Abstract
Background: Perinatal intimate partner violence (IPV) is common and has significant negative health outcomes for mothers and infants. This study evaluated the effectiveness of an IPV intervention in reducing violence among abused women in perinatal home visiting programs.
Materials and Methods: This assessor-blinded multisite randomized control trial of 239 women experiencing perinatal IPV was conducted from 2006 to 2012 in U.S. urban and rural settings. The Domestic Violence Enhanced Home Visitation Program (DOVE) intervention group (n = 124) received a structured abuse assessment and six home visitor-delivered empowerment sessions integrated into home visits. All participants were screened for IPV and referred appropriately. IPV was measured by the Conflicts Tactics Scale2 at baseline through 24 months postpartum.
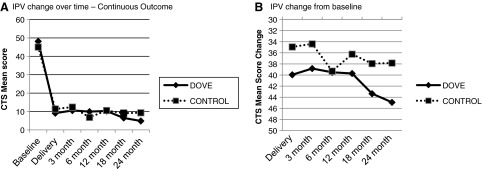
Results: There was a significant decrease in IPV over time (F = 114.23; p < 0.001) from baseline to 1, 3, 6, 12, 18, and 24 months postpartum (all p < 0.001). Additional models examining change in IPV from baseline indicated a significant treatment effect (F = 6.45; p < 0.01). Women in the DOVE treatment group reported a larger mean decrease in IPV scores from baseline compared to women in the usual care group (mean decline 40.82 vs. 35.87). All models accounted for age and maternal depression as covariates.
Conclusions: The DOVE intervention was effective in decreasing IPV and is brief, thereby facilitating its incorporation within well-woman and well-child care visits, as well as home visiting programs, while satisfying recommendations set forth in the Affordable Care Act for IPV screening and brief counseling.
Keywords: : intimate partner violence, perinatal health, home visiting, evidenced-based intervention, rural, urban
Introduction
Perinatal intimate partner violence (IPV), defined here as IPV occurring in the year before, during, or the year after birth,1 is a pervasive public health problem with prevalence estimates between 1% and 28% globally.2,3 The U.S. 2000–2003 PRAMS data demonstrated a prevalence of IPV during pregnancy of 3.9%. However, there are well-established risk factors associated with a higher prevalence of perinatal IPV, including young age, single relationship status, and poverty.4–6 Indeed, studies conducted among samples of low-income predominantly single women have noted that up to 30% of women experienced IPV during the perinatal period.7–9
IPV during pregnancy confers considerable risk to the physical and mental health of women,4,10,11 including an increased risk of homicide and suicide.12,13 The impact of IPV also extends to the health of abused women's children, including adverse neonatal outcomes (e.g., low birth weight, small for gestational age, preterm birth).8,14–16
Yet, there are few evidence-based interventions for women experiencing IPV.17 Passage of the Affordable Health Care Act (ACA) of 2010,18 with subsequent creation of the Maternal, Infant, and Early Childhood Home Visiting program (MIECHV), marks an unprecedented fiscal commitment to improving health outcomes for at-risk families. A key benchmark is the reduction of violence. To realize this benchmark, it is essential that home visitors are equipped with the knowledge, skills, and evidence-based interventions to best serve these families.
The objective of this study was to determine the effectiveness of the Domestic Violence Enhanced Home Visitation Program (DOVE) IPV intervention in reducing violence for women experiencing current violence or violence in the year before pregnancy, using community health nurse prenatal/postpartum home visitation by random assignment to the DOVE intervention or usual IPV care.
The conceptual model guiding the DOVE intervention used Dutton's empowerment model19 as the basis for the educational intervention delivered by home visitors. The empowerment model believes that violence against women is one facet of a syndrome of coercive control by the abuser; therefore, the empowerment intervention seeks to increase the woman's independence and control. This article presents findings for the primary trial outcome, which was to decrease reported perinatal IPV.
Materials and Methods
The DOVE was a multisite trial conducted from 2006 to 2012. Participant recruitment occurred between January 2007 and December 2011. Data analyses were conducted during 2012–2014. Approval was obtained by the institutional review board of participating academic institutions and all other participating agencies. A Certificate of Confidentiality was obtained from the National Institutes of Health.
Setting and study participants
Women were recruited from several different models of prenatal home visiting programs. The goal of the study was to test whether integrating a structured IPV intervention, DOVE, into a home visiting program, regardless of model, would increase the safety in perinatal women experiencing violence. All home visiting programs have an essential component of community health nursing practice to improve health outcomes for families (parents or children), but screening and intervening with women experiencing violence have not historically been integrated into the different models.
All home visiting programs target low-income, high-risk mothers such as single young mothers or families with low birth weight or preterm infants who are presumed to be at highest risk for poor physical and behavioral child outcomes. Visitation usually occurs prenatally through the first 2 years of the child's life.20
All women received the usual care (UC) of the home visiting program, which on an average included 4–6 visits prenatally and 6–12 visits up to 2 years postpartum. One urban health department on the East Coast and 13 home visiting agencies located in rural areas in the Midwest were used for recruitment and were equivalent in characteristics (Table 1). The rationale for including both populations was to determine if the DOVE intervention would be feasible and effective in both settings using home visiting programs.
Table 1.
