Abstract
Background
Financial barriers to health care are associated with worse outcomes following acute myocardial infarction (AMI). Yet, it is unknown whether the prevalence of financial barriers and their relationship with post‐AMI outcomes vary by sex among young adults.
Methods and Results
We assessed sex differences in patient‐reported financial barriers among adults aged <55 years with AMI using data from the Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients study. We examined the prevalence of financial barriers and their association with health status 12 months post‐AMI. Among 3437 patients, more women than men reported financial barriers to medications (22.3% vs 17.2%; P=0.001), but rates of financial barriers to services were similar (31.3% vs 28.9%; P=0.152). In multivariable linear regression models adjusting for baseline health, psychosocial status, and clinical characteristics, compared with no financial barriers, women and men with financial barriers to services and medications had worse mental functional status (Short Form‐12 mental health score: mean difference [MD]=−3.28 and −3.35, respectively), greater depressive symptomatology (Patient Health Questionnaire‐9: MD, 2.18 and 2.16), lower quality of life (Seattle Angina Questionnaire–Quality of Life: MD, −4.98 and −7.66), and higher perceived stress (Perceived Stress Score: MD, 3.76 and 3.90; all P<0.05). There was no interaction between sex and financial barriers.
Conclusions
Financial barriers to care are common in young patients with AMI and associated with worse health outcomes 1 year post‐AMI. Whereas women experienced more financial barriers than men, the association did not vary by sex. These findings emphasize the importance of addressing financial barriers to recovery post‐AMI in young adults.
Keywords: epidemiology, myocardial infarction, risk factors, women
Subject Categories: Quality and Outcomes, Women, Risk Factors, Epidemiology
Introduction
Young women (aged ≤55 years) with acute myocardial infarction (AMI) have worse health outcomes, including poorer health status, higher mortality, and greater risk for readmission, than similarly aged men.1, 2, 3, 4 The reasons for these disparities remain largely unexplained. Whereas some reports reveal higher rates of certain comorbidities among young women with AMI, many studies have found weak or no sex differences in relevant risk factors.5, 6, 7, 8 Few studies have evaluated the effect of socioeconomic factors on health outcomes in young patients. Yet, studies in older AMI populations have shown that older adults with financial barriers to health care have a greater risk of rehospitalization, poorer quality of life, and longer delays in seeking care than patients without financial barriers.9, 10
Financial barriers may be uniquely relevant for younger women with AMI. Women in the general population are more likely than men to delay needed care, postpone preventive health services, and skip doses of medications attributed to cost.11, 12, 13, 14 These differences may be attributed to financial inequities given that, in aggregate, women have higher rates of poverty and lower wages than men and have historically faced higher prices in the individual insurance market.11, 13 Additionally, financial barriers may be more prevalent in younger populations with AMI, given the higher rates of uninsurance, underinsurance, and medical debt compared with older adults who are eligible for Medicare.9, 15, 16 In addition, young men and women may encounter other financial stressors, such as caring for children and aging parents.17 Taken together, these observations suggest that young women with AMI may be at particularly high risk of financial barriers to health care, which may adversely impact health outcomes and contribute to why young women have worse health status and psychosocial outcomes post‐AMI than similarly aged men.
In this study, we characterized financial barriers among young women and men with AMI and their relationship with health status and psychosocial outcomes post‐AMI. Specifically, we used data from the VIRGO (Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients) Study, the largest multicenter, prospective study of young adults with AMI, to investigate sex differences in the prevalence and associations of financial barriers to health care services and medications with 12‐month patient‐reported outcomes, including health status (symptoms, functioning, and quality of life), stress, and depressive symptoms. These data can help to identify patients at elevated risk for adverse outcomes and inform strategies to improve outcomes.
Methods
Study Sample
The VIRGO study, as described previously,18 is a prospective, observational study aimed to examine sex differences in presentation, treatment, and outcomes of young patients with AMI. Patients aged 18 to 55 years with AMI presenting to 103 hospitals in the United States and 24 hospitals in Spain were eligible for enrollment.
AMI was confirmed by the presence of elevated cardiac biomarkers (troponin or creatinine kinase) and supporting evidence of myocardial ischemia, including at least 1 of the following: symptoms of ischemia or electrocardiographic changes suggestive of new ischemia (new ST‐T changes, new or presumably new left bundle branch block, or the development of pathological Q waves). To be eligible, participants had to either present directly to the enrolling institution or be transferred within the first 24 hours of symptoms. Patients with elevated cardiac markers as a complication of elective coronary revascularization, who were unable to provide informed consent or be contacted for follow‐up, were incarcerated, did not speak English or Spanish, or had an AMI as the result of physical trauma were excluded from the study.
Of the 5585 patients who were screened, 3572 (women‐to‐men ratio of 2:1) with clinically confirmed AMI were enrolled between August 2008 and May 2012. We excluded patients with missing data to questions about financial barriers to health care (n=64). Patients from Australia (n=72) were also excluded in this analysis, given that they were lost to follow‐up at a much higher rate than patients in the United States and Spain. Therefore, the final cohort in this study included 3437 patients. Patients missing data on financial barriers did not differ significantly from patients without missing data with respect to age, race, marital status, living alone, or employment (all P>0.1).
Demographic, clinical, and treatment data were collected by medical chart abstraction and standardized in‐person interviews administered by trained personnel during the index AMI admission. Follow‐up telephone interviews were administered by the Yale Follow‐Up Center in the United States and ANAGRAM‐ESIC in Spain at 1 and 12 months to assess patient‐reported outcomes. Institutional research board approval was obtained at each participating center, and informed consent was obtained from all participants.
Financial Barriers
We measured perceived financial barriers to medical care by patient self‐report. This approach of using patient‐reported questions allowed us to characterize financial barriers from the patient's perspective, rather than inferring how finances are impacting a patient's ability to obtain health care based on indirect measures like insurance status or income. Two questions, previously used to classify financial barriers to health care services or financial barriers to medications,9 were assessed during the index hospitalization: “In the past year, have you avoided obtaining health care services because of cost?” (yes/no) and “In the past year, how often have you not taken a medication that your doctor prescribed because of cost?” (5‐point Likert scale ranging from “never” to “always”). We collapsed responses to the question on cost‐related nonadherence to medications into a dichotomous variable indicating financial barriers to medications, with “never” or “rarely” categorized as no and “occasionally,” “often,” or “always” categorized as yes. Because financial barriers to services have been shown to relate to AMI outcomes differently than financial barriers to medications, patients were classified into 4 mutually exclusive groups based on their responses to the 2 questions9: (1) no barriers; (2) barriers to services only; (3) barriers to medications only; and (4) barriers to services and medications.
Health Outcome Measures
We assessed health status, quality of life, depressive symptoms, and perceived stress at baseline and 12 months post‐AMI. Health status was measured using the Short Form‐12 (SF‐12) physical and mental component scores (PCS and MCS). The SF‐12 quantifies patients’ mental and physical functional status and has been shown to be reliable and valid.19 The PCS and MCS scores range from 0 to 100, in which higher numbers indicate better health status. A score of 50 reflects the population mean, and 10 points represents 1 SD. Quality of life was evaluated using the Seattle Angina Questionnaire (SAQ), a validated instrument that measures patients’ disease‐specific health status through a 19‐item self‐administered questionnaire.20 The instrument measures 5 dimensions of coronary artery disease and has been used widely in research among patients with AMI and other cardiovascular disease.21, 22 The quality of life score ranges from 0 to 100, with higher scores representing higher quality of life. A mean difference of greater than 5 points between groups is considered clinically significant.20 Depressive symptomatology was measured using the 9‐item Patient Health Questionnaire (PHQ‐9). This instrument has been widely employed in cardiac populations.23, 24, 25 Scores range from 0 to 27, with higher scores representing greater depressive symptomatology.26, 27 A score greater than or equal to 10 suggests moderate depressive symptoms. Finally, perceived stress was evaluated using the Perceived Stress Scale (PSS), a 14‐item questionnaire that measures the degree to which a patient's life situation was perceived as stressful, unpredictable, uncontrollable, and overloading. Each item of the PSS uses a 5‐point Likert scale, resulting in an overall score ranging from 0 to 56 with higher scores indicating greater stress.28
Statistical Analyses
To examine whether financial barriers varied in prevalence and association with 12‐month outcomes between men and women, we classified men and women, separately, into the 4 financial barrier groups and compared baseline demographic, health care access and utilization, clinical, and process of care characteristics between financial barrier groups using chi‐squared tests for categorical variables and Student t tests or ANOVA for continuous variables. To assess the relationship between sex and reporting financial barriers to services and financial barriers to medications, we performed sequential logistic regression, adjusting for sex, other demographic characteristics, and cardiovascular risk factors hypothesized to be associated with financial barriers.
