Abstract
Background and Objectives:
Laparoscopic transcystic common bile duct exploration (LTCBDE) is a complex procedure requiring expertise in laparoscopic and choledochoscopic skills. The purpose of this study was to investigate the safety and feasibility of treating biliary calculi through laparoscopic transcystic exploration of the CBD via an ultrathin choledochoscope combined with dual-frequency laser lithotripsy.
Methods:
From August 2011 through September 2014, 89 patients at our hospital were treated for cholecystolithiasis with biliary calculi. Patients underwent laparoscopic cholecystectomy and exploration of the CBD via the cystic duct and the choledochoscope instrument channel. A dual-band, dual-pulse laser lithotripsy system was used to destroy the calculi. Two intermittent laser emissions (intensity, 0.12 J; pulse width 1.2 μs; and pulse frequency, 10 Hz) were applied during each contact with the calculi. The stones were washed out by water injection or removed by a stone-retrieval basket.
Results:
Biliary calculi were removed in 1 treatment in all 89 patients. No biliary tract injury or bile leakage was observed. Follow-up examination with type-B ultrasonography or magnetic resonance cholangiopancreatography 3 months after surgery revealed no instances of retained-calculi–related biliary tract stenosis.
Conclusion:
The combined use of laparoscopic transcystic CBD exploration by ultrathin choledochoscopy and dual-frequency laser lithotripsy offers an accurate, convenient, safe, effective method of treating biliary calculi.
Keywords: Biliary calculi, Dual-frequency laser, Laparoscope, Transcystic common bile duct exploration, Ultrathin choledochoscope
INTRODUCTION
With the development of minimally invasive surgical technology, laparoscopic cholecystectomy (LC) plus laparoscopic transcystic common bile duct exploration (LTCBDE) has become the first-choice treatment for cholecystolithiasis combined with biliary calculi.1,2 However, the LTCBDE operation is relatively complicated, requiring that surgeons be proficient in laparoscopic and choledochoscopic skills. Moreover, there are specific anatomic requirements of the cystic duct that must be met for the operation to be successful. For example, it is easy to insert an ultrathin (2.8- or 3.7-mm diameter) choledochoscope into the cystic and then the CBD. However, calculi that are large (>6 mm), hard, or incarcerated in the bile duct can be difficult to extract because they cannot be encased in the stone-retrieval basket. Even if they were to be encased, these calculi would be difficult to extract via the cystic duct, as extraction could cause the laceration of the junction between the cystic duct and the CBD.
Our hospital has applied dual-frequency laser lithotripsy in combination with ultrathin choledochoscope exploration of biliary calculi. This article reports our findings from using this technique.
MATERIALS AND METHODS
Study Design and Ethical Considerations
This study was designed as a retrospective cohort study of patients who underwent dual-pulse laser lithotripsy combined with ultrathin choledochoscopy of the CBD for treatment of biliary calculi. Although the best approach for treating cholecystocholedocholithiasis remains a matter of debate, we favor LTCBDE for the treatment of biliary calculi. LTCBDE with laser lithotripsy is better than some techniques, such as laparoscopic choledochendysis or endoscopic retrograde cholangiopancreatography and endoscopic sphincterotomy (ERCP+EST). Consecutive patients with cholecystolithiasis and biliary calculi who underwent these interventions at our hospital from August 2011 through September 2014 were considered for inclusion in the study. In total, 248 patients underwent LC+LTCBDE. All patients underwent LC, 140 patients were treated with traditional transcystic methods, and 89 patients underwent transcystic exploration by lithotripsy. Furthermore, 12 patients underwent choledochotomy, and 7 underwent a 2-stage procedure (ERCP+EST followed by LC). In all patients, biliary calculi were removed and cleaned through these methods of CBD exploration. The experimental protocol was approved by the Institutional Human Ethics Committee.
Patient Selection
Patients were included in this study if they had a diagnosis of cholecystolithiasis; were in need of bile duct exploratory lithotomy; were in good general condition [Karnofsky Performance Score (KPS) > 70]; received LC+LTCBDE; and did not have any contraindications for surgery. Patients were excluded if a simple choledochoscopy was sufficient to remove the calculi from the bile duct completely; bile duct exploration could not be completed via the cystic duct or required laparoscopic incision of the CBD; or there was conversion to laparotomy.
