Key Points
A BRAF gene fusion and small in-frame BRAF deletions were found in a subset of LCH lesions lacking BRAF-V600E or MAP2K1 mutations.
In LCH model systems, responses to MAPK pathway inhibitors depend on the specific genetic alteration that drives ERK activation.
Abstract
Langerhans cell histiocytosis (LCH) is characterized by inflammatory lesions containing pathologic CD207+ dendritic cells with constitutively activated ERK. Mutually exclusive somatic mutations in MAPK pathway genes have been identified in ∼75% of LCH cases, including recurrent BRAF-V600E and MAP2K1 mutations. To elucidate mechanisms of ERK activation in the remaining 25% of patients, we performed whole-exome sequencing (WES, n = 6), targeted BRAF sequencing (n = 19), and/or whole-transcriptome sequencing (RNA-seq, n = 6) on 24 LCH patient samples lacking BRAF-V600E or MAP2K1 mutations. WES and BRAF sequencing identified in-frame BRAF deletions in the β3-αC loop in 6 lesions. RNA-seq revealed one case with an in-frame FAM73A-BRAF fusion lacking the BRAF autoinhibitory regulatory domain but retaining an intact kinase domain. High levels of phospho-ERK were detected in vitro in cells overexpressing either BRAF fusion or deletion constructs and ex vivo in CD207+ cells from lesions. ERK activation was resistant to BRAF-V600E inhibition, but responsive to both a second-generation BRAF inhibitor and a MEK inhibitor. These results support an emerging model of universal ERK-activating genetic alterations driving pathogenesis in LCH. A personalized approach in which patient-specific alterations are identified may be necessary to maximize benefit from targeted therapies for patients with LCH.
Introduction
Langerhans cell histiocytosis (LCH) is a myeloid neoplasia characterized by inflammatory lesions including characteristic CD1a+/CD207+ dendritic cells (DCs).1,2 MAPK activation is universal in LCH lesion DCs,3,4 resulting from mutually exclusive somatic activating mutations in MAPK pathway genes including BRAF-V600E (50%-65%), MAP2K1 (10%-20%), and case reports of other pathway members (ARAF and ERBB3).2,3,5,6 The mechanism of pathologic ERK activation in the remaining 25% of pediatric LCH patients remains undefined.
MAPK pathway activation is known to result from diverse genetic alterations in other cancer types.7,8 To identify and characterize such alternative mechanisms of aberrant MAPK pathway activation in LCH, we performed WES, RNA-seq, and targeted sequencing of BRAF on a cohort of LCH cases without BRAF-V600E or MAP2K1 mutations. Candidate alterations were validated by targeted DNA and/or RNA-based sequencing. Mutation function and response to MAPK pathway inhibitors were assessed using in vitro constructs and LCH lesion primary cells.
Study design
Study patients and samples
Biopsy tissue and blood samples were collected from patients with LCH under a protocol approved by the Baylor College of Medicine institutional review board. Patients with known BRAF-V600E mutation or exon 2-3 MAP2K1 mutations (as determined by previous quantitative polymerase chain reaction (PCR), targeted sequencing, or WES) were excluded from analysis. DNA and RNA extracted from peripheral white blood cells were used as the “normal” sample for comparison, with analytic methods to determine somatic mutation status allowing for low levels of circulating LCH cells in patients with high-risk disease. Clinical data were recorded for each patient (Table 1). Sequencing methods were prioritized based on availability of viably preserved lesions for CD207+ sorting as well as the quantity and quantity of nucleic acids extracted from frozen unpurified LCH lesion biopsies.
Table 1.
