Abstract
Objectives:
The role of dental professionals in screening for oral cancer has been limited. The purpose of this study was to investigate and compare the educational priorities of oral medicine specialists, general dental practitioners, and doctors of dental surgery with regards to the diagnosis and management of oral cancers and potential malignant disorders.
Study Design:
This was a longitudinal survey.
Materials and Methods:
A Delphi survey was directed to a panel of 25 oral medicine specialists asking them to identify the major difficulties in diagnosing and managing patients with oral cancer or suspected malignancy. In a second phase, two groups of generalists were asked to express their ratings on the issues identified by experts.
Results:
The response rate of the experts to the survey was 84%, while only 44% of the generalists participated. Although the three groups agreed on most of the issues, there were significant differences of opinions on 10 of the items proposed by specialists (P < 0.05 from the Kruskal–Wallis test), which were observed mainly between experts and general dental practitioners (P < 0.017 from the Mann–Whitney U test). The opinion of the participants about future investments in the field of education resulted in similar results (P > 0.05 from the Chi-square test), with the specialists ranking highest on mandatory annual thematic courses, while the generalists prioritizing more interactive and extensive pre-graduation courses on oral cancer detection.
Conclusion:
This study confirms a clear need to improve the educational foundation on oral cancer by a didactic process starting with pre-graduation courses that should involve National Health Care Services, National Dental Associations, and academia.
Keywords: Delphi survey, dental education, oral cancer, potential malignant disorders screening, prevention
INTRODUCTION
Oral squamous cell carcinoma (OSCC) is a worldwide problem with increasing incidence and mortality rates affecting approximately 700000 people globally, and is within the first 10 most common cancers reported globally. Despite the diagnostic and therapeutic progresses, survival rates remain low except in few highly resourced cancer centers.[1,2] Epidemiological data reported above have considerable impact on the economy of the public healthcare system, particularly due to a large number of cases presenting at late stages (III/IV) for cancer treatment.[3,4]
To date, the best management approach for this disease is early diagnosis, which ensures improved prognosis and has much less burden on the healthcare system. For these reasons, education and training play a pivotal role in enabling physicians in early diagnosis of OSCC; it is essential to examine the process of educational practice, to realize if teachers are providing what the learners really need, and if learners are getting the right messages from the current teaching practices.
The purpose of this study was to survey the views of oral medicine leading experts in Italy using the Delphi methodology, asking them to identify any difficulties that exist in the clinical diagnostic approach to patients presenting with OSCC or suspected of malignancies and any lack of education among general dental practitioners (GDPs) and oral surgery specialists (DDSs) which contributes to the late diagnosis of OSCC.
Subsequently, the same questionnaire was submitted to GDPs and DDSs in primary care to identify any significant differences between the three groups. We explored what is perceived by oral medicine experts and the particular items that reflect the real difficulties for GDPs and DDSs (if different from the experts) to determine the real needs throughout their field of training and education.
MATERIALS AND METHODS
The study was developed in two phases [Figure 1]. In the first phase, a Delphi survey developed in four rounds was directed to a panel of experts who aimed to identify and prioritize the items related to OSCC diagnosis, management, and education issues. In the second phase, based on the responses of experts, we composed the survey and addressed similar questions to DDSs and GDPs. The results obtained from the three surveys were then statistically compared. The survey was approved by Institutional Review Board, Ethical Commitee, Federico II University of Naples (ID: 134/14).
Figure 1.
