Abstract
Adie’s pupil is characterised by pupil dilatation, segmental iris palsy, light-near dissociation, and slow re-dilatation. Most commonly, tonic pupils are unilateral and idiopathic, but can be caused by orbital disorders and autonomic neuropathies. There are only a few case reports of tonic pupils in patients with Sjögren’s syndrome, caused by an autoimmune ciliary ganglionitis. The authors report on two cases with bilateral tonic pupils as the initial manifestation of primary Sjögren’s syndrome. Both patients presented with blurred vision, bilateral tonic pupils, and sicca symptoms. The findings suggest that Sjögren’s syndrome should be considered in patients presenting with bilateral Adie’s tonic pupils.
Keywords: Adie’s tonic pupil; Sjögren’s syndrome
INTRODUCTION
Adie’s tonic pupil is characterised by pupil dilatation, segmental iris palsy, light-near dissociation, and slow re-dilatation. It results from damage to the ciliary ganglion, affecting the parasympathetic supply to the iris and ciliary body. Re-innervation and up-regulation of the post-synaptic receptors follows, a process known as denervation supersensitivity, classically demonstrated by pupillary constriction to very dilute concentrations of pilocarpine (0.0625–0.1%).1 However, the preferred dilutions of pilocarpine used in clinical practice include 0.1% and 0.125%, which are easier to re-constitute at the bedside. Holmes-Adie syndrome refers to tonic pupils associated with tendon areflexia, thought to be due to loss of different degrees of ciliary and spinal ganglia neurons.2 Most cases of tonic pupils are unilateral and idiopathic. Secondary causes include orbital tumours, inflammation, and trauma that affect the ciliary ganglion. Systemic dysautonomia from Guillain-Barré syndrome, diabetic autonomic neuropathy, amyloidosis, and hereditary neuropathies have also been reported to cause tonic pupils.3 There are only few reports of tonic pupils in patients with established Sjögren’s syndrome and evidence of co-existing peripheral neuropathy. The postulated mechanism of Adie’s tonic pupil in Sjögren’s syndrome is via an autoimmune ciliary ganglionitis.4 We report two cases of bilateral tonic pupils as the initial manifestation of primary Sjögren's syndrome. In both cases, informed consent to publish was obtained.
CASE REPORTS
Case 1
A 35-year-old Asian female presented with a 9-month history of intermittent redness of both eyes and blurring of near vision. On direct questioning, she reported daily, persistent dry eyes and dry mouth. She did not complain of other neurological, autonomic, or systemic symptoms and had no significant medical history. Both her parents had diabetes and hypertension. She was a non-smoker and did not consume alcohol or take any medication.