Clinical data and sequencing results for LCH cases without BRAF-V600E or MAP2K1 mutations
| Case | Dx | Age (y) | Disease burden | Progression or recurrence | WES | BRAF-seq | RNA- seq | BRAF alteration |
|---|---|---|---|---|---|---|---|---|
| LCH-01 | LCH | 1.7 | LR, multisystem, multiple lesions | Yes | No | Yes | No | Indel |
| LCH-02 | LCH | 3.5 | LR, multisystem, multiple lesions | Yes | Yes | No | Yes | Indel |
| LCH-03 | LCH | 16.4 | LR, multisystem, multiple lesions | Yes | Yes | Yes | Yes | Indel |
| LCH-04 | LCH | 40.6 | LR, multi-system, multiple lesions | Yes | No | Yes | No | Indel |
| LCH-05 | LCH | 8.1 | LR, single-system, single lesion | No | Yes | Yes | Yes | Indel |
| LCH-06 | LCH | 3.2 | LR, single-system, single lesion | No | No | Yes | Yes | Indel |
| LCH-07 | LCH | 14.9 | LR, single-system, single lesion | No | No | Yes | Yes | Fusion |
| LCH-08 | LCH | 1.2 | LR, single-system, multiple lesions | Yes | Yes | No | No | WT |
| LCH-09 | LCH/JXG | 6.7 | LR, single-system, multiple lesions | Yes | Yes | No | No | WT |
| LCH-10 | LCH | 0.7 | HR, multi-system, multiple lesions | Yes | Yes | No | No | WT |
| LCH-11 | LCH | 1.0 | HR, multi-system, multiple lesions | Yes | No | Yes | No | WT |
| LCH-12 | LCH | 5.8 | LR, multi-system, multiple lesions | Yes | No | Yes | No | WT |
| LCH-13 | LCH | 70.1 | HR, multi-system, multiple lesions | Yes | No | Yes | No | WT |
| LCH-14 | LCH | 30.5 | HR, multi-system, multiple lesions | Yes | No | Yes | No | WT |
| LCH-15 | LCH | 3.8 | LR, single-system, single lesion | No | No | Yes | No | WT |
| LCH-16 | LCH | 16.3 | LR, multi-system, multiple lesions | Yes | No | Yes | No | WT |
| LCH-17 | LCH | 8.6 | LR, single-system, single lesion | No | No | Yes | No | WT |
| LCH-18 | LCH | 2.1 | LR, single-system, multiple lesions | Yes | No | Yes | No | WT |
| LCH-19 | LCH | 29.9 | LR, multi-system, multiple lesions | No | No | Yes | No | WT |
| LCH-20 | LCH | 17.2 | LR, multi-system, multiple lesions | Yes | No | Yes | No | WT |
| LCH-21 | LCH | 0.1 | LR, single-system, multiple lesions | Yes | No | Yes | No | WT |
| LCH-22 | LCH | 0.1 | LR, single-system, single lesion | No | No | Yes | No | WT |
| LCH-23 | LCH | 1.9 | LR, multi-system, multiple lesions | No | No | Yes | No | WT |
| LCH-24 | LCH | 11.6 | HR, multi-system, multiple lesions | Yes | No | No | Yes | WT |
WES, BRAF-seq, and RNA-seq status refer to whether whole-exome sequencing (WES), targeted BRAF sequencing (BRAF-seq), and/or transcriptome sequencing (RNA-seq) were performed for that case. The shaded rows detail the information for patients with LCH in which alternative genetic alterations in BRAF were identified.
HR, high-risk; indel, in-frame deletion; JXG, juvenile xanthogranuloma; LCH, Langerhans cell histiocytosis; LR, low-risk; WT, wild-type.
Whole-exome sequencing
Illumina WES and orthogonal validation of putative mutations on the AmpliSeq mutation panel platform were performed as previously described2 using DNA isolated from sorted CD207+ cells from 6 LCH lesions (Table 1). Primary and somatic mutation data analyses are detailed in supplemental Methods, available on the Blood Web site.
Targeted BRAF gene sequencing
Targeted sequencing of the full BRAF coding sequence was performed on DNA extracted from 19 LCH lesions, including 2 cases from the WES cohort. Details are outlined in supplemental Methods and supplemental Table 1.
Transcriptome sequencing
RNA-seq was performed using total RNA extracted from 6 fresh-frozen LCH lesions. Of these 6 samples, 2 were also sequenced with both WES and targeted sequencing, 2 were sequenced using WES, and 2 were included in the targeted sequencing group. Details are outlined in supplemental Methods and Table 1.
