Abstract
Undernutrition and tuberculosis (TB) are linked and have a bidirectional relationship. Undernutrition increases the risk of TB which in turn, can lead to malnutrition. Undernutrition not only is a risk factor for progression of latent TB infection to active disease, but also increases the risk of drug toxicity, relapse and death once TB develops. The dietary intake of TB patients in the country is inadequate. Nutritional supplementation in patients with TB is associated with faster sputum conversion, higher cure and treatment completion rates, significant gain in body weight and body composition as well as better performance status.
The Government of India has various social support schemes (including nutrition supplementation schemes) and policies, at the Centre as well as State levels. Here we discuss some successful examples and suggest a few solutions to address this gap; like considering TB patients as a vulnerable group for “Targeted Public Distribution System” and providing extra rations for the duration of treatment. Recommendations for the research community, civil societies, government organizations, non-governmental and corporate sector on the actions needed to achieve the goals of the End TB Strategy are also provided. Ultimately, reduction of TB burden in India and its elimination will require improving the nutritional status of the community as a whole.
Keywords: Nutritional supplementation, risk factor, social support, tuberculosis, undernutrition
Introduction
Nutrition plays a vital role in the causal chain of many diseases. Malnutrition is one of the leading causes of morbidity in humans - be it overnutrition as in obesity and its related complications or undernutrition as in Kwashiorkor or marasmus. The impact of nutritional status on the occurrence, morbidity and mortality pattern in infectious diseases like diarrhoea, tuberculosis (TB) and HIV has been well documented1 but not given enough recognition. Tuberculosis and undernutrition are both problems of considerable magnitude and importance worldwide. Here we present the current situation of malnutrition and TB in India and the ways to deal with this double trouble in the country.
Situational analysis
Magnitude of TB disease in India
India one of the countries with the highest burden of TB in the world, accounts for approximately one fifth of the global incidence. In 2013, 2.1 out of the 9.0 million estimated global annual incidence of TB cases occurred in India2. World Health Organization (WHO) estimates that in India approximately 300,000 people die from TB each year3, while the Global Burden of Disease study (GBD 2013) estimates > 0.5 million deaths/year4. It is also estimated that approximately 40 per cent of the Indians are infected with tubercle bacillus, Mycobacterium tuberculosis, the vast majority of whom have latent (dormant) TB infection rather than active disease2.
Data from the Revised National TB Control Programme (RNTCP), show a decline in the prevalence and mortality rates of TB in the past 10 years3. However, the incidence is declining very slowly5 and at least a million patients are being “missed” by the programme - being either undiagnosed and untreated or managed in the private sector with no notification to the programme. Studies point to the role of various social, behavioural, economic and environmental factors like undernutrition, indoor air pollution, smoking and alcohol addiction, ignorance and poverty as barriers to complete elimination of TB6,7,8,9. Of these, undernutrition is the single most important predisposing factor for TB in India, with a population attributable fraction of over 50 per cent in most States10.
Magnitude of undernutrition in India
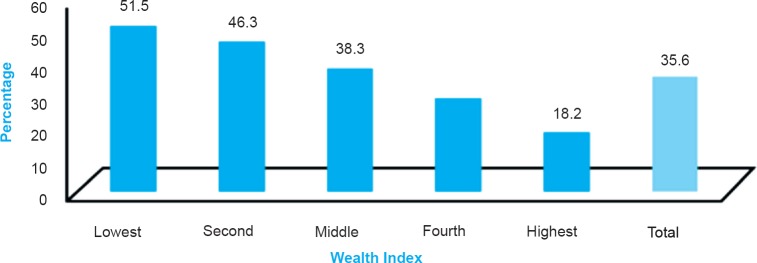
Despite the fast economic growth in the country, India continues to have a large number of undernourished and food insecure people. The Global Nutrition Report 2014, presenting the occurrence of undernourishment over a period of three decades in India, reports that though the rates of undernutrition have come down from 26 to 15 per cent, the period of progress over the decades is quite limited11. National Family Health Survey (NFHS-3) reports that 33 per cent of women and 28 per cent of men are malnourished12. In India, every third woman of reproductive age group is undernourished with a body mass index (BMI) less than 18.5 kg/m2 and they are most significantly observed in the lowest wealth index group, across the country (Fig. 1)13. Among under-5 children stunted growth was seen in 48 per cent (22% severely), 43 per cent were underweight (16% severely) and wasting was found in 20 per cent of children (8% severely)12. Children from poor households are approximately three times more likely to be undernourished than those from wealthier families. Similarly, prevalence of undernutrition is higher in tribal and rural areas compared to urban, and is greater in women than in men13.
Fig. 1.
Prevalence rate of undernourished women based on wealth quintile.
Source: Ref. 13, reproduced with permission.
