Abstract
Acquisition of arthroscopic skills is not always easy and can be time-consuming. Simulation in arthroscopy improves surgical skills and can bridge the gap between reduced surgical exposure and training time and the need to reach a required level of competency. We propose a method to create a simple and cost-effective arthroscopic skills simulator using readily available materials and a low-cost Web camera available from online shops. This arthroscopic simulation device can be used to improve skills of all levels of trainees at home, in a bioskills laboratory, or in the theater. It can also be used by experienced surgeons to train with instruments and devices before using them for the first time in theaters, thus ensuring safe use and improving patient safety. Further validation as a training tool is needed and should be the focus of additional research, but early results are very promising.
Advances in medical technology and arthroscopic techniques have allowed more procedures to be performed arthroscopically. Simulation in arthroscopy can improve the skills of surgeons and may serve to bridge the gap between reduced surgical exposure and training time and the need to reach a required level of competency. Simulation was used in the 2015 selection process for a national training number in orthopaedics. A laparoscopic skills trainer was used as part of the clinical skills station.
Errors and failures in surgery can be attributed to lack of training. Medical errors are a problem that requires attention, and every effort to improve training should be implemented.1 Simulation training has been identified as a reliable way to improve orthopaedic training2 and thus improve surgical outcomes. This is also reflected in the public view of simulators; Akhtar et al.3 have reported that no patient would want his or her operation to be performed by a surgeon who did not train on a simulator.
We propose a method to produce a simple and cost-effective training tool that can be used to improve technical skills and help progress training with daily exposure to simulation available either at home, in bioskills laboratories, or in theaters depending on local needs and possibilities.
Technique
For the purpose of creating a cost-effective arthroscopic skills simulator, we used simple and low-cost materials readily available from any hardware store and a low-cost Web camera (iTrust Primo) available from online shops.
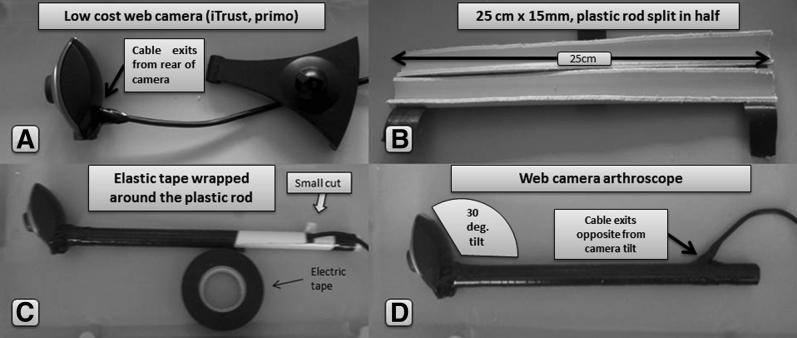
Camera Setup
Any Web camera can be used provided it has at least 640 × 480 hardware resolution and a Universal Serial Bus (USB) 2.0 interface (Table 1, Fig 1). Software to view video in real time and to record the video sequence is always supplied with the camera. A very important feature is to make sure that the USB cable exits from the rear of the camera casing.
Table 1.
Steps to Create Web Camera Arthroscope
| 1. Divide a water pipe into 2 halves (25-cm-long and 15-mm-diameter rigid plastic water pipe). |
| 2. Make a small cut in one of the halves, opposite the camera, about 5 cm from the end. Note that this is where the cable of the camera will exit. |
| 3. Pass the cable of the camera between the 2 halves of the pipe. Note that the camera should firmly attach to one end of the pipe and its cable should exit from the cut created in step 2. |
| 4. By use of electrical tape, reunite the 2 halves of the pipe. Note that tape should be wrapped around the pipe in a continuous fashion starting from the camera end. When approaching the cut, pull firmly on the camera cable exiting from the cut and wrap the tape around it. |
NOTE. Some hints should be noted: Step 4 can be used to customize the Web camera arthroscope using different colored tape; for ours, black was used. In addition, to make the Web camera arthroscope feel more like a real arthroscope, it is necessary for the Universal Serial Bus (USB) cable of the camera to exit from the rear of the casing, if possible, not from the center of it. When one is pulling the cable during step 4, the camera will be forced to tilt relative to the pipe and re-create the 30° field of view from the arthroscope. A camera with the cable exiting from the bottom should not be used because this will sit at a 90° angle to the plastic pipe when attached and will not be able to imitate the arthroscope.
Fig 1.
