Abstract
Background
Elderly patients are the fastest-growing group in need of renal transplantation. This study puts focus on renal transplant recipients in their 80th year or longer at time of engraftment. Is there evidence to support an absolute upper age limit for renal transplantation?
Methods
Recipients in their 80th year or longer, transplanted between 1983 and 2015, were included. Data were retrieved from the Norwegian Renal Registry in the end of October 2015. Graft and patient survivals were compared with recipients aged 70 to 79 years at transplantation.
Results
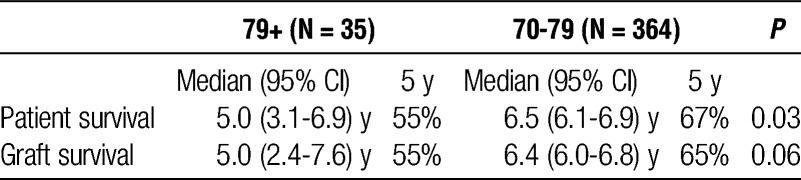
Forty-seven patients older than 79 years were transplanted in the defined period. Median age 80.1 years, 81% were men. Median time on dialysis before transplantation was 18.5 months. All patients received an allograft from a deceased donor (median donor age, 61.8 years). In the death-censored graft survival model, there was no statistical difference between the groups. We found improved patient and graft survivals after introduction of mycophenolate mofetil and induction with basiliximab. Patients transplanted before 2000 had increased risk of death compared with those transplanted after 2000 (hazard ratio, 3.2; 95% confidence interval, 1.2-8.7). Median uncensored graft survival for patients transplanted after the year 2000 was 5.0 year (95% confidence interval, 2.4-7.6). Median patient survival was 5.0 years (3.1-6.9) and 5-year patient survival was 55%.
Conclusions
Age by itself should not be an absolute contraindication against renal transplantation. An estimated 5-year survival rate of 55% post-engraftment for an 80-year-old patient is in our opinion more than acceptable.
The authors reveal an estimated 5 years survival rate of 55% postengraftment for an 80 years old patient with end-stage renal disease. In carefully selected octogenarians, kidney transplantation has an acceptable estimated 5 years survival rate in their opinion.
The global population ageing has changed the landscape of chronic disease with an increasing prevalence of older patients with end-stage renal disease (ESRD).1 Kidney transplantation is considered relatively safe and offers survival advantage over dialysis for the majority of patients and is therefore considered as the preferred treatment option.2,3 Several studies have reported acceptable outcomes also for selected elderly patients.4-6 Kidney transplantation has therefore changed from a relatively exclusive event in a highly selected few to a reality for a substantial proportion of elderly patients with ESRD.7 Publications have shown that even patients older than 70 years with ESRD have a survival benefit if transplanted compared with continued dialysis.8,9 Consequently, there is a general consensus that age per se should not represent a barrier to transplantation. Many centers are however reluctant to accept elderly patients to the waiting list. With increased comorbidity and shorter life expectancy, these centers argue that the magnitude of improved patient survival with transplantation is limited.
With the current organ shortage, there is a continuous debate whether elderly patients should be put on the waiting list for transplantation or remain in dialysis. The debate will vary from center to center and country to country. At our center, transplantation has been offered to all patients considered to benefit from the procedure, with no strict upper or lower age limit. Accordingly, we have had no upper formal age limit for live or deceased kidney donation, that is, willingly accepting expanded criteria donor kidneys to older recipients.10 Donation after circulatory death has so far not been an option at our transplant centre. Also, despite increasing transplant waiting lists, the overall advances in patient care during the last decade may have led to a relatively fitter subset of patients at the time of transplantation, including the older waitlisted recipients.
As the general population ages, an increasing number of patients with ESRD will eventually be in their 80s. It is obvious that patients in their 80s who are enlisted for transplantation is a selected group, but even so: How do they perform? Is it worthwhile to offer kidney transplantation to such old recipients or should we establish an upper age limit? The aim of this study was to investigate and compare the posttransplant graft and patient survivals of recipients in their 80s compared with recipients aged 70 to 79 years at time of engraftment.
