Abstract
Introduction
Obesity remains a significant threat to the current and long-term health of U.S. adolescents. The authors developed county-level estimates of adolescent obesity for the contiguous U.S., and then explored the association between 23 conceptually derived area-based correlates of adolescent obesity and ecologic obesity prevalence.
Methods
Multilevel small area regression methods applied to the 2007 and 2011–2012 National Survey of Children’s Health produced county-level obesity prevalence estimates for children aged 10–17 years. Exploratory multivariable Bayesian regression estimated the cross-sectional association between nutrition, activity, and macrosocial characteristics of counties and states, and county-level obesity prevalence. All analyses were conducted in 2015.
Results
Adolescent obesity varies geographically with clusters of high prevalence in the Deep South and Southern Appalachian regions. Geographic disparities and clustering in observed data are largely explained by hypothesized area-based variables. In adjusted models, activity environment, but not nutrition environment variables were associated with county-level obesity prevalence. County violent crime was associated with higher obesity whereas recreational facility density was associated with lower obesity. Measures of the macrosocial and relational domain, including community SES, community health, and social marginalization, were the strongest correlates of county-level obesity.
Conclusions
County-level estimates of adolescent obesity demonstrate notable geographic disparities, which are largely explained by conceptually derived area-based contextual measures. This ecologic exploratory study highlights the importance of taking a multidimensional approach to understanding the social and community context in which adolescents make obesity-relevant behavioral choices.
Introduction
Obesity remains a significant threat to the current and long-term health of U.S. adolescents. The prevalence of obesity among those aged 12–19 years exceeded 20% in 2011–2012.1 Obesity in adolescence is associated with a higher prevalence of cardiometabolic risk factors2; impeded social and emotional development3,4; increased risk of severe obesity in adulthood5; comorbidities in adulthood including diabetes, hypertension, asthma, mobility limitations, and sleep apnea6; and lower adult educational attainment and income status.7 Increasing autonomy during adolescence can influence the development of health behaviors that likely persist into adulthood, making this period of time particularly salient in the development and implementation of obesity prevention interventions.8
Growing recognition of the importance of social and environmental context in shaping individual choice and behavior has broadened the focus of obesity research and intervention beyond individual behavior alone.9–12 Ecologic models of health behavior posit that choices made by individuals are the result of a constant interplay between intrapersonal factors and features of the social, organizational, and community environments within which they are situated.13 It is hypothesized that the proliferation of “obesogenic” environments—where energy-dense and nutrient-poor foods are widely affordable and available, and transportation options and leisure time activities are often sedentary—has drastically altered the landscapes in which adolescents make dietary and physical activity–related choices.14 Further, persistent socioeconomic, ethnic, racial, and geographic disparities in adolescent and adult obesity prevalence have underscored the need to better understand how environmental features may manifest differently across populations.15–17
Harrison et al.18 propose a conceptual framework for understanding obesity that is adaptable to multiple stages of development from infancy through adolescence. The framework conceives of forces at multiple levels (cell, child, family, community, and culture) and across five domains (nutrition-related opportunities and resources, nutrition-related practices, activity-related opportunities and resources, activity-related practices, and personal and relational attributes).
This paper aimed to accomplish two tasks. First, small area estimates of county-level adolescent obesity for the contiguous U.S. were produced. Second, the authors tested the ecologic association between county-level adolescent obesity and multiple hypothesized obesogenic factors drawn from the “community” level of Harrison and colleagues’ multidimensional framework in order to characterize these relationships in a geographically diverse, population-based sample.
Methods
Data Sample
The National Survey of Children’s Health (NSCH)19 is a nationally representative telephone-based survey assessing parent-reported physical, mental, behavioral, and environmental health status of children from birth through age 17 years. To maximize sample size for small area analysis, data were pooled from the 2007 and 2011–2012 NSCH surveys in which there was an average of 1,800 respondents aged 0–17 years in every state and the District of Columbia. The interview completion rate, one marker of non-response, was 66% in 2007, and 54% and 41% for landline and cell phone sample frames, respectively, in 2011–2012.20 Respondents were weighted to account for non-response bias.
Parent-reported child weight and height were used to calculate BMI for children aged 10–17 years.21 Obesity was defined as BMI (weight [kg]/height [m2]) at or above the 95th percentile for children of the same sex and age.22,23 The post-stratification approach described below is optimized with fewer strata, and thus individual children were coarsely categorized by age (10–14 years, 15–17 years), sex, and race (white, non-white), producing eight demographic strata. These variables plus survey design weights were abstracted for analysis.
Statistical Analysis
There are two general approaches to producing small area estimates of disease prevalence: design-based sampling and model-based estimation.24 The NSCH uses a design-based approach drawing sufficiently large samples to permit statistically valid estimation at the state level. However, design-based approaches are expensive, and likely cost prohibitive at the scale of U.S. counties. A growing methodologic literature supports model-based estimation of population parameters for subareas from population-based surveys. To accomplish their first aim, the authors adapted a multilevel regression and post-stratification approach for the estimation of county-level obesity prevalence.25,26 Regression model-based small area estimates have been demonstrated to provide valid county-level estimates of chronic disease outcomes derived from state-level design-based surveys.27,28
The data preparation and modeling approach is more completely described in Appendix A; briefly, it consisted of three steps. First, a three-level mixed effects regression model was fit to individuals in NSCH adjusting for age, race, sex, survey year, county child poverty rate, and Census region. Random county and state intercepts nested individuals within counties, which were nested within states, and random slopes for age, race, and sex were estimated at the state level. This approach produced state-specific estimates of the relationship of individual age, race, and sex with obesity, while also allowing that county obesity prevalence may vary from the state average. Second, for counties without estimates (e.g., no NSCH respondents), the authors imputed county-level random intercepts as the average of geographically contiguous county intercepts. Finally, county, age-, race-, and sex-stratified population count estimates from the 2008–2012 American Community Survey were merged with the county and state random effects, and age-, race-, and sex-specific coefficients to produce post-stratified obesity prevalence for each county. Small area uncertainty was estimated by summarizing 1,000 draws from distributions described by model coefficients and SEs. To assess internal validity of small area estimates, two reference standards were defined: the design-based estimates for counties with a significant number of NSCH respondents (n>50), and the design-based estimates at the state level. Regression model-based estimates were compared with design-based reference values.29
In total, 23 county- and state-level variables that conceptually map onto the five “community”-level domains in the Harrison et al.18 framework were identified (Table 1 shows variable definitions and data sources). Harrison and colleagues’ “personal and relational attributes” domain was modified to be “macrosocial and relational,” reflecting the community, rather than individual-level focus of this analysis. Control variables including region, metropolitan status, and county-level population change were also included.