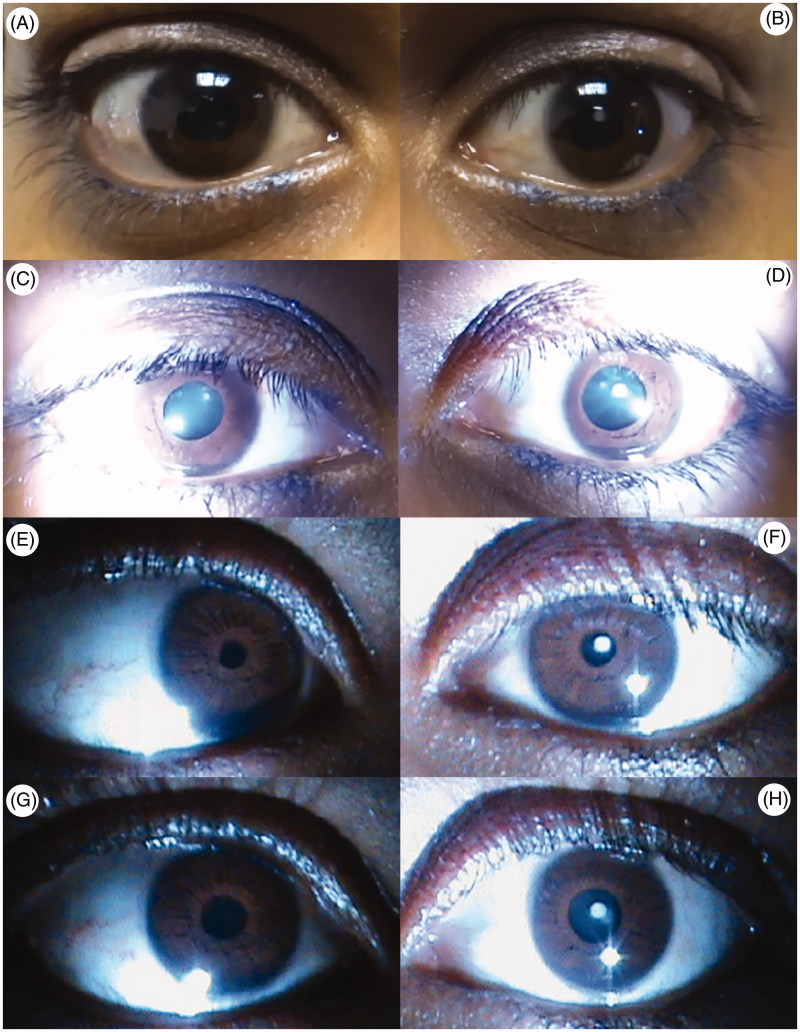
Neuro-ophthalmological examination revealed bilateral non-reactive pupils to direct light of 7 mm each (Figure 1C, D). On convergence, the pupils constricted and demonstrated slow re-dilatation (Figure 1E, F). After instillation of 0.1% pilocarpine, both pupils reduced in size (5 mm OS; 4 mm OD; Figure 1G, H). Slit-lamp examination revealed a small left central lens opacity, representing an early cataract. Best-corrected visual acuity was 6/6 OD and 6/9 OS. Tear film break up time was abnormally rapid in both eyes (2 seconds OD; 4 seconds OS), confirming severely dry eyes. The rest of her general and neurological examination was normal, including reflexes and sensation.
FIGURE 1.
Images of pupils, Case 1. Bilateral dilated pupils (A, B) that are non-reactive to direct light (C, D), but constrict on accommodation with slow re-dilatation suggesting tonicity (E, F), and their response to 0.1% pilocarpine demonstrating denervation supersensitivity (G, H), consistent with bilateral Adie’s pupils.
Laboratory investigations revealed an erythrocyte sedimentation rate (ESR) of 19 and normal glucose, rheumatoid factor (RF), and serum angiotensin-converting enzyme (SACE) levels. Syphilis serology was negative. Serum protein electrophoresis (SPEP) showed a polyclonal gammopathy. Autoimmune testing revealed positive anti-nuclear antibodies (ANA) with a titre of 1:640 and positive antibodies to Ro/SSA antigens (116.4 U/mL; reference range: 0–7 U/mL). Nerve conduction studies showed normal motor and sensory studies. Sympathetic skin response tested in both palms had normal amplitudes and latencies. Her cerebral magnetic resonance imaging (MRI) revealed a non-specific single T2 hyperinstensity in the left cerebral hemisphere, and cerebrospinal fluid (CSF) analysis was positive for oligoclonal bands with a normal immunoglobulin G (IgG) index, matched with serum oligoclonal bands. CSF chemistry, microbiology, virology, and cytology testing were all negative.
She was assessed as having isolated bilateral tonic pupils due to primary Sjögren’s syndrome and treated symptomatically for dry eyes. Steroids were not offered due to absence of clear benefit documented in previous studies.
Case 2
A 45-year-old Asian female presented with a 1-month history of numbness of the left side of her face and episodic blurring of vision. The episodes lasted a few minutes and occurred frequently throughout the day. She also complained of sicca symptoms. She was known to suffer from hypothyroidism and was well controlled on thyroid replacement therapy.
