Abstract
Intestinal epithelial cells provide an important colonization niche for Salmonella enterica serovar Typhimurium during gastrointestinal infections. In infected epithelial cells, a subpopulation of S. Typhimurium bacteria damage their internalization vacuole, leading to escape from the Salmonella-containing vacuole (SCV) and extensive proliferation in the cytosol. Little is known about the bacterial determinants of nascent SCV lysis and subsequent survival and replication of Salmonella in the cytosol. To pinpoint S. Typhimurium virulence factors responsible for these steps in the intracellular infectious cycle, we screened a S. Typhimurium multigene deletion library in Caco-2 C2Bbe1 and HeLa epithelial cells for mutants that had an altered proportion of cytosolic bacteria compared to the wild type. We used a gentamicin protection assay in combination with a chloroquine resistance assay to quantify total and cytosolic bacteria, respectively, for each strain. Mutants of three S. Typhimurium genes, STM1461 (ydgT), STM2829 (recA), and STM3952 (corA), had reduced cytosolic proliferation compared to wild-type bacteria, and one gene, STM2120 (asmA), displayed increased cytosolic replication. None of the mutants were affected for lysis of the nascent SCV or vacuolar replication in epithelial cells, indicating that these genes are specifically required for survival and proliferation of S. Typhimurium in the epithelial cell cytosol. These are the first genes identified to contribute to this step of the S. Typhimurium infectious cycle.
INTRODUCTION
Salmonella enterica serovar Typhimurium causes self-limiting diarrhea in humans and many animals but in some cases can lead to more severe infections. As an intracellular bacterium, S. Typhimurium can survive and replicate within different types of host cells, including epithelial cells, fibroblasts, macrophages, and dendritic cells (1). S. Typhimurium has been regarded as a strictly vacuolar pathogen, but emerging evidence indicates that it can also survive and replicate in the cytosol, at least in epithelial cells (2, 3). S. Typhimurium pathogenesis is largely dependent on type III secretion systems (T3SSs), specialized injection devices that translocate a multitude of bacterial effector proteins into host cells to modulate cell functions (4, 5). T3SS1 is encoded on Salmonella pathogenicity island 1 (SPI-1) and is required for the invasion of nonphagocytic cells (6), such as epithelial cells, and for the biogenesis of the nascent Salmonella-containing vacuole (SCV) (7). The expression of T3SS1 is rapidly downregulated after bacterial internalization (8, 9). T3SS2 encoded on SPI-2 is induced intracellularly (10) and is important for intracellular replication (11, 12) and the maintenance of the mature SCV membrane (13).
In epithelial cells, a proportion of S. Typhimurium bacteria (∼10 to 20%) damage their nascent vacuole via T3SS1-dependent mechanisms (3, 14, 15). Bacteria in compromised vacuoles that are not cleared by autophagic engulfment, called xenophagy (16), eventually hyperreplicate in the epithelial cell cytosol (2). Coincident with cytosolic replication is the expression of T3SS1 and flagella (2), two virulence factors that are normally induced extracellularly. Epithelial cells that harbor these cytosolic Salmonella bacteria eventually die by pyroptosis, characterized by plasma membrane rupture, the release of the proinflammatory cytokine interleukin-18 (IL-18), and cell shedding (2, 17, 18). Pyroptotic cell death could release invasion-primed bacteria (T3SS1 and flagellum induced) into the extracellular space in tissue culture models, or the gut lumen in vivo, which would allow bacterial spread within and between hosts.
The bacterial determinants of nascent vacuole lysis, the evasion of host cell xenophagy, and cytosolic proliferation remain largely unknown. We have screened an S. Typhimurium multigene deletion (MGD) library in the colonic epithelial cell line Caco-2 C2BBe1 for mutants that poorly colonized the cytosol at 7 h postinfection (p.i.) and identified numerous such MGD mutants. Through secondary screening of the single-gene deletion (SGD) mutants corresponding to these candidate regions, we identified four S. Typhimurium genes that recapitulate the phenotype of the corresponding MGD mutant. Three genes, corA (STM3952), recA (STM2829), and ydgT (STM1461), are required for optimal bacterial proliferation in the host cell cytosol, and one gene, asmA (STM2120), appears to affect pyroptotic cell death. Notably, none of the identified genes contribute to the lysis of the nascent SCV or vacuolar replication in epithelial cells. These four genes represent the first genes identified that specifically impact the cytosolic survival and/or proliferation of S. Typhimurium in this cell type.
MATERIALS AND METHODS
Bacterial strains.
Salmonella enterica serovar Typhimurium SL1344 (19) and 14028s (20) were used as wild-type strains. The collection of targeted MGD mutants and SGD mutants of 14028s was described previously (21). Bacteria were grown in Luria-Bertani–Miller (LB-Miller) broth or on LB-Miller agar supplemented with carbenicillin (100 μg/ml), chloramphenicol (30 μg/ml), kanamycin (50 μg/ml), or streptomycin (100 μg/ml), where appropriate.
Unmarked in-frame deletions of asmA (deletion of amino acids 2 to 618 of AsmA), ydgT (deletion of amino acids 2 to 76 of YdgT), recA (deletion of amino acids 2 to 353 of RecA), corA (deletion of amino acids 4 to 314 of CorA), srlR (deletion of amino acids 2 to 257 of SrlR), and hha (deletion of amino acids 4 to 70 of Hha) were constructed in S. Typhimurium SL1344 by allelic exchange. Two fragments of ∼1 kb upstream and downstream of the gene of interest were amplified from S. Typhimurium SL1344 genomic DNA by using Phusion high-fidelity DNA polymerase (Thermo Scientific) (primer sequences used for cloning are listed in Table S1 in the supplemental material). The two fragments were combined for a second round of amplification by overlap extension PCR (22). The fragment was digested with appropriate restriction enzymes, ligated into the suicide vector pRE112 (23), and electroporated into Escherichia coli SY327λpir cells. After sequence confirmation, the pRE112 plasmids were transferred to E. coli SM10λpir for conjugation into wild-type strain SL1344. For the second recombination event, sacB-based counterselection on LB agar containing 5% sucrose was used, and streptomycin-resistant, chloramphenicol-sensitive colonies were screened by PCR with primers outside the recombination region to confirm the deletion of each particular gene.
For complementation of the ΔcorA, ΔrecA, and ΔydgT deletion mutants, the respective genes were expressed on a low-copy-number plasmid under the control of their own promoter. Plasmid pWKS30-corA was described previously (24). To construct pWKS29-ydgT, the ydgT coding region and 980 bp of upstream sequence were amplified from S. Typhimurium SL1344 genomic DNA and ligated into KpnI/SacI-digested pWSK29 (25). Similarly, for pWSK29-recA, the recA coding region and 840 bp of upstream sequence were amplified and ligated into BamHI/KpnI-digested pWSK29. The ΔasmA mutant was complemented by Tn7 integration of asmA at the attTn7 site (26). The asmA coding region and 380 bp of upstream sequence were digested from pWSK29-STM2120 (H. Andrews-Polymenis, unpublished data) with KpnI/SacI and ligated into KpnI/SacI-digested pGP-Tn7-Cm (26). The pGP-Tn7-asmA construct was transferred to E. coli SM10λpir cells and conjugated into the S. Typhimurium ΔasmA strain bearing pSTNSK, carrying the Tn7 transposase-encoding genes tnsABCD (26). Chloramphenicol-resistant S. Typhimurium colonies were screened for the presence of asmA by PCR with asmA-specific primers and primers flanking glmS and sl3827 (26).
Mammalian cell culture.
