Abstract
The objective of this systematic review was to determine if dairy product consumption is detrimental, neutral, or beneficial to cardiovascular health and if the recommendation to consume reduced-fat as opposed to regular-fat dairy is evidence-based. A systematic review of meta-analyses of prospective population studies associating dairy consumption with cardiovascular disease (CVD), coronary artery disease (CAD), stroke, hypertension, metabolic syndrome (MetS), and type 2 diabetes (T2D) was conducted on the basis of the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement. Quality of evidence was rated by using the Grading of Recommendations Assessment, Development, and Evaluation scale. High-quality evidence supports favorable associations between total dairy intake and hypertension risk and between low-fat dairy and yogurt intake and the risk of T2D. Moderate-quality evidence suggests favorable associations between intakes of total dairy, low-fat dairy, cheese, and fermented dairy and the risk of stroke; intakes of low-fat dairy and milk and the risk of hypertension; total dairy and milk consumption and the risk of MetS; and total dairy and cheese and the risk of T2D. High- to moderate-quality evidence supports neutral associations between the consumption of total dairy, cheese, and yogurt and CVD risk; the consumption of any form of dairy, except for fermented, and CAD risk; the consumption of regular- and high-fat dairy, milk, and yogurt and stroke risk; the consumption of regular- and high-fat dairy, cheese, yogurt, and fermented dairy and hypertension risk; and the consumption of regular- and high-fat dairy, milk, and fermented dairy and T2D risk. Data from this systematic review indicate that the consumption of various forms of dairy products shows either favorable or neutral associations with cardiovascular-related clinical outcomes. The review also emphasizes that further research is urgently needed to compare the impact of low-fat with regular- and high-fat dairy on cardiovascular-related clinical outcomes in light of current recommendations to consume low-fat dairy.
Keywords: dairy, milk, cheese, yogurt, cardiovascular disease, coronary artery disease, stroke, hypertension, metabolic syndrome, type 2 diabetes
Introduction
The consumption of dairy, particularly low-fat dairy, is advocated in most dietary guidelines around the world. The main argument supporting the recommendation to consume low-fat dairy is that high plasma LDL-cholesterol concentrations are a key risk factor for coronary artery disease (CAD)8 and that regular- and high-fat dairy foods are a major source of cholesterol-increasing SFAs (1, 2). Although there is little doubt about the LDL cholesterol–increasing effects of SFAs per se, the extent to which the consumption of different forms of dairy products, including regular- and low-fat dairy, influences the risk of cardiovascular-related clinical outcomes has not yet been comprehensively examined, to our knowledge.
In an attempt to shed light on this complex issue, we have undertaken a systematic review to answer the following 2 key questions: 1) is dairy consumption detrimentally, neutrally, or beneficially associated with cardiovascular-related clinical outcomes, and 2) is the recommendation to consume low-fat, as opposed to regular- or high-fat dairy, evidence-based? This review focuses primarily on existing meta-analyses of prospective epidemiologic studies of dairy intake and cardiovascular-related clinical outcomes, that is, cardiovascular disease (CVD), coronary artery disease (CAD), stroke, hypertension, metabolic syndrome (MetS), and type 2 diabetes (T2D). Prospective epidemiologic studies of dairy intake and clinical outcomes of interest that were not included in published meta-analyses were also further reviewed. The association between dairy consumption and cardiovascular-related outcomes was ascertained while considering total and individual dairy (milk, yogurt, cheese), irrespective of fat content; regular- or high-fat and low-fat dairy as per the definition by investigators in the various studies; and finally, fermented dairy when possible. Butter is generally not considered part of the dairy food category in most dietary guidelines and thus was not included in this analysis. We believe that this extensive review encompasses all available epidemiologic evidence relating dairy product consumption to cardiovascular-related health outcomes. No a priori hypothesis was established.
Methods
Full details of the methods used are presented in the Supplemental Methods. Briefly, this systematic review was conducted according to the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analysis) statement Supplemental Table 1) (3). We first screened PubMed and Embase databases to identify meta-analyses of prospective cohort studies on the association between dairy product consumption (any form) and cardiovascular-related clinical outcomes (e.g., CVD, CAD, stroke, hypertension, MetS, and T2D). Meta-analyses of data from cross-sectional or case-control studies were not included. Individual prospective cohort studies that had not been included in the retrieved meta-analyses were also identified and reviewed. Two authors independently undertook the literature search in May 2015 with the use of keywords provided in Supplemental Table 2. The search was repeated in November 2015 before the original submission of the article and updated in March 2016 during the revision process.
The quality of each meta-analysis was evaluated and scored by 2 authors (J-PD-C and BL) independently by using the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) checklist (4), as detailed in the Supplemental Methods. The interrater reliability in the quality scoring was good (r = 0.79). Disagreement between raters (scores differing by >15%) was resolved by discussion. Meta-analyses with scores >80% were considered to be of good quality. Studies with scores between >60% and ≤80% were considered to be of moderate quality. Finally, studies with scores ≤60% were considered to be of poor quality. The complete list of meta-analyses included in this systematic review and their quality rating is presented in Table 1. The flow of retrieved meta-analyses and prospective cohort studies during the literature search is shown in Supplemental Tables 3 and 4.
TABLE 1.
List of meta-analyses included in this review and their quality score and funding source
| First author, year (reference) | Quality score,1 % | Funding source |
| Elwood et al., 2004 (5) | 53 | University of Wales College of Medicine and Bristol University, Food Standards Agency |
| Elwood et al., 2008 (6) | 54 | No funding |
| Elwood et al., 2010 (7) | 54 | No funding |
| Soedamah-Muthu et al., 2011 (8) | 74 | Dutch Dairy Association (unrestricted) |
| Tong et al., 2011 (9) | 60 | National Natural Science Foundation of China |
| Bendsen et al., 2011 (10) | 80 | Arla Food Amba |
| Ralston et al., 2012 (11) | 69 | National Health and Medical research Council of Australia |
| Soedamah-Muthu et al., 2012 (12) | 71 | Dutch Dairy Association (unrestricted), Global Dairy Platform |
| Aune et al., 2013 (13) | 69 | Liaison Committee between the Central Norway Regional Health Authority and the Norwegian University of Science and Technology |
| Gao et al., 2013 (14) | 80 | National Natural Science Foundation of China |
| O‘Sullivan et al., 2013 (15) | 83 | National Health and Medical research Council of Australia |
| Chen et al., 2014 (16) | 54 | NIH |
| Chowdhury et al., 2014 (17) | 100 | British Heart Foundation, Medical Research Council, Cambridge National Institute for Health Research Biomedical Research Centre, Gates Cambridge |
| Hu et al., 2014 (18) | 71 | Not indicated |
| Qin et al., 2015 (19) | 64 | Nestec Ltd. [Nestlé R&D (China) Ltd.] |
| de Souza et al., 2015 (20) | 77 | WHO |
| Larsson et al., 2015 (21) | 66 | Young Scholars Award Grant from the Strategic Research Area in Epidemiology, Karolinska Institutet |
| Chen et al., 2015 (22) | 67 | Yili Innovation Center, Inner Mongolia Yili Industrial Group Co., Ltd. |
| Kim and Je, 2016 (23) | 67 | Basic Science Research Program of the National Research Foundation of Korea, Ministry of Science, Information and Communication Technology and Future Planning |
| Alexander et al., 2016 (24) | 67 | Dairy Research Institute |
| Gijsbers et al., 2016 (25) | 73 | Wageningen University |
Quality score was calculated according to the MOOSE (Meta-analysis Of Observational Study in Epidemiology) checklist.
The quality of evidence relating dairy intake to cardiovascular-related clinical outcomes was assessed through consensus from 2 authors (J-PD-C and BL) by using an adaptation of the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) scale (26), as detailed in Supplemental Table 5. According to the GRADE scale (27, 28), high-quality evidence defines a situation in which “we are very confident that the true effect lies close to that of the estimate of the effect.” Moderate-quality evidence indicates that “we are moderately confident in the effect estimate. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.” Low-quality evidence indicates that “our confidence in the effect estimate is limited. The true effect may be substantially different from the estimate of the effect.” Very low-quality evidence indicates that “we have very little confidence in the effect estimate. The true effect is likely to be substantially different from the estimate of the effect.” Information pertaining specifically to associations supported by low- or very low-quality evidence has been included in the Supplemental Information in order to shorten the review. Setting this information as online supporting material should not be seen as a biased way to present the evidence, and we emphasize in each section of this review the importance of conducting more research in instances in which we are lacking high-quality evidence.
Dairy and Cardiovascular-Related Clinical Outcomes
CVD
Total dairy and CVD.
In 2013, O’Sullivan et al. (15) evaluated the association between total dairy intake and CVD mortality (Supplemental Table 6). Total dairy intake showed no association with CVD mortality rates (RR: 0.87; 95% CI: 0.62, 1.20). The authors reported no evidence of heterogeneity between studies and no publication bias. In their 2015 meta-analysis, Qin et al. (19) reported an inverse association between total dairy consumption and the risk of nonfatal CVD (RR: 0.88; 95% CI: 0.81, 0.96). There was no evidence of significant heterogeneity between studies or publication bias. Finally, Alexander et al. (24) recently reported no association between total dairy intake and CVD (RR: 0.85; 95% CI: 0.75, 1.04), with significant heterogeneity between studies but no publication bias. Two (15, 19) of the 3 meta-analyses were based on different pools of cohort studies with only 1 study in common. Associations differed slightly according to whether CVD mortality (15) or CVD incidence (19, 24) was considered. The search retrieved 1 additional cohort study (29) that had not been included in these meta-analyses and that reported no significant association between total dairy intake and risk of fatal CVD (Supplemental Table 7).
In summary, risk estimates based on 3 meta-analyses predicted either a favorable or neutral association between total dairy consumption and CVD risk. Thus, there is moderate-quality evidence that total dairy consumption is neutral in terms of CVD risk (Table 2).
TABLE 2.