Unadjusted associations between financial barriers and health outcome measures (SF‐12 PCS and MCS, PHQ‐9, PSS, and SAQ–Quality of Life [QoL]) stratified by sex were evaluated by plotting mean health and psychosocial status scores at baseline and 12 months by financial barrier groups and tested statistically by using ANOVA. To assess the independent relationship between financial barriers and 12‐month health outcomes, we used linear regression models with least squares means, adjusting for baseline health and psychosocial status (to account for the relationship between baseline and 12‐month health outcomes) and clinical characteristics. The group without financial barriers to services or medications was used as the reference category in all regression analyses. In addition, we tested interactions between sex and financial barriers to health care to determine whether the effect of financial barriers differed across sexes.
Covariates for the final models were selected using a combination of clinical judgment, past literature, and face validity (defined as P<0.1).1, 9, 10, 29 They included patient demographics (age, sex, race, marital status, living status, education, and employment) and clinical characteristics, such as cardiovascular risk factors and comorbidities (diabetes mellitus, hypertension, smoking, past myocardial infarction [MI], chronic obstructive pulmonary disease [COPD], heart failure, past stroke, depression [except in the model for depression 12 months post‐AMI], low social support [ENRICHD Social Support Inventory], alcohol abuse, and body mass index [BMI] groups), clinical presentation (ST‐segment elevation myocardial infarction [STEMI], Global Registry of Acute Coronary Events [GRACE] Score, renal dysfunction, and time to presentation), and inpatient care (reperfusion therapy).
Missing data on covariates were minimal. At baseline, only 5.1% of the sample was missing any covariate data, 0.6% was missing >1 covariate, and 0.3% was missing >2 covariates. At 12 months, each health outcome measure had missing information from between 21% and 23% of participants. Patients missing 12‐month outcomes who were excluded from the analysis were more likely to be of black race, less educated, unemployed, and uninsured. Patients missing 12‐month outcomes also had more comorbidities on admission, though clinical presentation and inpatient care did not vary. Our primary analysis excluded patients who died in the year post‐AMI (n=72; 2%) and those with loss to follow‐up (n=657; 19%). We therefore conducted a sensitivity analysis using multiple imputation for missing health outcome measures.
All statistical analyses were conducted with SAS software (version 9.2; SAS Institute Inc., Cary, NC).
Results
Baseline Characteristics by Sex and by Financial Group for the Overall Population
Of the 3437 patients in this cohort, 1049 (30.5%) reported having financial barriers to obtaining health care services and 708 (20.6%) reported financial barriers to taking medications (Table 1). Similar percentages of women and men reported financial barriers to health care services (31.3% vs 28.9%; P>0.1); however, significantly more women reported financial barriers to medications (22.3% vs 17.2%; P<0.01). These sex differences in financial barriers to medication persisted even after adjustment for demographics and cardiovascular risk factors (odds ratio [OR], 1.23; 95% CI, 1.01–1.51; Table 2). In addition, a greater percentage of women than men reported not having enough money to make ends meet at the end of the month, finding it difficult to receive care, and feeling that their medical costs in the past year were a moderate or a severe burden (all P<0.01).
Table 1.
Socioeconomic Characteristics of the Study Population by Sex
| Overall (N=3437) | Women (N=2306) | Men (N=1131) | P Value | |
|---|---|---|---|---|
| Demographic | ||||
| Age, mean (SD), y | 47.0 (6.2) | 47.0 (6.3) | 46.9 (6.0) | 0.660 |
| Race/ethnicity | <0.001 | |||
| White | 2693 (78.5) | 1750 (76.0) | 943 (83.5) | |
| Black | 539 (15.7) | 428 (18.6) | 111 (9.8) | |
| Other | 199 (5.8) | 124 (5.4) | 75 (6.6) | |
| Partnership status | <0.001 | |||
| Married | 1762 (51.8) | 1109 (48.6) | 653 (58.4) | |
| Living with partner | 231 (6.8) | 160 (7.0) | 71 (6.3) | |
| Divorced/separated/widowed | 944 (27.8) | 710 (31.1) | 234 (20.9) | |
| Single (never married) | 464 (13.6) | 303 (13.3) | 161 (14.4) | |
| Live alone | 431 (12.6) | 269 (11.7) | 162 (14.4) | 0.026 |
| Education status | 0.128 | |||
| <High school | 181 (5.4) | 134 (5.9) | 47 (4.3) | |
| Some high school | 1384 (41.0) | 921 (40.6) | 463 (41.9) | |
| >High school graduate | 1812 (53.7) | 1216 (53.4) | 596 (53.9) | |
| Employment | <0.001 | |||
| Full time | 1754 (51.3) | 1002 (43.6) | 752 (67.1) | |
| Part time | 362 (10.6) | 293 (12.8) | 69 (6.2) | |
| Unemployed | 1301 (38.1) | 1001 (43.6) | 300 (26.8) | |
| Socioeconomic | ||||
| Finances at end of month | <0.001 | |||
| Some money left over | 1013 (29.7) | 591 (25.9) | 422 (37.6) | |
| Just enough to make ends meet | 1279 (37.6) | 856 (37.5) | 423 (37.7) | |
| Not enough to make ends meet | 1114 (32.7) | 836 (36.6) | 278 (24.8) | |
| Health insurance type | <0.001 | |||
| None | 674 (20.1) | 432 (19.2) | 242 (22.0) | |
| Commercial/PPO | 1140 (34.0) | 719 (31.9) | 421 (38.2) | |
| HMO | 424 (12.6) | 277 (12.3) | 147 (13.3) | |
| Government (VA, CMS) | 510 (15.2) | 401 (17.8) | 109 (9.9) | |
| Other | 607 (18.1) | 424 (18.8) | 183 (16.6) | |
| Healthcare utilization and access | ||||
| Out‐of‐pocket spending ($) | 0.005 | |||
| 0 to 99 | 2505 (77.3) | 1664 (76.1) | 841 (79.8) | |
| 100 to 499 | 661 (20.4) | 478 (21.9) | 183 (17.4) | |
| >500 | 74 (2.3) | 44 (2.0) | 30 (2.9) | <0.001 |
| No PCP | 427 (12.5) | 227 (9.9) | 200 (17.9) | |
| Difficulty receiving care | 0.008 | |||
| Difficult | 550 (16.0) | 384 (16.7) | 166 (14.7) | |
| Somewhat difficult | 339 (9.9) | 248 (10.8) | 91 (8.1) | |
| Not difficult | 2543 (74.1) | 1671 (72.6) | 872 (77.2) | |
| Medical costs are an economic Burden (past 1 year) | <0.001 | |||
| Severe burden | 461 (13.5) | 330 (14.4) | 131 (11.6) | |
| Moderate burden | 1021 (29.8) | 727 (31.7) | 294 (26.1) | |
| Not a burden | 1941 (56.7) | 1240 (54.0) | 701 (62.3) | |
ACEI indicates angiotensin‐converting enzyme inhibitor; ARB, angiotensin II receptor blockers; CABG, coronary artery bypass grafting; CMS, Center for Medicare and Medicaid Services; ESSI, ENRICHD Social Support Inventory; HMO, health management organization; LVEF, left ventricular ejection fraction; OB/GYN, obstetrics and gynecology; PCI, percutaneous coronary intervention; PCP, primary care physician; PHQ‐9, Patient Health Questionnaire; PPO, preferred provider organization; VA, Veterans Affairs.