All cell lines were purchased from the American Type Culture Collection (ATCC) and used within 15 passages of receipt. HeLa cervical adenocarcinoma cells (ATCC CCL-2) were grown in Eagle's minimum essential medium (EMEM; Corning) containing 10% (vol/vol) heat-inactivated fetal bovine serum (HI-FBS; Invitrogen). Caco-2 C2BBe1 colorectal adenocarcinoma cells (ATCC CRL-2102) were grown in Dulbecco's modified Eagle's medium (DMEM; Corning) containing 0.01 mg/ml human transferrin (Sigma) and 10% (vol/vol) HI-FBS. J774A.1 mouse macrophage-like cells (ATCC TIB-67) were grown in DMEM (Corning) containing 10% (vol/vol) HI-FBS. Cells were seeded into 24- or 48-well tissue culture-treated plates (Nunc) 18 to 24 h prior to infection. For C2BBe1 cells, plates were coated with rat tail collagen I (Corning) to promote adherence. Seeding densities were 5 × 104 cells/well (HeLa cells in 24-well plates), 7 × 104 cells/well (C2BBe1 cells in 24-well plates), and 3.5 × 104 cells/well (C2BBe1 cells in 48-well plates). For fluorescence microscopy, HeLa, C2BBe1, and J774A.1 cells were seeded onto acid-washed glass coverslips in 24-well plates at 6 × 104, 8 × 104, and 1.4 × 105 cells/well, respectively. For cytokine secretion assays, C2BBe1 cells were polarized in Entero-STIM enterocyte differentiation medium (Corning) on collagen-coated 24-well cell culture inserts (1-μm pore size; Falcon) as we described previously (2).
Bacterial infection of mammalian cells.
C2BBe1 epithelial cells were used as the infection model for screening of the MGD library. The proportion of cytosolic bacteria was determined by the chloroquine (CHQ) resistance assay (3). S. Typhimurium 14028 wild-type and MGD strains were grown for 16 to 18 h at 37°C with shaking in 2 ml LB-Miller broth (containing kanamycin for MGD strains). The next day, cultures were diluted 1:40 in LB-Miller broth (no antibiotics) and grown at 37°C for 3 h with shaking (optical density at 600 nm [OD600] of ∼3.5). C2BBe1 cells were infected with invasive bacteria in 48-well plates (4 wells per strain) for 10 min (multiplicity of infection [MOI] of ∼100) at 37°C, and cells were then washed three times with Hanks' buffered saline solution (HBSS) and chased for 20 min in growth medium. Growth medium containing 50 μg/ml gentamicin was then added for 1 h, followed by 10 μg/ml gentamicin thereafter. At 6 h p.i., growth medium containing 10 μg/ml gentamicin and 600 μM freshly prepared CHQ (Sigma) was added to two of the four wells for each strain. At 7 h p.i., infected monolayers were washed once in phosphate-buffered saline (PBS) and solubilized in 0.2% (wt/vol) sodium deoxycholate, and serial dilutions were plated onto LB agar. Total bacteria were enumerated in gentamicin-treated wells, and cytosolic bacteria were enumerated in gentamicin-plus-CHQ-treated wells. For strains that gave <5,000 total CFU at 7 h p.i., the initial MOI was increased by 10-fold. In the event that this did not sufficiently increase total bacterial numbers, bacteria were added to monolayers at an MOI of ∼100, and plates were centrifuged for 5 min at 600 × g, followed by a 10-min incubation as described above.
For infections with S. Typhimurium SL1344, bacterial subcultures were grown for 3.5 h as described previously (9). HeLa epithelial cells, C2BBe1 epithelial cells, and J774A.1 macrophage-like cells were infected with invasive bacteria at MOIs of ∼100, 80, and 20, respectively, for 10 min, and infections were continued as described above. For CHQ resistance assays in HeLa cells, the final concentration of CHQ was 400 μM.
Bacterial exit assay.
Assays described previously for Pseudomonas aeruginosa (27) and Porphyromonas gingivalis (28) were adapted to quantify the exit of S. Typhimurium from epithelial cell monolayers. HeLa or C2BBe1 epithelial cells were infected with wild-type S. Typhimurium SL1344 or gene deletion mutants as described above. At 7 h p.i. (HeLa) or 8 h p.i. (C2BBe1), gentamicin-containing medium (10 μg/ml) was removed from wells and replaced with growth medium without antibiotics, and incubation was continued for an additional 1 h at 37°C. Supernatants containing exited bacteria were collected, and serial dilutions were plated onto LB agar for bacterial enumeration.
Measurement of secreted IL-18.
Supernatants were collected from infected HeLa cells, or apical supernatants were collected from polarized C2BBe1 cells, at 10 h p.i. Samples were centrifuged at 16,000 × g for 10 min at 4°C, and IL-18 levels were determined by a sandwich enzyme-linked immunosorbent assay (ELISA) that is specific for the mature form of human IL-18 (18).
Fluorescence microscopy.
HeLa and C2BBe1 epithelial cells and J774A.1 macrophage-like cells were infected with wild-type S. Typhimurium SL1344 or gene deletion mutants harboring pFPV-mCherry, a plasmid that encodes the red fluorescent protein mCherry under the control of the constitutive rpsM promoter (29). For scoring of the number of bacteria per cell, infected monolayers were fixed with 2.5% paraformaldehyde at 37°C for 10 min and incubated with Alexa Fluor 488-phalloidin (1:100; Thermo Fisher Scientific) in 10% (vol/vol) normal goat serum–0.2% (wt/vol) saponin–PBS for 15 min. Hoechst 33342 (1 μg/ml; Thermo Fisher Scientific) was then used to stain DNA. Glass coverslips were mounted on a glass slide in Mowiol, and samples were viewed on a Leica DM4000 fluorescence microscope.
Bacterial growth curves.
Cultures grown overnight were prepared by inoculating one colony into 2 ml LB-Miller broth containing streptomycin (100 μg/ml) and incubating the culture at 37°C with aeration (shaking at 220 rpm) for 16 to 18 h. The next day, a 100-μl aliquot of the overnight culture was subcultured into 10 ml LB-Miller broth in a 125-ml Erlenmeyer flask. Bacterial cultures were incubated at 37°C at 220 rpm, and growth was measured over 6 h by plating serial dilutions onto LB-Miller agar every hour for CFU enumeration.
Statistical analyses.
Except for the initial screen in Caco-2 C2BBe1 cells (see Fig. S1 in the supplemental material), all data are means ± standard deviations (SD) from at least three independent experiments. Statistical analyses were performed by using analysis of variance (ANOVA) with Dunnett's post hoc test (KaleidaGraph); P values of ≤0.05 were considered significant.
RESULTS
Screening of MGD mutants for cytosolic proliferation.
To identify mutants with altered cytosolic replication in human epithelial cells, we screened a library of 198 MGD S. Typhimurium mutants using a CHQ resistance assay. This library contains deletions of 2,543 nonessential genes of S. Typhimurium 14028s with 3 or more contiguous genes replaced by a kanamycin resistance cassette in each mutant (21). We screened the MGD mutants in Caco-2 C2BBe1 cells, a colonic epithelial cell line, using the CHQ resistance assay at 7 h p.i. CHQ is a lysosomotropic drug that targets vacuolar but not cytosolic bacteria and, combined with the gentamicin protection assay, allows the enumeration of the proportion of cytosolic bacteria in the total population (3). Any mutant that fell outside the arbitrary cutoff of the mean ± 2 SD for the proportion of cytosolic wild-type bacteria (28 MGD mutants) (see Fig. S1 in the supplemental material) was subjected to secondary screening in HeLa epithelial cells, again using the CHQ resistance assay at 7 h p.i. Two of these MGD mutants did not invade HeLa epithelial cells (ΔSTM2832–STM2877 [this mutant contains a deletion of genes STM2832 to STM2877] and ΔSTM4565–STM4579), so their phenotypes could not be confirmed in this cell line. The ΔSTM2832–STM2877 mutant had the strongest phenotype in C2BBe1 cells (see Fig. S1 in the supplemental material); this mutant is deleted for genes encoding structural components of T3SS1. The relative permissiveness of C2BBe1 cells to invasion by T3SS1 mutants was previously exploited to demonstrate the importance of T3SS1 for nascent SCV lysis and cytosolic proliferation (3), validating the output of our genetic screen. Furthermore, mutants of SPI-2 (ΔSTM1370–STM1422) or flagella (ΔSTM1183–STM1171, ΔSTM1910–STM1941, and ΔSTM1976–STM1982) had proportions of cytosolic bacteria similar to those of the wild type, in agreement with our previously reported findings (3). Four MGD mutants were chosen for further investigation based upon (i) a reproducible phenotype and (ii) a proportion of cytosolic bacteria being statistically different from the wild type in both epithelial cell lines; three MGD mutants had a lower proportion of cytosolic bacteria than the wild type (ΔSTM1450–STM1464, ΔSTM2843–STM2829, and ΔSTM3950–STM3956), and one MGD mutant (ΔSTM2120–STM2108) had a higher proportion of cytosolic bacteria (Fig. 1; see also Fig. S1 in the supplemental material).