Surgical Method
A flexible 2.8- or 3.7-mm choledochoscope (CHF-CB30 or CHF-XP20; Olympus, Tokyo, Japan) and a German WOM U100 Plus (FREDDY; Trust Medical, Wuppertal, Germany) dual-band, dual-pulse laser (420-μm optical fiber) were used. The patient was placed supine with raised head and lowered feet. After anesthesia, Veress needle puncture was used to establish a CO2 pneumoperitoneum with a gas pressure of 12 mm Hg.
The conventional four-hole method was used. The trocar below the rib at the right midclavicular line was placed closer to the costal margin than in simple LC surgery, to facilitate choledochoscopic exploration.
The cystic artery was occluded and then cut. The cystic duct was occluded near the gallbladder, which was stretched flat. At a position 5 mm from the CBD, half the circumference of the anterior wall of the cystic duct was incised. Then, 2 to 3 mm of the long diameter was incised along the cystic duct toward the side of the CBD, to create a T-shaped cystic duct incision (Figure 1). A needle was used to suture the anterior lower wall of the incised cystic duct.
Figure 1.
Incision of the cystic duct.
The trocar was inserted deep into the abdominal cavity through a port in the right upper abdomen. The choledochoscope was inserted through this trocar to perform bile duct exploration (Figures 2, 3). A laser fiber was inserted into the instrument channel of the choledochoscope and extended about 1 cm beyond the choledochoscope (Figure 4). Normal saline was provided continuously for washing. Calculi were carefully moved against one side of the bile duct wall or close to the papilla. The fiber was targeted to the center of the calculus for firing. Two intermittent laser emissions were given for each contact with the calculi with the following settings: laser energy intensity, 0.12 J; pulse width, 1.2 μs; and pulse frequency, 10 Hz. This process facilitated extraction of the calculi by the stone basket.
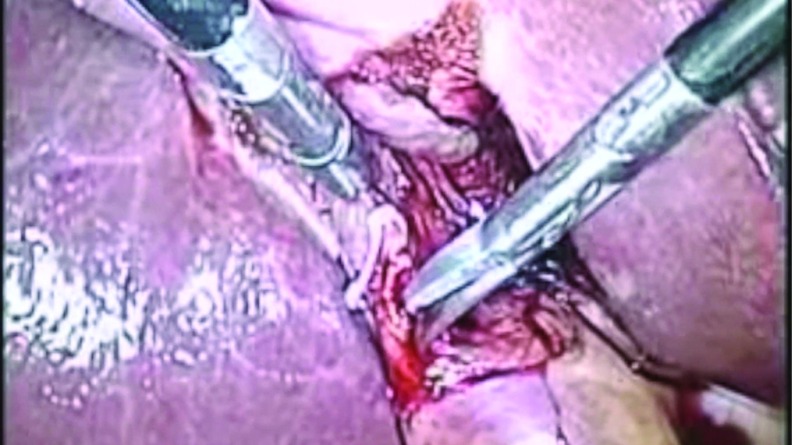
Figure 2.
Placement of the choledochoscope in the CBD via a transcystic approach.
Figure 3.
Visualization of a stone in the CBD with a choledochoscope.
Figure 4.
Insertion of laser fiber into the CBD through the choledochoscope working port.
We attempted to insert the choledochoscope into the duodenum via the sphincter of Oddi. The duodenal papilla was dilated to facilitate intra–bile duct washing. Under appropriate conditions, the choledochoscope can be inverted to explore the common hepatic duct and intrahepatic bile duct. Finally, the choledochoscope was withdrawn, the cystic duct was occluded by a Ham-lock clip, and the gallbladder was removed. A drainage tube was not placed. Postoperative treatment was similar to that of simple LC treatment.
We did not perform intraoperative cholangiography routinely. We did not use balloon dilators on the cystic duct.
