Abstract
Background
Discharge location is associated with short-term readmission rates following hospitalization for several medical and surgical diagnoses. We hypothesized that discharge location: home, home health, skilled nursing facility (SNF), long-term acute care (LTAC), or inpatient rehabilitation independently predicted the risk of 30-day readmission and severity of first readmission following orthotopic liver transplant (OLT).
Study Design
Retrospective cohort review using Healthcare Cost and Utilization Project (HCUP) State Inpatient Databases for Florida and California. Patients who underwent OLT from 2009 to 2011 were included and followed for 1 year. Mixed-effects logistic regression was used to model the effect of discharge location on 30-day readmission controlling for demographic, socioeconomic, and clinical factors. Total cost of first readmission was used as a surrogate measure for readmission severity and resource utilization.
Results
A total of 3,072 patients met our inclusion criteria. Overall 30-day readmission rate was 29.6%. Discharge to inpatient rehabilitation (aOR=0.43, p=0.013) or LTAC/SNF (aOR=0.63, p=0.014) were associated with decreased odds of 30-day readmission when compared to home. The severity of 30-day readmissions for patients discharged to inpatient rehabilitation were the same as those discharged home or home with home health. Severity was increased for those discharged to LTAC/SNF. The time to first readmission was longest for patients discharged to inpatient rehabilitation (17 days vs 8 days, p<0.001).
Conclusions
When compared to other locations of discharge, inpatient rehabilitation reduces the risk of 30-day readmission and increases the time to first readmission. These benefits come without increasing the severity of readmission. Increased utilization of inpatient rehabilitation following OLT is a strategy to improve 30-day readmission rates.
Keywords: discharge destination, inpatient rehabilitation, liver transplantation, readmission, disposition
INTRODUCTION
Hospital readmission rates following inpatient admissions are important quality metrics and have important financial implications.(1, 2) The Centers for Medicare and Medicaid Services (CMS) first brought readmissions into focus with public reporting of hospital rates in 2009.(3) With the introduction of the Hospital Readmission Reduction Program (HRRP) in 2012, as part of the Affordable Care Act, hospitals with excess readmissions were subject to CMS financial penalties. Beginning with acute myocardial infarction, heart failure, and pnuemonia, the program now also includes chronic obstructive pulmonary disease, elective primary total hip and/or total knee arthroplasty, and soon will include coronary artery bypass graft.(2,4) Although readmissions following liver transplantation are not currently penalized by CMS’s programs, several groups anticipate this could change as the HRRP continues to grow.(5,6)
Readmission rates following liver transplant are high, with reported rates ranging from 37.9% to 45%.(7–9) While the reasons for readmission following non-transplant surgery are largely attributable to new complications from the index operation, this is not clearly defined in liver transplantation.(10) Both surgical and medical reasons for readmission are described in this patient population and include infection, abnormal laboratory values, electrolyte disturbances, and postoperative pain.(8,11) As a result, efforts for reducing readmissions must be multifactorial and include prehospital, hospital, and post-hospital targets.
Recent studies have identified preoperative and immediate postoperative predictors for readmission after liver transplantation.(12) However, there is a paucity of data examining the period of time after discharge and the role discharge destination plays on unplanned readmission in this vulnerable population. The primary objective of this study was to determine the association between discharge location (home, home health, skilled nursing facility (SNF), long-term acute care (LTAC), or inpatient rehabilitation) and risk of 30-day readmission following liver transplantation. Secondary objectives included defining the severity of first readmission after surgery and determining the causes of readmission based on location of discharge.
METHODS
Data Sources
The Healthcare Cost and Utilization Project State Inpatient Databases (HCUP SID) for Florida and California were used to identify cases from 2009 – 2011. Each SID captures all inpatient stays at non-federal facilities for the respective state, regardless of primary payer. Encounters in the SID are obtained from participating state-level data organizations and based on data abstracted from inpatient discharge records.(13) The SID is organized using uniform formatting allowing for use of HCUP tools and software to facilitate clinical research.
A total of 17 states include variables to track sequential visits for an individual patient over time within the state. The consistency of encrypted person identifiers is measured by HCUP and varies by state. The states of California and Florida each have notably high reliability (88.3% and 96.0%).(14)
The study was deemed exempt from institutional review board approval based on the use of de-identified records.