Table 1.
Definition and Distribution of Ecologic Measures of Obesogenic Environments
| Ecological correlates of childhood obesity | Selected variables | Data source (year of measure) | Unit of geography | Mean | SD | Min | Max | |
|---|---|---|---|---|---|---|---|---|
| Domain | Sub-domain | |||||||
| Nutrition-related opportunities and resources | ||||||||
| Healthcare system structure | Pediatricians and primary care providers per 10,000 pop | U.S. DHHS and HRSA Area Health Resources File (2010) | County | 3.04 | 2.2 | 0 | 30.76 | |
| Hospitals per 10,000 pop | U.S. DHHS and HRSA Area Health Resources File (2010) | County | 0.58 | 0.91 | 0 | 9.61 | ||
| Uninsured children (%) | U.S. Census Bureau, Small Area Health Insurance Estimates (2009) | County | 8% | 5% | 2% | 36% | ||
| Breastfeeding practices | Infants ever breastfed (%) | CDC Breastfeeding Report Card (2009) | State | 71% | 9% | 47% | 90% | |
| State-mandated employer lactation support (1/0) | CDC Breastfeeding Report Card (2009) | State | 26% | |||||
| Accessibility/proximity of food outlets | Low access to food store (%)a | USDA Food Environment Atlas (2010) | County | 6% | 4% | 0% | 36% | |
| Grocery stores per 1,000 pop | USDA Food Environment Atlas (2010) | County | 0.29 | 0.22 | 0 | 3.23 | ||
| Nutrition-related practices | ||||||||
| Community food restriction/bans | Soda price (ratio of local price to national price) | USDA Food Environment Atlas (2010) | County | 1.04 | 0.06 | 0.93 | 1.32 | |
| Peer food choices | Adults with low fruit and vegetable intake (%)b | CDC Behavioral Risk Factor Surveillance System (2011) | State | 32% | 4% | 23% | 42% | |
| Activity-related opportunity and resources | ||||||||
| Crime rates | Violent crime rate per 10,000 pop | FBI Uniform Crime Reporting Program Data: County-level Detailed Arrest and Offense Data (2009) | County | 4.59 | 3.03 | 0 | 48.89 | |
| Access to recreation facilities | Natural amenity indexc | USDA Economic Research Service (1999) | County | 3.49 | 1.04 | 1 | 7 | |
| Recreation and fitness facility per 1,000 pop | USDA Food Environment Atlas, derived from U.S. Census Bureau, County Business Patterns (2007) | County | 0.09 | 0.09 | 0 | 1.49 | ||
| School activity requirements | State mandated school activity policy (1/0)d | Shape of the Nation Report (2012) | State | 80% | ||||
| Activity-related practices | ||||||||
| Local employment practice | Adults walking to work (%) | American Community Survey (2006–2010) | County | 3% | 3% | 0% | 34% | |
| Leisure time activity and media usage | Adolescents use electronics >1 hr/day (%) | National Survey of Children’s Health (2011–2012) | State | 34% | 4% | 25% | 44% | |
| Macrosocial and relational | ||||||||
| Community SES | Poverty rate (%) | USDA Food Environment Atlas, derived from U.S. Census (2010) | County | 17% | 6% | 3% | 50% | |
| Persistent child poverty (1/0)e | USDA Food Environment Atlas, derived from U.S. Census (2010) | County | 23% | |||||
| Food insecurity | Child food insecurity ratef | Map the Meal Gap 2011- Feeding America (2009) | County | 0.26 | 0.06 | 0.07 | 0.52 | |
| Social marginalization | Gini index of income inequality | American Community Survey (2006–2010) | County | 0.43 | 0.04 | 0.21 | 0.64 | |
| Black-white racial segregation (H Index) | U.S. Census Bureau (2010) | County | 0.06 | 0.08 | 0 | 0.66 | ||
| Community health/disease | Adult diabetes prevalence (%) | USDA Food Environment Atlas, derived from CDC Behavioral Risk Factor Surveillance System (2009) | County | 10% | 2% | 3% | 20% | |
| Place-based characteristics | ||||||||
| Population loss (1/0)g | USDA Food Environment Atlas, derived from U.S. Census (2010) | County | 19% | |||||
| Metropolitan area (1/0) | USDA Food Environment Atlas, derived from U.S. Census (2010) | County | 37% | |||||
| Census region | Northeast | U.S. Census Bureau (2010) | State | 7% | ||||
| Midwest | 34% | |||||||
| South | 46% | |||||||
| West | 13% | |||||||
Low food access is living >1 mile from supermarket in metropolitan area or >10 miles in rural area; our measure is the average of: % children with low access; % population with both low access and low income; and % of population with low access and no vehicle for each county.
% of adults who report eating less than 1 serving daily of fruit and vegetables.
The Natural Amenity Index is created by USDA Economic Research Service and ranges from 1 to 7, with higher values indicating higher amenities. It captures climate, topography, and water area that reflect environmental qualities most people prefer.
State mandated physical activity indicates whether states have two or more of the following: physical education mandated in middle school or in high school; or weekly physical activity mandated in middle school or high school.