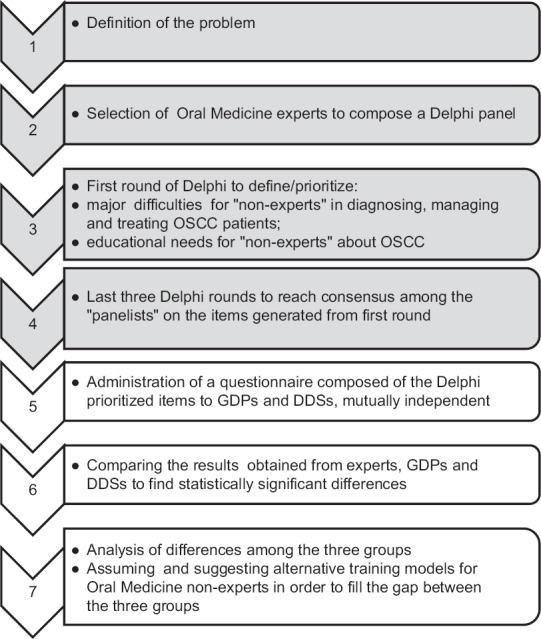
A schematic description of the project plan
Phase 1
A sample of 25 Italian specialists in oral medicine was selected.[5,6,7,8,9,10] The experts were full and associate professors and researchers with experience in the field of oral medicine. The level of experience was evaluated considering the number of scientific publications and years of clinical activity (at least 10 years).[7] The participants were approached by e-mail with a letter of invitation.
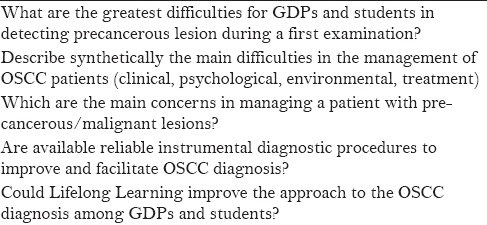
The questionnaire
The survey software was freely downloaded from a website (http://armstrong.wharton.upenn.edu/delphi2). The first round, was composed of 5 open-ended questions each of approximately 20–25 words [Table 1].[9,10,11,12,13] The experts were asked to respond by giving a maximum of 5 suggestions for each question. From the second round, the experts were asked to grade their agreement about the items derived from the first round on a 6-point Likert scale (0 = strongly disagree, 5 = strongly agree). A “don’t know” option was also available. An even-point Likert scale, without a neutral, was chosen because we wanted to force the experts to side, which is necessary to generate priority criteria in educational planning.
Table 1.
Delphi first round items
In the second round, we circulated two versions of the survey, one form with the questions arranged in the reverse order to determine if fatigue affected reliability of the survey. Both forms were analyzed using the Pearson's correlation coefficient. The alternate form reliability was estimated at 0.91, and thus results of only one form of the survey were used for the second round. The reliability of the survey was also evaluated by measuring the internal consistency through the Cronbach's Alpha, which was found to be 0.95.
To obtain a higher response rate, weekly email reminders were sent. To establish if consensus was reached, we set the following criteria:
median ≥ 3.5 or ≤ 1.5;
Interquartile range (IQR) ≤1;
80% of answer with a median ≥ 3 or ≤ 2.
For each item, at least 2 of the 3 criteria were expected to be fulfilled. As the responses to the questionnaire were expressed with ordinal data, descriptive statistics were considered more appropriate than mean and standard deviation.
At the end of the 4 rounds, the items without consensus were considered less influential on diagnostics and management difficulties of an OSCC patient and, consequently, were not circulated to GDPs and DDSs in Phase II.
Phase 2
We administered an anonymous questionnaire composed of the items prioritized by the Delphi panelists to GDPs and DDSs. The two groups were composed of 50 DDSs and 50 GDPs, randomly chosen among those graduated from 2000 to date. A database of all graduates was available for our use. The items from Phase I were replicated unchanged, excluding items that did not reach consensus. The participants were asked to respond on the same rating scale but were allowed to respond only once. At the end of Phase II, we asked the three groups to rank how they would recommend institutions to invest future funds in the field of education and training.
Statistical analysis
Statistical analysis encompassed the Kruskal–Wallis test for nonparametric data to globally compare globally the three groups, the Mann-Whitney U test for the pair-wise comparisons and the Chi-square test to compare rankings. Data being heteroskedastic, we performed a bootstrap by the Monte Carlo method.[14,15] A dedicated software was used (Statistical Package for the Social Sciences version 19, IBM inc, USA). The level of significance was set at 0.05 and 0.017 in case of Bonferroni post-hoc correction.