FAM73A-BRAF fusion gene and BRAF deletion–targeted sequencing
Targeted DNA and/or RNA sequencing was performed to confirm the presence of candidate alterations. Details are outlined in supplemental Methods and supplemental Table 1.
Functional analysis of FAM73A-BRAF gene fusion and BRAF deletions
Functional analysis of BRAF mutations was analyzed by overexpression in HEK293 cells as well as in primary LCH lesions harboring the mutations as previously described.2 Details are outlined in supplemental Methods.
Results and discussion
We hypothesized that novel genomic alterations in MAPK genes may drive pathologic ERK activation in cases without known mutations, and we therefore performed RNA-seq on whole lesions as well as WES and/or targeted BRAF sequencing on lesions from a cohort of patients with LCH without previously identified BRAF-V600E or MAP2K1 mutations.1,9
FAM73A-BRAF fusion
In 1 of the 6 cases analyzed, RNA-seq revealed an interchromosomal fusion event involving the FAM73A (MIGA1) gene on chromosome 1p31.1 and the BRAF gene on chromosome 7q34 (GRCh37 genome coordinates for fusion junctions: chr1: 78 309 092 and chr7: 140 487 384). The chimeric FAM73A-BRAF gene was predicted to result in an in-frame protein lacking the autoinhibitory domain of BRAF (exons 1-8) but retaining an intact kinase domain (Figure 1A), as has been observed for other known BRAF fusion genes.7,8 The presence of the FAM73A-BRAF fusion was confirmed by reverse-transcription PCR with breakpoint-flanking primers and subsequent targeted sequencing (supplemental Figure 1). No BRAF fusion events have been previously been reported for LCH; however, somatic RNF11-BRAF and CLIP2-BRAF fusions resulting in constitutive MAPK pathway activation have been described in 2 patients with other histiocytic disorders.10
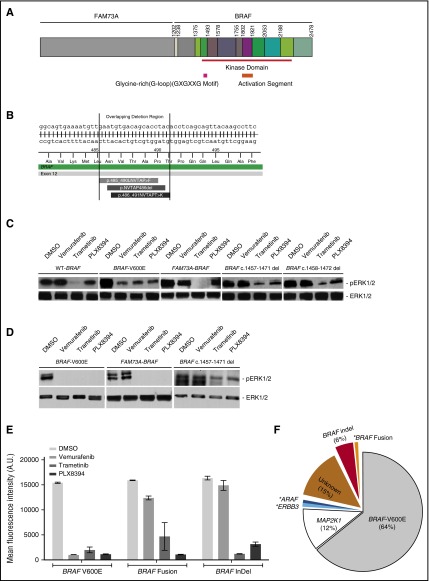
Figure 1.
Novel genomic alterations in BRAF in patients with LCH results in constitutive ERK activation, which is responsive to second-generation BRAF and MEK inhibitors but not to a BRAF-V600E inhibitor. (A) Illustration of the FAM73A-BRAF fusion identified in this study. (B) Illustration of the BRAF exon 12 in-frame deletions identified in this study. (C) HEK293 cells were transiently transfected with expression plasmids encoding the indicated BRAF wild-type, fusion, and mutant cDNAs, and corresponding lysates from cells maintained in serum were subjected to immunoblotting with the indicated antibodies. Where indicated, cells were treated with BRAF or MEK inhibitor for 4 hours before harvest. (D) LCH lesion biopsy cell suspension harboring indicated BRAF mutations or fusion were treated with BRAF or MEK inhibitor for 4 hours and corresponding lysates were subjected to immunoblotting with the indicated antibodies. (E) LCH lesion biopsy cell suspension harboring indicated BRAF mutations (BRAF-V600E or in-frame exon 12 deletions [indel]) or fusion (FAM73A-BRAF) were treated with BRAF or MEK inhibitor for 4 hours. Median fluorescent intensity (MFI) of p-ERK1/2 in CD207+ cells were determined through IFC analyses post treatment with various MAPK pathway inhibitors. (F) Pie chart showing the estimated distribution of genetic alterations identified in MAPK pathway genes in patients with LCH from an institutional cohort, including the novel BRAF fusion and deletions. The frequencies of MAPK pathway mutations were estimated based on previously reported data and the current study (supplemental Methods).2,4 The asterisk indicates single cases.