Patient Inclusion
Records for patients ≥18 years old who underwent orthotopic liver transplant were identified using the International Classification of Diseases, Version 9, Clinical Modification (ICD-9-CM) procedure code 505.9. Patients were only included if they also had the Diagnosis Related Group (version 24) 480 as part of their discharge record. Patients with concurrent renal transplant were excluded. Any unplanned inpatient admissions within 30 days of discharge were categorized as readmissions and all readmissions were in reference to the original operation. HCUP SID classifies each patient record as emergent, urgent, or elective. A readmission was considered unplanned if the patient encounter was urgent or emergent. Patients with repeat liver transplant ≤30 days from discharge were excluded.
Outcome and Exposure Variables
Our primary end-point was unplanned readmission within 30 days of discharge following initial liver transplant. Secondary outcomes included reason and severity of readmission. Severity of readmission was estimated using the total cost of an inpatient readmission encounter, not including the cost of post-discharge care. This was derived using charge to cost conversion and normalized to allow comparisons of patients at different hospitals.
Location of discharge was the principle exposure variable and assigned using uniform fields provided by HCUP. Crosswalk between HCUP indicators and assigned category of discharge location for study are shown in Supplementary Table 1 (online only). No missing values were present for discharge location in any of the discharge records that met our inclusion criteria.
Explanatory Variables
To capture the complexity of admission at time of liver transplant, patient demographic and clinical characteristics were used based on availability within the dataset. Charlson Comorbidity Index was calculated using an add-on STATA module.(15) Reason for transplant was determined using each patient’s coded diagnoses that were present on admission at time of transplant and categorized into the following groups: viral, alcohol, autoimmune, malignancy, other, unknown (Supplementary Table 2, online only).
Preoperative length of stay was defined as time from admission to surgery and postoperative length of stay from time of surgery to discharge. A major inpatient complication was defined as having at least one of the following: myocardial infarction, pulmonary embolism, septic shock. A moderate inpatient complication was defined as having at least one of the following: urinary tract infection, deep-vein thrombosis, wound complications, pneumonia. Complications were based on ICD-9-CM codes that were not present on admission.
Reason for readmission was determined using the principal coded diagnosis for the first readmission ≤30 days. If the primary diagnosis was Complications of transplanted liver (996.82), the remaining diagnoses on record that were present on admission were evaluated to find a more specific reason for readmission (Supplementary Table 3, online only).
Statistical Analysis
Standard descriptive statistics are reported with arithmetic means (standard deviation), medians (interquartile range), or frequencies (proportions). Bivariate statistical testing for comparisons of multiple groups was conducted with one-way ANOVA (parametric) or Kruskal-Wallis equality-of-populations test (non-parametric).
Unadjusted comparisons of exposure and outcome were performed using simple logistic regression. Multivariable models were fit using forward selection with a threshold of p<0.2 for inclusion using each of the variables present in Table 1. Variables not selected with clinical relevance were forced into the model. Relative model quality was assessed using the Akaike information criterion (AIC) where models with smaller AID values were selected and classification measured using the c-statistic.
Table 1.
Baseline Characteristics of Study Population, by Location of Discharge
| Variable | All patients (N=3,072) | Home (n=1,939) | Home health (n=779) | SNF/LTAC (n=193) | Inpatient rehabilitation (n=70) | p Value |
|---|---|---|---|---|---|---|
| Mean age, y, mean (SD) | 54.9 (10.1) | 54.2 (10.3) | 55.6 (9.8) | 57.2 (9.0) | 59.8 (7.6) | 0.001 |
| Sex, female, n (%) | 1,041 (33.9) | 620 (32.0) | 278 (35.7) | 88 (45.6) | 21 (30.0) | 0.002 |
| Race, n (%) | <0.001 | |||||
| Caucasian | 1,792 (58.8) | 1,171 (61.0) | 401 (51.9) | 111 (57.5) | 58 (82.9) | |
| African-American | 180 (5.9) | 114 (5.9) | 44 (5.7) | 15 (7.8) | <10* | |