Table 2.
Adjusted Odds of Having Financial Barriers by Sex
| Odds Ratio for Female Sex (95% CI) | P Value For Female Sex | Covariates Included in the Model |
|---|---|---|
| Financial barriers to services | ||
| 1.12 (0.96–1.31) | 0.152 | Sex |
| 1.11 (0.95–1.30) | 0.198 | Sex, age, race |
| 0.95 (0.80–1.12) | 0.514 | Sex, age, race, marital status, education, employment, cardiovascular risk factorsa |
| Financial barriers to medications | ||
| 1.39 (1.15–1.66) | 0.001 | Sex |
| 1.35 (1.12–1.62) | 0.002 | Sex, age, race |
| 1.23 (1.01–1.51) | 0.038 | Sex, age, race, marital status, education, employment, cardiovascular risk factorsa |
AMI indicates acute myocardial infarction; BMI, body mass index.
Includes diabetes mellitus, hypertension, past AMI, heart failure, stroke, smoking status, and BMI (groups).
Women and men reporting at least 1 financial barrier, compared to the group with no financial barriers, were more likely to be single, less educated, unemployed, and uninsured. They were also more likely to report lower social support and lacking sufficient finances to make ends meet (Tables 3 and 4). Women and men with any financial barrier, compared to the group without barriers, reported higher out‐of‐pocket spending, greater difficulty receiving care, less access to a primary care physician (PCP), and greater economic burden from medical costs. Delivery of reperfusion therapy, aspirin on admission, and aspirin at discharge did not vary by the presence of financial barriers (all P>0.05).
Table 3.
Baseline Characteristics by Financial Barriers to Health Care in Women (N=2306)
| Financial Barriers | |||||
|---|---|---|---|---|---|
| None (N=1465) | Services Only (N=327) | Medications Only (N=119) | Services and Medications (N=395) | P Valuea | |
| Demographic | |||||
| Age, mean (SD), y | 46.9 (6.4) | 47.2 (6.6) | 47.3 (5.3) | 47.2 (5.9) | 0.708 |
| Race/ethnicity | 0.233 | ||||
| White | 1110 (76.0) | 250 (76.5) | 89 (74.8) | 301 (76.2) | |
| Black | 261 (17.8) | 60 (18.3) | 27 (22.7) | 80 (20.3) | |
| Other | 90 (6.2) | 17 (5.2) | 3 (2.5) | 14 (3.5) | |
| Partnership status | <0.001 | ||||
| Married | 772 (53.2) | 143 (44.3) | 44 (37.0) | 150 (38.5) | |
| Living with partner | 99 (6.8) | 17 (5.2) | 13 (10.9) | 31 (8.0) | |
| Divorced/separated/widowed | 398 (27.5) | 112 (34.7) | 42 (35.3) | 158 (40.5) | |
| Single (never married) | 181 (12.5) | 51 (15.8) | 20 (16.8) | 51 (13.0) | |
| Live alone | 161 (11.0) | 44 (13.5) | 12 (10.1) | 52 (13.2) | 0.433 |
| Education status | <0.001 | ||||
| <High school | 112 (7.8) | 9 (2.8) | 3 (2.5) | 10 (2.5) | |
| Some high school | 541 (37.6) | 139 (43.0) | 62 (52.1) | 179 (45.7) | |
| >High school graduate | 784 (54.6) | 175 (54.2) | 54 (45.4) | 203 (51.8) | |
| Employment | <0.001 | ||||
| Full time | 707 (48.5) | 120 (37.0) | 39 (32.8) | 136 (34.4) | |
| Part time | 167 (11.5) | 57 (17.5) | 16 (13.4) | 53 (13.4) | |
| Unemployed | 583 (40.0) | 148 (45.5) | 64 (53.8) | 206 (52.2) | |
| Socioeconomic | |||||
| Finances at end of month | <0.001 | ||||
| Some money left over | 511 (35.3) | 47 (14.4) | 11 (9.3) | 22 (5.6) | |
| Just enough to make ends meet | 542 (37.4) | 136 (41.7) | 41 (34.8) | 137 (35.0) | |
| Not enough to make ends meet | 395 (27.3) | 143 (43.9) | 66 (55.9) | 232 (59.3) | |
| Health insurance type | <0.001 | ||||
| None | 84 (5.9) | 141 (43.5) | 17 (14.7) | 190 (49.0) | |
| Commercial/PPO | 524 (36.7) | 81 (25.0) | 35 (30.2) | 79 (20.3) | |
| HMO | 204 (14.3) | 31 (9.6) | 12 (10.3) | 30 (7.7) | |
| Government (VA, CMS) | 270 (19.0) | 40 (12.4) | 31 (26.7) | 60 (15.5) | |
| Other | 343 (24.1) | 31 (9.5) | 21 (18.1) | 29 (7.5) | |
| Health care utilization and access | |||||
| No PCP | 85 (5.8) | 60 (18.4) | 8 (6.7) | 74 (18.8) | <0.001 |
| Difficulty receiving care | <0.001 | ||||
| Difficult | 105 (7.2) | 88 (27.0) | 19 (16.0) | 172 (43.7) | |
| Somewhat difficult | 114 (7.8) | 51 (15.6) | 11 (9.2) | 72 (18.3) | |
| Not difficult | 1245 (85.0) | 187 (57.4) | 89 (74.8) | 150 (38.0) | |
| Risk factors and comorbidities | |||||
| Hypertension | 865 (59.0) | 213 (65.1) | 94 (79.0) | 305 (77.2) | <0.001 |
| Diabetes mellitus | 515 (35.2) | 131 (40.1) | 59 (49.6) | 193 (48.9) | <0.001 |
| BMI, kg/m2 | <0.001 | ||||
| 18.5–25.0 | 370 (25.3) | 61 (18.7) | 26 (21.9) | 57 (14.4) | |
| 25–30 | 421 (28.7) | 71 (21.7) | 30 (25.2) | 90 (22.8) | |
| 30–35 | 319 (21.8) | 75 (22.9) | 26 (21.9) | 101 (25.6) | |
| >35 | 355 (24.2) | 120 (36.7) | 37 (31.0) | 147 (37.2) | |
| COPD | 178 (12.2) | 28 (8.6) | 26 (21.9) | 57 (14.4) | 0.001 |
| Previous MI | 235 (16.0) | 51 (15.6) | 39 (32.8) | 110 (27.9) | <0.001 |
| Congestive heart failure | 71 (4.9) | 12 (3.7) | 7 (5.9) | 26 (6.6) | 0.315 |
| Past stroke | 68 (4.6) | 11 (3.4) | 14 (11.8) | 24 (6.1) | 0.002 |
| Smoking history | <0.001 | ||||
| Never smoker | 462 (31.5) | 77 (23.5) | 30 (25.2) | 85 (21.5) | |
| Past smoker | 242 (16.5) | 67 (20.5) | 20 (16.8) | 49 (12.4) | |
| Current smoker | 761 (52.0) | 183 (56.0) | 69 (58.0) | 261 (66.1) | |
| Alcohol abuse | 53 (3.6) | 22 (6.8) | 5 (4.2) | 24 (6.1) | 0.034 |
| Low social support (ESSI) | 160 (11.1) | 57 (17.8) | 15 (12.8) | 86 (22.1) | <0.001 |
| Diagnosed depression before MI | 645 (44.0) | 147 (45.0) | 77 (64.7) | 242 (61.3) | <0.001 |
| Clinical presentation | |||||
| Time to presentation >6 hours | 641 (43.9) | 160 (49.2) | 54 (45.4) | 174 (44.4) | 0.372 |
| GRACE score, mean (SD) | 75.1 (18.4) | 74.3 (19.8) | 77.2 (18.3) | 76.9 (19.3) | 0.162 |
| ST‐segment elevation AMI | 719 (49.1) | 151 (46.2) | 64 (53.8) | 168 (42.5) | 0.060 |
| Renal dysfunction | 150 (10.3) | 39 (11.9) | 18 (15.1) | 58 (14.8) | 0.052 |
| Inpatient care | |||||
| Reperfusion therapy | 0.416 | ||||
| None | 28 (1.9) | 2 (0.6) | 2 (1.7) | 7 (1.8) | |
| Catheterization only | 362 (24.7) | 74 (22.6) | 22 (18.5) | 89 (22.5) | |
| PCI/CABG | 1075 (73.4) | 251 (76.8) | 95 (79.8) | 299 (75.7) | |
| Aspirin on admission | 1394 (97.3) | 312 (96.9) | 109 (95.6) | 378 (97.7) | 0.678 |
| Aspirin at discharge | 1398 (97.8) | 316 (98.1) | 113 (100) | 380 (97.4) | 0.391 |
| Beta‐blockers at discharge | 1278 (94.4) | 293 (96.1) | 104 (94.6) | 361 (97.6) | 0.070 |
ACEI indicates angiotensin‐converting enzyme inhibitor; AMI, acute myocardial infarction; ARB, angiotensin II receptor blockers; BMI, body mass index; CABG, coronary artery bypass grafting; CMS, Center for Medicare and Medicaid Services; ESSI, ENRICHD Social Support Inventory; GRACE, Global Registry of Acute Coronary Event; HMO, health management organization; LVEF, left ventricular ejection fraction; MI, myocardial infarction; PCI, percutaneous coronary intervention; PCP, primary care physician; PHQ‐9, Patient Health Questionnaire; PPO, preferred provider organization; VA, Veterans Affairs.