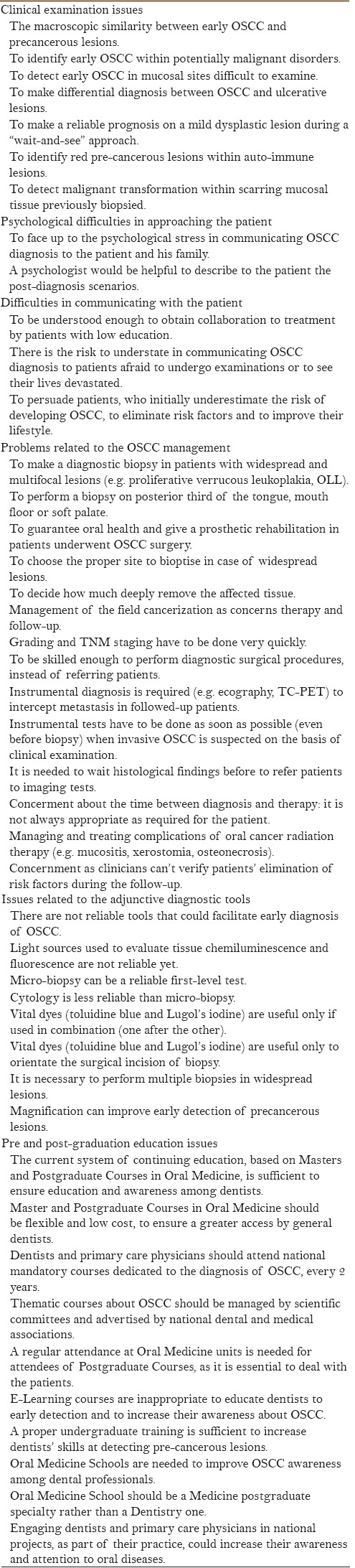
RESULTS
The study was completed in 7 months. The experts’ response rate for the Delphi first round was 84% (21/25 participants), with a dropout of 10% and 5% for the second and the third rounds, respectively. From the first round, 193 comments were received, of which those found to be similar (n = 149) in their meaning were excluded. After categorization and selection of common themes, 44 items were generated and proposed to the experts for the following rounds [Table 2]. Six main themes were identified as follows: (1) clinical examination issues, (2) psychological difficulties in approaching the patient, (3) difficulties in communicating with the patient, (4) problems related to the clinical management, (5) adjunctive diagnostic tools, and (6) pre and post-graduation educational issues. At the end of Phase I, consensus was reached on 33/44 (75%) of the proposed items. Most of the 11 items on which experts did not agree were related to the clinical management of cancer or potential malignant disorders (e.g., biopsy issues, post-radiation complications); experts considered that such issues were not directly related to the generalists’ clinical problems and educational needs. consequently, these items were not included in the questionnaire.
Table 2.
Delphi items grouped by theme
In Phase II, the response rate to the questionnaire was 44% (22/50 participants) for both of the 50 GDPs and 50 DDSs. At the end of the survey, the data from the three questionnaires were collected and analyzed [Tables 3–5].
Table 3.