Undernutrition and tuberculosis linked
The relationship between TB and nutrition is bidirectional, i.e. having active TB leads to loss of weight, and being underweight is considered a risk factor for developing TB, whether through reactivation of latent TB or developing progressive primary disease upon infection14. Undernutrition also leads to worse treatment outcomes once TB has developed. A systematic review of literature showed that across a variety of settings with different levels of TB burden, a strong and consistent log-linear relationship existed between BMI and TB incidence - for each unit reduction in BMI the risk of TB increased by about 14 per cent (Fig. 2)15. In an analysis of NFHS and other available data, the distribution of undernutrition was highest among younger age groups, women, rural people, members of the scheduled tribes and people in the lower quintiles of the wealth index. A notable finding in this study was that among the youngest age group (15-19 yr), up to two-third of incident TB cases could be attributable to undernutrition16. Modelling showed that in India, about 50 per cent of TB cases could be attributed to undernutrition, implying that improving nutritional status could have a dramatic impact on TB incidence17.
Fig. 2.
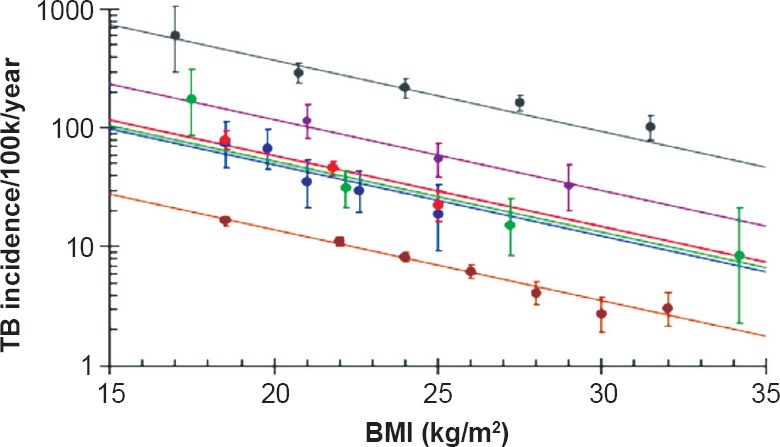
Dose-response relationship between body mass index (BMI) and TB incidence in various studies.
Source: Ref. 15, reproduced with permission.
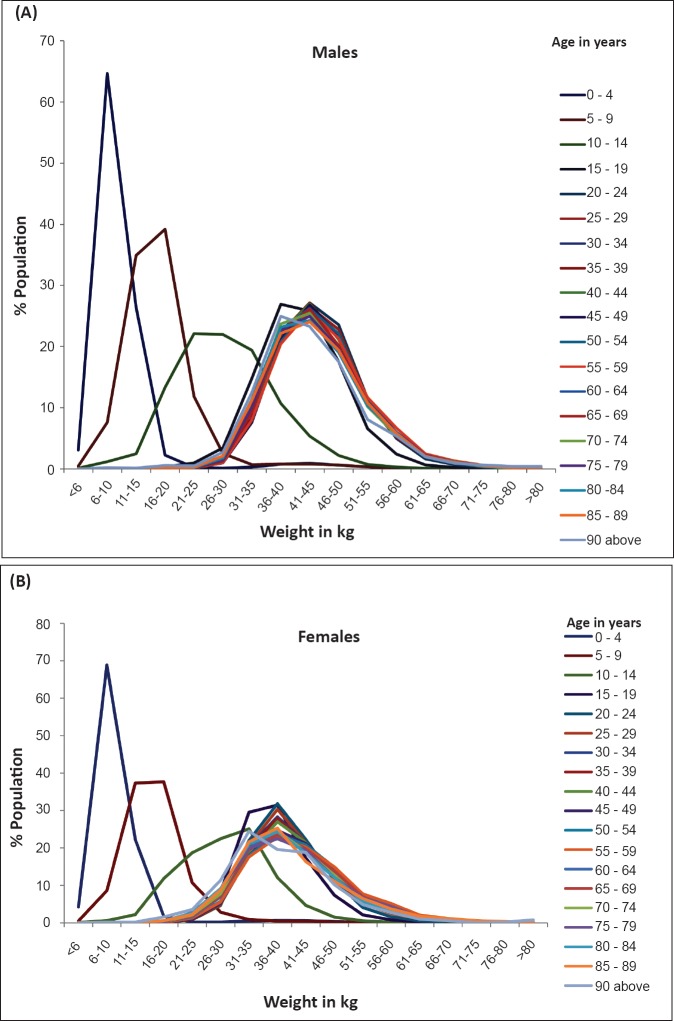
Data from the NIKSHAY portal (web-based tool that monitors TB patients in RNTCP) reveals that of the three million TB patients notified in the RNTCP, the median weight for adult men is 43 kg and for women 38 kg (Fig. 3) (personal communication with Central TB Division, Directorate General Health Services, Ministry of Health and Family Welfare, Government of India).
Fig. 3.
A, B. Gender and age-wise weight of tuberculosis patients notified in the Revised National TB Control Programme [Analysis of patient-wise information from case based electronic information (NIKSHAY) with the median weight for adult men (43 kg) and women (38 kg)].
In many parts of India, patients with active TB, especially those with pulmonary TB, have co-existing undernutrition, which can be severe and life-threatening, but is under-recognized and ignored18,19. In a report from Chattisgarh State among 1695 adult pulmonary TB patients, 90 per cent were found to have some degree of undernutrition20. At diagnosis, majority of patients (80% women and 67% men) had evidence of severe chronic undernutrition. Half of men had weight less than 42 kg while women were less than 34 kg. Many patients had levels of undernutrition that were incompatible with life. Nearly half of women had severe undernutrition at the end of treatment. Moreover, severe undernutrition at diagnosis has been shown to be associated with a 2-fold increased risk of death20.