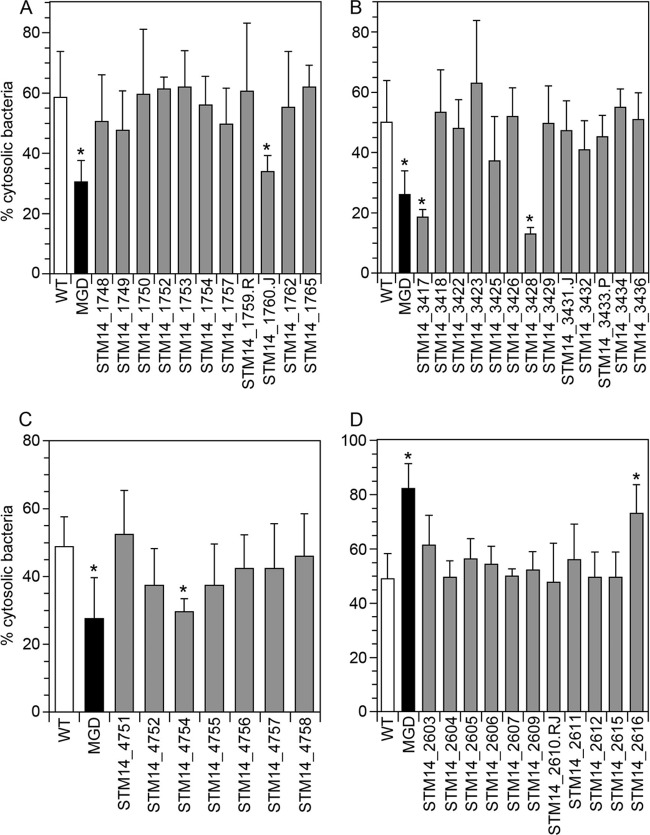
FIG 1.
Identification of the individual gene(s) responsible for each MGD phenotype. Wild-type (WT) S. Typhimurium strain 14028s (white bars), the MGD::Kan mutant (black bars), and the corresponding SGD::Kan mutants (gray bars) were screened in HeLa epithelial cells for the proportion of cytosolic bacteria at 7 h p.i. using a CHQ resistance assay. Means ± SD from at least three independent experiments are shown. Asterisks indicate data significantly different from those for the wild type. (A) MGD ΔSTM1450–STM1464 (ΔSTM14_1748–STM14_1765); (B) MGD ΔSTM2829–STM2843 (ΔSTM14_3417–STM14_3436); (C) MGD ΔSTM3950–STM3956 (ΔSTM14_4751–STM14_4758); (D) MGD ΔSTM2108–STM2120 (ΔSTM14_2603–STM14_2616).
To pinpoint the individual gene(s) within each of these regions responsible for the observed phenotype, we screened the corresponding 14028s SGD mutants (21) in HeLa cells using the CHQ resistance assay. The ΔSTM1450–STM1464 MGD mutant has 15 genes deleted and exhibits a lower proportion of cytosolic bacteria than the wild type in HeLa epithelial cells (29% ± 7.9% versus 59% ± 15%) (Fig. 1A) and C2BBe1 cells (see Fig. S1 in the supplemental material). Screening of the corresponding 14028s SGD mutants identified STM14_1760.J (STM1461), encoding YdgT, as the sole gene responsible for this phenotype (Fig. 1A and Table 1). YdgT is a nucleoid-associated protein that acts as a repressor of horizontally acquired genes, including those harbored on SPI-2 (30, 31).
TABLE 1.
Summary of S. Typhimurium MGD mutants chosen for further characterization
| MGD mutant | Genes deleted (LT2) | Gene responsible for phenotype |
Common name | ||
|---|---|---|---|---|---|
| LT2 | 14028s | SL1344 | |||
| 071/072 E6 | STM1450–STM1464 | STM1461 | STM14_1760.J | SL1344_1393 | ydgT |
| 071/072 G8 | STM2108–STM2120 | STM2120 | STM14_2616 | SL1344_2097 | asmA |
| 073/074 A9 | STM2829–STM2843 | STM2829 | STM14_3417 | SL1344_2809 | recA |
| 073/074 D7 | STM3950–STM3956 | STM3952 | STM14_4754 | SL1344_3906 | corA |
The ΔSTM2829–STM2843 MGD mutant also has fewer cytosolic bacteria than wild-type strain 14028s at 7 h p.i. in both HeLa cells (26% ± 7.9% versus 50% ± 14%) (Fig. 1B) and C2BBe1 cells (see Fig. S1 in the supplemental material) and has 15 genes deleted. The individual deletion of two genes in this region, STM14_3417 (STM2829) and STM14_3428 (STM2837), recapitulated the phenotype of the MGD mutant (Fig. 1B and Table 1). STM14_3417 encodes RecA, involved in homologous recombination (32), and STM14_3428 encodes the DNA-binding transcriptional repressor SrlR.
The third MGD mutant that had a lower proportion of cytosolic bacteria was the ΔSTM3950–STM3956 mutant (28% ± 12% in HeLa cells) (Fig. 1C), which has a deletion of eight genes. Screening of the corresponding 14028s SGD mutants identified STM14_4754 (STM3952), encoding the magnesium transporter CorA (33), as the sole gene conferring the observed phenotype (Fig. 1C and Table 1).
The ΔSTM2108–STM2120 MGD mutant has an increased proportion of cytosolic bacteria at 7 h p.i. in C2BBe1 cells (see Fig. S1 in the supplemental material) and HeLa cells (82% ± 9.1%) (Fig. 1D) compared to the wild type. This mutant is deleted for 13 genes. Only one gene in this region was responsible for the increase, STM14_2616 (STM2120), encoding AsmA, a membrane protein (34) (Fig. 1D and Table 1).
Identification of four S. Typhimurium genes required for cytosolic proliferation in epithelial cells.
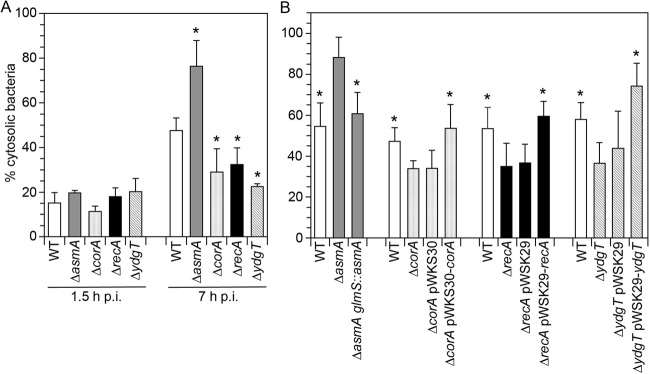
To avoid any problems of cross-contamination between wells in the MGD collection and to confirm our screening hits in a different S. Typhimurium strain background, we used allelic exchange to construct in-frame gene deletion mutants in S. Typhimurium SL1344. ΔasmA (SL1344_2097), ΔydgT (SL1344_1393), ΔrecA (SL1344_2809), ΔsrlR (SL1344_2817), and ΔcorA (SL1344_3906) mutants were compared to wild-type strain SL1344 for the proportion of cytosolic bacteria in HeLa epithelial cells at 1.5 h and 7 h p.i. The SL1344 ΔsrlR mutant did not have a defect in the proportion of cytosolic bacteria at 7 h p.i., nor did an SL1344 srlR::Kan mutant constructed by P22 transduction from the corresponding 14028s SGD mutant (STM14_3428) (not shown). The phenotype that we observed for this SGD mutant (Fig. 1) may be due to a defect elsewhere in the genome, such as an intergenic region or a second-site mutation, and we did not proceed with further characterization of this mutant. However, deletion of the four remaining genes in SL1344 recapitulated their respective phenotypes in the 14028s background (Fig. 2A). The proportion of cytosolic bacteria in HeLa cells at 7 h p.i., which was 48% ± 5.6% for wild-type strain SL1344, was significantly lower for the ΔrecA (32% ± 7.6%), ΔygdT (23% ± 1.3%), and ΔcorA (29% ± 10%) mutants and higher for the ΔasmA mutant (76% ± 12%) (Fig. 2A). Notably, the proportion of cytosolic bacteria for the ΔasmA, ΔcorA, ΔrecA, and ΔydgT mutants was indistinguishable from those of wild-type bacteria at 1.5 h p.i. (Fig. 2A), indicating that none of the deletion mutants are affected in lysis of the nascent SCV in epithelial cells. Complementation of the respective mutants with plasmid-borne recA (pWSK29-recA), ydgT (pWSK29-ydgT), and corA (pWKS30-corA) or chromosomal asmA (glmS::asmA) restored the proportion of cytosolic bacteria to wild-type levels at 7 h p.i. (Fig. 2B), directly linking the observed phenotypes with the corresponding genes.