Counties where the poverty rate of related children under age 18 was 20% or more over the last 30 years, as measured by 1980, 1990, and 2000 decennial censuses and the 2007–2011 American Community Survey 5-year estimates; where 1=persistent poverty and 0=otherwise
County level child food insecurity prevalence was estimated by Gunderson et al. for Feeding America (Gundersen CE. Waxman E, Engelhard, Brown J. Map the Meal Gap 2011: A Report on County Level Food Insecurity and Food Cost in the United States in 2009. Feeding America, 2011).
Counties where the number of residents declined both between 1980 and 1990 and between 1990 and 2000, where 1=population-loss county, 0=otherwise.
HRSA, Health Resources and Services Administration; CDC, Centers for Disease Control and Prevention; USDA, U.S. Department of Agriculture; FBI, Federal Bureau of Investigation
The associations between these candidate obesogenic factors and obesity prevalence were estimated with multilevel linear regression models, with counties nested within states. All continuous variables were standardized to make model coefficients interpretable as the change in obesity prevalence for each 1-SD change in the predictor. In settings with multiple candidate predictors, there is concern for variable collinearity and false positive associations due to multiple comparisons. Bayesian model shrinkage approaches permit estimation of multiple effects with reduced concern for variance inflation (Appendix B has details of the Bayesian model approach).30,31
Geographic patterns of disease can be summarized using aspatial measures of intergroup disparity including Theil’s Index, Mean Log Deviation and the Index of Disparity,32,33 and spatial measures of clustering including the global Moran’s I statistic for spatial autocorrelations.34 Measures of relative health disparity in unordered groups, such as geographic units, characterize the relative gap between highest and lowest prevalence counties, with larger values indicating greater intercounty disparity (additional details in Appendix A).32 Disparity measures were calculated on residuals from an empty model (intercept only, no covariates, indicative of crude observed disparities) and on the fully adjusted model (indicative of residual disparity above and beyond that accounted for by controlled variables). The relative change between the two estimates quantifies the proportion of the observed geographic disparity “explained” by included covariates. To estimate the overall degree of geographic clustering of high and low obesity prevalence among counties, Moran’s I statistics were calculated for the residuals from the empty and adjusted models. The Moran’s I quantifies the degree to which spatially contiguous counties have similar obesity prevalence (additional details in Appendix A). The proportional change in the Moran’s I of residuals from the empty (intercept only) versus the adjusted models characterizes the degree of total spatial clustering explained by controlled variables.
All analysis was carried out in 2015 using R, version 3.1 and maps were prepared in ArcGIS, version 10.1. Small area estimation required access to county identifiers, which are not part of the public use data files from NSCH. Restricted-access NSCH files that included respondent county code were analyzed through the Research Data Center of the Centers for Disease Control and Prevention. The study was reviewed by the Emory University IRB.
Results
There were 42,390 and 39,381 respondents aged 10–17 years with non-missing BMI from the 3,109 eligible counties in NSCH surveys from 2007 and 2011–2012, respectively. The survey design-based estimate of adolescent obesity in the target counties was 16.4% in 2007 and 15.7% in 2011–2012, with lower prevalence in older adolescents, girls, and whites (Table 2). Model-estimated county-level obesity prevalence is mapped in Figure 1. Adolescent obesity was greatest in the Deep South and Central Appalachia, the San Joaquin Valley in California, as well as in pockets in the four corners region, Oklahoma, and the Northern Plains. Modeled obesity prevalence uncertainty is mapped in Appendix Figure 1, where higher SEs are clustered along the Mississippi River valley, Gulf Coast, and Upper Peninsula of Michigan. In counties with ≥50 NSCH respondents, the Spearman correlation coefficient for design-based reference values versus model-based prevalence was r =0.95 (p<0.001). Model-estimated county prevalence averaged to the state level correlated with state-level design-based reference values (r =0.93, p<0.001).
Table 2.
Obesity Prevalence in National Survey of Children’s Health (NSCH)
| Eligible children, 10–17 years old | NSCH 2007 | NSCH 2011–2012 | ||||
|---|---|---|---|---|---|---|
| N | % Obese | SE | N | % Obese | SE | |
| Total | 42,390 | 16.4 | 0.49 | 39,381 | 15.7 | 0.42 |
| 10–14 years old | 23,894 | 18.3 | 0.65 | 23,091 | 18.0 | 0.57 |
| 15–17 years old | 18,496 | 13.3 | 0.72 | 16,290 | 12.1 | 0.61 |
| Male | 22,098 | 19.2 | 0.7 | 18,838 | 18.4 | 0.61 |
| Female | 20,292 | 13.5 | 0.68 | 20,543 | 12.9 | 0.58 |
| White | 30,374 | 14.0 | 0.55 | 27,482 | 13.6 | 0.46 |
| Non-white | 12,016 | 21.3 | 0.98 | 11,899 | 19.9 | 0.86 |
Note: N=3,109 target counties in lower 48 states and District of Columbia
Figure 1.
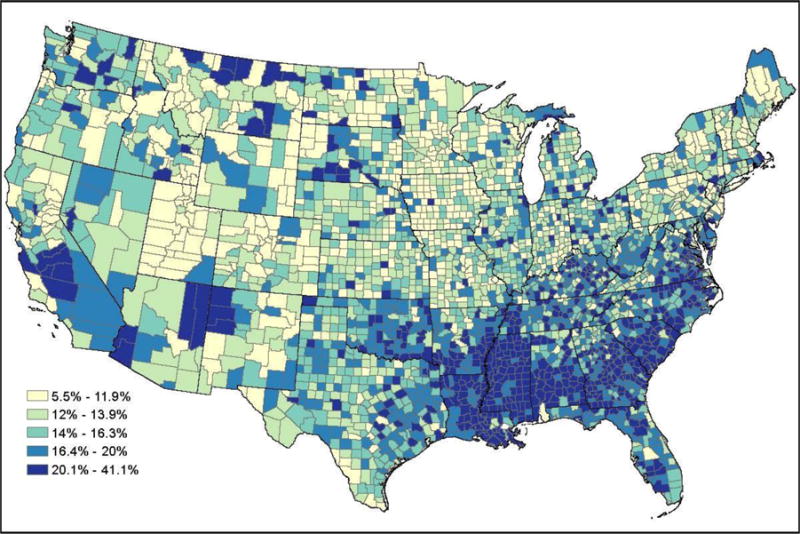
Model-estimated obesity prevalence for children 10–17 years old in U.S. counties, National Survey of Children’s Health 2007 and 2011–2012.