Kruska-Wallis analysis results
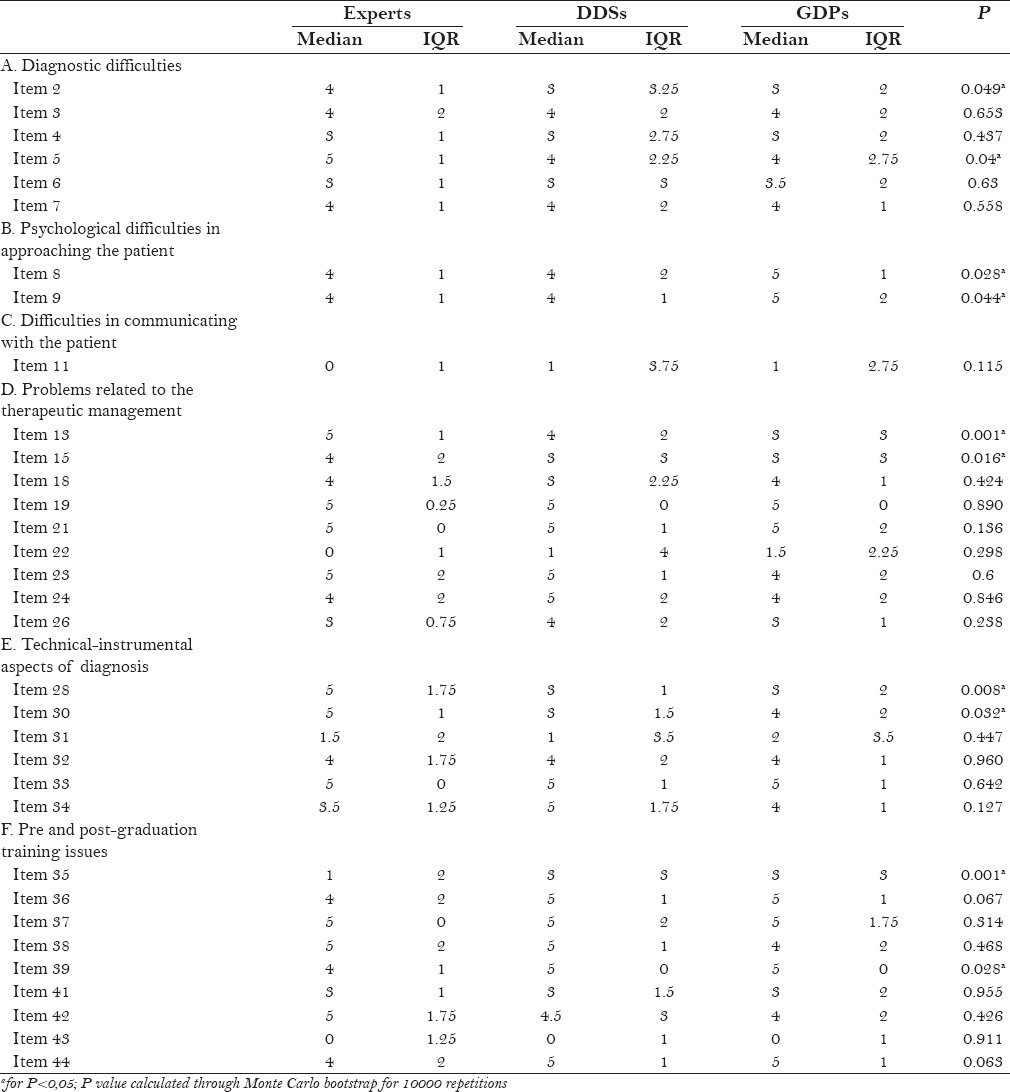
Table 5.
How would you invest future funds to improve early diagnosis of OSCC?
The three groups rated similarly (P > 0.05) for most of the items of the questionnaire (23/33), thus sharing the same views about clinical and educational needs on oral cancer detection [Table 3]. By the Kruskal–Wallis test, for 10 of the 33 items, statistically significant differences among median scores were detected. Subsequently, such items were further investigated comparing in a pair-wise manner for the three groups, using the Mann–Whitney U test; differences were found mainly comparing experts to GDPs, while views of experts and DDS were not significantly different [Table 4]. Experts’ and nonexperts’ opinions about how they would invest future funds in the field of education and training were further confirmed in the last question of the survey. Using the Chi-square test, the three groups gave similar priority to the available options (P > 0.05), with the specialists ranking highest on mandatory annual thematic courses, and the generalists prioritizing more interactive and extensive pre-graduation courses [Table 5].
Table 4.