P values indicate global statistical significance for the values reported in all 4 financial barrier groups.
Table 4.
Baseline Characteristics by Financial Barriers to Health Care in Men (N=1131)
| Financial Barriers | |||||
|---|---|---|---|---|---|
| None (N=766) | Services Only (N=171) | Medications Only (N=38) | Services and Medications (N=156) | P Valuea | |
| Demographic | |||||
| Age, mean (SD), y | 46.9 (5.9) | 46.5 (6.3) | 48.3 (5.9) | 47.0 (5.7) | 0.432 |
| Race/ethnicity | 0.008 | ||||
| White | 652 (85.2) | 145 (85.3) | 28 (73.7) | 118 (75.6) | |
| Black | 66 (8.6) | 14 (8.2) | 4 (10.5) | 27 (17.3) | |
| Other | 47 (6.2) | 11 (6.5) | 6 (15.8) | 11 (7.1) | |
| Partnership status | <0.001 | ||||
| Married | 481 (63.7) | 84 (49.1) | 25 (65.8) | 63 (40.7) | |
| Living with partner | 46 (6.1) | 13 (7.6) | 1 (2.6) | 11 (7.1) | |
| Divorced/separated/widowed | 128 (17.0) | 51 (29.8) | 7 (18.4) | 48 (31.0) | |
| Single (never married) | 100 (13.2) | 23 (13.5) | 5 (13.2) | 33 (21.2) | |
| Live alone | 101 (13.3) | 24 (14.0) | 3 (7.9) | 34 (21.8) | 0.029 |
| Education status | <0.001 | ||||
| <High school | 40 (5.4) | 4 (2.4) | 2 (5.4) | 1 (0.6) | |
| Some high school | 280 (37.5) | 89 (52.4) | 12 (32.4) | 82 (53.6) | |
| >High school graduate | 426 (57.1) | 77 (45.2) | 23 (62.2) | 70 (45.8) | |
| Employment | <0.001 | ||||
| Full time | 566 (74.8) | 91 (53.2) | 25 (65.8) | 70 (45.2) | |
| Part time | 34 (4.5) | 15 (8.8) | 3 (7.9) | 17 (11.0) | |
| Unemployed | 157 (20.7) | 65 (38.0) | 10 (26.3) | 68 (43.8) | |
| Socioeconomic | |||||
| Finances at end of month | <0.001 | ||||
| Some money left over | 364 (48.0) | 36 (21.1) | 9 (24.3) | 13 (8.3) | |
| Just enough to make ends meet | 276 (36.4) | 77 (45.0) | 12 (32.4) | 58 (37.2) | |
| Not enough to make ends meet | 119 (15.6) | 58 (33.9) | 16 (43.3) | 85 (54.5) | |
| Health insurance type | <0.001 | ||||
| None | 56 (7.5) | 86 (51.2) | 7 (18.4) | 93 (61.2) | |
| Commercial/PPO | 334 (44.9) | 36 (21.4) | 17 (44.7) | 34 (22.4) | |
| HMO | 117 (15.7) | 15 (8.9) | 6 (15.8) | 9 (5.9) | |
| Government (VA, CMS) | 68 (9.2) | 22 (13.1) | 3 (7.9) | 16 (10.5) | |
| Other | 169 (22.7) | 9 (5.4) | 5 (13.2) | 0 (0) | |
| Health care utilization and access | |||||
| No PCP | 82 (10.9) | 59 (34.5) | 6 (16.2) | 53 (34.4) | <0.001 |
| Difficulty receiving care | <0.001 | ||||
| Difficult | 40 (5.2) | 48 (28.0) | 7 (18.4) | 71 (45.8) | |
| Somewhat difficult | 40 (5.2) | 23 (13.5) | 5 (13.2) | 23 (14.8) | |
| Not difficult | 685 (89.6) | 100 (58.5) | 26 (68.4) | 61 (39.4) | |
| Risk factors and comorbidities | |||||
| Hypertension | 449 (58.6) | 112 (65.5) | 29 (76.3) | 118 (75.6) | <0.001 |
| Diabetes mellitus | 184 (24.0) | 45 (26.3) | 13 (34.2) | 59 (37.8) | 0.003 |
| BMI, kg/m2 | 0.338 | ||||
| 18.5–25.0 | 124 (16.2) | 29 (17.0) | 8 (21.1) | 16 (10.2) | |
| 25–30 | 317 (41.4) | 67 (39.2) | 13 (34.2) | 55 (35.3) | |
| 30–35 | 183 (23.9) | 45 (26.3) | 10 (26.3) | 48 (30.8) | |
| >35 | 142 (18.5) | 30 (17.5) | 7 (18.4) | 37 (23.7) | |
| COPD | 31 (4.1) | 10 (5.9) | 7 (18.4) | 12 (7.7) | <0.001 |
| Previous MI | 115 (15.0) | 41 (24.0) | 12 (31.6) | 65 (41.7) | <0.001 |
| Congestive heart failure | 16 (2.1) | 2 (1.2) | 1 (2.6) | 5 (3.2) | 0.642 |
| Past stroke | 13 (1.7) | 6 (3.5) | 2 (5.3) | 6 (3.9) | 0.155 |
| Smoking history | <0.001 | ||||
| Never smoker | 228 (29.8) | 41 (24.0) | 6 (15.8) | 26 (16.7) | |
| Past smoker | 158 (20.7) | 28 (16.4) | 12 (31.6) | 17 (17.3) | |
| Current smoker | 379 (49.5) | 102 (59.6) | 20 (52.6) | 103 (66.0) | |
| Alcohol abuse | 75 (9.8) | 15 (8.8) | 6 (15.8) | 23 (14.8) | 0.166 |
| Low social support (ESSI) | 70 (9.4) | 40 (23.4) | 7 (18.9) | 34 (21.9) | <0.001 |
| Diagnosed depression before MI | 177 (23.1) | 34 (19.9) | 11 (29.0) | 48 (30.8) | 0.095 |
| Clinical presentation | |||||
| Time to presentation >6 hours | 261 (34.2) | 68 (40.0) | 17 (44.7) | 64 (41.0) | 0.159 |
| GRACE score, mean (SD) | 72.8 (18.4) | 71.8 (18.4) | 75.6 (17.0) | 75.8 (18.3) | 0.166 |
| ST‐segment elevation AMI | 462 (60.3) | 109 (63.7) | 18 (47.4) | 80 (51.3) | 0.044 |
| Renal dysfunction | 58 (7.6) | 10 (5.9) | 5 (13.2) | 16 (10.3) | 0.295 |
| Inpatient care | |||||
| Reperfusion therapy | 0.413 | ||||
| None | 5 (0.7) | 2 (1.2) | 1 (2.6) | 3 (1.9) | |
| Catheterization Only | 79 (10.3) | 13 (7.6) | 6 (15.8) | 15 (9.6) | |
| PCI/CABG | 682 (89.0) | 156 (91.2) | 31 (81.6) | 138 (88.5) | |
| Aspirin on admission | 744 (98.3) | 167 (98.2) | 37 (100) | 153 (98.1) | 0.875 |
| Aspirin at discharge | 745 (98.2) | 169 (98.8) | 38 (100) | 153 (98.7) | 0.753 |
| Beta‐blockers at discharge | 703 (96.6) | 161 (98.2) | 36 (94.7) | 148 (98.7) | 0.337 |
ACEI indicates angiotensin‐converting enzyme inhibitor; AMI, acute myocardial infarction; ARB, angiotensin II receptor blockers; BMI, body mass index; CABG, coronary artery bypass grafting; CMS, Center for Medicare and Medicaid Services; ESSI, ENRICHD Social Support Inventory; GRACE, Global Registry of Acute Coronary Event; HMO, health management organization; LVEF, left ventricular ejection fraction; MI, myocardial infarction; PCI, percutaneous coronary intervention; PCP, primary care physician; PHQ‐9, Patient Health Questionnaire; PPO, preferred provider organization; VA, Veterans Affairs.