| Hispanic | 698 (22.9) | 374 (19.5) | 246 (31.9) | 42 (21.8) | 10 (14.3) | |
| Asian | 233 (7.7) | 155 (8.1) | 56 (7.3) | 16 (8.2) | <10* | |
| Other | 143 (4.7) | 107 (5.5) | 25 (3.2) | 10 (4.7) | <10* | |
| Insurance type | <0.001 | |||||
| Medicare, n (%) | 845 (27.5) | 488 (25.2) | 239 (30.7) | 70 (36.3) | 28 (40.0) | |
| Medicaid, n (%) | 488 (15.9) | 318 (16.4) | 132 (16.9) | 16 (8.3) | <10* | |
| Private, n (%) | 1,665 (54.2) | 1,085 (56.0) | 393 (50.5) | 104 (53.9) | 36 (51.4) | |
| Other, n (%) | 74 (2.4) | 48 (2.4) | 15 (1.9) | <10* | <10* | |
| CCI, mean (SD) | 3.8 (1.7) | 3.8 (1.7) | 3.9 (1.6) | 4.0 (1.7) | 3.9 (1.3) | 0.021 |
| Reason for transplant, n (%) | 0.001 | |||||
| Viral | 1,319 (42.9) | 891 (46.0) | 306 (39.3) | 63 (32.6) | 25 (35.7) | |
| Alcohol | 573 (18.7) | 321 (16.6) | 160 (20.5) | 52 (26.9) | 20 (28.6) | |
| Autoimmune | 533 (17.4) | 133 (6.9) | 47 (6.0) | 20 (10.3) | <10* | |
| Malignancy | 346 (11.3) | 225 (11.6) | 86 (11.0) | 20 (10.4) | <10* | |
| Other cirrhosis | 215 (7.0) | 315 (16.3) | 154 (19.8) | 34 (17.6) | 12 (17.1) | |
| Unknown | 86 (2.7) | 54 (2.6) | 26 (3.4) | <10* | <10* | |
| Clinical predictors | ||||||
| Preoperative LOS, n (range) | 1 (0 – 6) | 1 (0 – 1) | 1 (0–11) | 8 (1–18) | 1 (0–15) | <0.001 |
| Postoperative LOS, n (range) | 10 (7–17) | 8 (6–12) | 15 (10–24) | 22 (14–35) | 24 (13–36) | <0.001 |
| Major IP complications, n (%) | 359 (11.7) | 156 (8.1) | 88 (11.3) | 49 (25.4) | 17 (24.3) | <0.001 |
| Moderate IP complications, n (%) | 432 (14.1) | 172 (8.9%) | 161 (20.7) | 59 (30.6) | 16 (22.9) | <0.001 |
Cannot report due to HCUP protections.
IP, inpatient; LOS, length of stay; CCI, Charlson Comorbidity Index; SNF, Skilled nursing facility; LTAC, long-term acute care.
Time to event analysis using competing risk modeling was used to measure the risk of readmission for each post-discharge day, stratified by location of discharge. Event time was defined as time from discharge to first 30-day readmission and the event was first 30-day readmission. Death following discharge was the competing risk. The mean predicted subhazard ratio was calculated for each day following discharge to derive a predicted daily readmission hazard.
Statistical analysis was performed in STATA MP Version 13 (College Station, TX, 64 bit).
RESULTS
A total of 3,072 patients met our inclusion criteria and comprised the final analytic sample. Patients were further stratified based on location of discharge after liver transplantation with 1,939 (63.1%) discharged home, 779 (25.4%) discharged home with home health, 193 (6.3%) to a SNF or LTAC, and 70 (2.2%) to inpatient rehabilitation. A total of 91 (3.0%) died during the index hospitalization.
Patient demographic variables were compared across groups and results are shown in Table 1. Average age of the popluation was 54.9 years (SD=10.1 years) and the majority (66.1%) were male gender. Overall, patients were most commonly caucasian race (58.8%), privately insured (54.2%), and underwent liver transplant for viral etiologies (42.9%).
When compared to patients discharged home, those discharged to LTAC/SNF or inpatient rehabilitation had longer preoperative and postoperative length of stays (p<0.001, Table 1). Additionally, those discharged to LTAC/SNF or inpatient rehabilitation had higher incidence of complications, both major and moderate, when compared to those discharged home (p<0.001).
Overall 30-day readmission rate of the study population was 29.6%. This differed based on location of discharge, ranging from 17.1% to 32.7% (Table 2). Unadjusted analysis demonstrated decreased odds of readmission, when compared to home, for those discharged to inpatient rehabilitiation (OR=0.48, p=0.021). On multivariable analysis, inpatient rehabilitation remained significant (OR=0.43, p=0.013) and LTAC/SNF discharge also decreased the odds of readmission (0.63, p=0.014). Odds of readmission did not differ for those discharged home with home health compared to home.
Table 2.
Discharge Location and Odds of 30-Day Readmission (Adjusted and Unadjusted)
| Discharge destination | n | Inpatient readmission, n (%) | Unadjusted odds | p Value | Adjusted odds* | p Value |
|---|---|---|---|---|---|---|
| Home | 1,939 | 588 (30.3) | 1 [Reference] | 1 [Reference] | ||
| Home with home health | 779 | 255 (32.7) | 1.11 | 0.220 | 0.92 | 0.418 |
| LTAC/SNF | 193 | 53 (27.5) | 0.87 | 0.408 | 0.63 | 0.014 |
| Inpatient rehabilitation | 70 | 12 (17.1) | 0.48 | 0.021 | 0.43 | 0.013 |
Adjusted odds based on multivariable model reported in Table 3.