Home Visiting Program Characteristics
| Site | Home visiting program | Number of home visitors | Educational level of home visitors | No. of women participating |
|---|---|---|---|---|
| Rural site A/Usual care | Promising program | 2 | Licensed personnel | 28 |
| Rural site B/Usual care | Promising program | 6 | Unlicensed personnel | 16 |
| Rural site C/Usual care | Promising program | 8 | Licensed and unlicensed personnel | 10 |
| Rural site D/Usual care | Promising program | 7 | Licensed and unlicensed personnel | 10 |
| Rural site E/Usual care | Promising program | 2 | Licensed and unlicensed personnel | 1 |
| Rural site F/Usual care | Promising program | 3 | Licensed and unlicensed personnel | 4 |
| Rural site G/DOVE | Promising program | 8 | Licensed and unlicensed personnel | 34 |
| Rural site H/DOVEa | Promising program | 3 | Unlicensed personnel | 0 |
| Rural site I/DOVE | Promising program | 2 | Unlicensed personnel | 0 |
| Rural site J/DOVE | Promising program | 9 | Licensed and unlicensed personnel | 14 |
| Rural site K/DOVE Phelps | Promising program | 4 | Licensed and unlicensed personnel | 5 |
| Rural site L/DOVE Moberly | Promising program | 5 | Unlicensed personnel | 7 |
| Rural site M/DOVE Cape | Evidenced based | 4 | Licensed personnel | 18 |
| Urban site | Promising program | 10 | Licensed personnel | 92 (45 DOVE; 47 Control) |
Site lost their state contract right after study began.
DOVE, Domestic Violence Enhanced Home Visitation Program.
English-speaking pregnant women aged 14 years or older, low income (i.e., Medicaid eligible), less than 32 weeks gestation, experiencing perinatal IPV by a current or past partner, and enrolled in a perinatal home visiting program of a participating agency were eligible for study participation. Perinatal home visiting programs generally recruited families based on their home visitors' case load and usually followed infants through 12 months of age. The Abuse Assessment Scale (AAS)21 and the Women's Experience in Battering (WEB) scale22 were used by the research team to screen all women for perinatal IPV (physical, sexual, and/or severe psychological abuse). Both screening instruments are widely used and psychometrically sound.23 Women who screened positive for perinatal IPV on either instrument were eligible to participate.
Sample size
The sample size was determined a priori using existing published intervention research on violence against pregnant women available at the time of study design24 demonstrating moderate effect sizes (r = 0.50) for changes in violence after 12 and 18 months, respectively. A priori power calculations demonstrated ample power (≥0.80) with 40 participants per intervention and 40 for UC from each site (N = 160). These power calculations included a design effect calculation25 to anticipate mixed-effects modeling with random effects to account for the nested design and baseline covariates. Thus, our final sample of 239 participants possessed sufficient power to detect potential hypothesized effects and allowed for attrition.
Randomization and blinding
Randomization procedures varied by site. At the urban health department site, participants were randomized using computer-generated number assignments in blocks. Eligible participants were enrolled by the study's research nurses and assigned to DOVE versus UC according to the next random number assignment. In the rural sites, there were 13 rural health agencies that participated. Cluster randomization was used to assign seven health agencies to deliver the DOVE intervention and six health agencies were designated as UC. Cluster randomization was necessary in the rural sites because each health agency was small enough that intervention drift was a plausible threat if women were the unit of randomization. The data managers, database development team, and statistical analysis team members were blinded to group assignment.
Intervention
DOVE is a structured brochure-based IPV empowerment intervention based on the March of Dimes Protocol for Prevention of Battering during pregnancy and adaptations successfully used in other research studies. DOVE was developed to be integrated within home visiting programs.21,26 The DOVE intervention was delivered six times within regularly scheduled home visits, three sessions occurring during pregnancy and three during the postpartum period. DOVE sessions began after baseline data collection. Each session lasted ∼15–25 minutes and was integrated into the participating agency's routine home visits.
Home visitors delivering the DOVE intervention ranged from baccalaureate prepared nurses to community health workers supervised by nurses. Each intervention session included the home visitor reviewing the DOVE brochure that contained information addressing the cycle of violence, the Danger Assessment27 that assessed risk factors of homicide, choices available to the woman, safety planning information tailored to the context and level of danger, and IPV resources specific to each community, as well as national hotline information.28 The DOVE intervention focused on providing information and emphasized available options to each woman who supported her autonomy in decision-making.
While the intervention was brochure based and structured, it was not prescriptive; rather, home visitors discussed each woman's individual experiences and tailored the intervention to her expressed needs and level of danger at each visit. This process of intervention delivery empowered the women, enabling them to share their stories and make choices or decisions based upon their own priorities,19,28 using a brochure allowed for consistency of the intervention between sites and home visitors.
Women randomized to UC received the standard home visiting protocol for assessment and referral for perinatal IPV during the first home visit. During subsequent scheduled visits, the UC protocol included a discussion of perinatal IPV only if there was an indication of it occurring or if a woman raised a concern about it.
Intervention training
Study protocols were implemented following training sessions for home visitors in all participating agencies; these sessions were led by the co-Principal Investigators. The first 4-hour training session was for all home visitors and included information about IPV, perinatal IPV and health outcomes, and the importance of screening and intervening in perinatal IPV. The second 4-hour training session was for home visitors who implemented the DOVE intervention and study protocol. The second session reviewed information specific to the research protocol, including the use of the screening and assessment instruments, delivering the brochure-based DOVE intervention, developing individualized safety plans for each study participant, and appropriate documentation of the DOVE intervention, as well as other pertinent information about the visit.