Steps to create Web camera arthroscope. (A) Camera with Universal Serial Bus (USB) cable exiting from the rear of the casing. (B) Water pipe cut into 2 halves (25-cm-long and 15-mm-diameter rigid plastic water pipe). (C) Small cut opposite the camera about 5 cm from the end. This is where the cable of the camera exits. Electrical tape is used to reunite the 2 halves of the pipe. Tape should be wrapped around the pipe in a continuous fashion starting from the camera end. When one is approaching the cut, he or she should pull firmly on the camera cable exiting from the cut and wrap the tape around it. (D) Camera with tilt relative to the pipe, imitating the arthroscope's field of view. (deg, degrees.)
To create the camera for the simulator, the Web camera is attached to the end of a 25-cm-long and 15-mm-diameter plastic rod. The angle between the camera and rod is 30° in an attempt to imitate the field of view of the arthroscope. The USB cable of the camera exits the plastic rod on the other side of the camera and opposite the 30° inclination in an attempt to imitate the feeling of the arthroscopic camera. The Web camera arthroscope (WCA) can be attached to a laptop computer with a long USB 2.0 cable and generic camera software (AMCap) used in preview mode to view the video from the camera to the screen of the laptop computer.
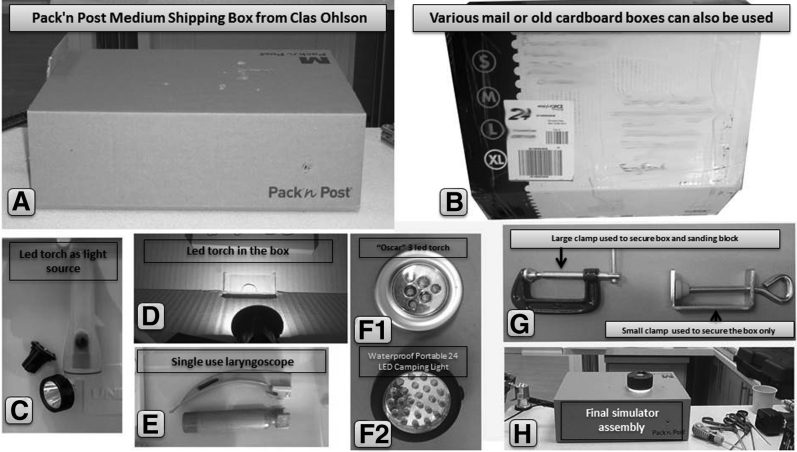
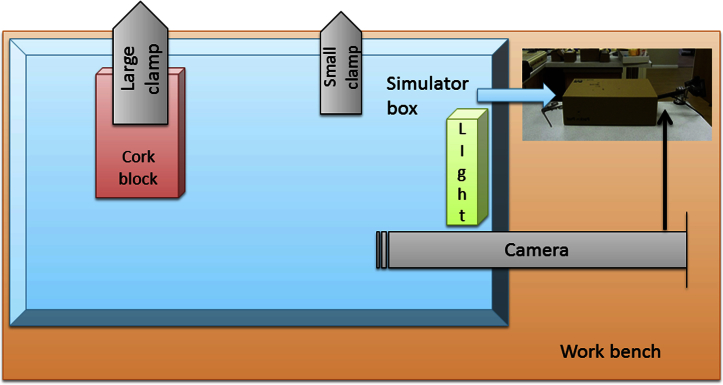
Cardboard Box Setup
Simulation exercises are performed in a cardboard box using the WCA (Table 2, Fig 2). Cardboard is easy to cut and can be pierced with arthroscopic instruments to simulate procedures and improve triangulation skills. A light source is required to be placed inside the box. This can be any light-emitting diode torch or light; it is better to choose a battery-operated device so that the entire construct is safer and easy to move.
Table 2.
Tips to Set Up Cardboard Box
| 1. Various cardboard boxes can be used but we have found 2 that are easy to set up: the medium-size Pack 'n Post shipping box from Clas Ohlson (335 × 250 × 110 mm) and the Brown Single Wall Dispatch Carton from Post Office UK (330 × 254 × 178 mm). |
| 2. The light source can be any battery-powered LED torch; for our system, we used the “waterproof portable 24 LED camping light outdoor LED tent lamp with hanging hook,” available from online shops such as Amazon. This can be placed inside the box and taped to the side where the camera will enter just anterior from the camera cutout in the box. |
| 3. The box must be securely attached to the working surface using C-clamps; 2 are recommended. The box is placed at the edge of the table or working surface along its long axis, and 2 openings are cut: one close to the camera side and one distal. A small clamp (e.g., the Screw Clamp from Clas Ohlson) is used to secure the box to the table proximal to the camera side. A larger clamp (e.g., the 50-mm Cocraft G-Clamp from Clas Ohlson) can be used to secure both the box and the sanding block distal to the camera side. |
LED, light-emitting diode.