LTAC, Long-term acute care; SNF, Skilled nursing facility.
Details of the risk model used to determine the adjusted odds for readmission are shown in Table 3. To assess the strength of association between measured covariates, forward selection was used to identify the order variables were entered into the model. Discharge destination was selected into the model early (coefficient −0.84, 95% C.I. −1.50, −0.18) and its inclusion improved model performance (AIC=3604.8 vs. 3599.7). Other variables selected into the model reflected the severity of inpatient admission and included inpatient complications (coefficient 0.37, 95% C.I. 0.12, 0.62), postoperative length of stay (coefficient 0.01, 95% C.I. 0.00, 0.02), and Charlson Comorbidity Index (coefficient 0.06, 95% C.I. 0.03, 0.11).
Table 3.
Model Covariates and Coefficients for Multivariable Model of 30-Day Readmission after Liver Transplantation
| Fixed-effects | Coefficient | 95% CI | AIC* |
|---|---|---|---|
| Moderate IP complications (binary) | 0.37 | 0.12, 0.62 | 3609.4 |
| Valvular disease (binary) | 0.53 | 0.16, 0.91 | 3603.7 |
| Postoperative LOS (continuous) | 0.01 | 0.00, 0.02 | 3604.8 |
| Discharge destination (factor) | 3599.7 | ||
| Home | [Reference] | ||
| Home with home health | −0.09 | −0.30, 0.12 | |
| LTAC/SNF | −0.47 | −0.84, −0.09 | |
| Inpatient Rehabilitation | −0.84 | −1.50, −0.18 | |
| Charlson comorbidity index (continuous) | 0.06 | 0.03, 0.11 | 3599.3 |
| Neurologic disorders (binary) | −0.28 | −0.64, 0.08 | 3599.3 |
| Race (factor) | 3569.2 | ||
| Caucasian | [Reference] | ||
| African American | 0.07 | −0.27, 0.42 | |
| Hispanic | −0.03 | −0.23, 0.18 | |
| Asian | −0.28 | −0.61, 0.05 | |
| Other | −0.45 | −0.87, −0.03 | |
| Forced in variables† | |||
| Preoperative LOS (continuous) | 0.002 | −0.008, 0.012 | 3570.9 |
| Reason for transplant | 3575.6 | ||
| Unknown | [Reference] | ||
| Unspecified | −0.34 | −0.84, 0.16 | |
| Autoimmune | −0.25 | −0.81, 0.31 | |
| Alcohol | −0.28 | −0.77, 0.22 | |
| Malignancy | −0.51 | −1.04, 0.03 | |
| Viral | −0.24 | −0.71, 0.24 | |
| Random effects, estimate, hospital | 0.39 | 0.25, 0.61 |
AIC for each additional fixed effect entered in model.
Forced in variables added to model although not selected with forward selection techniques.
AIC, Akaike Information Criterion; IP, inpatient; LOS, length of stay; LTAC, long term acute care; SNF, skilled nursing facility.
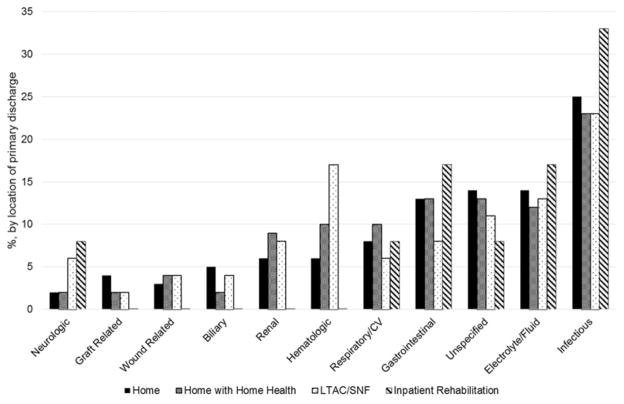
Reasons for 30-day readmissions are shown in Figure 1. For each discharge location, the most common cause for first readmission was related to infectious complications, ranging from 23% for those discharged home to 33% for those discharged to inpatient rehabilitation. Other reasons for readmission that were similar across discharge locations included electrolyte/fluid disturbances (range 12% – 17%) and respiratory/cardiovascular causes (6 – 10%).
Figure 1.