In addition, through the use of role playing, all home visitors who implemented the DOVE intervention as well as the research data collectors received safety protocol training. This training included how to respond to an abuser who came home during the visit (e.g., how to safely include the abuser during the home visit, how to safely conclude the visit if necessary).
Fidelity monitoring
Several measures were included to ensure standardization of DOVE intervention delivery, including the following: (1) annual booster training sessions for home visitors; (2) videotaping of the initial training session to use for subsequent home visitor trainings; and (3) intervention documentation forms completed by home visitors were reviewed by a nurse researcher with expertise in IPV interventions, as well as the co-Principal Investigators (PWS and LFB), who evaluated protocol adherence. Any deviations from study protocol were addressed with the individual home visitors. Finally, the co-PIs met with the home visiting program supervisors for each intervention site regularly during the 5-year study and addressed any issue with study implementation.
Study instruments
In addition to the AAS21 to screen for physical and sexual abuse and the WEB scale22 to detect severe psychological abuse with scores above a normed cutoff, the following instruments were used for major outcome data collection, which occurred at baseline and within 1, 3, 6, 12, 18, and 24 months after delivery.
The Conflict Tactics Scale 2 (CTS2)29 was used to measure IPV. The CTS2 assessed abused women's partners' use of a variety of violent behaviors. The instrument has five subscales (i.e., Negotiation, Psychological Aggression, Physical Assault, Sexual Coercion, and Injury). The total score for this study consisted of summed items from all subscales except negotiation, as those 6 items measure nonaggressive acts used to settle disagreements. Cronbach's alpha demonstrated adequate reliability with coefficients ranging from 0.90 to 0.94 for all study time points. At baseline, women were asked about acts in the past year; subsequent data collection time points asked if these acts had occurred since the previous data collection time point.
The Edinburgh Postnatal Depression Scale (EPDS), a 10-item scale, was used to measure depressive symptomatology in the perinatal period.30 Reliability and validity have been reported in multiple studies during the perinatal period.31 Cronbach's alpha at each time point demonstrated adequate reliability with values ranging from 0.85 to 0.89.
All data were collected by research nurses who were not associated with delivering the DOVE intervention. There were no changes to study outcome measures after the trial commenced.
Statistical methods
Preliminary analyses examined sociodemographic variables and key study variables of interest, which determined distribution of data, detected potential outliers and collinearity among variables, as well as described the location and percent of missing data. Missing data (described in detail below) were addressed using multiple imputation procedures, producing 100 fully imputed datasets used in all hypothesis-testing models. Multiple imputation procedures have been demonstrated as a robust method for handling missing data by producing unbiased estimates and enhancing power.32
Success of randomization procedures was determined by comparison of sociodemographic variables across site (rural vs. urban) and intervention groups using t-tests and chi-square analyses for continuous and categorical variables, respectively. Unadjusted comparisons across intervention groups examined mean violence scores at each time point using independent sample t-tests.
Intervention effectiveness was examined using intention-to-treat analyses and mixed-effects linear regression models. Site (urban/rural) was modeled as a random effect, while treatment and time were modeled as fixed effects. Both main effects and interaction terms were tested for treatment and time. Prior research provided evidence that younger age and maternal depression were significant correlates with IPV, and thus age and baseline maternal depression were modeled as additional fixed effects.33 The number of sessions delivered to each woman, as a measure of dose, and intervention fidelity monitors (e.g., fluctuations in setting, delivery of intervention) were examined as additional covariates in subsequent models.
Preliminary analyses demonstrated IPV change over time to be nonlinear for this study and thus time was modeled as a quadratic effect. The quadratic nature of the change in CTS2 scores over time demonstrated a salient change from baseline, but minimal change between subsequent time points (Fig. 2A). Accordingly, two main outcome variables of interest were examined. Initial mixed-effects models examined continuous CTS2 scores (change of violence over time) as the primary IPV outcome variable of interest. Subsequent models examined change from baseline (as a difference score) as the second IPV outcome variable of interest. All analyses were completed using SPSS 22.0 with the significance level set at 0.05 for main analyses and 0.01 for analyses with multiple comparisons. The unit of analysis was the individual.
FIG. 2.
IPV change measured continuously as a score (A, B). (A) IPV change over time—continuous outcome; (B) IPV change from baseline. IPV, intimate partner violence.