Summary of the association between dairy product consumption and clinical outcomes, with assessment of quality of evidence1
| CVD | CAD | Stroke | Hypertension | MetS | T2D | |
| Total dairy | Neutral | Neutral | Favorable | Favorable | Favorable | Favorable |
| Moderate | High | Moderate | High | Moderate | Moderate | |
| Regular- or high-fat dairy | Uncertain | Neutral | Neutral | Neutral | Uncertain | Neutral |
| Very low | High | Moderate | Moderate | Very low | Moderate | |
| Low-fat dairy | Uncertain | Neutral | Favorable | Favorable | Uncertain | Favorable |
| Very low | High | Moderate | Moderate | Very low | High | |
| Milk | Uncertain | Neutral | Neutral | Favorable | Favorable | Neutral |
| Very low | Moderate | Moderate | Moderate | Moderate | Moderate | |
| Cheese | Neutral | Neutral | Favorable | Neutral | Uncertain | Favorable |
| High | Moderate | Moderate | High | Very low | Moderate | |
| Yogurt | Neutral | Neutral | Neutral | Neutral | Uncertain | Favorable |
| Moderate | Moderate | Moderate | Moderate | Very low | High | |
| Fermented dairy | Uncertain | Uncertain | Favorable | Neutral | Uncertain | Neutral |
| Very low | Very low | Moderate | Moderate | Very low | Moderate |
Each of these associations is described in detail in the text. The association between dairy intake (any form) and the onset of any clinical outcome is described as “unfavorable” (increased risk with dairy intake), “neutral” (no association between dairy intake and risk), or “favorable” (reduced risk with increased intake of dairy). The quality of evidence (very low, low, moderate, or high) is described by using the GRADE grading system as described in Supplemental Table 5. High-quality evidence defines a situation in which “we are very confident that the true effect lies close to that of the estimate of the effect.” Moderate-quality evidence indicates that “we are moderately confident in the effect estimate. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.” Low-quality evidence indicates that “our confidence in the effect estimate is limited. The true effect may be substantially different from the estimate of the effect.” Very low-quality evidence indicates that “we have very little confidence in the effect estimate. The true effect is likely to be substantially different from the estimate of the effect.” CAD, coronary artery disease; CVD, cardiovascular disease; GRADE, Grading of Recommendations Assessment, Development, and Evaluation; MetS, metabolic syndrome; T2D, type 2 diabetes.
Dairy fat and risk of CVD.
The quality of evidence relating dairy fat intake to CVD risk is judged to be very low (Table 2), when considering the lack of meta-analyses and the limited number of cohort studies on this topic, the diversity of the methods used to assess dairy fat intake, and the inconsistent conclusions among studies (see Supplemental Information for details).
Milk and risk of CVD.
Despite the fact that the association between milk consumption and CVD risk has been evaluated in several meta-analyses of cohort studies (Supplemental Table 6), the direction of this association cannot be established with any confidence at this point because the estimates of effects remain uncertain (very low quality of evidence; Table 2). The Supplemental Information provides detailed information on this assessment. Future meta-analyses will have to include data from all published studies to better reflect these associations, with particular consideration of heterogeneity.
Cheese and risk of CVD.
The search retrieved 2 meta-analyses of the association between cheese consumption and CVD risk (Supplemental Table 6). O’Sullivan et al. (15) (RR: 1.00; 95% CI: 0.81, 1.24; no heterogeneity and no publication bias) and Alexander et al. (24) (RR: 0.89; 95% CI: 0.78, 1.01; no heterogeneity, publication bias not assessed) reported no significant association between cheese intake and CVD. One additional prospective study was retrieved, which also reported no association between CVD risk and the consumption of regular-fat or low-fat cheese (30) (Supplemental Table 7). On the basis of data from 2 meta-analyses that showed consistent results, there is high-quality evidence that cheese intake is not associated with the risk of CVD (Table 2).
Yogurt and risk of CVD.
Alexander et al. (24) in their meta-analysis reported no significant association between yogurt consumption and CVD risk (RR: 0.93; 95% CI: 0.78, 1.12). Heterogeneity and publication bias were not assessed. Of note, the authors did not identify references of individual studies included in this particular analysis and did not provide this information after being contacted. In summary, evidence suggests that the association between yogurt consumption and CVD risk is neutral, and this assessment is based on moderate-quality evidence (Table 2).
Fermented dairy and risk of CVD.
The association between the consumption of fermented dairy and the risk of CVD has not yet been meta-analyzed, to our knowledge. In that context, the assessment of the association between the consumption of fermented dairy and CVD risk is based on very low-quality evidence and thus remains uncertain at this point (Table 2). Additional information is available in the Supplemental Information.
Dairy and risk of CVD—summary.
The association between dairy consumption in various forms and CVD risk has been evaluated in a limited number of meta-analyses (Figure 1). Scientific evidence of moderate-to-high quality indicates that intakes of total dairy, cheese, and yogurt are neutral in terms of CVD risk. The quality of evidence relating high-fat dairy, low-fat dairy, milk, and fermented dairy intake to CVD risk is considered to be very low and hence no conclusion can be drawn with any confidence at this point (Table 2).
FIGURE 1.
Forest plot of RRs from meta-analyses of prospective cohort studies on the association between dairy intake and cardiovascular disease risk, with their 95% CIs. Each symbol represents data from an individual meta-analysis.
CAD
Total dairy and risk of CAD.
Soedamah-Muthu et al. (8) in their meta-analysis reported no significant association between total dairy intake and the risk of CAD (RR: 1.02; 95% CI: 0.93, 1.11; Supplemental Table 8). There was no evidence of heterogeneity between studies and publication bias was not assessed. Qin et al. (19) also reported no significant association between total dairy and CAD risk (RR: 0.94; 95% CI: 0.82, 1.07). There was significant heterogeneity between studies, but sensitivity analysis revealed little influence on the global interpretation of the data. There was no evidence of publication bias in the meta-analysis by Qin et al. (19). Finally, the recent meta-analysis by Alexander et al. (24) reported no significant association between total dairy intake and CAD risk (RR: 0.91; 95% CI: 0.80, 1.04). There was significant heterogeneity between studies but no evidence of publication bias. The search retrieved 1 small additional prospective cohort study (31) in which total dairy intake and CAD were not associated (Supplemental Table 7). In sum, there is high-quality evidence from 3 meta-analyses (8, 19, 24) that total dairy consumption is not associated with CAD risk (Table 2).
Dairy fat and risk of CAD.
In a dose-response meta-analysis of 4 prospective cohort studies, Soedamah-Muthu et al. (8) found no significant association between the intake of high-fat dairy and CAD risk (RR: 1.04; 95% CI: 0.89, 1.21; Supplemental Table 8) and between low-fat dairy intake and total CAD risk (RR: 0.93; 95% CI: 0.74, 1.17). Potential publication bias was not assessed, but there was no evidence of heterogeneity between studies. The meta-analysis by Qin et al. (19) came to the same conclusion for the analysis of both regular- and high-fat dairy and low-fat dairy. The authors did not provide the reference list specific to each of those analyses in the publication or after being contacted. In their meta-analysis, Alexander et al. (24) reported a neutral association between high-fat dairy intake and CAD risk (RR: 1.08; 95% CI: 0.93, 1.19) and an inverse association between low-fat dairy intake and CAD risk (RR: 0.90; 95% CI: 0.82, 0.98). Heterogeneity and publication bias were not assessed.
Dairy fat contains naturally occurring trans fatty acids (TFAs), mostly vaccenic acid (trans-18:1ω-7). In 2011, Bendsen et al. (10) published a meta-analysis of 4 cohort studies that assessed the association between the intake of TFAs from industrial and ruminant origins and CAD risk. Intakes of TFAs from ruminants showed no significant association with CAD risk (RR: 0.92; 95% CI: 0.76, 1.11). There was no evidence of heterogeneity between studies. Results from the more recent meta-analysis by de Souza et al. (20) also indicated that there was no association between ruminant TFA intake and CAD risk (RR: 0.93; 95% CI: 0.73, 1.18). In addition, de Souza et al. reported null associations between intakes of the dairy-specific FAs pentadecanoic acid (15:0; RR: 0.94; 95% CI: 0.44, 2.06) and heptadecanoic acid (17:0; RR: 0.92; 95% CI: 0.82, 1.03) and CAD risk. The authors reported significant heterogeneity between studies in the case of the association between the intake of pentadecanoic acid specifically and CAD risk, although publication bias was not evaluated (20). Finally, Chowdhury et al. (17) in their meta-analysis reported no significant association between plasma concentrations of pentadecanoic acid and CAD (RR: 0.94; 95% CI: 0.67, 1.32), whereas concentrations of heptadecanoic acid were inversely associated with the risk of CAD (RR: 0.77; 95% CI: 0.63, 0.93). Plasma concentrations of palmitoleic acid (cis-16:1ω-7) showed no association with CAD risk (RR: 0.96; 95% CI: 0.86, 1.08). Publication bias was not assessed specifically for these associations, and there was moderate heterogeneity between studies.
In summary, high-quality evidence from several meta-analyses based on either self-reported dairy fat intake (8, 19) or on biomarkers of dairy fat intake (10, 17, 20) suggests that high intakes of dairy fat are not associated with CAD risk (Table 2). There is also high-quality evidence indicating that the consumption of low-fat dairy products is not associated with the risk of CAD.
Milk and risk of CAD.
Elwood et al. (5–7) published 3 meta-analyses to assess the association between milk consumption specifically and CAD risk (Supplemental Table 8). In 2004 (5), the authors reported no significant association risk (RR: 0.84; 95% CI: 0.74, 1.03), whereas in 2008 they showed that high compared with low milk consumption was associated with a reduced risk of CAD (RR: 0.84; 95% CI: 0.76, 0.93) (6). In their 2010 meta-analysis (7), high compared with low consumption of milk was also associated with a significantly lower risk of CAD (RR: 0.92; 95% CI: 0.80, 0.99). There was no evidence of heterogeneity between studies, and publication bias was not assessed in any of the 3 meta-analyses, all of which had a low-quality score on the basis of the MOOSE scale. Soedamah-Muthu et al. (8) examined the dose-response relation between milk intake and total CAD risk. Increased consumption of milk showed no association with CAD risk (RR: 0.92; 95% CI: 0.80, 0.99), without evidence of heterogeneity between studies. Publication bias was not assessed. In their recent meta-analysis, Alexander et al. (24) also reported no significant association between milk consumption and CAD risk (RR: 1.05; 95% CI: 0.95, 1.16). The authors did not provide the list of studies included in this particular analysis and did not provide this information after being contacted.