Fig 2.
Tips to set up cardboard box. (A) Pack 'n Post shipping box (335 × 250 × 110 mm; Clas Ohlson). (B) Various cardboard boxes can be used. (C) The light source can be a battery-powered light. (D) Torch inside box. (E) A single-use laryngoscope can serve as another light source. (F1) Three light-emitting diode (LED) torch (Oscar). (F2) Waterproof portable 24-LED camping light with hanging hook. (G) Clamps to secure the box. (H) Box with Web camera arthroscope from the side and various instruments that can be used for simulation.
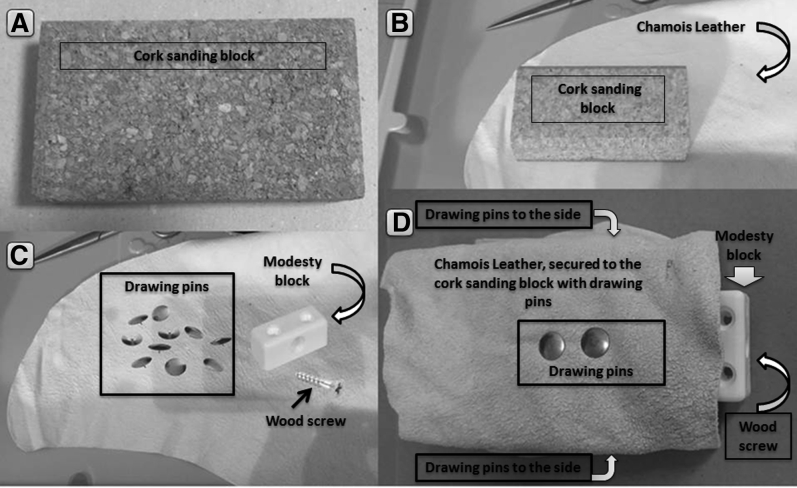
Cork Sanding Block and Chamois Leather
To imitate tissue, a piece of suede cloth is pinned to a cork sanding block (Table 3, Fig 3). This can be used for tissue-handling exercises, bone anchor insertion, knot tying, and use of an arthroscopic punch and arthroscopic manipulator or grasper. Both the box and the block can be secured to any working surface with 2 C-clamps.
Table 3.
Tips to Create Cork Sanding Block and Chamois Leather
| 1. Any cork sanding block can be purchased, even from online shops such as Amazon. The size of our block was 110 × 60 × 30 mm. |
| 2. A small piece is cut from a chamois leather cleaning cloth. It should be slightly larger than the cork block. For the 110 × 60 × 30–mm block, the cloth should be cut to 115 × 80 mm. |
| 3. The cut piece of chamois is placed on the sanding block and attached to the long sides with drawing pins. |
| 4. The cork block with the attached chamois is placed inside the box, with 1 of the 2 open sides toward the wall of the box, aligned with the opening for the C-clamp. A large clamp (50 mm) is used to secure the cork block and the box to the working surface. |
| 5. A screw modesty block is attached to the anterior of the cork block (the side on which the chamois leather is open). This can be used for knot-tying exercises. |
Fig 3.
Steps to create cork sanding block and chamois leather. (A) Cork sanding block measuring 110 × 60 × 30 mm. (B) Small piece to be cut from a chamois leather cleaning cloth slightly larger than the cork block. For the 110 × 60 × 30–mm block, the cloth should be cut to 115 × 80 mm. (C) Chamois leather, drawing pins, modesty block, and wood screw. (D) Chamois leather attached to the sanding block with drawing pins and modesty block screwed to the anterior of the cork block.
Suggested Exercises
After the creation of the WCA, exercises to improve hand-eye coordination and improve arthroscopic skills were designed (Table 4).
Table 4.