FIG 2.
The gene deletion mutants are defective for cytosolic proliferation but not nascent vacuole lysis. (A) HeLa epithelial cells were infected with wild-type (WT) S. Typhimurium SL1344 and the ΔasmA, ΔcorA, ΔrecA, and ΔydgT gene deletion mutants. The percentage of cytosolic bacteria was quantified by a CHQ resistance assay at 1.5 h and 7 h p.i. Data were obtained from at least three independent experiments (means ± SD). Asterisks indicate data significantly different from those for the wild type. (B) HeLa cells were infected with wild-type strain SL1344 and the gene deletion mutants complemented in trans (ΔcorA-pWSK30-corA, ΔrecA-pWSK29-recA, and ΔydgT-pWSK29-ydgT) or in the chromosome at the attTn7 site (ΔasmA glmS::asmA). ΔcorA, ΔrecA, and ΔydgT mutants harboring an empty pWSK29 or pWKS30 plasmid were also included as controls. The proportion of cytosolic bacteria at 7 h p.i. was determined by the CHQ resistance assay. Means ± SD from at least three independent experiments are shown. Asterisks indicate data significantly different from those for the respective gene deletion mutant.
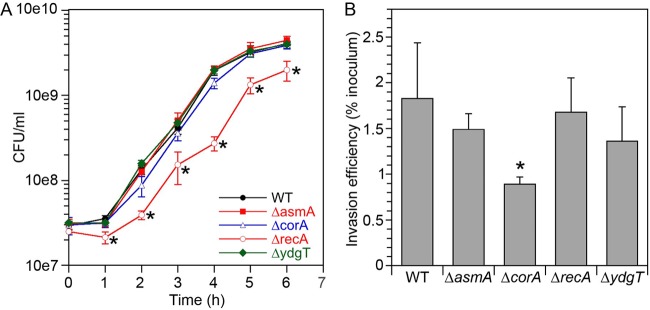
The four gene deletion mutants were tested for growth in rich media: the ΔasmA, ΔcorA, and ΔydgT mutants had no apparent growth phenotypes (Fig. 3A). However, the ΔrecA mutant reached a lower bacterial density than the wild type over the entire time course (Fig. 3A) (P < 0.001). Evaluation of the mutants' relative ability to invade HeLa epithelial cells (number of internalized bacteria at 1 h p.i./inoculum × 100%) (Fig. 3B) revealed that the abilities of the ΔasmA mutant (1.49% ± 0.17% of the inoculum) and the ΔydgT mutant (1.36% ± 0.38%) to invade were comparable to that of wild-type bacteria (1.83% ± 0.61%), whereas the ΔcorA mutant (0.89% ± 0.08%) was impaired (P < 0.01). Fewer ΔrecA bacteria were internalized into HeLa cells at 1 h p.i. (results not shown), but due to the growth defect in broth and, therefore, the lower inoculum, the invasion efficiency (1.68% ± 0.37%) was similar to that of the wild type. Based upon these results, the ΔcorA and ΔrecA inocula were doubled for subsequent infections to ensure that the number of internalized bacteria was comparable to that of wild-type strain SL1344.
FIG 3.
Growth in liquid medium and invasion efficiency of the S. Typhimurium deletion mutants. (A) Wild-type (WT) S. Typhimurium SL1344, ΔasmA, ΔcorA, ΔrecA, and ΔydgT bacteria were grown in rich medium, and CFU were enumerated by serial dilution and plating onto LB-Miller agar. Means ± SD of data from three independent experiments are shown. Asterisks indicate data significantly different from those for the wild type (P < 0.01). (B) HeLa epithelial cells were infected with wild-type S. Typhimurium SL1344, ΔasmA, ΔcorA, ΔrecA, and ΔydgT bacteria, and the number of intracellular bacteria at 1 h p.i. was quantified by a gentamicin protection assay. Invasion efficiency was calculated as the number of internalized bacteria/inoculum × 100%. Means ± SD from four independent experiments are shown. An asterisk indicates data significantly different from those for the wild type.
Single-cell analysis of cytosolic and vacuolar replication.
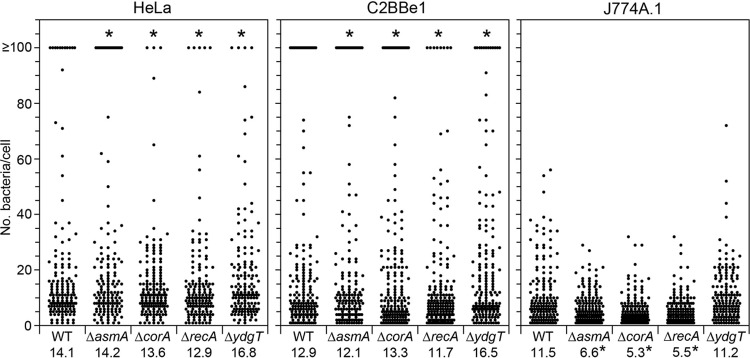
We previously reported two distinct subsets of replicating bacteria in epithelial cells that can be distinguished by fluorescence microscopy: cells with 1 to 40 bacteria harbor vacuolar Salmonella, whereas ≥100 bacteria/cell represent cytosolic Salmonella (2, 3, 17). We used this single-cell analysis technique to assess the ability of the four gene deletion mutants to replicate within the SCV and cytosol of epithelial cells. Wild-type SL1344, ΔrecA, ΔydgT, ΔcorA, and ΔasmA bacteria bearing a plasmid that constitutively expresses mCherry (pFPV-mCherry) were used to infect HeLa and C2BBe1 epithelial cells, and the number of bacteria in each cell was scored by fluorescence microscopy at 8 h p.i. In infections with wild-type bacteria, 7.3% ± 1.2% of HeLa cells contained ≥100 bacteria/cell at 8 h p.i. (Fig. 4). In agreement with the CHQ resistance assay results, significantly fewer infected cells contained ≥100 bacteria upon infection with ΔcorA (1.9% ± 1.9%), ΔrecA (3.3% ± 2.3%), and ΔydgT (2.7% ± 1.2%) bacteria, whereas more HeLa cells contained ≥100 bacteria/cell for the ΔasmA mutant (14.3% ± 1.9%) (Fig. 4). Comparable results were obtained in C2BBe1 epithelial cells, with 13.4% ± 1.3% of cells containing ≥100 bacteria/cell for wild-type bacteria compared to 9.2% ± 2.0%, 4.8% ± 1.9%, 7.2% ± 1.7%, and 21% ± 2.9% for the ΔcorA, ΔrecA, ΔydgT, and ΔasmA mutants, respectively (Fig. 4). To compare vacuolar replication in epithelial cells, we excluded any data points for ≥100 bacteria/cell (cells containing cytosolic Salmonella) and then calculated the mean number of bacteria in each cell for the remaining data set. For wild-type strain SL1344 in HeLa cells, the mean was 14.1 bacteria/cell; there was no statistical difference for the mean number of bacteria/cell for ΔasmA (14.2 bacteria/cell), ΔcorA (13.6 bacteria/cell), ΔrecA (12.9 bacteria/cell), or ΔydgT (16.8 bacteria/cell) infections (Fig. 4). Likewise, there was no significant difference in vacuolar replication between wild-type bacteria and the four deletion mutants in C2BBe1 cells (Fig. 4). Altogether, these results indicate that the observed phenotypes for these mutants are explained not by altered nascent SCV lysis or vacuolar replication in epithelial cells but rather by differences in cytosolic survival and/or proliferation.
FIG 4.
Single-cell analysis of cytosolic and vacuolar replication. HeLa epithelial cells (left), C2BBe1 epithelial cells (middle), or J774A.1 macrophage-like cells (right) were infected with wild-type (WT) S. Typhimurium strain SL1344 or deletion mutants harboring pFPV-mCherry. At 8 h p.i., monolayers were fixed, and the number of bacteria in each infected cell was scored by fluorescence microscopy. Each dot represents data for one infected cell, and data from three independent experiments were combined (≥150 cells in total). For HeLa and C2BBe1 cells, cells with ≥100 bacteria/cell contain cytosolic S. Typhimurium. Values at the bottom of all panels indicate the mean numbers of vacuolar bacteria per cell. Top and bottom asterisks in each panel indicate cytosolic and vacuolar replication significantly different from those of the wild type, respectively.