Overall, considering some degree of inconsistency among available meta-analyses and based on our adapted GRADE criteria (see Supplemental Methods), increased milk intake is suggested to show no association with the risk of CAD, and this is supported by moderate-quality evidence (Table 2). Whether skimmed or low-fat milk is more favorably associated with the risk of CAD than regular-fat milk has yet to be determined.
Cheese and risk of CAD.
In 2010, Elwood et al. (7) reported no significant association between cheese intake and the risk of ischemic heart disease [(IHD); RR: 0.90; 95% CI: 0.79, 1.03; Supplemental Table 8]. However, results are confounded by the fact that stroke was combined with IHD as a study endpoint, which limits their interpretation. Publication bias was not assessed, although there was no evidence of heterogeneity between the 2 studies included in the meta-analysis by Elwood et al. (7). Qin et al. (19) meta-analyzed 7 prospective cohort studies on the association between cheese consumption and CAD risk. The authors did not provide the list of studies included in this particular analysis. Cheese consumption tended to be inversely associated with CAD risk (RR: 0.84; 95% CI: 0.74, 1.00). There was no evidence of significant heterogeneity between studies and no publication bias. Alexander et al. (24), on the basis of 5 prospective cohort studies, concluded that there was a significant inverse association between cheese consumption and CAD risk (RR: 0.82; 95% CI: 0.72, 0.93).
In summary, cheese intake shows no significant association with the risk of CAD (Table 2). The evidence supporting this observation is considered to be of moderate quality because of the inconsistent results among meta-analyses. There is, to date, no evidence that indicates that low-fat cheese may be differentially associated with the risk of CAD compared with regular-fat cheese.
Yogurt and risk of CAD.
In the meta-analyses by Qin et al. (19) and by Alexander et al. (24), yogurt consumption showed no significant association with the risk of CAD (Supplemental Table 8). Our search retrieved 2 additional prospective cohort studies (31, 32), which may have been included in the recent meta-analysis by Alexander et al. (24). This remains unclear, because the authors did not provide the list of studies included in their meta-analysis. In these individual prospective cohort studies, high compared with low intakes of yogurt were also not associated with fatal or incident CAD risk (Supplemental Table 7).
The evidence that suggests a neutral association between yogurt consumption and CAD risk appears to be consistent, although existing meta-analyses lack important information. For this reason, we suggest that this neutral association between yogurt consumption and CAD risk is supported by moderate-quality evidence (Table 2). The difference between regular-fat and low-fat yogurt in terms of CAD risk cannot be determined at this point.
Fermented dairy and risk of CAD.
The association between the consumption of fermented dairy and the risk of CAD remains uncertain (Table 2), because only evidence of insufficient quality is available (Supplemental Table 7). Additional information is available in the Supplemental Information.
Dairy products and CAD—summary.
On the basis of available meta-analyses and prospective cohort studies, there is high-quality evidence that total dairy, high-fat dairy, and low-fat dairy consumption shows no association with the risk of CAD (Figure 2). The neutral association between intakes of milk, cheese, and yogurt and CAD risk is supported by evidence judged to be of moderate quality, and the association between fermented dairy consumption and CAD risk remains uncertain because of limited evidence (Table 2).
FIGURE 2.
Forest plot of RRs from meta-analyses of prospective cohort studies on the association between dairy intake and coronary artery disease risk, with their 95% CIs. Each symbol represents data from an individual meta-analysis. Arrows indicate that the 95% CIs exceed the figure scale. R-TFA, ruminant trans fatty acids.
Stroke
Total dairy and risk of stroke.
Hu et al. (18) assessed the relation between total dairy intake and the risk of stroke on the basis of data from 18 cohort studies (Supplemental Table 9). Total dairy intake was inversely associated with the risk of stroke (RR: 0.88; 95% CI: 0.82, 0.94). There was no evidence of publication bias, but there was significant heterogeneity between studies. However, the inverse association between total dairy intake and the risk of stroke remained significant when the 3 studies responsible for heterogeneity were excluded in sensitivity analyses. Qin et al. (19) in their meta-analysis of 12 cohort studies also showed that total dairy consumption was associated with a significant reduction in stroke risk (RR: 0.87; 95% CI: 0.77, 0.99). The authors reported significant heterogeneity between studies as well as significant publication bias. Alexander et al. (24) also recently reported an inverse association between total dairy intake and stroke risk (RR: 0.91; 95% CI: 0.83, 0.99), with again, significant heterogeneity between individual studies. Of note, all prospective studies included in the meta-analysis by Qin et al. (19) and Alexander et al. (24) were also included in the meta-analysis by Hu et al. (18). One additional cohort study (31) reported no association between total dairy intake and stroke risk (Supplemental Table 7). This study was very small compared with existing data from previous meta-analyses and therefore unlikely to have an impact on the reported pooled risk estimates from existing meta-analyses.
In summary, the inverse association between total dairy intake and the risk of stroke appears to be robust. However, because results from the 3 meta-analyses are based on a relatively homogeneous pool of cohort studies, we suggest that this favorable association between intake of total dairy and risk of stroke is based on moderate-quality evidence.
Dairy fat and risk of stroke.
In the meta-analysis by Hu et al. (18), no association was found between the intake of high-fat dairy (as per the definition by the authors) and the risk of stroke (RR: 0.96; 95% CI: 0.92, 1.01), whereas the intake of low-fat dairy products was associated with a 9% lower risk of stroke (RR: 0.91; 95% CI: 0.85, 0.97; Supplemental Table 9). There was no evidence of heterogeneity between studies or of publication bias. Qin et al. (19) reached similar conclusions for high-fat (RR: 0.95; 95% CI: 0.83, 1.08) and low-fat (RR: 0.93; 95% CI: 0.88, 0.99) dairy. The authors did not identify the individual cohort studies used in these specific analyses (19). However, we suspect that most of the studies used by Qin et al. were included in the meta-analysis by Hu et al., because this was the case when both groups assessed total dairy. Alexander et al. (24) in their recent meta-analysis reported inverse associations between both high-fat dairy intake (RR: 0.91; 95% CI: 0.84, 0.99) and low-fat dairy intake (RR: 0.90; 95% CI: 0.83, 0.96) and the risk of stroke. In additional prospective cohort studies (31, 33), high intakes of dairy fat or low-fat dairy were not associated with stroke risk (Supplemental Table 7).
In summary, because data from published meta-analyses may be derived mostly from the same pool of cohort studies, we conclude that there is moderate-quality evidence that the intake of regular- and high-fat dairy is not associated with the risk of stroke. On the other hand, the consumption of low-fat dairy is favorably associated with stroke risk on the basis of moderate-quality evidence (Table 2).
Milk and risk of stroke.
Elwood et al. (5–7) published 3 meta-analyses relating milk consumption to stroke risk. Articles published in 2004 (5), 2008 (6), and 2010 (7) all reported a reduced risk of stroke associated with high compared with low milk consumption (Supplemental Table 9). Heterogeneity between studies was observed in the 2010 meta-analysis (7), and publication bias was not assessed in any of the 3 meta-analyses. On the other hand, the dose-response meta-analysis of Soedamah-Muthu et al. (8) showed no association between milk consumption and the risk of stroke (RR: 0.87; 95% CI: 0.72, 1.07). There was no evidence of publication bias but significant heterogeneity between studies was observed, with milk intake being associated with a reduced risk of stroke among women but not among men. The degree of adjustment for confounding factors also appeared to attenuate the association between milk intake and risk of stroke. Hu et al. (18) reported no significant association between milk intake and the risk of stroke in their meta-analysis (RR: 0.91; 95% CI: 0.82, 1.01). There was also significant heterogeneity between studies, but further analysis that excluded the 3 studies responsible for this heterogeneity had no impact on the results. There was no evidence of publication bias. Finally, Alexander et al. (24) recently reported no significant association between milk consumption and stroke risk (RR: 0.90; 95% CI: 0.79, 1.02), with significant heterogeneity between studies. The authors did not provide the list of references for this specific analysis.
In summary, 3 meta-analyses by the same group of authors reported a favorable association between milk intake and the risk of stroke, whereas meta-analyses conducted by other groups, including 1 dose-response analysis, reported null associations between milk intake and stroke risk. Thus, milk consumption is not associated with the risk of stroke, which is supported by moderate-quality evidence. There is no evidence to date that skimmed or low-fat milk may be more favorably associated with the risk of stroke than regular-fat milk.
Cheese and risk of stroke.
Elwood et al. (7) reported in their meta-analysis no significant association between cheese intake and the risk of IHD and stroke combined (RR: 0.90; 95% CI: 0.79, 1.03). There was significant heterogeneity between studies, and publication bias was not assessed. However, the combined assessment of IHD and stroke and the limited number of cohort studies included (n = 2) limit the generalizability of the results. Hu et al. (18) reported a small but significantly lower risk of stroke with cheese consumption (RR: 0.94; 95% CI: 0.89, 0.995). No evidence of publication bias or heterogeneity between studies was found. Qin et al. (19) also reported an inverse association between cheese consumption and stroke risk (RR: 0.91, 95% CI: 0.84, 0.98). Their meta-analysis revealed no significant heterogeneity between studies and no publication bias. Alexander et al. (24), on the basis of data from 4 prospective cohort studies, reported an inverse association between cheese consumption and stroke risk (RR: 0.87; 95% CI: 0.77, 0.99). It is unclear how many cohort studies are common to these meta-analyses because Qin et al. (19) did not provide references for their analysis.
In summary, 3 meta-analyses with relatively large numbers of subjects concluded that cheese consumption is associated with a reduced risk of stroke, whereas a meta-analysis based on only 2 cohort studies with a low-quality score reported a null association. As per our a priori–defined criteria, we suggest that cheese intake is favorably associated with the risk of stroke, and that this is supported by moderate-quality evidence. More studies characterizing the association between regular-fat and low-fat cheese and the risk of stroke are needed.
Yogurt and risk of stroke.
Qin et al. (19) meta-analyzed data from prospective cohort studies and reported a null association between yogurt consumption and the risk of stroke (RR: 0.98, 95% CI: 0.92, 1.06). Two additional cohort studies (31, 32) also reported no significant association between yogurt consumption and the risk of stroke (Supplemental Table 7). The available meta-analysis has a relatively good quality score and suggests that yogurt consumption is not associated with the risk of stroke, and this is based on moderate-quality evidence (Table 2).
