ABSTRACT
The authors here report a case series where bilateral concurrent eye examination, using a head-mounted perimeter (imo®), was employed to facilitate diagnosis of functional visual loss, as regular ophthalmological tests were ineffective. Subjects (11-year-old female, 15-year-old male, and 24-year-old male) were diagnosed with unilateral functional visual loss by using the imo®, at the Kitasato University hospital. The results of the imo® and those of Goldmann perimetry or Humphrey Field Analyzer II differed for all subjects, which is indicative of potential functional visual loss. Bilateral concurrent examination with the imo® may become a standard for future diagnosis of unilateral functional visual loss.
KEYWORDS: Bilateral concurrent eye examination, functional visual loss, head-mounted perimetry
Introduction
Functional visual loss is encountered in daily ophthalmological practice; it often affects school-aged girls, but also occurs in adults and males. It is mainly caused by stress, such as trouble at school or home, but a desire to wear glasses could also be a cause. Several types of visual acuity trick tests are effective in diagnosis, and it is known to show distinctive spiral or tunnel visual fields.1–4
A head-mounted perimeter has recently been developed during the advance in glaucoma diagnosis.5,6 One of these devices, the imo® (CREWT Medical Systems, Inc., Tokyo, Japan), is now clinically available (Figure 1). This head-mounted device allows testing at the bedside, as it is small and light and can be used anywhere. Additionally, it allows measurement of bilateral visual fields simultaneously, by randomly showing targets to each eye without the subject being aware of which eye is being tested.
Figure 1.

Head-mounted perimeter imo® (CREWT Medical Systems, Inc.).
We here report a case series in which bilateral concurrent examination, using the imo®, was used to help diagnose unilateral functional visual loss, as the regular ophthalmological tests were not effective.
Case presentation
The subjects were three patients who were diagnosed with unilateral functional visual loss by using the imo® at Kitasato University hospital. Subjects included an 11-year-old female, a 15-year-old male, and a 24-year-old male.
The specifications of the imo® head-mounted perimeter are as follows. Its dimensions are (W) 190 × (D) 380 × (H) 220 mm, and its weight is 1.6 kg. The target is presented on a transmissive liquid crystal display with a high-intensity light-emitting diode (LED) backlight. The maximum brightness of the target is 10,000 asb and the backlight brightness is 31.4 asb. The target can be shown in an arbitrary size and form, within 35° from the centre of the visual field. We used a Bayesian estimate and adaptive measurement of the maximum-likelihood estimate as a threshold measurement algorithm. During the measurement, it is possible to monitor both eyes and each visual fixation continuously. The location of the target is adjusted each time fixation disparity occurs. The visual field can be measured in both eyes in the same session, by showing the target alternately and randomly to each eye, without the subject being aware of which eye is being tested.
In all cases, both eyes were tested concurrently with 30-2 or 24-2 AIZE. imo® is equipped with an original perimetric algorithm (AIZE: Ambient Interactive Zippy Estimated Sequential Testing). AIZE uses spatial information on every stimulus to estimate visual field thresholds and achieves high accuracy and less test times. We used Goldmann perimetry (GP) or the Humphrey Field Analyzer II (HFA) as a comparison perimetry test.
Case 1
The 11-year-old female subject was investigated for left temporal hemianopia associated with circadian variation, which had been diagnosed 1 year previously. Her head contrast-enhanced magnetic resonance imaging (MRI) was normal, and the cause of her condition was unknown. Her visual field had recovered since the initial diagnosis, but the subject again became aware of visual field loss on the left side that had lasted 11 days prior to visiting our hospital. Visual acuity was Vd = 0.1 (1.2 × +4.75D = Cyl −7.00D A5) and Vs = 0.8 (1.2 × +2.00 D = Cyl −1.50D A180). Critical flicker frequency (CFF) was 39 Hz for the right eye and 38 Hz for the left eye, and her light reflex was normal. The anterior segment of the eye, the ocular media, and the ocular fundus were normal. The results of GP (Figure 2) showed unilateral left temporal hemianopia as diagnosed previously. Circadian variation could not be recognised, and there was no change in symptoms of visual field loss. The result of imo® (Figure 3) did not show left temporal hemianopia as diagnosed by GP.