RESULTS
Patient Characteristics
The study cohort included 89 patients (48 men, 41 women; age range: 29–75 years; mean age: 52.4 years). Among them, 41 patients (46.1%) did not experience symptoms of acute cholecystitis or cholangitis and had not had any severe clinical symptoms for the prior 6 months. They had experienced only intermittent, mild postprandial abdominal distension and dull pain and discomfort, which would resolve on its own without treatment. Another 39 patients (43.8%) reported stomach ache, jaundice, and fever in the 2–3 months before undergoing surgery, which was achieved by conservative treatment. In addition, 9 patients (10.1%) had acute cholecystitis and cholangitis, and they underwent surgery within 2–6 days of receiving pharmacotherapy. The remaining 5 patients (5.6%) underwent immediate nasobiliary drainage.
Preoperative type-B ultrasonography and biliary tract magnetic resonance cholangiopancreatography (MRCP) detected calculi of the CBD in 72 patients (80.9%). Calculi were found in the CBD and common hepatic duct in 3 patients (3.4%) and in the CBD and grade II hepatic duct in 1 patient (1.1%). Preoperative B ultrasonography and MRCP failed to identify any biliary abnormality in 3 patients (3.4%), who had histories of acute biliary pancreatitis (2 patients) or jaundice (1 patient). Ten patients (11.2%) had metal implants and were thus unable to undergo MRCP; therefore, only type-B ultrasonography was used for these patients. Biliary calculi were not observed in these 10 patients. Half of this group of patients (5/10) exhibited widening of the CBD (diameter > 8 mm). Meanwhile, 3 of the 10 patients had a history of acute biliary pancreatitis, and 1 had a history of jaundice. One patient had abnormal liver function.
Surgical Outcomes
Surgeries were successful in all 89 cases. No calculi were detected in 13 patients during preoperative examination. Calculi were found in the CBD alone in 84 patients (94.4%), with a calculus diameter ranging from 0.2 to 1.3 cm. The number of calculi ranged from 1 calculus in 61 patients to 2–5 calculi in 23 patients. In those 84 patients, all calculi were located in the middle to lower segment of the CBD. Four patients (4.5%) had calculi in both the common hepatic duct and CBD. These patients had 2 to 4 calculi, with diameters ranging from 0.3 to 0.8 cm. One patient (1.1%) had 3 calculi, located in the common bile and left hepatic ducts. Calculus diameter in this patient ranged from 0.3 to 0.7 cm (Table 1).
Table 1.
Calculi Characteristics
| Parameter | Stone Location |
||
|---|---|---|---|
| CBD Only | CBD + CHD | CBD + LHD | |
| Patients, n | 84 | 2 | 1 |
| Stones per patient, n | 1–5 | 2 and 4 | 3 |
| Stone size, cm | 0.2–1.3 | 0.3–0.8 | 0.3–0.7 |
CHD, common hepatic duct; LHD, left hepatic duct.
All calculi in the bile duct were extracted after lithotripsy. In 77 cases, the choledochoscope could reach the duodenum through the sphincter of Oddi or the duodenal papilla. In these cases, the stone fragments were easily washed into the duodenum. In another 12 cases, the choledochoscope could not enter the duodenum, but the retrieval basket could be inserted in the duodenum. The duration of surgery ranged from 69 to 140 min (mean, 115 min). The blood volume lost ranged from 10 to 60 mL (mean, 17 mL). No complications, such as biliary tract injury, bile leakage, or hemobilia, were observed.
Postoperative and Follow-up Outcomes
Seventy-nine patients were able to consume food and were discharged on the first day after surgery without additional therapy. On the first postoperative day, 4 patients had elevated liver transaminase levels (ALT: 66–124 U/L, AST: 71–125 U/L [ normal ALT and AST: 0–40 U/L]) and 2 patients had elevated bilirubin levels (direct bilirubin: 9.67–11.56 μmol/L [normal: 0–6.84 μmol/L], indirect bilirubin: 23.6–29.5 μmol/L [normal: 0–12 μmol/L]). These elevated levels returned to normal after 2 d of therapy. The patients were discharged on postoperative day 3. Four patients had significant increases in postoperative white blood cell levels (13.4 × 109/L–15.8 × 109/L) plus fever (37.8–38.3°C), which were resolved by antibiotic treatment.
All patients were followed-up in the clinic 3 months after surgery and had no clinical symptoms at that time. In addition, neither type-B ultrasonography nor MRCP indicated retained calculi in the biliary tract. At the patients' 1-year follow-up evaluations, no biliary calculi were observed by type-B ultrasonography (67 patients) or MRCP (22 patients).