Undernutrition and TB mortality: Undernutrition as a risk factor for TB mortality has been documented in multiple studies across the world21,22,23. A study among TB patients in south India reported high death rates among patients with low baseline weights, even among patients with smear negative TB; mortality was 14 per cent among those weighing <35 kg compared to 4 per cent among those weighing > 45 kg21. In a population-based cohort study from Mumbai, underweight and smoking were attributable to around 27 per cent of male TB deaths, while use of smokeless tobacco with underweight attributed to 22 per cent of male and 37 per cent of female deaths24. Undernourished patients also have increased severity of disease, which in turn increases the risk of mortality25.
Undernutrition and post-TB treatment: Patients with a poor nutritional status at the end of treatment are likely to have poor performance status because of poor muscle strength. These patients also have a higher risk of TB relapse after completion of therapy26.
Undernutrition and paediatric TB: (i) Young children are at risk of developing primary progressive disease with the risk being higher among malnourished children and children under-3 years of age27. A study that conducted TB screening of severe acute malnourished children attending a nutritional rehabilitation centre in Karnataka28, demonstrated that 4 per cent of the 460 children were diagnosed with TB when they were actively screened for TB, using the diagnostic algorithm of National TB Programme while only 0.3 per cent of 763 children were diagnosed with TB when active case finding was not done.
(ii) Malnutrition can also impair the protective efficacy of Bacillus Calmette-Guerin (BCG) vaccine among a nutritionally deficient vaccinated population. In a study done in the 1960s it was shown that following BCG vaccination, malnourished children were twice as likely to develop TB as their well nourished peers29.
(iii) Undernourished contacts of drug-resistant TB patients showed a higher risk of developing active disease30.
(iv) Malnutrition is considered to be a marker of severity of TB-HIV disease, and is associated with higher rates of unfavourable treatment outcome, including death, among drug-resistant and HIV co-infected children31.
Effect of undernutrition on anti-TB drugs: (i) Undernourished patients have been shown to have poor bioavailability of key drugs like rifampicin which can contribute to treatment failure and development of multi-drug resistance32.
(ii) Undernourished patients have higher risk of hepatotoxicity, which is a major side effect of TB therapy and can contribute to default33.
Nutrition, TB and diabetes: Dye et al34 calculated the expected changes in TB incidence between 1998 and 2008 among rural and urban adult population of India accounting for the temporal changes in BMI, prevalence of diabetes and population age structure. As a result of rapid urbanization, increasing life expectancy, body mass index and rising prevalence of diabetes, TB incident cases would have increased 28 per cent, from 1.73 million to 2.11 million, faster than population size, generating an increase in TB incidence per capita of 5.5 per cent in 10 years34.
Nutritional status and immune functions: The link between poor nutritional status and malfunctioning of the immune system has been well established. Both macro- and micronutrient deficiencies affect the immune system. Undernutrition compromises mucosal barrier function, allowing microbial translocation and weakening of immune system (especially cell mediated immunity) thus reducing the ability of the patient to remove the pathogens once they enter the body35. Conversely, repeated infections can worsen nutritional status due to reduced appetite, lower intake and poor absorption, increased nutrient requirements as well as loss of nutrients. Thus, infections contribute to malnutrition leading to a vicious cycle, making the link between nutrition and health inextricable35.
Evidence of food and nutritional supplementation in tuberculosis: Although it is known that patients with TB suffer from malnutrition related to macronutrients, micronutrients and minerals, studies on the effect of nutritional supplements on patient outcomes have been limited and have shown varying results. The earliest study of the role of a nutritious diet was during the landmark Madras trial of sanatorium vs. home therapy, which showed that at 12 months weight gain in the sanatorium group was double than that of the home group, but the difference in the sputum culture conversion did not differ significantly36. In a re-analysis of the data, it was found that patients in the sanatorium group had a shorter time to sputum conversion (3 months in the sanatorium group as compared to 4 months in the home group), and a higher rate of persistent bacteriological cure (89.7 vs.74.7%)37.
In a clinical trial of nutritional supplementation among sputum positive TB patients with or without HIV co-infection at Vellore Tamil Nadu, India, poor outcome to treatment was observed among 1 of 35 (2.9%) in the supplemented and 5 of 42 (12%) in the unsupplemented group at the end of treatment. Among TB-HIV co-infected individuals, 4 of 13 (31%) in the supplemented and 3 of 7 (43%) in the unsupplemented group had poor outcomes. These differences were more marked after one year of follow up38. A recent randomized trial of nutritional supplements done on 100 patients in India showed that nutritional supplementation was associated with significant improvements in sputum conversion, cure rates, treatment completion rates, and performance status39. In a non-randomized interventional study of supplementation in TB/HIV and HIV-infected patients, at the end of six months of supplementation significant gains in body weight, mid-arm circumference, body mass index, fat-free mass, and body cell mass were observed in the supplemented group as compared to the control group; gains were greater in patients with severe immunodeficiency40.