BRAF exon12 in-frame deletions
Small 15-bp in-frame deletions in BRAF (nucleotides 1455-1469, 1457-1471, or 1458-1472) were detected in LCH lesions by WES of DNA extracted from patient lesion–sorted CD207+ cells (3/6 cases analyzed) or targeted sequencing of the coding exons of BRAF (3/19 cases analyzed) (Figure 1B and supplemental Tables 2 and 3). Similar ERK-activating, in-frame BRAF deletions have recently been described in other malignancies.11-15 All BRAF deletions were localized to exon 12 (supplemental Table 2), which encodes the β3-αC loop. This region coordinates movements of 2 structural elements of the BRAF protein required for kinase activation and the deletions render BRAF resistant to “first-generation” BRAF-V600E inhibitors.13,16,17
Functional analysis and response to MAPK pathway inhibition
We assessed the functional impact of these genomic alterations on BRAF signaling by analyzing phosphorylation of downstream target ERK in HEK293 cells transiently transfected with wild-type BRAF, BRAF-V600E, BRAF deletion mutants, or BRAF fusion constructs (Figure 1C). cDNA expression of BRAF deletions and the FAM73A-BRAF fusion, but not wild-type BRAF, resulted in a significant increase in ERK1/2 phosphorylation (Figure 1C). Constitutive MAPK signaling by FAM73A-BRAF fusion is consistent with previously described hyperactive ERK phosphorylation by BRAF fusions in other cancers that retain the BRAF kinase domain without the N-terminal regulatory region.18,19
We next evaluated the ability of the small-molecule BRAF-V600E inhibitor vemurafenib, the BRAF inhibitor PLX8394,20 and the MEK inhibitor trametinib to suppress pathway activation by specific BRAF alterations (Figure 1C-E). PLX8394 is a second-generation BRAF inhibitor able to inhibit BRAF signaling without paradoxical activation of MAPK pathway signaling in cells with wild-type BRAF that has been observed in first-generation agents such as vemurafenib.20,21 Vemurafenib, PLX8394, and trametinib inhibited ERK1/2 phosphorylation in HEK293 cells transiently transfected with plasmids encoding BRAF-V600E (Figure 1C) and also in BRAF-V600E LCH lesion CD207+ cells (Figure 1D-E). By contrast, ERK activation by either FAM73A-BRAF fusion or in-frame BRAF deletions was relatively resistant to vemurafenib, but decreased significantly by exposure to PLX8394 and trametinib (Figure 1C-E). These results are consistent with specific activity of vemurafenib against BRAF-V600E monomers, compared with the activity of PLX8394 and trametinib against a broader range of activating BRAF mutations.22,23
Genomic landscape of LCH and implications for treatment strategies
Previous LCH studies have identified frequent BRAF-V600E (50%-65%) and MAP2K1 (10%-20%) mutations in ∼75% of cases.2,3,5,6,10 In this study, genomic and transcriptomic analyses revealed novel BRAF alterations in approximately one fourth of LCH lesions lacking those mutations: recurrent in-frame deletions in exon 12 (estimated 6% overall frequency) and a single case of a BRAF gene fusion (Figure 1F).2 Of note, this suggests that BRAF deletions are the third most common MAPK pathway alteration in LCH lesions. Molecular analysis of LCH patients treated in clinical trials may inform future risk stratification based on tumor genotype; for example, BRAF-V600E has been associated with increased risk of relapse in 2 large series.4,24 Identification of the specific MAPK pathway mutation present in each patient with LCH may also predict response to targeted agents and enable personalized medicine approaches, as demonstrated by our functional analyses. We believe that these data support the potential utility of a staged approach to molecular characterization of LCH lesions in which tests such as quantitative PCR or analyses of circulating tumor DNA are used to identify BRAF-V600E mutations,25,26 followed by high-coverage targeted sequencing of MAPK pathway genes in BRAF-V600E–negative patients. More extensive genomic and transcriptomic analyses (eg, WES, RNA-seq) could be reserved for cases that remain unsolved. In cases where pathologic DCs compose only a small fraction of the LCH lesion, isolation of CD207+ cells from fresh or viably preserved lesions may improve the diagnostic yield.2 Prospective studies will be required to determine optimal molecular testing strategies and evaluate the benefit of personalized treatment approaches for patients with LCH.