The distributions of county- and state-level variables are summarized in Table 1. In adjusted models (Table 3), none of the nine variables measuring the “nutrition-related opportunities and resources” or “nutrition-related practices” domains were significantly associated with county-level obesity. In the activity-related domains, violent crime rates were positively associated with obesity prevalence, whereas natural amenity index and the proportion of adults walking to work were inversely associated with obesity prevalence. Five of six variables in the “macrosocial and relational” domain were significant. The two indicators of community SES, poverty rate and persistent county poverty, were associated with higher obesity prevalence, but the food insecurity measure was inversely correlated with obesity. The Gini index of income inequality was not significant, but the other indicator of social marginalization, black–white segregation index, was associated with higher obesity prevalence. Finally, as an indicator of community health and disease, the prevalence of adults with Type 2 diabetes was positively associated with adolescent obesity prevalence.
Table 3.
Exploratory Model Results for Selected Ecologic Obesogenic Factors and Adolescent Obesity Prevalence in U.S. Counties
| Harrison, et al. Ecological correlates of childhood obesity | Selected variables | Adjusted Bayesian model | |||
|---|---|---|---|---|---|
| Domain | Sub-domain | β | 95% CI | ||
| (Intercept) | 15.82 | 14.77 | 16.82 | ||
| Nutrition-related opportunities and resources | |||||
| Healthcare system structure | Pediatricians and primary care providers densitya | −0.05 | −0.21 | 0.11 | |
| Hospitals densitya | −0.05 | −0.21 | 0.11 | ||
| Uninsured children (%)a | 0.02 | −0.20 | 0.24 | ||
| Breastfeeding practices | Infants ever breastfed (%)a | 0.04 | −0.74 | 0.87 | |
| State-mandated employer lactation support (binary)b | −0.29 | −1.21 | 0.59 | ||
| Accessibility/proximity of food outlets | Low access to food store (%)a | 0.12 | −0.03 | 0.26 | |
| Grocery store densitya | −0.14 | −0.30 | 0.01 | ||
| Nutrition-related practices | |||||
| Community food restriction/bans | Soda price (ratio of local price to national price)a | 0.15 | −0.10 | 0.39 | |
| Peer food choices | Adults with low fruit and vegetable intake (%)a | 0.25 | −0.43 | 0.99 | |
| Activity-related opportunity and resources | |||||
| Crime rates | Violent crime ratea | 0.28 | 0.12 | 0.45 | |
| Access to recreation facilities | Natural amenity indexa | −0.39 | −0.59 | −0.19 | |
| Recreation and fitness facility densitya | 0.00 | −0.13 | 0.14 | ||
| School activity requirements | State mandated school activity policy (binary)b | −0.03 | −0.91 | 0.90 | |
| Activity-related practices | |||||
| Local employment practice | Adults walking to work (%)a | −0.22 | −0.38 | −0.05 | |
| Leisure time activity and media usage | Adolescents use electronics >1 hr/day (%)a | 0.14 | −0.46 | 0.80 | |
| Macrosocial and relational | |||||
| Community SES | Poverty rate (%)a | 1.44 | 1.19 | 1.70 | |
| Persistent child poverty (binary)b | 0.46 | 0.07 | 0.87 | ||
| Food insecurity | Child food insecurity ratea | −0.60 | −0.84 | −0.38 | |
| Social marginalization | Gini index of income inequalitya | −0.10 | −0.26 | 0.06 | |
| Black-white racial segregationa | 0.96 | 0.80 | 1.12 | ||
| Community health/disease | Adult diabetes prevalence (%)a | 1.14 | 0.93 | 1.35 | |
| Place-based characteristics | |||||
| Population loss (binary)b | −0.37 | −0.74 | −0.01 | ||
| Metropolitan area (binary)b | 0.20 | −0.12 | 0.53 | ||
| Northeast | ref | ||||
| Midwest | −0.10 | −1.01 | 0.78 | ||
| South | 0.45 | −0.48 | 1.54 | ||
| West | 0.16 | −0.79 | 1.11 | ||
| Variance componentsc | sigma – state | 1.86 | 1.46 | 2.37 | |
| sigma – residual | 3.58 | 3.50 | 3.67 | ||
| ICC | 0.34 | 0.29 | 0.39 | ||
| AIC/DIC | 16812 | ||||
Notes: Boldface indicates statistical significance (p<0.05)
N=3,109 counties nested within 48 states and District of Columbia
β-coefficients represent the change in county obesity prevalence per 1-SD change in the predictor.
β-coefficients represent the change in county obesity prevalence for having versus not having the binary indicator.
Variance components and fit statistics from the empty model (intercept only): sigma (state): 3.27; sigma(residual): 4.06; ICC: 0.45 (95% CI 0.40,0.49); AIC: 17705.
ICC, Intra-cluster Correlation Coefficient; AIC, Akaike Information Criterion; DIC, Deviance Information Criterion_
The Moran’s I statistic for global spatial autocorrelation of the residuals from the empty (intercept-only) model was 0.47 (p<0.001) suggesting a moderate degree of spatial clustering of obesity prevalence. By contrast, the Moran’s I for the residuals from the adjusted model was 0.05 (p<0.001), suggesting that very little spatial clustering remains above and beyond that explained by predictor variables. The Index of Disparity was 37.8 in the empty (intercept-only) model, and 25.8 in the adjusted model, representing a 32% reduction. The reduction in relative disparity after adjustment for covariates was 44% and 47% using Mean Log Deviation and Theil’s Index respectively (Appendix Table 1). Thus, from one third to one half of the total geographic disparity in county obesity prevalence was explained by included variables.