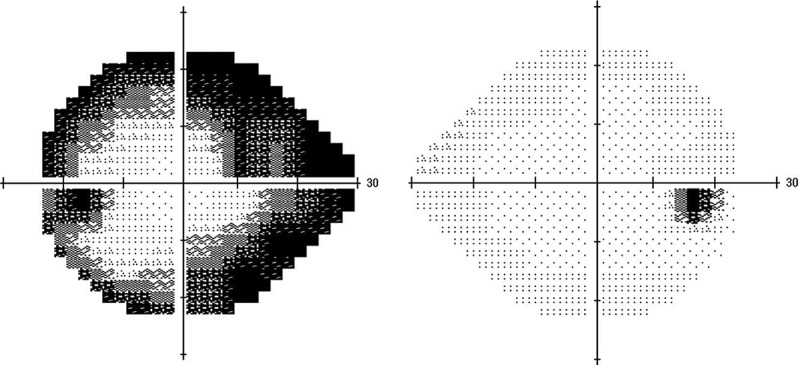
Figure 2.
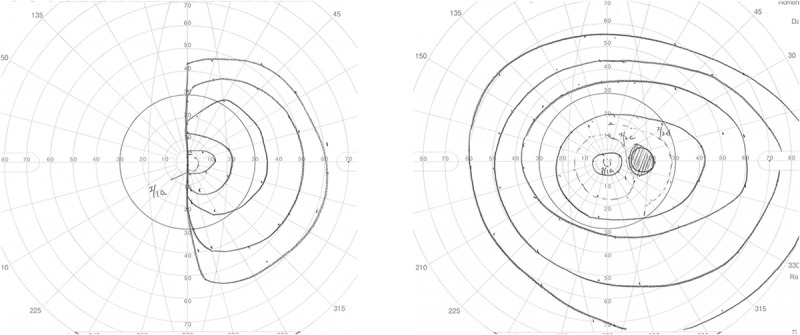
Case 1, GP, left: temporal hemianopia, right: normal.
Figure 3.
Case 1, results of bilateral concurrent examination with imo® at 30-2, AIZE: temporal hemianopia is not recognised in the left eye.
Case 2
The 15-year-old male subject complained about a sudden pain in the right eye, darkness, and a red field of vision in the morning on the 5th day before attending our hospital. He visited an ophthalmological clinic, but the cause remained unknown. He was referred to our hospital. The subject reported that there was no change in visual acuity or the visual field, although eye pain was absent. The visual acuity was Vd = 0.04 (0.4 × −3.50 D), Vs = 0.2 (1.2 × −2.50 D), and CFF was 15 Hz for the right eye and 42 Hz for the left eye. The light reflex was normal. Based on the HFA 30-2 SITA-Standard (Figure 4), the central fovea threshold was 22 dB for the right eye and 39 dB for the left eye, and cloverleaf visual field of the right eye was observed. The anterior segment of the eye, ocular media, and the ocular fundus were normal. On the 11th day after attending our hospital, visual acuity of the right eye was decreasing, and Vd = 0.01 (0.03 × −3.50 D) and Vs = (1.2 × −2.50 D). The CFF of the right eye was 25 Hz based on the vanishing method and 18 Hz based on the emerging method, which was markedly different. Based on the imo® (Figure 5), the central fovea threshold was 36 dB for the right and 34 dB for the left eye, and cloverleaf visual field of the right eye that had been diagnosed by HFA could not be recognised.