MATERIALS AND METHODS
We performed a single-center retrospective analysis. All patients in their 80th year (or older) at time of engraftment, transplanted at Oslo University Hospital between 1983 and 2015 were included in the study. All patients received prednisolone and a calcineurin inhibitor (CNI). Current trough level for tacrolimus is 3 to 7 μg/L from the day of transplantation. In addition, patients transplanted from 1983 until 1999 received azathioprine, whereas patients transplanted from 2000 to 2015 received mycophenolate mofetil. From 2007, induction treatment with basiliximab was added. For comparison, data of patients aged 70 to 79 years whom were transplanted between 2000 and 2014 were retrieved. All data were retrieved from the Norwegian Renal Registry by end of October 2015.
Statistics
Due to low number of octogenarians, continuous data were expressed as median (range) and distribution was compared using the nonparametric independent Mann-Whitney U test. Categorical data were compared using a 2-sided Fisher exact test. Survival analyses were performed using the Kaplan-Meier method as well as Cox regression models with patient survival, uncensored, and death-censored graft survival as outcomes. All statistical analyses were performed using the statistical software package IBM SPSS 22.
RESULTS
We included data from 47 patients older than 79 years whom were transplanted at our center between January 1, 1983, and October 1, 2015. During this time span, 129 patients (74.9% men) aged 79 years or older entering renal replacement therapy have been reported by their treating nephrologists, as potential candidates for renal transplantation. Among these 129 patients, 53 (41%) passed the medical screening and were put on the kidney waiting list and 47 (89%) have received a transplant (Figure 1). Median age at transplantation was 80.1 years (79.1-83.6 years). Patient and transplant characteristics are presented in Table 1. All octogenarians received an allograft from a deceased donor. In the death-censored graft survival model, there was no statistical difference between the groups (Figure 2). Median uncensored graft survival was 4.1 years (95% confidence interval [95% CI], 1.7-6.5) in octogenarians and 6.4 years (6.0-6.8 years) in 70 to 79 years. Median patient survival was 4.7 years (2.8-6.6 years) in octogenarians compared with 6.5 years (6.1-6.9 years) (log rank, P < 0.001; Figure 3). Two- and five-year patient survival rates were 78% and 47% in octogenarians versus 85% and 67% in 70 to 79 years. Patients transplanted before 2000 had increased risk of death compared with patients transplanted after 2000 (hazard ratio, 3.2; 95% CI, 1.2-8.7). Recipient age, recipient sex, donor age, and time on dialysis were tested in the same model without any significant association to patient survival. A separate Kaplan-Meier analysis revealed a median patient survival of 2.5 years (0.0-5.5 years) for octogenarians transplanted before 2000 (n = 12) versus 5.0 years (3.1-6.9 years; P = 0.028) for those transplanted after 2000.
FIGURE 1.

Transplantation eras in the 79+ group.
TABLE 1.
Patient and transplant characteristics continuous data are expressed as median (range), categorical data as number (%)

FIGURE 2.
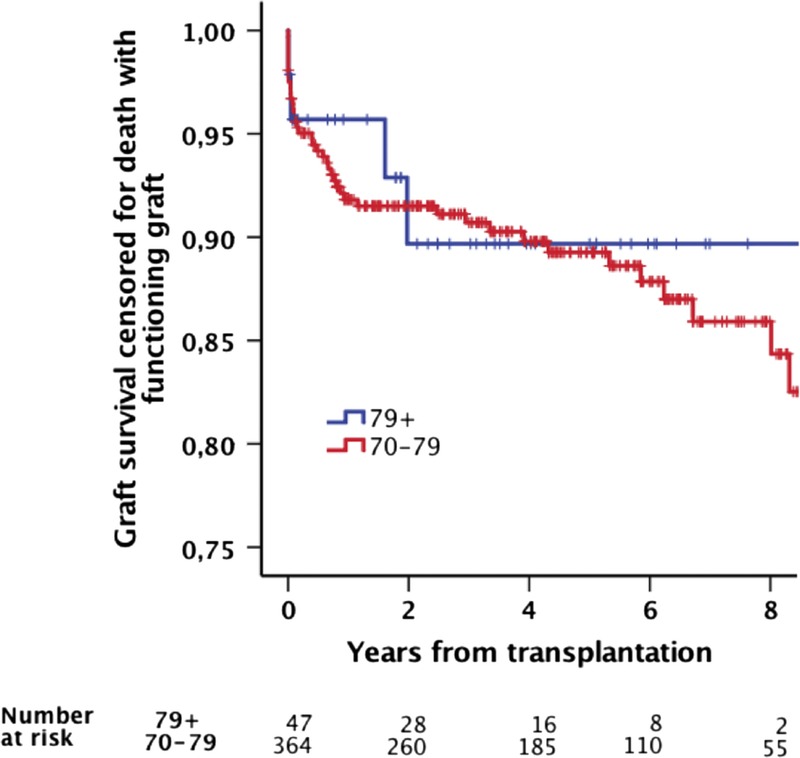
Death-censored graft survival.