Discussion
There are substantial geographic disparities and geographic clustering of adolescent obesity prevalence among counties in the contiguous U.S. Building on an existing conceptual framework for the determinants of childhood obesity at various stages of child development, the authors used an exploratory modeling process to contrast candidate obesogenic correlates of county-level adolescent obesity prevalence. Together, these correlates explained one third to one half of the geographic disparity and nearly all geographic clustering. The strongest predictors of county-level adolescent obesity prevalence include community health status, proxied as the percentage of adults with prevalent Type 2 diabetes, and measures of community SES (child poverty rate) and social marginalization (segregation index). Variables from the activity-related opportunities, resources, and practices domains were also significantly associated with county-level adolescent obesity. By contrast, no variables from the nutrition opportunities, resources, or practices domains were significant predictors of county-level adolescent obesity.
Existing studies have taken varied approaches to conceptualizing and measuring obesogenic environments, including the examination of socioeconomic environments, local food environments, and physical and built environments.35–39 Assessing measures similar to those included in the “macrosocial and relational” domain explored in this study, Rossen and Talih40 demonstrated that racial and ethnic disparities in adolescent obesity prevalence were significantly attenuated after accounting for fundamental neighborhood-level socioeconomic and demographic features, including indices of segregation and income inequality. However, the pathways through which such “fundamental causes” influence obesity are not fully understood. Disparities in adolescent obesity have been attributed to a higher exposure among disadvantaged populations to obesogenic environments, such as limited access to healthy foods and resources for physical activity.41–44 Yet, this study indicates that factors like persistent poverty and segregation remain significant even after accounting for features of the nutrition and activity environments. The results also point to an inverse association between ecologic child food insecurity rates and obesity prevalence. This is in contrast to some findings that at the individual level, food insecurity has been associated with higher obesity risk.45,46 The findings of ecologic correlations point to possible sources of contextual influence on obesity prevalence, but require further examination of mediating pathways and multilevel mechanisms through which area-based disadvantage could influence obesity.
Research on the associations among the local food environment, the physical and built environment, and obesity has produced mixed results. A recent systematic review of the literature on local food environments identified predominantly null associations, yet highlighted trends toward inverse associations between supermarket availability and obesity, and positive associations between fast food availability and obesity.36 It is possible that mixed results for the importance of food environment reflect measurement error in that most studies rely on administrative lists of food stores as proxies for food accessibility without explicit attention to food quality or cost, each of which could affect nutrition independent of proximity.47 As is the case with the current study, more-consistent results have been found for the physical and built environment correlates of obesity prevalence, including inverse associations between adolescent obesity and the presence of recreation centers, parks and playgrounds, and sidewalks and walking paths.38,39,48,49 This study also provides further evidence in support of the emerging relationship between area-based crime rates and adolescent physical activity and obesity prevalence.49,50 Overall, these findings are consistent with existing evidence on activity environments compared to nutrition environments.
This study helps to advance understanding of environmental correlates of, and disparities in, adolescent obesity prevalence in several ways. First, the geographic patterns of obesity prevalence among adolescents track closely with geography of adult obesity,51 suggesting common local variation in correlates of obesity in different life stages, and highlighting the public health importance of addressing obesity in a life course framework.52 Much of the extant literature has used localized samples, which occasionally provide richer local measurement, but have limited generalizability.36,38 The national scope of the adolescent obesity epidemic necessitates the identification of more widely applicable factors that may be intervened upon to facilitate population level change. In this ecologic study, characterizing obesity at the county level allowed for explicit acknowledgement of important within-state variations in both predictors and obesity prevalence.
This study also contributes to the growing body of literature recognizing the complexity of environmental influences on obesity. The number of studies simultaneously examining multiple domains of the obesogenic environments, including the food, built, social, and economic environments of adolescents, remains limited.37,49,53–55 The wide array of measures from multiple diverse domains included in this study explained most of the spatial clustering and one third to one half of the geographic disparity in obesity, underscoring the importance of comprehensive approaches to exploring environmental correlates of obesity.
Limitations
This study design was descriptive and exploratory, and thus limited in several ways. First, the findings are dependent on both the validity of parent-reported height and weight in the NSCH, and on the assumptions of small area estimation methods. Although parent-reported height and weight may be systematically biased for younger children, estimates of BMI for children aged 10 years older are more reliable.56,57 There is also evidence for geographic variation in the accuracy of self-reported height and weight among adults,58 although it is unclear whether this is true for parent-reported values of children. However, the broad geographic patterns observed are consistent with those obtained from other data sources for adolescents59 and adults.60
This study design is ecologic, and reported obesity prevalence is marginal (e.g., not race-, sex- or age-specific). The marginal nature of the prevalence estimates limits the opportunity to comment on race, gender, or age differences in the importance of area-based factors, but the small area estimation techniques required aggregation across demographic strata to produce valid county-level estimates. The ecologic design also limited examination of behavioral mediators between environment and obesity. However, both the ecologic design and marginal prevalence lend themselves to the goal of characterizing the population burden of adolescent obesity in places, and characterizing places with higher or lower obesity prevalence.
Finally, it is likely that area-based factors for units other than counties (e.g., neighborhoods, cities) affect obesity prevalence, although it has been argued that counties represent the smallest analytic unit with useful policy implications.61,62 Variable selection was limited by conceptual linkage with the Harrison et al.18 framework, and availability at the county or state scale; missing variables could result in biased estimates or residual unexplained geographic disparities.
Conclusions
Nationwide small area estimates of adolescent obesity prevalence demonstrated substantial geographic variation and patterning. The domain most strongly associated with county-level obesity prevalence was the “macrosocial and relational” domain, including community SES, community health, and social marginalization. By applying a multidimensional conceptual model of the determinants of childhood obesity, no ecologic correlation between nutrition-related factors and obesity prevalence was identified, but there were some associations between activity-related factors and obesity prevalence, including county-level crime rates, recreational facility density, and prevalence of adults walking to work. These results highlight the importance of multidimensional thinking in developing public health responses to the obesity epidemic. Although individual behaviors are likely intervening variables, the social and community context in which adolescents are exposed to norms and develop behaviors may need additional etiologic and interventional focus to meaningfully reduce geographic disparities in obesity prevalence.