Reasons for first readmission after liver transplant, stratified by location of discharge. CV, cerebrovascular; LTAC/SNF, long-term acute care/skilled nursing facility.
Next, the severity of 30-day readmission was assessed using inpatient costs during a readmission encounter. When studying only the first 30-day readmission, the median cost of readmission was similar for patients readmitted to home or home with home health ($10,703.60 [IQR $6,149.81 – 21,306.53] vs. $10,423.65 [IQR $5,659.31 – 26,252.12]). These costs were less than readmissions for patients discharged to LTAC/SNF ($22,285.23 [IQR $6,304.15 – 44,705.29]) and inpatient rehabilitation ($14,629.20 [IQR $11,126.03 – 72,138]). This appeared to suggest readmissions following home discharges were less severe than those following non-home discharges.
Importantly, the number of readmissions within 30 days differed based on location of discharge (Table 4). To account for these differences, the total costs of all readmissions within 30 days were measured. Following this adjustment, total costs of 30-day readmissions for patients discharged home, home with home health, and inpatient rehabilitation were similar. Costs for readmission for patients discharged from LTAC/SNF remained higher than other locations.
Table 4.
Time to First Readmission, Number of Readmissions, and Costs of First and All 30-Day Readmissions after Liver Transplant
| Home (n=1,939) | Home health (n=779) | LTAC/SNF (n=193) | Inpatient rehabilitation (n=70) | |
|---|---|---|---|---|
| Time to first readmission, d, median (IQR) | 8 (3–16) | 8 (4–15) | 8 (6–17) | 17 (10.5–21) |
| No. of 30-d readmissions, n (%) | ||||
| 1 | 441 (75.0) | 192 (75.3) | 41 (77.4) | 12 (100.0) |
| >1 | 147 (25.0) | 63 (24.7) | 12 (22.6) | 0 (0.0) |
| Cost of first 30-d readmission, median (range) | $10,703.60 ($6,149.81 – 21,306.53) | $10,423.65 ($5,659.31 – 26,252.12) | $22,285.23 ($6,304.15 – 44,705.29) | $14,629.20 (11,126.03 – 72,138.54) |
| Total cost of 30-day readmissions, $, median (IQR) | $12,424.24 ($6,524.93 – 25,929.96) | $12,959.45 ($6,353.88 – 28,967.34) | $25,535.94 ($6,793.57 – 53,165.93) | $14,629.20 ($11,126.03 – 72,138.54) |
LTAC, Long-term acute care; SNF, Skilled nursing facility; IQR, Interquartile range.
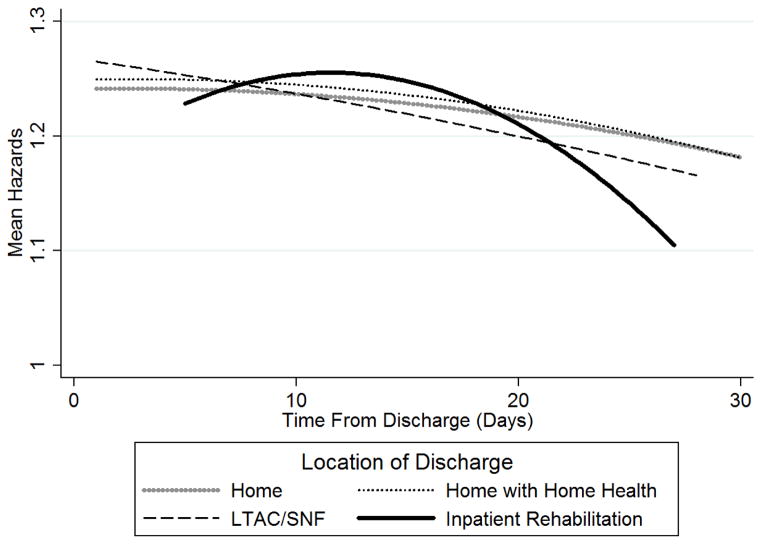
Last, we calculated the predicted subdistribution hazard ratio (SHR) for each day following discharge to quantify the daily risk of readmission (Figure 2). The mean SHR represents the readmission hazard for each discharge destination relative to the baseline hazard when all model covariates equal zero. The postoperative SHR for patients discharged home, home with home health, and LTAC/SNF gradually decreased over time. For patients discharged to inpatient rehabilitation, the SHR peaked at 16 days before decreasing.
Figure 2.
Post-discharge trajectories based on mean subdistribution hazards for 30-day readmission, stratified by location of discharge: home, home with home health, long-term acute care/skilled nursing facility (LTAC/SNF), inpatient rehabilitation.