Fermented dairy and risk of stroke.
One meta-analysis (18) showed that intake of fermented dairy was associated with a reduced risk of stroke (RR: 0.80; 95% CI: 0.71, 0.89), without evidence of publication bias or heterogeneity between studies (Supplemental Table 9). It must be stressed that there were only 2 prospective cohort studies included in this meta-analysis and its quality was rated as moderate (Table 1). However, 2 recent prospective cohort studies reported no association between fermented dairy and the risk of stroke (31, 32) (Supplemental Table 7). The large number of individuals in these studies may change the risk estimates when included in an updated meta-analysis.
On the basis of this finding, we suggest that there is moderate-quality evidence that the consumption of fermented dairy is associated with a reduced risk of stroke (Table 2). Indeed, the meta-analysis available is based on only 3 prospective cohort studies and thus risk estimates may change with future studies on this topic. The difference between regular-fat and low- or no-fat yogurt intake in terms of stroke risk is unknown.
Dairy and risk of stroke—summary.
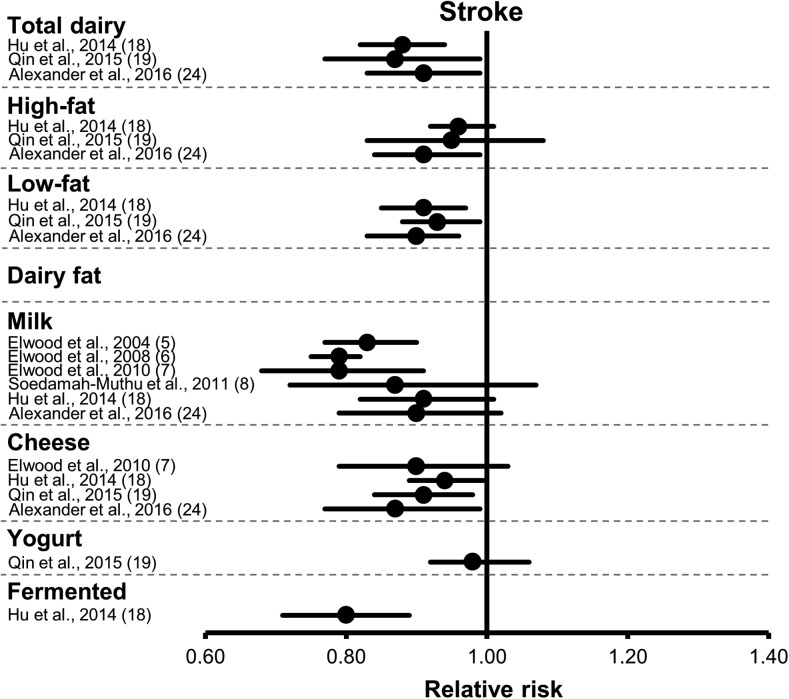
Although the consumption of total dairy, low-fat dairy, cheese, and fermented dairy may be associated with a reduced risk of stroke, intakes of regular- and high-fat dairy, yogurt, and milk specifically show no association with stroke risk (Table 2, Figure 3). More research is warranted to further examine if the reduced-fat version of a specific dairy product is more favorably associated with the risk of stroke than its regular-fat version.
FIGURE 3.
Forest plot of RRs from meta-analyses of prospective cohort studies on the association between dairy intake and the risk of stroke, with their 95% CIs. Each symbol represents data from an individual meta-analysis.
Hypertension
Total dairy and risk of hypertension.
In the meta-analysis by Soedamah-Muthu et al. (12), for every 200-g/d increase in total dairy intake, there was a significant 3% reduction in the risk of hypertension (RR: 0.97; 95% CI: 0.95, 0.99; Supplemental Table 10). There was no heterogeneity between studies, and no evidence of publication bias. In the meta-analysis by Ralston et al. (11), total dairy intake was inversely associated with the risk of hypertension (RR: 0.87; 95% CI: 0.81, 0.94). There was no evidence of heterogeneity between studies. Publication bias was not assessed. Four prospective cohort studies were common to both meta-analyses. Six prospective cohort studies were not included in these meta-analyses (Supplemental Table 11). Four of these studies (34–37) reported a significant inverse association between total dairy intake and the risk of hypertension, whereas the other 2 reported no significant association (38, 39). Although not all significant, the direction and magnitude of the hypertension risk estimates with total dairy intake in these small prospective cohort studies are comparable to numbers reported in the meta-analyses by Soedamah-Muthu et al. (12) and Ralston et al. (11). Data from these individual cohort studies are therefore unlikely to materially modify risk estimates from available meta-analyses, which are based on combined sample sizes of >40,000 individuals.
Thus, data from available meta-analyses and prospective cohort studies are fairly consistent in suggesting that total dairy consumption is associated with a reduced risk of hypertension (Table 2). This assessment is based on high-quality evidence according to the GRADE system.
Dairy fat and risk of hypertension.
Soedamah-Muthu et al. (12) in their meta-analysis (Supplemental Table 10) reported no association between the consumption of high-fat dairy and the risk of hypertension (RR: 0.99; 95% CI: 0.95, 1.03), whereas low-fat dairy intake was associated with a significant reduction in the risk of hypertension (RR: 0.96; 95% CI: 0.93, 0.99). Publication bias was not assessed, and results were not found to be heterogeneous between studies for either the low-fat or the high-fat dairy analysis. Similarly, the consumption of high-fat dairy in the meta-analysis by Ralston et al. (11) showed no association with the risk of hypertension (RR: 1.00; 95% CI: 0.89, 1.11), whereas low-fat dairy consumption was associated with a significant reduction in the risk of hypertension (RR: 0.84; 95% CI: 0.74, 0.95). There was significant heterogeneity between studies but no mention of potential publication bias. All of the studies included in the meta-analysis by Ralston et al. (11) were included in the meta-analysis by Soedamah-Muthu et al. (12). The consumption of high-fat as well as low-fat dairy foods has been associated with a reduced risk of elevated blood pressure or hypertension in some (34, 37), but not all (37, 40), additional prospective cohort studies, depending on how dairy products were categorized (Supplemental Table 11).
Data from meta-analyses and additional prospective cohort studies suggest that the consumption of high-fat dairy is not associated with the risk of hypertension or high blood pressure, whereas low-fat dairy consumption may be associated with a reduced risk of hypertension (Table 2). Evidence supporting this assessment is of moderate quality because the 2 independent meta-analyses are based on essentially the same pool of cohort studies.
Milk and risk of hypertension.
In the only meta-analysis available on this topic so far, Soedamah-Muthu et al. (12) showed an inverse association between milk intake and the risk of hypertension (RR: 0.96; 95% CI: 0.94, 0.98; Supplemental Table 10). Potential publication bias was not assessed, but there was no apparent heterogeneity between studies. Additional prospective cohort studies reported either significant inverse associations (34, 39) or null associations (37, 38) between milk consumption and the risk of hypertension (Supplemental Table 11).
On the basis of results from 1 meta-analysis and from additional prospective cohort studies, milk consumption may be associated with a reduced risk of hypertension. The evidence supporting this association is of moderate quality (Table 2). The extent to which reduced-fat milk may be more favorably associated with a reduced risk of hypertension than regular-fat milk is uncertain and needs further consideration in future studies on this topic.
Cheese and risk of hypertension.
In the meta-analysis by Soedamah-Muthu et al. (12), cheese consumption showed no significant association with the risk of hypertension (RR: 1.00; 95% CI: 0.98, 1.03; Supplemental Table 10). No evidence of heterogeneity was noted between studies, and publication bias was not assessed. The meta-analysis by Ralston et al. (11) came to similar conclusions (RR: 1.00; 95% CI: 0.89, 1.12). The two meta-analyses had 4 cohort studies in common. Other retrieved prospective cohort studies (34–37, 39) reported no significant association between cheese consumption and hypertension risk (Supplemental Table 11).
In sum, the 2 available meta-analyses and additional cohort studies were consistent in showing no significant association between cheese intake and the risk of hypertension. Thus, there is high-quality evidence that cheese consumption per se is not associated with the risk of hypertension (Table 2). Whether the consumption of low-fat cheese is associated with more favorable blood pressure outcomes than regular-fat cheese is uncertain.
Yogurt and risk of hypertension.
Soedamah-Muthu et al. (12) reported no significant association between yogurt consumption (per 50 g/d) and the risk of hypertension (RR: 0.99; 95% CI: 0.96, 1.01; Supplemental Table 10) in their meta-analysis of 5 prospective cohort studies. Results appeared to be consistent between the different studies, and publication bias was not assessed. Data from the prospective CARDIA (Coronary Artery Risk Development in Young Adults) (34) and SUN (Seguimiento University of Navarra) (40) cohorts are consistent with these findings in showing no significant association between yogurt consumption and hypertension risk (Supplemental Table 11). On the other hand, an inverse association between yogurt consumption and hypertension risk was reported in the Framingham Heart Study (37) (RR: 0.95; 95% CI: 0.90, 0.99). In summary, moderate-quality evidence suggests that yogurt consumption is not associated with the risk of hypertension (Table 2).
Fermented dairy and risk of HTN.
Soedamah-Muthu et al. (12) pooled results from 4 prospective cohort studies (Supplemental Table 10) and showed no significant association between the consumption of fermented dairy and the risk of hypertension (RR: 0.99; 95% CI: 0.94, 1.04). The only additional published study on this topic was conducted by Wang et al. (37), who reported an inverse association between the consumption of fermented dairy and the risk of hypertension (Supplemental Table 11). This study has an important weight (n = 2340) relative to data from the meta-analysis by Soedamah-Muthu et al. (12) (n = 7641) and is likely to modify pooled risk estimates. In this context, we suggest that moderate-quality evidence supports a neutral association between the consumption of fermented dairy and the risk of hypertension, with the need for further studies on the topic to yield better quality evidence.
Dairy and risk of hypertension—summary.
There is moderate- to high-quality evidence that the consumption of total dairy, low-fat dairy, and milk is associated with a lower risk of hypertension (Figure 4, Table 2). There is also moderate- to high-quality evidence that the consumption of high-fat dairy (as per the authors’ definition), cheese, yogurt, and fermented dairy is not associated with the risk of hypertension. Although the recommendation to consume low-fat dairy foods in place of regular-fat products is partly consistent with data from blood pressure studies, further investigation is warranted in this area to assess whether the low-fat version of a dairy product (e.g., skimmed milk) is indeed more favorable than its regular-fat version (whole milk) in terms of influencing blood pressure.