Hyperreplication of S. Typhimurium in the cytosol is not evident in phagocytic cells, perhaps because Salmonella bacteria are restricted by host cell factors in the macrophage cytosol that remain to be identified (35). We wished to determine whether the four gene deletion mutants that we identified as being altered in cytosolic replication in epithelial cells also had phenotypes in macrophages, a cell type where replication occurs strictly within the SCV. J774A.1 mouse macrophage-like cells were infected with S. Typhimurium wild-type SL1344, ΔrecA, ΔydgT, ΔcorA, and ΔasmA bacteria bearing pFPV-mCherry and fixed at 8 h p.i., and the number of bacteria per cell was scored by fluorescence microscopy (Fig. 4). For wild-type and ΔydgT bacteria, the mean numbers of bacteria per cell were comparable, 11.5 and 11.2, respectively. Despite replicating like the wild type in the SCV of epithelial cells, mutants lacking asmA, corA, and recA replicated poorly in phagocytic cells: infections by ΔasmA, ΔcorA, and ΔrecA bacteria resulted in significantly fewer bacteria per macrophage than did infections with wild-type strain SL1344 at 8 h p.i. (Fig. 4). Therefore, ΔasmA, ΔcorA, and ΔrecA bacteria, but not ΔydgT bacteria, are compromised for growth and/or survival within the SCV of macrophages.
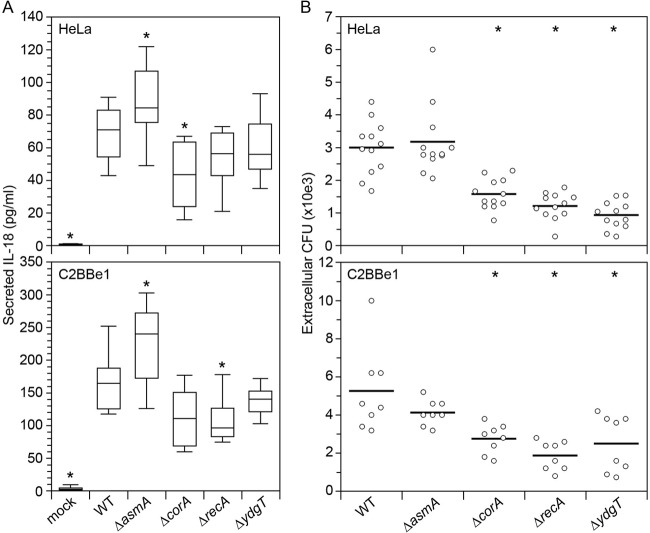
Bacterial egress and inflammasome activation for cytosolic proliferation mutants.
Cytosolic proliferation of S. Typhimurium in epithelial cells leads to the activation of the noncanonical inflammasome via sensing of cytosolic LPS and the release of the proinflammatory cytokine IL-18 in its cleaved and active form (2, 18). We predicted that altered cytosolic proliferation of the S. Typhimurium mutants would affect IL-18 secretion. To test this, we infected HeLa and C2BBe1 epithelial cells with wild-type S. Typhimurium and the four gene deletion mutants, collected cell culture supernatants at 10 h p.i., and assayed for mature IL-18 by ELISAs. Infection of HeLa cells with wild-type bacteria led to the release of IL-18 into the supernatant at 10 h p.i. (mean of 68 pg/ml) (Fig. 5A), consistent with data from previous reports (2, 18). Less IL-18 was detected in supernatants upon infection with the ΔcorA (42 pg/ml; P < 0.05), ΔrecA (53 pg/ml), and ΔydgT (60 pg/ml) mutants, and more IL-18 was detected for infections with the ΔasmA mutant (87 pg/ml; P ≤ 0.05) (Fig. 5A). A similar profile of IL-18 secretion was observed in apical supernatants upon infection of polarized C2BBe1 cells, with less IL-18 being detected for ΔcorA (mean of 112 pg/ml), ΔrecA (108 pg/ml; P ≤ 0.05), and ΔydgT (138 pg/ml) infections and more IL-18 being detected for ΔasmA infections (225 pg/ml; P < 0.05) than for wild-type infections (166 pg/ml) (Fig. 5A). Thus, the amount of IL-18 released by epithelial cells is directly proportional to the level of cytosolic Salmonella bacteria.
FIG 5.
IL-18 release and bacterial exit from epithelial cells for the S. Typhimurium mutants. HeLa and C2BBe1 epithelial cells were infected with wild-type (WT) S. Typhimurium strain SL1344 or the indicated gene deletion mutants. (A) At 10 h p.i., cell culture supernatants were collected from HeLa cells and apical supernatants from polarized C2BBe1 cells. The amount of secreted IL-18 was quantified by an ELISA. Shown are box plots of data from ≥4 independent experiments. Asterisks indicate data significantly different from those for wild-type infection. (B) At 7 h p.i. (HeLa) or 8 h p.i. (C2BBe1), gentamicin-containing medium was removed and replaced with gentamicin-free medium for 1 h. Supernatants were collected, and extracellular CFU were enumerated after serial dilution and plating. Each data point is for one well on a 24-well plate, and data from ≥3 independent experiments are shown (2 to 3 wells per experiment). The horizontal bar indicates the mean. Asterisks indicate data significantly different from those for wild-type infection.
Noncanonical inflammasome activation by S. Typhimurium leads to epithelial cell death by pyroptosis (2, 18). Pyroptotic epithelial cells have a compromised plasma membrane and are eventually shed from the monolayer via a process known as epithelial extrusion (2, 18), providing a potential mechanism for bacterial dissemination. We have previously shown that the majority (>60%) of extruded epithelial cells harbor cytosolic Salmonella (≥100 bacteria/cell); the remaining cells harbor vacuolar Salmonella (18). The mutants that we identified are affected in cytosolic, but not vacuolar, replication in epithelial cells (Fig. 4), providing us a tool to assess which intracellular population of Salmonella is released from epithelial cells. We therefore compared the abilities of wild-type, ΔasmA, ΔcorA, ΔrecA, and ΔydgT bacteria to exit from epithelial cells into the culture medium over a defined time period. HeLa and C2BBe1 cells were infected, and at 7 h p.i. (HeLa) or 8 h p.i. (C2BBe1), gentamicin-containing medium was replaced with gentamicin-free medium. One hour later, the supernatant was collected, and extracellular CFU were enumerated by serial dilution and plating. Despite an increased cytosolic proliferation of the ΔasmA mutant, there was no significant difference in the number of wild-type and ΔasmA bacteria in the extracellular medium for HeLa cells or C2BBe1 cells (Fig. 5B). However, significantly fewer ΔcorA, ΔrecA, and ΔydgT bacteria were released from HeLa cells and C2BBe1 cells (Fig. 5B), indicating that mutants defective in cytosolic proliferation are consequently affected for egress from epithelial cells.
DISCUSSION
The host cell cytosol serves as the preferred site of replication for a number of Gram-negative pathogens, including Shigella flexneri, Burkholderia spp., and Francisella tularensis. The majority of these bacteria lyse their internalization vacuoles before vacuole maturation and fusion with lysosomes. For example, 62% of S. flexneri bacteria are located in the macrophage cytosol by 2 h p.i. (36), 77% of Burkholderia cenocepacia J2315 bacteria are located in compromised phagosomes or free in the cytosol of the human monocytic cell line THP-1 by 3 h p.i. (37), and 95% of F. tularensis bacteria have escaped their phagosome in murine bone marrow-derived macrophages by 1 h p.i. (38). In comparison, only 10 to 20% of internalized S. Typhimurium bacteria lyse their nascent SCV in epithelial cells (1 to 1.5 h p.i.) (3, 14, 15), and even fewer escape the SCV in macrophages (14, 39). Once S. Typhimurium reaches the cytosol of epithelial cells, and after a lag period of 2 to 3 h, it replicates very quickly, and up to half of the total population occupies the cytosol late in infection (3). Interestingly, the doubling time of S. Typhimurium in the cytosol of epithelial cells (2) is comparable to that of professional cytosol-dwelling pathogens such as those mentioned above (40, 41). Given the potential importance of this cytosolic population for bacterial dissemination, we adopted an unbiased approach to identify S. Typhimurium genes required for this phase of intracellular growth.