Pairwise comparisons between Experts, DDSs, GDPs by Mann-Whitney U test
DISCUSSION
Much of today's dental education is based upon traditional didactic approaches, which are ineffective for the learning needs of GDPs or DDSs. This project was initiated considering the need for change, and hence improve dentists’ knowledge about disorders managed by oral medicine experts and approaches to it, investigating the reasons that lie beyond the difficulties of early diagnosis of OSCC both in primary and secondary care. Numerous efforts in this direction have been made in recent years, however, the methodologies adopted have not been driven by recognized technology.[16,17,18,19] Using the Delphi method, it is possible to achieve this goal, encouraging opinion exchanges and sharing the responsibility of resolving certain issues.[20,21]
The major issue to be discussed is the early diagnosis, based on a widespread awareness of the signs and symptoms of the disease among the medical and dental professionals, on the acquisition of a clinical attitude that brings all the professionals to inspect oral mucosa systematically. The dentists’ role is crucial for opportunistic screening because people undergo a dental examination at least once in their life and regular attendees do so at least twice a year.
As it concerns the present study, the high response rate to the Delphi survey (84%) in Phase I has been possible thanks to the “face-to-face” motivation to participate to the study, as well as the weekly reminders.[11,22] Among experts’ opinions, education and training on OSCC are very salient and debated issues, and one of the first targets to be achieved in the medical and dental undergraduate classes.
The low response rate of the nonexperts’ questionnaires (44%) in Phase II is hard to understand, considering the participants were personally motivated to attend the survey, and one of the aims of the study was also to improve the training models of the pre- and postgraduate courses in which they are directly involved. It is likely that professionals took into account that replying to the questionnaire was too “time-consuming.” Dental school educational programs in Italy provide specific training modules on the primary and secondary prevention of OSCC, including anamnesis and examination of the oral mucosa, however, very often we are faced with dental graduates unprepared to make a proper “first examination,” in approaching the patient and intercepting early oral precancerous lesions. This leads, on one hand, to question the traditional teaching methods in oral medicine and, on the other hand, reflects the “negligence” usually shown by professionals during patient examination. National annual mandatory free-cost courses in postgraduate training of oral medicine and pathology are strongly recommended and the Ministry of Education, Universities and Research should encourage this essential issue in the “lifelong learning programs,” improving practice through recommendations on scientific review.
From the Kruskal–Wallis test results [Table 3] it is evident that, for 10 out of 33 (30%) items, there is a statistically significant difference (P < 0.05) among the three groups. On the basis of the Mann–Whitney U test [Table 4], the differences (P < 0.017 after Bonferroni correction) are observed mainly comparing experts to GDPs.[23] At the same time, it is comforting to note that, for 70% of the items, the three groups appear to share the same views on the majority of the issues related to the management, approach, diagnosis, and education on OSCC. This is encouraging when planning future education strategies.
Experts and nonexperts give different priority to certain aspects of the diagnostic, therapeutic, and psychological approach to the patient with OSCC.
Among the diagnostic difficulties, GDPs, while differing with the other two groups, believe to a lesser extent that recognizing a frank carcinoma from a potentially malignant lesion is a relevant issue (item 2). Similarly, both groups of nonexperts are less concerned than experts about a wait-and-see approach of mild dysplastic lesions (item 5); this is likely linked to the fact that nonexperts usually refer patients with potentially malignant disorders to specialists rather than follow-up them directly. The same could be said about biopsy management in case of widespread/multifocal lesions; GDPs, compared to DDSs and experts, who usually perform biopsies in their clinical practice and are well-conversed with biopsy techniques, do not give considerable relevance to this issue (item 13).
Another interesting observation is that both the groups of nonexperts reveal having emotional difficulties in the verbal communication with patients diagnosed with OSCC. The three groups agree on the need for support from a behavioral psychologist when they communicate with patients, and this is particularly true for nonexperts, who are less prepared to manage the fragility, anxiety, and fear of patients with OSCC (item 8–9).