FIGURE 4.
Forest plot of RRs from meta-analyses of prospective cohort studies on the association between dairy intake and the risk of hypertension, with their 95% CIs. Each symbol represents data from an individual meta-analysis.
MetS
Two meta-analyses (22, 23) recently examined the association between dairy consumption and the risk of MetS. Analyses were based on data from a total of 9 individual prospective cohort studies, of which 3 used National Cholesterol Education Program–Adult Treatment Panel III MetS criteria (35, 41, 42), 1 study used National Cholesterol Education Program–Adult Treatment Panel III criteria with modified waist circumference thresholds (38), 1 study used the insulin-resistance syndrome criteria (34), 1 study used the American Heart Association criteria (43), 2 studies used the International Diabetes Federation criteria (44, 45), and 1 study used both American Heart Association and International Diabetes Federation criteria (40).
Total dairy and risk of MetS.
Chen et al. (22) reported an inverse association between total dairy consumption and the risk of MetS (RR: 0.86; 95% CI: 0.79, 0.92; Supplemental Table 12). There was no heterogeneity between studies, and no evidence of publication bias. A dose-response analysis revealed that each daily serving of dairy was associated with a 6% reduction in the risk of MetS (RR: 0.94; 95% CI: 0.90, 0.98). The meta-analysis by Kim and Je (23) also revealed an inverse association between total dairy consumption and the risk of MetS (RR: 0.85; 95% CI: 0.73, 0.98), with no evidence of heterogeneity between studies or publication bias. Similar results were obtained in their dose-response meta-analysis, in which the risk of MetS was reduced by 12%/daily serving of total dairy (RR: 88; 95% CI: 0.82, 0.95). The inclusion of the cohort study by Sayón-Orea et al. (40), which was based on yogurt intake only, appeared to have no impact on the overall results reported by Kim and Je. The meta-analyses by Chen et al. and Kim and Je both received moderate-quality scores. One additional prospective cohort study suggested no significant association between total dairy consumption and the risk of MetS (46), although the risk estimate was similar to the one reported in the meta-analyses (Supplemental Table 13).
In summary, data from 2 recent meta-analyses, which were based on almost identical pools of prospective cohort studies, suggest that total dairy consumption is inversely associated with the risk of MetS. Data from 1 additional small prospective cohort study reported a similar association, although it did not reach significance. According to the adapted GRADE criteria, this indicates that the favorable association between total dairy consumption and the risk of MetS is supported by moderate-quality evidence (Table 2).
Dairy fat and risk of MetS.
To the best of our knowledge, no meta-analysis has yet evaluated the association between dairy fat and the risk of MetS, and data from available prospective cohort have been inconsistent. Thus, in light of very low-quality evidence, the association between dairy fat and the risk of MetS remains uncertain. A more detailed discussion on this topic is available in the Supplemental Information.
Milk and risk of MetS.
On the basis of pooled data from 3 prospective cohort studies, Chen et al. (22) reported an inverse association between milk consumption and the risk of MetS (RR: 0.75; 95% CI: 0.63, 0.89; Supplemental Table 12). There was no heterogeneity between studies, and publication bias was not evaluated specifically in this meta-analysis. Additionally retrieved data from prospective cohort studies showed either an inverse association (46) or no association (46, 47) between milk consumption with various fat contents and MetS risk (Supplemental Table 13).
The assessment of the association between milk consumption and MetS risk is based on data from 1 meta-analysis of only 4 prospective cohort studies (22), whereas data from additionally retrieved prospective cohort studies are mixed. In that context, we suggest that moderate-quality evidence supports a favorable association between milk consumption and the risk of MetS (Table 2). The extent to which skimmed or low-fat milk compared with regular-fat milk shows different associations with the risk of MetS remains unclear and warrants further research.
Cheese and risk of MetS.
To our knowledge, the association between cheese consumption and the risk of MetS has not been examined in a meta-analysis, and the limited number of prospective cohort studies on this topic have yielded inconclusive evidence. The quality of evidence relating cheese intake to MetS risk is considered to be very low and thus the association remains uncertain (Table 2). Additional information is provided in the Supplemental Information.
Yogurt and risk of MetS.
There is a limited number of prospective cohort studies and no meta-analysis on the association between yogurt consumption and MetS risk. We judge the quality of the evidence relating yogurt intake to the incidence of MetS to be very low, and thus the association remains uncertain. Additional information is available in the Supplemental Information.
Fermented dairy and risk of MetS.
To our knowledge, there are currently no available studies on this topic.
Dairy and risk of MetS—summary.
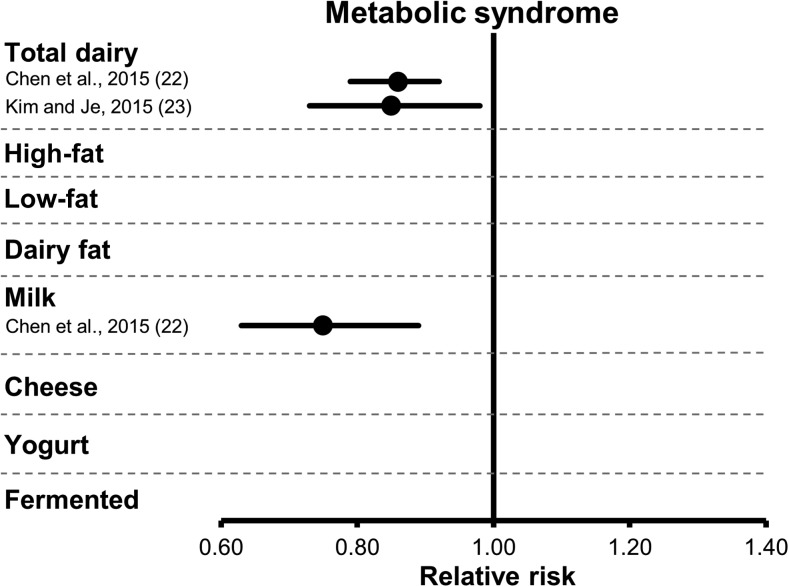
Overall, data on the association between dairy intake and risk of MetS are limited (Figure 5). Because total dairy and milk intake may be inversely associated with the risk of MetS (moderate-quality evidence), evidence for other dairy foods are much limited and of very low quality (Table 2). Additional prospective cohort studies and meta-analyses are required to shed new light on this topic.
FIGURE 5.
Forest plot of RRs from meta-analyses of prospective cohort studies on the association between dairy intake and the risk of metabolic syndrome, with their 95% CIs. Each symbol represents data from an individual meta-analysis.
T2D
Total dairy and risk of T2D.
In the meta-analysis by Elwood et al. (7), total dairy intake was associated with a significantly reduced risk of T2D (RR: 0.85; 95% CI: 0.75, 0.96; Supplemental Table 14). Results from the individual cohort studies were relatively homogeneous, and there was no analysis of potential publication bias. Tong et al. (9) in their meta-analysis also showed that the intake of dairy products was inversely associated with the risk of T2D (RR: 0.86; 95% CI: 0.79, 0.92). There was no heterogeneity between studies, and no evidence of publication bias. Gao et al. (14) reported an inverse association between total dairy intake and the risk of T2D (RR: 0.89; 95% CI: 0.81, 0.98); and in a dose-response analysis, the risk of T2D was reduced by 5% for each 200-g/d increase in total dairy intake (RR: 0.95; 95% CI: 0.92, 0.98). The authors indicated that there was significant heterogeneity between studies in both analyses but no evidence of publication bias. Aune et al. (13) meta-analyzed results from essentially the same pool of prospective cohort studies, with a few exceptions, and reproduced the inverse association between total intake of dairy products and the risk of T2D (RR: 0.89; 95% CI: 0.82, 0.96; RR: 0.93 · 400 g−1 · d−1; 95% CI: 0.87, 0.99). The authors reported moderate heterogeneity in results from the various cohort studies. Interestingly, the meta-analysis conducted by Chen et al. (16), which was based on the largest sample size (n = 459,770), showed no significant association between the total consumption of dairy products and the risk of T2D (RR: 0.98; 95% CI: 0.96, 1.01). There was significant heterogeneity between studies, but no evidence of publication bias. Finally, the most recent meta-analysis conducted by Gijsbers et al. (25) also reported no association between total dairy consumption and T2D risk (RR: 0.97; 95% CI: 0.95, 1.00). Only 1 additional prospective cohort study was retrieved, and no significant association was reported between total dairy intake and T2D risk (48) (Supplemental Table 15).
In sum, results from available meta-analyses are not entirely consistent, showing either favorable (4 meta-analyses) or neutral (2 meta-analyses) associations between dairy intake and the risk of T2D, despite the fact that all were based largely on the same pool of prospective cohort studies. Considering the weight of favorable meta-analyses compared with neutral analyses, we suggest that there is moderate-quality evidence supporting a favorable relation between total dairy intake and incident T2D (Table 2). As emphasized throughout this review, dairy products are heterogeneous, and pooling them into a single analysis may lead to significant heterogeneity, thus providing only partial perspectives on their association with clinical outcomes. This appears to be particularly the case for T2D.
Dairy fat and risk of T2D.