Bacterial genes encoding biosynthetic enzymes or nutrient uptake genes have been identified in previous genetic screens seeking to identify factors needed for the cytosolic proliferation of S. flexneri, F. tularensis subsp. novicida, and B. pseudomallei (42–44), indicating that energy and nutrient sources are key to the rapid doubling time of bacteria in the mammalian cytosol. Surprisingly, we did not identify such genes in our Salmonella MGD screen, although if these are required for S. Typhimurium growth in broth, they would not have been targeted in the MGD library collection (21). However, we identified CorA, the primary Mg2+ influx channel in S. Typhimurium, as being required for the efficient colonization of the epithelial cell cytosol, implicating magnesium uptake as a requirement for Salmonella growth within the host cell cytosol. CorA is considered ubiquitous in bacteria and archaea (45) and is an essential S. Typhimurium virulence determinant required for systemic infection of BALB/c mice after oral or intraperitoneal inoculation (24). A recent transposon-directed insertion site sequencing (TraDIS) screen identified CorA as a putative determinant of intestinal colonization of cows, pigs, and chickens (46). In addition to poor Mg2+ influx, ΔcorA mutants have altered gene regulation: 87 genes are upregulated and 45 genes are repressed in a ΔcorA mutant grown in LB broth to log phase (24). Among these misregulated genes are key virulence determinants, such as SPI-1, SPI-2, and flagella, that are all repressed 2- to 4-fold in a ΔcorA mutant (24). These data agree with the moderate invasion defect of a ΔcorA mutant in epithelial cells (Fig. 3B) (24). While SPI-2 and flagella do not contribute to the cytosolic replication of S. Typhimurium, SPI-1 mutants are defective for nascent vacuole lysis and subsequent proliferation in the epithelial cell cytosol (see Fig. S1 in the supplemental material) (3). Thus, we currently cannot specify whether the phenotype of the ΔcorA mutant in the epithelial cell cytosol is a direct effect of poor Mg2+ influx, an indirect effect on SPI-1 gene regulation, or a combination of both. In gentamicin protection assays, a ΔcorA mutant has a replication defect in epithelial cells (24), and from our single-cell analysis (Fig. 4), this replication defect can be specifically attributed to the cytosolic population in epithelial cells. ΔcorA mutants are not defective for vacuolar replication in epithelial cells, but they are defective in mouse macrophages (Fig. 4) (24). These data, along with similar cell type-specific defects in vacuolar replication for ΔrecA and ΔasmA mutants (Fig. 4), indicate that the bacterial requirements for proliferation within the SCV are different for epithelial cells and macrophages, likely due to distinct SCV microenvironments.
We also demonstrated that ΔrecA mutants are defective for cytosolic proliferation in epithelial cells. RecA is a recombinase involved in homologous recombination and recombinational DNA repair (32). The ΔrecA mutant is defective for vacuole survival and/or replication in J774A.1 macrophages (Fig. 3) (47), but this defect is no longer apparent in mouse macrophages that are unable to generate an oxidative burst, which is a source of DNA damage (47). In epithelial cells, the ΔrecA mutant is defective for replication and/or survival only in the cytosol and not the SCV (Fig. 4). Reduced growth in the cytosol might be explained, in part, by the relatively poor growth of a ΔrecA mutant in rich liquid broth (Fig. 3A). However, the host cell cytosol may also be a site of bacterial DNA damage, in which case recA would be required for DNA repair. Interestingly, F. tularensis mutants in DNA repair proteins, such as recR, mutL, and uvrC, also have a replication defect in U937 human macrophages, specifically within the cytosol (43), implicating DNA recombination and repair as a generalized requirement for bacterial colonization of the mammalian cytosol.
The third gene that we identified as being needed for appropriate cytosolic replication is ydgT. The ΔydgT mutant replicates poorly in the epithelial cell cytosol but replicates at wild-type levels in the SCV of epithelial cells and macrophages. YdgT and its paralogue, Hha (STM0473), are widely present in the Enterobacteriaceae. Both proteins are nucleoid-associated proteins that act as negative regulators of horizontally acquired genes in S. Typhimurium, including SPI-1, SPI-2, and SPI-5, by a poorly characterized mechanism (30, 31, 48). Deletion of hha in the ΔSTM0468–STM0475 MGD mutant did not result in a defect in the proportion of cytosolic bacteria at 7 h p.i. in our initial screen (see Fig. S1 in the supplemental material), but a S. Typhimurium Δhha mutant was compromised (M. Wrande and L. A. Knodler, unpublished data). This finding indicates that (i) both ydgT and hha contribute to S. Typhimurium survival and/or replication in the epithelial cell cytosol and (ii) the medium-throughput nature of our initial screen was not exhaustive in identifying candidate genetic regions. A ydgT deletion increases SPI-2 transcription and protein levels (30), and the overexpression of a subset of virulence genes by the Δhha mutant is dependent upon the response regulator that activates SPI-2 genes, SsrB (31, 49, 50). However, the effect of ydgT on cytosolic proliferation in epithelial cells is not dependent on SsrB (Wrande and Knodler, unpublished). Therefore, the decreased cytosolic proliferation of ΔydgT and Δhha mutants is not due to an increased production of SPI-2-encoded proteins or dependent upon SPI-2.
In our genetic screen, the ΔasmA mutant was the only mutant that we identified that proliferated more in the cytosol of epithelial cells than wild-type bacteria. This increased cytosolic replication correlated with increased IL-18 release from epithelial cells, indicating enhanced inflammasome activation but not an increased capacity to exit from epithelial cells. AsmA is an inner membrane protein in E. coli K-12 (51) and an outer membrane protein in S. Typhimurium (34). E. coli and S. Typhimurium ΔasmA mutants reportedly have an altered membrane organization and/or fluidity (34, 51). These altered membrane dynamics could account for the increased sensitivity of an E. coli K-12 strain lacking asmA to rifampin, novobiocin, and erythromycin (51), hydrophobic antibiotics that permeate the outer bacterial membrane bilayer. Malik-Kale et al. (17) showed that cytosolic Salmonella bacteria are susceptible to killing by gentamicin, another hydrophobic antibiotic, most likely due to a compromised plasma membrane allowing direct access of the antibiotic to the host cell cytosol. If S. Typhimurium ΔasmA mutants were more susceptible to gentamicin, their viability in the cytosol could be affected and compromise their eventual exit from epithelial cells. However, we did not find a reproducible difference in the sensitivities of S. Typhimurium wild-type and ΔasmA bacteria to gentamicin (L. A. Knodler, unpublished data). Alternatively, if the ΔasmA mutant has a reduced ability to exit epithelial cells or induce pyroptotic cell death, this finding could explain the increased proportion of cytosolic bacteria at later time points. TraDIS analysis indicated that S. Typhimurium ST4/74 asmA mutants are candidates under selection during intestinal colonization of cattle but do not appear to be under selection in pigs or chickens (46). In a separate study, asmA was identified as being required for the survival of S. Typhimurium UK-1 in the stomach contents of pigs by using signature-tagged mutagenesis (52). In competition assays against wild-type S. Typhimurium strain 14028, the ΔasmA mutant is attenuated after oral, but not intraperitoneal, infection of BALB/c mice (34). Collectively, these studies implicate AsmA in S. Typhimurium virulence specifically during the intestinal stages of disease in some hosts (cattle and mice) but not others (pigs and chickens). Potentially, increased inflammasome activation in intestinal epithelial cells (Fig. 5A), which, via IL-18 release, drives the recruitment and activation of neutrophils and macrophages, could lead to this virulence attenuation in the intestine.
Our unbiased genetic screen has identified the first S. Typhimurium genes required for bacterial growth in the epithelial cell cytosol. Interestingly, these genes are not Salmonella specific and have diverse functions, including Mg2+ transport, DNA recombination, transcriptional regulation, and outer membrane composition. This diversity likely reflects the complexity of genes required for the adaptation of Salmonella to the cytosol after its release from the vacuolar environment. We anticipate that future genetic screens may reveal additional genes involved in the colonization of the host cell cytosol that could provide clues to the environmental changes that the organism encounters upon shifting from niche to niche within the cell.