Results
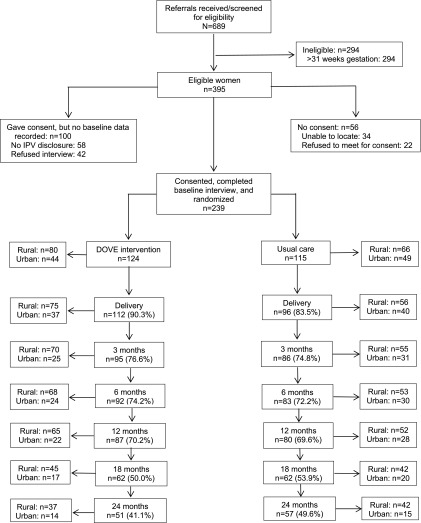
Participating agencies referred 689 women, and 352 women were ineligible due to gestational age >31 weeks or no IPV (Fig. 1). Of the 337 eligible women, 64 women refused the study, the majority at both sites refusing due to lack of time or a preference to maintain privacy regarding their IPV status. In addition, 34 women were unable to be located. Thus, 239 women were randomized to DOVE (n = 124) or UC (n = 115) and completed the baseline assessment. A proportion (22.6%) of women did not have a chance to complete their 18- or 24-month assessments due to recruitment being extended beyond the initial time frame and the inability of employing staff to complete all data collection time points. These women (n = 33 urban; n = 21 rural) were compared to the larger group as well as other women who did not complete all study measures. No significant differences across groups were found on baseline study variables of interest (all p > 0.05).
FIG. 1.
The study enrollment flow diagram for rural and urban recruitment sites.
The demographic characteristics of the women according to study group are shown in Table 2. Comparisons across location and intervention group demonstrated minimal differences in baseline demographics, which suggested that randomization was successful. There were significant differences across location for race, with the urban site enrolling a higher percentage of African American women (86%) compared to the rural site (23%; p < 0.001), which approximated the racial proportions in the two geographic regions. There were no statistically significant sociodemographic differences within sites across the intervention group. The entire sample was Medicaid eligible, a requirement to receive home visiting services.
Table 2.
Baseline Demographic Characteristics of Participants
| Characteristic | DOVE intervention, n = 124 n (%) | Usual care, n = 115 n (%) | p |
|---|---|---|---|
| Race | |||
| African American | 43.5 (54) | 51.3 (59) | 0.49 |
| White non-Hispanic | 44.4 (55) | 40.0 (46) | |
| Other | 11.3 (14) | 8.7 (10) | |
| Missing | 0.8 (1) | 0.0 (0) | |
| Marital status | |||
| Single | 51.6 (64) | 48.7 (56) | 0.14 |
| Partnered, not married | 24.2 (30) | 26.1 (30) | |
| Married | 14.5 (18) | 7.8 (9) | |
| Other (divorced, widowed) | 8.9 (11) | 16.5 (19) | |
| Missing | 0.8 (1) | 0.9 (1) | |
| Employment status | |||
| Full time | 12.1 (15) | 12.2 (14) | 0.17 |
| Part time | 11.3 (14) | 20.9 (24) | |
| Unemployed | 70.2 (87) | 65.2 (75) | |
| Other (homemaker, training)a | 5.6 (7) | 1.7 (2) | |
| Missing | 0.8 (1) | 0.0 (0) | |
| Education level | |||
| <HS | 39.5 (49) | 40.0 (46) | 0.84 |
| HS graduate/GED | 25.8 (32) | 23.5 (27) | |
| Some college/trade school | 23.4 (29) | 21.7 (25) | |
| College/trade school graduate | 8.9 (11) | 12.2 (14) | |
| Missing | 2.4 (3) | 2.6 (3) | |
| Age, mean (SD) | 24.3 (5.6) | 23.4 (5.4) | 0.18 |
Due to low cell numbers, the “other” category was not included in the chi-square analysis.
HS, high school; GED, General Education Diploma.
Preliminary analyses and missing data
Preliminary analyses found all study variables (violence as measured by the CTS2 and depressive symptomatology as measured by the EPDS) to be within expected ranges and detected no outliers or collinearity. Maternal depressive symptomatology did not differ across intervention groups at any time point across the study (all p > 0.05). For the overall study, retention rates ranged from 70% to 90% between each time point,34 with missing data for the study constructs herein ranging from 9% to 30% across all time points, almost entirely due to attrition. Missing data analyses demonstrated that higher proportions of rural women remained in the study than those from urban locations at three time points (3 months χ2 = 3.95, p < 0.05; 18 months χ2 = 5.33, p < 0.05; and 24 months χ2 = 10.66, p < 0.01).
Additional missing data comparisons demonstrated significantly higher mean physical abuse scores for women who did not remain in the study at 6 months (t = 2.02, p < 0.05) and a similar although nonsignificant difference at 12 months (t = 1.74, p < 0 .10). Women who remained in the study were also less likely to have the father of the baby in the house at 3 months (χ2 = 4.12, p < 0.05) with nonsignificant trends of the same at 1 and 6 months.
Additional comparisons between women remaining at 24 months and those who dropped out were not significantly different. Missing data analyses demonstrated that the assumptions for multiple imputation (missing completely at random or missing based on variables included in the study; MCAR, MAR) were met for this study and thus multiple imputation procedures provided an acceptable method for reducing bias in hypothesis testing models.35
Outcomes and estimation
Examining continuous CTS2 scores as the outcome demonstrated no significant treatment effects (main effect nor interaction), but a significant quadratic time effect (F = 114.23; p < 0.001; Fig. 2A). Post hoc pairwise comparisons with Bonferroni correction demonstrated significant differences in mean IPV scores over time from baseline to each of the 1, 3, 6, 12, 18, and 24 month postpartum time points (all p < 0.001). To examine whether the change from baseline differed by intervention group, IPV change from baseline was examined as an outcome new model. In this second model, results demonstrated a significant treatment effect (F = 6.45; p < 0.01; Fig. 2B) such that women in the DOVE intervention group reported a larger mean decrease in IPV scores from baseline with an estimated marginal mean decline of 40.82 compared to 35.87 for women in the UC group. The random effect for site was not statistically significant in either model (p > 0.05), but remained to account for variation by location.