Supplementary Material
Acknowledgments
Dr. Kramer was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of NIH under Award Number K01HD074726. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. http://dx.doi.org/10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Skinner AC, Perrin EM, Moss LA, Skelton JA. Cardiometabolic Risks and Severity of Obesity in Children and Young Adults. N Engl J Med. 2015;373(14):1307–1317. doi: 10.1056/NEJMoa1502821. http://dx.doi.org/10.1056/NEJMoa1502821. [DOI] [PubMed] [Google Scholar]
- 3.Must A, Strauss RS. Risks and consequences of childhood and adolescent obesity. Int J Obes Relat Metab Disord. 1999;23(Suppl 2):S2–S11. doi: 10.1038/sj.ijo.0800852. http://dx.doi.org/10.1038/sj.ijo.0800852. [DOI] [PubMed] [Google Scholar]
- 4.Pearce MJ, Boergers J, Prinstein MJ. Adolescent Obesity, Overt and Relational Peer Victimization, and Romantic Relationships. Obes Res. 2002;10(5):386–393. doi: 10.1038/oby.2002.53. http://dx.doi.org/10.1038/oby.2002.53. [DOI] [PubMed] [Google Scholar]
- 5.The NS. Suchindran C, North KE, Popkin BM, Gordon-Larsen P. Association of adolescent obesity with risk of severe obesity in adulthood. JAMA. 2010;304(18):2042–2047. doi: 10.1001/jama.2010.1635. http://dx.doi.org/10.1001/jama.2010.1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Inge TH, King WC, Jenkins TM, et al. The effect of obesity in adolescence on adult health status. Pediatrics. 2013;132(6):1098–1104. doi: 10.1542/peds.2013-2185. http://dx.doi.org/10.1542/peds.2013-2185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gortmaker SL, Must A, Perrin JM, Sobol AM, Dietz WH. Social and economic consequences of overweight in adolescence and young adulthood. N Engl J Med. 1993;329(14):1008–1012. doi: 10.1056/NEJM199309303291406. http://dx.doi.org/10.1056/NEJM199309303291406. [DOI] [PubMed] [Google Scholar]
- 8.Story M, Neumark-Sztainer D, French S. Individual and Environmental Influences on Adolescent Eating Behaviors. J Am Diet Assoc. 2002;102(3 Suppl):S40–S51. doi: 10.1016/s0002-8223(02)90421-9. http://dx.doi.org/10.1016/S0002-8223(02)90421-9. [DOI] [PubMed] [Google Scholar]
- 9.Egger G, Swinburn B. An “ecological” approach to the obesity pandemic. BMJ. 1997;315(7106):477–480. doi: 10.1136/bmj.315.7106.477. http://dx.doi.org/10.1136/bmj.315.7106.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sallis JF, Glanz K. Physical Activity and Food Environments: Solutions to the Obesity Epidemic. Milbank Q. 2009;87(1):123–154. doi: 10.1111/j.1468-0009.2009.00550.x. http://dx.doi.org/10.1111/j.1468-0009.2009.00550.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brownell KD, Schwartz MB, Puhl RM, Henderson KE, Harris JL. The Need for Bold Action to Prevent Adolescent Obesity. J Adolesc Heal. 2009;45(3 Suppl):S8–S17. doi: 10.1016/j.jadohealth.2009.03.004. http://dx.doi.org/10.1016/j.jadohealth.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 12.Slack T, Myers CA, Martin CK, Heymsfield SB. The geographic concentration of U.S. adult obesity prevalence and associated social, economic, and environmental factors. Obesity. 2014;22(3):868–874. doi: 10.1002/oby.20502. http://dx.doi.org/10.1002/oby.20502. [DOI] [PubMed] [Google Scholar]
- 13.Sallis JF, Owen N, Fisher E. Ecological Models of Health behavior. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. 4th. California: Jossey-Bass; 2008. pp. 465–482. [Google Scholar]
- 14.Story MT, Kaphingst KM, Robinson-O’Brien, Glanz K. Creating Healthy Food and Eating Environments: Policy and Environmental Approaches. Annu Rev Public Health. 2008;29:253–272. doi: 10.1146/annurev.publhealth.29.020907.090926. http://dx.doi.org/10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- 15.Frederick CB, Snellman K, Putnam RD. Increasing socioeconomic disparities in adolescent obesity. Proc Natl Acad Sci. 2014;111(4):1338–1342. doi: 10.1073/pnas.1321355110. http://dx.doi.org/10.1073/pnas.1321355110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bethell C, Read D, Goodman E, et al. Consistently inconsistent: a snapshot of across- and within-state disparities in the prevalence of childhood overweight and obesity. Pediatrics. 2009;123(Suppl):S277–S286. doi: 10.1542/peds.2008-2780F. http://dx.doi.org/10.1542/peds.2008-2780F. [DOI] [PubMed] [Google Scholar]
- 17.Myers CA, Slack T, Martin CK, Broyles ST, Heymsfield SB. Regional disparities in obesity prevalence in the United States: A spatial regime analysis. Obesity. 2015;23(2):481–487. doi: 10.1002/oby.20963. http://dx.doi.org/10.1002/oby.20963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harrison K, Bost KK, McBride BA, et al. Toward a Developmental Conceptualization of Contributors to Overweight and Obesity in Childhood: The Six-Cs Model. Child Dev Perspect. 2011;5(1):50–58. http://dx.doi.org/10.1111/j.1750-8606.2010.00150.x. [Google Scholar]
- 19.The Child and Adolescent Health Measurement Initiative. The National Survey of Children’s Health. http://childhealthdata.org/learn/NSCH. Accessed August 16, 2015.