Supplementary Material
ACKNOWLEDGMENTS
We thank Joyce Karlinsey, Ferric Fang, and Yi Zheng for providing plasmids and Tregei Starr for expert technical assistance.
The funders of this work had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Funding Statement
This work, including the efforts of Michael McClelland and Steffen Porwollik, was funded by CDMRP (W81XWH-08-1-0720), USDA (2010-65201-20692, 2011-67017-30127, and 2014-67017-21707), Centre for Produce Safety, Binational Agricultural Research and Development Fund, and North American Meat Institute. This work, including the efforts of Helene Andrews-Polymenis, was funded by NIAID/NIH (R56 AI077645, R01 AI083646, R21 AI083964, R01 AI052237, R01 075093, and R01 AI034829). This work, including the efforts of Leigh A. Knodler, was funded by Paul G. Allen School for Global Animal Health and Stanley L. Adler Research Fund. This work, including the efforts of Marie Wrande, was funded by Swedish Research Council Formas and Wenner-Gren Foundation. This work, including the efforts of Olivia Steele-Mortimer, was funded by NIAID/NIH (1ZIAAI000909).
Footnotes
Supplemental material for this article may be found at http://dx.doi.org/10.1128/IAI.00734-16.
REFERENCES
- 1.Santos RL, Bäumler AJ. 2004. Cell tropism of Salmonella enterica. Int J Med Microbiol 294:225–233. doi: 10.1016/j.ijmm.2004.06.029. [DOI] [PubMed] [Google Scholar]
- 2.Knodler LA, Vallance BA, Celli J, Winfree S, Hansen B, Montero M, Steele-Mortimer O. 2010. Dissemination of invasive Salmonella via bacterial-induced extrusion of mucosal epithelia. Proc Natl Acad Sci U S A 107:17733–17738. doi: 10.1073/pnas.1006098107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Knodler LA, Nair V, Steele-Mortimer O. 2014. Quantitative assessment of cytosolic Salmonella in epithelial cells. PLoS One 9:e84681. doi: 10.1371/journal.pone.0084681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agbor TA, McCormick BA. 2011. Salmonella effectors: important players modulating host cell function during infection. Cell Microbiol 13:1858–1869. doi: 10.1111/j.1462-5822.2011.01701.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McGhie EJ, Brawn LC, Hume PJ, Humphreys D, Koronakis V. 2009. Salmonella takes control: effector-driven manipulation of the host. Curr Opin Microbiol 12:117–124. doi: 10.1016/j.mib.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Galán JE, Curtiss R. 1989. Cloning and molecular characterization of genes whose products allow Salmonella typhimurium to penetrate tissue culture cells. Proc Natl Acad Sci U S A 86:6383–6387. doi: 10.1073/pnas.86.16.6383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Steele-Mortimer O, Brumell JH, Knodler LA, Méresse S, Lopez A, Finlay BB. 2002. The invasion-associated type III secretion system of Salmonella enterica serovar Typhimurium is necessary for intracellular proliferation and vacuole biogenesis in epithelial cells. Cell Microbiol 4:43–54. doi: 10.1046/j.1462-5822.2002.00170.x. [DOI] [PubMed] [Google Scholar]
- 8.Boddicker JD, Jones BD. 2004. Lon protease activity causes down-regulation of Salmonella pathogenicity island 1 invasion gene expression after infection of epithelial cells. Infect Immun 72:2002–2013. doi: 10.1128/IAI.72.4.2002-2013.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ibarra JA, Knodler LA, Sturdevant DE, Virtaneva K, Carmody AB, Fischer ER, Porcella SF, Steele-Mortimer O. 2010. Induction of Salmonella pathogenicity island 1 under different growth conditions can affect Salmonella-host cell interactions in vitro. Microbiology 156:1120–1133. doi: 10.1099/mic.0.032896-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cirillo DM, Valdivia RH, Monack DM, Falkow S. 1998. Macrophage-dependent induction of the Salmonella pathogenicity island 2 type III secretion system and its role in intracellular survival. Mol Microbiol 30:175–188. doi: 10.1046/j.1365-2958.1998.01048.x. [DOI] [PubMed] [Google Scholar]
- 11.Shea JE, Hensel M, Gleeson C, Holden DW. 1996. Identification of a virulence locus encoding a second type III secretion system in Salmonella typhimurium. Proc Natl Acad Sci U S A 93:2593–2597. doi: 10.1073/pnas.93.6.2593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ochman H, Soncini FC, Solomon F, Groisman EA. 1996. Identification of a pathogenicity island required for Salmonella survival in host cells. Proc Natl Acad Sci U S A 93:7800–7804. doi: 10.1073/pnas.93.15.7800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beuzón CR, Méresse S, Unsworth KE, Ruíz-Albert J, Garvis S, Waterman SR, Ryder TA, Boucrot E, Holden DW. 2000. Salmonella maintains the integrity of its intracellular vacuole through the action of SifA. EMBO J 19:3235–3249. doi: 10.1093/emboj/19.13.3235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Du J, Reeves AZ, Klein JA, Twedt DJ, Knodler LA, Lesser CF. 2016. The type III secretion system apparatus determines the intracellular niche of bacterial pathogens. Proc Natl Acad Sci U S A 113:4794–4799. doi: 10.1073/pnas.1520699113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Birmingham CL, Smith AC, Bakowski MA, Yoshimori T, Brumell JH. 2006. Autophagy controls Salmonella infection in response to damage to the Salmonella-containing vacuole. J Biol Chem 281:11374–11383. doi: 10.1074/jbc.M509157200. [DOI] [PubMed] [Google Scholar]
- 16.Knodler LA, Celli J. 2011. Eating the strangers within: host control of intracellular bacteria via xenophagy. Cell Microbiol 13:1319–1327. doi: 10.1111/j.1462-5822.2011.01632.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Malik-Kale P, Winfree S, Steele-Mortimer O. 2012. The bimodal lifestyle of intracellular Salmonella in epithelial cells: replication in the cytosol obscures defects in vacuolar replication. PLoS One 7:e38732. doi: 10.1371/journal.pone.0038732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Knodler LA, Crowley SM, Sham HP, Yang H, Wrande M, Ma C, Ernst RK, Steele-Mortimer O, Celli J, Vallance BA. 2014. Noncanonical inflammasome activation of caspase-4/caspase-11 mediates epithelial defenses against enteric bacterial pathogens. Cell Host Microbe 16:249–256. doi: 10.1016/j.chom.2014.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoiseth SK, Stocker BA. 1981. Aromatic-dependent Salmonella typhimurium are non-virulent and effective as live vaccines. Nature 291:238–239. doi: 10.1038/291238a0. [DOI] [PubMed] [Google Scholar]
- 20.Fields PI, Swanson RV, Haidaris CG, Heffron F. 1986. Mutants of Salmonella typhimurium that cannot survive within the macrophage are avirulent. Proc Natl Acad Sci U S A 83:5189–5193. doi: 10.1073/pnas.83.14.5189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Porwollik S, Santiviago CA, Cheng P, Long F, Desai P, Fredlund J, Srikumar S, Silva CA, Chu W, Chen X, Canals R, Reynolds MM, Bogomolnaya L, Shields C, Cui P, Guo J, Zheng Y, Endicott-Yazdani T, Yang H-J, Maple A, Ragoza Y, Blondel CJ, Valenzuela C, Andrews-Polymenis H, McClelland M. 2014. Defined single-gene and multi-gene deletion mutant collections in Salmonella enterica sv Typhimurium. PLoS One 9:e99820. doi: 10.1371/journal.pone.0099820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Horton RM, Hunt HD, Ho SN, Pullen JK, Pease LR. 1989. Engineering hybrid genes without the use of restriction enzymes: gene splicing by overlap extension. Gene 77:61–68. doi: 10.1016/0378-1119(89)90359-4. [DOI] [PubMed] [Google Scholar]
- 23.Edwards RA, Keller LH, Schifferli DM. 1998. Improved allelic exchange vectors and their use to analyze 987P fimbria gene expression. Gene 207:149–157. doi: 10.1016/S0378-1119(97)00619-7. [DOI] [PubMed] [Google Scholar]