FIGURE 3.
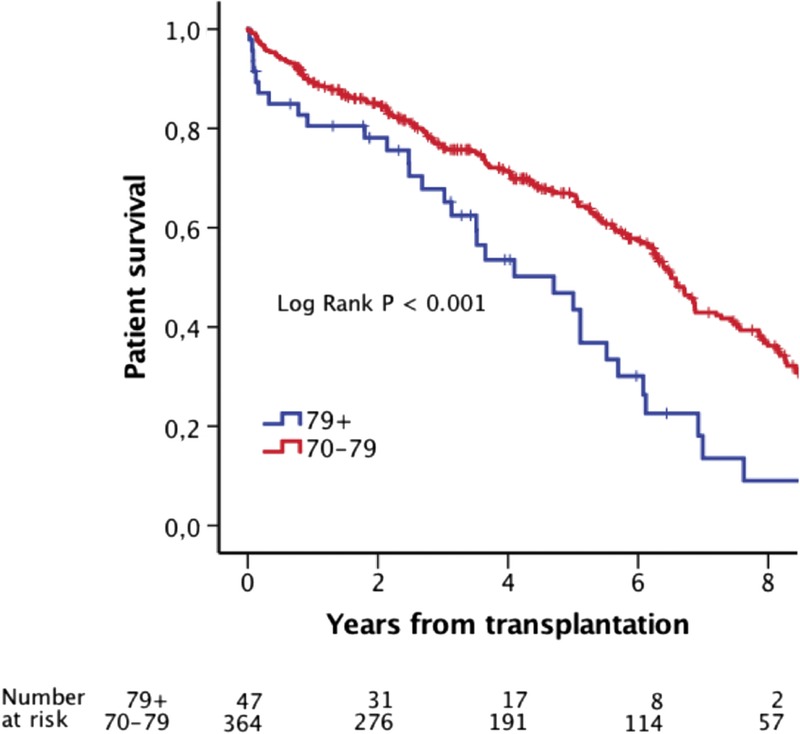
Patient survival.
Only 12 of the patients were transplanted before year 2000. Median donor age before year 2000 was 43.0 years (range, 17.5-72.6 years) compared with 67.5 years (range, 36.0-85.0 years) in those transplanted after 2000 (P < 0.001). Patients transplanted before 2000 had increased risk of death compared with patients transplanted after 2000 (hazard ratio, 3.2; 95% CI, 1.2-8.7). Recipient age, recipient sex, donor age, and time on dialysis were tested in the same model without any significant association to patient survival. A separate Kaplan-Meier analysis revealed a median patient survival of 2.5 years (0.0-5.5 years) for octogenarians transplanted before 2000 (n = 12) versus 5.0 years (3.1-6.9 years) for those transplanted after 2000 (P = 0.028). We performed subgroup analyses limiting the 79+ cohort to those transplanted from year 2000 (n = 35) and comparing the results to those previously reported for the 70 to 79 group. Patient and graft survivals in these recipients are compared in Table 2. Five-year death-censored graft survival was 89% in both groups (P = 0.805).
TABLE 2.