Suggested Exercises
| Exercises | Skills Improved |
|---|---|
| Line and shape tracing | 2-dimensional hand coordination and hand-eye dissociation |
| Building blocks | 3-dimensional triangulation, hand-eye dissociation, and object handling using arthroscopic grasper |
| Exercises with sanding block and chamois leather | Triangulation and training in specific tasks depending on needs |
| Knot tying using modesty block | Arthroscopic knot tying |
| Suture anchor insertion | Use of anchor before application in theater; training of trainee on use of implants used in real surgery |
| Punch or grabber on chamois leather | Safe training of tissue handling |
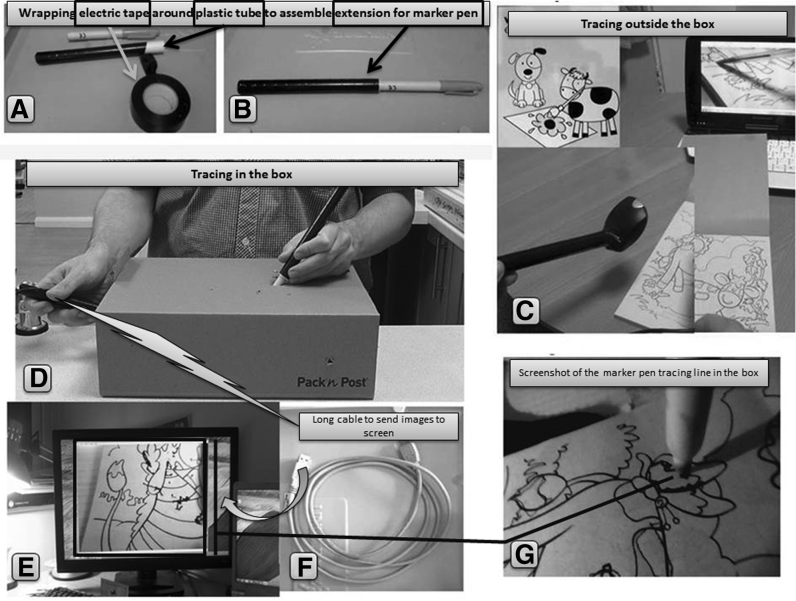
Line and Shape Tracing
For the basic entry-level exercises, the WCA is placed inside the box and a marker pen is attached to the end of another 25-cm plastic rod (Figs 4 and 5). Tracing exercises can be performed outside the box and then inside the box using a tracing book initially. Paper with 4 different shapes (line, triangle, circle, and square) (Fig 5) can then be placed inside the box, and the trainee tries to trace the lines and shapes while looking at the laptop computer screen.
Fig 4.
Drawing tasks. (A, B) A piece of a water pipe is wrapped with electrical tape and attached to the end of a marker pen. (C) Tracing shapes outside the box. (D) Tracing shapes inside the box. (E, F) Images can be sent to a monitor using a long Universal Serial Bus (USB) cable. (G) View from inside the box, showing tracing of objects in a coloring book.
Fig 5.
Shapes for tracing.
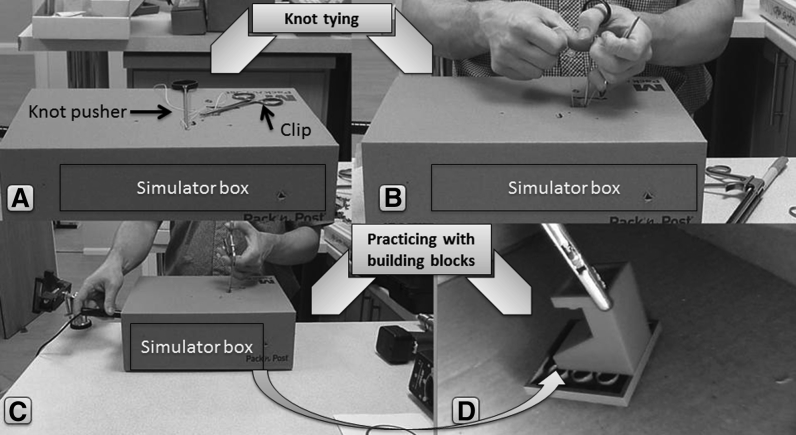
Building Blocks
To improve skills in 3 dimensions, the trainee, using an arthroscopic grabber, tries to build 4 layers of building blocks (Fig 6).
Fig 6.
Additional tasks. (A) Preparation for knot tying. (B) Knot-tying training using box. (C) Block building, viewed from outside. (D) Finished building blocks.