- 24.Papp-Wallace KM, Nartea M, Kehres DG, Porwollik S, McClelland M, Libby SJ, Fang FC, Maguire ME. 2008. The CorA Mg2+ channel is required for the virulence of Salmonella enterica serovar Typhimurium. J Bacteriol 190:6517–6523. doi: 10.1128/JB.00772-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang RF, Kushner SR. 1991. Construction of versatile low-copy-number vectors for cloning, sequencing and gene expression in Escherichia coli. Gene 100:195–199. doi: 10.1016/0378-1119(91)90366-J. [DOI] [PubMed] [Google Scholar]
- 26.Crépin S, Harel J, Dozois CM. 2012. Chromosomal complementation using Tn7 transposon vectors in Enterobacteriaceae. Appl Environ Microbiol 78:6001–6008. doi: 10.1128/AEM.00986-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alarcon I, Evans DJ, Fleiszig SMJ. 2009. The role of twitching motility in Pseudomonas aeruginosa exit from and translocation of corneal epithelial cells. Invest Ophthalmol Vis Sci 50:2237–2244. doi: 10.1167/iovs.08-2785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Takeuchi H, Furuta N, Morisaki I, Amano A. 2011. Exit of intracellular Porphyromonas gingivalis from gingival epithelial cells is mediated by endocytic recycling pathway. Cell Microbiol 13:677–691. doi: 10.1111/j.1462-5822.2010.01564.x. [DOI] [PubMed] [Google Scholar]
- 29.Drecktrah D, Levine-Wilkinson S, Dam T, Winfree S, Knodler LA, Schroer TA, Steele-Mortimer O. 2008. Dynamic behavior of Salmonella-induced membrane tubules in epithelial cells. Traffic 9:2117–2129. doi: 10.1111/j.1600-0854.2008.00830.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Coombes BK, Wickham ME, Lowden MJ, Brown NF, Finlay BB. 2005. Negative regulation of Salmonella pathogenicity island 2 is required for contextual control of virulence during typhoid. Proc Natl Acad Sci U S A 102:17460–17465. doi: 10.1073/pnas.0505401102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Silphaduang U, Mascarenhas M, Karmali M, Coombes BK. 2007. Repression of intracellular virulence factors in Salmonella by the Hha and YdgT nucleoid-associated proteins. J Bacteriol 189:3669–3673. doi: 10.1128/JB.00002-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shen P, Huang HV. 1986. Homologous recombination in Escherichia coli: dependence on substrate length and homology. Genetics 112:441–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Snavely MD, Florer JB, Miller CG, Maguire ME. 1989. Magnesium transport in Salmonella typhimurium: expression of cloned genes for three distinct Mg2+ transport systems. J Bacteriol 171:4752–4760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Prieto AI, Hernández SB, Cota I, Pucciarelli MG, Orlov Y, Ramos-Morales F, García-Del Portillo F, Casadesús J. 2009. Roles of the outer membrane protein AsmA of Salmonella enterica in the control of marRAB expression and invasion of epithelial cells. J Bacteriol 191:3615–3622. doi: 10.1128/JB.01592-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beuzón CR, Salcedo SP, Holden DW. 2002. Growth and killing of a Salmonella enterica serovar Typhimurium sifA mutant strain in the cytosol of different host cell lines. Microbiology 148:2705–2715. doi: 10.1099/00221287-148-9-2705. [DOI] [PubMed] [Google Scholar]
- 36.Guichon A, Hersh D, Smith MR, Zychlinsky A. 2001. Structure-function analysis of the Shigella virulence factor IpaB. J Bacteriol 183:1269–1276. doi: 10.1128/JB.183.4.1269-1276.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Al-Khodor S, Marshall-Batty K, Nair V, Ding L, Greenberg DE, Fraser IDC. 2014. Burkholderia cenocepacia J2315 escapes to the cytosol and actively subverts autophagy in human macrophages. Cell Microbiol 16:378–395. doi: 10.1111/cmi.12223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Checroun C, Wehrly TD, Fischer ER, Hayes SF, Celli J. 2006. Autophagy-mediated reentry of Francisella tularensis into the endocytic compartment after cytoplasmic replication. Proc Natl Acad Sci U S A 103:14578–14583. doi: 10.1073/pnas.0601838103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Meunier E, Dick MS, Dreier RF, Schürmann N, Kenzelmann Broz D, Warming S, Roose-Girma M, Bumann D, Kayagaki N, Takeda K, Yamamoto M, Broz P. 2014. Caspase-11 activation requires lysis of pathogen-containing vacuoles by IFN-induced GTPases. Nature 509:366–370. doi: 10.1038/nature13157. [DOI] [PubMed] [Google Scholar]
- 40.Cersini A, Salvia AM, Bernardini ML. 1998. Intracellular multiplication and virulence of Shigella flexneri auxotrophic mutants. Infect Immun 66:549–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chong A, Wehrly TD, Nair V, Fischer ER, Barker JR, Klose KE, Celli J. 2008. The early phagosomal stage of Francisella tularensis determines optimal phagosomal escape and Francisella pathogenicity island protein expression. Infect Immun 76:5488–5499. doi: 10.1128/IAI.00682-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Runyen-Janecky LJ, Payne SM. 2002. Identification of chromosomal Shigella flexneri genes induced by the eukaryotic intracellular environment. Infect Immun 70:4379–4388. doi: 10.1128/IAI.70.8.4379-4388.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Asare R, Abu Kwaik Y. 2010. Molecular complexity orchestrates modulation of phagosome biogenesis and escape to the cytosol of macrophages by Francisella tularensis. Environ Microbiol 12:2559–2586. doi: 10.1111/j.1462-2920.2010.02229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pilatz S, Breitbach K, Hein N, Fehlhaber B, Schulze J, Brenneke B, Eberl L, Steinmetz I. 2006. Identification of Burkholderia pseudomallei genes required for the intracellular life cycle and in vivo virulence. Infect Immun 74:3576–3586. doi: 10.1128/IAI.01262-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kehres DG, Lawyer CH, Maguire ME. 1998. The CorA magnesium transporter gene family. Microb Comp Genomics 3:151–169. doi: 10.1089/omi.1.1998.3.151. [DOI] [PubMed] [Google Scholar]
- 46.Chaudhuri RR, Morgan E, Peters SE, Pleasance SJ, Hudson DL, Davies HM, Wang J, van Diemen PM, Buckley AM, Bowen AJ, Pullinger GD, Turner DJ, Langridge GC, Turner AK, Parkhill J, Charles IG, Maskell DJ, Stevens MP. 2013. Comprehensive assignment of roles for Salmonella Typhimurium genes in intestinal colonization of food-producing animals. PLoS Genet 9:e1003456. doi: 10.1371/journal.pgen.1003456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Buchmeier NA, Lipps CJ, So MY, Heffron F. 1993. Recombination-deficient mutants of Salmonella typhimurium are avirulent and sensitive to the oxidative burst of macrophages. Mol Microbiol 7:933–936. doi: 10.1111/j.1365-2958.1993.tb01184.x. [DOI] [PubMed] [Google Scholar]
- 48.Vivero A, Baños RC, Mariscotti JF, Oliveros JC, García-Del Portillo F, Juárez A, Madrid C. 2008. Modulation of horizontally acquired genes by the Hha-YdgT proteins in Salmonella enterica serovar Typhimurium. J Bacteriol 190:1152–1156. doi: 10.1128/JB.01206-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Walthers D, Carroll RK, Navarre WW, Libby SJ, Fang FC, Kenney LJ. 2007. The response regulator SsrB activates expression of diverse Salmonella pathogenicity island 2 promoters and counters silencing by the nucleoid-associated protein H-NS. Mol Microbiol 65:477–493. doi: 10.1111/j.1365-2958.2007.05800.x. [DOI] [PubMed] [Google Scholar]
- 50.Worley MJ, Ching KH, Heffron F. 2000. Salmonella SsrB activates a global regulon of horizontally acquired genes. Mol Microbiol 36:749–761. [DOI] [PubMed] [Google Scholar]
- 51.Deng M, Misra R. 1996. Examination of AsmA and its effect on the assembly of Escherichia coli outer membrane proteins. Mol Microbiol 21:605–612. doi: 10.1111/j.1365-2958.1996.tb02568.x. [DOI] [PubMed] [Google Scholar]
- 52.Bearson SMD, Bearson BL, Rasmussen MA. 2006. Identification of Salmonella enterica serovar Typhimurium genes important for survival in the swine gastric environment. Appl Environ Microbiol 72:2829–2836. doi: 10.1128/AEM.72.4.2829-2836.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.