Discussion
We combined the ultrathin choledochoscope with dual-band, dual-pulse laser lithotripsy to treat relatively large calculi by a transcystic approach. LC with LTCBDE was successful in all 89 cases, with gallbladder and biliary calculi being eliminated in a single treatment. Successful calculus removal was achieved in all patients, with no case of biliary tract injury or bile leakage. Three months after the operations, there were no cases of retained calculi in the biliary tract or biliary tract stenosis.
Since it was first reported in 1991,3 CBD exploration by a laparoscopic transcystic approach has been widely applied. Patients undergoing this technique experience a short hospitalization time and quick recovery after surgery. Surgical trauma is minimal and similar to that generated by LC. There are many advantages to using the cystic duct in bile duct exploration. Use of this duct avoids the iatrogenic injuries induced by CBD incision and the possible adverse results arising from T-tubule placement. The cystic duct approach maintains the integrity and normal physiological function of the biliary tract, while avoiding the trauma and pain induced by invasive treatments, such as ERCP+EST, and maintaining the function of the sphincter of Oddi.4
LC+LTCBDE is the first-choice treatment for cholecystolithiasis plus calculus of the bile duct.1,2,5–8 Although it boasts great advantages, its use is limited by its strict anatomical requirements for the cystic duct. Some circumstances that make it difficult for a choledochoscope to enter the cystic duct include an undersized lumen, distortion or obstruction of the cystic duct, inflammation-induced wall thickening or luminal stenosis, alterations of the Heister valve, as well as anatomic variations or serious adhesions at the junction between the cystic duct and CBD.
The reported success rate of LTCBDE is highly variable.8–10 At our hospital, the success rate exceeds 90%.11 We have performed LTCBDE on nearly 1000 patients and have accumulated abundant experience, especially in the application of the ultrathin choledochoscope. The fine caliber of this instrument facilitates insertion into and penetration of the cystic duct, movement and torsion in the cystic duct and CBD, and exploration of the common hepatic duct and intrahepatic bile duct via instrument inversion.
We found that the use of an ultrathin choledochoscope can improve the success rate of cystic duct entry. However, calculi that are large, have a cast form, or are incarcerated in the duodenal papilla are difficult to retrieve because of difficulty in opening the basket or extracting calculi via the cystic duct. Forceful retrieval can rupture the cystic duct and CBD, increasing the risk of injury and making it difficult to occlude the cystic duct. Although it is convenient to use a conventional, 4.9-mm diameter choledochoscope to extract calculi, this instrument sometimes is difficult to insert into the CBD via the cystic duct. As a result, a microincision is needed at the junction. The incision is extended to the lateral wall of the CBD, which increases the probability of bile duct injury and difficulty in occlusion.
Use of laser devices for biliary lithotripsy have been reported since the 1980s.12–14 Reports have described the combined use of a choledochoscope with lithotripsy in treating calculi of the bile duct.15,16 The dual-band, dual-pulse laser lithotripsy developed in the 1990s has replaced the holmium laser as the optimal laser lithotripsy method. Moreover, this method is more suitable for use in treating biliary calculi.17,18 The dual-band, dual-pulse laser lithotripsy system is a pulse Nd:YAG laser generator. In essence, pulse laser plasma shockwave lithotripsy technology uses mechanical energy, rather than thermal cracking. A short-wavelength (532 nm, 20% energy) laser is used to irradiate the calculi and form a plasma zone on the surface. Then, a long-wavelength (1064 nm, 80% energy) laser is used to irradiate the preformed plasma zone. Infrared light energy is fully absorbed, and the ion and electron volumes in this zone are rapidly expanded to generate a mechanical shockwave to crush the calculi. This technique is effective for most calculi in the human body (with the exception of cystine calculi, eg, cholesterol and calcium, uric acid, and bile pigment calculi) and is applicable to biliary tract lithotripsy.