Patient and graft survival in patients transplanted after 2000
DISCUSSION
Our results show that old age by itself should not be considered as an absolute contraindication against renal transplantation. In carefully selected octogenarians, kidney transplantation has an acceptable estimated 5-year survival rate. The reality of worldwide organ shortage for transplantation is a challenge, but should not automatically disqualify elderly recipients.
The majority of ESRD patients who are reaching their 80s have a burden of comorbidities and are obviously not considered eligible for kidney transplantation. Appropriate pretransplant evaluation is extremely important. At our center, we use the same standardized medical evaluation criteria for octogenarians as for younger recipients. Additional fragility tests are only performed when the referring nephrologist is in doubt. An important consideration for elderly patients undergoing transplant evaluation is their likelihood of a favorable perioperative outcome. Huang et al11 published data from the OPTN/UNOS database and compared outcome of elderly recipients (divided into groups 60-69, 70-79, >80) using death during the first 30 transplant days as a metric for perioperative mortality. The overall rate of perioperative mortality was low (1.5%) and only 2.5% in the oldest age group. At 2 years, Huang et al, as anticipated, find that survival was lower for 80 years or older (73%) and 70 to 79 years (86%) compared with recipients aged 60 to 69 years (89%). This difference is, however, similar to the patient survival in the age-matched general US population and to our findings (79+ [78%], 70-79 [85%]).
The benefits of renal transplantation on patient survival are generally not realized until 1.5 to 2 years after transplantation,2,9,12 that is, patients who are unlikely to survive this long should not undergo transplantation. When dealing with a lifesaving but scarce medical resource, such as kidney transplantation, one may ask if it is appropriate that any octogenarians should be advised referral for transplantation. In general, elderly patients with ESRD compared with younger patients have a lower referral rate and chance for placement on the waiting list, even in the absence of absolute contraindication for transplantation. Preclusion based on age alone is considered not fair, but the difficulty in selection, taking biological age, and comorbid conditions along with increased operative risk into account continues to pose a significant challenge to the transplant community. Although there has been an increase in living donation in some countries, both patients and their caretakers unfortunately often remain reluctant toward elderly spousal donations, paired kidney exchange, and the principle of “transplanting one generation up.” Knowing the importance of preemptive transplantation/reduced waiting time, specifically in the elderly, it was surprising to find that no octogenarian received a kidney from a living donor.9,13 With an increasing number of octogenarians entering renal replacement therapy and being evaluated for transplantation, this will need to change. Use of living donors would also, most likely, improve the posttransplant outcome. In most countries, the reality of organ scarcity and prolonged waiting times for a deceased donor kidney transplant otherwise indicate that less than 50% of the selected elderly on the waiting list may have a realistic hope to receive a timely transplant.14 In addition, delayed pretransplant workup or late referral is not uncommon. This may have major impact, especially in the elderly, on the chance for posttransplant success. Time on dialysis before transplantation has been identified as a risk factor for posttransplant survival in elderly patients.13,15 Compared with other transplant centers, the recipients in our study had a relatively short time on dialysis before transplantation, and the mean cold ischemia time was generally short.16,17
After a renal transplantation, there is a need for lifelong immunosuppressive therapy. The optimal immunosuppressive treatment for elderly patients after renal transplantation is not clarified. A leading cause of death in elderly recipients is infections. On the other hand, acute rejection episodes has been identified as a risk factor for death in elderly recipients,15 and the outcome after introducing modern immunosuppressive protocols has been remarkably improved.18 At our center, we have registered improved posttran'splant outcome after switch from azathioprin to mycophenolate mofetil and the introduction of induction therapy with basiliximab.15,18,19 It is important to administer sufficient immunosuppressive treatment to avoid rejection while ensuring that the treatment is not so intense as to increase the danger of infection. There are also some indications that there is slower elimination of CNI in elderly recipients, indicating it might be safe to aim for lower CNI trough levels.20 Currently, we aim for tacrolimus trough levels 3 to 7 μg/L from time of transplantation. Additionally, it is important to have in mind the possibility of reducing the total immunosuppressive load.19,20
Most recipients received kidneys from older donors. Graft failure is known to be higher with increasing donor age.21,22 However, if kidneys from donors as old as 90 years can be accepted for implantation, there is no justification why an increased number of elderly patients could not receive a kidney graft in an old-for-old program.23-25 An active and functioning program would eliminate allocation obstacles and shift organs from younger donors to younger recipients According to the Norwegian transplant program, living donor transplantation is warranted whenever possible—also in the elderly. We have no good explanation as to why this has not been the case in the octogenarians.