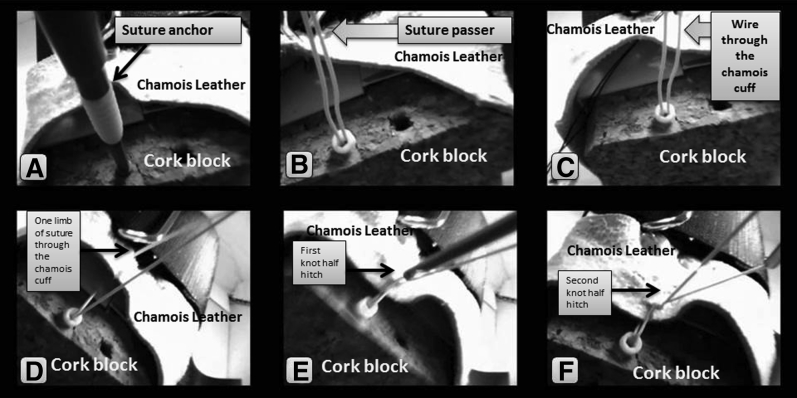
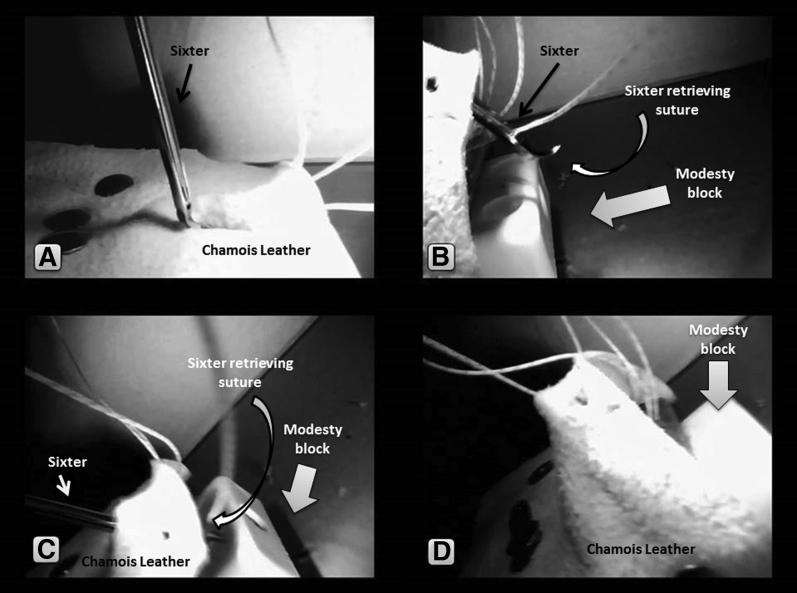
Exercises With Sanding Block and Chamois Leather
Using the cork block, the trainee can practice various surgical techniques including inserting suture anchors, passing sutures through tissues, tying knots, using the punch, or placing arthroscopic sutures (Figs 6 and 7). A variety of instruments and implants were used with the cork block including Sixter penetrating graspers (TAG Medical Products, Kibbutz Gaaton, Israel; DePuy Mitek, Warsaw, IN). Use of the Sixter requires skills and can be difficult if not familiar with the instrument. With the help of the simulator, trainees are able to improve their skills under safe and controlled conditions (Fig 8). The block can also be used by more senior surgeons to practice techniques with materials and instruments.
Fig 7.
Cuff repair task. (A) Anchor insertion into cork block. (B) Suture passer through chamois cuff. (C) Wire through chamois cuff. (D) One limb of suture through chamois cuff. (E) First knot half-hitch. (F) Second knot half-hitch.
Fig 8.
Sixter task. (A) Passing of Sixter through chamois cuff. (B) Suture retrieval. (C) Suture passing through chamois cuff, with wire through chamois cuff. (D) One limb of suture through chamois cuff using Sixter.
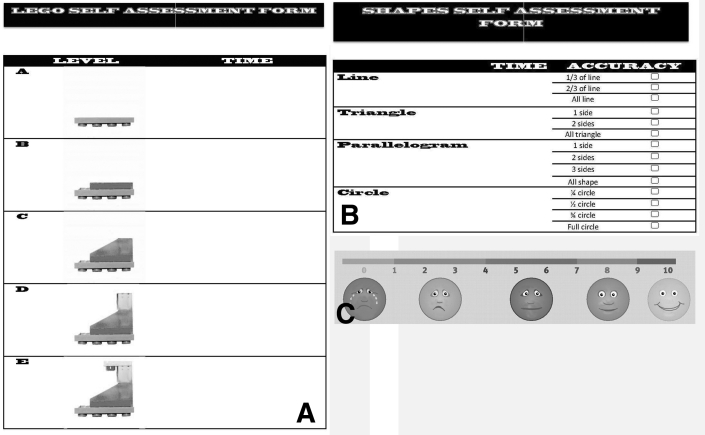
Self-Assessment
A self-assessment form was created for all simulated skills, and the time and ease of completion and self-reported subjective ease during surgery can be recorded by the trainee (Fig 9, Video 1).