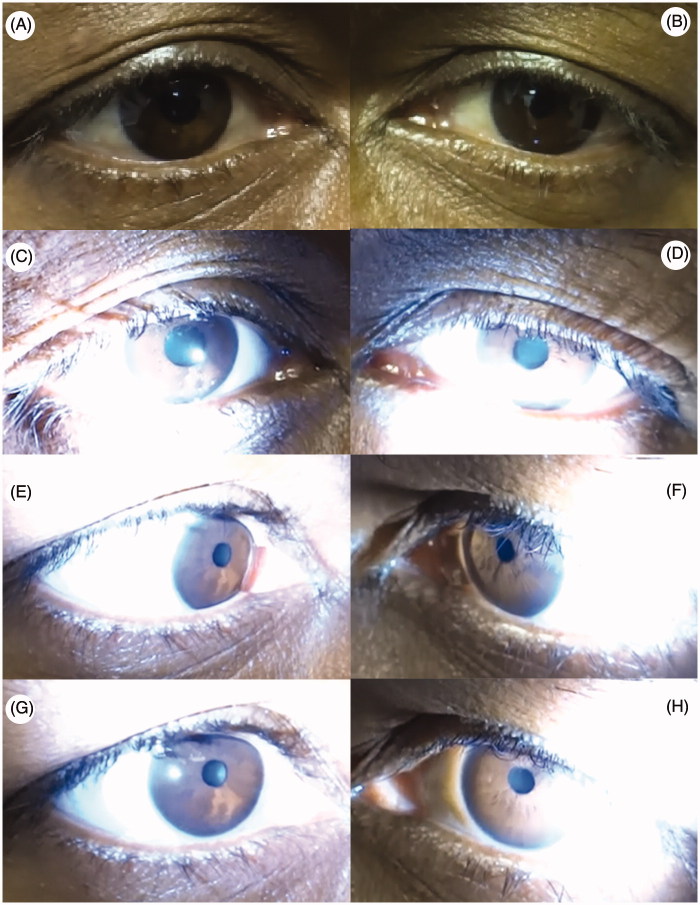
On examination, anisocoria was noted (5 mm OD and 4 mm OS). Both pupils displayed light-near dissociation with slow re-dilatation (Figure 2A–F). After instillation of dilute pilocarpine (0.1%), both pupils constricted (2.5 mm OU; Figure 2G, H). Funduscopy was normal and best-corrected visual acuity was 6/12 OD and 6/6 OS. Tear film break-up time was abnormally rapid (2–3 seconds OU), confirming severely dry eyes. Further examination revealed pain and light touch sensory loss in V1, 2, and 3 distributions of the left trigeminal nerve with associated reduced corneal sensation. She was hyporeflexic in her upper limbs and areflexic in her lower limbs. The rest of her general and neurological examination was normal.
FIGURE 2.
Images of pupils, Case 2. Bilateral dilated pupils (A, B) that are non-reactive to direct light (C, D), but constrict on accommodation with slow re-dilatation suggesting tonicity (E, F), and their response to 0.1% pilocarpine demonstrating denervation supersensitivity (G, H), consistent with bilateral Adie’s pupils.
Results of laboratory investigations included normal ESR, glucose, SACE, and RF, with SPEP showing a polyclonal gammopathy. Paraneoplastic antibodies and syphilis serology were negative. Autoimmune tests revealed positive ANA (titre 1:640), with positive antibodies to Ro/SSA antigens (271 U/mL; reference range: 0–7 U/mL). Nerve conduction studies showed normal motor and sensory studies. Blink reflex was absent on the left, confirming the left trigeminal neuropathy. Sympathetic skin responses were absent in both palms; however, reliability of the test was obscured by excessive interference. MRI of the brain and CSF results were all normal.
We concluded that she had Holmes-Adie syndrome and left trigeminal sensory neuropathy secondary to primary Sjögren’s syndrome. She was given a 5-day course of 30 mg daily intravenous immunoglobulin, after which her left sided facial symptoms resolved but pupils remained unchanged. She presented again 3 years later with recurrent sensory trigeminal neuropathy and persistence of features of the Holmes-Adie syndrome. A course of intravenous steroids was given without any measurable response.
