. 2014;163:1–9. doi: 10.1016/j.jad.2014.03.045. [DOI] [PubMed] [Google Scholar]
- 16.Cho HD, Kim NY, Gil HW, Jeong DS, Hong SY. Comparison of families with and without a suicide prevention plan following a suicidal attempt by a family member. J Korean Med Sci. 2015;30:974–978. doi: 10.3346/jkms.2015.30.7.974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiol Rev. 2008;30:133–154. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kposowa AJ. Marital status and suicide in the national longitudinal mortality study. J Epidemiol Community Health. 2000;54:254–261. doi: 10.1136/jech.54.4.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lorant V, Kunst AE, Huisman M, Costa G, Mackenbach J. EU Working Group on Socio-Economic Inequalities in Health. Socio-economic inequalities in suicide: a European comparative study. Br J Psychiatry. 2005;187:49–54. doi: 10.1192/bjp.187.1.49. [DOI] [PubMed] [Google Scholar]
- 20.Rubenowitz E, Waern M, Wilhelmson K, Allebeck P. Life events and psychosocial factors in elderly suicides--a case-control study. Psychol Med. 2001;31:1193–1202. doi: 10.1017/s0033291701004457. [DOI] [PubMed] [Google Scholar]
- 21.Duberstein PR, Conwell Y, Conner KR, Eberly S, Evinger JS, Caine ED. Poor social integration and suicide: fact or artifact? A case-control study. Psychol Med. 2004;34:1331–1337. doi: 10.1017/s0033291704002600. [DOI] [PubMed] [Google Scholar]
- 22.Stravynski A, Boyer R. Loneliness in relation to suicide ideation and parasuicide: a population-wide study. Suicide Life Threat Behav. 2001;31:32–40. doi: 10.1521/suli.31.1.32.21312. [DOI] [PubMed] [Google Scholar]
- 23.Schneider B, Baumert J, Schneider A, Marten-Mittag B, Meisinger C, Erazo N, Hammer GP, Ladwig KH. The effect of risky alcohol use and smoking on suicide risk: findings from the German MONICA/KORA-Augsburg cohort study. Soc Psychiatry Psychiatr Epidemiol. 2011;46:1127–1132. doi: 10.1007/s00127-010-0287-y. [DOI] [PubMed] [Google Scholar]
- 24.Wolitzky-Taylor K, Bobova L, Zinbarg RE, Mineka S, Craske MG. Longitudinal investigation of the impact of anxiety and mood disorders in adolescence on subsequent substance use disorder onset and vice versa. Addict Behav. 2012;37:982–985. doi: 10.1016/j.addbeh.2012.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu RT, Miller I. Life events and suicidal ideation and behavior: a systematic review. Clin Psychol Rev. 2014;34:181–192. doi: 10.1016/j.cpr.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 26.Beautrais AL. Suicides and serious suicide attempts: two populations or one? Psychol Med. 2001;31:837–845. doi: 10.1017/s0033291701003889. [DOI] [PubMed] [Google Scholar]
- 27.Ro J, Park J, Lee J, Jung H. Factors that affect suicidal attempt risk among Korean elderly adults: a path analysis. J Prev Med Public Health. 2015;48:28–37. doi: 10.3961/jpmph.14.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Waern M, Rubenowitz E, Wilhelmson K. Predictors of suicide in the old elderly. Gerontology. 2003;49:328–334. doi: 10.1159/000071715. [DOI] [PubMed] [Google Scholar]
- 29.Bae SM, Lee YJ, Cho IH, Kim SJ, Im JS, Cho SJ. Risk factors for suicidal ideation of the general population. J Korean Med Sci. 2013;28:602–607. doi: 10.3346/jkms.2013.28.4.602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Webb RT, Kontopantelis E, Doran T, Qin P, Creed F, Kapur N. Suicide risk in primary care patients with major physical diseases: a case-control study. Arch Gen Psychiatry. 2012;69:256–264. doi: 10.1001/archgenpsychiatry.2011.1561. [DOI] [PubMed] [Google Scholar]