Dose and intervention fidelity monitor variables were not salient in intervention effect models and thus were excluded from final analyses. Presence versus absence of the father of the baby in the house was examined as an additional covariate due to results from missing data analyses. Results did not change with inclusion of this additional covariate and thus the variable did not remain in final models for parsimony. No adverse events, such as IPV-related deaths, were reported.
Discussion
Our results showed a significant decrease in violence using the structured IPV/DOVE intervention in a real-world clinical trial that integrated a perinatal IPV protocol of screening and intervening into several existing home visiting models. The DOVE study was a pragmatic trial in which study participants were not different than women typically enrolled in home visiting programs with regard to sociodemographic characteristics and other vulnerabilities.
Although IPV decreased over time for participants in both groups, a larger and statistically significant decrease was demonstrated for women in the DOVE intervention group. It could be that the study enrollment and data collection procedures functioned as an intervention itself. Home visitors in both study arms were taught how to appropriately screen for IPV and how to coordinate necessary referrals. Thus, all women received basic IPV referral information.
Findings from the Hawaii Healthy Start Home visitation program demonstrated similar effects, wherein IPV decreased when home visitors were taught to be alert for IPV and to provide referrals, but the home visitors said they felt ill equipped to effectively intervene with IPV.36 Other clinical trials of IPV interventions, such as the SHARE trial,37 have found similar results; that is, the ethical obligation of providing abused women with referral information provided at least some intervention. Furthermore, continued assessment for IPV during data collection may have heightened women's motivation to address their concerns.
The DOVE study adds to the evidence supporting empowerment interventions for abused pregnant women and can be used for those home visiting programs receiving MIECHV funds allocated in the ACA. Considering the findings of a recent meta-analysis38 that did not demonstrate improved outcomes for women who were screened for IPV, DOVE is one of the few IPV interventions39 that has demonstrated efficacy. The home visitors who implemented the DOVE protocol had established relationships with women, which facilitated the provision of support, critical to any empowerment intervention. The DOVE protocol was integral in helping women use tailored safety strategies for themselves and their children.
Evidence-based IPV assessment and intervention that is easily implemented can greatly impact the outcomes perinatal home visiting programs seek to achieve, such as improved maternal and child health outcomes. One of the most widely known evidence-based programs, Olds' Nurse Family Partnership program, was less effective at decreasing child abuse in homes where the mother experienced more frequent incidents of abuse.40 Although a variety of home visiting programs have demonstrated improvement in maternal and child outcomes to some degree,41 the DOVE intervention provides a promising adjunct for any home visitation program.
Perhaps one of the most important aspects of this low-cost intervention is that it provided an avenue for the home visitor and the woman to discuss the IPV occurring in the home. It empowered women with strategies to increase their safety as well as the safety of their children and enabled them to leave the relationship safely when they deemed it appropriate. While most studies have not followed abused women over time,38 one of the distinguishing features of our study is that we followed participants from pregnancy through 24 months postpartum. Because of this long follow-up, we provide evidence of long-term decreased IPV.
These findings should encourage researchers and healthcare providers to use the many opportunities for women to receive IPV interventions, including during preconception, prenatal, postpartum, and well-child visits. Findings also suggest that researchers should include long follow-up periods to examine efficacy of IPV interventions as decreasing or ending IPV is a complex process that takes time.
Our findings also demonstrated that the DOVE intervention can be integrated into evidence-based and promising perinatal home visiting programs. The study tested the DOVE intervention in the Nurse–Family Partnership program as well as several promising programs in both urban and rural settings, serving diverse populations. Importantly, the DOVE intervention benefits were realized regardless of the type of program or demographic characteristics of agency personnel, including educational background and professional roles of the home visitors who delivered the DOVE protocol.
Limitations
There were several limitations to the study. First, there was an 18.8% refusal rate, which might be related, in part, to a portion of more severely abused women not wanting an intervention delivered in their home. Anecdotally, we know that some abused women eligible for study participation did not want their home visitor to know about the abuse. It is hard to know what bias this may have introduced into the results, however, we did not find significant differences by intervention group for physical abuse scores (p = 0.93) or women who reported having the father of the baby in the home versus not (p = 0.58). In the most comparable trial, there was a 16% refusal rate suggesting that the refusal rate for this study was not unusual for this population.41
There was also substantial attrition from both groups with the greatest attrition occurring at the 18- and 24-month time points (Fig. 1). In consideration of this, multiple imputation was conducted given its acceptance as the most robust method for handling missing data in a longitudinal study such as this. It has been shown to mitigate the risk of bias that would otherwise be associated with study results using list wise or complete case analyses.35 Examination of the results demonstrates that removal of 18- and 24-month time points (data not shown) do not change substantive findings, providing further support for study results.
Although substantive study results were not affected, attention must be given to the fact that women were less likely to remain in the study if they experienced higher levels of physical abuse, but were more likely to remain if the father of the baby was not in the home. This suggests that more severe abusers, who were most often the father of the baby, may have discouraged the woman from remaining in the study or staying in the home visitation program. More severely abused women may have dropped out of the study because they feared for their safety or the safety of their unborn children or other children in the home. This is a reality for severely abused women. However, it does not negate the findings that DOVE was effective in reducing violence in women with lower levels of violence, thus potentially preventing the violence from becoming more severe and perhaps progressing to its most severe outcome, maternal death from homicide.