DISCUSSION
Tonic pupils are considered an ocular manifestation of dysautonomia, most likely due to degeneration of the ciliary ganglion.4 The association of autonomic dysfunction and primary Sjögren’s syndrome has been established in previous studies.5 Newton et al.’s 2012 study of 317 patients with primary Sjögren’s syndrome demonstrated a 55% prevalence of dysautonomia, predominantly orthostatic hypotension.5 However, very few cases of tonic pupils have been reported in Sjögren’s syndrome.4,6–12
Our cases demonstrate bilateral tonic pupils as the initial manifestation of Sjögren’s-associated autonomic neuropathy/neuronopathy. Both patients were diagnosed as having primary Sjögren’s syndrome based on the revised international classification criteria for Sjögren’s syndrome.13 They both had sicca symptoms of dry eyes and mouth, reduced tear film break up times, and positive serological markers, fulfilling four of the six criteria, sufficient for diagnosis.
Neuropathy is the most common neurological complication of primary Sjögren’s syndrome, occurring in 5–15% of cases with variable involvement of sensory, motor, and autonomic fibres and ganglia.14,15 Vetrugno et al., Vermesch et al., and Waterschoot et al. all presented cases of Sjögren’s syndrome with bilateral tonic pupils and features of co-existent sensory neuropathy.4,6,8 Tajima et al. described a similar case with multiple mononeuritis.7 Goto et al. reported bilateral tonic pupils in a patient with Sjögren’s syndrome as part of a more extensive chronic autonomic neuropathy, including bilateral Horner syndrome, orthostatic hypotension, abnormal cardiovascular reflexes, and anihydrosis.10 In our second case, the Holmes-Adie syndrome with left sensory trigeminal neuropathy most likely reflects a shared process of autoimmune ganglionitis affecting sensory and autonomic ganglia in Sjögrens syndrome.
Case 1 had no clinical or electrophysiological evidence of sensorimotor polyneuropathy. The presence of bilateral tonic pupils as the only manifestation of neurological involvement in Sjögrens syndrome is rare, with only one other report by Bachmeyer et al.11 As described, most cases of tonic pupils in Sjögrens syndrome are bilateral; however, there have been two reports of unilateral involvement.4,9
In patient 2, similar to previous cases,4,6,11 steroids were ineffective in the treatment of Sjögren’s-associated tonic pupils. The use of intravenous immunoglobulin has been shown beneficial in patients with Sjögren's syndrome–associated neuropathy, particularly sensorimotor neuropathy.16 In this case, intravenous immunoglobulin was administered, resulting in improvement of her trigeminal neuropathy alone, with no clinical change in the underlying autonomic neuropathy. A previous case report using plasma exchange also showed recovery of the patient’s sensorimotor neuropathy, but Holmes-Adie syndrome remained unchanged.11 Thus, effective treatment of tonic pupils in Sjögren’s syndrome is yet to be established and in patients with minimal or no symptoms referable to the Adie’s pupil, intravenous immunoglobulin (IVIG) is certainly excessive. In such cases, it would therefore be more prudent to address the Sjögren’s-related sicca symptoms and systemic problems rather than the Adie’s pupil alone. Most patients with tonic pupils do not require treatment, unless symptomatic from accommodative impairment. Such cases can be managed with topical low dose pilocarpine or physostigmine.3
Bilateral Adie’s pupils, however, do provide an early indicator for the emergence of Sjögren’s syndrome, and a high index of suspicion is warranted in such a presentation.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- 1.Thompson HS. Adie's syndrome: some new observations. Trans Am Ophthalmol Soc 1977;75:587–626 [PMC free article] [PubMed] [Google Scholar]