- 20.The National Survey of Children’s Health 2011–2012 Technical Appendix. 2012 [Google Scholar]
- 21.Findley S. Age limits and adolescents. Paediatr Child Health. 2003;8(9):577–578. doi: 10.1093/pch/8.9.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barlow SE, Dietz WH. Obesity Evaluation and Treatment: Expert Committee Recommendations. Pediatrics. 1998;102(3):e29. doi: 10.1542/peds.102.3.e29. http://dx.doi.org/10.1542/peds.102.3.e29. [DOI] [PubMed] [Google Scholar]
- 23.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11. 2002;(246):1–190. [PubMed] [Google Scholar]
- 24.Rao JNK. Small Area Estimation. Hoboken, NJ: John Wiley & Sons, Inc; 2003. http://dx.doi.org/10.1002/0471722189. [Google Scholar]
- 25.Zhang X, Holt JB, Lu H, et al. Multilevel regression and poststratification for small-area estimation of population health outcomes: a case study of chronic obstructive pulmonary disease prevalence using the behavioral risk factor surveillance system. Am J Epidemiol. 2014;179(8):1025–1033. doi: 10.1093/aje/kwu018. http://dx.doi.org/10.1093/aje/kwu018. [DOI] [PubMed] [Google Scholar]
- 26.Zhang X, Onufrak S, Holt JB, Croft JB. A multilevel approach to estimating small area childhood obesity prevalence at the census block-group level. Prev Chronic Dis. 2013;10(8):E68. doi: 10.5888/pcd10.120252. http://dx.doi.org/10.5888/pcd10.120252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goodman MS. Comparison of Small-Area Analysis Techniques for Estimating Prevalence by Race. Prev Chronic Dis. 2010;7(2):A33. [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang X, Holt JB, Yun S, Lu H, Greenlund KJ, Croft JB. Validation of Multilevel Regression and Poststratification Methodology for Small Area Estimation of Health Indicators From the Behavioral Risk Factor Surveillance System. Am J Epidemiol. 2015;182(2):127–137. doi: 10.1093/aje/kwv002. http://dx.doi.org/10.1093/aje/kwv002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Srebotnjak T, Mokdad AH, Murray CJ. A novel framework for validating and applying standardized small area measurement strategies. Popul Health Metr. 2010;8(1):26. doi: 10.1186/1478-7954-8-26. http://dx.doi.org/10.1186/1478-7954-8-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Greenland S. Invited Commentary: Variable Selection versus Shrinkage in the Control of Multiple Confounders. Am J Epidemiol. 2008;167(5):523–529. doi: 10.1093/aje/kwm355. http://dx.doi.org/10.1093/aje/kwm355. [DOI] [PubMed] [Google Scholar]
- 31.Gelman A, Hill J. Data Analysis Using Regression and Multilevel/Hierarchical Models. New York, NY: Cambridge University Press; 2007. https://books.google.com/books?hl=en&lr=&id=c9xLKzZWoZ4C&oi=fnd&pg=PR17&dq=gelman+hill+multilevel&ots=baQcL-Ktlb&sig=FS4V7-seQqH6l4FkYm0fPV04RZU Accessed December 3, 2015. [Google Scholar]
- 32.Harper S, Lynch J, Health P, Hall P. Methods for Measuring Cancer Disparities : Using Data Relevant to Healthy People 2010 Cancer-Related Objectives. Ann Arbor, MI: 2010. http://surveillance.cancer.gov/publications/factsheets/SEER_Health_Disparities-1.pdf. [Google Scholar]
- 33.Pearcy JN, Keppel KG. A summary measure of health disparity. Public Health Rep. 2002;117(3):273–280. doi: 10.1016/S0033-3549(04)50161-9. http://dx.doi.org/10.1016/S0033-3549(04)50161-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Waller L, Gotway C. Applied Spatial Statistics for Public Health Data. Hoboken, NJ: John Wiley & Sons, Inc; 2004. http://dx.doi.org/10.1002/0471662682. [Google Scholar]
- 35.Ding D, Gebel K. Built environment, physical activity, and obesity: What have we learned from reviewing the literature? Health Place. 2012;18(1):100–105. doi: 10.1016/j.healthplace.2011.08.021. http://dx.doi.org/10.1016/j.healthplace.2011.08.021. [DOI] [PubMed] [Google Scholar]
- 36.Cobb LK, Appel LJ, Franco M, Jones-Smith JC, Nur A, Anderson CAM. The relationship of the local food environment with obesity: A systematic review of methods, study quality, and results. Obesity. 2015;23(7):1331–1344. doi: 10.1002/oby.21118. http://dx.doi.org/10.1002/oby.21118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carroll-Scott A, Gilstad-Hayden K, Rosenthal L, et al. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: The role of built, socioeconomic, and social environments. Soc Sci Med. 2013;95:106–114. doi: 10.1016/j.socscimed.2013.04.003. http://dx.doi.org/10.1016/j.socscimed.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dunton GF, Kaplan J, Wolch J, Jerrett M, Reynolds KD. Physical environmental correlates of childhood obesity: a systematic review. Obes Rev. 2009;10(4):393–402. doi: 10.1111/j.1467-789X.2009.00572.x. http://dx.doi.org/10.1111/j.1467-789X.2009.00572.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Black JL, Macinko J. Neighborhoods and obesity. Nutr Rev. 2008;66(1):2–20. doi: 10.1111/j.1753-4887.2007.00001.x. http://dx.doi.org/10.1111/j.1753-4887.2007.00001.x. [DOI] [PubMed] [Google Scholar]
- 40.Rossen LM, Talih M. Social determinants of disparities in weight among U.S. children and adolescents. Ann Epidemiol. 2014;24(10):705–713. doi: 10.1016/j.annepidem.2014.07.010. http://dx.doi.org/10.1016/j.annepidem.2014.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built Environments and Obesity in Disadvantaged Populations. Epidemiol Rev. 2009;31(1):7–20. doi: 10.1093/epirev/mxp005. http://dx.doi.org/10.1093/epirev/mxp005. [DOI] [PubMed] [Google Scholar]