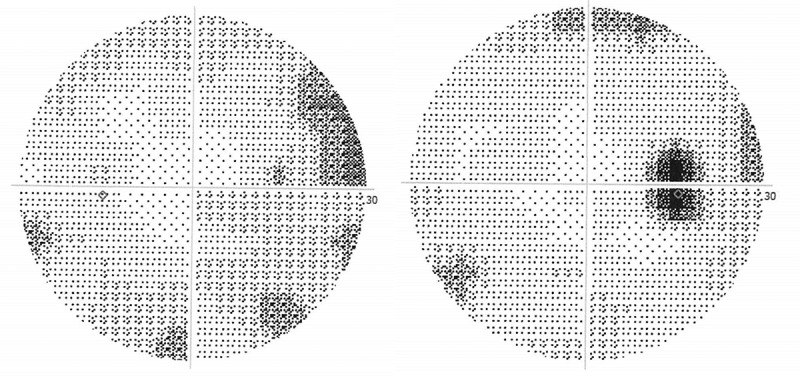
Figure 4.
Case 2, results of HFA 30-2 SITA-Standard: central fovea thresholds are 22 and 39 dB for the right and left eyes, respectively; cloverleaf visual field in the right eye.
Figure 5.
Case 2, results of bilateral concurrent examination with imo® at 30-2, AIZE: central fovea threshold is 36 dB for the right eye and 34 dB for the left eye, recognising no concentric visual field in the right eye.
Case 3
The 24-year-old male subject had slept only 2–3 hours the previous night, as he had been busy. He became aware of a sudden decrease in the visual acuity of the left eye that had lasted for 2 weeks; he then visited an ophthalmological clinic, but the cause was unknown. He was referred to our hospital for further examination. His visual acuity was Vd = 0.08 (1.2 × −4.25 D = Cyl −2.50 D A180) and Vs = 0.02 (0.03 × −4.25 D = Cyl −2.50 D A180), and CFFs were 40 and 25 Hz for the right and left eyes, respectively. The light reflex was normal. Based on HFA 24-2 SITA-Standard (Figure 6), the central fovea thresholds were 38 and 27 dB for the right and left eyes, respectively, and a concentric visual field defect was recognised in the left eye. The anterior segment of the eye, ocular media, and ocular fundus were normal. Based on the imo® (Figure 7), the central fovea threshold was 36 dB for the right eye and 30 dB for the left eye, and the concentric visual field defect that was diagnosed in the left eye by HFA could not be recognised.
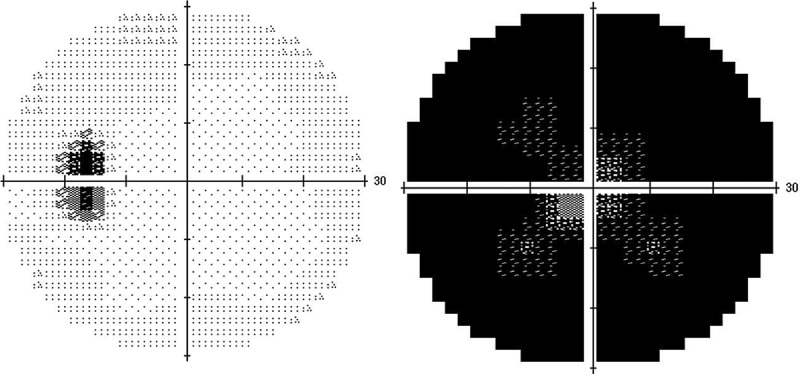
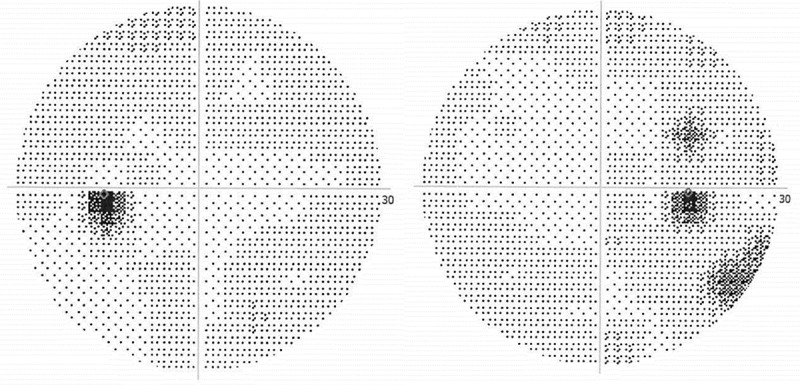
Figure 6.