Although some normal soft tissues can absorb only a low amount of dual-wavelength laser energy, the use of pulse-wave laser emission rarely results in thermal injury to surrounding tissues, which can occur with continuous laser radiation lithotripsy. Continuous flushing with normal saline prevents injury to surrounding tissues, such as the bile duct wall. When the laser fiber was aimed directly at rabbit bladder mucosa, mild mucosal engorgement and edema were observed, but no perforation or injury of the muscle layers.19–21
The dual-frequency, 420-nm laser fiber is soft and pliable. It can cooperate well enough with the choledochoscope to pass the 1.2-mm operation hole of the choledochoscope. The hydrogalvanic microblasting guide wire that is commonly used in lithotripsy cannot pass the operation hole of the ultrathin choledochoscope. Holmium laser fiber can enter and exit the choledochoscope without any obstruction and generate good lithotripsy effects, but this fiber causes injury, bleeding, and perforation of the bile duct wall.
Some precautions must be taken when performing this surgery in patients. First, the laser fiber should be about 1 cm beyond the choledochoscope to avoid damage to the scope. Second, the calculi should be pushed to the lower segment of the bile duct or fixed to the bile duct wall to reduce drifting and movement. Reducing movement will improve the lithotripsy effects by allowing the optical fiber to focus persistently on the calculi. Third, under direct vision, the optical fiber should be fired at the center of the calculus. Calculi can be easily destroyed by continuous impact targeted at one point. Firing at the side wall of the calculi is less effective at destroying the calculi and increases the probability of injury to the bile duct wall. Fourth, calculi can be crushed into smaller masses of 4–5 mm in diameter for easy extraction. Crushing calculi into smaller masses, however, makes basket retrieval of the masses very difficult. Fifth, hepatic duct calculi should be washed with normal saline or brought by the basket into the CBD and then crushed and extracted. Finally, one should attempt to pass the choledochoscope into the duodenum via the duodenal papilla while dilating the sphincter of Oddi, to facilitate washing of the bile duct and discharge of fine calculus debris. If the duodenal papilla does not markedly deviate and there is no inflammatory stenosis in the lower end of the bile duct or sphincter of Oddi, then the choledochoscope should be able to pass the papilla.
Conclusion
Application of laparoscopy and the ultrathin choledochoscope in combination with dual-band, dual-pulse laser lithotripsy via a transcystic approach is a safe, feasible, and highly effective technique for treating gallbladder and biliary tract calculi, especially those that are difficult to extract. This approach is characterized by minimal trauma, quick recovery, and very good clinical efficacy. It should be considered for extensive use and as one of the best choices to treat cholecystolithiasis and secondary bile duct stones.
Acknowledgments
The authors thank Medjaden Bioscience Limited for scientific editing of the manuscript.
Contributor Information
Jun Liu, Department of General Surgery, Beijing Friendship Hospital, Capital Medicine University Beijing, China..
Lan Jin, Department of General Surgery, Beijing Friendship Hospital, Capital Medicine University Beijing, China..
Zhongtao Zhang, Department of General Surgery, Beijing Friendship Hospital, Capital Medicine University Beijing, China..
References:
- 1. Chiarugi M, Galatioto C, Decanini L, et al. Laparoscopic transcystic exploration for single-stage management of common duct stones and acute cholecystitis. Surg Endosc. 2012;26:124–129. [DOI] [PubMed] [Google Scholar]