In Delhi, a randomized, blinded, placebo-controlled trial assessed the effect of micronutrient supplementation in 403 children treated with anti-tuberculosis therapy. It did not show any gain in weight or enhanced clearance of radiographic lesions in children with intrathoracic TB. However, over six months, children in the micronutrient supplement group had a faster height gain than those who did not receive the supplement (height-for-age, z score Δ = 0.08; P = 0.014)41. However, a Cochrane review of 12 trials involving 3393 people on various types of nutritional supplements found only limited evidence to support the role of nutritional supplements in TB42. This review shows that high energy supplements and combinations of zinc with other micronutrients like vitamin A may help TB patients to gain weight and reduce deaths in HIV-TB co-infection. In a systematic review on the effect of food assistance on enabling treatment adherence, eight of ten studies found that provision of food could improve adherence thus assist in treatment completion among both TB as well as HIV-TB co-infected patients43. This emphasizes the fact that unresolved food insecurity could act as a barrier to adherence to TB treatment which in turn can adversely affect the completion and outcome of TB treatment.
World Health Organization (WHO) has brought out a set of guiding principles for the nutritional care and support of TB patients44. These include:
-
(i)
Patients with active TB disease should receive prompt diagnosis and treatment should be initiated early based on WHO/RNTCP guidelines and the national standards of care. If malnutrition is identified at the time of TB diagnosis, it should be considered as a key causal factor to be addressed. Concerns about further weight loss from pre-treatment values or failure to gain weight during TB treatment should trigger detailed clinical re-assessment for co-morbid conditions (like glucose intolerance, HIV, etc.), poor adherence to treatment or development of resistance to anti-TB medications. Nutritional assessment should be done to identify the most appropriate interventions.
-
(ii)
An adequate diet (with all essential macro- and micronutrients), is mandatory for the health and well-being TB patients and also those with TB infection.
-
(iii)
As both undernutrition and TB have been shown to have a bidirectional causal link, nutritional screening, assessment and management must form an integral components of TB care and prevention.
-
(iv)
Poverty and food insecurity can be both cause and consequence of TB. Hence, these have to be recognized and addressed by those involved in the management of TB patients.
-
(v)
TB can also be accompanied by co-morbidities like diabetes mellitus, HIV, and habits like smoking, alcohol or substance abuse. These have their own nutritional implications and should be addressed while screening a TB patient for nutritional fitness.
Response analysis
(i) Existing nutrition-relevant policies/Schemes of Government of India
The Prime Minister's National Council for India's Nutrition Challenges provides reviews, policy directions, and coordinates amongst various programmes. For pregnant women, nursing mothers and children below six years of age supplementary feeding (as a gap filling measure) is provided as one of the services under the Integrated Child Development Services Scheme (ICDS). The “Midday Meal Scheme”, in schools supplies free lunch on working days for children in primary and upper primary classes in Government, Government aided, Local Body, and Alternate Innovative Education Centers nationwide, to improve the nutritional status of school-age children. The Rajiv Gandhi Schemes for Empowerment of Adolescent Girls (RGSEAG), namely SABLA provides a package of services including health and nutrition to adolescent girls not currently studying in the school in age group of 11-14 yr, and nutrition for all girls between in 200 districts. Also, the Indira Gandhi Matritva Sahyog Yojana (IGMSY) provides cash assistance to pregnant and lactating mothers for improving health and nutrition and also supports to provide early and exclusive breastfeeding for the first six months of life. For general public, essential food items are available at subsidized cost through Targeted Public Distribution System (TPDS)13.
The “Antyodaya Anna Yojana” (AAY), launched in December 2000, contemplates providing food grains (wheat and rice) at a highly subsidized rate for one crore poorest of the poor families amongst those below the poverty line within the States. The Government has also introduced the Food Security Bill. The National Food Security Act, 2013 (also Right to Food Act) aims to provide subsidized food grains to approximately two thirds of India's population. Under the provisions of this bill, beneficiaries of the public distribution system are entitled to 5 kg of cereals per person per month at subsidized rate. Pregnant women, lactating mothers, and certain categories of children are eligible for “take home rations” or daily free meals45.
(ii) Response at State level to tackle undernutrition among tuberculosis patients
In Tamil Nadu, Chennai Corporation has been providing free breakfast for TB patients in certain DOTS centres, through the AMMA canteens. Under the Uzhavar Pathukapu Thittam (Farmer's benefit scheme) of the Government of Tamil Nadu,  1000 is provided monthly during treatment to all TB patients who have a farmer's card46. Certain non-government organizations (NGOs) in Tamil Nadu provide nutritional aids to TB patients based on their socio-economic background. They provide health mix, dal to patients and this has resulted in improved adherence and treatment results47. One such example is the REACH (Resource Group for Education and Advocacy for Community Health) organization. In 2008, REACH started to provide assistance of food supplements to deserving patients on individual case basis. Deserving TB patients were given five kg of rice; one kg of pulse (dal) and some health mix every month till they completed their treatment. This support enabled patients to adhere regularly to treatment. A small study done by the same team on food insecurity among 72 TB patients revealed that nearly two-thirds of the families were food insecure47.