Fig 9.
Self-assessment forms. (A) Block building. (B) Shape tracing. (C) Self-reported subjective ease during surgery.
Discussion
Alvand et al.4 suggested that some individuals have an innate ability to learn arthroscopic skills but others need focused training for them to progress and therefore arthroscopic skills are like many other learned skills. There may be a limitation as to how realistic simulation is compared with performing surgery, but it allows trainees to obtain familiarity with equipment and a basic skill set before performing procedures on patients. Simulation training became initially popular in laparoscopic residency programs, and significant improvements in all skills were evident in residents exposed to simulation skills training complementing traditional exposure to procedures in the operating room. Successful integration of simulators in surgery has created the need for similar methods to be included in orthopaedic training programs.5 Interest in simulation in orthopaedics has significantly increased, and a search of PubMed for the term “arthroscopic skills” retrieved 10 articles on simulation in the first quarter of 2016.
Obtaining arthroscopic skills can be challenging but is essential for orthopaedic surgeons. Despite the fact that reported arthroscopic complication rates are low,6 even a complication rate of 1% would amount to 10,000 complications in the United States alone given the large number of procedures performed. Moreover, errors during surgery not only result in complications but may lead to an unsatisfactory outcome or may significantly increase operating time and reduce productivity.
Errors can be attributed to knowledge or skills.7 Skills can be evaluated by task time, task repetition, misplaced position, dropped objects during the procedure, 3-dimensional depth perception, and volume and economy of motion.7 The most commonly reported skill-evaluating outcome of simulation is time to perform the task.8 Simulation can be used to improve both skills and knowledge and decrease the time required to obtain the necessary skills to perform arthroscopic procedures. Anatomic virtual-reality simulators can improve knowledge, technical simulators such as ours can improve skills, and cadaveric surgery can improve both knowledge and skills.
Recent research has shown that proficiency-based progression training can gradually replace the older apprenticeship model.9 Simulation can improve the skills of all levels of trainees, but it has to be part of a formal training curriculum with specific skills and assessments.10 In a recent study Angelo et al.11 have shown that simulation alone is not enough. When 3 groups of trainees performing an arthroscopic Bankart repair were compared, the trainees exposed to simulation were 1.4 times more likely to achieve the final benchmark but the group receiving proficiency-based progression training was 7.5 times more likely to successfully complete the repair.
Improvement in arthroscopic dexterity has been measured by global rating scales and motion analysis, and significant correlation between virtual-reality and bench-top knee arthroscopy simulators has been measured.12 The more basic and simple the simulator, the easier it would be to incorporate it into everyday training.13 Another very important aspect of training is maintaining the skills achieved with simulation or any other form of skills development. It has been proved that although exposure to simulation increases the skills of trainees after 1 year, this effect has been lost.14 It is therefore crucial that any type of simulation should ideally be simply and easily available for continuing training and not a one-off laboratory encounter with a complex virtual-reality device.
Continual development of skills and ease of use are the main advantages of the simulation device we propose. Triangulation skills and hand-eye coordination15 are very important basic arthroscopic skills and form part of all basic arthroscopic skills simulation and training programs. In addition, haptic feedback is very important for training and our simulator provides this without the use of complex electronics. Similar simple devices have already been reported for use in laparoscopic surgery16; however, our WCA has the advantage of mimicking the 30° of an arthroscopic camera and providing the experience of using the arthroscope to explore the space and the feeling of having to turn the camera cable opposite the field of view to visualize items during training.