P values indicate global statistical significance for the values reported in all 4 financial barrier groups.
Compared to patients with financial barriers to only medications, women and men with barriers to only services were more likely to report not having any health insurance, not having a PCP, and experiencing difficulty receiving care. By contrast, a greater proportion of patients with barriers to only medications reported not having enough money to make ends meet at the end of the month compared to patients with barriers to only services.
Women and men with at least 1 financial barrier had a greater prevalence of hypertension, diabetes mellitus, past MI, and smoking than patients without financial barriers. At baseline, women and men with at least 1 financial barrier reported lower functional status and quality‐of‐life scores, more depressive symptomatology, and more stress than patients with no financial barriers (Figures 1 and 2). Additionally, at baseline, women in any given financial barrier group reported poorer functional status and quality of life along with more depressive symptoms and stress than men in the peer financial group.
Figure 1.
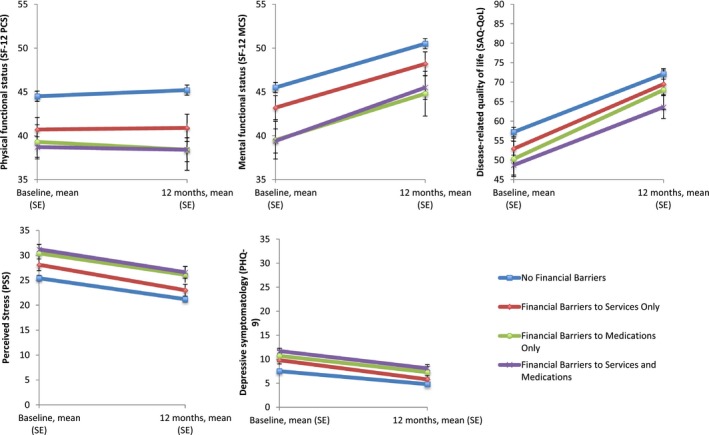
Unadjusted association of baseline financial barriers with 12‐month outcomes in women. Mean health status, quality of life, depression, and stress score trajectories at 12 months post‐AMI in patients with no financial barriers (blue lines), financial barriers to services only (red lines), financial barriers to medications only (green lines), and financial barriers to services and medications (purple lines). These values represent crude baseline 12‐month scores and are not adjusted for baseline health scores. AMI indicates acute myocardial infarction; MCS, Mental Component Summary; PCS, Physical Component Summary; PHQ‐9, Patient Health Questionnaire; PSS, Perceived Stress Scale; SAQ‐QoL, Seattle Angina Questionnaire–Quality of Life; SF‐12, 12‐Item Short‐Form.
Figure 2.
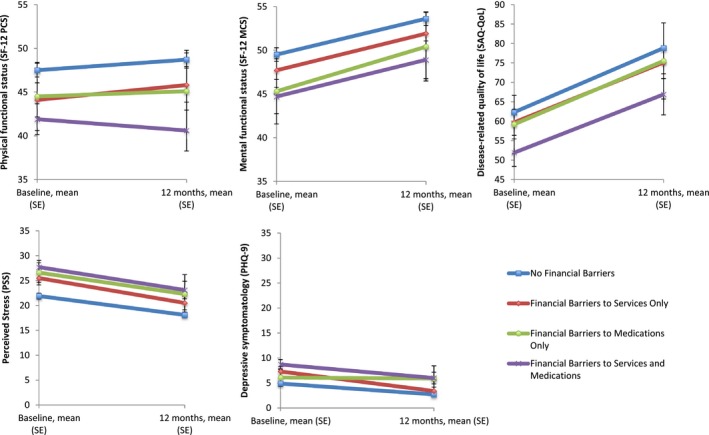
Unadjusted association of baseline financial barriers with 12‐month outcomes in men. Mean health status, quality of life, depression, and stress score trajectories at 12 months post‐AMI in patients with no financial barriers (blue lines), financial barriers to services only (red lines), financial barriers to medications only (green lines), and financial barriers to services and medications (purple lines). These values represent crude baseline 12‐month scores and are not adjusted for baseline health scores. AMI indicates acute myocardial infarction; MCS, Mental Component Summary; PCS, Physical Component Summary; PHQ‐9, Patient Health Questionnaire; PSS, Perceived Stress Scale; SAQ‐QoL, Seattle Angina Questionnaire–Quality of Life; SF‐12, 12‐Item Short‐Form.
Association of Financial Barriers With 12‐Month Health Outcomes
At 12 months following hospitalization for AMI, adults in the 4 financial barrier groups had higher unadjusted mental functional status, quality of life, and perceived stress scores compared with baseline (Figures 1 and 2). Additionally, most groups reported improved physical functional status and depressive symptomatology. However, 12‐month health status outcomes differed by financial barrier group. The group with no financial barriers reported the highest physical and mental functional status and quality‐of‐life scores and lowest depression and stress scores; by contrast, the group with financial barriers to both medications and services reported the lowest physical functional status and quality‐of‐life scores and highest depression and stress scores.
These associations remained similar after adjustment for baseline health and psychosocial status as well as demographic and clinical characteristics. After adjustment, in comparison to patients without financial barriers, women and men with financial barriers to both services and medications reported lower mental functional status (SF‐12 MCS: women, β −3.28, SE 0.73, P<0.001; men, β −3.35, SE 1.10, P=0.003), greater depressive symptomatology (PHQ‐9: women, β 2.18, SE 0.34, P<0.001; men, β 2.16, SE 0.54, P<0.001), lower quality of life (SAQ‐QoL: women, β −4.98, SE 1.50, P=0.001; men, β −7.66, SE 2.39, P=0.002), and higher perceived stress (PSS: women, β 3.76, SE ,0.61, P<0.001; men, β 3.90, SE 0.94, P<0.001; Figures 3 and 4). Women with financial barriers to both services and medications also reported lower physical status at 12 months (SF‐12 PCS: β −2.68, SE 0.66, P<0.001) than women without financial barriers. No interactions between sex and financial barriers were observed in any of the fully adjusted models (all P>0.1; Table 5). Analyses performed with missing data imputed show nearly identical results for all health outcomes.
Figure 3.