1000 is provided monthly during treatment to all TB patients who have a farmer's card46. Certain non-government organizations (NGOs) in Tamil Nadu provide nutritional aids to TB patients based on their socio-economic background. They provide health mix, dal to patients and this has resulted in improved adherence and treatment results47. One such example is the REACH (Resource Group for Education and Advocacy for Community Health) organization. In 2008, REACH started to provide assistance of food supplements to deserving patients on individual case basis. Deserving TB patients were given five kg of rice; one kg of pulse (dal) and some health mix every month till they completed their treatment. This support enabled patients to adhere regularly to treatment. A small study done by the same team on food insecurity among 72 TB patients revealed that nearly two-thirds of the families were food insecure47.
During 2010-2011 the TB Forum of Kasargod, Kerala, supported 101 deserving TB patients with a nutritional kit for six months48. Deserving TB patients were selected based on their family condition and body mass index (BMI). The TB Forum identified a nutritional kit for the TB patients which included rice, green gram, groundnut, garlic, and ghee.
Brihanmumbai Municipal Corporation (BMC), Mumbai, provided calorie-rich food, in the form of Upma or Sheera, to all multi drug resistant and extensively drug resistant (MDR and XDR) TB patients under a pilot project mode in 36 centres of Mumbai49. The initial response was good in terms of weight gain and treatment adherence though a few patients had expressed fatigue and monotony to the type of food given. Following the success of this model, food supplementation either as cooked food or additional monthly rations for drug-resistant TB patients is being planned to be replicated in other parts of the city49.
Gap analysis
Despite many schemes to address undernutrition in India, nutrient gaps are still rampant across the country. The gaps observed in food and nutrient intake reveals that though average diet is adequate in cereals, it lacks adequate and good sources of quality protein such as pulses or dairy products, fat, fat-soluble vitamins A, D and K and micronutrients such as iron, zinc, folic acid and this gap widens as the wealth index of the population decreases13. Decreased intake of micronutrients constitutes a major public health problem as it adversely affects the growth, survival and brain development of individuals13.
Critical gaps in existing programmes/Difficulty in implementation
-
(i)
All government programmes are vertical programmes. There is poor cross-linkage and no programme supports TB patients.
-
(ii)
Involvement of local governments like Gram Panchayats, Municipal councils and local headmen like Sarpanch, Councilors, etc. in public health programmes is lacking and hence the follow up or involvement from the grass root level is suboptimal.
-
(iii)
No link between health programme and social security programme.
-
(iv)
Nutritional aspect not addressed in government health programme related to infectious dieases. There is a lack of civil society, corporate or private sector interaction with government programmes.
-
(v)
Lack of awareness about the importance of nutrition in prevention and control of infectious diseases among both patients as well as health providers.
Research needs to improve evidence for nutritional support for tuberculosis patients
There is not enough evidence to support the claim that nutritional management of patients with active TB should be in any way different from those individuals without active TB. Policymakers and stakeholders require evidence from basic and clinical sciences as well as at epidemiological and operational levels, on the need for additional nutritional supplement and support for patients with active TB disease. There are many unanswered questions in this field:
-
(i)
Is the resting energy expenditure different (more or less) between patients with active TB disease and those without TB?
-
(ii)
What is an optimal diet for a patient with active TB disease and for their close contacts with latent TB infection?
-
(iii)
Can macronutrient supplementation improve TB treatment outcomes among patients on treatment for active TB disease? Which group - children, adolescents, adults or pregnant and lactating women, will benefit the maximum by it?
-
(iv)
Is there a role for micronutrient supplementation for patients on anti-TB treatment? If so, which micronutrient (alone, combined or as multiple micronutrients) should be recommended?
-
(v)
Can population-level nutritional interventions reduce the progression from latent TB infection to active TB disease among close household contacts of patients with active TB disease?
-
(vi)
Is there an optimal BMI above which TB relapse can be prevented among individuals already treated for TB?
Suggested solutions/measures to address undernutrition in tuberculosis
(A). Recommendations for Government organizations
-
(i)
Link programmes of Ministry of Women & Child Development and Ministry of Health and Family Welfare to identify common beneficiaries.
-
(ii)
Extend TB and HIV control programmes to ensure nutrition and food adequacy to patients.
-
(iii)
Extension of scope of Nutritional Rehabilitation Centres (NRCs) to deal with patients with infectious diseases who have nutritional deficiencies through hospitalization, therapeutic feeding and nutritional rehabilitation.
-
(iv)
Mainstream nutrition and food security assessment and care into health programmes. Prioritize beneficiary groups most vulnerable to nutritional challenges like TB or HIV infected patients for maximum and long-term impact of nutritional intervention.
-
(v)
Consider TB patients as a vulnerable group for TPDS and increased food allowances to patients and family through vouchers, food stamps in PDS, NRCs, Anganwadis, etc. For example, (a). Propose household food baskets for TB patients to meet 50 per cent of the recommended daily allowances of cereals, pulses and edible oil, taking into consideration their local preferences. Different types of pulses and oils can be issued on a rotation basis. (b). Fortify the staple foods mainly rice or wheat in the food basket specifically for TB/HIV patients, with micronutrients and vitamins like vitamins A, D, zinc, calcium, etc. and (c). Consider supplying locally cultivated and preferred food substances rather than providing same type of food items across the country.