DISCUSSION
This study demonstrates discharge destination following liver transplantation plays an important role in influencing the risk of 30-day readmission. Discharge to inpatient rehabilitation and LTAC/SNF each are associated with decreased odds of 30-day readmission when compared to home or home with home health. For patients discharged to inpatient rehabilitation, the decrease in 30-day readmissions did not correspond with a compensatory increase in the severity of readmission.
The results of our study are consistent with a growing body of literature examining the role of post-acute care on outcomes, including readmission. In the medical literature, inpatient rehabilitation following admission for stroke can reduce readmissions and mortality.(16, 17) Similar findings have been seen in congestive heart failure and myocardial infarction.(18,19) Following major abdominal surgery, discharge home with home health can increase the risk of readmission.(20) Riggs et al. (21) showed discharge to inpatient rehabilitation independently protected against 180 day readmissions following hip repair. These studies establish that discharge location can be an important determinant of outcomes and our data support that.
The role of discharge disposition on readmission following liver transplantation has previously been evaluated – although not as a primary outcome. In these studies, discharge destination is included as a binary covariate in multivariable models, where it takes the value of either home or non-home discharge. Non-home discharges appear to increase the risk of readmission.(7,12) Unlike those studies, we separated non-home discharges into more specific categories to better understand the complex interactions between discharge location and readmission. At our own institution, we observe lower readmission rates in patients discharged to inpatient rehabilitation compared to other non-home discharge locations. The specificity to which we assigned discharge destination (home, home with home health, LTAC/SNF, inpatient rehabilitation) and our treatment of destination as the primary exposure variable may explain why our results are different than prior studies.
In our study, both LTAC/SNF and inpatient rehabilitation discharge decreased the risk of 30-day readmission after controlling for multiple patient factors. For patients discharged to inpatient rehabilitation, this benefit came without a compensatory increase in the severity of illness during a readmission. Unlike patients discharged to LTAC/SNF, home, or home with home health where the risk of readmission was greatest early following discharge, those discharged to inpatient rehabilitation had a peak risk at 16 days. Together, there appears to be a benefit for patients discharged to inpatient rehabilitation both in terms of the rate, timing, and severity of readmission.
These benefits of inpatient rehabilitation on readmission were realized by only a small proportion of patients that underwent liver transplant in our study population (<3%). Although the specific reasons for the low utilization of inpatient rehabilitation cannot be determined from HCUP SID, several explanations include delays in evaluation for admission to inpatient rehabilitation, regulatory concerns, and payment considerations.(22,23,24) Therefore, one potential way to increase the opportunity for patients to go to inpatient rehabilitation following discharge is through reshaping health policy to overcome these barriers – particularly for patients discharged home or home with home health since they had the highest readmission rates in this study. Increasing resource availability, modifying payment structures, and streamlining evaluation processes each are possible starting points.(24)
An important question is how inpatient rehabilitation mitigates the risk for 30-day readmission without increasing readmission severity. While our data cannot answer that question directly, several explanations can be offered based on prior study of hospital readmissions. Broadly, risk factors for 30-day readmission are well-described and include limited access to care, decreased functional status, inadequate social support, and poor health literacy.(25) Following liver transplant, patients can be vulnerable to all of these risk factors.(5,26) We propose that inpatient rehabilitation reduces 30-day readmissions by creating a transitional care environment that mitigates the risk factors for readmission. This likely occurs through around-the-clock interaction with health professionals, close monitoring of medications, easy access to diagnostics, and therapies to combat deconditioning.(27)
An alternative explanation is that the protection provided by inpatient rehabilitation is a reflection of a stronger overall support system for patients discharged to these facilities. Several statistically significant differences were seen when we compared baseline demographic and socioeconomic features to location of discharge, suggesting Caucasian race, older patients, and patients with non-Medicaid insurance were more likely to go to inpatient rehabilitation. These characteristics may create a strengthened post-discharge atmosphere and help decrease readmission. The specific impact of socioeconomic status on readmission following liver transplant warrants further study.
There are limitations of the study that must be weighed when considering the conclusions. The HCUP SID datasets are advantageous for allowing the longitudinal follow-up of patients regardless of primary insurer. For liver transplant, this is especially important given the number of privately insured patients undergoing surgery. Still, the data are based on administrative coding and are subject to the weaknesses described by many authors when used for outcomes research.(28,29) Some examples where administrative data created challenges unique to this study included difficulty with determining the exact cause and condition at readmission, defining the etiology for liver transplant, and the inability to obtain clinical measures necessary for preoperative MELD scores for risk-adjustment.