These findings emphasize the need for incorporation of an intervention such as DOVE into home visitation. The DOVE intervention, which includes the Danger Assessment, is critical in identifying women at highest risk for danger. Women at highest risk for danger may benefit from additional safeguards, which were not examined in this study, but are an important area for further research. Potentially, women who experienced higher levels of IPV may not have been able to end the relationship, or continue the study, out of fear for their safety or the safety of their children. This was demonstrated in our missing data analyses, wherein women who did not remain in the study after 6 months reported higher physical abuse scores. Even if they were not able to complete all sessions of the DOVE intervention, women received information tailored to their situation that may have facilitated their making changes that decreased their risk for further IPV victimization.
An additional concern was whether women in the intervention group were more likely to report IPV to the research nurses as a result of the intervention experience. We did not see this as a plausible threat to our study conclusions given that women in both groups reported similar levels of violence and the mean difference between groups, although clinically important and statistically significant, was relatively small. This suggests that there may not have been a reporting bias introduced into the study. As an additional examination of this potential threat, we examined reporting of maternal depression across study intervention groups. Mean levels of the maternal depression study covariate did not differ across intervention groups at any point in time across the study (all p > 0.05).
Finally, while culturally acceptable with diverse populations, the DOVE intervention cannot be generalized to non-English speaking women or home visitors. Nonetheless, this study provides support of an evidence-based intervention to decrease women's exposure to IPV in rural Caucasian women and urban African American women. Importantly, this intervention can be incorporated into home visiting programs serving these populations.
The results found in this trial also have important policy implications. The number one reason for maternal mortality in the entire state of Maryland and all the urban cities where it has been examined is IPV homicide, and the most important risk factor for IPV homicide is prior DV.12,42 Women in the DOVE intervention group reported a larger mean decrease in IPV scores from baseline (40.82) compared to women in the UC group (35.87). Although this is a small difference (mean of 4.95), it is both statistically (p < 0.01) and clinically significant. The CTS2 is scored using a frequency scale of 1 (once), 2 (twice), 3 (3–5 times), 4 (6–10 times), 5 (11–20 times), or 6 (more than 20 times).29
Thus, the average five-point reduction would be equivalent to, for example, a reduction in frequency of a violent act such as punching or slapping or slamming against a wall or choking in some combination from 20 or more times down to once or 0. This kind of reduction in abusive incidents and the resulting reduction in physical and mental trauma is important to any abused woman who is carefully calibrating the pros and cons of keeping her relationship and her baby's relationship with its father, the chances of continued improvement in her safety versus that the abuse will continue or get worse.
Follow-up studies with recruitment and retention strategies to obtain larger samples will help to determine if the difference between intervention groups might be larger than reported herein. Results support DOVE as an evidence-based program that meets policy guidelines for delivering evidence-based interventions during home visits. Recently, MIECHV legislation has mandated home visiting as a primary service delivery strategy for improving maternal, infant, and child health outcomes in at-risk families.18 DOVE can be implemented to address IPV, while realizing MIECHV program aims. In addition, these results help to support the case for universal screening for IPV of all pregnant women.43 Only if abused pregnant women are identified as such can DOVE or other DV interventions44 be implemented.
Conclusion
The DOVE intervention was completed at 3 months postpartum, yet the effects were sustained through 24 months postpartum with a reduction in violence. Although attrition reduced the number of participants at 18 and 24 months, the sustained reduction of IPV was significant using robust missing data analyses. Therefore, findings provide evidence that a structured IPV intervention such as DOVE, with support from participating home visiting agencies, can be incorporated into the content of existing perinatal home visiting programs, ultimately improving the health and safety of women and children. Home visiting programs aiming for the best maternal and child outcomes can implement universal screening for perinatal IPV and this evidence-based DOVE intervention used to mitigate the effects of IPV during the perinatal period.
Certainly, IPV presents many challenges to providers working with at-risk families. Continuity of care in a woman's home may allow for more reliable disclosure of IPV during screening as well as more effective opportunities to intervene in ways that equip women for long-term safety. An important goal of Healthy People 2020 is to improve perinatal health in an effort to decrease infant mortality.45 Similarly, the World Health Organization recommendations for responding to IPV and sexual violence against women include the delivery of interventions addressing IPV in antenatal care.3 Findings from our study support the DOVE intervention as an important component in realizing these critical goals and recommendations.
Acknowledgments
This study was supported by NIH/NINR grant R01009093. NIN/NINR had no role or made no contribution to the scientific design of the study, implementation, data collection, or analysis and made no contribution to this article.
Human Subjects/Ethics Approval
The study received human subjects approval from the Institutional Review Boards of the Johns Hopkins University, University of Missouri, participating health departments in Baltimore (urban) and Missouri. The IRB approvals and the NIH Certificate of Confidentiality approvals were obtained before any aspect of the study was implemented and the approval status was maintained for the duration of the study and data analysis.