Acknowledgments
The authors thank Munu Bilgi, Linna Zhang, Maria S. Diaz, and Elizabeth Pacheco for data management support. PLX8394 was kindly provided by Plexxikon.
This study was supported in part by a Dan L. Duncan Cancer Center support grant (P30CA125123); the Lester and Sue Smith Foundation and the HistioCure Foundation (TXCH Histiocytosis Program); National Institutes of Health, National Cancer Institute grants R01 CA154489 (C.E.A. and K.L.M.), R01 CA154947 (M.M. and C.E.A.), SPORE in Lymphoma grant P50CA126752 (C.E.A.), and U54 HG003273 (D.A.W.); Alex’s Lemonade Stand Foundation Young Investigator Grant (R.C.); American Society of Hematology Scholar Award (R.C.); the St Baldrick’s Foundation (North American Consortium for Histiocytosis Research) (C.E.A., K.L.M., M.M., and D.W.P.); and Howard Hughes Medical Institute to the Baylor College of Medicine Med into Grad Initiative (K.P.H.L.).
Footnotes
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: R.C. and T.M.B. designed and performed research, collected data, analyzed and interpreted data, and wrote the manuscript; O.A.H. analyzed and interpreted data and wrote the manuscript; D.J.Z. designed and performed research and collected data; H.A., K.P.H.L., B.S., V.K., N.K., P.I.P., and M.M. performed research and collected data; D.A.W. designed research and analyzed and interpreted data; A.R. designed research; K.L.M., D.W.P., and C.E.A. designed research, analyzed and interpreted data, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: D. Williams Parsons, 1102 Bates St, Suite 1030.15, Houston, TX 77030; e-mail: dwparson@txch.org; and Carl Allen, 1102 Bates St., Suite 1025.22, Houston, TX 77030; e-mail: ceallen@txch.org.
References
- 1.Allen CE, Parsons DW. Biological and clinical significance of somatic mutations in Langerhans cell histiocytosis and related histiocytic neoplastic disorders. Hematol Am Soc Hematol Educ Program. 2015;2015:559-564. [DOI] [PubMed] [Google Scholar]
- 2.Chakraborty R, Hampton OA, Shen X, et al. . Mutually exclusive recurrent somatic mutations in MAP2K1 and BRAF support a central role for ERK activation in LCH pathogenesis. Blood. 2014;124(19):3007-3015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Badalian-Very G, Vergilio JA, Degar BA, et al. . Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood. 2010;116(11):1919-1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berres ML, Lim KP, Peters T, et al. . BRAF-V600E expression in precursor versus differentiated dendritic cells defines clinically distinct LCH risk groups. J Exp Med. 2015;212(2):281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nelson DS, Quispel W, Badalian-Very G, et al. . Somatic activating ARAF mutations in Langerhans cell histiocytosis. Blood. 2014;123(20):3152-3155. [DOI] [PubMed] [Google Scholar]
- 6.Nelson DS, van Halteren A, Quispel WT, et al. . MAP2K1 and MAP3K1 mutations in Langerhans cell histiocytosis. Genes Chromosomes Cancer. 2015;54(6):361-368. [DOI] [PubMed] [Google Scholar]
- 7.Collins VP, Jones DT, Giannini C. Pilocytic astrocytoma: pathology, molecular mechanisms and markers. Acta Neuropathol. 2015;129(6):775-788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ross JS, Wang K, Chmielecki J, et al. . The distribution of BRAF gene fusions in solid tumors and response to targeted therapy. Int J Cancer. 2016;138(4):881-890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rollins BJ. Genomic alterations in Langerhans cell histiocytosis. Hematol Oncol Clin North Am. 2015;29(5):839-851. [DOI] [PubMed] [Google Scholar]