- 42.Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the U.S. Am J Prev Med. 2009;36(1):74–81. doi: 10.1016/j.amepre.2008.09.025. http://dx.doi.org/10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 43.Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the Built Environment Underlies Key Health Disparities in Physical Activity and Obesity. Pediatrics. 2006;117(2):417–424. doi: 10.1542/peds.2005-0058. http://dx.doi.org/10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- 44.Oreskovic NM, Kuhlthau KA, Romm D, Perrin JM. Built Environment and Weight Disparities Among Children in High- and Low-Income Towns. Acad Pediatr. 2009;9(5):315–321. doi: 10.1016/j.acap.2009.02.009. http://dx.doi.org/10.1016/j.acap.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 45.Dinour LM, Bergen D, Yeh M-C. The Food Insecurity–Obesity Paradox: A Review of the Literature and the Role Food Stamps May Play. J Am Diet Assoc. 2007;107(11):1952–1961. doi: 10.1016/j.jada.2007.08.006. http://dx.doi.org/10.1016/j.jada.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 46.Council on Community Pediatrics, Committee on Nutrition. Promoting Food Security for All Children. Pediatrics. 2015;136(5):e1431–e1438. doi: 10.1542/peds.2015-3301. http://dx.doi.org/10.1542/peds.2015-3301. [DOI] [PubMed] [Google Scholar]
- 47.Fleischhacker SE, Evenson KR, Sharkey J, Pitts SBJ, Rodriguez DA. Validity of secondary retail food outlet data: a systematic review. Am J Prev Med. 2013;45(4):462–473. doi: 10.1016/j.amepre.2013.06.009. http://dx.doi.org/10.1016/j.amepre.2013.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nesbit KC, Kolobe TH, Sisson SB, Ghement IR. A structural equation model of environmental correlates of adolescent obesity for age and gender groups. Pediatr Obes. 2015;10(4):288–295. doi: 10.1111/ijpo.259. http://dx.doi.org/10.1111/ijpo.259. [DOI] [PubMed] [Google Scholar]
- 49.Wall MM, Larson NI, Forsyth A, et al. Patterns of Obesogenic Neighborhood Features and Adolescent Weight: A comparison of statistical approaches. Am J Prev Med. 2012;42(5):e65–e75. doi: 10.1016/j.amepre.2012.02.009. http://dx.doi.org/10.1016/j.amepre.2012.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Forsyth A, Wall M, Choo T, Larson N, Van Riper D, Neumark-Sztainer D. Perceived and Police-Reported Neighborhood Crime: Linkages to Adolescent Activity Behaviors and Weight Status. J Adolesc Heal. 2015;57(2):222–228. doi: 10.1016/j.jadohealth.2015.05.003. http://dx.doi.org/10.1016/j.jadohealth.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Slack T, Myers CA, Martin CK, Heymsfield SB. The geographic concentration of U.S. adult obesity prevalence and associated social, economic, and environmental factors. Obesity (Silver Spring) 2014;22(3):868–874. doi: 10.1002/oby.20502. http://dx.doi.org/10.1002/oby.20502. [DOI] [PubMed] [Google Scholar]
- 52.Cunningham SA, Kramer MR, Narayan KMV. Incidence of childhood obesity in the United States. N Engl J Med. 2014;370(5):403–411. doi: 10.1056/NEJMoa1309753. http://dx.doi.org/10.1056/NEJMoa1309753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Saelens BE, Sallis JF, Frank LD, et al. Obesogenic Neighborhood Environments, Child and Parent Obesity: The Neighborhood Impact on Kids Study. Am J Prev Med. 2012;42(5):e57–e64. doi: 10.1016/j.amepre.2012.02.008. http://dx.doi.org/10.1016/j.amepre.2012.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Meyer KA, Boone-Heinonen J, Duffey KJ, et al. Combined measure of neighborhood food and physical activity environments and weight-related outcomes: The CARDIA study. Health Place. 2015;33:9–18. doi: 10.1016/j.healthplace.2015.01.004. http://dx.doi.org/10.1016/j.healthplace.2015.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nelson MC, Gordon-Larsen P, Song Y, Popkin BM. Built and social environments associations with adolescent overweight and activity. Am J Prev Med. 2006;31(2):109–117. doi: 10.1016/j.amepre.2006.03.026. http://dx.doi.org/10.1016/j.amepre.2006.03.026. [DOI] [PubMed] [Google Scholar]
- 56.Akinbami LJ, Ogden CL. Childhood overweight prevalence in the United States: the impact of parent-reported height and weight. Obesity (Silver Spring) 2009;17(8):1574–1580. doi: 10.1038/oby.2009.1. http://dx.doi.org/10.1038/oby.2009.1. [DOI] [PubMed] [Google Scholar]
- 57.Shields M, Connor Gorber S, Janssen I, Tremblay MS. Obesity estimates for children based on parent-reported versus direct measures. Health Rep. 2011;22(3):47–58. [PubMed] [Google Scholar]
- 58.Le A, Judd SE, Allison DB, et al. The geographic distribution of obesity in the U.S. and the potential regional differences in misreporting of obesity. Obesity (Silver Spring) 2014;22(1):300–306. doi: 10.1002/oby.20451. http://dx.doi.org/10.1002/oby.20451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Centers for Disease Control and Prevention. Percentage of high school students who were obese. Obese Youth Over Time. 2015 www.cdc.gov/healthyschools/obesity/obesity-youth.htm. Accessed March 20, 2016.
- 60.Centers for Disease Control and Prevention. Obesity Prevalence Maps. Div Nutr Phys Act Obes. 2015 www.cdc.gov/obesity/data/prevalence-maps.html. Accessed March 20, 2016.
- 61.Allen DW. Social class, race, and toxic releases in American counties, 1995. Soc Sci J. 2001;38(1):13–25. http://dx.doi.org/10.1016/S0362-3319(00)00109-9. [Google Scholar]
- 62.Lobao L. The Emerging Roles of County Governments in Metropolitan and Nonmetropolitan Areas: Findings From a National Survey. Econ Dev Q. 2005;19(3):245–259. http://dx.doi.org/10.1177/0891242405276514. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