Authors' Contributions
Drs. Sharps and Bullock had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Ghazarian is responsible for the data analysis. Study concept and design: Sharps, Bullock, and Campbell. Acquisition of data: Sharps, Bullock, Alhusen, and Bhandari. Analysis and interpretation: Sharps, Bullock, Ghazarian, and Campbell. Drafting of the article: Sharps, Bullock, Alhusen, Ghazarian, and Schminkey. Critical revision of the article for important intellectual content: Sharps, Bullock, Alhusen, Campbell, Ghazarian, Bhandari, and Schminkey. Statistical analysis: Ghazarian. Obtained funding: Sharps, Bullock, and Campbell. Study supervision: Sharps, Bullock, and Campbell. Trial Registration: clinicaltrials.gov Identifier: NCT00465556. Additional contribution: We wish to thank the DOVE research team as well as all staff at participating home visiting agencies for their contributions.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Sharps PW, Laughon K, Giangrande SK. Intimate partner violence and the childbearing year: Maternal and infant health consequences. Trauma Violence Abuse 2007;8:105–116 [DOI] [PubMed] [Google Scholar]
- 2.Devries KM, Kishor S, Johnson H, et al. Intimate partner violence during pregnancy: Analysis of prevalence data from 19 countries. Reprod Health Matters 2010;18:158–170 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Responding to intimate partner violence and sexual violence against women: WHO clinical and policy guidelines. Geneva: WHO, 2013 [PubMed] [Google Scholar]
- 4.Silverman JG, Decker MR, Reed E, Raj A. Intimate partner violence around the time of pregnancy: Association with breastfeeding behavior. J Womens Health (Larchmt) 2006;15:934–940 [DOI] [PubMed] [Google Scholar]
- 5.Tjaden P, Thoennes N. Extent, nature, and consequences of intimate partner violence: Findings from the National Violence against Women Survey. Washington, DC: Department of Justice (US) 2000. [Publication No. NCJ 181867] [Google Scholar]
- 6.Vest JR, Catlin TK, Chen JJ, Brownson RC. Multistate analysis of factors associated with intimate partner violence. Am J Prev Med 2002;22:156–164 [DOI] [PubMed] [Google Scholar]
- 7.Bailey BA, Daugherty RA. Intimate partner violence during pregnancy: Incidence and associated health behaviors in a rural population. Matern Child Health J 2007;11:495–503 [DOI] [PubMed] [Google Scholar]
- 8.Alhusen JL, Lucea MB, Bullock L, Sharps P. Intimate partner violence, substance use, and adverse neonatal outcomes among urban women. J Pediatr 2013;163:471–476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alhusen JL, Bullock L, Sharps P, Schminkey DL, Comstock E, Campbell J. Intimate partner violence during pregnancy and adverse neonatal outcomes in a low-income women. J Womens Health (Larchmt) 2014;23:920–926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taillieu TL, Brownridge DA. Violence against pregnant women: Prevalence, patterns, risk factors, theories, and directions for future research. Aggress Violent Behav 2010;15:14–35 [Google Scholar]
- 11.Shah PS, Shah J; Knowledge Synthesis Group on Determinants of Preterm/LBW Births. Maternal exposure to domestic violence and pregnancy and birth outcomes: A systematic review and meta-analyses. J Womens Health (Larchmt) 2010;19:2017–2031 [DOI] [PubMed] [Google Scholar]
- 12.Cheng D, Horon IL. Intimate-partner homicide among pregnant and postpartum women. Obstet Gynecol 2010;115:1181–1186 [DOI] [PubMed] [Google Scholar]
- 13.Palladino CL, Singh V, Campbell J, Flynn H, Gold KJ. Homicide and suicide during the perinatal period: Findings from the National Violent Death Reporting System. Obstet Gynecol 2011;118:1056–1063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bauer NS, Gilbert AL, Carroll AE, Downs SM. Associations of early exposure to intimate partner violence and parental depression with subsequent mental health outcomes. JAMA Pediatr 2013;167:341–347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen PH, Jacobs A, Rovi SL. Intimate partner violence: Childhood exposure to domestic violence. FP Essent 2013;412:24–27 [PubMed] [Google Scholar]
- 16.Levendosky AA, Leahy KL, Bogat GA, Davidson WS, von Eye A. Domestic violence, maternal parenting, maternal mental health, and infant externalizing behavior. J Fam Psychol 2006;20:544–552 [DOI] [PubMed] [Google Scholar]
- 17.Ramsay J, Carter Y, Davidson L, et al. Advocacy interventions to reduce or eliminate violence and promote the physical and psychosocial well-being of women who experience intimate partner abuse. Cochrane Database Syst Rev 2009;8:CD005043. [DOI] [PubMed] [Google Scholar]
- 18.The Patient Protection and Affordable Care Act (PPACA). 2010, Pub. L. No. 111–148, 124 Stat
- 19.Dutton MA. Empowering and healing the battered women. New York: Springer, 1992 [Google Scholar]
- 20.Olds DL, Hill P, Robinson J, Song N, Little C. Update on home visiting for pregnant women and parents of young children. Curr Probl Pediatr 2000;30:107–141 [DOI] [PubMed] [Google Scholar]
- 21.Parker B, McFarlane J. Identifying and helping battered pregnant women. MCN Am J Matern Child Nurs 1991;16:161–164 [DOI] [PubMed] [Google Scholar]