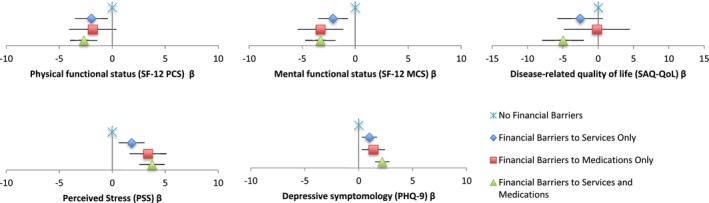
Adjusted mean differences in 12‐month outcomes between patients with and without financial barriers in women*. Adjusted mean health status, quality of life, depression, and stress score differences at 12 months post‐AMI in patients with no financial barriers (light blue), financial barriers to services only (dark blue), financial barriers to medications only (red), and financial barriers to services and medications (green). These values represent adjusted differences between baseline and 12‐month scores. Adjusted for demographic (age, sex, race, marital status, live alone, education, and employment), risk factors and comorbidities (diabetes mellitus, hypertension, smoking, past MI, COPD, heart failure, past stroke, depression [except in the PHQ‐9 model], low social support, alcohol abuse, and BMI groups), clinical presentation (STEMI, GRACE score, renal dysfunction, and time to presentation), and inpatient care (reperfusion therapy). AMI indicates acute myocardial infarction; BMI, body mass index; COPD, chronic obstructive pulmonary disorder; GRACE, Global Registry of Acute Coronary Event; MCS, Mental Component Summary; MI, myocardial infarction; PCS, Physical Component Summary; PHQ‐9, Patient Health Questionnaire; PSS, Perceived Stress Scale; SAQ‐QoL, Seattle Angina Questionnaire–Quality of Life; SF‐12, 12‐Item Short‐Form; STEMI, ST‐elevation myocardial infarction. *Reference category is “no financial barriers” group.
Figure 4.
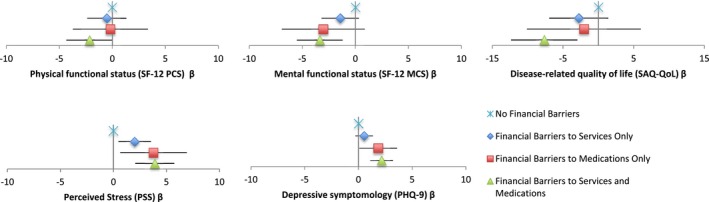
Adjusted mean differences in 12‐month outcomes between patients with and without financial barriers in men*. Adjusted mean health status, quality of life, depression, and stress score differences at 12 months post‐AMI in patients with no financial barriers (light blue), financial barriers to services only (dark blue), financial barriers to medications only (red), and financial barriers to services and medications (green). These values represent adjusted differences between baseline and 12‐month scores. Adjusted for demographic (age, sex, race, marital status, live alone, education, and employment), risk factors and comorbidities (diabetes mellitus, hypertension, smoking, past MI, COPD, heart failure, past stroke, depression [except in the PHQ‐9 model], low social support, alcohol abuse, and BMI groups), clinical presentation (STEMI, GRACE score, renal dysfunction, and time to presentation), and inpatient care (reperfusion therapy). AMI indicates acute myocardial infarction; BMI, body mass index; COPD, chronic obstructive pulmonary disorder; GRACE, Global Registry of Acute Coronary Event; MCS, Mental Component Summary; MI, myocardial infarction; PCS, Physical Component Summary; PHQ‐9, Patient Health Questionnaire; PSS, Perceived Stress Scale; SAQ‐QoL, Seattle Angina Questionnaire–Quality of Life; SF‐12, 12‐Item Short‐Form; STEMI, ST‐elevation myocardial infarction. *Reference category is “no financial barriers” group.
Table 5.
P Values for Interactions Between Sex and Financial Barriers in the Fully Adjusted Overall Model
| 12‐Month Health Status Outcome | P Value |
|---|---|
| Physical functional status (SF‐12 PCS) | |
| Female×barriers to services only | 0.357 |
| Female×barriers to medications only | 0.417 |
| Female×barriers to both services and medications | 0.558 |
| Mental functional status (SF‐12 MCS) | |
| Female×barriers to services only | 0.609 |
| Female×barriers to medications only | 0.858 |
| Female×barriers to both services and medications | 0.743 |
| Depressive symptomatology (PHQ‐9) | |
| Female×barriers to services only | 0.185 |
| Female×barriers to medications only | 0.398 |
| Female×barriers to services and medications | 0.854 |
| Disease‐related quality of life (SAQ‐QoL) | |
| Female×barriers to services only | 0.826 |
| Female×barriers to medications only | 0.633 |
| Female×barriers to both services and medications | 0.378 |
| Perceived stress (PSS) | |
| Female×barriers to services only | 0.558 |
| Female×barriers to medications only | 0.925 |
| Female×barriers to both services and medications | 0.943 |
MCS indicates Mental Component Summary; PCS, Physical Component Summary; PHQ‐9, Patient Health Questionnaire; PSS, Perceived Stress Scale; SAQ‐QoL, Seattle Angina Questionnaire–Quality of Life; SF‐12, 12‐Item Short‐Form.
Discussion
In this study of young women and men with AMI, financial barriers to health care were more common among women, though the negative association with health outcomes was similar by sex. Women and men with financial barriers to health care services and medications reported worse health and psychosocial status during the index hospitalization and 12 months later, manifested as poorer mental functional status, lower quality of life, greater depressive symptomatology, and higher perceived stress. These differences across financial barrier groups persisted after adjustment for potential confounding factors, including clinical comorbidities and baseline health status.
With over 3400 young patients and comprehensive data on socioeconomic status (SES), the VIRGO study provided an opportunity to fill a gap in understanding whether financial barriers contribute to sex‐based disparities in AMI outcomes among young men and women. We extend past literature showing a relationship between economic status and health outcomes among older populations with AMI by showing that financial barriers are common in the young adult population with AMI, with young women having a modestly greater prevalence of financial barriers than men.9, 10 These sex differences in prevalence may reflect the greater poverty, lower wages, or greater vulnerability to underinsurance that women in the general population face.11, 13 Moreover, the overall prevalence of financial barriers among young patients with AMI in VIRGO was higher than in other populations. Nearly 1 in 3 patients reported financial barriers to health care services and approximately 1 in 5 patients reported financial barriers to medications. Although these proportions are comparable to a Kaiser Family Foundation survey of the general population aged 18 to 65 years,11 they are higher than the rates of financial barriers to services (1 in 5) and medications (1 in 8) observed among older AMI patients in the Prospective Registry Evaluating Myocardial Infarction: Event and Recovery (PREMIER) study.9 Moreover, women were also more likely to report not having enough money to make ends meet at the end of the month, finding it difficult to receive care, and feeling that their medical costs in the past year were a moderate or a severe burden. Collectively, these findings convey that many young women experience substantial financial barriers impacting their ability to afford medications and receive the services they need.
However, contrary to our hypothesis that the effect of financial barriers on health outcomes would be stronger among women than among men with AMI, we did not find such a difference. Although the medical literature is limited, there is some evidence to suggest that sex may modify the effect of SES on health outcomes. For example, a recent study showed that the gap in life expectancy between people of low and high income varied by sex.30 Additionally, past work in other populations has found sex differences in the relationship between SES and health measures, including cardiovascular risk factors (obesity,31 hypertension,32 and diabetes mellitus33, 34, 35, 36) and outcomes.37, 38, 39, 40 A broader social science literature has also tried to disentangle the interplay between SES, sex, and health.41, 42 The findings of our study indicate that financial barriers to health care universally hamper recovery post‐AMI, regardless of sex. This observation may indicate that financial barriers act as an “equalizer,” such that the continued need to access costly services and guideline‐based medications recommended for optimal recovery post‐AMI is jeopardized for men and women with financial barriers equally.43, 44 Taken together, these findings suggest that financial barriers are a risk factor for poor health outcomes post‐AMI for both young women and men.