- 10.Diamond EL, Durham BH, Haroche J, et al. . Diverse and targetable kinase alterations drive histiocytic neoplasms. Cancer Discov. 2016;6(2):154-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Estep AL, Palmer C, McCormick F, Rauen KA. Mutation analysis of BRAF, MEK1 and MEK2 in 15 ovarian cancer cell lines: implications for therapy. PLoS One. 2007;2(12):e1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fabbri G, Khiabanian H, Holmes AB, et al. . Genetic lesions associated with chronic lymphocytic leukemia transformation to Richter syndrome. J Exp Med. 2013;210(11):2273-2288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foster SA, Whalen DM, Özen A, et al. . Activation mechanism of oncogenic deletion mutations in BRAF, EGFR, and HER2. Cancer Cell. 2016;29(4):477-493. [DOI] [PubMed] [Google Scholar]
- 14.Hanrahan AJ, Schultz N, Westfal ML, et al. . Genomic complexity and AKT dependence in serous ovarian cancer. Cancer Discov. 2012;2(1):56-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jeck WR, Parker J, Carson CC, et al. . Targeted next generation sequencing identifies clinically actionable mutations in patients with melanoma. Pigment Cell Melanoma Res. 2014;27(4):653-663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Endicott JA, Noble ME, Johnson LN. The structural basis for control of eukaryotic protein kinases. Annu Rev Biochem. 2012;81:587-613. [DOI] [PubMed] [Google Scholar]
- 17.Chen SH, Zhang Y, Van Horn RD, et al. . Oncogenic BRAF deletions that function as homodimers and are sensitive to inhibition by RAF dimer inhibitor LY3009120. Cancer Discov. 2016;6(3):300-315. [DOI] [PubMed] [Google Scholar]
- 18.Jones DT, Kocialkowski S, Liu L, et al. . Tandem duplication producing a novel oncogenic BRAF fusion gene defines the majority of pilocytic astrocytomas. Cancer Res. 2008;68(21):8673-8677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Palanisamy N, Ateeq B, Kalyana-Sundaram S, et al. . Rearrangements of the RAF kinase pathway in prostate cancer, gastric cancer and melanoma. Nat Med. 2010;16(7):793-798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang C, Spevak W, Zhang Y, et al. . RAF inhibitors that evade paradoxical MAPK pathway activation. Nature. 2015;526(7574):583-586. [DOI] [PubMed] [Google Scholar]
- 21.Karoulia Z, Wu Y, Ahmed TA, et al. . An integrated model of RAF inhibitor action predicts inhibitor activity against oncogenic BRAF signaling. Cancer Cell. 2016;30(3):501-503. [DOI] [PubMed] [Google Scholar]
- 22.Flaherty KT, Robert C, Hersey P, et al. ; METRIC Study Group. Improved survival with MEK inhibition in BRAF-mutated melanoma. N Engl J Med. 2012;367(2):107-114. [DOI] [PubMed] [Google Scholar]
- 23.Swaika A, Crozier JA, Joseph RW. Vemurafenib: an evidence-based review of its clinical utility in the treatment of metastatic melanoma. Drug Des Devel Ther. 2014;8:775-787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Héritier S, Emile JF, Barkaoui MA, et al. . BRAF mutation correlates with high-risk Langerhans cell histiocytosis and increased resistance to first-line therapy. J Clin Oncol. 2016;34(25):3023-3030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berres ML, Allen CE, Merad M. Pathological consequence of misguided dendritic cell differentiation in histiocytic diseases. Adv Immunol. 2013;120:127-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hyman DM, Diamond EL, Vibat CR, et al. . Prospective blinded study of BRAFV600E mutation detection in cell-free DNA of patients with systemic histiocytic disorders. Cancer Discov. 2015;5(1):64-71. [DOI] [PMC free article] [PubMed] [Google Scholar]