The strengths of the dataset lie in longitudinal follow-up, accurately assigned discharge locations, and cost data making this type of study feasible. It is important to highlight that cost data presented only capture the readmission encounter, without factoring in the costs associated with obtaining care in institutional discharge locations (i.e. inpatient rehabilitation or LTAC/SNF). Therefore, cost was used to measure the severity of a readmission – not to estimate the overall cost-effectiveness of utilizing these facilities.
Finally, by restricting our follow-up to 30 days we are unable to capture the impact of discharge destination on later readmissions. With increasing attention being placed on measuring patient outcomes beyond the 30-day postoperative period, understanding the factors influencing readmissions beyond 30 days will be an important area of future research.
CONCLUSION
Discharge destination after orthotopic liver transplantation is an important contributor to 30-day readmission rates. Specifically, discharge to inpatient rehabilitation decreases the risk of 30-day readmission without a compensatory increase in readmission severity. With continued focus on readmission as a quality and financial measure, increasing the utilization of inpatient rehabilitation is one possible mechanism to improve readmission rates in this complex patient population.
Supplementary Material
Acknowledgments
Support: This work supported by NIH T32 GM08750-16.
ABBREVIATIONS AND ACRONYMS
- CMS
Centers for Medicare and Medicaid Services
- HRRP
Hospital Readmission Reduction Program
- SNF
skilled nursing facility
- LTAC
long-term acute care
- HCUP SID
Healthcare Cost and Utilization Project State Inpatient Databases
- ICD-9-CM
International Classification of Diseases, Version 9, Clinical Modification
- OR
odds ratio
- AIC
Akaike information criterion
- SHR
subdistribution hazard ratio
- MELD
model for end-stage liver disease
Footnotes
Disclosure Information: Nothing to disclose.
Presented at the Western Surgical Association 123rd Scientific Session, Napa Valley, CA, November 2015.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kastenberg ZJ, Morton JM, Visser BC, et al. Hospital readmission after a pancreaticoduodenectomy: An emerging quality metric? HPB. 2013;15:142–148. doi: 10.1111/j.1477-2574.2012.00563.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fontanarosa PBMR. Revisiting hospital readmissions. JAMA. 2013;309:398–400. doi: 10.1001/jama.2013.42. [DOI] [PubMed] [Google Scholar]
- 3.30-day unplanned readmission and death measures [homepage on the Internet] 2015 Available from: https://www.medicare.gov/hospitalcompare/Data/30-day-measures.html.
- 4.Williams MV. A requirement to reduce readmissions: Take care of the patient, not just the disease. JAMA. 2013;309:394–396. doi: 10.1001/jama.2012.233964. [DOI] [PubMed] [Google Scholar]
- 5.Serper M, Goldberg DS. Liver transplant readmissions: The cost of the revolving door. Liver Transplantation. 2015 doi: 10.1002/lt.24155. [DOI] [PubMed] [Google Scholar]
- 6.Ladner DP, Skaro AI, Abecassis MM. Are all readmissions the same? Liver Transplantation. 2012;18:1007–1008. doi: 10.1002/lt.23517. [DOI] [PubMed] [Google Scholar]
- 7.Wilson GC, Hoehn RS, Ertel A, et al. Variation by center and economic burden of readmissions after liver transplantation. Liver Transplantation. 2015 doi: 10.1002/lt.24112. [DOI] [PubMed] [Google Scholar]
- 8.Yu J, Hosmer A, Parks T, et al. Predictors of early hospitalization after deceased donor liver transplantation. Dig Dis Sci. 2015:1–6. doi: 10.1007/s10620-015-3753-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen P, Wang W, Yan L, et al. Risk factors for first-year hospital readmission after liver transplantation. Eur J Gastroenterol Hepatol. 2015;27:600–606. doi: 10.1097/MEG.0000000000000327. [DOI] [PubMed] [Google Scholar]
- 10.Merkow RP, Ju MH, Chung JW, et al. Underlying reasons associated with hospital readmission following surgery in the united states. JAMA. 2015;313:483–495. doi: 10.1001/jama.2014.18614. [DOI] [PubMed] [Google Scholar]
- 11.Paterno F, Wilson GC, Wima K, et al. Hospital utilization and consequences of readmissions after liver transplantation. Surgery. 2014;156:871–879. doi: 10.1016/j.surg.2014.06.018. [DOI] [PubMed] [Google Scholar]
- 12.Pereira AA, Bhattacharya R, Carithers R, et al. Clinical factors predicting readmission after orthotopic liver transplantation. Liver Transplantation. 2012;18:1037–1045. doi: 10.1002/lt.23475. [DOI] [PubMed] [Google Scholar]
- 13.Healthcare Cost and Utilization Project (HCUP) HCUP Databases. Agency for Healthcare Research and Quality; Rockville, MD: Nov, 2014. [homepage on the Internet]. Available from: www.hcup-us.ahrq.gov/sidoverview.jsp. [PubMed] [Google Scholar]
- 14.HCUP Supplemental Files for Revisit Analyses [homepage on the Internet] 2015 Available from: www.hcup-us.ahrq.gov/toolssoftware/revisit/revisit.jsp.