-
(vi)
The RNTCP does not offer direct nutritional support to TB patients within the programme, as this was not the mandate of the Ministry of Health and Family Welfare. However, programme does encourage States, districts or any other agency to generate evidence and improve adherence and confidence of public in the programme.
(B). Recommendations to civil societies
-
(i)
Impart education and awareness on role of nutrition in TB and infections.
-
(ii)
Community based programmes to educate on the various benefits of adequate food, healthy diet and nutrition intake thus avoiding both under- and overnutrition.
-
(iii)
Involvement of ASHAs (accredited social health activities) and DOT providers, both community and family, in nutrition support and nutritiona counselling programmes for TB patients.
-
(vi)
Organize outreach programmes / activities, to increase accessibility, awareness of balanced food and nutrients to TB / TB-HIV infected population.
-
(v)
Capacity building through organization of community vegetable gardens. Help the government in getting the fortified food for the food baskets in the targeted PDS.
(C). Recommendations for private sector
-
(a)
Development of low cost high nutritious products using indigenous foods like nutribars, chews, cookies, etc. and training Self Help Groups to produce, promote and market such products.
-
(b)
As corporate social responsibility, corporates can adopt all TB patients in a few villages or districts and provide them with nutritional support or vouchers for a meal in some local hotels.
-
(c)
Create more local TB forums/Voice of Community, etc. who can help mobilize local resources in the form of sponsors who can support at least one TB patient with one meal a day till they complete their treatment.
-
(d)
Recommendations for academia, universities and research agencies, etc.
Generate evidence on the following areas: (i) Magnitude of the problem; (ii) Link between malnutrition and infectious diseases like TB and HIV; (iii) Randomized clinical trials to generate evidence on the effect of nutritional intervention for TB; Plan research activities to develop and use nutrient rich products; (iv) Develop nutritional and food security assessment, screening and training tools like checklists to identify vulnerable populations; and (v) Take steps to convert the evidence to policy.
-
(e)
Recommendations for UN agencies / World Food Programme: (i) Support pilot implementation projects and generate evidence; (ii) Work with National Governments at policy level; and (iii) Provide technical support and guidance.
Conclusions
The link between nutrition and tuberculosis is inextricable. The WHO End TB Strategy envisages a reduction in TB incidence of 75 per cent from current levels, by 202550. If India is to achieve this goal, the role of nutrition and food security as an important factor in both prevention and control of TB will need to be recognized and acted upon.
Acknowledgment
Authors thank Dr K.S. Sachdeva, ADDG, Central TB Division; Dr Kiran Rade, National Consultant, TB Epidemiologist, WHO/Central TB Division; Dr Shibu Balakrishnan, WHO-RNTCP Consultant, Kerala and Dr Jyothi Salve, WHO-RNTCP consultant, Mumbai for their inputs and comments in completing this review.
Footnotes
Conflicts of Interest: None.
References
- 1.Katona P, Katona-Apte J. The interaction between nutrition and infection. Clin Infect Dis. 2008;46:1582–8. doi: 10.1086/587658. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Global Tuberculosis Report. Geneva: 2014. [accessed on April 2, 2015]. Available from: http://apps.who.int/iris/bitstream/10665/137094/1/9789241564809_eng.pdf?ua=1 . [Google Scholar]
- 3.TB in India: RNTCP, TB care and Drug resistant TB. [accessed on January 2, 2014]. Available from: http://www.tbfacts.org/tb-india.html .
- 4.Murray CJL, Ortblad KF, Guinovart C, Lim SS, Wolock TM, Roberts DA, et al. Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:1005–70. doi: 10.1016/S0140-6736(14)60844-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dye C, Lonnroth K, Jaramillo E, Williams BG, Raviglione M. Trends in tuberculosis incidence and their determinants in 134 countries. Bull World Health Organ. 2009;87:683–91. doi: 10.2471/BLT.08.058453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta KB, Gupta R, Atreja A, Verma M, Vishvkarma S. Tuberculosis and nutrition. Lung India. 2009;26:9–16. doi: 10.4103/0970-2113.45198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sumpter C, Chandramohan D. Systematic review and meta-analysis of the associations between indoor air pollution and tuberculosis. Trop Med Int Health. 2013;18:101–8. doi: 10.1111/tmi.12013. [DOI] [PubMed] [Google Scholar]
- 8.Yen YF, Yen MY, Lin YS, Lin YP, Shih HC, Li LH, et al. Smoking increases risk of recurrence after successful anti-tuberculosis treatment: a population-based study. Int J Tuberc Lung Dis. 2014;18:492–8. doi: 10.5588/ijtld.13.0694. [DOI] [PubMed] [Google Scholar]
- 9.Lonnroth K, Williams BG, Stadlin S, Jaramillo E, Dye C. Alcohol use as a risk factor for tuberculosis - a systematic review. BMC Public Health. 2008;8:289. doi: 10.1186/1471-2458-8-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Global Health Risks. Mortality and burden of disease attributable to selected major risks. [accessed on January 2, 2015]. Available from: http://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf .
- 11.Global Nutrition Report 2014. Actions and Accountability. [accessed on January 5, 2015]. Available from: http://www.ifpri.org/sites/default/files/publications/gnr14.pdf .