The important perspective remains that a successful transplantation is associated with a substantial improvement in longevity and most likely also in quality of life.26 There is currently limited data available in elderly, and no data on octogenarians, describing how quality of life is affected by kidney transplantation. In a previous article from Heldal et al, transplant recipients older than 70 years transplanted between 2000 and 2005 had a survival benefit after 2.5 years compared with age-matched dialysis patients remaining on the waiting list.9 This may improve even further if an increased number of living donors are used. Further studies evaluating the impact on transplantation on survival and quality of life in the elderly are strongly warranted.
A limitation of our study is the small numbers of octogenarians being transplanted. This gives insufficient numbers to make reliable analysis. The majority was transplanted in the last decade, and outcome has improved from 1983 (Figure 1). Our findings are from a population consisting of primarily whites with high socioeconomic status. In addition, one must remember that Norway has a socialized healthcare system taking equally good care of every patient, indicating that similar results may not be found in larger more diverse countries with lower overall healthcare. The strengths of our study are that no patient was lost to follow-up, we have had a uniform single-center approach toward octogenarians and that we historically not have been hampered by lack of organs for transplantation.
We conclude that transplantation in octogenarians is worthwhile. An estimated 5-year survival rate of 55% postengraftment for an 80-year-old patient with ESRD is in our opinion more than acceptable. Increasing number of living donor transplantation in this cohort will most likely improve outcome. Careful selection rather than a fixed age-limit should be used to ensure a satisfactory graft and patient survivals.
Footnotes
K.L. received funding from the Norwegian Extra Foundation for Health and Rehabilitation through EXTRA funds.
The authors declare no conflicts of interest.
K.L., K.H., and K.M. designed and wrote the article. T.L. supplied data from the Norwegian Renal Registry. T.L., A.V.R., A.H., and P.-D.L. participated in writing and evaluating the article. All authors approve of the submitted article.
REFERENCES
- 1.Port FK, Merion RM, Roys EC, et al. Trends in organ donation and transplantation in the United States, 1997-2006. Am J Transplant. 2008;8:911–921. [DOI] [PubMed] [Google Scholar]
- 2.Wolfe RA, Ashby VB, Milford EL, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341:1725–1730. [DOI] [PubMed] [Google Scholar]
- 3.Danovitch G, Savransky E. Challenges in the counseling and management of older kidney transplant candidates. Am J Kidney Dis. 2006;47:S86–S97. [DOI] [PubMed] [Google Scholar]
- 4.Heldal K, Hartmann A, Leivestad T, et al. Risk variables associated with the outcome of kidney recipients >70 years of age in the new millennium. Nephrol Dial Transplant. 2011;26:2706–2711. [DOI] [PubMed] [Google Scholar]
- 5.McAdams-DeMarco MA, James N, Salter ML, et al. Trends in kidney transplant outcomes in older adults. J Am Geriatr Soc. 2014;62:2235–2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sørensen VR, Heaf J, Wehberg S, et al. Survival benefit in renal transplantation despite high comorbidity. Transplantation. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ponticelli C, Podestà MA, Graziani G. Renal transplantation in elderly patients. How to select the candidates to the waiting list? Transplant Rev (Orlando). 2014;28:188–192. [DOI] [PubMed] [Google Scholar]
- 8.Knoll GA. Is kidney transplantation for everyone? The example of the older dialysis patient. Clin J Am Soc Nephrol. 2009;4:2040–2044. [DOI] [PubMed] [Google Scholar]