- 15.Stagg V. CHARLSON: Stata module to calculate Charlson index of comorbidity. Statistical Software Components. 2006 [Google Scholar]
- 16.Bettger JP, Liang L, Xian Y, et al. Inpatient rehabilitation facility care reduces the likelihood of death and rehospitalization after stroke compared with skilled nursing facility care. Stroke. 2015;46:A146. [Google Scholar]
- 17.Ottenbacher KJ, Graham JE, Ottenbacher AJ, et al. Hospital readmission in persons with stroke following postacute inpatient rehabilitation. J Gerontol A Biol Sci Med Sci. 2012;67:875–881. doi: 10.1093/gerona/glr247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vinson JM, Rich MW, Sperry JC, et al. Early readmission of elderly patients with congestive heart failure. J Am Geriatr Soc. 1990;38:1290–1295. doi: 10.1111/j.1532-5415.1990.tb03450.x. [DOI] [PubMed] [Google Scholar]
- 19.Dunlay SM, Pack QR, Thomas RJ, et al. Participation in cardiac rehabilitation, readmissions, and death after acute myocardial infarction. Am J Med. 2014;127:538–546. doi: 10.1016/j.amjmed.2014.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Martin RC, Brown R, Puffer L, et al. Readmission rates after abdominal surgery: The role of surgeon, primary caregiver, home health, and subacute rehab. Ann Surg. 2011;254:591–597. doi: 10.1097/sla.0b013e3182300a38. [DOI] [PubMed] [Google Scholar]
- 21.Riggs RV, Roberts PS, Aronow H, Younan T. Joint replacement and hip fracture readmission rates: Impact of discharge destination. PM&R. 2010;2:806–810. doi: 10.1016/j.pmrj.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 22.New PW, Andrianopoulos N, Cameron P, et al. Reducing the length of stay for acute hospital patients needing admission into inpatient rehabilitation: A multicentre study of process barriers. Intern Med J. 2013;43:1005–1011. doi: 10.1111/imj.12227. [DOI] [PubMed] [Google Scholar]
- 23.Shay PD, Ozcan YA. Freestanding inpatient rehabilitation facility performance following the 60 percent rule: A matter of fit. Med Care Res Rev. 2013;70:46–67. doi: 10.1177/1077558712453206. [DOI] [PubMed] [Google Scholar]
- 24.Granger CV, Carlin M, Diaz P, et al. Medical necessity: Is current documentation practice and payment denial limiting access to inpatient rehabilitation? Am J Phys Med Rehabil. 2009;88:755–765. doi: 10.1097/PHM.0b013e3181aa71a8. [DOI] [PubMed] [Google Scholar]
- 25.Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: A systematic review. JAMA. 2011;306:1688–1698. doi: 10.1001/jama.2011.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McAdams-DeMarco M, Grams M, et al. Early hospital readmission after kidney transplantation: Patient and Center-Level associations. Am J Transplantation. 2012;12:3283–3288. doi: 10.1111/j.1600-6143.2012.04285.x. [DOI] [PubMed] [Google Scholar]
- 27.Patcai JT, Disotto-Monastero MP, Gomez M, Adcock LE. Inpatient rehabilitation outcomes in solid organ transplantation: Results of a unique partnership between the rehabilitation hospital and the multi-organ transplant unit in an acute hospital. Open J Therapy Rehabilitation. 2013;2013 [Google Scholar]
- 28.Grimes DA. Epidemiologic research with administrative databases: Red herrings, false alarms and pseudo-epidemics. Hum Reprod. 2015;30:1749–1752. doi: 10.1093/humrep/dev151. [DOI] [PubMed] [Google Scholar]
- 29.Sarrazin MSV, Rosenthal GE. Finding pure and simple truths with administrative data. JAMA. 2012;307:1433–1435. doi: 10.1001/jama.2012.404. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.