- 22.Coker AL, Smith PH, McKeown RE, King MJ. Frequency and correlates of intimate partner violence by type: Physical, sexual, and psychological battering. Am J Public Health 2000;90:553–559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rabin RF, Jennings JM, Campbell JC, Bair-Merritt MH. Intimate partner violence screening tools: A systematic review. Am J Prev Med 2009;36:439–445.e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McFarlane J, Soeken K, Wiist W. An evaluation of interventions to decrease intimate partner violence to pregnant women. Public Health Nurs 2000;17:443–445 [DOI] [PubMed] [Google Scholar]
- 25.Heo M, Kim Y, Xue X, Kim MY. Sample size requirement to detect an intervention effect at the end of follow-up in a longitudinal cluster randomized trial. Stat Med 2010;29:382–390 [DOI] [PubMed] [Google Scholar]
- 26.Parker B, McFarlane J, Soeken K, Silva C, Reel S. Testing an intervention to prevent further abuse to pregnant women. Res Nurs Health 1999;22:59–66 [DOI] [PubMed] [Google Scholar]
- 27.Campbell JC, Webster DW, Glass NE. The danger assessment: Validation of a lethality risk assessment instrument for intimate partner femicide. J Interpers Violence 2009;24, 653–674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sharps P. Domestic violence enhanced home visitation program-DOVE. Bethesda, MD: National Institutes of Health/National Institutes of Nursing Research, 2004. [NIH/NINR–R01 NR009093] [Google Scholar]
- 29.Straus MA, Douglas EM. A short form of the Revised Conflict Tactics Scales, and typologies for severity and mutuality. Violence Vict 2004;19:507–520 [DOI] [PubMed] [Google Scholar]
- 30.Cox JL, Chapman G, Murray D, Jones P. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in non-postnatal women. J Affect Disord 1996;39:185–189 [DOI] [PubMed] [Google Scholar]
- 31.Matthey S, Henshaw C, Elliott S, Barnett B. Variability in use of cut-off scores and formats on the Edinburgh Postnatal Depression Scale: Implications for clinical and research practice. Arch Womens Ment Health 2006;9:309–315 [DOI] [PubMed] [Google Scholar]
- 32.Mistler SA, Enders CK. Planned missing data designs for developmental research. In: Laursen B, Little TD, Card NA, eds. Handbook of developmental research methods. New York: The Guilford Press; 2012:742–754 [Google Scholar]
- 33.Devries KM, Child JC, Bacchus LJ, et al. Intimate partner violence victimization and alcohol consumption in women: A systematic review and meta-analysis. Addiction 2014;109:379–391 [DOI] [PubMed] [Google Scholar]
- 34.Sharps P, Alhusen J, Bullock L, et al. Engaging and retaining abused women in perinatal home visitation programs. Pediatrics 2013;132(Suppl 2):S134–S139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Little T. Longitudinal structural equation modeling. New York: Guilford Press, 2013 [Google Scholar]
- 36.Bair-Merritt MH, Jennings JM, Chen R, et al. Reducing maternal intimate partner violence after the birth of a child: A randomized controlled trial of the Hawaii Healthy Start Home Visitation Program. Arch Pediatr Adolesc Med 2010;164:16–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wagman JA, Gray RH, Campbell JC, et al. Effectiveness of an integrated intimate partner violence and HIV prevention intervention in Rakai, Uganda: Analysis of an intervention in an existing cluster randomised cohort. Lancet Glob Health 2015;3:e23–e33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.O'Doherty LJ, Taft A, Hegarty K, Ramsay J, Davidson LL, Feder G. Screening women for intimate partner violence in healthcare settings: Abridged Cochrane systematic review and meta-analysis. BMJ 2014;348:g2913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mejdoubi J, van den Heijkant SCCM, van Leerdam FJM, et al. Effect of nurse home visits vs. usual care on reducing intimate partner violence in young high-risk pregnant women: A randomized controlled trial. PLoS One 2013;8:e78185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Olds DL, Kitzman HJ, Cole RE, et al. Enduring effects of prenatal and infancy home visiting by nurses on maternal life course and government spending: Follow-up of a randomized trial among children at age 12 years. Arch Pediatr Adolesc Med 2010;164:419–424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sharps PW, Campbell J, Baty ML, Walker KS, Bair-Merritt MH. Current evidence on perinatal home visiting and intimate partner violence. J Obstet Gynecol Neonatal Nurs 2008;37:480–490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Krulewitch CJ. Epidemiology of intimate partner homicide-suicide events among women of childbearing age in Maryland, 1994–2003. Am J Forensic Med Pathol 2009;30:362–365 [DOI] [PubMed] [Google Scholar]
- 43.Chamberlain L, Levenson R. A guide for obstetric, gynecologic and reproductive health care settings, 2nd ed. American Congress of Obstetricians and Gynecologists Position Statement, 2012. Available at: www.acog.org/-/media/Departments/Violence-Against-Women/Reproguidelines.pdf?dmc=1&ts=20151229T1441508783 Accessed December1, 2015 [Google Scholar]
- 44.Kiely M, El-Mohandes AE, El-Khorazaty MN, Gantz MG. An integrated intervention to reduce intimate partner violence in pregnancy: A randomized controlled trial. Obstet Gynecol 2010;115(Pt 1):273–283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2020. Washington, DC, 2010. Available at: www.healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-child-health Accessed December1, 2015 [Google Scholar]