- 2. Kroh M, Chalikonda S, Chand B, Walsh RM. Laparoscopic completion cholecystectomy and CBD exploration for retained gallbladder after single-incision cholecystectomy. JSLS. 2013;17:143–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fletcher DR. Percutaneous (laparoscopic) cholecystectomy and exploration of the common bile duct: the common bile duct stone reclaimed for the surgeon. Aust N Z J Surg. 1991;61:814–815. [DOI] [PubMed] [Google Scholar]
- 4. Petelin JB. Laparoscopic common bile duct exploration. Surg Endosc. 2003;17:1705–1715. [DOI] [PubMed] [Google Scholar]
- 5. Mattila A, Luhtala J, Mrena J, Kautiainen H, Kellokumpu I. An audit of short- and long-term outcomes after laparoscopic removal of common bile duct stones in Finland. Surg Endosc. 2014;28:3451–3457. [DOI] [PubMed] [Google Scholar]
- 6. Reinders JS, Gouma DJ, Ubbink DT, van Ramshorst B, Boerma D. Transcystic or transductal stone extraction during single-stage treatment of choledochocystolithiasis: a systematic review. World J Surg. 2014;38:2403–2411. [DOI] [PubMed] [Google Scholar]
- 7. Zhu JG, Han W, Zhang ZT, Guo W, Liu W, Li J. Short-term outcomes of laparoscopic transcystic common bile duct exploration with discharge less than 24 hours. J Laparoendosc Adv Surg Tech A. 2014;24:302–305. [DOI] [PubMed] [Google Scholar]
- 8. Hanif F, Ahmed Z, Samie MA, Nassar AH. Laparoscopic transcystic bile duct exploration: the treatment of first choice for common bile duct stones. Surg Endosc. 2010;24:1552–1556. [DOI] [PubMed] [Google Scholar]
- 9. Paganini AM, Guerrieri M, Sarnari J, et al. Thirteen years' experience with laparoscopic transcystic common bile duct exploration for stones: effectiveness and long-term results. Surg Endosc. 2007;21:34–40. [DOI] [PubMed] [Google Scholar]
- 10. Han W, Zhang ZT, Li JS, et al. The surgical skills of transcystic approach with intra-operative choledochoscope in laparoscopic common bile duct exploration: an analysis of 292 cases. Chin J Pract Surg. 2010;30:200–202. [Google Scholar]
- 11. Guo W, Han W, Jin L, et al. Laparoscopic transcystic common bile duct exploration: a report of 546 cases. J Surg Concepts Pract. 2011;16:359–361. [Google Scholar]
- 12. Birkett DH. Biliary laser lithotripsy. Surg Clin North Am. 1992;72:641–654. [DOI] [PubMed] [Google Scholar]
- 13. Josephs LG, Birkett DH. Laser lithotripsy for the management of retained stones. Arch Surg. 1992;127:603–604, discussion 604–605. [DOI] [PubMed] [Google Scholar]
- 14. Lanzafame RJ. Applications of lasers in laparoscopic cholecystectomy. J Laparoendosc Surg. 1990;1:33–36. [DOI] [PubMed] [Google Scholar]
- 15. Ji YC, Liu C, Xu J, Wan HK, Yin HL. Laparoscopy combined with choledochofiberoscopy for Holmium Laser Cholelithotripsy: report of 16 Cases. Chin J Min Inv Surg. 2012;12:730–732. [Google Scholar]
- 16. Varban O, Assimos D, Passman C, Westcott C. Laparoscopic common bile duct exploration and holmium laser lithotripsy: a novel approach to the management of common bile duct stones (video). Surg Endosc. 2010;24:1759–1764. [DOI] [PubMed] [Google Scholar]
- 17. Jiang ZJ, Chen Y, Wang WL, et al. Management hepatolithiasis with operative choledochoscopic FREDDY laser lithotripsy combined with or without hepatectomy. Hepatobiliary Pancreat Dis Int. 2013;12:160–164. [DOI] [PubMed] [Google Scholar]
- 18. Liu F, Jin ZD, Zou DW, Li ZS. Efficacy and safety of endoscopic biliary lithotripsy using FREDDY laser with a radiopaque mark under fluoroscopic guidance. Endoscopy. 2011;43:918–921. [DOI] [PubMed] [Google Scholar]
- 19. Wang MJ, Naim JO, Rogers DW, Lanzafame RJ. The effect of Nd:YAG laser-induced hyperthermia on local tumor recurrence in experimental rat mammary tumors. J Clin Laser Med Surg. 1992;10:265–268. [DOI] [PubMed] [Google Scholar]
- 20. Lanzafame RJ, Naim J. Preliminary assessment of the tissue effects of a 1.44-micron laser via direct fiber contact on soft tissue. J Clin Laser Med Surg. 1997;15:23–27. [DOI] [PubMed] [Google Scholar]
- 21. Zorcher T, Hochberger J, Schrott KM, Kuhn R, Schafhauser W. In vitro study concerning the efficiency of the frequency-doubled double-pulse Neodymium:YAG laser (FREDDY) for lithotripsy of calculi in the urinary tract. Lasers Surg Med. 1999;25:38–42. [DOI] [PubMed] [Google Scholar]