Tong et al. (9) showed that the consumption of high-fat dairy foods (as per the authors’ definition) was not associated with incident T2D (RR: 1.00; 95% CI: 0.89, 1.10), whereas the consumption of low-fat dairy was associated with a significantly reduced risk of T2D (RR: 0.82; 95% CI: 0.74, 0.90). Data from the Gao et al. (14) meta-analysis are consistent with these findings. Indeed, a reduced risk of T2D was associated with the intake of low-fat dairy (RR: 0.81; 95% CI: 0.74, 0.89) but not with the intake of high-fat dairy (RR: 0.95; 95% CI: 0.85, 1.07). There was no evidence of heterogeneity between studies. Dose-response analysis of these cohort studies led to similar observations. Aune et al. (13) reported no association between the intake of high-fat dairy and incident T2D (RR: 0.96; 95% CI: 0.87, 1.06) in their meta-analysis, without heterogeneity between studies. On the other hand, a significant inverse association was reported for low-fat dairy intake and the risk of T2D (RR: 0.83; 95% CI: 0.76, 0.90). Again, the dose-response analysis confirmed these results. Recently, Gijsbers et al. (25) reported no association between T2D risk and the consumption of high-fat (RR: 0.97; 95% CI: 0.95, 1.00) or low-fat (RR: 0.98; 95% CI: 0.93, 1.04) dairy. There was significant heterogeneity between individual studies, but no evidence of publication bias. The association between biomarkers of dairy fat and T2D incidence was assessed in the meta-analysis by de Souza et al. (20). In this particular analysis, inverse associations were reported between T2D risk and circulating concentrations of total ruminant TFAs (RR: 0.58; 95% CI: 0.46, 0.74), pentadecanoic acid (RR: 0.64; 95% CI: 0.46, 0.87) and heptadecanoic acid (RR: 0.67; 95% CI: 0.63, 0.71). Of note, these analyses were based on a limited number of prospective cohort studies (from 2 to 5).
In summary, studies that ascertained the association between low-fat dairy consumption and the risk of T2D appear to be relatively consistent, hence providing high-quality evidence to support a favorable association. On the other hand, data from cohort studies of self-reported high-fat dairy intake and from analysis of biomarkers of dairy fat intake are somehow at odds. Thus, we suggest there is moderate-quality data to support the thesis that the consumption of high-fat dairy has neutral effects on the risk of T2D (Table 2). The extent to which further analyses of dairy fat intake with the use of biomarkers, as in the meta-analysis by de Souza et al. (20), will modify this perspective by confirming a favorable association between dairy fat intake and the risk of T2D is of interest in the future.
Milk and risk of T2D.
Elwood et al. (6) in their meta-analysis reported an inverse association between milk intake and the risk of T2D (RR: 0.92; 95% CI: 0.86, 0.97; Supplemental Table 14). The intake of whole milk showed no association with the risk of T2D (RR: 0.95; 95% CI: 0.86, 1.05) in the meta-analysis by Tong et al. (9). In the Gao et al. (14) meta-analysis, high compared with low intakes of milk were not significantly associated with a lower risk of T2D (RR: 0.89; 95% CI: 0.78, 1.01). Analyses revealed moderate heterogeneity between studies. A specific analysis based on milk-fat content indicated that the intake of low-fat milk was associated with a significant reduction in the risk of T2D (RR: 0.82; 95% CI: 0.69, 0.97), whereas the intake of whole-fat milk was not (RR: 1.12; 95% CI: 0.99, 1.27) (14). Aune et al. (13) reported no significant association between milk intake and T2D risk (RR: 0.87; 95% CI: 0.70, 1.07) on the basis of data from 7 prospective cohort studies. In the most recent meta-analysis, Gijsbers et al. (25) reported no significant association between total milk intake and T2D risk (RR: 0.97; 95% CI: 0.93, 1.02). Significant heterogeneity was observed, with no evidence of publication bias. The authors reported similar associations with T2D risk for high-fat (whole) milk (RR: 0.99; 95% CI: 0.88, 1.11) and low-fat milk (RR: 1.01; 95% CI: 0.97, 1.05). In 2 additional prospective cohort studies (48, 49), milk consumption was not associated with the risk of T2D (Supplemental Table 15).
In summary, 3 of the 4 available meta-analyses showed that the intake of milk is not associated with a reduced risk of T2D, whereas data from 1 meta-analysis suggested a favorable inverse association between milk intake and T2D risk. The meta-analyses by Gao et al. (14) and Aune et al. (13) are based on very similar pools of studies. Conversely, the meta-analyses by Elwood et al. (6) and by Tong et al. (9), both published before 2013, are based on smaller pools of cohort studies. Considering the quality of the meta-analyses available, their findings, and their similarities, we suggest that there is moderate-quality evidence that indicates that milk intake is not associated with the risk of T2D, because it remains possible that risk estimates will be modified once all prospective cohort studies are combined (Table 2). Further studies differentiating low-fat and regular-fat milk with regard to the risk of T2D are also needed.
Cheese and T2D.
According to the meta-analysis by Gao et al. (14), cheese consumption is associated with a reduced risk of T2D (RR: 0.82; 95% CI: 0.77, 0.87; Supplemental Table 14). Their dose-response analysis also revealed a significant inverse association between cheese intake (30 g/d) and incident T2D (RR: 0.80; 95% CI: 0.69, 0.93). There was, however, significant heterogeneity between studies. In the meta-analysis by Aune et al. (13), cheese consumption, when analyzed on a high- compared with low-intake basis (RR: 0.91; 95% CI: 0.84, 0.98) or by using a dose-response approach (RR: 0.92 per increment of 50 g/d; 95% CI: 0.86, 0.99), was also associated with a lower risk of T2D. In their 2016 meta-analysis, Gijsbers et al. (25) did not confirm the inverse association between cheese consumption and T2D risk (RR: 1.00 · 10 g−1 · d −1; 95% CI: 0.99, 1.02). Significant heterogeneity was present with an increased risk of T2D in men with higher cheese consumption (RR: 1.05 · 10 g−1 · d −1; 95% CI: 1.02, 1.09).
Because the available meta-analyses are based on the same pool of prospective cohort studies, because of inconsistencies among meta-analyses, and because of significant heterogeneity between the various individual cohort studies, we suggest that the reduced risk of T2D associated with cheese consumption is supported by moderate-quality evidence (Table 2). More studies are needed to substantiate if low-fat cheese is more favorably associated with T2D risk than regular-fat cheese.
Yogurt and risk of T2D.
Tong et al. (9) showed that high compared with low yogurt consumption was associated with a significantly lower risk of T2D (RR: 0.83; 95% CI: 0.74, 0.93). Heterogeneity between studies was not assessed, but there was no evidence of publication bias. In their meta-analysis, Gao et al. (14) also reported that high compared with low intake of yogurt was inversely associated with incident T2D (RR: 0.85; 95% CI: 0.75, 0.97). Analysis of the dose-response association did not quite reach significance (RR: 0.91 · 50 g−1 · d −1; 95% CI: 0.82, 1.00). The authors reported significant heterogeneity between studies. Finally, Aune et al. (13) indicated that the intake of yogurt was associated with a significantly reduced risk of T2D (RR: 0.86; 95% CI: 0.75, 0.98), which was not the case in the dose-response analysis (RR: 0.78 · 200 g−1 · d −1; 95% CI: 0.60, 1.02). On the basis of an updated meta-analysis of 14 studies, Chen et al. (16) reported a favorable association between yogurt consumption and the risk of T2D (RR: 0.82; 95% CI: 0.70, 0.96). There was significant heterogeneity between studies, but no publication bias. Finally, Gijsbers et al. (25) pooled data from 12 studies and reported an inverse, nonlinear dose-response association between yogurt consumption and T2D risk (RR: 0.94; 95% CI: 0.90, 0.97). In 2 additional prospective cohort studies not included in these meta-analyses, yogurt consumption was also inversely associated with T2D risk (48, 50).
The 5 meta-analyses on the association between yogurt intake and the risk of T2D reported consistent results. Hence, we suggest that there is high-quality evidence that supports an inverse association between the intake of yogurt and the risk of T2D (Table 2). The extent to which low-fat yogurt is more favorable that regular-fat yogurt in influencing the risk of T2D is unknown.
Fermented dairy and risk of T2D.
In the meta-analysis by Gao et al. (14), there was no significant association between intakes of fermented dairy products and the risk of T2D (RR: 0.94; 95% CI: 0.75, 1.18). On the other hand, the intake of fermented dairy was associated with a significant reduction in the risk of T2D (RR: 0.88; 95% CI: 0.79, 0.98) in the meta-analysis by Aune et al. (13). Gijsbers et al. (25) reported no association between fermented dairy product consumption and the risk of T2D (RR for low-fat fermented dairy: 0.98; 95% CI: 0.90, 1.06; RR for high-fat fermented dairy: 0.92; 95% CI: 0.83, 1.03). No heterogeneity and no publication were reported. In one additional prospective cohort study (56), total fermented and regular- and high-fat fermented dairy intakes were not associated with the risk of T2D [RR (95% CI): 0.85 (0.68, 1.08) and 1.16 (0.91,1.49), respectively], whereas the consumption of low-fat fermented dairy was associated with a reduced risk of T2D (RR: 0.76; 95% CI: 0.60, 0.99; Supplemental Table 15).
In sum, the consumption of fermented dairy does not appear to be associated with the risk of T2D. This is based on moderate-quality evidence, because the 3 meta-analyses available relied on almost the same pools of prospective cohort studies (Table 2).
Dairy and T2D—summary.
There is high-quality evidence that intakes of low-fat dairy and yogurt are associated with a reduced risk of T2D (Table 2, Figure 6). There is moderate-quality evidence that suggests that intakes of total dairy and cheese are also associated with a reduced risk of T2D. Finally, the neutral association between intakes of high-fat dairy, milk, and fermented dairy and T2D is supported by evidence of high to moderate quality.
FIGURE 6.
Forest plot of RRs from meta-analyses of prospective cohort studies on the association between dairy intake and the risk of type 2 diabetes, with their 95% CIs. Each symbol represents data from an individual meta-analysis. HF, high-fat; LF, low-fat; R-TFA, ruminant trans fatty acids.
Interpretation and Conclusions
Investigating the impact of food products such as dairy on health is highly challenging. There are obviously no randomized controlled trials with hard endpoints available on this topic, and such a trial is highly unlikely in the future. Thus, the assessment of the association between dairy consumption and clinical outcomes needs to rely primarily on data from observational studies. This review used data from meta-analyses in an attempt to draw the most reliable, evidence-based conclusions relating dairy intake to cardiovascular-related clinical outcomes. Table 2 summarizes the quality of evidence from the adapted GRADE scale as well as the direction of associations between dairy intake in various forms and clinical outcomes, thereby answering the following key nutrition- and health-related questions.
Is dairy consumption detrimentally, neutrally, or beneficially associated with the risk of cardiovascular-related clinical outcomes, including MetS and T2D?