There are several explanations as to why patients with financial barriers may have poorer 12‐month health outcomes than patients without barriers. In our study, we found that the gap in health status, quality of life, stress, and depression between patients with and without financial barriers was present at the time of AMI and then persisted at 12 months, suggesting that patients with financial barriers are at a disadvantage at all points during recovery. However, this relationship between financial barriers and adverse 12‐month outcomes remained even after adjustment for baseline health and psychosocial status. Additionally, patients with financial barriers may utilize health care resources at lower rates than patients without financial barriers post‐AMI. Indeed, we found that women and men in this study with financial barriers to both medications and services were more likely than patients with no financial barriers 1 month post‐AMI to report not adhering to medications (12.4% vs 6.0%), greater difficulty scheduling follow‐up visits (12.0% vs 3.0%), and higher rates of not participating in cardiac rehabilitation after referral attributed to cost (48.0% vs 15.6%). Moreover, the economic burden of medical costs may have downstream effects on psychosocial health and quality of life for patients with financial barriers. In VIRGO, patients with financial barriers were more likely to report that their medical costs were a severe economic burden (41.8% vs 10.8%) and had greater out‐of‐pocket spending on health care than patients with no financial barriers at 1 month post‐AMI.
There are numerous implications of our findings. Although we are unable to draw inferences about cause and effect in an observational study, our results suggest that self‐reported financial barriers may identify young patients at risk for poor outcomes post‐AMI. Future research and interventions focusing on the determinants of financial barriers that are specific to young adults, including individual‐level factors (eg, employment status, household income, insurance status, insurance premiums and co‐pays, caregiver responsibilities, and household chores) and community‐level factors (eg, neighborhood resources, access to primary care), would be beneficial. Additionally, the strong relationship between financial barriers and health outcomes emphasizes the need to address the downstream effects of these barriers on adoption of guidelines‐based care and self‐management, given that patients with financial barriers may be discharged with evidence‐based secondary prevention treatments that they cannot afford. Although a comprehensive review of effective interventions is beyond the scope of this article, initiatives that reduce uninsurance and underinsurance, such as expansion of state Medicaid programs and low‐premium health plans may be helpful in addressing some of the financial barriers to health care.45
This study has several limitations. First, with a small number of patients in certain financial barrier groups, there may be some imprecision in the derived estimates. However, this should have biased our results to the null. Second, 12‐month outcomes were missing in approximately one quarter of responders. Given that patients missing 12‐month outcomes data were more likely to be less educated, unemployed, and uninsured and had a greater disease burden, the association of financial barriers with post‐AMI outcomes may be underestimated in the present study. Nonetheless, analyses repeated using multiple imputations for missing health outcomes data showed nearly identical results. Third, we did not study the association between financial barriers and mortality, recurrent MI, or revascularization, given that these events were uncommon in this study cohort. In this observational study of sex differences in AMI outcomes, extensive in‐hospital interviews were conducted to obtain patients’ baseline health status. Although randomization did not exclude critically ill patients (and efforts were made to enroll them in the study), the nature of the study may have selected for a healthier population. Future research should seek to understand the relationship between financial barriers and these clinical outcomes among young adults with AMI. Fourth, the findings in our study may not be generalizable to patients with AMI seen at hospitals that did not participate in VIRGO. Nonetheless, the VIRGO study is the largest multicenter prospective study of young adults with AMI (including 103 sites in the United States and 24 in Spain) and has one of the largest cohorts of young adults aged ≤55 years hospitalized with AMI. The composition of the VIRGO study cohort is consistent with other studies of younger patients with AMI.46 Finally, we relied on self‐reported measures of financial barriers and health outcomes, which may be susceptible to potential biases of reporting. However, to the extent possible, we adopted validated self‐reported surveys that have been widely used among AMI populations. There has been no evidence of directional misclassification, whereby patients systematically under‐ or over‐report a finding.19, 20, 21, 22, 23, 24, 25, 26, 27, 28
This study observed that financial barriers to health care are common among young women and men with AMI and strongly associated with poor health outcomes 12 months after the event. These findings indicate that researchers, health care providers, and policy makers should continue to devote attention to patients who experience financial barriers to health care, which may capture the patient's experience more comprehensively than indirect measures like insurance status and income. Financial barriers are common, especially among young women, which may create stress and lead them to forego services or medications attributed to cost, thereby impacting outcomes. Future research aimed to improve post‐AMI health outcomes, such as health status, depression, stress, and quality of life, should consider how best to address financial barriers to health care and ameliorate their effect.
Sources of Funding
This work was supported by grant R01 HL081153 (VIRGO). IMJOVEN (Spanish component of VIRGO) is supported in Spain by the Fondo de Investigaciones Sanitarias del Institute Carlos III, Ministry of Science and Technology (PI 081614), and additional funds from the Centro Nacional de Investigaciones Cardiovasculares (CNIC). Dr Krumholz is supported by grant U01 HL105270‐05 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung and Blood Institute. Dr Spatz is supported by grant K12HS023000 from the Agency for Healthcare Research and Quality Patient Centered Outcomes Research (PCOR) Institutional Mentored Career Development Program.
Disclosures
Drs Krumholz and Spatz report receiving support from the Centers for Medicare and Medicaid Services to develop and maintain performance measures that are used in public reporting programs. Dr Krumholz is a recipient of research agreements from Medtronic and from Johnson & Johnson (Janssen), through Yale University, to develop methods of clinical trial data sharing and chairs a cardiac scientific advisory board for UnitedHealth. Dr Spertus reports owning the copyright to the Seattle‐Angina Questionnaire (SAQ). No other authors report conflicts of interest. The funding organizations had no role in the views presented in this piece.
(J Am Heart Assoc. 2016;5:e003923 doi: 10.1161/JAHA.116.003923)
References
- 1. Vaccarino V, Horwitz RI, Meehan TP, Petrillo MK, Radford MJ, Krumholz HM. Sex differences in mortality after myocardial infarction: evidence for a sex‐age interaction. Arch Intern Med. 1998;158:2054–2062. [DOI] [PubMed] [Google Scholar]
- 2. Vaccarino V, Parsons L, Every NR, Barron HV, Krumholz HM. Sex‐based differences in early mortality after myocardial infarction. N Engl J Med. 1999;341:217–225. [DOI] [PubMed] [Google Scholar]
- 3. Dreyer RP, Ranasinghe I, Wang Y, Dharmarajan K, Murugiah K, Nuti SV, Hsieh AF, Spertus JA, Krumholz HM. Sex differences in the rate, timing, and principal diagnoses of 30‐day readmissions in younger patients with acute myocardial infarction. Circulation. 2015;132:158–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dreyer RP, Wang Y, Strait KM, Lorenze NP, D'Onofrio G, Bueno H, Lichtman JH, Spertus JA, Krumholz HM. Gender differences in the trajectory of recovery in health status among young patients with acute myocardial infarction: results from the variation in recovery: role of gender on outcomes of young AMI patients (VIRGO) study. Circulation. 2015;131:1971–1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bucholz EM, Strait KM, Dreyer RP, Geda M, Spatz ES, Bueno H, Lichtman JH, D'Onofrio G, Spertus JA, Krumholz HM. Effect of low perceived social support on health outcomes in young patients with acute myocardial infarction: results from the VIRGO (variation in recovery: role of gender on outcomes of young AMI patients) study. J Am Heart Assoc. 2014;3:e001252 doi: 10.1161/JAHA.114.001252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gupta A, Chui P, Zhou S, Spertus JA, Geda M, Lorenze N, Lee I, D'Onofrio G, Lichtman JH, Alexander KP, Krumholz HM, Curtis JP. Frequency and effects of excess dosing of anticoagulants in patients ≤55 years with acute myocardial infarction who underwent percutaneous coronary intervention (from the VIRGO study). Am J Cardiol. 2015;116:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Leifheit‐Limson EC, D'Onofrio G, Daneshvar M, Geda M, Bueno H, Spertus JA, Krumholz HM, Lichtman JH. Sex differences in cardiac risk factors, perceived risk, and health care provider discussion of risk and risk modification among young patients with acute myocardial infarction: the VIRGO study. J Am Coll Cardiol. 2015;66:1949–1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dreyer RP, Xu X, Zhang W, Du X, Strait KM, Bierlein M, Bucholz EM, Geda M, Fox J, D'Onofrio G, Lichtman JH, Bueno H, Spertus JA, Krumholz HM. Return to work after acute myocardial infarction comparison between young women and men. Circ Cardiovasc Qual Outcomes. 2016;9:S45–S52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rahimi AR, Spertus JA, Reid KJ, Bernheim SM, Krumholz HM. Financial barriers to health care and outcomes after acute myocardial infarction. JAMA. 2007;297:1063–1072. [DOI] [PubMed] [Google Scholar]
- 10. Smolderen KG, Spertus JA, Nallamothu BK, Krumholz HM, Tang F, Ross JS, Ting HH, Alexander KP, Rathore SS, Chan PS. Health care insurance, financial concerns, and delays to hospital presentation in acute myocardial infarction. JAMA. 2010;303:1392–1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Salganicoff A, Ranji U, Beamesderfer A, Kurani N. Women and health care in the early years of the ACA: key findings from the 2013 Kaiser Women's Health Survey. 2014.