Braman et al.13 have developed a basic arthroscopic simulator based on similar principles, but the advantage of our device is that it can be created by any trainee and is very inexpensive to use and replace. It is therefore simpler to incorporate into any training program or even use at home to maintain acquired skills. Validated skills of triangulation and object manipulation13 can be acquired with our device. In addition, all 6 basic arthroscopic tasks using the box model reported by Coughlin et al.17 can be performed with our simulator: (1) probing, (2) grasping, (3) tissue resection, (4) shaving, (5) tissue liberation and suture passing, and (6) knot tying. Dal Molin et al.,18 using the Shoulder Arthroscopy Model (Sawbones Europe) and video arthroscopy, showed significant improvement in triangulation skills, time to complete skills, and volume and economy of motion. Patient safety can be improved using simulation even for simpler procedures such as diagnostic shoulder arthroscopy.8 In a recent review study, Aïm et al. evaluated 10 trials involving 303 participants and concluded that virtual-reality simulation can lead to improvement in arthroscopic skills.19 Furthermore, Boutefnouchet and Laios concluded, after identifying 2 randomized controlled trials, that arthroscopic skills achieved with computer simulation can be transferred to the operating theater.20
Building our simulator is simple and easy (Fig 10). It can be used at home, in a bioskills laboratory, or in the theater to improve skills. The simulator has not been validated as a training tool but has been used by trainees to improve skills during their fellowships.
Fig 10.
How to assemble all parts of simulator.
A disadvantage meriting mention is the fact that some do-it-yourself and technical skills are needed to build the simulator, which is not anatomic (Table 5). Even though basic training can be performed, with inexpensive materials, to practice advanced techniques, suture anchors from industry for demonstration purposes and real arthroscopic instruments are needed. Advantages of our simulator are that it is very inexpensive and relatively easy to build with readily available materials. It permits real instruments and implants to be used and tested before live surgery and can improve triangulation skills. Feeling and force reaction mimic reality. The main advantage is that every trainee can build a simulator and improve skills either using our suggested tasks or even improvising with his or her own techniques. Further validation of the simulator's as a training tool is needed and is the focus of additional research, but early results are very promising.
Table 5.
Advantages and Disadvantages
| Advantages |
| The simulator is inexpensive. |
| The simulator is easy to build and set up, all materials are readily available, and trainees can make their own simulation box. |
| Real instruments can be used. |
| The feeling and force are similar to reality. |
| Triangulation skills are acquired. |
| Disadvantages |
| To practice advanced techniques, suture anchors from industry for demonstration purposes are needed. |
| Some do-it-yourself and technical skills are required to assemble the simulator. |
| There is a need for arthroscopic instruments for more complicated skills. |
| Simulation is nonanatomic. |
| Simulation is performed using a dry simulator. |
Our arthroscopic simulation device can be used to improve skills of all levels of trainees. It can also be used by experienced surgeons to train with techniques, instruments, and devices before using them for the first time in the theater, thus ensuring safe use and improving patient safety.
Acknowledgment
The authors thank Simon Cliff for his technical support during the creation of the arthroscopic camera.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Advice on how to build the simulator is presented. The materials used and methods of building are described. The shape-tracing exercise is displayed, followed by block building. Two advanced techniques are shown: cuff repair using Sixters and knot tying. The self-assessment forms are shown.
References
- 1.Harris J.D., Staheli G., LeClere L., Andersone D., McCormick F. What effects have resident work-hour changes had on education, quality of life, and safety? A systematic review. Clin Orthop Relat Res. 2015;473:1600–1608. doi: 10.1007/s11999-014-3968-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cannon W.D., Garrett W.E., Jr., Hunter R.E. Improving residency training in arthroscopic knee surgery with use of a virtual-reality simulator. A randomized blinded study. J Bone Joint Surg Am. 2014;96:1798–1806. doi: 10.2106/JBJS.N.00058. [DOI] [PubMed] [Google Scholar]