On the contrary, GDPs and DDSs are not so concerned about the prosthetic rehabilitation of their patients who have undergone OSCC surgery (item 15).
In regards to the item 28, experts believe that adjunctive diagnostic tools such as optical instruments, which evaluate tissue fluorescence and chemiluminescence, are useful only to confirm the presence of an oral mucosal disorder, but are completely unable to discriminate high/low risk lesions.[24,25,26] In contrast nonexperts consider the same tools to be a valid help. This opens ample food for thought because often such devices, marketed by commercial companies as infallible methods, up to date do not have enough scientific support, validating their sensitivity and specificity on a large case-series in primary care. Furthermore, experts appear significantly distant from oral surgeons in regards to the reliability of cytology compared to microbiopsy (item 30), considering it unreliable. More efforts should be made to educate nonexperts to the rational use of adjunctive diagnostic tools because histopathology is the only means to diagnosis. There is a difference between experts’ and nonexperts’ sense of possessing the necessary skills and employing them in daily practice. Nonexperts recognized this lack of knowledge and expressed their willingness to improve these skills by further training.
It is imperative that nonexperts be able to apply simple algorithms in the management of patients to practice a biopsy, if deemed appropriate, and to refer to more complex cases to the special centers. Biopsy is technically easy to perform as a surgical technique, however, it requires much experience to know when, how, and where do it correctly; therefore, it is challenging to a practitioner with limited skills or working single-handed in their practices.
For what concerns the education, the experts believe that the current system of postgraduate training is insufficient to ensure adequate preparation; highlighting the need for suggesting mandatory annual courses (item 35). GDPs, instead, clearly express their will to attend more actively oral medicine units (item 39). As confirmed by Broomfield et al., nonexperts ascribe their difficulty to manage patients affected by potential malignant disorders and/or OSCC to the need of clinical training and of a more interactive way of learning rather than to own cultural problems.[27,28]
More practical sessions are needed giving the learners the possibility to develop skills in clinical reasoning, either talking directly with patients or through problem-based learning (PBL) in working groups. For this purpose, we ended the study by asking the three groups to rank how they would recommend to invest future funds in the field of education and training [Table 5]. The Chi-square test results clearly shows (P > 0.05) that participants would invest funds in undergraduate courses involving more activity by the trainees (e.g., PBL) in a higher attendance at oral medicine units, as well as for attending national/regional mandatory annual thematic meetings. Postgraduation courses and masters were chosen with a lower frequency maybe because, being optional, they have no wide spread acceptance among dental professionals. In addition, only experts have given priority to the development of a residency in oral medicine, which would create a larger number of reference centers on the territory but would not directly improve screening skills programs for GDPs on a large scale.
Targeted policies and strategies should be promoted by competent organizations, such as the NHS and the national dental associations, in order to make people aware of the possibility that no one is immune to mouth cancer.
This survey has some limitations. The first is related to the small number of respondents among the groups of nonexperts, and hence, the results may not reflect the average population but only that of the individuals most interested in the project. The second is tied to the fact that the experts, unlike nonexperts, have had the opportunity to evaluate the items of the questionnaire in subsequent rounds, which may have generated distortions at the time of the comparison between the groups. It is worth noting that, if the Delphi method is applied to nonexperts, agreement is the result of conformity to the general average, more than a constructive exchange of views on the basis of feedback received from other participants.[29] Finally, it would have been interesting to explore the opinions of patients diagnosed with OSCC, which are pivotal to understand the phenomenon of “diagnostic delays” and to understand healthcare priorities of who is going to receive the care, but this was not the purpose of the present study.[30,31]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors wish to thank the following colleagues who kindly accepted to help us starting this survey: Dr. Abati Silvio, Dr. Biasotto Matteo, Dr. Campisi Giuseppina, Dr. Carbone Mario, Dr. Carrassi Antonio, Dr. Colella Giuseppe, Dr. Di Lenarda Roberto, Dr. Favia Gianfranco, Dr. Ficarra Giuseppe, Dr. Gandolfo Sergio, Dr. Giuliani Michele, Dr. Lajolo Carlo, Dr. Lo Muzio Lorenzo, Dr. Lo Russo Lucio, Dr. Lodi Giovanni, Dr. Majorana Alessandra, Dr. Manfredi Maddalena, Dr. Meleti Marco, Dr. Montebugnoli Lucio, Dr. Pentenero Monica, Dr. Sardella Andrea, Dr. Spadari Francesco, and Dr. Vescovi Paolo.