- 12. [accessed on January 5, 2015];National Family Health Survey (NFHS-3) 2005-2006. India. 2 Available from: http://www.rchiips.org/nfhs/NFHS-3%20Data/VOL-2/Report-%20Volume-II%281632K%29.pdf . [Google Scholar]
- 13.Targetted Public Distribution System. World Food Programme. 2014. Nov, [accessed on June 25, 2015]. Available from: http://documents.wfp.org/stellent/groups/public/documents/communications/wfp271199.pdf .
- 14.Semba RD, Darnton-Hill, de Pee S. Addressing tuberculosis in the context of malnutrition and HIV coinfection. Food Nutr Bull. 2010;31:S345–64. [PubMed] [Google Scholar]
- 15.Lonnroth K, Williams BG, Cegielski P, Dye C. A consistent log-linear relationship between tuberculosis incidence and body mass index. Int J Epidemiol. 2010;39:149–55. doi: 10.1093/ije/dyp308. [DOI] [PubMed] [Google Scholar]
- 16.Bhargava A, Benedetti A, Oxlade O, Pai M, Menzies D. Undernutrition and the incidence of tuberculosis in India: National and subnational estimates of the population attributable fraction related to undernutrition. Natl Med J India. 2014;27:132–7. [PubMed] [Google Scholar]
- 17.Murray M, Oxlade O, Lin HH. Modeling social, environmental and biological determinants of tuberculosis. Int J Tuberc Lung Dis. 2011;15:S64–70. doi: 10.5588/ijtld.10.0535. [DOI] [PubMed] [Google Scholar]
- 18.WHO. Global Tuberculosis Report. Geneva: WHO; 2013. [accessed on January 6, 2015]. Available from: http://www.who.int/tb/publications/global_report/en . [Google Scholar]
- 19.The UNICEF India. Children and nutrition. [accessed on January 6, 2015]. Available from: http://www.unicef.org/india/children_2356.htm .
- 20.Bhargava A, Chatterjee M, Jain Y, Chatterjee B, Kataria A, Bhargava M, et al. Nutritional status of adult patients with pulmonary tuberculosis in rural Central India and its association with mortality. PLoS One. 2013;8:e77979. doi: 10.1371/journal.pone.0077979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Santha T, Garg R, Frieden T, Chandrasekaran V, Subramani R, Gopi P. Risk factors associated with default, failure and death among tuberculosis patients treated in a DOTS programme in Tiruvallur District, South India, 2000. Int J Tuberc Lung Dis. 2002;6:780–8. [PubMed] [Google Scholar]
- 22.Zachariah R, Spielmann MP, Harries AD, Salaniponi FML. Moderate to severe malnutrition in patients with tuberculosis is a risk factor associated with early death. Trans R Soc Trop Med Hyg. 2002;96:291–4. doi: 10.1016/s0035-9203(02)90103-3. [DOI] [PubMed] [Google Scholar]
- 23.Gustafson P, Gomes V, Vieira C, Samb B, Nauclér A, Aaby P, et al. Clinical predictors for death in HIV-positive and HIV-negative tuberculosis patients in Guinea-Bissau. Infection. 2007;35:69–80. doi: 10.1007/s15010-007-6090-3. [DOI] [PubMed] [Google Scholar]
- 24.Pednekar MS, Hakama M, Gupta PC. Tobacco use or body mass - do they predict tuberculosis mortality in Mumbai, India. Results from a population-based cohort study? PLoS One. 2012;7:e39443. doi: 10.1371/journal.pone.0039443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim HJ, Lee CH, Shin S, Lee JH, Kim YW, Chung HS, et al. The impact of nutritional deficit on mortality of in-patients with pulmonary tuberculosis. Int J Tuberc Lung Dis. 2010;14:79–85. [PubMed] [Google Scholar]
- 26.Khan A. Lack of weight gain and relapse risk in a large tuberculosis treatment trial. Am J Respir Crit Care Med. 2006;174:344–8. doi: 10.1164/rccm.200511-1834OC. [DOI] [PubMed] [Google Scholar]
- 27.Marais BJ, Gie RP, Hesseling AH, Beyers N. Adult-type pulmonary tuberculosis in children 10-14 years of age. Pediatr Infect Dis J. 2005;24:743–4. doi: 10.1097/01.inf.0000173305.04212.09. [DOI] [PubMed] [Google Scholar]
- 28.Bhat PG, Kumar AMV, Naik B, Satyanarayana S, Deepak KG, Nair SA, et al. Intensified tuberculosis case finding among malnourished children in nutritional rehabilitation centres of Karnataka, India: Missed opportunities. PLoS One. 2013;8:e84255. doi: 10.1371/journal.pone.0084255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Comstock GW, Palmer CE. Long-term results of BCG vaccination in the southern United States. Am Rev Respir Dis. 1966;93:171–83. doi: 10.1164/arrd.1966.93.2.171. [DOI] [PubMed] [Google Scholar]
- 30.Morán-Mendoza O, Marion SA, Elwood K, Patrick D, FitzGerald JM. Risk factors for developing tuberculosis: a 12-year follow-up of contacts of tuberculosis cases. Int J Tuberc Lung Dis. 2010;14:1112–9. [PubMed] [Google Scholar]