- 12. Shartzer A, Long SK, Benatar S. Health care costs are a barrier to care for many women. 2015.
- 13. Kaiser Family Foundation . Women's health insurance coverage. 2016.
- 14. U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau . Barriers to care and unmet need for care. Women's Health USA 2011.
- 15. Carman KG, Eibner C, Paddock SM. Trends in health insurance enrollment, 2013–15. Health Aff (Millwood). 2015;34:1044–1048. [DOI] [PubMed] [Google Scholar]
- 16. Smith JC, Medalia C. Health insurance coverage in the United States. US Department of Commerce, Economics and Statistics Administration, Bureau of the Census. 2014.
- 17. Parker K, Patten E. The sandwich generation: rising financial burdens for middle‐aged Americans. Pew Research Center, Social & Demographic Trends Project. 2013.
- 18. Lichtman JH, Lorenze NP, D'Onofrio G, Spertus JA, Lindau ST, Morgan TM, Herrin J, Bueno H, Mattera JA, Ridker PM, Krumholz HM. Variation in recovery: role of gender on outcomes of young AMI patients (VIRGO) study design. Circ Cardiovasc Qual Outcomes. 2010;3:684–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ware J, Kosinski M, Keller SD. A 12‐Item Short‐Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. [DOI] [PubMed] [Google Scholar]
- 20. Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Prodzinski J, McDonnell M, Fihn SD. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25:333–341. [DOI] [PubMed] [Google Scholar]
- 21. Krumholz HM, Peterson ED, Ayanian JZ, Chin MH, DeBusk RF, Goldman L, Kiefe CI, Powe NR, Rumsfeld JS, Spertus JA, Weintraub WS. Report of the National Heart, Lung, and Blood Institute working group on outcomes research in cardiovascular disease. Circulation. 2005;111:3158–3166. [DOI] [PubMed] [Google Scholar]
- 22. Spertus JA, Jones P, McDonell M, Fan V, Fihn SD. Health status predicts long‐term outcome in outpatients with coronary disease. Circulation. 2002;106:43–49. [DOI] [PubMed] [Google Scholar]
- 23. Mallik S. Depressive symptoms after acute myocardial infarction: evidence for highest rates in younger women. Arch Intern Med. 2006;166:876. [DOI] [PubMed] [Google Scholar]
- 24. Ruo B, Rumsfeld JS, Hlatky MA, Liu H, Browner WS, Whooley MA. Depressive symptoms and health‐related quality of life: the Heart and Soul Study. JAMA. 2003;290:215–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Whooley MA, de Jonge P, Vittinghoff E, Otte C, Moos R, Carney RM, Ali S, Dowray S, Na B, Feldman MD, Schiller NB, Browner WS. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA. 2008;300:2379–2388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self‐report version of PRIME‐MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–1744. [DOI] [PubMed] [Google Scholar]
- 27. Kroenke K, Spitzer RL, Williams JB. The PHQ‐9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 29. Georgiades A, Janszky I, Blom M, László KD, Ahnve S. Financial strain predicts recurrent events among women with coronary artery disease. Int J Cardiol. 2009;135:175–183. [DOI] [PubMed] [Google Scholar]
- 30. Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, Bergeron A, Cutler D. The association between income and life expectancy in the United States, 2001–2014. JAMA. 2016;315:1750–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wardle J, Waller J, Jarvis MJ. Sex differences in the association of socioeconomic status with obesity. Am J Public Health. 2002;92:1299–1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Baek T‐H, Lee H‐Y, Lim N‐K, Park H‐Y. Gender differences in the association between socioeconomic status and hypertension incidence: the Korean Genome and Epidemiology Study (KoGES). BMC Public Health. 2015;15:852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Müller G, Hartwig S, Greiser KH, Moebus S, Pundt N, Schipf S, Völzke H, Maier W, Meisinger C, Tamayo T, Rathmann W, Berger K. Gender differences in the association of individual social class and neighbourhood unemployment rate with prevalent type 2 diabetes mellitus: a cross‐sectional study from the DIAB‐CORE consortium. BMJ Open. 2013;3:e002601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tang M, Chen Y, Krewski D. Gender‐related differences in the association between socioeconomic status and self‐reported diabetes. Int J Epidemiol. 2003;32:381–385. [DOI] [PubMed] [Google Scholar]
- 35. Rathmann W, Haastert B, Icks A, Giani G, Holle R, Meisinger C, Mielck A. Sex differences in the associations of socioeconomic status with undiagnosed diabetes mellitus and impaired glucose tolerance in the elderly population: the KORA Survey 2000. Eur J Public Health. 2005;15:627–633. [DOI] [PubMed] [Google Scholar]
- 36. Robbins JM, Vaccarino V, Zhang H, Kasl SV. Socioeconomic status and type 2 diabetes in African American and non‐Hispanic white women and men: evidence from the Third National Health and Nutrition Examination Survey. Am J Public Health. 2001;91:76–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Fabreau GE, Leung AA, Southern DA, Knudtson ML, McWilliams JM, Ayanian JZ, Ghali WA. Sex, socioeconomic status, access to cardiac catheterization, and outcomes for acute coronary syndromes in the context of universal healthcare coverage. Circ Cardiovasc Qual Outcomes. 2014;7:540–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nishi A, Kawachi I, Shirai K, Hirai H, Jeong S, Kondo K. Sex/gender and socioeconomic differences in the predictive ability of self‐rated health for mortality. PLoS One. 2012;7:e30179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Salcedo N, Saez M, Bragulat B, Saurina C. Does the effect of gender modify the relationship between deprivation and mortality? BMC Public Health. 2012;12:574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bassuk SS, Berkman LF, Amick BC. Socioeconomic status and mortality among the elderly: findings from four US communities. Am J Epidemiol. 2002;155:520–533. [DOI] [PubMed] [Google Scholar]
- 41. Matthews S, Manor O, Power C. Social inequalities in health: are there gender differences? Soc Sci Med. 1999;48:49–60. [DOI] [PubMed] [Google Scholar]
- 42. Macintyre S, Hunt K. Socio‐economic position, gender and health: how do they interact? J Health Psychol. 1997;2:315–334. [DOI] [PubMed] [Google Scholar]
- 43. Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, Jaffe AS, Jneid H, Kelly RF, Kontos MC, Levine GN, Liebson PR, Mukherjee D, Peterson ED, Sabatine MS, Smalling RW, Zieman SJ; American College of Cardiology; American Heart Association Task Force on Practice Guidelines; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons; American Association for Clinical Chemistry . 2014 AHA/ACC guideline for the management of patients with non–ST‐elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64:e139–e228. [DOI] [PubMed] [Google Scholar]
- 44. O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis‐Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines . 2013 ACCF/AHA guideline for the management of ST‐elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:529–555. [DOI] [PubMed] [Google Scholar]
- 45. Obama B. United States health care reform: progress to date and next steps. JAMA. 2016;316:525–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Gupta A, Wang Y, Spertus JA, Geda M, Lorenze N, Nkonde‐Price C, D'Onofrio G, Lichtman JH, Krumholz HM. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol. 2014;64:337–345. [DOI] [PMC free article] [PubMed] [Google Scholar]