REFERENCES
- 1.Warnakulasuriya S. Living with oral cancer epidemiology with particular reference to prevalence and life-style changes that influience survival. Oral Oncol. 2010;46:407–10. doi: 10.1016/j.oraloncology.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 2.Monteiro LS, Antunes L, Bento MJ, Warnakulasuriya S. Incidence rates and trends of lip, oral and oro-pharyngeal cancers in Portugal. J Oral Pathol Med. 2013;42:345–51. doi: 10.1111/jop.12010. [DOI] [PubMed] [Google Scholar]
- 3.Güneri P, Epstein JB. Late stage diagnosis of oral cancer: Components and possible solutions. Oral Oncol. 2014;50:1131–6. doi: 10.1016/j.oraloncology.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 4.Van Agthoven M, Van Ineveld BM, De Boer MF, Leemans CR, Knegt PP, Snow GB, et al. The costs of head and neck oncology: Primary tumors, recurrent tumours and long-term follow-up. Eur J Cancer. 2001;37:2204–11. doi: 10.1016/s0959-8049(01)00292-1. [DOI] [PubMed] [Google Scholar]
- 5.Hasson F, Keeney S, Mckenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32:1008–15. [PubMed] [Google Scholar]
- 6.McMillan SS, King M, Tully MP. How to use the nominal group and Delphi techniques. Int J Clin Pharm. 2016;38:655–62. doi: 10.1007/s11096-016-0257-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baker J, Lovell K, Harris N. How expert are the experts? An exploration of the concept of ‘expert’ within Delphi panel techniques. Nurse Res. 2006;14:59–70. doi: 10.7748/nr2006.10.14.1.59.c6010. [DOI] [PubMed] [Google Scholar]
- 8.Diamond IR, Grant RC, Feldman BM, Pencharz PB, Ling SC, Moore AM, et al. Defining consensus: A systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol. 2014;67:401–9. doi: 10.1016/j.jclinepi.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 9.Cramer CK, Klasser GD, Epstein JB, Sheps SB. The Delphi process in dental research. J Evid Based Dent Pract. 2008;8:211–20. doi: 10.1016/j.jebdp.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 10.Mullen P. Delphi: Myths and reality. J Health Organ Manag. 2003;17:37–52. doi: 10.1108/14777260310469319. [DOI] [PubMed] [Google Scholar]
- 11.Keeney S, Hasson F, McKenna H. Consulting the oracle: Ten lessons from using the 12. Delphi technique in nursing research. J Adv Nurs. 2006;53:205–12. doi: 10.1111/j.1365-2648.2006.03716.x. [DOI] [PubMed] [Google Scholar]
- 12.Keeney S, Hasson F, McKenna HP. A critical review of the Delphi technique as a research methodology for nursing. Int J Nurs Stud. 2001;38:195–200. doi: 10.1016/s0020-7489(00)00044-4. [DOI] [PubMed] [Google Scholar]
- 13.Salancik JR, Wenger W, Helfer E. The construction of Delphi event statements. Technol Forecast Soc Change. 1971;3:65–73. [Google Scholar]
- 14.Ruxton GD, Beauchamp G. Some suggestions about appropriate use of the Kruskal–Wallis test. Animal Behav. 2008;76:1083–7. [Google Scholar]
- 15.Reiczigel J, Land Z, Rozsa L, Tothmerez B. Measures of sociality: Two different views of group size. Animal Behav. 2008;75:715–21. [Google Scholar]