- 31.Hicks RM, Padayatchi N, Shah NS, Wolf A, Werner L, Sunkari VB. Malnutrition associated with unfavorable outcome and death among South African MDR-TB and HIV co-infected children. Int J Tuberc Lung Dis. 2014;18:1074–83. doi: 10.5588/ijtld.14.0231. [DOI] [PubMed] [Google Scholar]
- 32.Ramachandran G, Kumar AKH, Bhavani PK, Poorana Gangadevi N, Sekar L, Vijayasekaran D, et al. Age, nutritional status and INH acetylator status affect pharmacokinetics of anti-tuberculosis drugs in children. Int J Tuberc Lung Dis. 2013;17:800–6. doi: 10.5588/ijtld.12.0628. [DOI] [PubMed] [Google Scholar]
- 33.Pande JN, Singh SP, Khilnani GC, Khilnani S, Tandon RK. Risk factors for hepatotoxicity from antituberculosis drugs: a case-control study. Thorax. 1996;51:132–6. doi: 10.1136/thx.51.2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dye C, Bourdin Trunz B, Lonnroth K, Roglic G, Williams BG. Nutrition, diabetes and tuberculosis in the epidemiological transition. PLoS One. 2011;6:e21161. doi: 10.1371/journal.pone.0021161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Calder PC, Jackson AA. Undernutrition, infection and immune function. Nutr Res Rev. 2000;13:3–29. doi: 10.1079/095442200108728981. [DOI] [PubMed] [Google Scholar]
- 36.Tuberculosis Research Centre. A concurrent comparison of home and sanatorium treatment of tuberculosis in south India. Bull World Health Organ. 1959;21:51–144. [PMC free article] [PubMed] [Google Scholar]
- 37.Schwenk A, Macallan DC. Tuberculosis, malnutrition and wasting. Curr Opin Clin Nutr Metab Care. 2000;3:285–91. doi: 10.1097/00075197-200007000-00008. [DOI] [PubMed] [Google Scholar]
- 38.Sudarsanam TD, John J, Kang G, Mahendri V, Gerrior J, Franciosa M, et al. Pilot randomized trial of nutritional supplementation in patients with tuberculosis and HIV-tuberculosis coinfection receiving directly observed short-course chemotherapy for tuberculosis. Trop Med Int Health. 2011;16:699–706. doi: 10.1111/j.1365-3156.2011.02761.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jahnavi G, Sudha CH. Randomised controlled trial of food supplements in patients with newly diagnosed tuberculosis and wasting. Singapore Med J. 2010;51:957–62. [PubMed] [Google Scholar]
- 40.Swaminathan S, Padmapriyadarsini C, Yoojin L, Sukumar B, Iliayas S, Karthipriya J, et al. Nutritional supplementation in HIV-infected individuals in South India: a prospective interventional study. Clin Infect Dis. 2010;51:51–7. doi: 10.1086/653111. [DOI] [PubMed] [Google Scholar]
- 41.Lodha R, Mukherjee A, Singh V, Singh S, Friis H. Effect of micronutrient supplementation on treatment outcomes in children with intrathoracic tuberculosis: a randomized controlled trial. Am J Clin Nutr. 2014;100:1287–97. doi: 10.3945/ajcn.113.082255. [DOI] [PubMed] [Google Scholar]
- 42.Sinclair D, Abba K, Sudarsanam TD, Grobler L, Volmink J. Nutritional supplements for people being treated for active Tuberculosis. Cochrane Database Sys Rev. 2011;(II):CD006086. doi: 10.1002/14651858.CD006086.pub3. [DOI] [PubMed] [Google Scholar]
- 43.de Pees S, Grede N, Mehra D, Bloem MW. The enabling effect of food assistance in improving adherence and/or treatment completion for antiretroviral therapy and tuberculosis treatment: a literature review. AIDS Behav. 2014;18(Suppl 5):S531–41. doi: 10.1007/s10461-014-0730-2. [DOI] [PubMed] [Google Scholar]
- 44.Nutritional care and support for patients with tuberculosis. Guideline: World Health Organization. 2013. [accessed on June 7, 2015]. Available from: http://apps.who.int/iris/bitstream/10665/94836/1/9789241506410_eng.pdf . [PubMed]
- 45.National Food Security Bill, 2013. [accessed on June 7,2015]. Available from: http://indiacode.nic.in/acts-in-pdf/202013.pdf .
- 46.Commissionerate of Land Reforms. Chief Minister's Uzhavar Pathukappu Thittam 2011. [accessed on May 23, 2015]. Available from: http://www.landreforms.tn.gov.in/UPT.html .
- 47.REACH, Public-Private Mix. [accessed on May 22, 2015]. Available from: http://www.reachtbnetwork.org/public-private-mix/
- 48.KCBC Health Commission & CHAI Kerala. [accessed on May 20, 2015]. Available from: http://www.chaikerala.com/activities.php .
- 49.Multi-drug resistant TB patients to get food support from BMC. [accessed on January 31, 2015]. Available from: http://www.dnaindia.com/mumbai/report-multi-drug-resistant-tb-patients-to-get-food-supportfrom-bmc-2056960 .
- 50.The End TB Strategy. World Health Organization. [accessed on June 10, 2016]. Available from: www.who.int/tb/post2015_TBstrategy.pdf .