Case 3, results of HFA 24-2 SITA-Standard: central fovea thresholds are 38 and 27 dB for the right and left eyes, respectively, recognising concentric visual field in the left eye.
Figure 7.
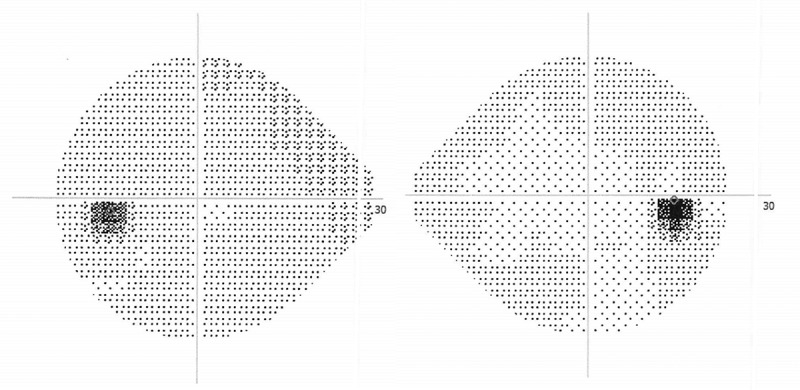
Case 3, results of bilateral concurrent examination with imo® 24-2, AIZE: central fovea thresholds are 36 and 30 dB for the right and left eyes, respectively, recognising no concentric visual field in the left eye.
Discussion
There was a difference between the findings of the imo® and those obtained by GP or the HFA, indicating that unilateral functional visual loss is suspicious. Generally, functional visual loss is diagnosed by several types of visual acuity trick tests and by studying distinctive spiral or tunnel visual fields.1–4 However, diagnosis is often difficult, as there is no response to visual acuity trick tests in some patients and the visual field variation is atypical. In some cases of functional visual loss, patients are incorrectly diagnosed with optic neuritis and undergo steroid pulse therapy, or examinations are continuously repeated unnecessarily. Additionally, as in Case 1, functional visual loss sometimes presents with unilateral horizontal hemianopia, which has been reported as the “missing half”.3,7 The diagnosis of functional visual loss cannot be determined from other findings even if the disorder is suspected; thus, a “watch and wait” approach is required. However, the imo® facilitates diag-nosis by examining the eyes bilaterally and simultaneously, even in cases where the disorder could not be diagnosed, as the patients showed no response to several types of visual acuity trick tests, or where no spiral or tunnel visual fields were observed. imo®has the potential to demonstrate full visual fields and foveal threshold. Bilateral concurrent examination may become a standard for future diagnosis of unilateral functional visual loss.
Acknowledgements
We would like to thank Editage (www.editage.jp) for English language editing.
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
References
- [1].Scott JA, Egan RA.. Prevalence of organic neuro-ophthalmologic disease in patients with functional visual loss. Am J Ophthalmol 2003;135:670–675. [DOI] [PubMed] [Google Scholar]
- [2].SA1 Lim, RM Siatkowski, Farris BK.. Functional visual loss in adults and children patient characteristics, management, and outcomes. Ophthalmology 2005;112:1821–1828. [DOI] [PubMed] [Google Scholar]
- [3].Bruce BB, Newman NJ.. Functional visual loss. Neurol Clin 2010;28:789–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Grant TL, Nicholas JV, Steven LG.. Neuro-Ophthalmology Diagnosis and Management. Philadelphia, PA: Sanders Elsevier; 2001. [Google Scholar]
- [5].Hollander DA, Volpe NJ, Moster ML, Liu GT, Balcer LJ, Judy KD, Galetta SL.. Use of a portable head mounted perimetry system to assess bedside visual fields. Br J Ophthalmol 2000;84:1185–1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Wroblewski D, Francis BA, Sadun A, Vakili G, Chopra V.. Testing of visual field with virtual reality goggles in manual and visual grasp modes. Biomed Res Int 2014;2014:206082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Keane JR. Hysterical hemianopia. The ‘missing half’ field defect. Arch Ophthalmol 1979;97:865–866. [DOI] [PubMed] [Google Scholar]