- 16.Carter LM, Ogden GR. Oral cancer awareness of undergraduate medical and dental students. BMC Med Educ. 2007;7:44. doi: 10.1186/1472-6920-7-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rahman B, Hawas N, Rahman MM, Rabah AF, Al Kawas S. Assessing dental students’ knowledge of oral cancer in the United Arab Emirates. Int Dent J. 2013;63:80–4. doi: 10.1111/idj.12017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Colella G, Gaeta GM, Moscariello A, Angelillo IF. Oral cancer and dentists: Knowledge, attitudes, and practices in Italy. Oral Oncol. 2008;44:393–9. doi: 10.1016/j.oraloncology.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 19.Horowitz AM, Drury TF, Canto MT. Practices of Maryland dentist: Oral cancer prevention and early detection-baseline data from 1995. Oral Dis. 2000;6:282–8. doi: 10.1111/j.1601-0825.2000.tb00140.x. [DOI] [PubMed] [Google Scholar]
- 20.Turoff M, Linstone HA. The Delphi method techniques and applications. Reading, MA: Addison-Wesley; 1975. [Google Scholar]
- 21.Kerstin Cuhls. Kerstin Cuhls. Delphi method. 2003. Available from: http://www.unido.org/fileadmin/import/16959_DelphiMethod.pdf .
- 22.McKenna HP. The Delphi technique: A worthwhile approach for nursing? J Adv Nurs. 1994;19:1221–5. doi: 10.1111/j.1365-2648.1994.tb01207.x. [DOI] [PubMed] [Google Scholar]
- 23.Swinscow TD, Campbell MJ. Statistics at Square One. 10th Ed. London: BMJ Books; 2002. p. 168. [Google Scholar]
- 24.Awan KH, Morgan PR, Warnakulasuriya S. Evaluation of an autofluorescence based imaging system (VELscope) in the detection of oral potentially malignant disorders and benign keratoses. Oral Oncol. 2011;47:274–7. doi: 10.1016/j.oraloncology.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 25.Awan KH, Morgan PR, Warnakulasuriya S. Utility of chemiluminescence (ViziLite™) in the detection of oral potentially malignant disorders and benign keratosis. J Oral Pathol Med. 2011;40:541–4. doi: 10.1111/j.1600-0714.2011.01048.x. [DOI] [PubMed] [Google Scholar]
- 26.Rashid A, Warnakulasuriya S. The use of light-based (optical) detection systems as adjuncts in the detection of oral cancer and oral potentially malignant disorders: A systematic review. J Oral Pathol Med. 2015;44:307–28. doi: 10.1111/jop.12218. [DOI] [PubMed] [Google Scholar]
- 27.Broomfield D, Humphris GM. Using the Delphi technique to identify the cancer education requirements of general practitioners. Med Educ. 2001;35:928–37. [PubMed] [Google Scholar]
- 28.Welch DR, Antalis TM, Burnstein K, Vona-Davis L, Jensen RA, Nakshatri H, et al. Essential Components of Cancer Education. Cancer Res. 2015;75:5202–5. doi: 10.1158/0008-5472.CAN-15-2077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Greatorex J, Dexter T. An accessible analytical approach for investigating what happens between the rounds of a Delphi study. J Adv Nurs. 2000;32:1016–24. [PubMed] [Google Scholar]
- 30.Efstathiou N, Coll AM, Ameen J, Daly W. Do Greek healthcare users and healthcare providers share cancer care priorities? Analysing the results from two Delphi studies. Eur J Cancer Care. 2011;20:179–86. doi: 10.1111/j.1365-2354.2009.01176.x. [DOI] [PubMed] [Google Scholar]
- 31.Grant L, Silver K, Bauld L, Warnakulasuriya S. The experiences of young oral cancer patients in Scotland; Symptom recognition and delays in seeking professional help. Br Dent Journal. 2010;208:465–71. doi: 10.1038/sj.bdj.2010.450. [DOI] [PubMed] [Google Scholar]