- 9.Heldal K, Hartmann A, Grootendorst DC, et al. Benefit of kidney transplantation beyond 70 years of age. Nephrol Dial Transplant. 2010;25:1680–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Foss A, Heldal K, Scott H, et al. Kidneys from deceased donors more than 75 years perform acceptably after transplantation. Transplantation. 2009;87:1437–1441. [DOI] [PubMed] [Google Scholar]
- 11.Huang E, Poommipanit N, Sampaio MS, et al. Intermediate-term outcomes associated with kidney transplantation in recipients 80 years and older: an analysis of the OPTN/UNOS database. Transplantation. 2010;90:974–979. [DOI] [PubMed] [Google Scholar]
- 12.Rao PS, Merion RM, Ashby VB, et al. Renal transplantation in elderly patients older than 70 years of age: results from the Scientific Registry of Transplant Recipients. Transplantation. 2007;83:1069–1074. [DOI] [PubMed] [Google Scholar]
- 13.Sutherland AI, IJzermans JN, Forsythe JL, et al. Kidney and liver transplantation in the elderly. Br J Surg. 2016;103:e62–e72. [DOI] [PubMed] [Google Scholar]
- 14.Schold J, Srinivas TR, Sehgal AR, et al. Half of kidney transplant candidates who are older than 60 years now placed on the waiting list will die before receiving a deceased-donor transplant. Clin J Am Soc Nephrol. 2009;4:1239–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heldal K, Hartmann A, Leivestad T, et al. Clinical outcomes in elderly kidney transplant recipients are related to acute rejection episodes rather than pretransplant comorbidity. Transplantation. 2009;87:1045–1051. [DOI] [PubMed] [Google Scholar]
- 16.Kayler LK, Magliocca J, Zendejas I, et al. Impact of cold ischemia time on graft survival among ECD transplant recipients: a paired kidney analysis. Am J Transplant. 2011;11:2647–2656. [DOI] [PubMed] [Google Scholar]
- 17.Matas AJ, Smith JM, Skeans MA, et al. OPTN/SRTR 2013 Annual Data Report: kidney. Am J Transplant. 2015;15:1–34. [DOI] [PubMed] [Google Scholar]
- 18.Heldal K, Thorarinsdottir S, Hartmann A, et al. Induction with interleukin-2 antagonist for transplantation of kidneys from older deceased donors: an observational study. Transplant Res. 2013;2:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heldal K, Midtvedt K. Managing transplant rejection in the elderly: the benefits of less aggressive immunosuppressive regimens. Drugs Aging. 2013;30:459–466. [DOI] [PubMed] [Google Scholar]
- 20.Falck P, Asberg A, Byberg KT, et al. Reduced elimination of cyclosporine A in elderly (>65 years) kidney transplant recipients. Transplantation. 2008;86:1379–1383. [DOI] [PubMed] [Google Scholar]
- 21.Lee CM, Carter JT, Randall HB, et al. The effect of age and prolonged cold ischemia times on the national allocation of cadaveric renal allografts. J Surg Res. 2000;91:83–88. [DOI] [PubMed] [Google Scholar]
- 22.Morris PJ, Johnson RJ, Fuggle SV, et al. Analysis of factors that affect outcome of primary cadaveric renal transplantation in the UK. HLA Task Force of the Kidney Advisory Group of the United Kingdom Transplant Support Service Authority (UKTSSA). Lancet. 1999;354:1147–1152. [DOI] [PubMed] [Google Scholar]
- 23.Midtvedt K, Namtvedt T, Scott H, et al. Single transplanted kidneys from a 90-year-old deceased donor perform acceptably at 1 year. Transplant Proc. 2011;43:2107–2109. [DOI] [PubMed] [Google Scholar]
- 24.Reisaeter AV, Foss A, Hartmann A, et al. The kidney transplantation program in Norway since 2000. Clin Transpl. 2011:111–118. [PubMed] [Google Scholar]
- 25.Fabrizii V, Kovarik J, Bodingbauer M, et al. Long-term patient and graft survival in the eurotransplant senior program: a single-center experience. Transplantation. 2005;80:582–589. [DOI] [PubMed] [Google Scholar]
- 26.Griva K, Davenport A, Harrison M, et al. The impact of treatment transitions between dialysis and transplantation on illness cognitions and quality of life—a prospective study. Br J Health Psychol. 2012;17:812–827. [DOI] [PubMed] [Google Scholar]