- 3.Akhtar K., Sugand K., Wijendra A., Standfield N.J., Cobb J.P., Gupte C.M. Training safer surgeons: How do patients view the role of simulation in orthopaedic training? Patient Saf Surg. 2015;9:11. doi: 10.1186/s13037-015-0058-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alvand A., Auplish S., Gill H., Rees J. Innate arthroscopic skills in medical students and variation in learning curves. J Bone Joint Surg Am. 2011;93:e115(1-9). doi: 10.2106/JBJS.K.00199. [DOI] [PubMed] [Google Scholar]
- 5.Tay C., Khajuria A., Gupte C. Simulation training: A systematic review of simulation in arthroscopy and proposal of a new competency-based training framework. Int J Surg. 2014;12:626–633. doi: 10.1016/j.ijsu.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 6.Dodds J.A. But I don't have any complications. Sports Med Arthrosc. 2013;21:61. doi: 10.1097/JSA.0b013e318291b175. [DOI] [PubMed] [Google Scholar]
- 7.Karahan M., Kerkhoffs G.M.M.J., Randelli P., Tuijthof G. Springer; Berlin: 2014. Effective training of arthroscopic skills. [Google Scholar]
- 8.Waterman B.R., Martin K.D., Cameron K.L., Owens B.D., Belmont P.J., Jr. Simulation training improves surgical proficiency and safety during diagnostic shoulder arthroscopy performed by residents. Orthopedics. 2016;39:e479–e485. doi: 10.3928/01477447-20160427-02. [DOI] [PubMed] [Google Scholar]
- 9.Lubowitz J.H., Provencher M.T., Brand J.C., Rossi M.J. The apprenticeship model for surgical training is inferior. Arthroscopy. 2015;31:1847–1848. doi: 10.1016/j.arthro.2015.07.014. [DOI] [PubMed] [Google Scholar]
- 10.Safir O., Dubrowski A., Mirsky L., Lin C., Backstein D., Carnahan H. What skills should simulation training in arthroscopy teach residents? Int J Comput Assist Radiol Surg. 2008;3:433–437. doi: 10.1007/s11548-013-0833-7. [DOI] [PubMed] [Google Scholar]
- 11.Angelo R.L., Ryu R.K., Pedowitz R.A. A proficiency-based progression training curriculum coupled with a model simulator results in the acquisition of a superior arthroscopic Bankart skill set. Arthroscopy. 2015;31:1854–1871. doi: 10.1016/j.arthro.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 12.Chang J., Banaszek D.C., Gambrel J., Bardana D. Global rating scales and motion analysis are valid proficiency metrics in virtual and benchtop knee arthroscopy simulators. Clin Orthop Relat Res. 2016;474:956–964. doi: 10.1007/s11999-015-4510-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Braman J.P., Sweet R.M., Hananel D.M., Ludewig P.M., Van Heest A.E. Development and validation of a basic arthroscopy skills simulator. Arthroscopy. 2015;31:104–112. doi: 10.1016/j.arthro.2014.07.012. [DOI] [PubMed] [Google Scholar]
- 14.Dunn J.C., Belmont P.J., Lanzi J. Arthroscopic shoulder surgical simulation training curriculum: Transfer reliability and maintenance of skill over time. J Surg Educ. 2015;72:1118–1123. doi: 10.1016/j.jsurg.2015.06.021. [DOI] [PubMed] [Google Scholar]
- 15.Burden C., Fox R., Lenguerrand E., Hinshaw K., Draycott T.J., James M. Curriculum development for basic gynaecological laparoscopy with comparison of expert trainee opinions; prospective cross-sectional observational study. Eur J Obstet Gynecol Reprod Biol. 2014;180:1–7. doi: 10.1016/j.ejogrb.2014.05.036. [DOI] [PubMed] [Google Scholar]
- 16.van Duren B.H., van Boxel G.I. Use your phone to build a simple laparoscopic trainer. J Minim Access Surg. 2014;10:219–220. doi: 10.4103/0972-9941.141534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Coughlin R.P., Pauyo T., Sutton J.C., III, Coughlin L.P., Bergeron S.G. A validated orthopaedic surgical simulation model for training and evaluation of basic arthroscopic skills. J Bone Joint Surg Am. 2015;97:1465–1471. doi: 10.2106/JBJS.N.01140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dal Molin F.F., Mothes F.C., Feder M.G. Effectiveness of the videoarthroscopy learning process in synthetic shoulder models. Rev Bras Ortop. 2012;47:83–91. doi: 10.1016/S2255-4971(15)30350-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aim F., Lonjon G., Hannouche D., Nizard R. Effectiveness of virtual reality training in orthopaedic surgery. Arthroscopy. 2016;32:224–232. doi: 10.1016/j.arthro.2015.07.023. [DOI] [PubMed] [Google Scholar]
- 20.Boutefnouchet T., Laios T. Transfer of arthroscopic skills from computer simulation training to the operating theatre: A review of evidence from two randomised controlled studies. SICOT J. 2016;2:4. doi: 10.1051/sicotj/2015039. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Advice on how to build the simulator is presented. The materials used and methods of building are described. The shape-tracing exercise is displayed, followed by block building. Two advanced techniques are shown: cuff repair using Sixters and knot tying. The self-assessment forms are shown.