First, there is no evidence that the consumption of any form of dairy product is detrimentally associated with the risk of any cardiovascular-related clinical outcome. In fact, high-quality evidence supports favorable associations (i.e., decreased risk) between:
total dairy intake and the risk of hypertension, and
low-fat dairy and yogurt intake and the risk of T2D.
On the basis of the adapted GRADE criteria, we are confident that these associations are robust and hence unlikely to be modified by further research.
Moreover, moderate-quality evidence suggests favorable associations between:
intakes of total dairy, low-fat dairy, cheese, and fermented dairy products and the risk of stroke;
intakes of low-fat dairy and milk and the risk of hypertension;
intakes of total dairy and milk and the risk of MetS; and
intakes of total dairy and cheese and the risk of T2D.
On the basis of the adapted GRADE criteria, these favorable associations are very likely. However, future studies may modify risk estimates toward confirmed favorable associations or toward the null.
Finally, there is high- to moderate-quality evidence that:
consumption of total dairy, cheese, and yogurt is neutral in terms of CVD risk;
consumption of all forms of dairy, except for fermented, is neutral in terms of CAD risk;
consumption of regular- and high-fat dairy, milk, and yogurt is neutral in terms of stroke risk;
consumption of regular- and high-fat dairy, cheese, yogurt, and fermented dairy is neutral in terms of risk of hypertension; and
consumption of regular- and high-fat dairy, milk, and fermented dairy is neutral in terms of risk T2D.
2. Is the recommendation to consume low-fat as opposed to regular- and high-fat dairy supported by the existing evidence?
First, there is no evidence from this extensive review that the consumption of dairy fat or of regular- and high-fat dairy is detrimental to cardiovascular-related clinical outcomes. More specifically, the:
consumption of regular- and high-fat dairy is neutral in terms of risk of CAD, stroke, hypertension, and T2D, which is supported by high- to moderate-quality evidence;
consumption of low-fat dairy is neutral in terms of CAD risk, which is supported by high-quality evidence; and
consumption of low-fat dairy is favorably associated with the risk of stroke, hypertension, and T2D, which is supported by high- to moderate-quality evidence.
Examining the association of dairy intake to health according to fat content is tremendously challenging for several reasons. In most epidemiologic studies, the “low-fat” terminology generally referred to fat-reduced products such as skimmed or low-fat milk (0–1% fat), nonfat yogurt (0% fat), and low-fat cheese (15–20% fat). Inversely, whole milk (3% fat) has been analyzed in population studies along with regular-fat cheese (>30% fat) as regular- and high-fat dairy products. The fat and nutrient profile is highly variable within each of those categories. Grouping them into simplistic classes such as regular- and high-fat or low-fat may confound the analysis of their association with clinical outcomes. A good example of this pertains to cheese, which even in its low-fat version is a product that is much higher in fat, and thus that contributes more to SFA intake, than whole-fat milk. Cheese intake is inversely associated with the risk of stroke and T2D (supported by moderate-quality evidence), whereas the intake of regular-fat dairy shows a neutral association with these outcomes (moderate- to high-quality evidence). The use of biomarkers of dairy fat intake provides a certain perspective on the association between regular- and high-fat dairy and health. However, it is limited by the fact that it does not allow the study of the association between whole foods and health.
It is unclear in dietary guidelines if the recommendations to consume low-fat dairy imply that individuals select the low-fat version in place of the regular- and high-fat version of a dairy product or choose an intrinsically low-fat dairy (e.g., skimmed milk) instead of intrinsically high-fat dairy (e.g., cheese). The first scenario represents a key research gap that needs proper research. Indeed, high- or moderate-quality evidence that shows that low-fat milk compared with whole-milk or low-fat cheese compared with regular-fat cheese is better for health is utterly lacking. The consumption of low-fat dairy may provide some advantages with respect to the risk of stroke, hypertension, and T2D, but there are currently no data indicating that this is the case for each dairy product taken individually. For the second scenario (e.g., choosing skimmed milk instead of cheese), again, the evidence is weak because in some instances (e.g., stroke, T2D), cheese consumption is actually associated with a reduced risk. Replacing a solid dairy such as cheese with a liquid dairy such as milk is a much more complex dietary change than switching between 2 liquid foods or between 2 solid foods. Thus, more research that addresses this particular scenario is also warranted, not just from a health perspective but also from a dietary change perspective. In the meantime, we hypothesize that the recommendation to focus on low-fat in place of regular- and high-fat dairy products is a concept that may be not be fully captured by the population, that such a concept may not reflect food choices that people make at the individual level, and that such a recommendation is not based on the current state of evidence.
As indicated above, additional studies are needed to address the following key research gaps:
to compare the impact of regular-fat dairy products with their reduced-fat or skimmed versions on health outcomes;
to assess the association between milk and fermented dairy and the risk of CVD specifically, because these associations are currently uncertain;
to assess the association between cheese, yogurt, and fermented dairy intakes specifically and the risk of MetS specifically, because these associations are currently uncertain; and
to conduct higher quality meta-analyses, because 18 of the 21 available to date (Table 1) have been scored as being of moderate quality or lower on the basis of the recognized MOOSE grading system.
Assessing publication bias systematically in future meta-analyses will also greatly enhance the quality of evidence. This is identified as a major shortcoming in the existing literature.
Some of the meta-analyses presented in this review have revealed heterogeneity between prospective cohort studies. Most studies have adjusted risk estimates for various covariables, limiting the risk of confounding. However, one cannot exclude the possibility of uncontrollable bias in large, prospective, epidemiologic cohort studies. Kratz et al. (51) stressed that dietary assessment that uses FFQ in prospective cohort studies may be influenced by the social value associated with the food. In Western countries, high-fat dairy consumption is much less prevalent than low-fat dairy consumption. This has an obvious impact on the statistical power to measure associations with high-fat dairy. Kratz et al. also discussed the impact of differences in bovine feeding practices between countries, which affect the quality and composition of the dairy fat. This has not been taken into account in existing prospective cohort studies. Finally, the extent to which the association between dairy intake and health outcomes is fully independent of concurrent variations in other health-related variables, such as diet, socioeconomic status, and other factors, is unclear (51). Additional studies are therefore also needed to assess the association between dairy intake and clinical outcomes in various populations (obese compared with nonobese, males compared with females, different geographical areas) (16, 51).
In conclusion, this systematic review provides an in-depth perspective on the association between dairy product consumption and the risk of cardiovascular-related clinical outcomes, including MetS and T2D. Although there are still key research gaps to address, evidence suggests either a neutral or a favorable association between dairy intake and cardiovascular-related outcomes. These data are consistent with current dietary guidelines, which place dairy as one of the pillars of healthy eating. However, the review also emphasized that the recommendation to focus on low-fat in place of regular- and high-fat dairy is currently not evidence-based. Further research is needed to specifically address this key research gap.
Acknowledgments
All authors read and approved the final manuscript.
Footnotes
Abbreviations used: CAD, coronary artery disease; CVD, cardiovascular disease; GRADE: Grading of Recommendations Assessment, Development, and Evaluation; IHD, ischemic heart disease; MetS, metabolic syndrome; MOOSE, Meta-analysis Of Observational Study in Epidemiology; T2D, type 2 diabetes; TFA, trans fatty acid.
References
- 1.Weinberg LG, Berner LA, Groves JE. Nutrient contributions of dairy foods in the United States, Continuing Survey of Food Intakes by Individuals, 1994–1996, 1998. J Am Diet Assoc 2004;104:895–902. [DOI] [PubMed] [Google Scholar]
- 2.de Oliveira Otto MC, Mozaffarian D, Kromhout D, Bertoni AG, Sibley CT, Jacobs DR Jr, Nettleton JA. Dietary intake of saturated fat by food source and incident cardiovascular disease: the Multi-Ethnic Study of Atherosclerosis. Am J Clin Nutr 2012;96:397–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008–12. [DOI] [PubMed] [Google Scholar]
- 5.Elwood PC, Pickering JE, Hughes J, Fehily AM, Ness AR. Milk drinking, ischaemic heart disease and ischaemic stroke II. Evidence from cohort studies. Eur J Clin Nutr 2004;58:718–24. [DOI] [PubMed] [Google Scholar]
- 6.Elwood PC, Givens DI, Beswick AD, Fehily AM, Pickering JE, Gallacher J. The survival advantage of milk and dairy consumption: an overview of evidence from cohort studies of vascular diseases, diabetes and cancer. J Am Coll Nutr 2008;27:723S–34S. [DOI] [PubMed] [Google Scholar]
- 7.Elwood PC, Pickering JE, Givens DI, Gallacher JE. The consumption of milk and dairy foods and the incidence of vascular disease and diabetes: an overview of the evidence. Lipids 2010;45:925–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Soedamah-Muthu SS, Ding EL, Al-Delaimy WK, Hu FB, Engberink MF, Willett WC, Geleijnse JM. Milk and dairy consumption and incidence of cardiovascular diseases and all-cause mortality: dose-response meta-analysis of prospective cohort studies. Am J Clin Nutr 2011;93:158–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tong X, Dong JY, Wu ZW, Li W, Qin LQ. Dairy consumption and risk of type 2 diabetes mellitus: a meta-analysis of cohort studies. Eur J Clin Nutr 2011;65:1027–31. [DOI] [PubMed] [Google Scholar]