- 2.Martinelli P, Minardi C. [Tonic pupil and tendon areflexia: the Holmes-Adie's syndrome]. Recenti Prog Med 2001;92:605–608. [Italian] [PubMed] [Google Scholar]
- 3.Lee AG. Tonic Pupil Walham: UpToDate Wolters Kluwer Health; 2014. Available at: http://www.yhdp.net/uptodate/contents/mobipreview.htm?43/5/44117?source=related_link#H7. Updated 23 January 2014. Accessed 15 October 2014
- 4.Vetrugno R, Liguori R, Cevoli S, Salvi F, Montagna P. Adie's tonic pupil as a manifestation of Sjögren's syndrome. Ital J Neurol Sci 1997;18:293–295 [DOI] [PubMed] [Google Scholar]
- 5.Newton JL, Frith J, Powell D, Hackett K, Wilton K, Bowman S, Price E, Pease C, Andrews J, Emery P, Hunter J, Gupta M, Vadivelu S, Giles I, Isenberg D, Lanyon P, Jones A, Marian Regan M, Annie Cooper A, Robert Moots R, Sutcliffe N, Bombardieri M, Pitzalis C, McLaren J, Young-Min S, Dasgupta B, Griffiths B, Dennis D, Mitchell S, Ng W-F. Autonomic symptoms are common and are associated with overall symptom burden and disease activity in primary Sjögren's syndrome. Ann Rheum Dis 2012;71:1973–1979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vermersch P, Dufourd-Delalande S, Defoort-Dhellemmes S, Stojkovic T, Launay D, de Seze J. [Tonic pupils in Sjögren's syndrome]. Rev Neurol 2005;161:963–966. [French] [DOI] [PubMed] [Google Scholar]
- 7.Tajima Y, Tsukishima E, Sudo K, Aimoto Y, Tashiro K. [A case of Sjögren syndrome associated with multiple mononeuritis and dysautonomia including bilateral tonic pupils]. No to shinkei [Brain and Nerve] 1997;49:825–828. [Japanese] [PubMed] [Google Scholar]
- 8.Waterschoot MP, Guerit JM, Lambert M, de Barsy T. Bilateral tonic pupils and polyneuropathy in Sjögren's syndrome: a common pathophysiological mechanism? Eur Neurol 1991;31:114–116 [DOI] [PubMed] [Google Scholar]
- 9.Gemignani F, Manganelli P, Pavesi G, Marbini A. Polyneuropathy in Sjögren's syndrome. A case of prevalently autonomic neuropathy with tonic pupil and hypohidrosis. Funct Neurol 1988;3:337–348 [PubMed] [Google Scholar]
- 10.Goto H, Matsuo H, Fukudome T, Shibuya N, Ohnishi A, Nakamura H. Chronic autonomic neuropathy in a patient with primary Sjögren's syndrome. J Neurol Neurosurg Psychiatry 2000;69:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bachmeyer C, Zuber M, Dupont S, Blanche P, Dhote R, Mas JL. Adie syndrome as the initial sign of primary Sjögren syndrome. Am J Ophthalmol 1997;123:691–692 [DOI] [PubMed] [Google Scholar]
- 12.Luong M, Jomir L, Labauge P, Dandurand M, Meunier L, Stoebner PE. Ross syndrome with sweating anomaly associated with Sjögren syndrome: an infrared thermo-graphic case study. Acta Dermato Venereol 2011;91:80–81 [DOI] [PubMed] [Google Scholar]
- 13.Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, Daniels TE, Fox PC, Fox RI, Kassan SS, Pillemer SR, Talal N, Weisman MH, European Study Group on Classification Criteria for Sjögren's Syndrome. Classification criteria for Sjögren's syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis 2002;61:554–558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berkowitz AL, Samuels MA. The neurology of Sjögren's syndrome and the rheumatology of peripheral neuropathy and myelitis. Pract Neurol 2014;14:14–22 [DOI] [PubMed] [Google Scholar]
- 15.Tobon GJ, Pers JO, Devauchelle-Pensec V, Youinou P. Neurological disorders in primary Sjögren's syndrome. Autoimmune Dis 2012;2012:645967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rist S, Sellam J, Hachulla E, Sordet C, Puechal X, Hatron PY, Benhamou CL, Sibilia J, Mariette X. Experience of intravenous immunoglobulin therapy in neuropathy associated with primary Sjögren's syndrome: a national multicentric retrospective study. Arthritis Care Res 2011;63:1339–1344 [DOI] [PubMed] [Google Scholar]