- 10.Bendsen NT, Christensen R, Bartels EM, Astrup A. Consumption of industrial and ruminant trans fatty acids and risk of coronary heart disease: a systematic review and meta-analysis of cohort studies. Eur J Clin Nutr 2011;65:773–83. [DOI] [PubMed] [Google Scholar]
- 11.Ralston RA, Lee JH, Truby H, Palermo CE, Walker KZ. A systematic review and meta-analysis of elevated blood pressure and consumption of dairy foods. J Hum Hypertens 2012;26:3–13. [DOI] [PubMed] [Google Scholar]
- 12.Soedamah-Muthu SS, Verberne LD, Ding EL, Engberink MF, Geleijnse JM. Dairy consumption and incidence of hypertension: a dose-response meta-analysis of prospective cohort studies. Hypertension 2012;60:1131–7. [DOI] [PubMed] [Google Scholar]
- 13.Aune D, Norat T, Romundstad P, Vatten LJ. Dairy products and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Am J Clin Nutr 2013;98:1066–83. [DOI] [PubMed] [Google Scholar]
- 14.Gao D, Ning N, Wang C, Wang Y, Li Q, Meng Z, Liu Y, Li Q. Dairy products consumption and risk of type 2 diabetes: systematic review and dose-response meta-analysis. PLoS One 2013;8:e73965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O’Sullivan TA, Hafekost K, Mitrou F, Lawrence D. Food sources of saturated fat and the association with mortality: a meta-analysis. Am J Public Health 2013;103:e31–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen M, Sun Q, Giovannucci E, Mozaffarian D, Manson JE, Willett WC, Hu FB. Dairy consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. BMC Med 2014;12:215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chowdhury R, Warnakula S, Kunutsor S, Crowe F, Ward HA, Johnson L, Franco OH, Butterworth AS, Forouhi NG, Thompson SG, et al. . Association of dietary, circulating, and supplement fatty acids with coronary risk: a systematic review and meta-analysis. Ann Intern Med 2014;160:398–406. [DOI] [PubMed] [Google Scholar]
- 18.Hu D, Huang J, Wang Y, Zhang D, Qu Y. Dairy foods and risk of stroke: a meta-analysis of prospective cohort studies. Nutr Metab Cardiovasc Dis 2014;24:460–9. [DOI] [PubMed] [Google Scholar]
- 19.Qin LQ, Xu JY, Han SF, Zhang ZL, Zhao YY, Szeto IM. Dairy consumption and risk of cardiovascular disease: an updated meta-analysis of prospective cohort studies. Asia Pac J Clin Nutr 2015;24:90–100. [DOI] [PubMed] [Google Scholar]
- 20.de Souza RJ, Mente A, Maroleanu A, Cozma AI, Ha V, Kishibe T, Uleryk E, Budylowski P, Schünemann H, Beyene J, et al. . Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies. BMJ 2015;351:h3978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Larsson SC, Crippa A, Orsini N, Wolk A, Michaelsson K. Milk consumption and mortality from all causes, cardiovascular disease, and cancer: a systematic review and meta-analysis. Nutrients 2015;7:7749–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen GC, Szeto IM, Chen LH, Han SF, Li YJ, van Hekezen R, Qin LQ. Dairy products consumption and metabolic syndrome in adults: systematic review and meta-analysis of observational studies. Sci Rep 2015;5:14606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim Y, Je Y. Dairy consumption and risk of metabolic syndrome: a meta-analysis. Diabet Med 2016;33:428–40. [DOI] [PubMed] [Google Scholar]
- 24.Alexander DD, Bylsma LC, Vargas AJ, Cohen SS, Doucette A, Mohamed M, Irvin SR, Miller PE, Watson H, Fryzek JP. Dairy consumption and CVD: a systematic review and meta-analysis. Br J Nutr 2016;115:737–50. [DOI] [PubMed] [Google Scholar]
- 25.Gijsbers L, Ding EL, Malik VS, de Goede J, Geleijnse JM, Soedamah-Muthu SS. Consumption of dairy foods and diabetes incidence: a dose-response meta-analysis of observational studies. Am J Clin Nutr 2016;103:1111–24. [DOI] [PubMed] [Google Scholar]
- 26.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336:924–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schunemann HJ. What is “quality of evidence” and why is it important to clinicians? BMJ 2008;336:995–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, Brozek J, Vist GE, Falck-Ytter Y, Meerpohl J, Norris S, et al. . GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011;64:401–6. [DOI] [PubMed] [Google Scholar]
- 29.van Aerde MA, Soedamah-Muthu SS, Geleijnse JM, Snijder MB, Nijpels G, Stehouwer CD, Dekker JM. Dairy intake in relation to cardiovascular disease mortality and all-cause mortality: the Hoorn Study. Eur J Nutr 2013;52:609–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.von Ruesten A, Feller S, Bergmann MM, Boeing H. Diet and risk of chronic diseases: results from the first 8 years of follow-up in the EPIC-Potsdam study. Eur J Clin Nutr 2013;67:412–9. [DOI] [PubMed] [Google Scholar]
- 31.Praagman J, Franco OH, Ikram MA, Soedamah-Muthu SS, Engberink MF, van Rooij FJ, Hofman A, Geleijnse JM. Dairy products and the risk of stroke and coronary heart disease: the Rotterdam Study. Eur J Nutr 2015;54:981–90. [DOI] [PubMed] [Google Scholar]
- 32.Praagman J, Dalmeijer GW, van der Schouw YT, Soedamah-Muthu SS, Monique Verschuren WM, Bas Bueno-de-Mesquita H, Geleijnse JM, Beulens JW. The relationship between fermented food intake and mortality risk in the European Prospective Investigation into Cancer and Nutrition-Netherlands cohort. Br J Nutr 2015;113:498–506. [DOI] [PubMed] [Google Scholar]
- 33.Yakoob MY, Shi P, Hu FB, Campos H, Rexrode KM, Orav EJ, Willett WC, Mozaffarian D. Circulating biomarkers of dairy fat and risk of incident stroke in U.S. men and women in 2 large prospective cohorts. Am J Clin Nutr 2014;100:1437–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pereira MA, Jacobs DR Jr, Van Horn L, Slattery ML, Kartashov AI, Ludwig DS. Dairy consumption, obesity, and the insulin resistance syndrome in young adults: the CARDIA study. JAMA 2002;287:2081–9. [DOI] [PubMed] [Google Scholar]
- 35.Fumeron F, Lamri A, Abi Khalil C, Jaziri R, Porchay-Balderelli I, Lantieri O, Vol S, Balkau B, Marre M. Dairy consumption and the incidence of hyperglycemia and the metabolic syndrome: results from a French prospective study, Data from the Epidemiological Study on the Insulin Resistance Syndrome (DESIR). Diabetes Care 2011;34:813–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Samara A, Herbeth B, Ndiaye NC, Fumeron F, Billod S, Siest G, Visvikis-Siest S. Dairy product consumption, calcium intakes, and metabolic syndrome-related factors over 5 years in the STANISLAS study. Nutrition 2013;29:519–24. [DOI] [PubMed] [Google Scholar]
- 37.Wang H, Fox CS, Troy LM, McKeown NM, Jacques PF. Longitudinal association of dairy consumption with the changes in blood pressure and the risk of incident hypertension: the Framingham Heart Study. Br J Nutr 2015;114:1887–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shin H, Yoon YS, Lee Y, Kim CI, Oh SW. Dairy product intake is inversely associated with metabolic syndrome in Korean adults: Anseong and Ansan cohort of the Korean Genome and Epidemiology Study. J Korean Med Sci 2013;28:1482–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Livingstone KM, Lovegrove JA, Cockcroft JR, Elwood PC, Pickering JE, Givens DI. Does dairy food intake predict arterial stiffness and blood pressure in men?: Evidence from the Caerphilly Prospective Study. Hypertension 2013;61:42–7. [DOI] [PubMed] [Google Scholar]
- 40.Sayón-Orea C, Bes-Rastrollo M, Marti A, Pimenta AM, Martin-Calvo N, Martinez-Gonzalez MA. Association between yogurt consumption and the risk of metabolic syndrome over 6 years in the SUN study. BMC Public Health 2015;15:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Snijder MB, van Dam RM, Stehouwer CD, Hiddink GJ, Heine RJ, Dekker JM. A prospective study of dairy consumption in relation to changes in metabolic risk factors: the Hoorn Study. Obesity (Silver Spring) 2008;16:706–9. [DOI] [PubMed] [Google Scholar]
- 42.Damião R, Castro TG, Cardoso MA, Gimeno SG, Ferreira SR. Dietary intakes associated with metabolic syndrome in a cohort of Japanese ancestry. Br J Nutr 2006;96:532–8. [PubMed] [Google Scholar]
- 43.Lutsey PL, Steffen LM, Stevens J. Dietary intake and the development of the metabolic syndrome: the Atherosclerosis Risk in Communities Study. Circulation 2008;117:754–61. [DOI] [PubMed] [Google Scholar]
- 44.Baik I, Lee M, Jun NR, Lee JY, Shin C. A healthy dietary pattern consisting of a variety of food choices is inversely associated with the development of metabolic syndrome. Nutr Res Pract 2013;7:233–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Louie JC, Flood VM, Rangan AM, Burlutsky G, Gill TP, Gopinath B, Mitchell P. Higher regular fat dairy consumption is associated with lower incidence of metabolic syndrome but not type 2 diabetes. Nutr Metab Cardiovasc Dis 2013;23:816–21. [DOI] [PubMed] [Google Scholar]
- 46.Babio N, Becerra-Tomas N, Martinez-Gonzalez MA, Corella D, Estruch R, Ros E, Sayon-Orea C, Fito M, Serra-Majem L, Aros F, et al. . Consumption of yogurt, low-fat milk, and other low-fat dairy products is associated with lower risk of metabolic syndrome incidence in an elderly Mediterranean population. J Nutr 2015;145:2308–16. [DOI] [PubMed] [Google Scholar]
- 47.Duffey KJ, Gordon-Larsen P, Steffen LM, Jacobs DR Jr, Popkin BM. Drinking caloric beverages increases the risk of adverse cardiometabolic outcomes in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Clin Nutr 2010;92:954–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.O’Connor LM, Lentjes MA, Luben RN, Khaw KT, Wareham NJ, Forouhi NG. Dietary dairy product intake and incident type 2 diabetes: a prospective study using dietary data from a 7-day food diary. Diabetologia 2014;57:909–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bergholdt HK, Nordestgaard BG, Ellervik C. Milk intake is not associated with low risk of diabetes or overweight-obesity: a Mendelian randomization study in 97,811 Danish individuals. Am J Clin Nutr 2015;102:487–96. [DOI] [PubMed] [Google Scholar]
- 50.Díaz-López A, Bullo M, Martinez-Gonzalez MA, Corella D, Estruch R, Fito M, Gomez-Gracia E, Fiol M, Garcia de la Corte FJ, Ros E, et al. . Dairy product consumption and risk of type 2 diabetes in an elderly Spanish Mediterranean population at high cardiovascular risk. Eur J Nutr 2016;55:349–60. [DOI] [PubMed] [Google Scholar]
- 51.Kratz M, Baars T, Guyenet S. The relationship between high-fat dairy consumption and obesity, cardiovascular, and metabolic disease. Eur J Nutr 2013;52:1–24. [DOI] [PubMed] [Google Scholar]